Jan Lindhe. Clinical Periodontology
Подождите немного. Документ загружается.

REGENERATIVE PERIODONTAL THERAPY •
6
55
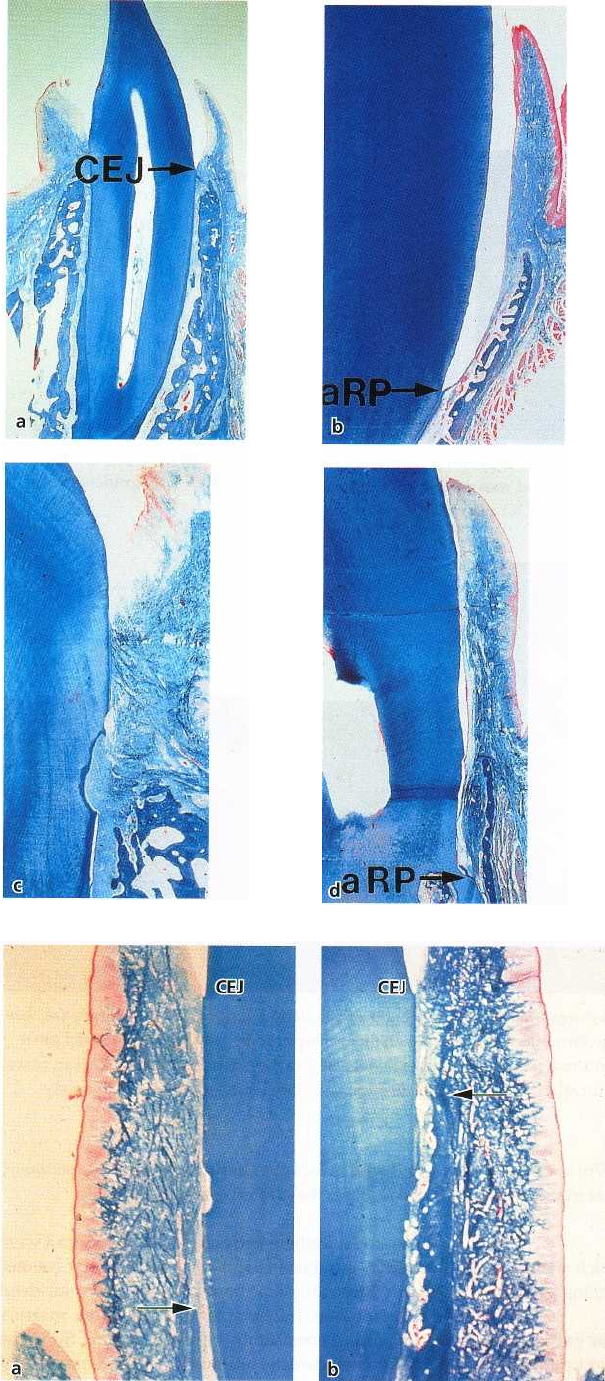
Fig. 28-5. Microphotographs show-
ing the histological features after 6
months of healing, under the four
experimental conditions (a-d) il-
lustrated in Fig. 28-4. The teeth in
(
b) and (d) are those root planed
in
their coronal portion, and the
teeth (
a) and (b) are those reim
planted in
sockets with normal
bone height. A
fibrous reunion
was established in
areas where the connective tissue
attachment was
retained (a and c)
while the epithe
lium has migrated
to the apical ex-tension of root
instrumentation (a
RP) where the
attachment was re-
moved (b and d).
CEJ: cemento
enamel junction.
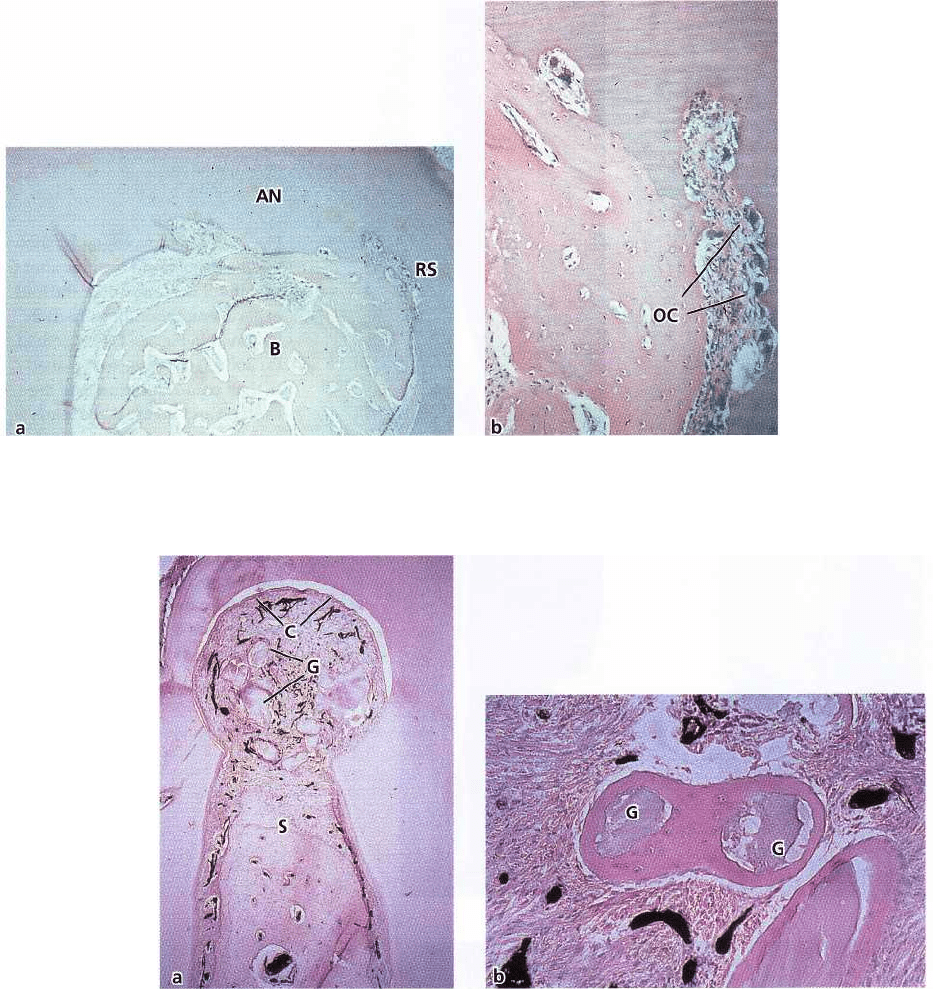
Fig. 28-6. Microphotograph of a
tooth retained in its labially dis-
placed position (a) and a tooth (b)
moved back to its original posi
tion.
