Markovchick Vincent J., Pons Peter T., Bakes Katherine M.(ed.) Emergency medicine secrets. 5th ed
Подождите немного. Документ загружается.

Chapter 16 SYNCOPE, VERTIGO, AND DIZZINESS108
9. What targeted bedside tests aid in the diagnosis of vertigo?
Examine the eyes for ocular palsies and nystagmus. Examine the ears for infection,
perforation, and hearing function (using the Weber and Rinne tests). Perform a full neurologic
examination including cranial nerves, gait, stance, and cerebellar function. The Dix-Hallpike
and Epley for BPPV and head thrust maneuvers to diagnose labyrinthitis or neuronitis may be
beneficial if these specific etiologies are suspected.
10. How is nystagmus evaluated in the work-up of vertigo?
With peripheral etiologies, asymmetric impulses from the semicircular canals cause the eyes to
drift toward the diseased side and correct with the fast component of nystagmus to the opposite
normal side. By convention, the direction of the fast component determines the direction. Vertical,
changing direction, and nonsuppressible nystagmus are characteristics of central etiologies.
11. What is the head thrust maneuver? What does it mean?
The examiner stands in front of the patient and holds the patient’s head in both hands
instructing the patient to look at the examiner’s nose. The head is rapidly turned 5 to 10
degrees to one side and the response of the eyes is noted. Normally, the eyes continue to fix
on the examiner’s nose (intact vestibulo-ocular reflex), but if one side has a unilateral lesion
such as vestibular neuritis, the eyes don’t stay fixed on the target and need to correct to
refocus on the target after head movement. Turning the head in the opposite direction serves
as control. A patient with unidirectional horizontal nystagmus, a positive head thrust test
opposite the fast phase direction of the nystagmus and no other neurological features, is likely
to have vestibular neuritis or labyrinthitis.
12. What is the Dix-Hallpike maneuver?
This diagnostic maneuver tests for BPPV and involves moving the patient rapidly from a
sitting position with the head turned 45 degrees to one side with the head hanging down in a
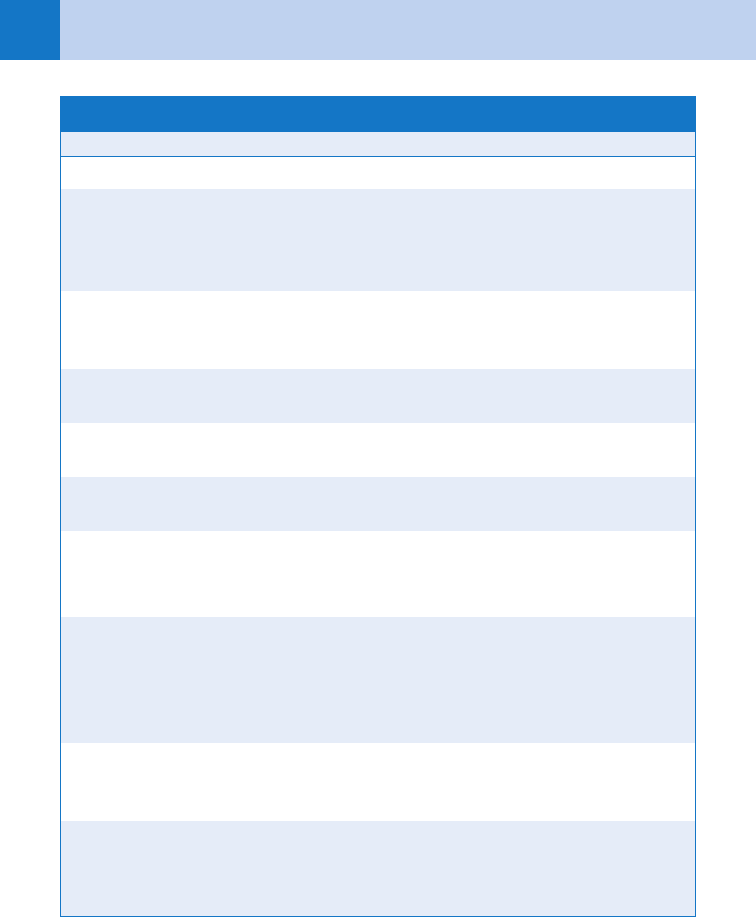
TABLE 16-1. KEY POINTS FOR THE MAIN CAUSES
OF PERIPHERAL VERTIGO
Benign paroxysmal positional vertigo
Most common cause (50%)
Recurrent ,1 minute paroxysms elicited with head turning
Normal between brief attacks
Due to otolith dislodgement into a semicircular canal
Responds to Epley maneuver
Vestibular Neuritis
Less common cause (20%)
Probable viral etiology
Positive asymmetric head thrust test
May respond to steroids
Ménière Disease
Less common cause (10%)
Less acute onset (hours)
Associated with hearing loss, tinnitus
Due to high endolymph volume
Responds to diuretics or fluid restriction
Chapter 16 SYNCOPE, VERTIGO, AND DIZZINESS 109
supine position. Nystagmus, often toward the dependent eye or forehead, is characteristically
associated with a delay of a few seconds and fatigable symptoms of vertigo on repetition.
