Jan Lindhe. Clinical Periodontology
Подождите немного. Документ загружается.

REGENERATIVE PERIODONTAL THERAPY • 675
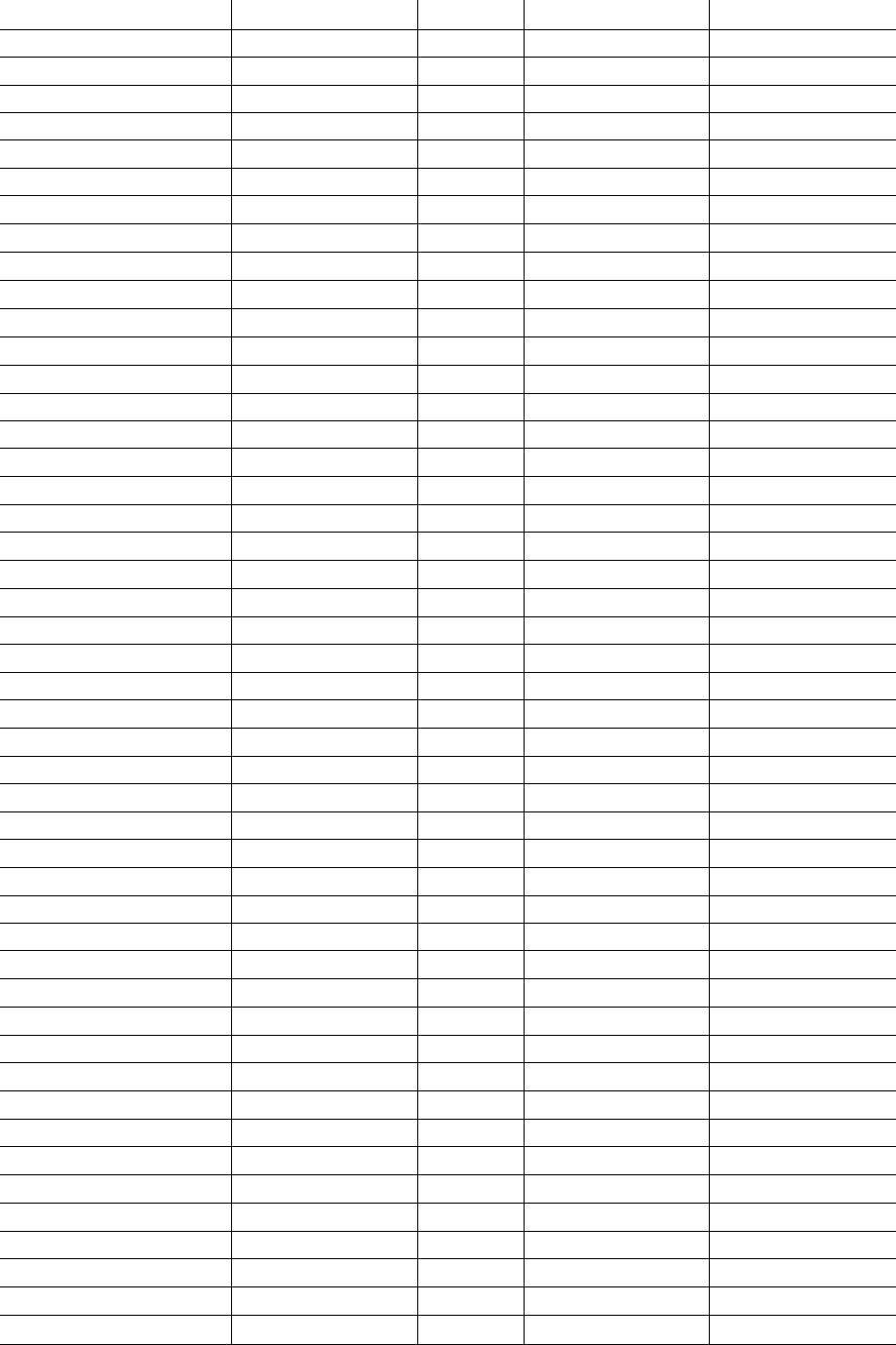
Table 28-1. Clinical outcomes of GTR treatment of deep intrabony defects
Authors
Membranes
N
Gains in CAL ± SD (mm)
Residual PPD
±
SD (mm)
Becker et al. 1988 e-PTFE
9
4.5 ± 1.7 3.2 ± 1.0
Chung et at 1990
collagen
10
0.6 ± 0.6
Handelsman et at 1991
e-PTFE
9
4.0 ± 1.4 3.9 ± 1.4
Karsten et al. 1992
e-PTFE
13
1.0 ± 1.1 5.1 ± 0.9
Proestakis et al. 1992
e-PTFE
9
1.2 ± 1.3 3.5 ± 0.9
Quteish & Dolby 1992
collagen
26
3.0 ± 1.5 2.2 ± 0.4
Selvig et al. 1992
e-PTFE
26
0.8 ± 1.3
5.
4
Becker & Becker 1993
e-PTFE
32 4.5
3.9 ± 0.3
Cortellini et al. 1993b
e-PTFE
40
4.1 ± 2.5 2.0 ± 0.6
Falk et al. 1993
polylactic acid
25
4.5 ± 1.6 3.0 ± 1.1
Cortellini & Rini-Prato 1994
rubber dam
5
4.0 ± 0.7 2.4 ± 0.5
Laurell et al. 1994
polylactic acid
47
4.9 ± 2.4 3.0 ± 1.4
Al-Arrayed et al. 1995
collagen
19 3.9
2.
5
Chen et al. 1995
collagen
10
2.0 ± 0.4 4.2 ± 0.4
Cortellini et al. 1995c
e-PTFE
15
4.1 ± 1.9 2.7 ± 1.0
Cortellini et al. 1995c e-PTFE+titanium
15
5.3 ± 2.2 2.1 ± 0.5
Cortellini et al. 1995a
e-PTFE+FGG
14
5.0 ± 2.1 2.6 ± 0.9
Cortellini et al. 1995a
e-PTFE
14
3.7 ± 2.1 3.2 ± 1.8
Cortellini et al. 1995b
e-PTFE+fibrin
11
4.5 ± 3.3
1.
7
Cortellini et al. 1995b
e-PTFE
11
3.3 ± 1.9
1.
9
Mattson et al. 1995
collagen
13
2.5 ± 1.5 3.6 ± 0.6
Mattson et al. 1995
collagen
9
2.4 ± 2.1 4.0 ± 1.1
Mellado et al. 1995
e-PTFE
11
2.0 ± 0.9
Becker et al. 1996
polylactic acid
30
2.9 ± 2.0 3.6 ± 1.3
Cortellini et al. 1996c
polylactic acid
10
4.5 ± 0.9 3.1 ± 0.7
Cortellini et al. 1996b
e-PTFE
12
5.2 ± 1.4 2.9 ± 0.9
Cortellini et al. 1996b
polylactic acid
12
4.6 ± 1.2 3.3 ± 0.9
Gouldin et al. 1996
e-PTFE
25
2.2 ± 1.4 3.5 ± 1.3
Kim et al. 1996
e-PTFE
19
4.0 ± 2.1 3.2 ± 1.1
Murphy 1996
e-PTFE+ITM
12
4.7 ± 1.4 2.9 ± 0.8
Tonetti et al. 1996b
e-PTFE
23
5.3 ± 1.7
2.
