Markovchick Vincent J., Pons Peter T., Bakes Katherine M.(ed.) Emergency medicine secrets. 5th ed
Подождите немного. Документ загружается.

Chapter 19 LOW BACK PAIN128
15. What happens to patients with LBP when they leave the ED?
The prognosis for patients having a first episode of mechanical LBP is good: 70% are better
by 1 week, 80% by 2 weeks, and 90% by 1 month. Most studies comparing medical
management, chiropractic manipulation, and other treatment modalities rarely find significant
differences in long-term outcome because almost everyone gets better no matter what you do.
Patients who do not improve with conservative management may have significant medical
disorders (e.g., inflammatory disorders, malignancy, infections, or disk disease) that were not
apparent at the time of initial evaluation or, alternatively, may suffer from psychiatric
disorders, drug dependence, or job dissatisfaction.
BIBLIOGRAPHY
1. Anderson GBJ: Epidemiological features of chronic low-back pain. Lancet 354:581–585, 1999.
2. Atlas SJ, Nardin RA: Evaluation and treatment of low back pain: An evidence-based approach to clinical care.
Muscle Nerve 27:265–284, 2003.
3. Chou R, Qaseem A, Snow V, et al: Diagnosis and treatment of low back pain: a joint clinical practice guideline
from the American College of Physicians and the American Pain Society. Ann Intern Med 147(2): 478–491,
2007.
4. Chou R, Huffman LH: Nonpharmacologic therapies for acute and chronic low back pain: a review of the
evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern
Med 147:492–504, 2007.
5. Cohen SP, Argoff CE, Carragee EJ: Management of low back pain. BMJ 338:100–106, 2009.
6. Devereaux M: Low back pain. Med Clin North Am 93(2): 477–501, 2009.
7. Deyo RA, Weinstein JN: Low back pain. N Engl J Med 344:363–370, 2001.
8. Hagen KB, Hilde G, Jamtvedt G, et al: Bed rest for acute low-back pain and sciatica. Cochrane Database
System Rev DOI: 10.1002/14651858.CD001254.pub2, 2004.
9. King HA: Back pain in children. Orthop Clin North Am 30:467–474, 1999.
10. van Tulder MW, Touray T, Furlan AD, et al: Muscle relaxants for non-specific low-back pain. Cochrane
Database System Rev DOI: 10.1002/14651858.CD004252, 2003.
129
III. NONTRAUMATIC ILLNESS
CHAPTER 20
NONTRAUMATIC OCULAR EMERGENCIES
Martin R. Huecker, MD, and Daniel F. Danzl, MD
1. What are some tricks to evaluate the red eye?
Always document near or far visual acuity in each eye independently. Topical application of
anesthetic drops should decrease or eradicate pain secondary to an abrasion or conjunctivitis
(not so with iritis or glaucoma). Redness at the corneal-scleral junction (perilimbic flush)
suggests iritis or glaucoma. Shining a light into the normal eye should make the opposite eye
hurt if the patient has iritis (because of consensual movement of the inflamed affected
contralateral iris). In addition to the consensual pupillary reflex test, the accommodative test is
suggestive, which is simply pain precipitated by accommodation. Pain with either maneuver
suggests ciliary spasm.
