Jan Lindhe. Clinical Periodontology
Подождите немного. Документ загружается.

REGENERATIVE PERIODONTAL THERAPY . 685
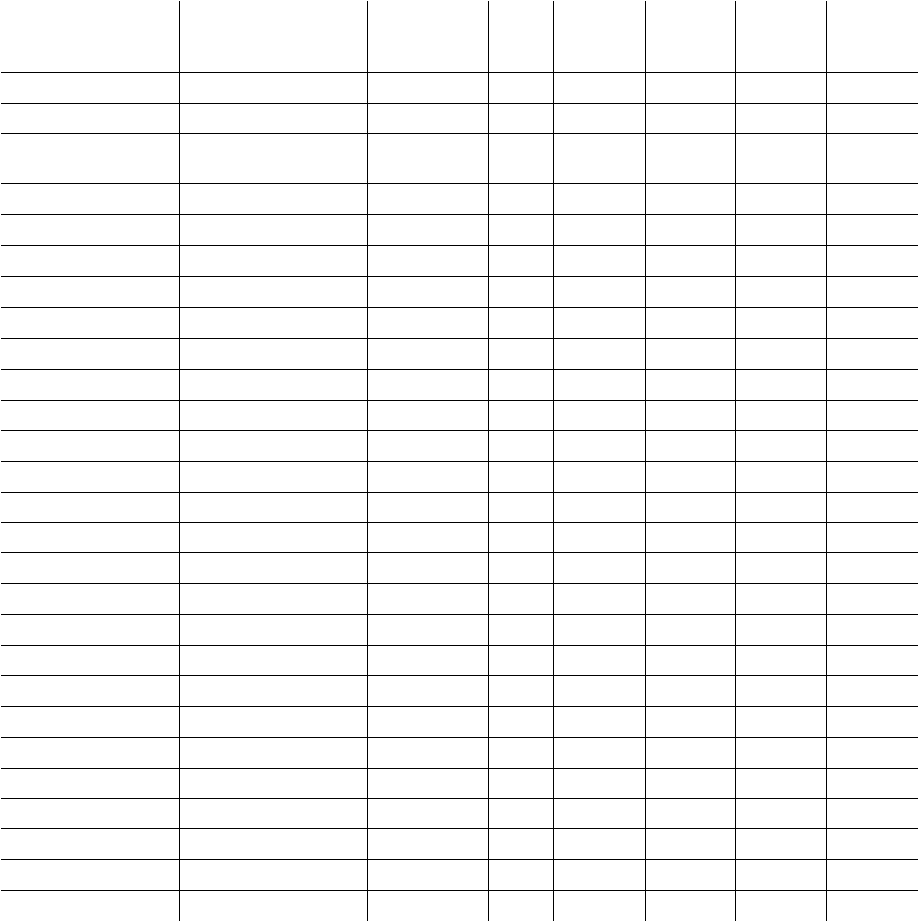
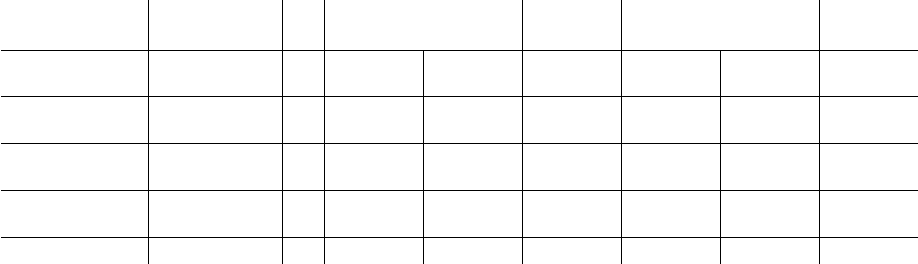
Table 28-3. Clinical outcomes and weighted mean of GTR treatment of mandibular degree II furcations
Authors
Type of Study
Treatment
N
Defect
Depth
(mm)
H-CAL
Gain (mm)
H-OPAL
Gain (mm)
N
of
Furca
closed
Pontoriero et al. 1988
Controlled clinical trial
e-PTFE
21
4.4 ± 1.2 3.8 ± 1.2
NA
14 (67%)
Becker et al. 1988
Case cohort
e-PTFE
6
8.3 ± 2.3
NA
1.8 ± 1.5
0
Schallhorn & McClain
1988
Case cohort
e-PTFE
16
NA NA
3.1 ± 1.7
5 (31%)
Lekovic et al. 1989
Controlled clinical trial
e-PTFE
6
NA NA
0.2 ± 0.5
NA
Lekovic et al. 1990
Controlled clinical trial
e-PTFE
15
4.2 ± 0.2
NA
0.1 ± 0.1
NA
Caffesse et al. 1990
Controlled clinical trial
e-PTFE
9
4.
8
± ?
0.
8
± ?
NA NA
Anderegg et al. 1991
Controlled clinical trial
e-PTFE
15
4.2 ± 2.2
NA
1.0 ± 0.8
NA
Yukna 1992
Controlled clinical trial
e-PTFE
11
3.
0
± ?
NA
1.
0
± ?
0
FDDMA
11
4.
0
±?
NA
2.
0
±?
0
Blumenthal 1993
Controlled clinical trial
e-PTFE
12
4.4 ± 0.9
1.8 ± 1
1.7 ± 0.5
4 (33%)
Collagen
12
4.5 ± 0.9 2.5 ± 0.8 2.5 ± 0.7
1 (8%)
Bouchard et al. 1993
Controlled clinical trial
e-PTFE
12
NA
2.8 ± 1.3 2.2 ± 1.4
4 (33%)
Conn. Graft
12
NA
1.5 ± 1.5 1.5 ± 1.1
2 (17%)
Machtei et al. 1993
Controlled clinical trial
e-PTFE
18
NA
2.3 ± 1.7
NA NA
Parashis & Mitsis 1993
Controlled clinical trial
e-PTFE
9
5.7 ± 0.7 4.7 ± 1.5
NA
4 (44%)
Van Swol et al. 1993
Controlled clinical trial
Collagen
28
5.1 ± 1.4
2.3 ± 1
1.
7
± ?
NA
Wallace et al. 1994
Controlled clinical trial
e-PTFE
7
NA NA
2.
3
± ?
NA
Black et al. 1994
Controlled clinical trial
e-PTFE
13
4.3 ± 2
0.8 ± 2.2
NA NA
Collagen
13
4.4 ± 1.5
1.5 ± 2
NA NA
Laurell et al. 1994
Case cohort
Polylactic Acid
19
NA
3.3 ± 1.4
NA
9 (47%)
Machtei et al. 1994
Controlled clinical trial
e-PTFE
30
7.7 ± 1.8 2.6 ± 1.7
NA NA
Mellonig et al. 1994
Controlled clinical trial
e-PTFE
11
8.4 ± 1.2
NA
4.5 ± 1.6
1 (9%)
Wang et al. 1994
Controlled clinical trial
Collagen
12
6.0 ± 2.7 2.0 ± 0.4
2.
5
± ?