7
Banque et al. 1997
collagen
52
3.6 ± 2.2
3.9 ± 1.7
Caffesse et al. 1997
polylactic acid
6
2.3 ± 2.0 3.8 ± 1.2
Caffesse et a l . 1997
e-PTFE
6
3.0 ± 1 . 2 3.7 ± 1.2
Christgau et al. 1997
e-PTFE
10
4.3 ± 1.2 3.6 ± 1.1
Christgau et al. 1997
polyglactin
10
4.9 ± 1.0 3.9 ± 1.1
Falk et al. 1997
polylactic acid
203
4.8 ± 1.5
3.4±
1.6
Kilic et al. 1997
e-PTFE
10
3.7 ± 2.0 3.1 ± 1.4
Cortellini et al. 1998
polylactic acid
23
3.0 ± 1.7 3.0 ± 0.9
Eickholz et al. 1998
polylactic acid
14
3.4 ± 1.6 3.2 ± 0.7
Smith MacDonald et a].1998
e-PTFE
10
4.3 ± 2.1 3.7 ± 0.9
Smith MacDonald et al. 1998
polylactic acid
10
4.6 ± 1.7 3.4 ± 1.2
Parashis et al. 1998
polylactic acid
12
3.8 ± 1.8 3.5 ± 1.4
Tonetti et al. 1998
polylactic acid
69
3.0 ± 1.6 4.3 ± 1.3
Cortellini et al. 1999 polylactic acid
18
4.9 ± 1.8 3.6 ± 1.2
Pontoriero et al. 1999
Jiff. barriers
30
3.1 ± 1.8 3.3 ± 1.3
Sculean et al. 1999a
polylactic acid
52
3.4 ± 1.4 3.6 ± 1.3
676 • CHAPTER 28
Table
28-1
(contd)
Authors
Membranes
N
Gains in CAL ± SD (mm)
Residual PPD
±
SD (mm)
Dorfer et al. 2000
polylactic acid
15
4.0 ± 1.2 2.7 ± 0.7
Dorfer et al. 2000
polidiossanon
15
3.4 ± 1.9 3.1 ± 1.1
Eickholz et al. 2000
polylactic acid
30
3.9 ± 1.2 2.6 ± 1.0
Karapataki et al. 2000
polylactic acid
10
4.7 ± 0.7 4.2 ± 1.4
Karapataki et al. 2000
e-PTFE
9
3.6 ± 1.7 4.6 ± 1.3
Ratka-Kruger et al. 2000
polylactic acid
23
3.1 ± 2.3 4.7 ± 1.4
Zybutz et al. 2000
polylactic acid
15
2.4 ± 1.9
Zubutz et al. 2000
e-PTFE
14
2.4±
0.8
Cortellini & Tonetti 2001
diff. barriers
26
5.4 ± 1.2 3.3 ± 0.6
Cortellini et al. 2001 polylactic acid
55
3.5 ± 2.1 3.8 ± 1.5
Weighted mean
1283 3.8
±
1.7 3.4
±
1.2
FGG = Free gingival graft
ITM = Interproximal tissue maintenance
REGENERATIVE PERIODONTAL THERAPY • 677
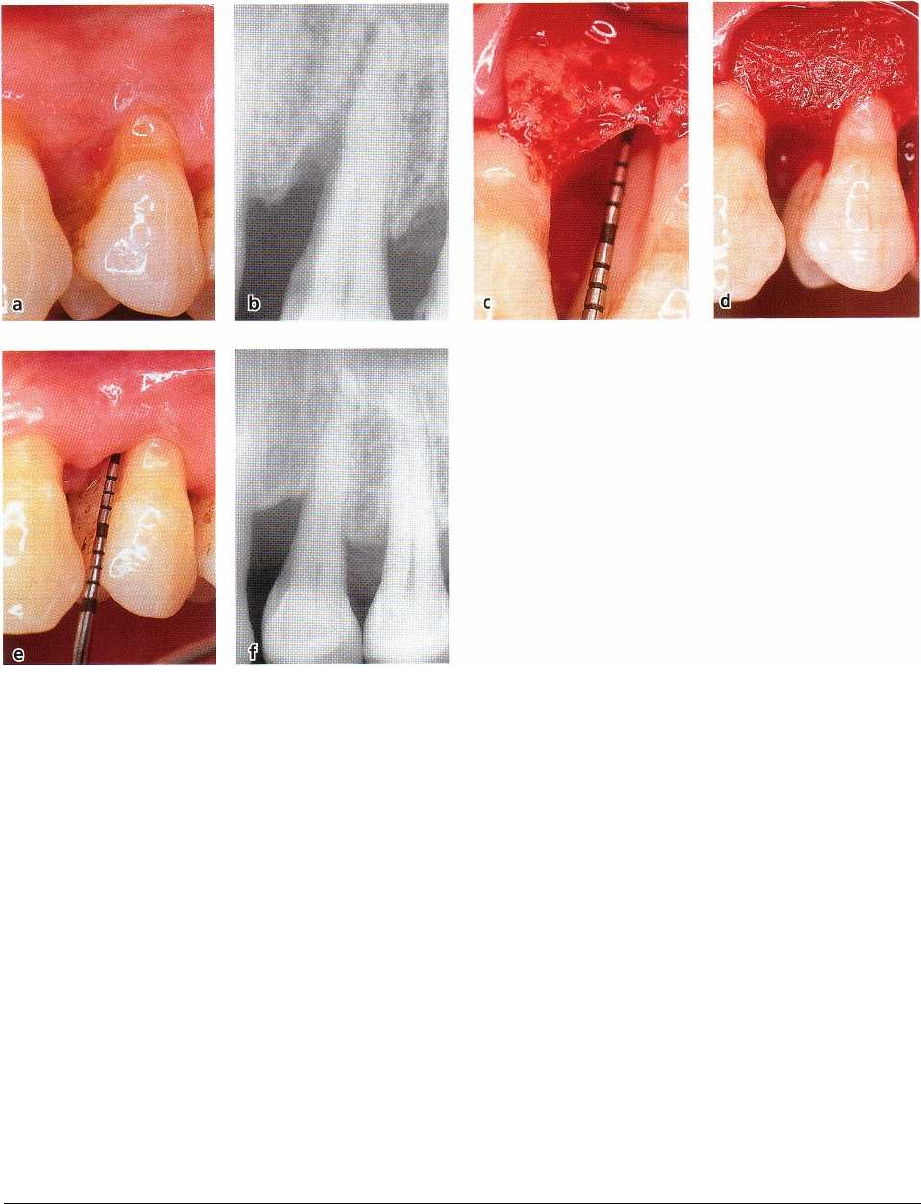
Fig. 28-29. Intrabony defect on the mesial aspect of a left maxillary premolar treated with a bioabsorbable barrier
membrane. (a) Clinical attachment loss was 12 mm. (b) Radiograph showing the presence of a deep interproximal
intrabony defect approaching the apex of the tooth. (c) A 7 mm interproximal intrabony defect was measured after
flap elevation, defect debridement and root planing. (d) A bioabsorbable barrier membrane has been placed and su
-
tured to cover the defect. (e) At 1 year a 4 mm pocket depth and 5 mm clinical gain of attachment were recorded. (f)
The 1-year radiograph shows that the intrabony defect is almost resolved.
treated with GTR was 3.3 ± 1.8 mm (95% CI 2.8-3.6
mm), while the flap surgery resulted in a mean gain
of
2.1 ± 1.5 mm (95% Cl 1.8-2.4 mm). These clinical
results
strongly indicate that there is an added bene
ficial
effect of placing a barrier material over an in
trabony
defect in conjunction with surgery.