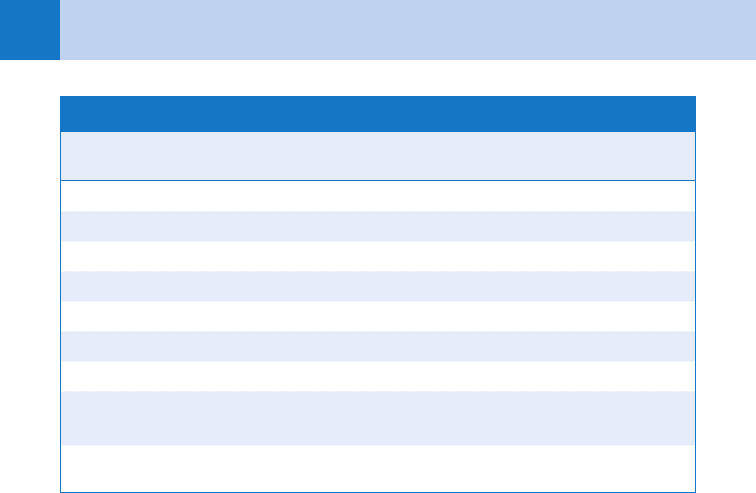
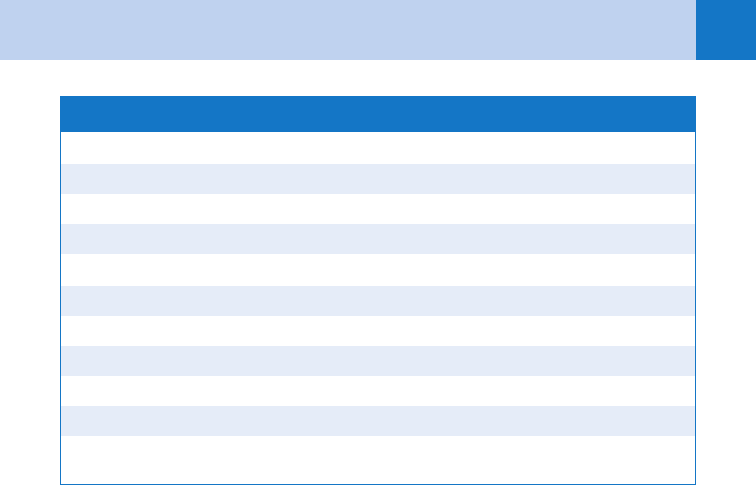
2. What typical findings help with the differential diagnosis of the red eye?
See Table 20-1.
3. What is conjunctivitis?
Inflammation of the bulbar and palpebral conjunctivae or mucous membranes. Viral
conjunctivitis is usually bilateral with clear epiphora or tearing and may be associated with an
upper respiratory infection (URI). A preauricular node suggests epidemic keratoconjunctivitis
(adenovirus). Two common viral pathogens are herpes simplex, with dendritic ulcers, and
herpes zoster, with involvement of the fifth cranial nerve. Ocular zoster is suggested by
involvement of the nasociliary branch of V
1,
manifested by lesions on the tip of the nose
(Hutchinson’s sign).
Bacterial conjunctivitis initially may be unilateral with purulent crusty drainage. Always
consider an undiagnosed foreign body with unilateral conjunctivitis. Chlamydia or Gonococcus
should be considered in neonates or adults with sexually transmitted diseases. Allergies may
cause papillae under the lids, chemosis, and itching.
4. How is conjunctivitis treated?
Common agents include aminoglycoside drops and sulfacetamide; the latter stings, which can
decrease compliance. Erythromycin 0.5% is available only in ointment form. Reserve the
topical fluoroquinolones for more severe infections and for contact lens wearers who are at
risk for Pseudomonas. Avoid neomycin because hypersensitivity reactions are common.
5. What is endophthalmitis?
Infection or inflammation within the globe. It usually is seen as a collection of pus in the
anterior chamber (hypopyon) that resembles a dependent meniscus similar to the blood
collection in a hyphema. Antecedent causes include corneal ulcers, direct inoculation or
hematogenous spread, and conjunctivitis with organisms capable of penetrating the cornea
(e.g., Neisseria gonorrhoeae, Corynebacterium, Listeria, or Haemophilus aegyptius).
6. What is the difference between periorbital and orbital cellulitis?
Periorbital (preseptal) cellulitis is soft-tissue infection of eye structures anterior to the tarsal
plate, usually localized to the eyelids and conjunctivae. Orbital cellulitis is a more serious
infection (behind the septum) that involves posterior eye structures. Both tend to be unilateral
and may be preceded by trauma and upper respiratory, sinus, or dental infections. Orbital
Chapter 20 NONTRAUMATIC OCULAR EMERGENCIES130
cellulitis is most often the result of direct spread from ethmoid sinusitis, whereas periorbital
cellulitis usually is caused by hematogenous spread of bacteria.
7. How do I differentiate clinically between periorbital and orbital cellulitis?
The two may be difficult to distinguish clinically, especially in children. Periorbital cellulitis
tends to cause local eyelid symptoms and occasionally ocular discharge and may be
associated with fever or leukocytosis. Visual acuity and pupillary reflexes are normal.