NA
Hugoson et al. 1995
Controlled clinical trial
e-PTFE
38
5.9 ± 1.3 1.4 ± 2.2
NA
4 (11%)
Polylactic Acid
38
5.6 ± 1.4
2.2 ± 2
NA
13 (34%)
Poison et al. 1995
Case cohort*
Polylactic Acid
29
5.4 ± 0.2 2.5 ± 0.1
NA
0
Weighted Mean
423 5.4
±
1.3 t 2.3
±
1.4$ 1.9
± 1 ^
H-CAL = Horizontal Clinical Attachment. H-OPAL = Horizontal Open Probing Attachment. NA = data not available. e-PTFE = expanded
Polytetrafluoroethylene. FDDMA = Freeze Dried Dura Mater Allograft. Conn. Graft = Connective Tissue Graft. t N = Mean (340) ± S.D. (
302); $ N = Mean (325) ± S.D. (316);
A
N = Mean (186) ± S.D. (177). * Mandibular and maxillary molars.
volved sites would represent a considerable progress
in periodontics.
Mandibular
degree
II furcations
Pontoriero et al. (1988) reported a controlled random-
ized clinical trial in which significantly greater
amounts of horizontal clinical attachment (H-CAL)
gain (3.8 ± 1.2 mm) were obtained in 21 mandibular
degree II furcations treated with e-PTFE membranes
as compared to that in a control group treated with
open flap debridement alone (H-CAL gains of 2.0 ± 1.2
mm). Complete closure of the furcation was observed
in 67% of the test sites and in only 10% of the control
sites. Other studies, however, have failed to confirm
these promising results to the same extent (Becker et
al. 1988, Lekovic et al. 1989, Caffesse et al. 1990).
Analysis of a series of studies published between 1988
and 1996 demonstrates a great variability in the clini-
cal outcomes (Figs. 28-36 and 28-37). Table 28-3
summarizes the outcomes of 21 clinical trials in
which a total of 423 mandibular degree II furcations
were
treated with different types of non-bioabsorbable
and
bioabsorbable barrier membranes. The weighted
mean of the reported results shows a H-CAL gain of
2.
3 ± 1.4 mm with a 95% confidence interval ranging
from 2.0 to 2.5 mm in defects with a baseline horizon-
tal probing depth of 5.4 ± 1.3 mm. The reported num-
ber of complete furcation closures after GTR range
from 0 to 67%. In three studies none of the treated
furcations were closed (Becker et al. 1988, Yukna 1992,
686 • CHAPTER 28
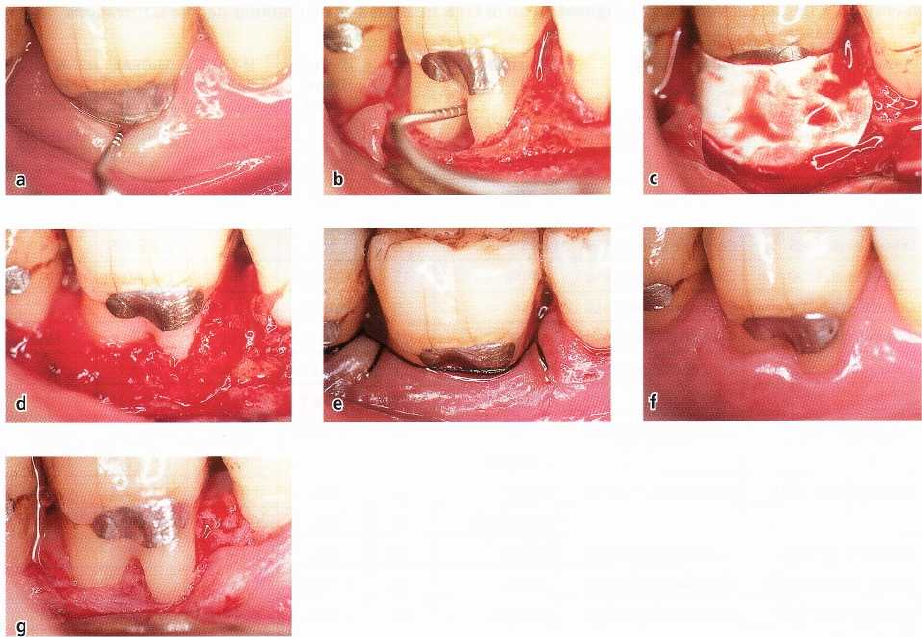
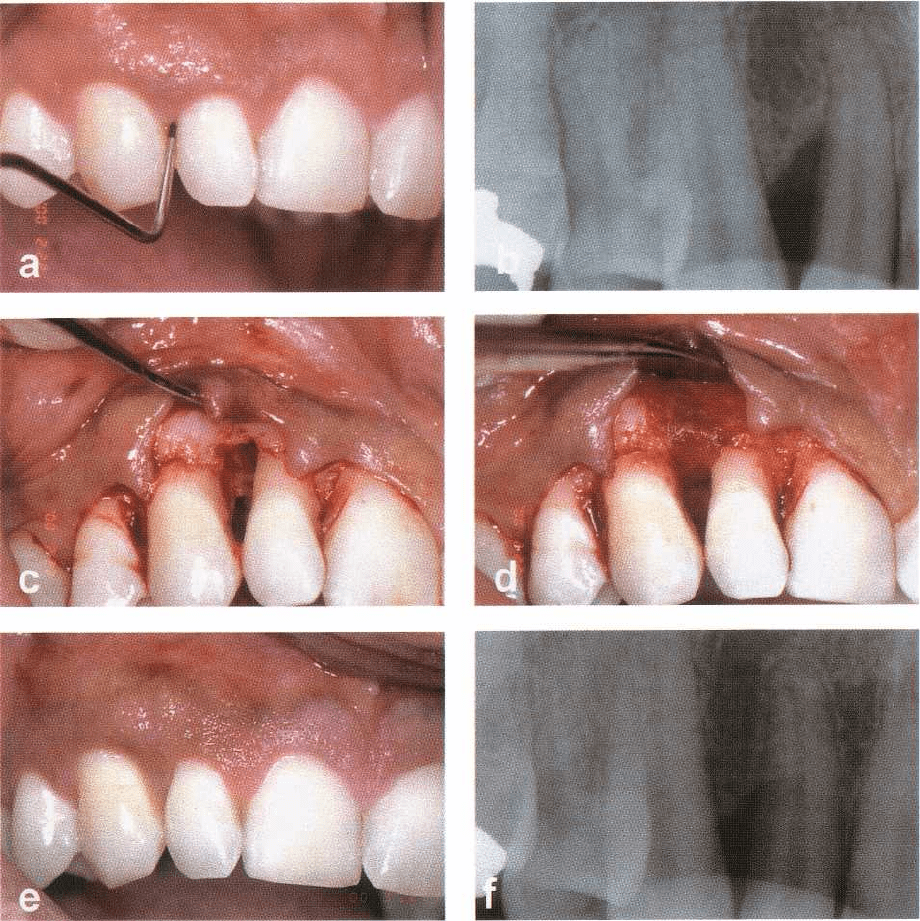
Fig. 28-36. (a) Right mandibular first molar presenting with a degree II furcation involvement. (b) Full thickness
buccal flaps have been raised, the defect debrided and the root carefully planed. (c) A non-bioabsorbable barrier
membrane has been placed to cover the defect. (d) After membrane removal, newly formed tissue appears to fill the
furcation completely (e) The regenerated tissue is covered with the flap. (f) Clinical appearance and surgery en-
try (
g) after 1 year shows that the degree II furcation is almost completely resolved.