Factors affecting clinical outcomes of GTR in intrabony
defects
The results reported in Table 28-1 indicate that clinical
improvements beyond that of flap surgery can be
obtained by treating intrabony defects with GTR, but
they also suggest a great variability in clinical out-
comes among the different studies. In addition, it is
apparent from the results that the complete resolution
of the intrabony component of the defect is observed
in
only a minority of sites. A series of factors associated
with the clinical outcomes were identified using mul-
tivariate approaches (Tonetti et al. 1993a, 1995, 1996a,
Cortellini et al. 1994, Machtei et al. 1994). These studies
have evaluated three types of factors associated with
the
observed variability of the results:
1.
patient factors
2.
defect factors
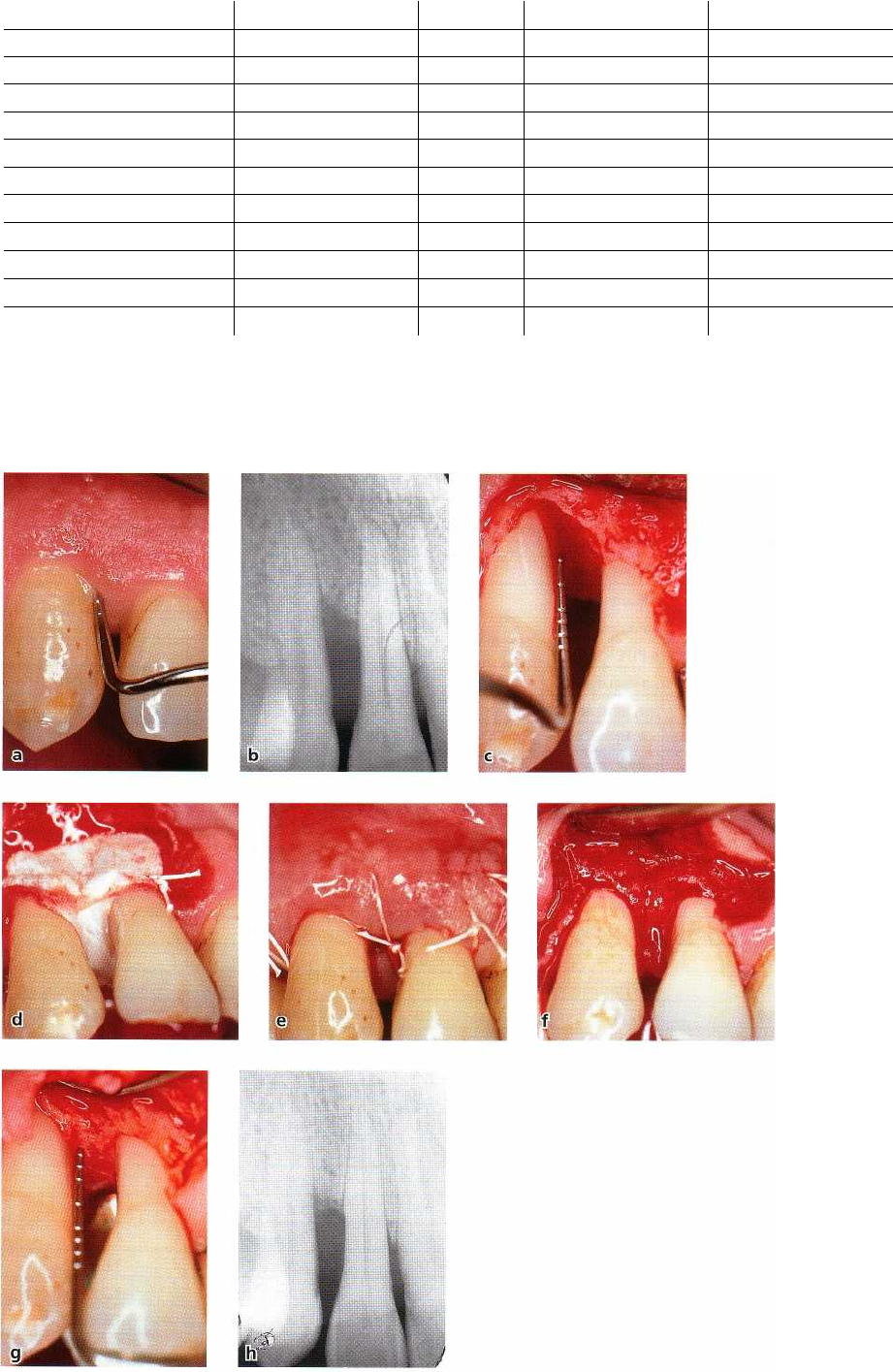
Fig. 28-28. Intrabony defect on the mesial aspect of a right maxillary canine treated with a non-bioabsorbable bar
rier
membrane. (a) The pocket depth is 9 mm and the loss of clinical attachment 10 mm. (b) Radiograph showing the
presence of an interproximal intrabony defect. (c) After full thickness flap elevation, defect debridement, and
root
planing, a 4 mm intrabony defect is evident. (d) An e-PTFE non-bioabsorbable barrier membrane has been tai
lored,
positioned and tightly sutured around the teeth adjacent to the defect. (e) The flap has been repositioned and
sutured
to cover the membrane. Optimal preservation of the soft tissues has been accomplished with an intrasulcu
lar
incision. (f) After removal of the membrane at 5 weeks, the defect appears to be completely filled with newly
formed
tissue. (g) The treated site has been surgically re-entered after 1 year. The intrabony defect is completely
filled with
bone. (h) The 1-year radiograph confirms the complete resolution of the intrabony defect.