Orbital cellulitis may present with all of the previous symptoms plus exophthalmos, fever,
and pain with extraocular movements. Decreased visual acuity, loss of sensation over the
ophthalmic and maxillary branches of the trigeminal nerve in V
1
and V
2
(division of cranial
nerve V), and increased intraocular pressure are uncommon findings. Contrast computed
tomography (CT) scanning of the orbit is liberally indicated with periorbital swelling when
there is a possibility of postseptal infection.
8. What is the common clinical presentation of cavernous sinus thrombosis?
Patients often progress from fever, headache, and chemosis to ophthalmoplegia,
exophthalmos, and altered level of consciousness. Paralysis of cranial nerves III, IV, and VI
is usually noted. In exophthalmos, the sclera is visible above and below the cornea. Magnetic
resonance imaging (MRI) is indicated.
9. Describe the clinical presentation of iritis.
Patients often present with perilimbic injection, ciliary spasm, and a constricted miotic pupil. Iritis
can be bilateral and misdiagnosed as conjunctivitis. Perform a slit lamp examination of the anterior
chamber for cells, flare, and for keratotic precipitates (white cells) on the back of the cornea.
10. How is iritis treated?
Iritis is treated with systemic analgesics and a topical cycloplegic, not simply a mydriatic, to
paralyze accommodation and dilate the iris. This prevents adhesions between the iris and the
lens (posterior synechiae). Consider steroids in consultation with an ophthalmologist.
11. What is acute angle-closure glaucoma?
Glaucoma is optic nerve damage from increased intraocular pressure. In a patient with a
narrow anterior chamber angle, reduced illumination causes mydriasis; folds of the peripheral
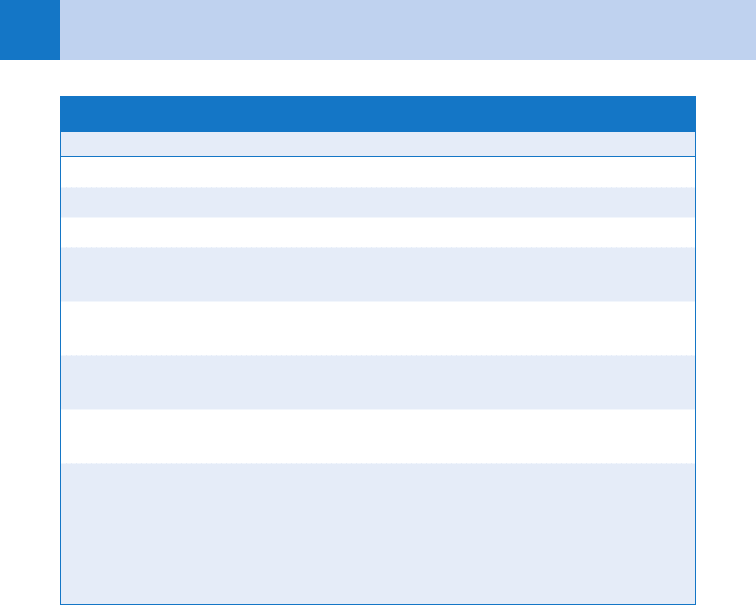
TABLE 20-1. DIFFERENTIAL DIAGNOSIS OF THE RED EYE
Conjunctivitis Acute Iritis
Angle-Closure
Glaucoma
Incidence Extremely common Common Uncommon
Discharge Moderate to copious Reflex epiphora None
Vision Normal Slightly blurred Very blurred (halos)
Pain Gritty Moderate Severe
Conjunctival injection Diffuse Perilimbic Perilimbic
Cornea Clear Keratotic precipitates Steamy or hazy
Pupil size Normal Constricted or dilated Dilated
Pupillary light
response
Normal Poor and painful Poor
Intraocular pressure Normal Normal Elevated
Chapter 20 NONTRAUMATIC OCULAR EMERGENCIES 131
iris can block the angle, which prevents aqueous humor outflow. The rapid elevation of
intraocular pressure causes a hazy cornea, ciliary flush, firm globe, and optic nerve damage if
not treated promptly. The diagnosis may be delayed by the misleading systemic complaints of
nausea, vomiting, and abdominal pain.
12. How is acute angle-closure glaucoma treated?
Acute glaucoma is treated with intravenous mannitol or glycerol to decrease intraocular pressure
by osmotic diuresis, topical miotics (i.e., 2% pilocarpine or 0.5% timolol) if not contraindicated to
decrease pupil size and increase aqueous outflow, and acetazolamide intravenously to decrease
aqueous production. Topical sympathomimetics such as apraclonidine also reduce aqueous
humor production. Emergent ophthalmologic consultation is indicated.