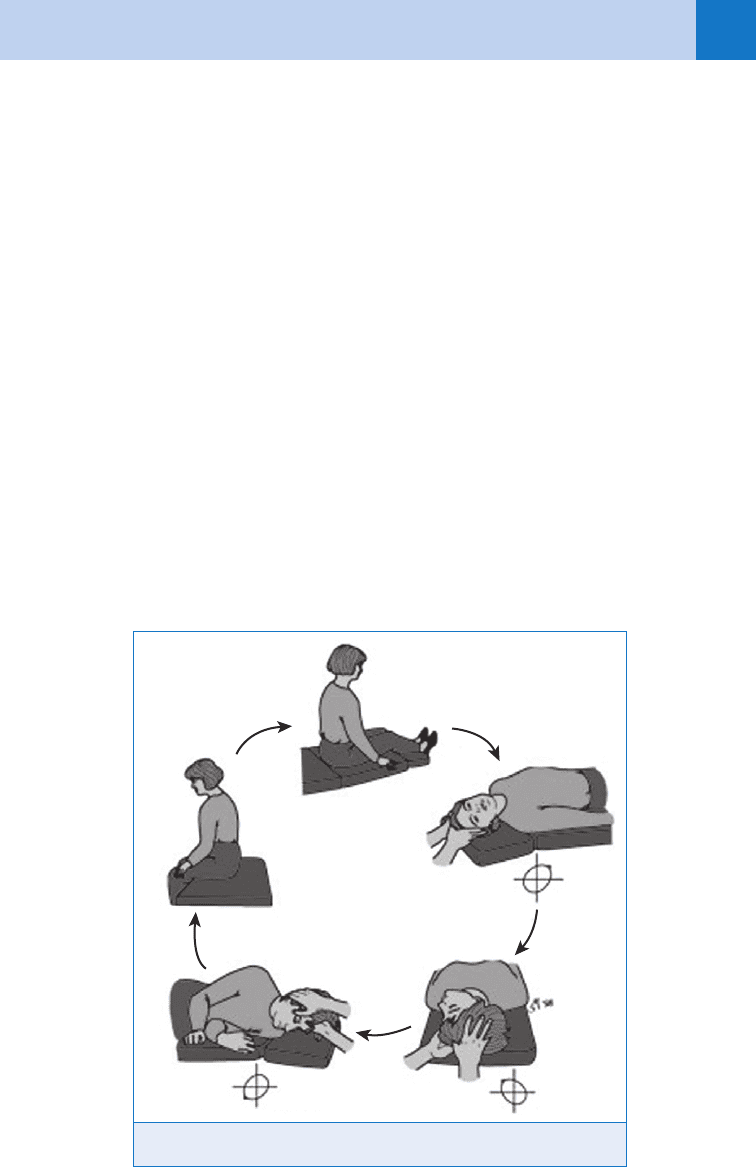
13. What is the Epley maneuver?
The Epley maneuver treats BPPV and is utilized to physically move otoliths, most commonly
in the posterior semicircular canal into the utricle. It is successful about 75% of the time on
first attempt and up to 98% on two attempts. The technique involves performing the Dix-
Hallpike maneuver, then turning the head to the opposite side while still supine and then
turning over in the same direction prior to rising. (See Fig. 16-1)
14. How do I treat peripheral (and central) vertigo?
Vestibular neuritis benefits from steroids in a 22-day taper. BPPV is treated by the Epley
maneuver. Nonspecific vestibular suppressants include:
n
Anticholinergics (e.g., scopolamine transdermal)
n
Antihistamines (meclizine 25–50 mg PO every 6 hours, dimenhydrinate 50 mg PO every
4–6 hours, and diphenhydramine 25–50 mg PO every 4–6 hours)
n
Benzodiazepines (diazepam 5–10 mg PO every 6 hours)
Central vertigo requires evaluation by neurology or neurosurgery. If the patient cannot walk or
has intractable symptoms, magnetic resonance imaging (MRI) to evaluate the posterior fossa
and brainstem and admission is recommended.