The level of alveolar bone (ar
row) is
reduced in (a) while it has
regenerated to its normal level (ar-
row) in (b). The apical termination
of
the junctional epithelium is at the
cemento-enamel junction (CEJ) in
both situations.
656 • CHAPTER
28
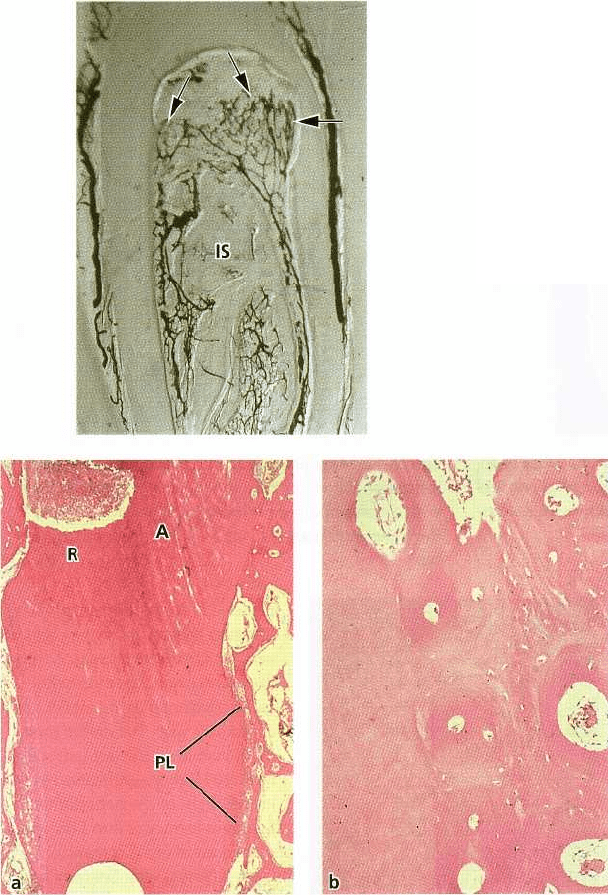
Fig. 28-7. Microphotograph of furcation 6 weeks after grafting with iliac crest marrow (a). The furcation is com
pletely filled with bone (B), but ankylosis (AN) and root resorption (RS) can be seen. (b) Higher magnification
of
the area in (a) showing ankylosis and resorption. OC: osteoclasts.
Fig. 28-8. Microphotograph of a healed bifurcation defect following transplantation of non-vital bone grafts (a). The
grafts (G) have not been reached by bone formation from the interradicular septum (S), but occur as isolated parti
-
cles surrounded by "cementu
m
"
. Cementum (C) and new connective tissue attachment formation have taken place
along the entire circumference of the bifurcation. (b) High magnification of isolated bone grafts (G) with newly
formed "cementum" on the surface.
Ellegaard et al. (1973, 1974, 1975, 1976) and Nielsen
et al. (1980) reported that grafting materials in peri-
odontal bony defects may be:
1.
osteoproliferative
(osteogenetic), which means that
new bone is formed by bone forming cells con-
tained in the grafted material
2.
osteoconductive,
which means that the grafted mate-
rial does not contribute to new bone formation
per
se
but serves as scaffold for bone formation origi
nating
from adjacent host bone
3.
osteoinductive,
which means that bone formation is
induced in the surrounding soft tissue immediately
adjacent to the grafted material.
These studies, where various types of bone graft were
placed in intrabony defects or interradicular lesions,
revealed that only iliac bone marrow grafts survived
transplantation. Transplantation of iliac bone marrow
grafts almost consistently resulted in bone fill in the
experimental defects, but healing was frequently ac-
companied by ankylosis and root resorption (Fig. 28-
7).