Poison et al. 1995b), in seven studies fewer than 50%
were closed (Schallhorn & McClain 1988, Blumenthal
1993, Bouchard et al. 1993, Parashis & Mitsis 1993,
Laurell et al. 1994, Mellonig et al. 1994, Hugoson et al.
1995), and in only one study were more than 50% of
the treated furcations completely resolved (Pontoriero
et al. 1988).
A subset analysis of the studies reported in Table
28-3 indicated that furcations treated with non-bioab
-
sorbable barrier membranes (287) showed a gain in
horizontal clinical attachment of 1.8 ± 1.4 mm (95% CI
1.5-2.1 mm) as compared with 2.3 ± 1.2 mm H-CAL
gain (95% CI 2-2.6 mm) in 174 defects treated with
bioabsorbable barrier membranes. Five controlled
clinical trials compared treatment with non-resor-
bable e-PTFE membranes and treatment with differ-
ent types of bioabsorbable membranes (Table 28-4). In
particular, one investigation reported significantly
greater H-CAL gain in the non-bioabsorbable group
(
Bouchard et al. 1993), while another one (Hugoson et
al. 1995) showed a significantly greater H-CAL gain in
the bioabsorbable group. The remaining three inves-
tigations failed to detect any significant differences
between the outcomes of treatment with bioabsor-
bable or non-bioabsorbable membranes. Generally
the results indicate that the predictability of GTR in
the treatment of mandibular degree II furcations is
questionable, if the treatment objective is the complete
resolution of the furcation involvement.
Significant gain in vertical attachment level (V-
CAL) and reduction in pocket depth (PPD) was also
reported by several investigators following treatment
of mandibular degree II furcation defects (Pontoriero
et al. 1988, Lekovic et al. 1989, 1990, Blumenthal 1993,
Machtei et al. 1993, 1994, Black et al. 1994, Laurell et
al. 1994, Mellonig et al. 1994, Wang et al. 1994, Hu-
goson et al. 1995, Poison et al. 1995b). The reported
mean values ranged from 0.1 mm to 3.5 mm for V-CAL
gain and from 1 mm to 4 mm for PPD reduction.
The effect of using barrier membranes for the treat
-
ment of mandibular degree II furcations was investi-
gated in six controlled randomized clinical trials in
which GTR procedures were directly compared to flap
surgery (Table 28-5). Sixty-six furcations treated with
flap surgery and 87 treated with GTR were included.
Three of the four studies reporting H-CAL gains con-
cluded that GTR resulted in statistically significantly
greater horizontal attachment level gains than flap
surgery (Pontoriero et al. 1988, Van Swol et al. 1993,
Wang et al. 1994). The weighted mean of the results
reported in Table 28-5 indicated that the H-CAL in
furcations treated with GTR was 2.5 ± 1 mm (95% CI
REGENERATIVE PERIODONTAL THERAPY . 687
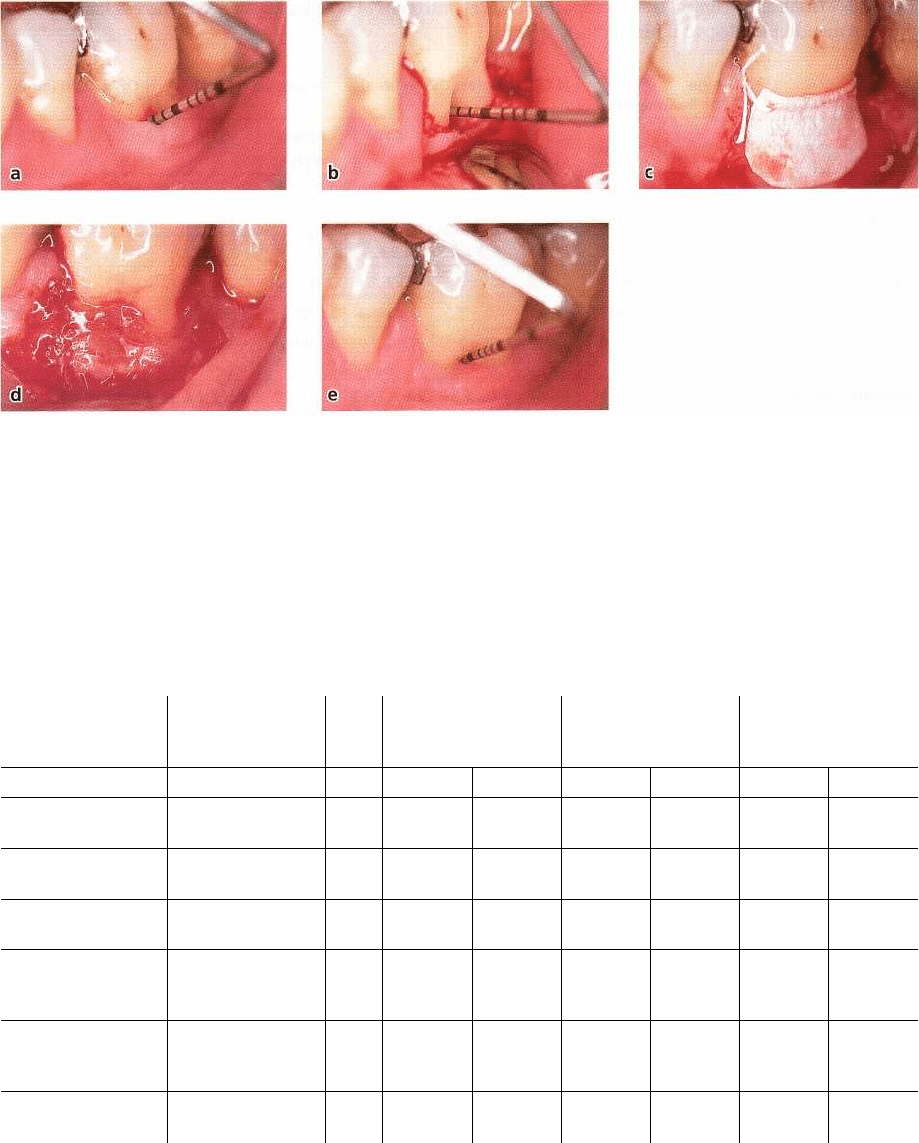
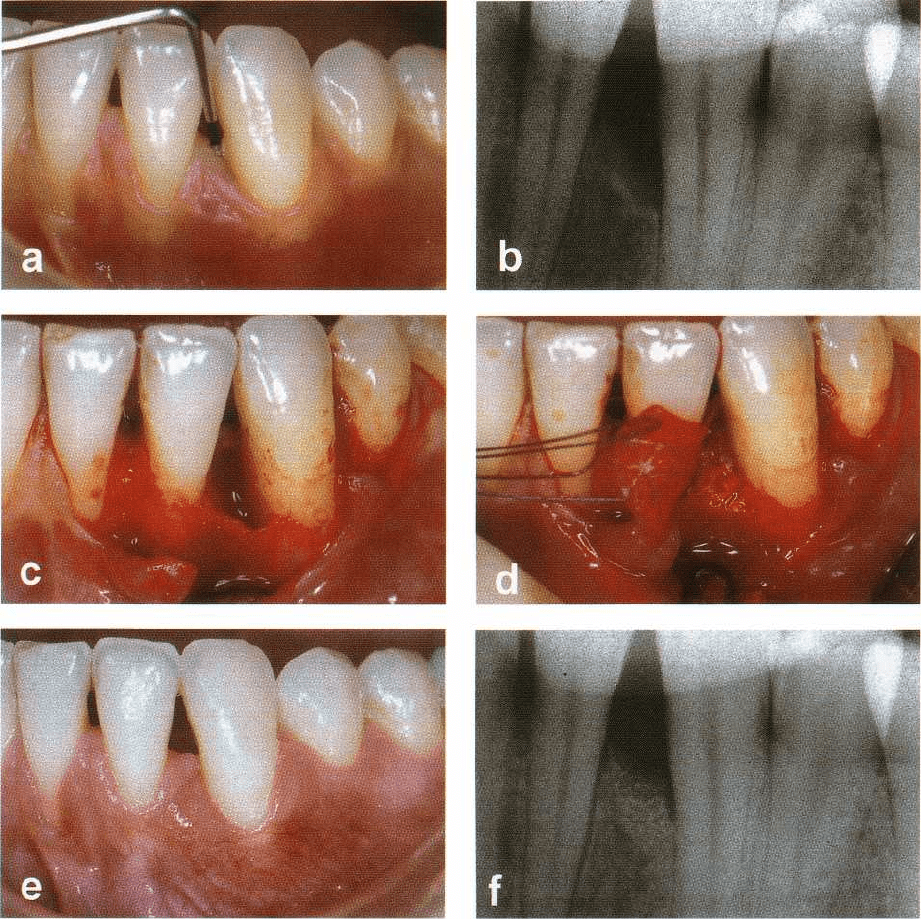
Fig. 28-37. (a) Left mandibular first molar presenting with a deep degree II furcation involvement. (b) Horizontal
loss
of tooth support of 7 mm was probed. (c) An e-PTFE barrier membrane has been trimmed and sutured to cover
the
furcation. (d) At membrane removal after 5 weeks, newly formed tissue fills the furcation completely. (e) At 1
year,
a 3 mm gain of tooth support was measured, but a residual 4 mm degree II furcation involvement was still
present.