678 • CHAPTER 28
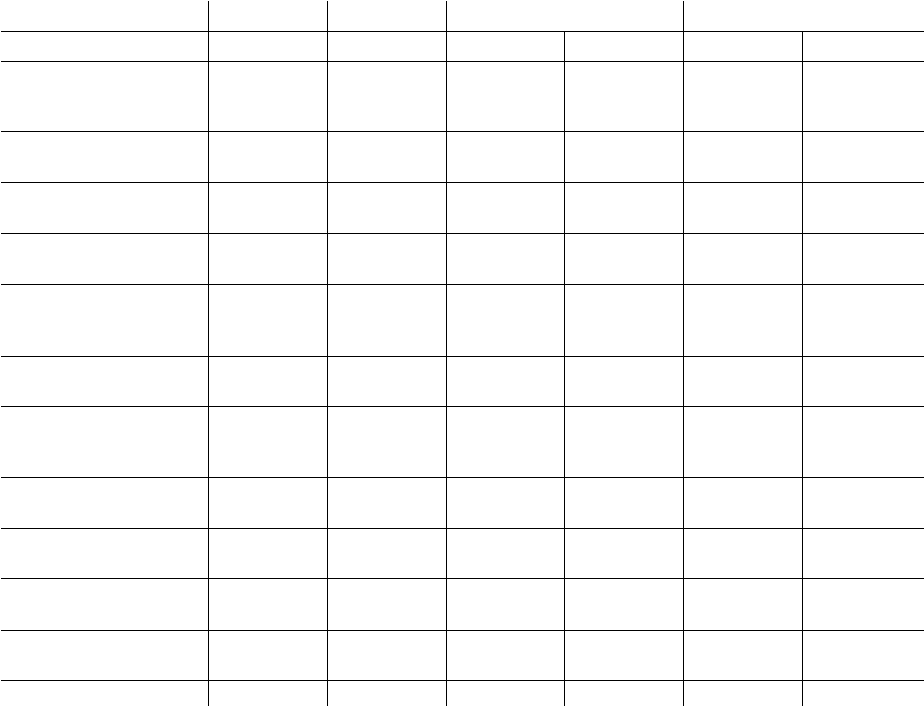
Table 28-2. Controlled clinical trials comparing clinical outcomes of GTR procedures with access flap proce-
dures in deep intrabony defects
CAL = Clinical attachment level
PPD = Probing pocket depth SD =
Standard deviation
3. factors associated with the GTR technique and the
healing period.
Patient factors
The level of self-performed plaque control had a para-
mount influence on the outcome of GTR. In fact, better
clinical attachment level gains were observed in pa-
tients with optimal levels of plaque control as com-
pared with those in patients with poor oral hygiene
(
Cortellini et al. 1994, Tonetti et al. 1995, 1996a). Pa-
tients with plaque on < 10% of the tooth surfaces (full
mouth plaque score, FMPS) had a gain of clinical
attachment which was 1.89 mm greater than that ob
-
served in patients with FMPS > 20% (Tonetti et al.
1995). The authors also demonstrated that cigarette
smoking was associated with reduced attachment
level gains. The attachment gain in subjects smoking
more than 10 cigarettes/day was 2.1 ± 1.2 mm versus
5.2 ± 1.9 mm in non-smokers (Tonetti et al. 1995).
Another important variable is the level of residual
periodontal infection in the dentition. The higher the
level of residual infection, the lower was the attach-
ment gain (Tonetti et al. 1993a, Machtei et al. 1994). It
can be concluded that patient selection is critical to the
success of GTR therapy (Fig. 28-30).
Defect factors
Defect morphology plays a major role in healing fol-
lowing GTR treatment of intrabony defects. This was
demonstrated in studies showing that the depth and
width of the intrabony component of the defect influ-
ence the amount of clinical attachment and bone
gained at 1 year. The deeper the defect, the greater was
the amount of clinical improvements, while the wider
the defect, the lower were the attachment and bone
gains (Garrett et al. 1988, Tonetti et al. 1993a, 1996a).
In a recent controlled study, however, it was dem-
onstrated that deep and shallow defects have the
"
same potential" for regeneration. In this study, deep
defects (deeper than 3 mm) resulted in larger linear
amounts of CAL gains than shallow defects (3.7 ± 1.7
mm versus 2.2 ± 1.3 mm), but the percentage of CAL
gains as related to baseline defect depth was similar
in deep (76.7 ± 27.7%) and in shallow (75.8 ± 45%)
Gains in CAL ± SD (mm) Residual PPD ± SD (mm)
Authors Membranes N GTR Access flap
GTR Access flap
Chung et al. 1990 collagen
10
0.6 ± 0.6
collagen 9 2.4 ± 2.1 4.0 ± 1.1
control
14 -0.7 ± 0.9
Proestakis et al. 1992 e-PTFE 9 1.2 ± 1.3 3.5 ± 0.9
control
9 0.6 ± 1.0 3.7 ± 3.0
Quteish & Dolby 1992 collagen
26
3.0 ± 1.5
2.2 ± 0.4
control
26 1.8 ± 0.9 3.4 ± 0.6
Al-Arrayed et al. 1995 collagen
19 3.9 2.5
control
14 2.7 3.5
Cortellini et al. 1995c e-PTFE
15
4.1 ± 1.9
2.7 ± 1.0
e-PTFE+titanium
15 5.3 ± 2.2
2.1 ± 0.5
control
15 2.5 ± 0.8
3.7 ± 1.3
Mattson et al. 1995 collagen 13 2.5 ± 1.5
3.6 ± 0.6
control 9 0.4 ± 2.1
4.5 ± 1.8
Cortellini et al. 1996b e-PTFE 12 5.2 ± 1.4
2.9 ± 0.9
polylactic acid 12 4.6 ± 1.2
3.3 ± 0.9
control
12 2.3 ± 0.8
4.2 ± 0.9
Tonetti et al. 1998 polylactic acid
69
3.0 ± 1.6
4.3 ± 1.3
control 67 2.2 ± 1.5
4.2 ± 1.4
Pontoriero et al. 1999 diff. barriers
30
3.1 ± 1.8
3.3 ± 1.3
control 30 1.8 ± 1.5
4.0 ± 0.8
Ratka-Kruger et at 2000 polylactic acid
23
3.1 ± 2.3
4.7 ± 1.4
control 21 3.3 ± 2.7
4.9 ± 2.1
Cortellini et al. 2001 polylactic acid 55 3.5 ± 2.1
3.8 ± 1.5
control 54 2.6 ± 1.8
4.7 ± 1.4
Weighted mean 584 3.3 ± 1.8 2.1 ± 1.5
3.5 ± 1.1 4.1 ± 1.3
REGENERATIVE PERIODONTAL THERAPY •
6
79
defects. The width of the intrabony component of the
defects is measured as the angle that the bony wall of
the defect forms with the long axis of the tooth. In a
recent study on 242 intrabony defects, Cortellini &
Tonetti (1999) demonstrated that defects with a radio-
graphic angle of 25° or less gained consistently more
attachment (1.6 mm on average) than defects of 37° or
more.
It was also shown that the number of residual bony
walls was related to the outcomes of various regenera-
tive approaches (Goldman & Cohen 1958, Schallhorn
et al. 1970). This issue as related to GTR therapy was
addressed in three investigations (Selvig et al. 1993,
Tonetti et al. 1993a, 1996a). In one study, the reported
1 year mean clinical attachment level gain was 0.8 ±
1.3 mm. This gain corresponded to the depth of the
three-wall intrabony component of the defect (Selvig
et al. 1993). In the other two investigations, on the
contrary, gains in attachment were not related to the
defect configuration in terms of one-wall, two-wall
and three-wall subcomponents (Tonetti et al. 1993a,
1996a). A total of 70 defects were examined in these
two latter studies, utilizing a multivariate approach.
The treatment resulted in mean attachment gains of
4.1 ± 2.5 mm and 5.3 ± 2.2 mm, and it was observed
that the most coronal portion of the defects which is
most susceptible to negative influences from the oral
environment were often incompletely filled with
bone.