13. What is a subconjunctival hemorrhage?
Subconjunctival hemorrhage occurs when a blood vessel ruptures under the conjunctiva.
Without trauma, it often results from a Valsalva maneuver associated with coughing or
vomiting. Reassure the patient that vision will not be affected and that the blood will be
absorbed over 10 to 14 days. Patients on anticoagulants should have their international
normalized ratio (INR) measured.
14. What are some common diseases of the cornea?
Ulcerations are often surrounded by a cloudy white cornea. Emergent ophthalmologic
recommendations often include a topical fluoroquinolone, such as moxifloxacin.
A pterygium is a wedge of conjunctival fibrovascular tissue that extends over the cornea,
unlike a pinguecula. Both are benign and can be electively excised.
15. What are some of the unique issues regarding ophthalmologic
pharmacology?
Topical agents may have systemic effects, so exercise caution when prescribing b-blockers,
vasoconstrictors, and anticholinergics. Ointments have a longer duration of action, but blur
vision. Generally wait 10 minutes before instilling different drops.
Diagnostic medications include stains, such as fluorescein, that help identify corneal
and conjunctival abnormalities, and topical anesthetics, which should never be dispensed.
Nonsteroidal anti-inflammatory drugs, such as ketorolac or diclofenac, are useful for pain
relief. Topical corticosteroids should generally be used after consultation with an
ophthalmologist.
Miotic eye drop bottles have green tops, and mydriatic/cycloplegic agents have red tops. Never
allow Hemoccult® drops (yellow or blue top) in an eye room because severe alkali burns can occur.
Some patients will present with a pupil dilated from a medication. If 1% pilocarpine fails
to constrict the pupil, it is pharmacologically blocked, most commonly by phenylephrine,
handling a scopolamine patch, or aerosolized anticholinergics/b-agonists. Other causes of a
unilateral dilated pupil include post-traumatic mydriasis, third nerve palsy, or a normal variant.
16. Name some of the considerations involving pupillary dilation.
Phenylephrine (2.5%) is a direct sympathomimetic and mydriatic. Dilation may last 4 hours,
and patients with a shallow anterior chamber may develop acute glaucoma after leaving the ED.
Pupils generally do not require dilation in the ED. A panoptic ophthalmoscope provides a five
times larger view of the undilated fundus. For short-term cycloplegia, consider tropicamide
(1–6 hours) or 2% to 5% homatropine (1–2 days); never use atropine (1–3 weeks).
17. What does the presence of an afferent pupillary defect (APD), also known as a
Marcus Gunn pupil, indicate?
If the patient has an APD, it confirms damage in the retina or optic nerve. To perform the
swinging flashlight test, swing the light after several seconds from the normal eye to the other
eye. After a brief pupillary constriction in the abnormal eye, the redilation in response to light
reflects afferent deprivation; response may only be appreciated in a dark room.
Chapter 20 NONTRAUMATIC OCULAR EMERGENCIES132
KEY POINTS: COMMON CAUSES OF AN APD
1. Central retinal artery occlusion
2. Central retinal vein occlusion
3. Optic neuritis
4. Retrobulbar neuritis
18. In a patient with anisocoria, how does one determine which pupil is
abnormal?
Begin the examination in a darkened room; if there is more anisocoria in the light, the large pupil
is failing to constrict and is abnormal. More anisocoria that develops going into the dark indicates
that the miotic pupil is failing to dilate. Never just assume that the larger pupil is abnormal.
KEY POINTS: COMMON CAUSES OF ANISOCORIA
1. Horner’s syndrome
2. Argyll-Robertson pupil
3. Adie’s pupil
4. Post-traumatic or medication-induced mydriasis
5. Third nerve palsy
19. What are common causes of a miotic pupil?
The two most common are Horner’s syndrome and an Argyll-Robertson pupil. The clinical
manifestations of Horner’s syndrome include ptosis, miosis, and anhydrosis (in a cold ED,
check for dilated conjunctival vessels). Bronchogenic carcinoma, stroke, and brachial plexus
pathology may present with Horner’s syndrome.
