Cui Dongmei. Atlas of Histology: with functional and clinical correlations. 1st ed
Подождите немного. Документ загружается.

CHAPTER 9
■
Circulatory System
165
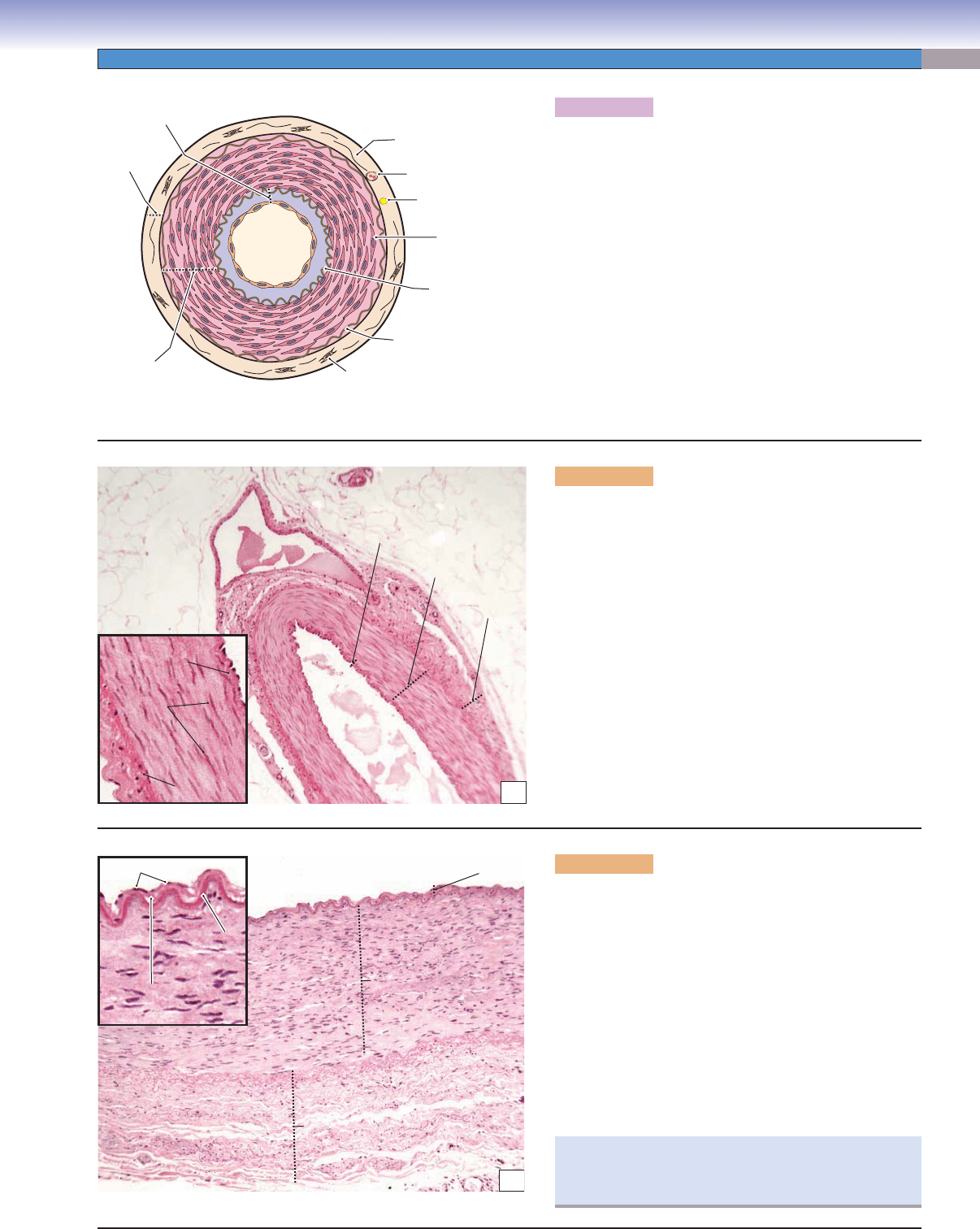
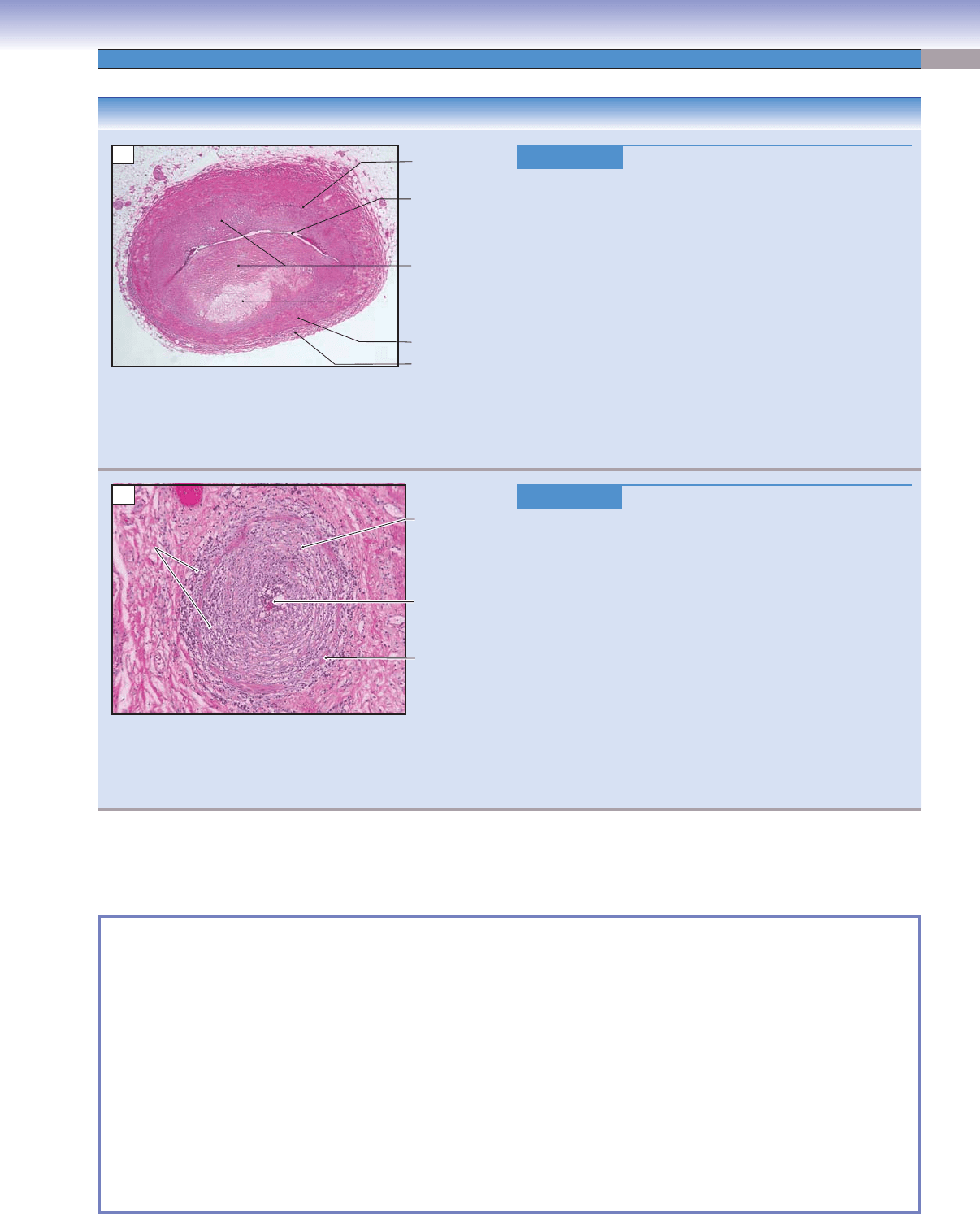
Figure 9-8A. A representation of a medium artery
(muscular or distributing artery).
The medium arteries are also called muscular arteries, refer-
ring to the fact that the arterial wall is dominated by smooth
muscle. There are about 6 to 40 layers of smooth muscle cells
that form a distinct sheath in the tunica media. In general,
the tunica media is much thicker than the tunica adventitia.