The iliac bone marrow grafts exerted an osteo
geneic
effect, and it was suggested that this was re-
REGENERATIVE PERIODONTAL THERAPY • 657
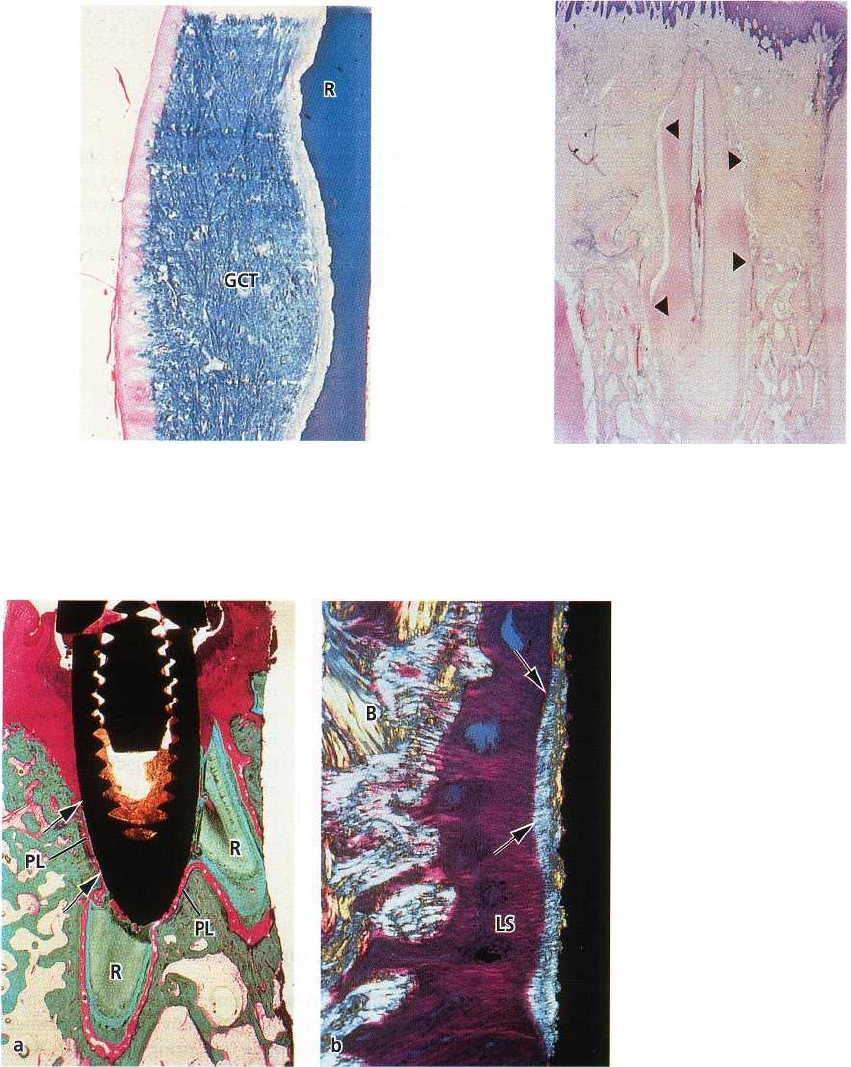
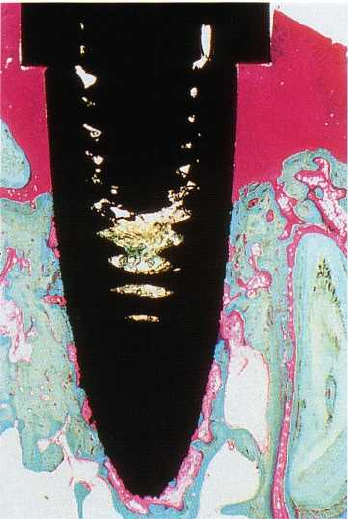
Fig. 28-9. Cleared specimen from a 1-week-old bifurca
-
tion defect treated with bone grafts. Judged from the
course of the blood vessels, the granulation tissue in
the defect has developed mainly from the periodontal
ligament (arrows) and only to a minor extent from the
interradicular septum (IS).
Fig. 28-10. Microphotograph of a
reimplanted root after 3 months of
healing (a). A periodontal liga
ment
(PL) has become re-estab
lished in
the apical portion of the
root
whereas ankylosis (A) and
root
resorption (R) is the predomi
nant
feature in the coronal por
tion. (b)
High magnification of the
ankylosis
seen in (a).
sponsible for the induction of root resorption (Elle-
gaard et al. 1973, 1974). Jaw bone grafts and xenografts
did not actively contribute to bone formation but
served as a scaffold for bone regeneration (i.e. osteo-
conductive effect). Often, however, these bone grafts
were not reached by the new bone growing out from
the host bone, but occurred as isolated particles sur-
rounded by a bone-like or cementum-like substance
(
Fig. 28-8). It was found that the treated bifurcation
defects became filled mainly with granulation tissue
derived from the periodontal ligament (Fig. 28-9). The
authors (Nielsen et al. 1980) suggested that this in-
growth of ligament tissue inhibited bone formation
and
that the new cementum on the root surface in the
bifurcation defects, including the cementum-like sub-
stance observed around the implanted bone particles,
were formed by periodontal ligament cells (Fig. 28-8).
Thus, it appeared from these studies that the key cells
in periodontal regeneration are periodontal ligament
cells rather than bone cells.
Regenerative capacity of bone cells
The ability of newly formed tissue originated from
bone
to produce a new connective tissue attachment
was
examined in a study by Karring et al. (1980). Roots
of
periodontitis-affected teeth were extracted and
placed
in surgically created sockets in edentulous ar
eas of
dogs. The implanted roots were covered with
tissue
flaps (submerged) and the results of healing
were
examined histologically after 3 months. A peri
odontal
ligament was re-established in the apical por
tion of
the reimplanted roots where, at the time of
implantation, remnants of periodontal ligament tissue
were preserved. In the coronal portion of the roots
which were previously exposed to periodontitis and
then scaled and planed, healing had consistently re-
sulted in ankylosis and root resorption (Fig. 28-10). On
the basis of this finding, it was concluded that tissue
derived from bone lacks cells with the potential to
produce a new connective tissue attachment.