The endodontic status of the tooth has also been
suggested as a potential relevant factor in periodontal
therapy. Emerging evidence (see Chapter 14) indicates
that root canal treated teeth may respond differently
to periodontal therapy. A clinical study on 208 con-
secutive patients with one intrabony defect each dem-
onstrated that root canal treatment does not nega-
tively affect the healing response and the long-term
stability of results of deep intrabony defects treated
with GTR (Cortellini & Tonetti 2000b). Finally, a con-
trolled clinical trial demonstrated that severe tooth
hypermobility can negatively affect the clinical out-
comes of regeneration (Cortellini et al. 2001). Based on
these results, it can be concluded that deep and narrow
intrabony defects at either vital or endodontically
treated teeth are the ones in which the most beneficial
outcomes can be achieved by GTR treatment (Fig.
28-31). Severe dental hypermobility may impair the
clinical outcomes.
Technical factors
Successful GTR requires careful flap design, correct
placement of the material, good closure of the wound
and optimal post-operative plaque control.
Membrane exposure is reported to be a major com-
plication with a prevalence in the range of 50 to 100%
(Becker et al. 1988, Cortellini et al. 1990, 1993b, Selvig
et al. 1992, 1993, Murphy 1995a, DeSanctis et al.
1996a,b, Falk et al. 1997, Trombelli et al. 1997, Mayfield
et al. 1998). Cortellini et al. (1995c,d) reported that the
prevalence of membrane exposure can be highly re-
duced with the use of access flaps, specifically de-
signed to preserve the interdental tissues (modified
papilla preservation technique) (Fig. 28-32).
Many studies have shown that the exposed mem-
branes are contaminated with bacteria (Selvig et al.
1990, 1992, Grevstad & Leknes 1992, Machtei et al.
1993, Mombelli et al. 1993, Tempro & Nalbandian
1993, Nowzari & Slots 1994, Novaes-Jr et al. 1995,
Nowzari et al. 1995, DeSanctis et al. 1996a,b). Con-
tamination of exposed non-bioabsorbable as well as
bioabsorbable membranes was associated with lower
probing attachment level gains in intrabony defects
(
Selvig et al. 1992, Nowzari & Slots 1994, Nowzari et
al. 1995, DeSanctis et al. 1996a,b). The impaired
clini-
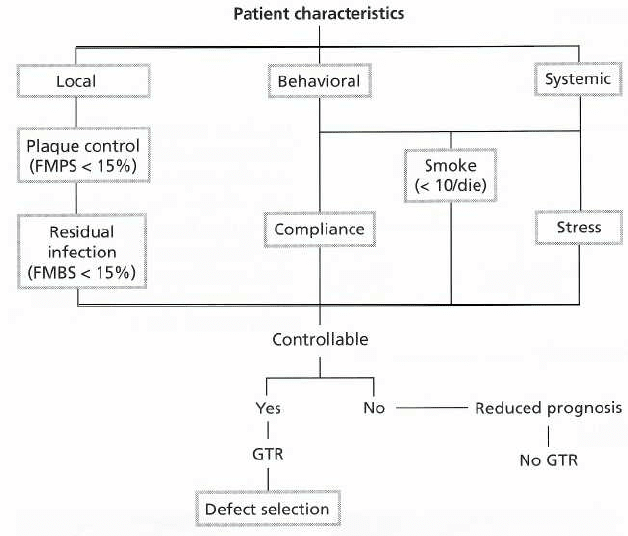
Fig. 28-30. Diagram illustrating pa-
tient selection criteria. It can be
seen that control of local, behav-
ioral and systemic patient charac-
teristics may improve the treat-
ment outcomes. (Modified from
Cortellini & Bowers 1995).
FMPS = full mouth plaque score.
FMBS = full mouth bleeding score.
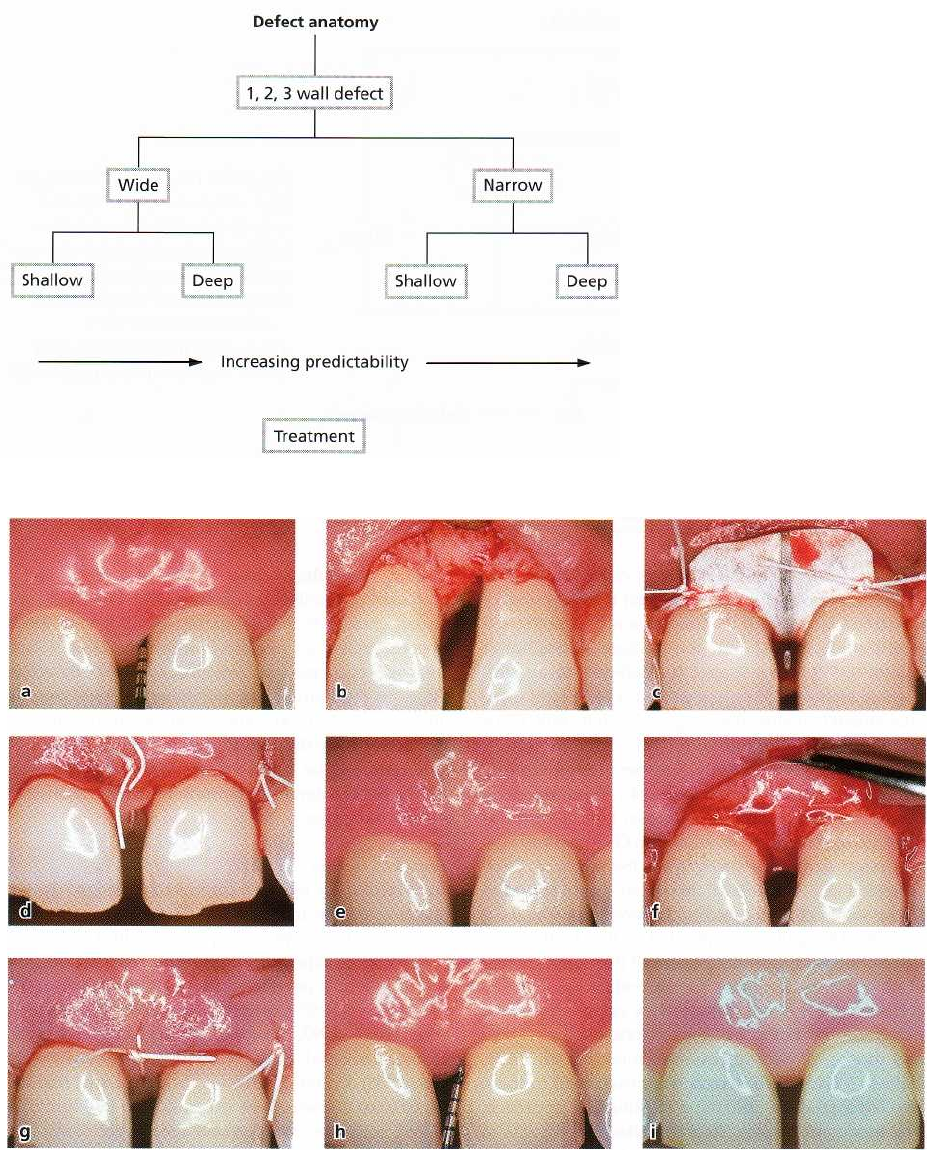
Fig. 28-32. (a) Left maxillary central incisor with a 10 mm pocket depth and 11 mm of clinical attachment loss on
the
mesial surface. A diastema is present between the two central incisors. (b) Full thickness buccal and palatal flaps
have been raised and an intrabony defect can be seen. The interdental papilla has been incised on the buccal
aspect
and elevated with the palatal flap (modified papilla preservation technique). (c) A titanium-reinforced
e-PTFE barrier
membrane has been placed and fixed close to the level of the cemento-enamel junction. (d) The membrane is
completely covered. This primary closure has been obtained by preserving the interdental papilla and
by coronal
displacement of the buccal tissue flap. (e) At 6 weeks, the membrane is completely covered with healthy tissue. (f)
After membrane removal at 6 weeks, dense newly formed tissue is evident in the defect and in the
supracrestal space
maintained by the titanium-reinforced membrane. (g) The newly formed tissue is completely
covered by the raised
and well preserved tissue flaps. (h) The photograph after 1 year shows a 4 mm residual pocket depth. A gain of
clinical attachment of 6 mm was recorded, and no recession has occurred compared to base-line. (j) 1 year
photograph showing the optimal preservation of the interdental tissues.