Vasoconstriction can be caused by smooth muscle contrac-
tion that is controlled by the sympathetic nervous system.
Internal and external elastic laminae are obvious in medium
arteries. The IEL separates the tunica intima from the tunica
media; the external elastic lamina (EEL) separates the tunica
media from the tunica adventitia. The tunica adventitia is
composed of connective tissues (fi broblasts and connective
tissue fi bers). Vasa vasorum may also be present. Medium
arteries, also sometimes called distributing arteries, distribute
blood to the small arteries in various organs of the body.
D. Cui /T. Yang
Tunica
adventitia
Tunica
media
Tunica
intima
Connective tissue
Fibroblast
Smooth
muscle cell
External elastic
lamina
Internal elastic
lamina
Vasa vasorum
Nerve
A
B
Smooth
Smooth
muscle
muscle
cells
cells
Smooth
muscle
cells
Tunica
intima
Tunica
media
Tunica
adventitia
Vein
Lumen of the
medium artery
Internal elastic
Internal elastic
lamina
lamina
Internal elastic
lamina
External
External
elastic lamina
elastic lamina
External
elastic lamina
Figure 9-8B. Medium artery (small muscular artery).
H&E, 68; inset 207
The size of medium arteries (muscular arteries) varies
depending upon the location. This is an example of a small
segment, which has 10 to 12 layers of smooth muscle cells
in the tunica media. Smooth muscle cells are arranged in
a circular orientation around the lumen, are connected
to each other by gap junctions, and are surrounded by
a network of extracellular matrix (see Fig. 6-13). This
arrangement allows the smooth muscle cells to function
as one unit. When smooth muscle contracts, the lumen
size decreases and blood pressure increases, thereby keep-
ing blood moving forward from medium arteries to small
arteries. Smooth muscle cells in the tunica media are the
targets of various neural and endocrine substances. Both
the IEL and EEL are prominent, appearing red-pink with
H&E stain.
C
Internal
Internal
elastic
elastic
lamina
lamina
Internal
elastic
lamina
Endothelium
Endothelium
Subendothelium
Subendothelium
Tunica
intima
Tunica
media
Tunica
adventitia
Endothelium
Subendothelium
Figure 9-8C. Medium artery (large muscular artery).
H&E, 68; inset 218
This is an example of a large segment of a medium artery,
which has about 20 to 40 layers of smooth muscle cells. The
tunica intima is composed of endothelium, subendothelial
connective tissue, and an IEL. The thin subendothelial
connective tissue layer may become thicker with age and in
atherosclerosis. The IEL is a wavy pink sheet forming the
boundary between the tunica intima and tunica media. In
general, the tunica media is the thickest layer, composed of
smooth muscle cells. The tunica adventitia is composed of
a layer of dense irregular connective tissue. Vasa vasorum
and nerve fi bers can be found in this layer but are not as
prominent as in elastic arteries.
Damage to endothelial cells can lead to various types
of cardiovascular diseases, such as atherosclerosis and
arteriosclerosis (see Synopsis 9-2).