15. What is syncope?
A sudden temporary loss of consciousness with the inability to maintain postural tone. It is a
symptom, not a disease, with a wide variety of benign and life-threatening causes. Coma, head
trauma, shock, and seizures may mimic syncope.
A
B
C
D
E
Figure 16–1. Epley maneuver.
Chapter 16 SYNCOPE, VERTIGO, AND DIZZINESS110
16. What are the odds of determining the cause of a syncopal episode?
Despite extensive and expensive work-ups, no cause is found in about 50% of cases. This
should be discussed with the patient so that there are no unrealistic expectations.
KEY POINTS: CAUSES OF SYNCOPE
1. HEAD (hypoxemia, epilepsy, anxiety, dysfunctional brain)
2. HEART (heart attack, embolism of pulmonary artery, aortic obstruction, rhythm disturbance,
tachydysrhythmia)
3. VESSELS (vasovagal, ectopic, situational, subclavian steal, ENT, low systemic vascular
resistance, sensitive carotid sinus)
17. Discuss the causes of syncope as related to the head.
Diffuse cerebral malfunction from lack of vital nutrients, such as oxygen (hypoxemia) or sugar
(hypoglycemia), are often correctable, but easily overlooked. Seizures don’t cause but can
mimic syncope. Vertebrobasilar insufficiency and SAH represent a dysfunctional brain.
18. Discuss the cardiovascular causes of syncope.
Cardiac causes of syncope comprise the riskiest group of patients and include acute coronary
syndrome (ACS), pulmonary embolism, physical aortic outflow obstructions (from
hypertrophic obstructive cardiomyopathy, aortic stenosis, and atrial myxoma), slow rhythms
such as sick sinus syndrome, and tachyarrhythmias. Brugada syndrome, pre-excitation, and
long QT syndrome can precipitate lethal dysrhythmias.
19. What about the vascular causes of syncope?
Vascular causes include:
n
The common faint (vasovagal)
n
Hypovolemia
n
Situational faints (e.g., micturition, defecation, cough, or Valsalva maneuver)
n
Subclavian steal
n
Ear, nose, and throat (ENT) causes (e.g., glossopharyngeal and trigeminal neuralgia)
n
Low systemic vascular resistance (from medications and autonomic insufficiency)
n
Carotid sinus sensitivity (only accounting for 4% of syncope cases)
20. Summarize the initial concerns when treating a patient with syncope.
Most patients with syncope rapidly return to a normal mental status and have stable vital
signs. There are treatment priorities, however.
a. Obtain vital signs and evaluate and treat for immediate life threats.
b. Oxygen, intravenous access, and cardiac and blood pressure monitoring should be initiated
on patients who have abnormal vital signs, a persistent altered level of consciousness,
chest pain, dyspnea, abdominal pain, or a significant history of cardiac disease.
c. Assess for any trauma secondary to fall. Elderly patients are more likely to suffer head
trauma secondary to syncope, and this may be a greater life threat initially than the cause
of the syncope.
21. Okay, I’ve ruled out the immediate life threats. Now what do I do?
Obtain a detailed history, do a directed physical examination, and obtain an electrocardiogram
(ECG). Then do a risk assessment to determine whether further testing or admission is
indicated.
Chapter 16 SYNCOPE, VERTIGO, AND DIZZINESS 111
22. What components of the history are most important?
The most important historical clue is the patient’s recollection of the events just before the
syncope. An abrupt onset of loss of consciousness with a brief (,5 seconds) prodrome is
indicative of a cardiac etiology. Similarly, syncope associated with exercise, or while reclining
or recumbent, is associated with cardiac obstructive causes or arrhythmias. Patients who have
vasovagal syncope often have premonitory symptoms of dizziness, yawning, nausea, and
diaphoresis, and the event is during a period of some psychosocial stress. Clues to
hypovolemia include thirst, postural dizziness, decreased oral intake, melena, or unusually
heavy vaginal bleeding. Syncope after micturition, cough, head turning, defecation,
swallowing, or meals suggests situational syncope. Note previous episodes of syncope, upper
extremity exertion (e.g., subclavian steal syndrome), and the presence of cardiac risk factors.