658 • CHAPTER 28
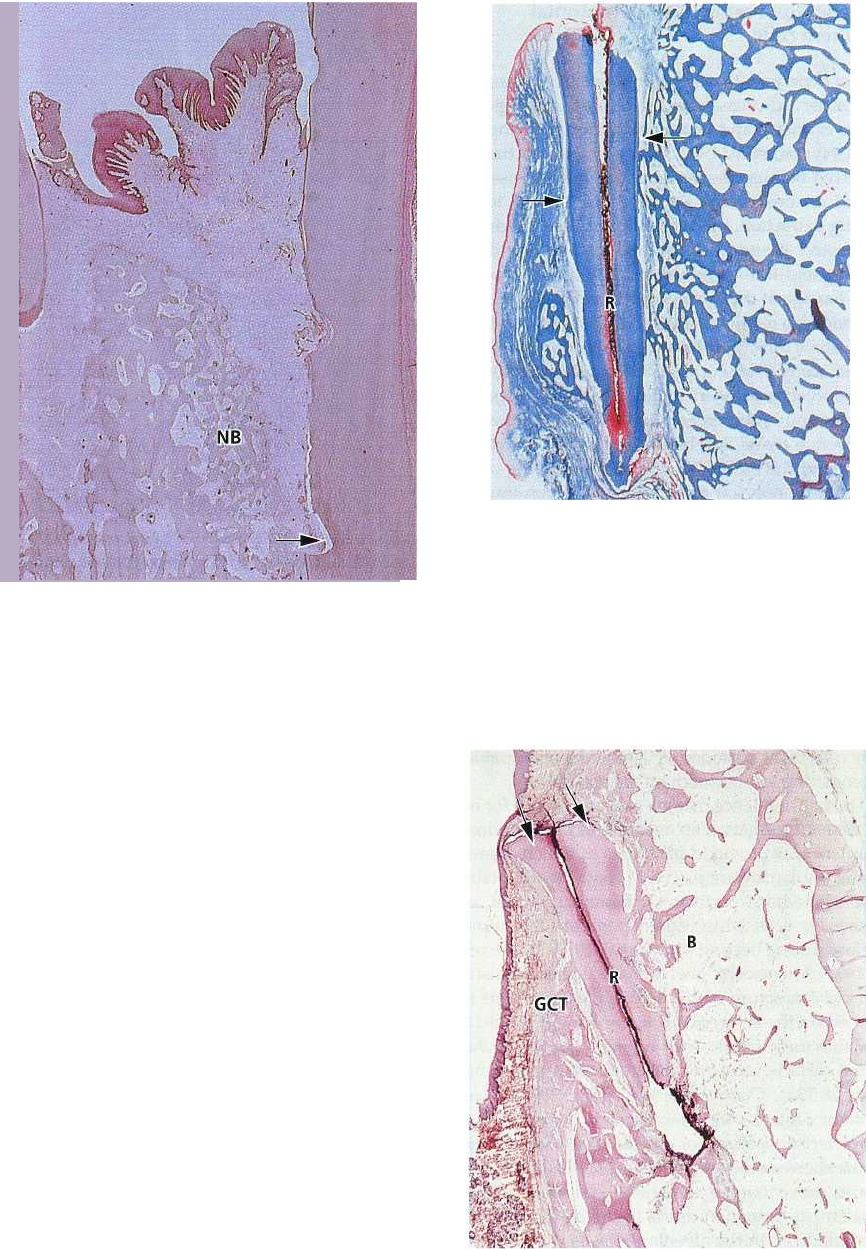
Fig. 28-11. Microphotograph of root (R) which has been
reimplanted with its surface facing the gingival connec-
tive tissue (GCT). The surface exhibits extensive resorp-
tion.
Fig. 28-12. Microphotograph showing new attachment
formation (between the arrows) on a submerged root
with a non-impaired periodontal ligament. Coronal to
the cementum, root resorption is the predominant fea-
ture.
Fig. 28-13. Microphotograph of a
titanium implant placed in contact
with retained root tips (a). A dis-
tinct cementum layer (arrows)
and
periodontal ligament (PL) in
continuity with that on the roots
(
R) is visible on the implant sur-
face. (b) High magnification in po-
larized light of the periodontal
ligament formed around the im-
plant seen in (a). A cementum
layer
(arrows) with Sharpey's fi
bers is
present at the implant sur
face.
Principal fibers, oriented per-
pendicular to the surface, are run-
ning across the ligament space
(
LS) and are inserting in the op-
posing bone (B) as in natural teeth
(see Fig. 1-71).
Regenerative capacity of gingival connective
tissue cells
Another experiment (Nyman et al. 1980) was carried
out
in order to examine the potential of gingival con
nective
tissue to produce a new connective tissue
attachment.
The teeth were treated as described in the
experiment
above but were not transplanted into
sockets. Instead
they were placed in bone concavities
prepared on the
buccal aspect of the jaw and sub
sequently covered by
tissue flaps. Thus, half the cir
cumference of the roots
was in contact with bone while the remaining part was
facing the gingival connective
tissue at the subsurface of
the flaps. Histologic exami-
nation after 3 months of healing showed areas with
periodontal ligament in the apical portion of the roots
where, at the time of implantation, periodontal ligament
tissue was preserved. In the coronal, previously
exposed
part of the roots, no signs of new connective
tissue
attachment were present. The root portion lo
cated in
contact with gingival connective tissue dem
onstrated a
connective tissue with fibers oriented par
allel to the
root surface and without attachment to the
root.
However, root resorption occurred at the majority of the
surfaces (Fig. 28-11). On the basis of this
result it was
concluded that gingival connective tissue also lacks cells
with the potential to produce a new
connective tissue
attachment.
REGENERATIVE PERIODONTAL THERAPY •
6
59
Regenerative capacity of periodontal
ligament cells
In the experiments described above, root resorption
was observed occasionally, also in the apical portion
of the extracted and reimplanted roots (Karring et al.