CUI_Chap09.indd 165 6/17/2010 10:22:45 AM
166
UNIT 3
■
Organ Systems
Erythocytes
Erythocytes
Lumen
Lumen
Endothelium
Endothelium
Erythrocytes
Lumen
Endothelium
External
External
elastic lamina
elastic lamina
External
elastic lamina
Tunica
Tunica
media
media
Tunica
media
Internal
Internal
elastic lamina
elastic lamina
Internal
elastic lamina
Endothelial
Endothelial
cell junction
cell junction
Endothelial
cell junction
Collagen
Collagen
fibers
fibers
Collagen
fibers
Tunica
Tunica
media
media
Dense
Dense
bodies
bodies
Basal lamina
Basal lamina
Tunica
media
Dense
bodies
Basal lamina
Internal
Internal
elastic
elastic
lamina
lamina
Internal
elastic
lamina
A
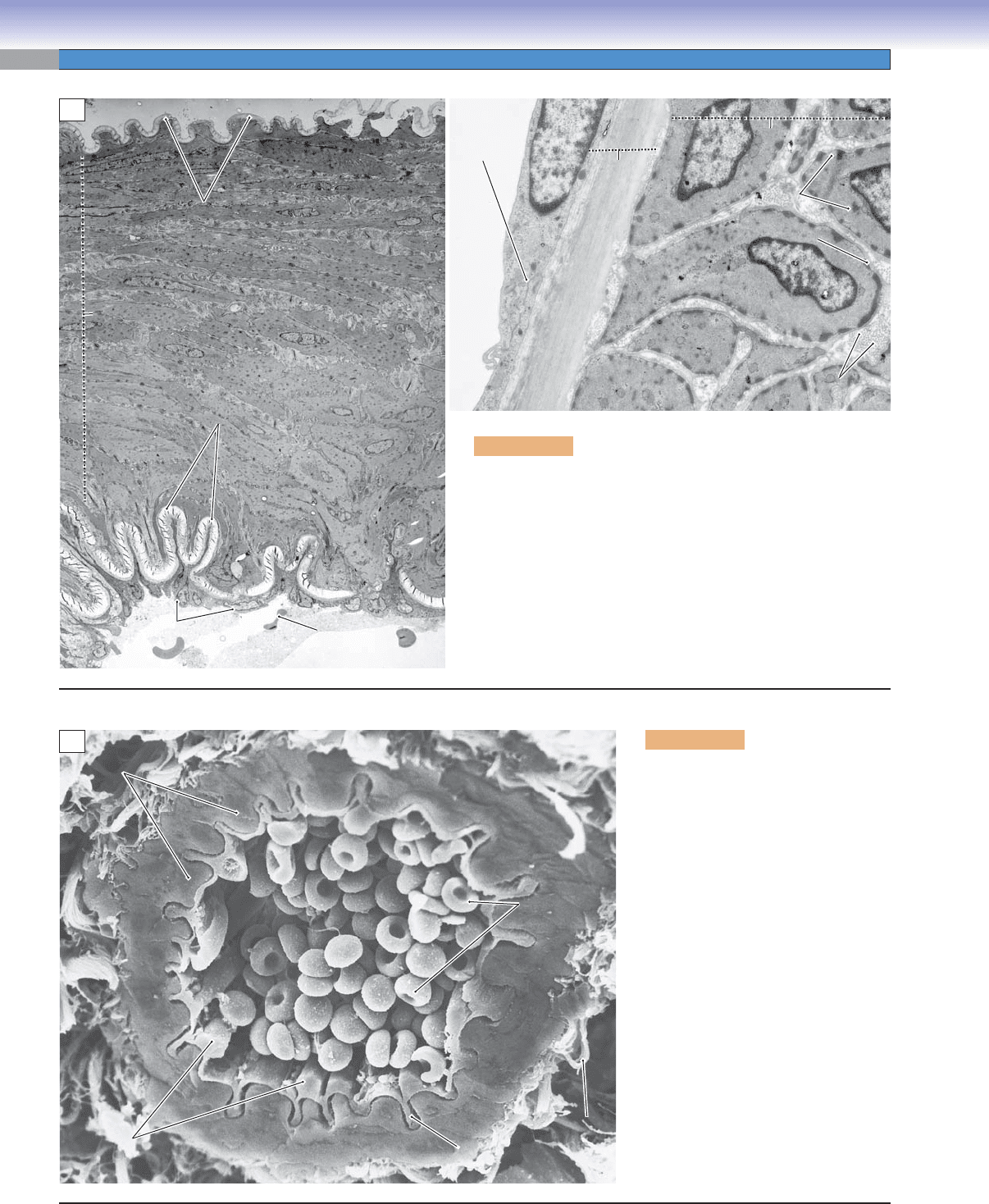
Figure 9-9B. Small artery. SEM,
1,300
In this scanning electron micrograph of
a small artery, the endothelial cells are
extremely squamous, and they are so
closely apposed to the internal elastic
membrane that the interface between
the two layers is indistinguishable.
The smooth muscle cells of the tunica
media are also closely apposed to each
other so that boundaries between cells
are diffi cult to discern. The ground
substance of the tunica adventitia and
the surrounding connective tissue has
been removed during specimen pro-
cessing so that only some bundles of
collagen fi bers remain.