A family history of sudden death may suggest Brugada, pre-excitation, or long QT syndromes.
Many medications and medication interactions can cause syncope, so determine all of the
patient’s current medications, especially when treating the elderly.
23. How do I know it was not a seizure?
Victims of arrhythmias and vasovagal faints often exhibit myoclonic jerks that may mimic a
seizure. Recovery from syncope is usually rapid, whereas a generalized seizure patient
awakens slowly with prolonged confusion or postictal state. Both may have trauma. The
absence of an anion gap on blood drawn within 30 minutes of the event or no postictal state
argues against a generalized seizure. Lateral tongue biting has been shown to be specific but
insensitive for a seizure.
24. What is a directed physical examination?
Be a detective, using head, heart, and vessels as a guide. The patient with abrupt effort or
exercise syncope may have aortic stenosis or hypertrophic cardiomyopathy; look for narrow
pulse pressure, systolic murmur, or change in murmur with Valsalva. The presence of physical
signs of congestive heart failure (CHF) places the patient at high risk. Examine the head
carefully for trauma, bruits, and focal neurologic signs. Check blood pressure in both arms
looking for subclavian steal. Search for occult blood loss or autonomic insufficiency.
25. What tests are needed to assist in diagnosis?
Other than a urine pregnancy test in females, a detailed history, physical examination, and
ECG are often sufficient. The addition of a specific confirmatory test (e.g., echocardiography)
is recommended for suspected cardiomyopathy.
26. Who needs an ECG? What am I looking for?
Almost all patients with syncope should have an ECG because it is not invasive, may be
diagnostic of a problem such as Brugada syndrome or long QT, and helps in risk stratification
for ACS. Check for markers of cardiac disease, such as ischemia, infarction, arrhythmias,
pre-excitation, long QT intervals, and conduction abnormalities. Left ventricular hypertrophy
may be a clue to aortic stenosis, hypertension, or cardiomyopathy.
27. If the basic evaluation is not diagnostic, who should receive further testing?
Patients with CHF, older age, abnormal ECG and unexplained syncope who have suspected
heart disease should be admitted and evaluated for an acute coronary syndrome.
Echocardiography, exercise treadmill testing, Holter ECG monitoring, and electrophysiologic
studies also may be helpful.
28. What factors help to assign a patient to a high-risk or low-risk group?
Physician gestalt plays a large role. Studies attempting to determine highly sensitive risk
factors have had mixed results (see Table 16-2). For example, the San Francisco Syncope Rule
was found to have only 75% sensitivity on external validation.

Chapter 16 SYNCOPE, VERTIGO, AND DIZZINESS112
29. My consultant wants orthostatic vital signs; are they helpful?
Yes and no. Orthostatic hypotension (defined as a blood pressure drop of 20 mm Hg on
standing for 3–4 minutes) is associated with volume loss or autonomic insufficiency and an
increased risk of fall and syncope. However, parameters for orthostatic hypotension are
neither sensitive nor specific. A blood pressure drop of 20 mm Hg has only 29% sensitivity
and 81% specificity for 5% or greater fluid deficit. Of normal euvolemic patients older than
65 years, more than 25% generate false-positive results. Reproducible symptoms are a better
predictor than any number change.
30. Are there guidelines for the evaluation of syncope?
Yes.
a. American College of Emergency Physicians (ACEP): Clinical policy: critical issues in the
evaluation and management of patients presenting with syncope. Ann Emerg Med 49:771, 2007.
b. Brignole M, Alboni P, Benditt DG, et al: Guidelines on management (diagnosis and
treatment) of syncope-Update 2004. Europace 6:467–537, 2004.
c. Strickberger SA, Benson W, Biaggioni I, et al: AHA ACCF Scientific statement on the
evaluation of syncope. Circulation 113:316, 2006.