The Argyll-Robertson pupil is miotic and irregular, and displays light-near dissociation.
The pupil constricts to accommodation but not to light. This finding is common with diabetes
and syphilis. A common testing error is to hold and shine a penlight directly in front of the
eye, which can cause the pupil to constrict from accommodation, not light.
20. Is there another cause of light-near dissociation?
The only other cause is Adie’s pupil, which results from idiopathic parasympathetic denervation in
the ciliary ganglion in the eye. The patient is often a young female with a mydriatic pupil that
accommodates but does not react to light. Herpes zoster is another cause of Adie’s pupil. There
are no diseases that cause a pupil to react to light but fail to accommodate.
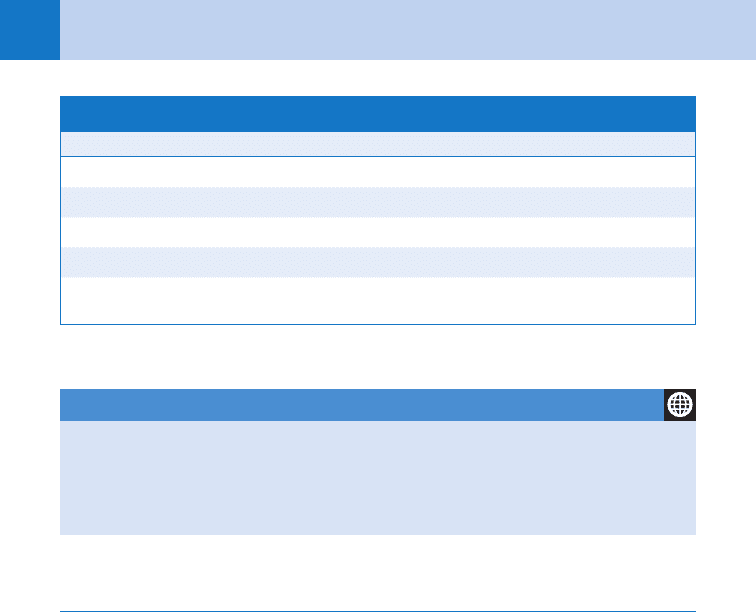
21. What are some common causes of nontraumatic loss of vision?
See Table 20-2.
22. Describe the presentation and treatment of central retinal artery and central
retinal vein occlusion.
Both occur in middle-aged atherosclerotic patients or elderly hypertensive patients and
present as sudden painless loss of vision. Embolic occlusion of the retinal artery or its
branches results in a dilated nonreactive pupil with an APD on the affected side. The retina is
Chapter 20 NONTRAUMATIC OCULAR EMERGENCIES 133
pale with a cherry-red spot at the macula (macular blood supply is from the choroidal
circulation). Occasionally, amaurosis fugax precedes central retinal artery occlusion. The
funduscopic examination of an ischemic central retinal vein occlusion is described as a blood
and thunder fundus because of the presence of multiple large hemorrhages. Efforts to
decrease intraocular pressure and dilate retinal vessels by increasing the pCO
2
(e.g., paper
bag or carbogen), and globe massage are rarely useful acutely for arterial occlusions.
Prognosis for both entities is poor.
23. What are other causes of sudden painless monocular loss of vision?
Suspect vitreous hemorrhage in diabetics with an obscured red reflex and retinal details.
Nontraumatic retinal detachments are more common in patients with significant myopia.
Patients often see flashing lights or a falling curtain. Most commonly, patients report dark
floating spots or floaters, which reflect vitreous separations and not a retinal detachment.
24. How do optic neuritis and papilledema differ?
Although these two processes appear similar on funduscopic examination, optic neuritis
involves focal demyelination of the optic nerve, resulting in a hyperemic nerve head
developing over hours to days. The average age of onset is in the thirties, and there is a 40%
association with multiple sclerosis.
Papilledema is swelling of the optic disc caused by increased intracranial pressure. It is
usually bilateral but may be asymmetric and may be the result of brain abscess or tumor,
intracranial bleeding, meningitis or encephalitis, hydrocephalus, severe hypertension, or
pseudotumor cerebri. The earliest sign of papilledema is the loss of spontaneous venous
pulsations normally present in 75% of patients. When difficult to appreciate, they can be
elicited with ipsilateral jugular compression. (See Table 20-3.) Bedside ocular ultrasonography
can facilitate the diagnosis of vitreous hemorrhage, a detached retina, and increased
intracranial pressure (nerve sheath diameter).