1980, Nyman et al. 1980). It was suggested that this
occurred because the periodontal ligament tissue re-
tained on this part of the root had become injured
during extraction, thereby allowing bone or gingival
connective tissue to contact the root surface during
healing and induce resorption. It was assumed that
this damage of the retained periodontal ligament tis-
sue had also restricted its potential of proliferating in
the coronal direction along the root surface. Indeed, in
a later study (Karring et al. 1985), where periodonti-
tis-involved roots were retained in their sockets and
subsequently submerged, significant amounts of new
connective tissue attachment formed on the coronal
portion of the roots (Fig. 28-12). The finding of new
attachment only on the roots with a non-impaired
periodontal ligament, but never on the extracted and
reimplanted roots with an impaired ligament, indi-
cates that periodontal ligament tissue contains cells
with the potential to form a new connective tissue
attachment on a detached root surface.
Active root resorption occurred consistently at the
root surfaces above the coronal extension of new at-
tachment. It was suggested that this resorption was
induced by gingival connective tissue which had pro-
liferated apically from the covering tissue flap. Thus,
only cells in the periodontal ligament seem capable of
regenerating lost periodontal attachment.
The final evidence that the progenitor cells for new
attachment formation are residing in the periodontal
ligament was provided in studies in which titanium
dental implants were placed in contact with retained
root tips whose periodontal ligament served as a
source for cells which could populate the implant
surface during healing (Buser et al. 1990a,b, Warrer et
al. 1993). Microscopic analysis revealed that a distinct
layer of cementum with inserting collagen fibers had
formed on the surfaces of the implants (Fig. 28-13a),
and that these fibers, often oriented perpendicularly
to the surface, were embedded in the opposite bone
(
Fig. 28-13b). Control implants (Fig. 28-14) placed
without contact with retained roots healed with the
characteristic features of osseointegration (i.e. direct
contact between bone and the implant surface). These
results prove that the progenitor cells for periodontal
attachment formation reside in the periodontal liga-
ment and not in the alveolar bone as previously as-
sumed (Melcher et al. 1987).
Role of epithelium in periodontal wound
healing
Some of the roots in the experiment described above (
Karring et al. 1985) penetrated the covering mucosa
Fig. 28-14. Microphotograph of a titanium implant
placed without contact with retained roots (control).
This implant has healed with a direct contact between
the bone and the implant surface (osseointegration)
.
at early stages of healing, thereby allowing the epithe-
lium to grow apically along the root surface. The
amount of new connective tissue attachment on these
roots was considerably smaller than that formed on
the roots which remained submerged throughout the
study. This finding and those of other investigators
(Moscow 1964, Kon et al. 1969, Proye & Polson
1982)
indicate that the apical migration of
epithelium re-
duces the coronal gain of attachment,
evidently by preventing periodontal ligament cells
from repopulat-
ing the root surface (Fig. 28-15).
Downgrowth of epithelium into the periodontal
lesion has most likely occurred to a varying extent
during healing following most flap and grafting pro-
cedures applied in regenerative periodontal therapy,
which may explain the varying results reported. This
view is supported by the results of the monkey study
by Caton et al. (1980). These investigators examined
healing in ligature-induced periodontal lesions fol-
lowing treatment with four different modalities of
regenerative surgical procedures:
root planing and soft tissue curettage
Widman flap surgery without bone grafting
Widman flap surgery with the placement of frozen
autogeneous red bone marrow and cancellous
bone, or
beta tricalcium-phosphate in intrabony defects.
Healing following all treatment modalities resulted in
the formation of a long junctional epithelium extend-
ing to or close to the same level as before treatment.
66o •
CHAPTER
28
Fig. 2845. Microphotograph illustrating an intrabony
defect after regenerative treatment. New bone (NB) has
formed in the defect but epithelium has migrated api-
cally along the root surface to the notch (arrow) in the
root surface indicating the bottom of the defect before
treatment.
Root resorption
In the experimental studies described previously,
granulation tissue, derived from gingival connective
tissue or bone, produced root resorption when con-
tacting the curetted root surface during healing fol-
lowing surgery (Karring et al. 1980, 1985, Nyman et
al.
1980). It should be expected, therefore, that this
phenomenon would occur as a frequent complication
to regenerative periodontal surgery, particularly fol-
lowing those procedures which include the placement
of grafting materials to stimulate bone formation. The
reason that root resorption is rarely seen is most likely
that postoperatively, the dento-gingival epithelium
migrates apically along the root surface, forming a
protective barrier towards the root surface (Fig. 28-15).
This view is supported by the results of an experimen-
tal study in monkeys (Karring et al. 1984) in which
roots, which previously had been subjected to liga-
ture-induced periodontitis, were extracted and reim-
planted into contact with bone and connective tissue
and covered with a tissue flap (submerged). After
varying time intervals the submerged roots were ex-
posed to the oral cavity by a second incision (wound-
ing) through the covering mucosa, thereby permitting
the epithelium to migrate into the wound. In speci-
mens where the wounding occurred within 2 weeks
(
Fig. 28-16), the previously diseased part of the roots
Fig. 28-16. Microphotograph of an implanted root (R)
where epithelium was allowed to migrate into the
wound after 2 weeks. The epithelium has migrated
along the coronal, previously periodontitis-involved
root surfaces down to the level indicated by the arrows.
In the areas covered by epithelium, there are no signs
of resorption. Apical to this level the root surfaces dem
-
onstrate root resorption.
Fig. 28-17. Microphotograph of an implanted root (R)
where epithelium was allowed to migrate into the
wound after 4 weeks. The epithelium (arrows) covers
only the coronal cut root surface. Extensive resorption
is seen on the surface facing the gingival connective tis
-
sue (GCT) and resorption and ankylosis are seen on the
surface facing the bone tissue (B).