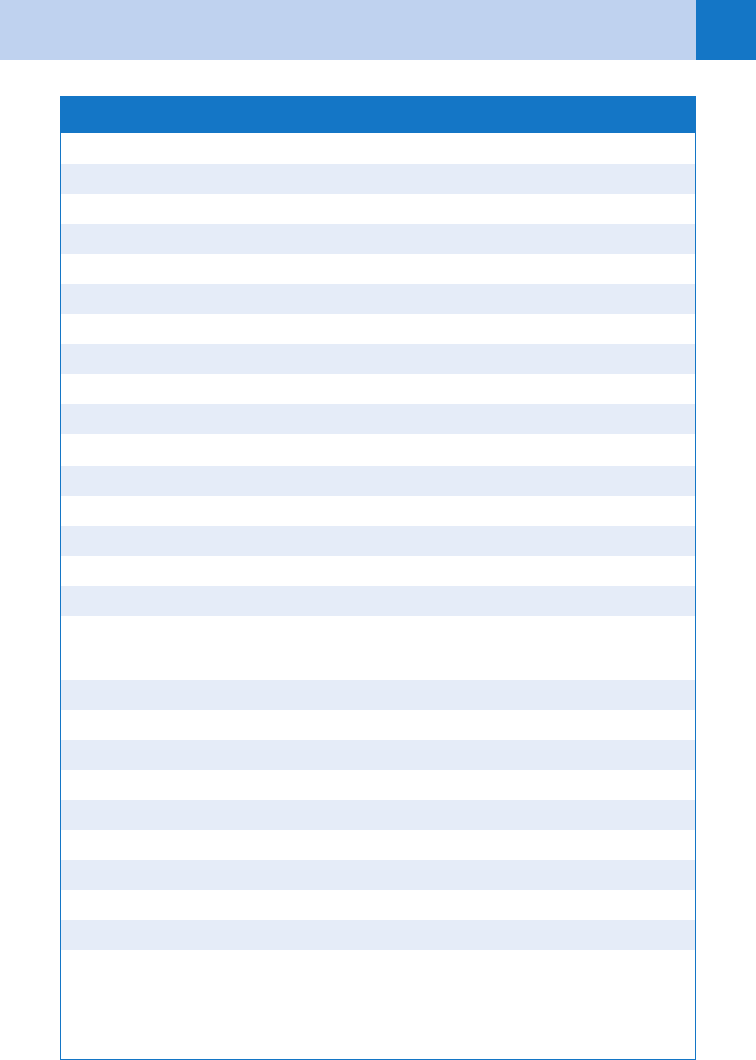
TABLE 16-2. SYNCOPE AT HIGH RISK FOR CARDIAC ETIOLOGY
Historical ED evaluation
Age .65 years
Cardiovascular disease history
Lack of prodrome
Exertional
Chest pain with event
Palpitations preceding the event
Family history of sudden death
Abnormal vital signs
Systolic blood pressure ,90
Evidence of congestive heart failure
Abnormal electrocardiogram
BIBLIOGRAPHY
1. Bhattacharyya N, Baugh RF, Orvida L, et al: Clinical practice guideline; benign paroxysmal positional vertigo.
Otolaryngology 139:S47, 2008.
2. Birnbaum A, Esses D, Bijur, et al: Failure to validate the San Francisco syncope rule in an independent
emergency department population. Ann Emerg Med 52:151, 2008.
3. Chan Y: Differential diagnosis of dizziness. Curr Opin Otolaryngol Head Neck Surg 17:200, 2009.
4. Colivicchi F, Ammirati F, Melina D, et al: Development and prospective validation of a risk stratification system
for patients with syncope in the emergency department: the OESIL risk score. Eur Heart J 24:811, 2003
5. Costantino G, Perego F, Dipaola F, et al: Short and long term prognosis of syncope, risk factors and role of
hospital admission. J Am Coll Cardiol 51:276, 2008.
6. Del Rosso A, Ungar A, Maggi R, et al: Clinical predictors of cardiac syncope at initial evaluation in patients
referred urgently to a general hospital: EGSYS score. Heart 94:1620, 2008.
7. Edlow JA, Newman-Toker DE, Savitz SI: Diagnosis and initial management of cerebellar infarction. Lancet
7:951, 2008.
8. Grossman SA, Fischer C, Lipsitz L, et al: Predicting adverse outcomes in syncope. J Emerg Med 33:233,
2007.
9. Kerber KA: Vertigo and dizziness in the emergency department. Emerg Med Clin North Am 27:39, 2009.
10. Kerber KA, Meurer WJ, West BT, et al: Dizziness presentations in US emergency departments, 1995–2004.
Acad Emerg Med 15:744, 2008.