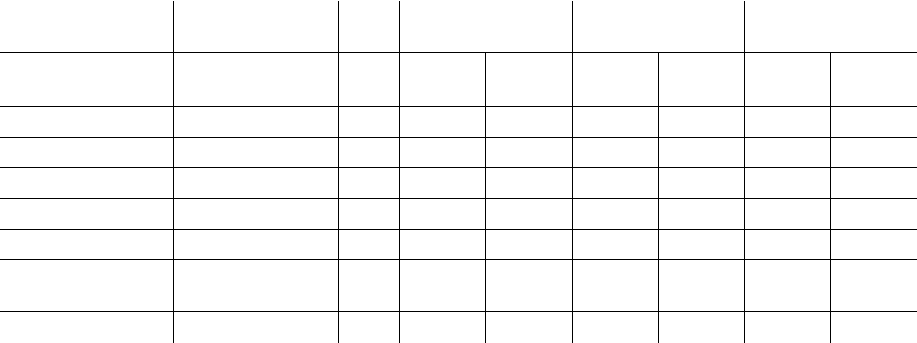
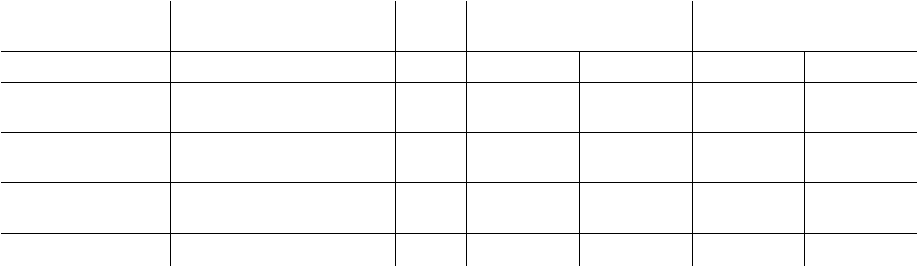
Table 28-4. Controlled clinical trials comparing clinical outcomes of GTR procedures with e-PTFE non- bioab-
sorbable barrier membranes with different types of bioabsorbable barrier membranes in mandibular degree
II
furcations
Authors
Design
&
Treatment (GTR
C/GTR T)
N C/T
Defect Depth (mm)
H-CAL Gain (mm) H-OPAL Gain (mm)
GTR C GTR T GTR C GTR T GTR C GTR T
Yukna 1992 Intraindividual
(e-PTFE/FDDMA)
11/11
3.0±? 4.0±?
NA NA
1.0±? 2.0±?
Blumenthal 1993
Intraindividual
(e-PTFE/Collagen)
12/12
4.4 ± 0.9 4.5 ± 0.9 1.8 ± 1 2.5 ± 0.8 1.7 ± 0.5 2.5 ± 0.7
Bouchard et al. 1993
Intraindividual
(e-PTFE/Conn. Graft)
12/12
NA NA
2.8 ± 1.3*
1.5 ± 2 2.2 ± 1.4 1.5 ± 1.1
Black et al. 1994
Intraindividual
(e-PTFE/Collagen)
13/13
4.3 ± 2 4.4 ± 1.5 0.8 ± 2.2 1.5 ± 2
NA NA
Hugoson et al. 1995
Intraindividual
(e-PTFE/Polytetra-
fluoroethylene)
38/38
5.9 ± 1.3 5.6 ± 1.4
1.4 ± 2.2* 2.2 ± 2.0*
NA NA
Weighted Mean
86/86
4.9±1.4§
5±1.3§
1.6±1.9#
2±1.7# 1.3±1#
1.4±0.9#
GTR C = Guided Tissue Regeneration Control Treatment. GTR T = Guided Tissue Regeneration Test Treatment.
N Cif = Number of defects in the Control (C) and in the Test (T) treatment arm.
H-CAL = Horizontal Clinical Attachment. H-OPAL = Horizontal Open Probing Attachment. NA = data not available.
e-PTFE = expanded Polytetrafluoroethylene. FDDMA = Freeze Dried Dura Mater Allograft. Conn. Graft = Connective Tissue Graft.
= Difference between treatments statistically significant. § N = Mean (74) ± S.D. (63); * N = Mean (75) ± S.D. (75); # N = Mean (35) ± S.D. (24).
2.1-2.9 mm) while the flap surgery resulted in a mean
H-CAL gain of 1.3 ± 1 mm (95% CI.0.8-1.8 mm). These
results indicate an added benefit from GTR in the
treatment of mandibular degree II furcations.
Maxillary degree
II
furcations
Results reported in three controlled studies (Metzeler
et al. 1991, Mellonig et al. 1994, Pontoriero & Lindhe
1995a) comparing GTR treatment of maxillary degree
II
furcations with non-bioabsorbable e-PTFE mem
branes
and with open flap debridement, indicate that
GTR
treatment of such defects is generally unpredictable.