68o •
CHAPTER
28
Fig. 28-31. Diagram illustrating de-
fect selection criteria. It can be
seen that deep and narrow de-
fects, whether they are one-wall,
two-wall or three-wall defects,
have the greatest possibility to
show gain of attachment after
treatment. (Modified from Cortel-
lini & Bowers 1995.)
REGENERATIVE PERIODONTAL THERAPY • 681
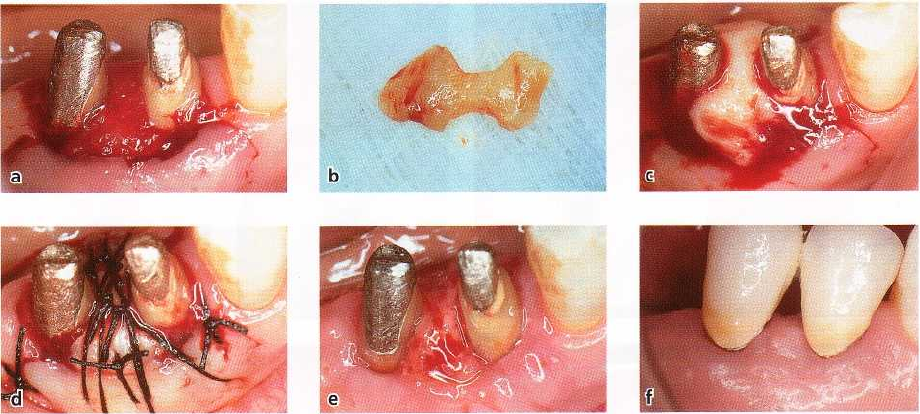
Fig. 28-33. (a) At 5 weeks after treatment of an intrabony defect with a non-resorbable barrier membrane, the cover
-
ing tissue was largely dehiscent. After membrane removal, the flaps could not properly cover the newly formed
tissue. (b) A free gingival graft has been harvested from the palate and saddle shaped to fit the interdental space.
(c)
The free gingival graft is placed to cover the newly regenerated tissue. (d) The graft is kept in position by inter
rupted and suspended sutures. (e) Healing after 1 week. (f) Appearance of the treated site after 1 year.
cal results in some studies were associated with high
counts of bacteria and with the presence of P.
gingivalis
and A. actinomycetemcomitans
(Machtei et al. 1994,
Nowzari & Slots 1994, Nowzari et al. 1995).
Bacterial contamination of the membrane may oc-
cur during surgery, but also during the postoperative
healing phase. After placement, bacteria from the oral
cavity may colonize the coronal part of the membrane.
Frequently, this results in recession of the gingival
tissues, which allows colonization of the membrane
material further apically. In addition, "pocket" forma-
tion may occur on the outer surface of the membrane
due to apical migration of the epithelium on the inner
surface of the covering gingival tissue. This may allow
bacteria from the oral cavity to colonize the subgingi-
val area. The significance of bacterial contamination
was addressed in an investigation in monkeys (Sander
& Karring 1995). The findings of this study showed
that new attachment and bone formation occurred
consistently when bacteria were prevented from in-
vading the membrane and the wound during healing.
In order to prevent wound infection, some investi-
gators have administered systemic antibiotics to pa-
tients before and during the first weeks after mem-
brane application (Demolon et al. 1993, Nowzari &
Slots 1994). However, despite the application of sys-
temic antibiotics, occurrence of postoperative wound
infection related to implanted barrier membranes was
noticed. This indicates that either the drug adminis-
tered is not directed against the microorganisms re-
sponsible for the wound infection, or that the drug
does not reach the infected site at a concentration
sufficiently high to inhibit the target microorganisms.
An improved effect on periodontal healing after GTR
in association with local application of metronidazol
was reported by Sander et al. (1994). Twelve patients
with one pair of intrabony defects participated in the
study. Metronidazol was placed in the defects and on
the membrane prior to wound closure, while the con-
trols were treated with a membrane alone. Six months
following membrane removal the medium gain in
probing attachment level, presented as a percentage
of the initial defect depth, was 92% for test defects
versus 50% for the control defects. Other clinical pa-
rameters, like plaque index, bleeding on probing,
pocket depth reduction or recession of the gingival
margin were similar in the test and control sites. Al-
though the use of local or systemic antibiotics may
reduce the bacterial load on exposed membranes, it
seems ineffective in preventing the formation of a
microbial biofilm (Frandsen et al. 1994, Nowzari et al.
1995). Apart from the erythema and swelling related
to such infection of the wound, more severe postop-
erative complications such as suppuration, sloughing
or perforation of the flap, membrane exfoliation, and
post-operative pain have been reported (Murphy
1995a, b).
Another important issue associated with the clini-
cal results is the coverage of the regenerated tissue
after removal of a non-bioabsorbable membrane.
Many authors have reported that the frequent occur-
rence of a gingival dehiscence over the membrane is
likely to result in insufficient protection of the inter-
proximal regenerated tissue (Becker et al. 1988, Selvig
et al. 1992, Cortellini et al. 1993b, Tonetti et al. 1993a).
Exposure of the regenerated tissue to the oral environ
-
ment entails the risks of mechanical and infectious
insults which in turn may prevent complete matura-
tion of the regenerated tissue into a new connective
tissue attachment. In fact, incomplete coverage of the
regenerated tissue was associated with reduced at-
tachment and bone gain at 1 year (Tonetti et al. 1993a).