25. What are a couple of tricks to prove that a patient can see?
Induce nystagmus by spinning an opticokinetic drum, or simply hold a mirror in front of the
eyes and slowly move it—tracking requires vision.
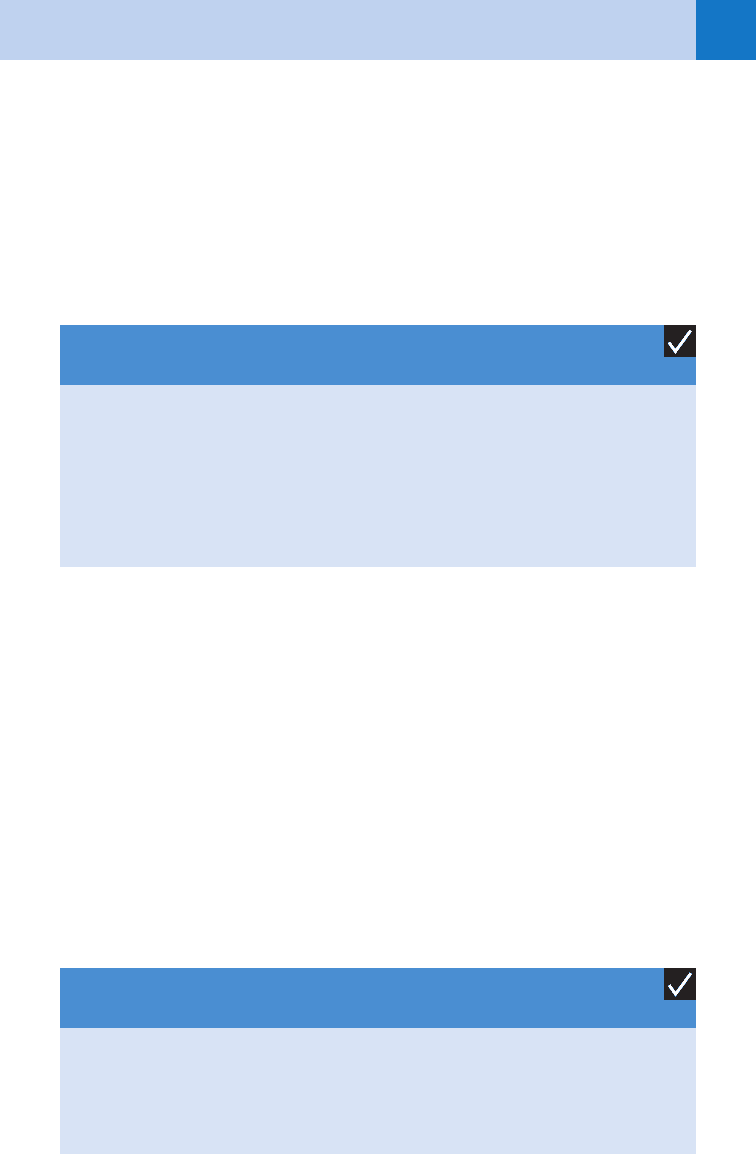
TABLE 20-2. COMMON CAUSES OF NONTRAUMATIC LOSS OF VISION
Transient monocular Acute binocular
Amaurosis fugax Migraine
Temporal arteritis Vertebral basilar insufficiency
Migraine Cerebrovascular disease
Persistent monocular or binocular Toxins (e.g., methanol, salicylates, quinine)
Central retinal artery occlusion Hysteria
Central retinal vein occlusion Malingering
Retinal detachment or hemorrhage
Vitreous or macular hemorrhage
Optic or retrobulbar neuritis
Macular degeneration
Chapter 20 NONTRAUMATIC OCULAR EMERGENCIES134
TABLE 20-3. OPTIC NEURITIS VERSUS PAPILLEDEMA
Optic Neuritis Papilledema
Pupil reactivity Slow Normal
Visual acuity Decreased Normal
Ocular pain Present Absent
Usual localization Unilateral Bilateral
Fundus Blurred disc margins Blurred disc margins
WEBSITES
1. www.redatlas.org
2. www.atlasophthalmology.com
3. www.uptodate.com
BIBLIOGRAPHY
1. American Academy of Ophthalmology, Bradford CA, editors: Basic ophthalmology, ed 8, San Francisco, 2004,
American Academy of Ophthalmology.