Metzeler et al. (1991) in a study including 17
pairs of
degree II furcations measured CAL gains of
688 • CHAPTER 28
Table 28-5. Controlled clinical trials comparing clinical outcomes of GTR procedures with access flap proce
-
dures in mandibular degree II furcations
Authors
Design
(GTR Treatment)
N C/T
Defect Depth (mm)
H-CAL Gain (mm) H-OPAL Gain (mm)
Access
Flap
GTR
Access
Flap
GTR
Access
Flap
GTR
Pontoriero et al. 1988
Intraindividual (e-PTFE)
21/21
4.0 ± 0.8
4.4
±
1.2
2.0 ± 1.2* 3.8 ± 1.2*
NA NA
Lekovic et al. 1989
Intraindividual (e-PTFE)
6/6
NA NA NA
-0.1 ± 0.3
0.2 ± 0.5
Caffesse et al. 1990
Parallel (e-PTFE)
6/9
5.3 ± ?
4.8
0.3 ± ? 0.8 ± ?
NA NA
Van Swol et al. 1993
Parallel (Collagen)
10/28
5.7 ± 2.5
5.1
±
4
0.7 ± 1.2* 2.3 ± 1*
0.8 ± ? 1.7 ± ?
Mellonig et al. 1994
Intraindividual (e-PTFE)
6/6
7.5 ± 2.3
:
NA NA
1.1 ± 1.3* 4.5 ± 1.6*
Wang et al. 1994
Intraindividual
(Collagen)
12/12
5.6 ± 2.7
• 1
±
2.7
1.1 ± 0.6* 2.0 ± 0.4*
1.5 ± ? 2.5 ± ?
Weighted Mean
66/87
5.4±1.8§5.5±1.5$
1.3±1^
2.5±1#
1±1°
2.3±1.2t
N C/T = Number of defects in the Control (C) and in the Test (T) treatment arm.
H-CAL = Horizontal Clinical Attachment. H-OPAL = Horizontal Open Probing Attachment. NA = data not available.
e-PTFE = expanded Polytetrafluorethylene. * = Difference between treatments statistically significant.
§ N = Mean (60) ± S . D. (54); $ N = Mean (81) ± S. D. (72);
A
N = Mean (49) ± S.D. (43); # N = Mean (70) ± S. D. (61); N = Mean (39) ± S.D. (17); N
= Mean (57) ± S.D. (17).
1.0 ± 0.9 mm in the GTR treated sites versus 0.2 ± 0.6
mm in the control sites. Following re-entry, horizontal
probing attachment gains (H-OPAL) of 0.9 ± 0.4 mm
and 0.3 ± 0.6 mm were detected in the GTR and flap
treated furcations, respectively. No differences were
found and none of the furcations of the two groups
were completely resolved. Similarly, Mellonig et al.
(
1994) treated eight pairs of maxillary degree II furca-
tions which resulted in H-OPAL gains of 1.0 mm (GTR
sites) and 0.3 mm (flap treated sites). No differences
were found and none of the treated furcations were
completely closed. Pontoriero & Lindhe (1995a), on
the other hand, in a study on 28 maxillary degree II
furcations found a significant gain in CAL (1.5 mm)
and horizontal bone (1.1 mm) in buccal degree II
furcations.
Although these three investigations show a slight
clinical improvement following treatment of degree II
maxillary furcations with GTR, the results are gener-
ally inconsistent.
Degree III fir reations
Four investigations on the treatment of mandibular
degree III furcations (Becker et al. 1988, Pontoriero et
al. 1989, Cortellini et al. 1990, Pontoriero & Lindhe
1995b) indicate that the treatment of such defects with
GTR is unpredictable. A controlled study of Pontori-
ero et al. (1989) showed that only 8 out of 21 "through
and through" mandibular furcations treated with
non-bioabsorbable barrier membranes healed with
complete closure of the defect. Another ten defects
were partially filled, and three remained open. In the
control group, treated with open flap debridement,10
were partially filled and 11 remained open. Similar
results were reported by Cortellini et al. (1990) who,
in a case cohort of 15 degree III mandibular furcations,
found that 33% of the defects had healed completely,
33% were partially closed, and 33% were still through
and through following treatment. Becker et al (1988)
did not observe complete closure of any of 11 treated
degree III mandibular furcations. Similarly, in a con-
trolled clinical trial of Pontoriero & Lindhe (1995b) on
11 pairs of maxillary degree III furcations randomly
assigned to GTR or flap surgery, none of the furcation
defects were closed.
Factors affecting the clinical outcomes of GTR in
furcations
The studies considered above have demonstrated that
treatment of maxillary degree II furcations and maxil-
lary and mandibular degree III furcation involve-
ments with GTR is unpredictable, while clinical im-
provements can be expected treating mandibular de-
gree II furcations. The great variability in clinical out-
comes, following treatment of mandibular degree II
furcations with GTR, is probably related to the factors
discussed relative to intrabony defects.
Regarding defect factors, it was shown that first and
second mandibular molars and buccal and lingual
furcations respond equally well to GTR treatment
(
Pontoriero et al. 1988, Machtei et al. 1994). It was also
demonstrated that the preoperative horizontal pocket
depth is directly correlated with the magnitude of
attachment gain and bone formation in the furcation
area (Machtei et al. 1993, 1994). The deeper the base
-
line horizontal pocket, the greater was the H-CAL and
bone gain. The anatomy of the furcations in terms of
height, width, depth and volume, however, did not
correlate with the clinical outcome (Machtei et al.
1994). Anderegg et al. (1995) demonstrated that sites
with a gingival thickness of > 1 mm exhibited less
gingival recession post surgery than sites with a gin-
gival thickness of < 1 mm. The authors concluded that
the thickness of the gingival tissue covering a barrier
REGENERATIVE PERIODONTAL THERAPY •
689
Table 28-6. Summary of controlled clinical trials evaluating the combined effects of decalcified freeze-dried
bone allografts (DFDBA) and barrier membranes in deep intrabony defects
Authors
Design
(GTR Treatment)
N*
Gains in CAL
(mm)
Significance
Residual PD
(mm)
Significance
GTR GTR
+
GTR GTR
+
DFDBA DFDBA
Chen et al. 1995
Intraindividual
(Collagen)
8
2.0 ± 0.4 2.3 ± 0.5
P > 0.05,NS
4.2 ± 0.4 4.2 ± 0.5
P > 0.05,NS
Mellado et al. 1995
Intraindividual
(e-PTFE)
11
2.0 ± 0.9 2.0 ± 1.4
P = 0.86,NS
NA NA NA
Gouldin et al. 1996
Intraindividual
(e-PTFE)
26
2.2 ± 1.4 2.4 ± 1.6 NS 3.7 ± 1.6 3.7 ± 1.8 NS
Weighted Mean
45 2.1
±
1.1 2.3
±
1.4 3.8
±
1.3
§
3.8
±
1.5
§
= Defects per treatment arm. CAL = Clinical Attachment Level. PD = Pocket Depth. e-PTFE = expanded Polytetrafluoroethylene.
DFDBA = Decalcified Freeze Dried Bone Allograft.
NS = not significant. NA = Data not available. § N = Mean (34) ± S.D. (34).
material must be considered if post-treatment reces-
sion is to be minimized or avoided.
Based on present evidence, it seems that mandibu
-
lar degree II furcations in the first or second molars,
either buccal or lingual, with deep pockets at baseline
and a gingival thickness of > 1 mm, may benefit from
GTR treatment.