REGENERATIVE PERIODONTAL THERAPY • 661
Fig. 28-18. Progression of perio-
dontitis at a different rate on
neighboring tooth surfaces results
in the development of intrabony
defects. Based on the number of
surrounding bone walls such de-
fects are classified as one-wall (a),
two-wall (b) or three-wall (c) de-
fects.
was covered by epithelium and showed no signs of
resorption. With increasing intervals between implan-
tation of the roots and the wounding, a steadily dimin
-
ishing part of the diseased root surface was covered
by epithelium, and root resorption and ankylosis be-
came progressively pronounced (Fig. 28-17). This ob-
servation concurs with results presented by Bjorn et
al. (1965) who treated 11 periodontally diseased teeth
in seven human volunteers, using the submerging
technique which prevented apical migration of the
dentogingival epithelium. The authors reported that
root resorption was indeed a common complication
following this kind of therapy.
REGENERATIVE PROCEDURES
One of the first methods used in attempts to obtain
new attachment was scaling and root planing com-
bined with soft tissue curettage (i.e. mechanical re-
moval of the diseased root cementum and the pocket
epithelium). Studies in humans (e.g. Younger 1899,
McCa111926, Orban 1948, Beube 1952, Waerhaug 1952,
Schaffer & Zander 1953, Carranza 1954, 1960) and in
animals (e.g. Beube 1947, Ramfjord 1951, Kon et al.
1969) showed that this type of periodontal therapy
resulted not only in the establishment of gingival
health but also in a reduction of the initially recorded
pocket depth. This decrease in the depth of the peri-
662 • CHAPTER 28
odontal pocket was assumed to be partly the result of
shrinkage of the initially inflamed gingiva, but partly
also the effect of the formation of a new connective
tissue attachment in the apical part of the pocket.
The possibility of obtaining new attachment be-
came widely accepted with the work of Prichard
(
1957a,b) in which new attachment formation in in-
trabony periodontal lesions was reported as a predict
-
able outcome of treatment. Seventeen cases were pre-
sented out of which four were subjected to a re-entry
surgical procedure, revealing that these defects were
filled with bone. The technique of Prichard (1957b,
1960) was only used for the treatment of three-wall
intrabony defects, and the results obtained suggested
that the morphology of the periodontal bony defect
was essential for the establishment of a predictable
prognosis. Goldman & Cohen (1958) introduced a
classification of periodontal intrabony defects which
was based on the number of osseous walls surround-
ing the defect, being either three-wall, two-wall or
one-wall defects or a combination of such situations
(
Fig. 28-18).
The technique of Prichard (1957a,b, 1960) included
the elevation of tissue flaps in order to get access to
the defect. All granulation tissue in the defect was
removed and the root surface was scaled and planed.
In order to enhance regeneration of bone, small perfo
-
rations were made with a bur at several sites of the
bone walls. The flaps were sutured to accomplish
complete coverage of the defect. Many clinical inves-
tigators have claimed that new attachment resulted
following this type of treatment but there is little
quantitative or qualitative documentation (Patur &
Glickmann 1962, Wade 1962, 1966, Ellegaard & Loe
1971, Yukna et al. 1976). Patur & Glickmann (1962)
reported a clinical study including 24 intrabony de-
fects treated according to the Prichard technique
(
1957a,b). The outcome was evaluated by comparing
preoperative and postoperative radiographs, meas-
urements of the alveolar bone level adjacent to the root
and study casts taken during operation and postop-
eratively after reflecting buccal and lingual flaps. The
authors reported that new attachment had occurred in
two-wall and three-wall intrabony defects but not in
one-wall defects. Results from a study by Ellegaard &
Loe (1971) comprising 191 defects in 24 patients with
periodontal disease indicated that complete regenera-
tion, determined radiographically and by periodontal
probing, had occurred in around 70% of the three-wall
defects, in 40% of the combined two-wall and three-
wall defects and in 45% of the two-wall defects.
In a later study by Rosling et al. (1976), 124 in-
trabony defects in 12 patients were treated by means
of the modified Widman flap procedure (Ramfjord &
Nissle 1974). Following treatment the patients were
recalled twice per month for professional tooth clean-
ing. Re-examination performed clinically and on ra-
diographs 2 years after therapy demonstrated bone fill
in two-wall as well as three-wall defects. The authors
suggested that this regrowth of bone was also associ
ated with the formation of new connective tissue at-
tachment and ascribed the successful healing mainly
to the optimal standard of oral hygiene which was
maintained in all patients during healing. A clinical
study with almost identical results was presented by
Polsen & Heijl (1978). The results of several histologic
studies in animals and humans, on the other hand,
indicate that formation of new periodontal attach-
ment is by no means predictable following subgingi-
val curettage or flap surgery (Listgarten & Rosenberg
1979, Caton & Nyman 1980, Caton et al. 1980, Steiner
et el. 1981, Stahl et al. 1983, Bowers et al. 1989a).
Grafting procedures
In a number of clinical trials and animal experiments,
the flap approach was combined with the placement
of bone grafts or implant materials into the curetted
bony defects with the aim of stimulating periodontal
regeneration. The various graft and implant materials
used so far can be placed into four categories:
1. Autogenous grafts:
Grafts transferred from one po-
sition to another within the same individual. This
type of graft comprises (1) cortical bone or (2) can-
cellous bone and marrow, and is harvested either
from intraoral or extraoral donor sites.
2.
Alto ;eneic grafts: Grafts transferred between
geneti
cally dissimilar members of the same
species. (1) Frozen cancellous bone and marrow, and
(2) freeze
-
dried bone have been used.
3. Xenogencic grafts:
Grafts taken from a donor of an-
other species.
4. Alloplastic materials:
Synthetic or inorganic implant
materials which are used as substitutes for bone
grafts.