2. Ehlers JP, Shah CP, Fenton GL, et al: The wills eye manual: office and emergency room diagnosis and treatment
of eye disease, ed 5, Philadelphia, 2008, Lippincott Williams & Wilkins.
3. Marx J, Hockberger R, Walls R: Rosen’s emergency medicine, ed 7, St. Louis, 2009, Mosby.
135
CHAPTER 21
NONTRAUMATIC ENT EMERGENCIES
Christopher Davis, MD, and Katherine M. Bakes, MD
EPISTAXIS
1. What are the most common causes of epistaxis?
Nosebleeds usually occur spontaneously, often secondary to dry nasal mucosa or
infection. Infectious causes are most commonly viral or bacterial rhinitis. Local trauma
from nose picking and direct blows to the nose are also frequent causes. Less
commonly seen causes include foreign bodies, tumors, coagulopathies, use of
anticoagulant drugs such as aspirin, Plavix, or warfarin, and exposure to toxic or
caustic materials, such as cocaine. Approximately 60% of people experience at least
one nosebleed in their lifetime, and 6% of those seek medical attention for it.
2. Doesn’t hypertension cause epistaxis?
Probably not acutely. The hypertensive patient who presents with a nosebleed typically
has hypertension as a chronic condition and has developed atherosclerosis, which
makes the blood vessels relatively fragile and more prone to bleeding. Recent studies
suggest an association between hypertension and epistaxis, but proof of a causal
relationship has not been established.
3. Does bleeding originate from any one particular source?
Approximately 90% of nosebleeds originate from the anterior portion of the nose, a rich
vascular network on the anterior-inferior portion of the septum known as Kiesselbach’s
plexus or Little’s area. The blood supply for most of this region is derived from the external
carotid system. From a practical standpoint, a nosebleed with a source that can be seen
directly or is controlled after proper placement of an anterior nasal pack is considered
anterior. Posterior bleeds arise from a branch of the sphenopalatine artery and tend to be
more difficult to control. Posterior bleeds usually occur in patients older than 50. The
hemorrhage tends to be more severe with patients often swallowing large amounts of blood.
4. List the key questions to ask the patient.
a. Is there a prior history of nosebleeds?
b. A history of excessive alcohol use or bleeding dyscrasias?
c. Was trauma involved? Nose picking?
d. On which side did the bleeding start?
e. Any recent sinus infections or surgeries?
f. Warfarin, Plavix or aspirin use?
5. Summarize the key points to successful management of nosebleeds.
There are two key considerations. The first is preparation. Because epistaxis rarely presents
as a life-threatening condition, there is time to assemble the necessary equipment and
supplies for treatment (Table 21-1). While obtaining the history and quickly assessing the
ABCs (airway, breathing, and circulation), have the patient pinch the nose firmly (bilateral
nasal ala compressing the septum) or place a nasal clamp on the patient with firm pressure
on the septum. The examiner should wear disposable gloves, mask, and eye protection.
The second key is to identify the source of the hemorrhage.
Chapter 21 NONTRAUMATIC ENT EMERGENCIES136
6. How do I treat epistaxis?
Using a nasal speculum, suction, and water-moistened cotton swabs, remove the existing
clots in an effort to identify the bleeding site. Alternatively you can ask the patient to blow the
nose, which helps in the removal of clot. Insert a pledget soaked with topical anesthetic plus a
vasoconstrictor (e.g., lidocaine 4% and phenylephrine) for 5 to 10 minutes. Remove the
pledget and attempt to identify the bleeding site. If the source is in Kiesselbach’s plexus and is
less than 1 cm
2
, use silver nitrate or electrocautery. Alternatively, a small piece of absorbable
gelatin sponge (Gelfoam), absorbable cellulose (Surgicel), or similar substance may be
moistened with a vasoconstrictor and applied to the bleeding site.
If these methods are unsuccessful, an anterior nasal packing should be inserted. A dry
Merocel sponge or nasal tampon should be placed by coating the outside with antibiotic
ointment with insertion into the nostril. Once in place, moisten this with saline or
phenylephrine until it expands to tamponade the nasal cavity. If inspection of the posterior
pharynx reveals no continued bleeding after the vasoconstrictor wears off (about 30 minutes),
the patient may be discharged.