GTR combined with other regenerative procedures
Compromised results after GTR may be obtained in
cases where the membrane collapses/falls (partially
or totally) into the defect and/or towards the root
surface, thereby reducing the space available for inva
-
sion of new tissue capable of forming periodontal
ligament and bone in particular. Reduced amounts of
regenerated bone due to membrane collapse were
noticed in early studies of GTR. In the study of
Gottlow et al. (1984), it was observed that collapse of
the membrane towards the root surface resulted in
new cementum formation on the entire exposed root
surfaces, whereas bone regeneration was minimal.
Although the authors reported that the degree of coro
-
nal regrowth of bone was unrelated to the amount of
new cementum formation, they did not comment on
what effect membrane collapse might have had. Re-
cent experimental studies, however, recognized the
negative effect of membrane collapse on periodontal
regeneration generally and on bone formation in par-
ticular (Caton et al. 1992, Haney et al. 1993, Sigurdsson
et al. 1994, Sallum et al. 1998). Haney et al. (1993)
observed a highly significant correlation between the
space provided by the membrane and the amount of
regenerated alveolar bone using a supra-alveolar de-
fect model in dogs. This finding corroborates that of
Cortellini et al. (1995c) who reported that clinical ap-
plication of self-supporting (reinforced with titanium)
e-PTFE membranes, which could be positioned more
coronally than ordinary e-PTFE membranes, yielded
statistically significantly more PAL-gain in intrabony
defects. A particular risk for membrane collapse exists
in cases where the configuration of the defect is inca-
pable of supporting/preserving the membrane at the
position where it was originally placed.
As already discussed, membrane materials must
possess certain characteristics in order to be efficient.
Among those it is important that the membrane is
capable of keeping its shape and integral features,
thereby maintaining the space created adjacent to the
root surface. The e-PTFE membranes reinforced with
titanium are the closest in meeting these requirements
but they have the disadvantage that they are non-re-
sorbable. At present there are no resorbable mem-
branes available that fulfill this requirement suffi-
ciently, which means that the placement of a resor-
bable membrane on, for instance, a wide one-wall
defect involves the risk of membrane collapse. The
collapse may be prevented by means of implantation
of a biomaterial into the defect to support the mem-
brane so that it preserves its original position. How-
ever, the biomaterial to be used for this purpose must
not interfere with the process of periodontal regenera
-
tion and ideally it may also promote bone regenera-
tion.
As previously described, periodontal regeneration
has been attempted with a variety of grafting materi-
als, among which demineralized freeze-dried bone
allografts (DFDBA) apparently facilitated regenera-
tion in humans (Ouhayoun 1996). Schallhorn and
McClain (1988) reported on improved clinical results
in intrabony defects and degree II furcations, follow-
ing a combination therapy including barrier mem-
branes plus DFDBA and citric acid root conditioning.
In three controlled clinical trials, the treatment of a
total of 45 pairs of intrabony defects with DFDBA
grafting and GTR were compared to GTR alone (Table
28-6). The weighted mean of the results of the reported
investigations showed similar gain in CAL in the GTR
group (2.1 ± 1.1 mm, 95% Cl 1.6-2.6 mm) and in the
GTR plus DFDBA group (2.3 ± 1.4 mm, 95% Cl 1.7-2.9
mm). The differences between the two treatments did
690 • CHAPTER 28
Table
28-7.
Controlled clinical trials comparing clinical outcomes of GTR procedures with e-PTFE non- bioab
-
sorbable barrier membranes with or without the adjunctive use of grafts in mandibular degree II furcations
Authors
Design
&
Treatment
(GTR C/GTR T)
N C/T
Defect Depth (mm)
H-OPAL Gain (mm)
GTR C
GTR T
GTR C
GTR T
Lekovic et al. 1990
Intraindividual
(e-PTFE/e-PTFE + HA)
15/15 4.2 ± 0.2 4.3 ± 0.2 0.1 ± 0.1 1.6 ± 0.2
Anderegg et al. 1991
Intraindividual
(e-PTFE/e-PTFE + DFDBA)
15/15 4.2 ± 2.2 5.3 ± 2.6
1.0 ± 0.8* 2.4 ± 1.5*
Wallace et al. 1994
Parallel
(e-PTFE/e-PTFE + DFDBA)
7/10
6.0 ± ? 6.5 ± ? 2.3 ± ? 2.4 ± ?
Weighted Mean
37/40
4.5
±
1.2 §
5.2
±
1.4 t
0.9
±
0.5 § 2.1
±
0.9 #
GTR C = Guided Tissue Regeneration Control Treatment. GTR T = Guided Tissue Regeneration Test Treatment. N C/T = Number of defects in the
Control
(C) and in the Test (T) treatment arm. H-OPAL = Horizontal Open Probing Attachment.
e-PTFE = expanded Polytetrafluoroethylene. I-IA = Hydroxylapatite. DFDBA = Decalcified Freeze Dried Bone Allograft.
= Difference between treatments statistically significant. N = Mean (37) ± S.D. (30); t N = Mean (40) ± S.D. (30)
# N = Mean (35) ± S. D. (24).
not reach statistical significance, thus indicating no
added effect of combining DFDBA with barrier mate-
rials in the treatment of intrabony defects. Guillemin
et al.
(1993),
on the other hand, compared the effect of
DFDBA alone with a combination of barrier materials
and DFDBA in 15 pairs of intrabony defects. Both
treatments resulted in significant amounts of CAL
gains and bone fill at
6
months, but no difference was
found between the treatments.
In three studies on mandibular degree II furcations,
GTR treatment alone was compared with GTR treat-
ment combined with hydroxylapatite or DFDBA (Ta-
ble
28-7).
In one of these investigations, a statistically
significant improvement was found in terms of hori-
zontal open probing attachment levels (H-OPAL) in
the group of furcations treated with the combination
therapy (Anderegg et al. 1991).
In another of these
three studies the difference between the two treat-
ments was not statistically significant, but the combi-
nation therapy resulted in a greater extent of furcation
fill (Lekovic et al.
1990).
In the third investigation
(
Wallace et al.
1994),
the two treatments were equiva-
lent in terms of H-OPAL gains. The weighted mean of
the cited studies showed greater H-OPAL gains in the
cases treated with the combination therapy
(2.1 ± 0.9
mm,
95%
Cl
1.6-2.6
mm) when compared to GTR
treatment alone
(0.9 ± 0.5
mm,
95%
Cl
0.6-1.1
mm),
indicating a possible added benefit from the use of
grafting materials in combination with non-bioabsor-
bable barrier membranes for the treatment of
mandibular degree II furcations.
Promising clinical results with a PAL-gain of
1.0-5.5
mm were obtained in human case reports, in which
the GTR technique was combined with grafting of
Bio-Oss
®
for the treatment of intrabony periodontal
defects (Lundgren & Slotte
1999,
Mellonig
2000,
Pao-
lantonio et al.
2001).
The combined Bio-Os
s
®
and GTR
treatment resulted in greater PPD reduction, PAL gain
and defect fill than the mere implantation of Bio-Os
s
®
in case series (Camelo et al.
1998,
Hutchens
1999)
and
than flap surgery alone in a split-mouth study
(
Camargo et al. 2000).
In a recent randomized controlled clinical study
including
60 patients (Stavropoulos et al.
2002),
Bio-
Oss
®
alone or impregnated with gentamicin was used
as an adjunct to GTR in the treatment of one-wall or
two-wall intrabony defects, and the outcomes were
compared to those obtained following GTR alone or
flap surgery. Treatment with a membrane alone (Fig.