682 • CHAPTER 28
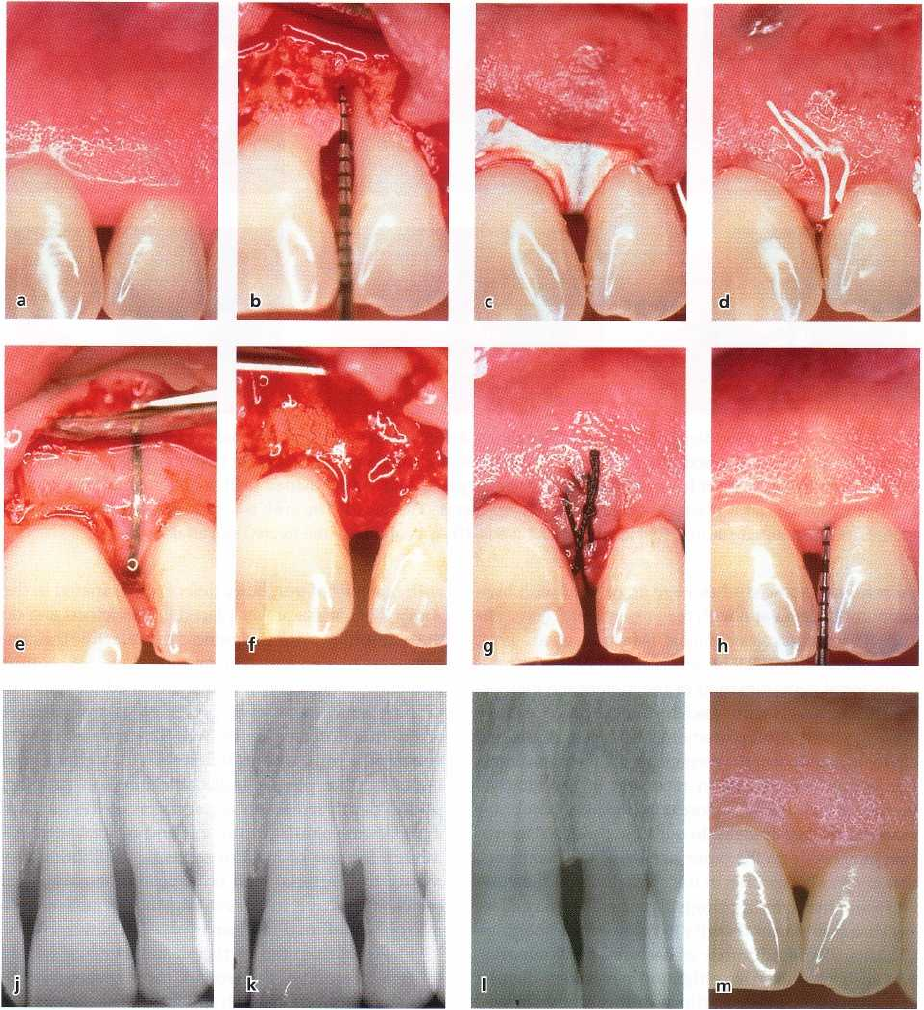
Fig. 28-34. (a,b) Left maxillary lateral incisor with a deep interproximal intrabony defect on the mesial surface. (c)
Flaps are raised according to the modified papilla preservation technique, and a titanium reinforced barrier mem-
brane is placed over the defect. (d) By coronal displacement of the flap and preservation of the interdental papilla,
the membrane is completely covered. (e,f) After 6 weeks of uneventful postoperative healing the membrane was re-
moved, (g) and the newly formed tissue was completely covered. (h) At 1 year, residual probing pocket depth was
2
mm and no buccal or interdental recession had occurred. (j) The baseline radiograph shows radiolucency ap-
proaching the apex of the tooth, but (k) after 1 year the intrabony defect is resolved and some supracrestal bone ap
-
position seems to have occurred (k). The radiograph taken at 6 years confirms the supracrestal bone regeneration
(
1) and the clinical image shows the integrity of the interdental papilla with optimal preservation of the esthetic ap
-
pearance (m).
Recently, the positioning of a saddle-shaped free gin-
gival graft over the regenerated interproximal tissue
(Fig.
28-33) was suggested (Cortellini et al. 1995a) to
offer
better coverage and protection than a dehiscent gingival
flap. In this randomized controlled study,
more gain of
attachment was observed in the 14 sites
where a free gingival graft was positioned after mem-
brane removal (5.0 ± 2.1 mm), than in the 14 sites
where a conventional protection of the regenerated
tissue
was accomplished (3.7 ± 2.1 mm).
In order to increase the space for regeneration, and
in order to achieve and maintain primary closure of
REGENERATIVE PERIODONTAL THERAPY •
683
the flap in the interdental area, the modified papilla
preservation technique (MPPT) was developed
(
Cortellini et al. 1995c,d). This approach combines
special soft tissue management with use of a self-sup-
porting titanium-reinforced membrane capable of
maintaining a supra-alveolar space for regeneration.
The MPPT allows primary closure of the interdental
space, resulting in better protection of the membrane
from the oral environment (Cortellini et al. 1995d). The
technique involves the elevation of a full thickness
palatal flap which includes the entire interdental pa-
pilla. The buccal flap is mobilized with vertical and
periosteal incisions, coronally positioned to cover the
membrane, and sutured to the palatal flap through a
horizontal internal crossed mattress suture over the
membrane. A second internal mattress suture war-
rants primary closure between the flap and the inter-
dental papilla. A representative case is shown in Fig.
28-34. In a randomized controlled clinical study on 45
patients (Cortellini et al. 1995c), significantly greater
amounts of attachment gain were obtained with the
MPPT (5.3 ± 2.2 mm), in comparison with either con-
ventional GTR (4.1 ± 1.9 mm) or flap surgery (2.5 ± 0.8
mm), demonstrating that a modified surgical ap-
proach can result in improved clinical outcomes.
In this study 100% of the sites were closed on top of
a
titanium-reinforced membrane and 73% remained
closed for up to 6 weeks, when the barrier membrane
was removed. The reported procedure can be success-
fully applied in sites where the interdental space width
is at least 2 mm at the most coronal portion of
the
papilla. When interdental sites are narrower, the
reported technique is difficult to apply. In order to
overcome this problem, a different papilla preservation
procedure (the simplified papilla preservation
flap) has
been proposed to apply in narrow interden
tal spaces (
Cortellini et al. 1999). This approach in
cludes an
oblique incision across the defect-associated
papilla,
starting from the buccal angle of the defect associated
tooth to reach the mid-interdental part of
the papilla at
the adjacent tooth under the contact point. In this way,
the papilla is cut into two equal parts of which the
buccal is elevated with the buccal
flap and the lingual
with the lingual flap. In the cited study, 100% of the
narrow interdental papilla could be
closed on top of
bioresorbable barriers, and 67% main
tained primary
closure over time, resulting in 4.9 ± 1.8
mm of clinical
attachment level gains. This approach
has been
successfully applied in different multicenter
randomized clinical trials designed to test the gener-
alizability of the added benefits of using barrier mem-
branes on deep intrabony defects (Tonetti et al. 1998,
Cortellini et al. 2001).