Smooth muscle
Smooth muscle
Smooth muscle
Erythrocytes
Erythrocytes
Erythrocytes
Collagen
Collagen
fiber
fiber
bundle
bundle
Collagen
fiber
bundle
Internal elastic
Internal elastic
lamina
lamina
Internal elastic
lamina
Endothelial cells
Endothelial cells
Endothelial cells
B
Figure 9-9A. Medium artery. TEM, 1,000 left; 8,700 above
In the wall of the healthy medium artery on the left, the layer
of squamous endothelial cells adheres closely to the prominent,
highly corrugated, internal elastic membrane. The external elastic
membrane is also corrugated but thinner. The thick tunica media
is composed of many layers of closely apposed smooth muscle
cells. In the higher magnifi cation view on the right, the dense bod-
ies and basal laminae that are characteristic of smooth muscle cells
are readily apparent. The amorphous appearance of the internal
elastic membrane is typical of elastic membranes in transmission
electron micrographs.
CUI_Chap09.indd 166 6/17/2010 10:22:50 AM
CHAPTER 9
■
Circulatory System
167
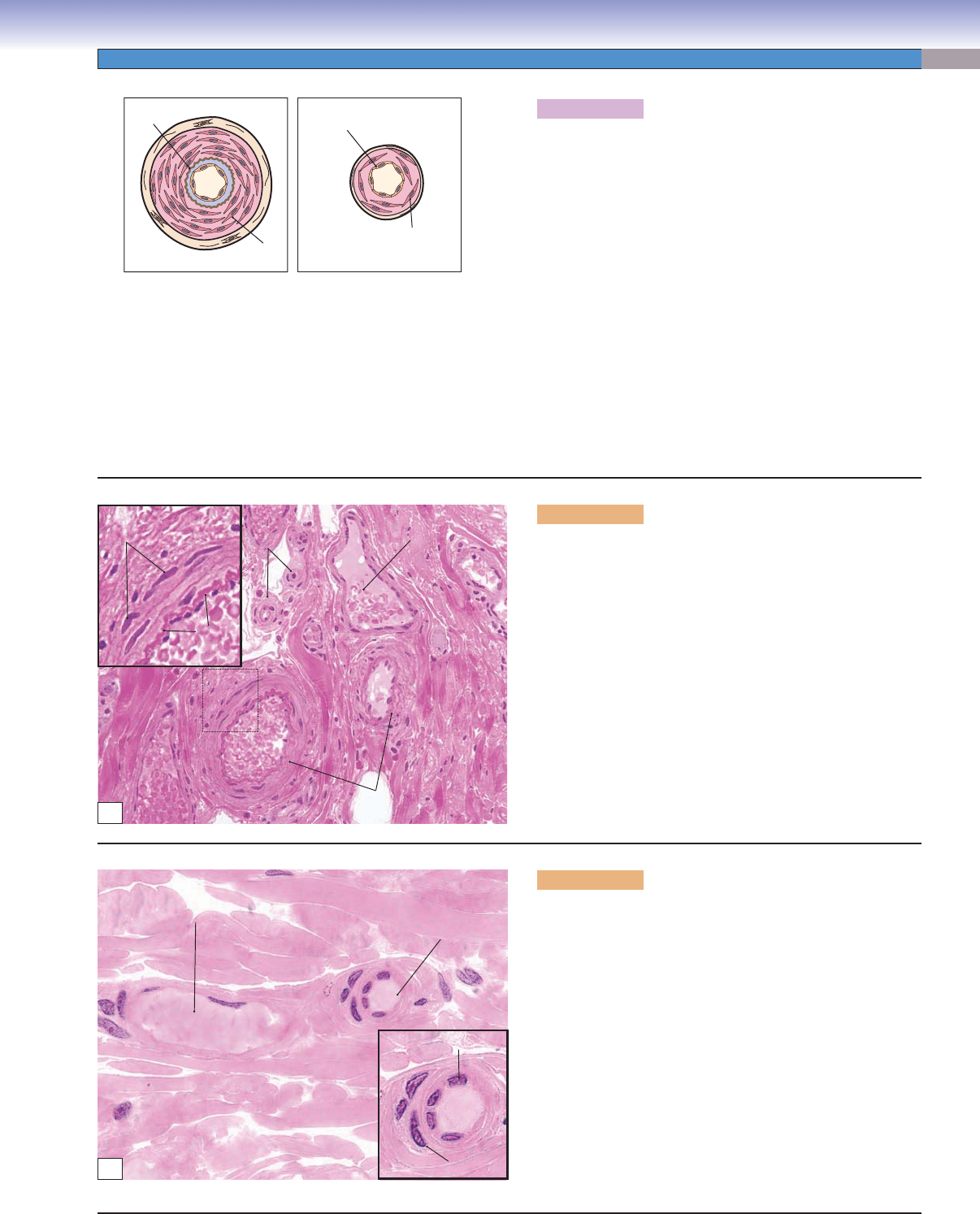
Figure 9-10A. A representation of a small artery and an
arteriole.