28-38)
resulted in a mean PAL gain of
2.9
mm, while it
was
3.8
and
2.5
mm, respectively, when Bio-Oss
®
grafts with or without gentamicin were placed in the
defects prior to membrane coverage (Fig. 28-39).
The
control defects treated with flap surgery demon-
strated a gain of PAL of only
1.5
mm. The clinical
improvements in defects treated with GTR alone or in
combination with Bio-Oss
®
grafting were signifi-
cantly better than those obtained with flap surgery,
whereas the differences between the groups treated
with membranes were not statistically significant.
In a controlled study (Pietruska
2001),
similar clini-
cal improvements were obtained when Bio-Oss
®
com-
bined with GTR was compared with biomodification
of the root surface with enamel matrix protein (Em-
dogain
"
).
Camelo et al.
(1998)
and Mellonig
(2000)
presented
histologic data indicating that the use of Bio-Oss
®
under a membrane may result in partial regeneration
of the periodontal apparatus, but in all the cases, most
of the defect was still occupied by deproteinized bone
particles. Bone was not observed near the root, and the
connective tissue fibers of the "new" periodontal liga-
ment were mostly oriented parallel to the root surface.
These results corroborate findings reported by Pao-
lantonio et al.
(2001),
who observed only limited bone
formation in the vicinity of the pre-existing bone in a
biopsy, taken from a site treated
8 months earlier with
Bio-Os
s
®
and a collagen membrane. Most of the space
in the defect was occupied by Bio-Oss ® particles em-
bedded in connective tissue. However, in a case report,
REGENERATIVE PERIODONTAL THERAPY • 691
Fig. 28-38. Right lateral maxillary incisor with an 8 mm deep pocket associated with an intrabony defect on the dis
tal aspect (a), as seen on the radiograph (b). Full thickness buccal and palatal flaps have been raised and the
defect
has been debrided (c). A bioabsorbable membrane has been adopted over the defect (d). The level of the
interdental
gingiva is maintained after 1 year (e) and the intrabony defect (f) is resolved.
where intrabony defects were treated with Bio-Oss
®
combined with intraoral autogenous bone and GTR,
new attachment formation had occurred consistently,
but a major portion of the regenerated osseous tissue
consisted of deproteinized bone particles (Camelo et
al. 2001). The effect of combining citric acid root bio-
modification with GTR treatment was evaluated in
two randomized controlled clinical trials in intrabony
defects. The first investigation (Handelsman et al.
1991) demonstrated significant amounts of CAL gains
in both the test (e-PTFE membranes and citric acid;
CAL gain 3.5 ± 1.6 mm) and control sites (e-PTFE
membranes alone; CAL gain 4.0 ± 1.4 mm). Less favor
-
able results following these two treatment modalities
were reported by Kersten et al. (1992) who found CAL
gains of 1.0 ± 1.1 mm in the test group, and CAL gains
of 0.7 ± 1.5 mm in the control group. Both studies,
however, failed to demonstrate any added effect of the
use of citric acid in combination with non-bioabsor-
bable barrier membranes.
Root surface biomodification with tetracycline
alone and in combination with GTR was evaluated in
two controlled studies on degree II furcations (
Machtei et al. 1993, Parashis & Mitsis 1993). Both
investigations failed to show significant differences
between sites treated with non-bioabsorbable barrier
membranes alone or in combination with tetracycline
root surface biomodification. Similarly, the use of
other surface active chemicals like EDTA also failed to
692 • CHAPTER 28
Fig. 28-39. Left mandibular canine with an 8 mm deep pocket (a) associated with an intrabony defect on its mesial
aspect (b). The defect is debrided after flap elevation (c) and Bio-Os
s
®
particles are placed in the defect (d) prior to
placement of a bioabsorbable membrane. After 1 year (e) no gingival recession has occurred and the intrabony de
-
fect is almost resolved (f).
provide a significant added effect to GTR treatment in
humans (Lindhe & Cortellini
1996).
Evaluation of GTR
Several reports, case series and controlled clinical tri-
als have demonstrated successful results following
GTR treatment of a variety of periodontal defects (for
review see Cortellini & Tonetti 2000a, Sanz & Giovan
-
noli
2000,
Trombelli
1999).
These results have been
confirmed in animal experiments involving GTR
treatment of intrabony defects (Caffesse et al.
1988,
Caton et al.
1992),
furcation defects (Niedermann et al.
1989,
Caffesse et al.
1990,
Araujo et al.
1996)
and
recession defects (Gottlow et al.
1990,
Cortellini et al.
1991).
The effect of placing non-bioabsorbable or
bioabsorbable membranes on degree II and III furca-
tion defects as compared to that in control defects
treated without membranes was evaluated in dogs
(
Claffey et al.
1989,
Caffesse et al.
1990,
Pontoriero et
al.
1992,
Lindhe et al.
1995).
In both degree II and III
furcation defects, GTR treatment resulted in signifi-
cantly more gain of connective tissue attachment and
regrowth of alveolar bone than control therapy.
In the studies of Pontoriero et al.
(1992)
and Lindhe
et al.
(1995),
complete closure of through and through
furcation defects with the formation of a periodontal
ligament and regrowth of the alveolar bone was
achieved (Fig.
28-40).
It was suggested that the size of
the furcation defects as well as the shape of the sur-
rounding alveolar bone were determining for the out-
REGENERATIVE PERIODONTAL THERAPY •
6
93
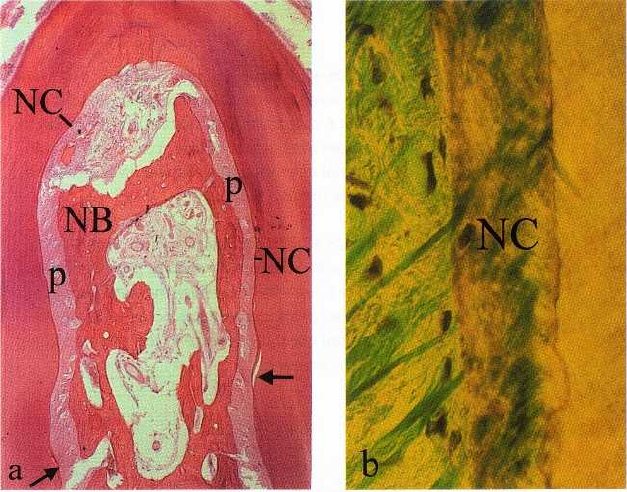
Fig. 28-40. (a) Photomicro-
graph of a degree III furcation
in a dog 5 months after GTR
treatment in combination with
coronally displaced flaps. The
defect has become filled with
new bone (NB), and a peri-
odontal ligament (p) and new
cementum (NC) can be seen
along the entire surface of the
furcation defect. The arrows in
dicate the apical level of the
original defect. (b) A high mag-
nification of the cementum
formed on the root surface in a
healed bifurcation defect. Note
the cellular nature of the new
cementum (NC).
come of GTR treatment. The treatment failures were
consistently associated with recession of the covering
tissue flaps, which resulted in exposure of the furca-
tion defect. Provided this was prevented, even com-
paratively large furcation defects were successfully
regenerated by GTR therapy. The results also demon-
strated that bioabsorbable membranes provided a bar
-
rier which was equally as effective as that of non-
bioabsorbable Teflon membranes.