In the cited studies, GTR therapy of deep intrabony
defects performed by different clinicians on various
patient populations resulted in both greater amounts
and improved predictability of CAL gains than access
flap alone. The issue of soft tissue manipulation to
obtain a stable protection of the regeneration site has
been further explored, applying a microsurgical ap-
proach in the regenerative therapy of deep intrabony
defects (Fig. 28-35). In a patient cohort study on 26
patients with 26 intrabony defects treated with papilla
preservation techniques, primary closure on the bar-
rier was obtained in 100% of the cases and maintained
over time in 92.3% of the sites. Treatment resulted in
large amounts of CAL gains (5.4 ± 1.2 mm) and mini-
mal gingival recession (0.4 ± 0.7 mm). Thus, the im-
proved vision and better soft tissue handling im-
proved the predictability of periodontal regeneration.
Postoperative morbidity
To date, little consideration has been given to critical
elements that could contribute to the patient's assess-
ment of the cost-benefit ratio of GTR procedures.
These
include postoperative pain, discomfort, compli
cations,
and the perceived benefits from the treatment.
A
parallel group, randomized, multicenter and con-
trolled clinical trial designed to test the efficacy of GTR
and flap surgery alone assessed these patient issues
(
Cortellini et al. 2001). During the procedure, 30.4% of
the test and 28.6% of the controls reported moderate
pain and subjects estimated the hardship of the proce-
dure as 24 ± 25 units on a visual analog scale (VAS in
a scale from 0 to 100) in the test group and to 22 ± 23
VAS in the controls. Test surgery with membranes
required longer chair time than flap surgery (on aver-
age 20 minutes longer). Among the postoperative
complications, edema was most prevalent at week 1
and most frequently associated with the GTR treat-
ment, while postoperative pain was reported by fewer
than 50% of both test and control patients. Pain inten-
sity was described as mild and lasted on average 14.1
± 15.6 hours in the test patients and 24.7 ± 39.1 hours
in the controls. Postoperative morbidity was limited
to
a minority of subjects: 35.7% of the test and 32.1%
of
the controls reported that the procedures interfered
with daily activities for an average of 2.7 ± 2.3 days in
the test group and 2.4 ± 1.3 days in the control group.
These data indicate that GTR adds almost 30 minutes
to a flap procedure and is followed by a greater preva-
lence of post surgical edema, while no difference could
be observed between GTR and flap surgery alone in
terms of postoperative pain, discomfort and interfer-
ence with daily activities.
Furcation involvements
The invasion of the furcation area of multirooted teeth
by periodontitis represents a serious complication in
periodontal therapy. The furcation area is often inac-
cessible to adequate instrumentation, and frequently
the roots present concavities and furrows which make
proper cleaning of the area impossible (see Chapter
29)
. As long as the pathologic process is extending
only a
minor distance (< 5 mm; degree I and II involve
ments)
into the furcation area, further progress of the
disease
can usually be prevented by scaling and root
planing,
provided a proper oral hygiene program is
established
after treatment. In more advanced cases
(5-6 mm;
degree II involvements), the initial cause-re-
684. • CHAPTER 28
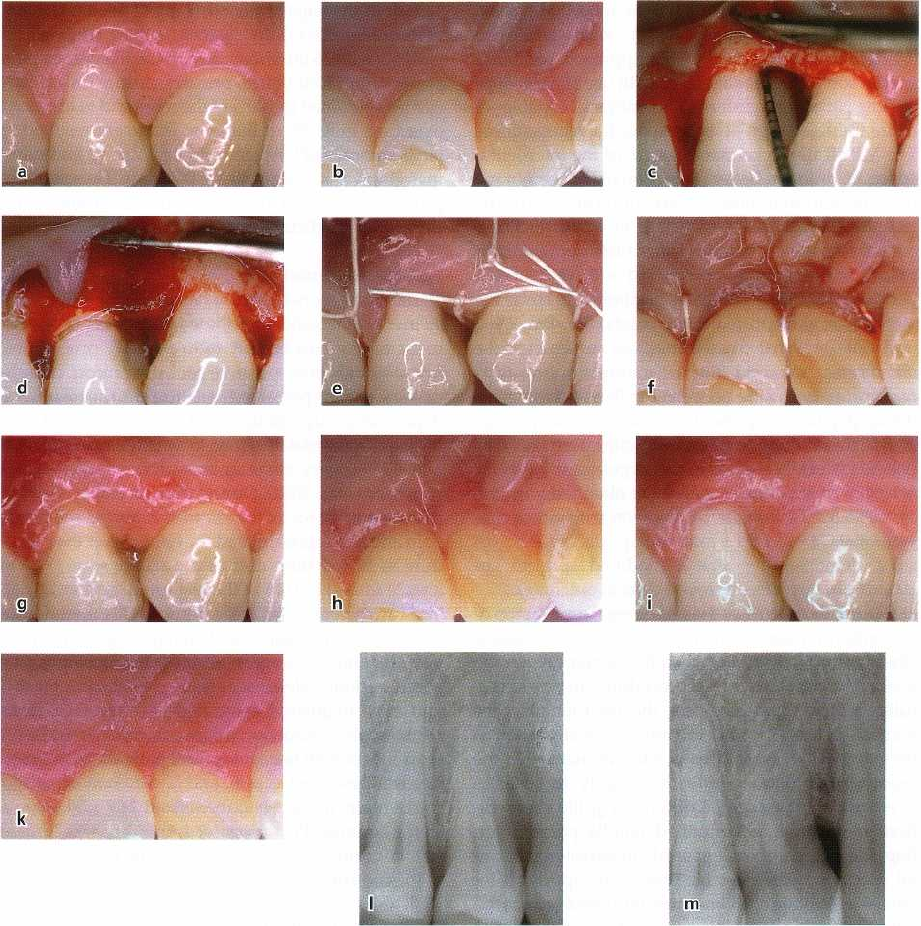
Fig. 28-35. (a) Right first maxillary premolar with a 7 mm pocket on the mesial surface. The interdental space (b) is
very narrow (> 2 mm), and is accessed with a simplified papilla preservation flap. The 5 mm deep intrabony defect
(
c) is covered with a bioresorbable barrier membrane (d). Primary closure of the flap over the membrane (e,f) is
maintained over time (g,h). After 1 year the interdental papilla is completely preserved and the residual pocket
depth is 3 mm (j,k). The radiograph taken at baseline (1) compared with that taken 1 year after treatment (m) shows
that the intrabony defect has healed completely.
lated treatment is frequently supplemented with sur-
gery involving contouring of the interradicular bone
(
osteoplasty) or reduction of the tooth prominence at
the furcation entrance by grinding (odontoplasty), in
order to reduce the horizontal extension of the furca-
tion involvement. In cases where the involvement is
extending deeper into the furcation area (> 5 mm;
degree II involvements), or a through and through
defect (degree III involvements) has developed, tun
nel
preparation or root resection has been advocated
as
the choice of treatment. However, both of these
latter
treatments involve a risk of complications on a
long-
term basis. Following tunnel preparation, caries
frequently develops in the furcation area and root
resected teeth often present complications of non-peri
-
odontal nature, although controversial reports exist
regarding the long-term results of these treatment
modalities (Hamp et al. 1975, Langer et al. 1981, Er-
penstein 1983, Biihler 1988, Little et al. 1995).
Considering the complexity of current techniques
for the treatment of furcation problems, and in view
of the long-term results and complications reported
following treatment of advanced furcation involve-
ments by traditionally resective therapy, predictable
regeneration of the periodontium at furcation-in-