11. Seemungal BM, Bronstein AM: A practical approach to acute vertigo. Pract Neurol 8:211, 2008.
12. Strupp M, Zingler VC, Arbusow V, et al: Methylprednisolone, valacyclovir, or the combination for vestibular
neuritis. N Engl J Med 351:354, 2004.
113
CHAPTER 17
SEIZURES
Kent N. Hall, MD
1. What is a seizure?
A seizure is an episode of abnormal brain function caused by excessive and aberrant
electrical discharge in the brain. This electrical discharge may, or may not, result in
characteristic muscle activity that is recognized as seizure activity. In addition to tonic-
clonic muscle activity, generalized seizures may also manifest as staring episodes, lip
smacking or other minor motor activity, or complete disruption of muscle tone (drop
attacks). Generalized seizures are often followed by a postictal phase characterized by
confusion and/or lethargy. This phase usually lasts for 5 to 15 minutes, although it may
last longer.
The recognition and appropriate management of seizures are critically important to
the patient and the emergency physician because they are a common ED presenting
problem. Prolonged excessive electrical activity in the brain causes neuronal destruction.
This destruction is not due to build-up of metabolic by-products but is actually directly
related to the electrical activity itself. For an unknown reason, the hippocampus is
particularly sensitive to the damage from this electrical activity.
2. How are seizures classified?
Seizures are classified according to the amount of brain involved in the abnormal
electrical activity, its resulting physical manifestation, and its underlying cause. In
general, seizures are divided into two groups, generalized and focal (Table 17-1).
Generalized seizures affect a large volume of brain tissue in the abnormal electrical
activity, whereas focal seizures involve a specific brain area. Because of this, the
manifestations of focal seizures, whether simple or complex, may lead to bizarre
manifestations including hallucinations, memory disturbance, visceral symptoms
(abdominal symptoms), and perceptual distortions. This has often resulted in the
patient with partial seizures being misdiagnosed as having a psychiatric problem.
Often the emergency physician is presented with a patient who is not actively seizing
but has had a seizure. In this case, it is important to evaluate for secondary signs of
seizure activity. These include bowel or bladder incontinence, biting of the tongue or
buccal mucosa, and postictal confusion.
3. What are the causes of seizures?
Seizures are abnormal electrical activity in the brain. Primary seizures are recurrent
episodes without an underlying cause. This is classically referred to as epilepsy.
Secondary seizures (also called reactive seizures) have a (usually non-neurologic)
underlying condition. Table 17-2 lists the most common etiologies for secondary
seizures.
4. What is included in the differential diagnosis of seizure?
Anything that can cause a sudden disturbance of neurologic function may be mistaken
for a seizure. Common processes that fall into this category include syncope,
hyperventilation syndrome, migraines, movement disorders, and narcolepsy.
Pseudoseizure is a special category and is discussed later.
Chapter 17 SEIZURES114
5. What should my priorities be in managing a patient who is actively seizing?
Clinical priorities are the ABCs. Attention is always directed to the airway first. It is rare that a
seizure patient needs to be intubated. Supplemental oxygen, usually via nasal cannula, should
be given because of the increased oxygen demand caused by the generalized muscle activity.
Supplemental ventilation (bag-valve-mask) is rarely needed. Evaluation of the circulatory
status can be readily accomplished by noting blood pressure, pulse, and capillary refill. Check
the temperature and administer antipyretics in appropriate doses when needed.
Airway protection can usually be accomplished by positioning the patient on his or her
side. Suctioning of the patient’s oral secretions will also help decrease the chance of
aspiration. However, nothing should be put into the patient’s mouth that might be bitten off
TABLE 17-1. CLASSIFICATION OF SEIZURES
Type Manifestations
Generalized
Tonic-clonic (grand mal) Loss of consciousness followed immediately by tonic contractions
of muscles, then clonic contractions of muscles (jerking) that
may last for several minutes. A period of disorientation (postictal
period) occurs after the tonic-clonic activity.
Absence (petit mal) Sudden loss of awareness with cessation of activity or body
position control. The period usually lasts for seconds to minutes
and is followed by a relatively short postictal phase.
Atonic (drop attacks) Complete loss of postural control with falling to the ground,
sometimes causing injury. It usually occurs in children.
Myoclonic Brief, vigorous, spasmodic muscle contractions. These may affect
the entire body or only specific areas.