The rationale behind the use of bone grafts or alloplas
-
tic materials is the assumption that both the regrowth
of alveolar bone and the formation of new attachment
would be stimulated because these materials may
either (1) contain bone forming cells (osteogenesis), or
(
2) serve as a scaffold for bone formation (osteocon-
duction), or because (3) the matrix of the bone grafts
contains bone-inducing substances (osteoinduction)
(
Urist 1980, Brunsvold & Mellonig 1993). Such com-
plete regeneration of the periodontal attachment ap-
paratus following grafting procedures would imply
that cells derived from bone possess the ability to form
new cementum with inserting collagen fibers on a
previously periodontitis-involved root surface (Mel-
cher et al. 1987).
The value of using bone grafts or alloplastic mate-
rials for periodontal regeneration has mainly been
examined in case reports, while histologic evidence of
new attachment and controlled clinical studies is lim-
ited. The results from such reports vary and the docu
-
mentation presented usually consists of preoperative
REGENERATIVE PERIODONTAL THERAPY •
663
and postoperative probing attachment levels, radio-
graphic interpretations or re-entry procedures.
Autogenous grafts
Autogenous grafts (autografts) may retain some cell
viability and are considered to promote bone healing
mainly through osteogenesis and/or osteoconduc-
tion. They are gradually resorbed and replaced by
new viable bone. In addition, potential problems of
histocompatibility and disease transmission are elimi
-
nated with autogenous grafts. Autogenous grafts can
be harvested from intraoral or extraoral sites.
Intraoral autogenous grafts
Intraoral autogenous grafts obtained from edentulous
areas of the jaw, healing extraction sites, maxillary
tuberosities or the mandibular retromolar area were
commonly used in periodontal regenerative surgery
(
Mann 1964, Ellegaard & Loe 1971, Rosenberg 1971a,b,
Dragoo & Sullivan 1973a, b, Hiatt & Schallhorn 1973,
Froum et al. 1983, Stahl et al. 1983). Generally cancel
lous bone is preferred as graft material but cortical
bone, applied as small chips (Rosenberg et al. 1979),
or mixed with blood prior to the placement in the
defects (Robinson 1969, Froum et al. 1976), was also
reported to be effective in producing regeneration in
periodontal intrabony defects.
The effect of intraoral autogenous grafts has been
evaluated in both animals and humans. In a study in
monkeys, Rivault et al. (1971) observed that intrabony
defects filled with intraoral autogenous bone chips
mixed with blood (osseous coagulum) healed with
new bone formation, but no more bone was found in
such experimental defects than was observed in simi
-
lar control defects treated with surgical curettage.
Other studies in monkeys and dogs also failed to
demonstrate significant differences in bone formation
between grafted and non-grafted intrabony or furca-
tion defects (Ellegaard et al. 1974, Coverly et al. 1975,
Nilveus et al. 1978).
In clinical case-series where intraoral autogenous
grafts were used for the treatment of intrabony peri-
odontal defects, a mean bone fill ranging from 3.0 mm
to 3.5 mm was reported (Nabers & O'Leary 1965,
Robinson 1969, Hiatt & Schallhorn 1973, Froum et al.
1975). Hiatt & Schallhorn (1973) treated 166 intrabony
lesions with intraoral autogenous cancellous bone.
They reported a mean increase in bone height of 3.5
mm, evaluated by clinical measurements. One-wall,
two-wall and three-wall defects were included, and
the largest bone fill was observed in defects with the
highest number of bone walls. A block section ob-
tained from a patient treated in this study presented
histologic evidence of new cementum, bone and peri-
odontal ligament formation. In controlled clinical
studies, intraoral autogenous grafts were found supe
-
rior to surgical debridement alone in terms of bone fill
(Froum et al. 1976), or probing attachment (PAL) gain
(Carraro et al. 1976) in two-wall defects. However,
there are controlled studies that demonstrate more
modest results regarding bone fill or PAL gain after
intraoral grafting when compared to ungrafted con-
trols (Ellegaard & Loe 1971, Renvert et al. 1985).
Ross & Cohen (1968) reported new bone and ce-
mentum formation in a human histologic specimen
from an intrabony defect retrieved 8 months following
debridement and placement of intraoral autogenous
grafts. They also found that the grafts were without
osteocytes and that the deposition of new alveolar
bone had taken place around the grafts. Nabers et al.
(
1972) observed that new cementum and functionally
oriented periodontal ligament fibers were present in
half the length of a defect which was biopsied about
4
1
/2
years after treatment with intraoral autogenous
bone grafts. In other human histologic reports, bone
fill and new attachment were observed coronal to
reference notches placed on the treated roots at the
apical termination of root planing (Hiatt et al. 1978) or
at the most apical level of previously existing calculus
(Froum et al. 1983, Stahl et al. 1983). Other investiga
tors, however, observed an epithelial lining which
occupied a varying portion of the previously diseased
part of the root (Hawley & Miller 1975, Listgarten &
Rosenberg 1979, Moscow et al. 1979). The results from
these studies indicate that the treatment of periodon
-
tal osseous defects with intraoral bone grafts may
result in periodontal regeneration, but not
predictably.
Extraoral autogenous grafts
Schallhorn (1967, 1968) introduced the use of auto-
geneous hip marrow grafts (iliac crest marrow) in the
treatment of furcation and intrabony defects. Later
several studies were published demonstrating the
osteogenic potentials of this material (Schallhorn et al.
1970, Schallhorn & Hiatt 1972, Patur 1974, Froum et al.
1975), and as much as 3-4 mm gain in crestal bone was
reported following the treatment of intrabony defects
with hip marrow grafts. The effect of iliac crest mar-
row and of intraoral cancellous bone grafts in one-
wall, two-wall and three-wall bony defects in humans
was evaluated by Patur (1974). He reported that bone
fill occurred to a varying extent with both types of
graft. The amount of bone fill in one-wall bony defects
was larger with iliac crest marrow than with cancel-
lous bone or when no grafts were used. Some defects
within all three groups showed bone fill, and no dif-
ference was observed between the control defects and
those treated with intraoral cancellous bone grafts.