7. Any other pearls about treatment with silver nitrate?
n
Silver nitrate is only helpful when the bleeding is slow or minimal. It won’t work in the
presence of brisk bleeding.
n
Only hold the silver nitrate to the septum for 5 to 10 seconds and only use electrocautery
or chemical cauterization (silver nitrate) on one side of the septum. Cauterizing for too long
or to both sides of the septum can lead to perforation or permanent damage to the blood
supply of the region.
From Lucente F, Har-EI G, editors: Essentials of otolaryngology, ed 4, New York, 1999, Lippincott, Williams
& Wilkins; Kucik CJ, Clenney T: Management of epistaxis. Am Fam Physician 7(12):305–311, 2005.
TABLE 21-1. SUPPLIES FOR THE TREATMENT OF NOSEBLEEDS
Examination Stabilization Treatment
Protective garb Bayonet forceps Silver nitrate cautery sticks
Head lamp or light Cotton pledgets Electrocautery (if available)
Nasal speculum Lidocaine 4% Gelfoam (or similar material)
Cotton swabs Epinephrine 1:1000 Merocel sponge or nasal
tampon
Fraser tip suction Tetracaine 0.5% 1/2-inch petroleum-
impregnated gauze
Emesis basin Oxymetazoline
hydrochloride (Afrin)
Antibiotic ointment
4 3 4 gauze 0.25% phenylephrine
(Neo-Synephrine)
Foley catheter or commercial
balloon
Rolled 4 3 4 gauze with
silk suture
Chapter 21 NONTRAUMATIC ENT EMERGENCIES 137
8. What are the important discharge instructions?
a. The pack (any type) should be left in place for 2 to 3 days.
b. Treat each patient who has packing with prophylactic antistaphylococcal antibiotics to
prevent sinusitis or toxic shock syndrome. Sinusitis may occur because the paranasal
sinuses cannot drain properly with a pack in place. Either cephalexin or trimethoprim-
sulfamethoxazole is a typical choice.
c. Any recurrent epistaxis that fails to respond to direct firm pressure for 10 minutes should
be seen in the ED.
d. Regular application of petroleum jelly or antibiotic ointment and use of room humidifiers
may prevent bleeding from desiccated nasal mucosa.
KEY POINTS: INSTRUCTIONS FOR PATIENTS WITH
AN ANTERIOR NASAL PACKING
1. The pack should be left in place for 2 to 3 days.
2. Treat each patient who has packing with prophylactic antistaphylococcal antibiotics.
3. If recurrences fail to respond to direct firm pressure for 10 minutes, the patient should seek
medical attention.
4. Regular application of petroleum jelly or antibiotic ointment and use of room humidifiers may
prevent bleeding from desiccated nasal mucosa.
9. How do I diagnose posterior epistaxis?
If a properly placed anterior pack fails, the patient may have a posterior bleed and more
aggressive treatment is required. Posterior packs are accomplished with rolled 4 3 4 inch
gauze, a Foley catheter (French 16 or 18), or other commercially available balloon products.
Take a Foley and place in the nose until you can see it in the oropharynx. Fill the balloon with
10 to 15 mL of saline and pull gently but firmly until the balloon is wedged in the far posterior
nasal cavity. Clamp the Foley in this position with an umbilical clamp placed just outside the
nose. Because the Foley will be stretched a bit, place gauze between the nose and clamp so as
not to cause pressure necrosis of the nose.
10. Do I discharge a patient to home with a posterior pack?
No. All patients who require posterior packing require an admission and otolaryngology (ENT)
consultation. Although the mechanism is unclear, posterior packing stimulates the
nasopulmonary reflex, which can lead to hypoxia and apnea. The patient should be on
supplemental oxygen and continuous pulse oximetry. It should be noted that 10% of posterior
bleeds are not controlled by posterior packing.
KEY POINTS: DIAGNOSIS AND MANAGEMENT OF
POSTERIOR EPISTAXIS
1. When an anterior packing fails to control epistaxis, a posterior bleed originating from
sphenopalatine artery should be suspected.
2. Treatment consists of an ENT consult, posterior nasal packing and hospital admission to
monitor for hypoxia and apnea secondary to the nasopulmonary reflex.