Tonic Prolonged muscle contraction. It occurs usually with associated
deviation of the head and eyes in a particular direction.
Clonic Repetitive jerking motions occur without any associated tonic
muscle contraction.
Partial or focal
Simple partial Multiple patterns are possible depending on the area of the
brain affected. If the motor cortex is involved, the patient will have
contraction of the corresponding body area. If nonmotor areas
of the brain are involved, the sensation may be paresthesias,
hallucinations, or déjà vu.
Complex partial Usually there is loss of ongoing volitional major motor activity with
repetitive minor motor activity, such as lip smacking and walking
aimlessly.
Partial with secondary
generalization
Initial manifestations are the same as partial. However, the activity
progresses to involve the entire body, with loss of postural control
and possibly tonic-clonic muscle activity.
Chapter 17 SEIZURES 115
TABLE 17-2. ETIOLOGIES OF SECONDARY SEIZURES
Metabolic
Hypoglycemia, hyperglycemia
Hyponatremia, hypernatremia
Hypocalcemia
Hypomagnesemia
Uremia
Hypothyroidism
Hepatic encephalopathy
High anion gap acidosis
Fever (“febrile seizures”)
Infectious diseases
Meningitis
Encephalitis
Cerebral abscess
Cerebral parasitosis
HIV
Drugs/toxins (multiple)
Subtherapeutic antiepileptic drug levels
Cocaine, lidocaine
Antidepressants
Theophylline
Alcohol withdrawal
Drug withdrawal
Structural
Trauma (recent and remote)
Intracranial hemorrhage
Vascular lesions
Mass lesions
Eclampsia
Hypertensive encephalopathy
Chapter 17 SEIZURES116
6. What do I do if the patient doesn’t stop seizing?
Most seizures last for less than 2 minutes. When a seizure lasts longer, pharmacologic
intervention is generally indicated. Benzodiazepines are the accepted first-line therapy.
The intravenous (IV) route is the preferred route of administration. Lorazepam (2–4 mg
intravenously) is the conventional first choice because of theoretical issues related to duration
of action. However, diazepam (5–10 mg intravenously) may also be used. Diazepam may be
administered intravenously, rectally, or intraosseously but is not recommended for
intramuscular use because of uneven uptake.
Once the seizure has ceased, anticonvulsants are used to keep it from recurring. Phenytoin
is considered the first-line therapy. Table 17-3 shows the medications in this class along with
their dosage and route of administration.
7. What is status epilepticus? How is it managed?
When seizures last longer than 5 minutes despite acute pharmacologic intervention or recur
so frequently that normal mentation does not resume between the seizures, it is called status
epilepticus. In this case, immediate pharmacologic intervention is indicated. Table 17-4 gives
an algorithm that can be used to manage the patient with status epilepticus.
8. Is the history important?
The history if vitally important! The mnemonic COLD can be used to ensure you have covered
the aspects of the seizure activity itself.
n
Character: What type of seizure activity occurred?
n
Onset: When did it start? What was the patient doing?
n
Location: Where did the activity start?
n
Duration: How long did it last?
In general, seizures start abruptly, are stereotyped (similar seizure activity recurs from attack
to attack in an individual patient), are not provoked by environmental stimuli, are manifested
by purposeless or inappropriate motor activity, and except for petit mal seizures, are followed
by a period of confusion or lethargy (the postictal phase). Other important historical aspects
include the patient’s past medical history (especially previous seizure history), alcohol use,
(including fingers) and thus become an obstructing foreign body. Gently restraining the
patient so he or she is not harmed is also important.
Diagnostic priorities should focus on likely secondary causes of seizures that are
reversible. Hypoglycemia is a common cause of secondary seizures that is treatable with rapid
results. Similarly, immediate evaluation of significant electrolyte abnormalities (i.e., sodium,
calcium, magnesium) in a patient with prolonged seizure activity is warranted.