The author stated that even with fresh iliac crest mar
-
row, bone regeneration is variable and unpredictable.
Healing of interradicular and intrabony lesions fol
-
lowing placement of iliac crest marrow was evaluated
in monkeys by Ellegaard et al. (1973, 1974). Regenera
tion occurred more frequently with the use of grafts,
but iliac crest marrow frequently resulted in ankylosis
and root resorption (Fig. 28-19).
Histologic evidence of periodontal regeneration in
humans following the use of iliac crest marrow grafts
was provided by Dragoo and Sullivan (1973a,b). At 8
months following therapy a mature periodontal liga-
664 • CHAPTER 28
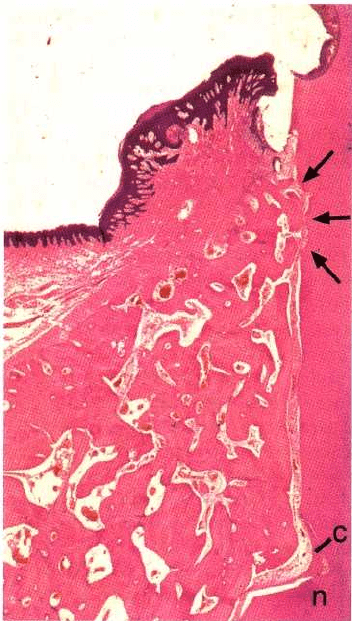
Fig. 28-19. Photomicrograph illustrating an intrabony
defect 2 months following grafting with iliac crest mar
-
row. The defect is completely filled with bone, but new
cementum (c) is lacking on the root surface except for
the most apical part (n) of the defect. Note that anky-
losis and root resorption (arrows) are occurring in the
coronal part of the defect.
ment was present at the grafted sites and about 2 mm
supracrestal new attachment had also formed. Clini-
cal evidence of root resorption was noted in 7 of the
250 grafted sites.
Due to the morbidity associated with the donor site
and that root resorption sometimes results, iliac crest
marrow grafts are not used in regenerative periodon-
tal therapy today.
Allogeneic grafts
Allogeneic grafts (allografts) were utilized in attempts
to stimulate bone formation in intrabony defects in
order to avoid the additional surgical insult associated
with the use of autogenous grafts. However, the use
of allogeneic grafts involves a certain risk regarding
antigenicity, although, in order to suppress foreign
body reactions, the grafts are usually pretreated by
freezing, radiation or chemicals.
The types of allogeneic grafts used are frozen iliac
cancellous bone and marrow, mineralized freeze-
dried
bone grafts (FDBA) and decalcified freeze-dried bone
grafts (DFDBA). The need for cross-matching to
decrease the likelihood of graft rejection as well as the
risk of disease transmission virtually eliminated the
use of frozen iliac allogeneic grafts in periodontics.
FDBA is a mineralized bone graft, which through
the manufacturing process loses cell viability and,
therefore, is supposed to promote bone regeneration
through osteoconduction (Goldberg & Stevenson
1987). The freeze drying also markedly reduces the
antigenicity of the material (Turner & Mellonig 1981,
Quattlebaum et al. 1988). The efficacy of freeze-dried
bone allogeneic grafts (FDBA) was evaluated in a
study
which included 89 clinicians (Mellonig 1991). At
re-
entry surgery it was found that 67% of the sites
treated with FDBA alone and 78% of the sites treated
with FDBA plus autogenous bone grafts demon-
strated complete or more than 50% bone fill. Thus,
FDBA plus autogenous bone appeared more effective
than FDBA alone. In split-mouth studies where FDBA
was combined with autogenous grafts or tetracycline
powder (Sanders et al. 1983, Mabry et al. 1985), a
defect fill of 60% and 80% of the initial lesion was
reported. In a split-mouth study it was also shown that
FDBA implantation had a similar effect on defect reso
-
lution as that achieved by DFDBA (Rummelhart et al.
1989) or granular porous hydroxyapatite (Barnett et
al. 1989). However, the only controlled clinical trial
comparing treatment of intrabony defects with FDBA
implantation versus flap surgery failed to demon-
strate any difference in terms of clinical attachment
gain and bone fill between test and control sites at 1
year re-entry examination (Altiere et al. 1979). In ad-
dition, human histologic specimens demonstrated
that implantation of FDBA in intrabony defects
yielded no periodontal regeneration but resulted in a
long epithelial attachment on the previously diseased
root surface (Dragoo & Kaldahl 1983).
Several animal studies suggested that deminerali-
zation of a cortical bone allograft (DFDBA) enhances
its osteogenic potential by exposing bone morpho-
genic proteins (BMPs) which presumably have the
ability to induce host cells to differentiate into
osteoblasts (Urist & Strates 1970, Mellonig et al. 1981).
Several case reports presented clinical improvements
and bone fill after implantation of DFDBA into in-
trabony defects (Quintero et al. 1982, Werbitt 1987,
Fucini et al. 1993, Francis et al. 1995), and controlled
clinical studies documented considerable gain of at-
tachment and bone fill in sites treated with DFDBA as
compared with non-grafted sites (Pearson et al. 1981,
Mellonig 1984, Meadows et al. 1993). However, no
statistical differences regarding attachment level
changes and bone fill were found when comparing
sites treated with FDBA and sites treated with DFDBA
(Rummelhart et al. 1989).
Histologic evidence of regeneration following
grafting with DFDBA was provided by Bowers et al.
(
1989b,c). Complete regeneration with new cemen-
tum, periodontal ligament and bone amounting to
80% of the original defect depth was reported at sites
treated with DFDBA, which was considerably more
than that observed in defects treated with surgical
debridement alone. However, animal experiments