Histologic evidence in humans that regeneration of
the attachment apparatus on previously periodontitis
affected roots can be attained by means of the GTR
technique was provided in several reports (Nyman et
al. 1982, Gottlow et al. 1986, Becker et al. 1987, Stahl et
al. 1990a, Stahl & Froum 1991b, Cortellini et al. 1993a,
Parodi et al. 1997, Vincenzi et al. 1998, Sculean et al.
1999a). New cementum, periodontal ligament and
variable amounts of new bone formation were ob-
served in these studies, also above notches placed in
the root surface at the apical extent of calculus. Thus,
the GTR technique is fulfilling the criteria set by the
American Academy of Periodontology at the World
Workshop in Periodontics in 1996, and is also based
on a biologic concept that, according to the current
knowledge about periodontal wound healing, can ex-
plain why this method leads to periodontal regenera-
tion.
Long-term evaluation
A pertinent question with respect to regenerative
treatment is whether the achieved attachment gain
can be maintained over an extended period of time. In
a study in monkeys (Kostopoulos & Karring 1994),
periodontal breakdown was produced by the place-
ment and retention of orthodontic elastics on experi-
mental teeth until 50% bone loss was recorded. The
experimental teeth were endodontically treated and
subjected to a flap operation and all granulation
tissue
was removed. The crowns of the teeth were resected
at the level of the cemento-enamel junction and a
barrier membrane was placed to cover the roots before
they were submerged. Following 4 weeks of healing,
the membranes were removed. At the same time the
contralateral teeth which served as controls were en-
dodontically treated and subjected to a sham opera-
tion during which the crowns were resected at the
level of the cemento-enamel junction. Artificial com-
posite crowns were then placed on both the experi-
mental and the control roots. The sites were allowed
to heal for 3 months during which period careful
plaque control was performed. At the end of this
period cotton-floss ligatures were placed on both ex-
perimental and control teeth to induce periodontal
tissue breakdown. After another 6 months, the ani-
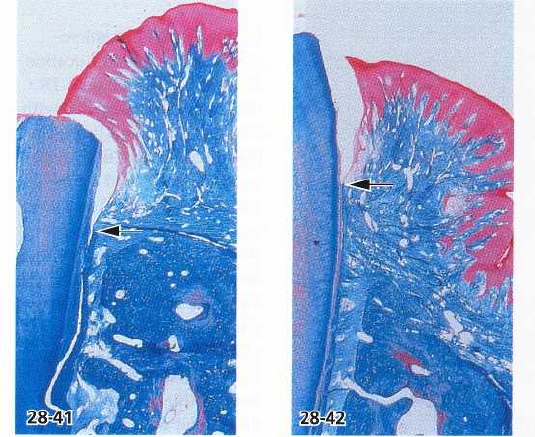
mals were sacrificed. With respect to attachment level,
bone level, pocket depth and gingival recession, simi-
lar results were recorded in histologic specimens of
experimental (Fig. 28-41) and control (Fig. 28-42) teeth.
This indicates that the new connective tissue attach-
ment formed with GTR is not more susceptible to
periodontitis than the naturally existing periodon-
tium.
In a long-term follow-up study, Gottlow et al. (1992)
assessed the stability of new attachment gained
through GTR procedures. Eighty sites in 39 patients,
which 6 months after surgery exhibited a gain of
clinical attachment of 2 mm (2-7 mm), were moni-
tored during additional periods of 1 to 5 years. Of the
80 sites, 65 were monitored for 2 years, 40 for 3 years,
17 for 4 years and 9 sites for 5 years. The results of this
study and those of other trials indicate that attachment
gain obtained following GTR treatment can be main-
tained on a long-term basis (Becker & Becker 1993,
McClain & Schallhorn 1993).
An investigation on intrabony defects demon-
strated that the stability of sites treated with GTR was
694 • CHAPTER
28
Fig. 28-41. Microphotograph of test specimen
with a reformed connective tissue attachment.
After 6 months of ligature induced periodonti
-
tis, loss of attachment has occurred from the
coronal cut root surface to the level indicated
by the arrow.
Fig. 28-42. Microphotograph of control speci-
men with a naturally existing periodontium.
After 6 months of ligature induced periodonti
-
tis, loss of attachment has occurred from the
coronal cut tooth surface to the level indicated
by the arrow.
dependent on participation of the patients into a recall
program, and on the absence of bacterial plaque,
bleeding on probing and re-infection of the treated
sites with periodontal pathogens (Cortellini et al.
1994). In addition, the susceptibility to disease recur-
rence at sites treated with non-bioabsorbable barrier
membranes was compared to that at sites treated with
root planing in a controlled clinical trial (Cortellini et
al. 1996a). The results indicated that patient factors
such as compliance with oral hygiene, smoking hab-
its, and susceptibility to disease progression rather
than the employed treatment modality, were the major
determinants of stability of the treated sites.
A few studies have evaluated the long-term prog-
nosis for furcation defects treated with regenerative
therapy. Sixteen mandibular degree II furcation de-
fects, following coronal flap positioning and citric acid
root biomodification with and without implantation
of
demineralized freeze-dried bone allografts
(DFDBA),
were determined as completely resolved
with bone fill
assessed by re-entry surgery. They were
re-evaluated
after 4-5 years (Haney et al. 1997), when
12 of the 16
sites exhibited recurrent degree II furca
tions and all
16 sites demonstrated probable buccal
furcation
defects. The investigators concluded that
these
findings question the long-term stability of bone
regeneration in furcations following coronally ad-
vanced flap procedures.
The long-term stability of mandibular furcation de-
fects regenerated following GTR alone or in combina-
tion with root surface biomodification with citric acid
and bone grafting, was also evaluated by McClain &
Schallhorn (1993). Out of the 57% of the furcation
defects which were assessed as completely filled at 6
and 12 months, only 29% were completely filled after
4 to 6 years. However, 74% of the furcations treated
with GTR in combination with the placement of
DFDBA were completely filled at both the short and
long-term evaluation, suggesting that the results ob-
tained with the combined procedure were more stable
over time. Long-term results of GTR treatment of
mandibular degree II furcations with e-PTFE mem-
branes were also reported by Machtei et al. (1996). The
teeth were followed up to 4 years and compared with
non-furcated molars. Improvements assessed in ver-
tical (V-CAL) and horizontal (H-CAL) clinical attach-
ment levels after treatment were maintained also after
4 years, suggesting that changes obtained in degree II
furcation defects by GTR are stable. Only 9% of the
treated defects were unstable, which was similar to
that observed for non-furcated molars. Good oral hy-
giene as reflected in low plaque scores and elimination
of periodontal pathogens were closely related to the
long-term stability. On the basis of these results, it was
concluded that furcation defects treated with mem-
brane barriers can be maintained in health for at least
4 years, provided good oral hygiene and frequent
recall visits are established.
CONCLUSIONS
GTR represents the most well-documented regenera-
tive procedure for obtaining periodontal regeneration
in intrabony defects and in degree II furcations. GTR
has demonstrated significant clinical improvements
beyond that achieved with only debridement in such
defects. Regarding degree II maxillary furcations, the
results following GTR treatment are inconsistent, and
the treatment of degree III furcation defects is unpre-
dictable. An added benefit may be obtained by the use
of grafting materials in combination with GTR in some
situations.