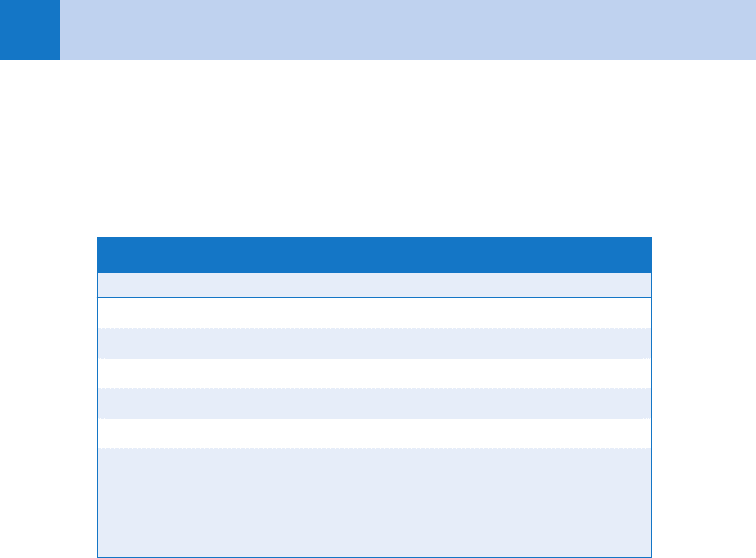
TABLE 17-3. ANTICONVULSANTS
Drug Adult dose
Phenytoin 15–20 mg/kg IV at ,50 mg/min
Fosphenytoin 15–20 mg PE/kg at 100–150 mg PE/min; may be given IM
Phenobarbital 20 mg/kg IV at 60–100 mg/min. May be given as IM loading dose
Valproate 15–30 mg/kg IV should be given over one hour
Pentobarbital 5 mg/kg IV at 25 mg/min, then titrate to EEG. Intubation required
Isoflurane Via general endotracheal anesthesia
EEG, electroencephalogram; IM, intramuscularly; IV, intravenously; PE, phenytoin sodium equiva-
lents; PR, per rectum.
Chapter 17 SEIZURES 117
toxic ingestions, current medications, any history of central nervous system (CNS)
neoplasms, and history of recent or remote trauma.
9. In addition to the neurologic examination, what other parts of the physical
examination are important?
A complete head-to-toe examination is important. In addition to looking for causes of the
seizure, the physician should look for trauma caused by the seizure. The examination is often
normal but occasionally may give clues to an underlying problem. Specifically, examination of
the skin might reveal lesions from meningococcemia, other infectious problems, or stigmata
of liver failure. Examine the head for trauma. If nuchal rigidity is found, meningitis or
subarachnoid hemorrhage should be suspected.
The neurologic examination is most important. Focal neurologic findings, such as focal
paresis after the seizure (Todd’s paralysis), may indicate a focal cerebral lesion (i.e., tumor,
abscess, or cerebral contusion) as the cause of the seizure. Evaluation of the cranial nerves
and the fundi can point to increased intracranial pressure.
10. What ancillary testing should I do in the patient with a history of seizures?
Extensive ancillary testing is reserved for the patient with new onset seizure. For patients with
a prior history of seizures who have an unprovoked attack, measurement of appropriate serum
anticonvulsant levels is all that is required. The decision to proceed with further testing
depends on the patient’s history and physical findings at the time of presentation. If there is a
question whether the patient had a major motor seizure, then measurement of the anion gap
within 1 hour of the seizure might be of benefit.
TABLE 17-4. PROPOSED GUIDELINES FOR MANAGEMENT OF THE PATIENT WITH STATUS EPILEPTICUS
Time Frame Measures
Establish/maintain airway
IV/oxygen/monitor
0–5 min Dextrose, 0.5 gm/kg IV, if indicated
Consider thiamine, 100 mg IV, and magnesium 1–2 gm IV for alcoholic or
malnourished patients
Lorazepam, 1 mg per min IV up to 0.1 mg/kg (or diazepam, 5 mg IV every
5 min up to 20 mg)
10–20 min Phenytoin, 20 mg/kg IV at 50 mg/min, or fosphenytoin, 20 mg/kg PE IV at
150 mg/min
Phenobarbital up to 20 mg/kg IV at 50–75 mg/min IV
Valproate up to 30 mg/kg IV over 1 hour
30 min And/or
General anesthesia with midazolam, 0.2 mg/kg slow IVP, then
0.75–10 mg/kg/min
Or propofol, 1–2 mg/kg IV, then 1–15 mg/kg/hr
Or pentobarbital, 10–15 mg/kg IV over 1 hour, then 0.5–1.0 mg/kg/hr
IV, intravenous; IVP, intravenous push; PE, phenytoin sodium equivalents. Adapted from Lowenstein DH,
Aldredge BK: Status epilepticus. N Engl J Med 338:970, 1998.