Small arteries (left) have the general structure of muscular
arteries but with a smaller diameter and no EEL. The tunica
media usually contains about three to six layers of smooth
muscle cells. An IEL is usually present but not prominent.
Small arteries help control and modulate blood pressure.
Arterioles (right) are the smallest arteries, leading blood fl ow
into capillary beds. They play an important role in regulat-
ing blood pressure and controlling the blood fl ow entering
capillaries. Arterioles have a very small diameter and narrow
lumen. There are only one to two layers of smooth muscle
cells in the arteriolar walls, and the tunica adventitia is barely
visible. Both an IEL and a subendothelial layer are often
absent.
Small arteries and arterioles are sometimes referred to as
resistance vessels because of their function in reducing and
stabilizing blood pressure before blood fl ows into the capil-
lary network.
A
D. Cui /T. Yang
Internal elastic
Small artery Arteriole
lamina
Tunica
media
D. Cui /T. Yang
Endothelial
cell
Smooth
muscle cell
Lumen of
Lumen of
small vein
small vein
Arteriole
Arteriole
Nuclei of smooth
Nuclei of smooth
muscle cells
muscle cells
Small arteries
Small arteries
Internal
Internal
elastic
elastic
lamina
lamina
Nuclei of smooth
muscle cells
Internal
elastic
lamina
Arteriole
Lumen of
small vein
Small arteries
B
Figure 9-10B. Small arteries, small intestine (ileum).
H&E, 136; inset 408
An example of a small artery in the tissue of the small intestine
is shown. Small arteries can be found in various types of tis-
sues and organs where oxygen, nutrients, and other materials
must be exchanged. Small arteries have a thin tunica intima
and tunica adventitia. The tunica media, the most obvious
layer in small arteries, contains three to six layers of circu-
larly arranged smooth muscle cells. An IEL is often present.
Smooth muscle is innervated by the autonomic nervous sys-
tem and regulates blood pressure by causing vasoconstriction
(sympathetic nervous system) and vasodilation (parasympa-
thetic nervous system).
Lumen of
venule
Arteriole
Endothelial cell
Smooth muscle cell
C
Figure 9-10C. Arterioles, tongue. H&E, 680; inset
1,020
Arterioles have a very small, round lumen (<0.5 mm in diam-
eter) and one or two layers of smooth muscle cells in the arte-
riolar wall. Arterioles are the last segment of the arterial sys-
tem. They connect small arteries to the capillary network. The
endothelium of these small vessels is able to sense changes in
blood pressure, blood fl ow, and oxygen tension and to respond
to these changes by releasing signals, such as endothelin (vaso-
constrictor) and nitric oxide (vasodilator). These signals regu-
late the tone of adjacent smooth muscle cells. Changes in muscle
tone control blood fl ow into the capillaries. Arterioles can be
structurally distinct depending on their location. For example,
arterioles in the lung are not structured identically to those in
the kidney. A venule accompanying an arteriole is shown here.
Venules have very thin walls consisting mainly of endothelium.
Smooth muscle cells are not prominent in venules.
CUI_Chap09.indd 167 6/17/2010 10:22:53 AM
168
UNIT 3
■
Organ Systems
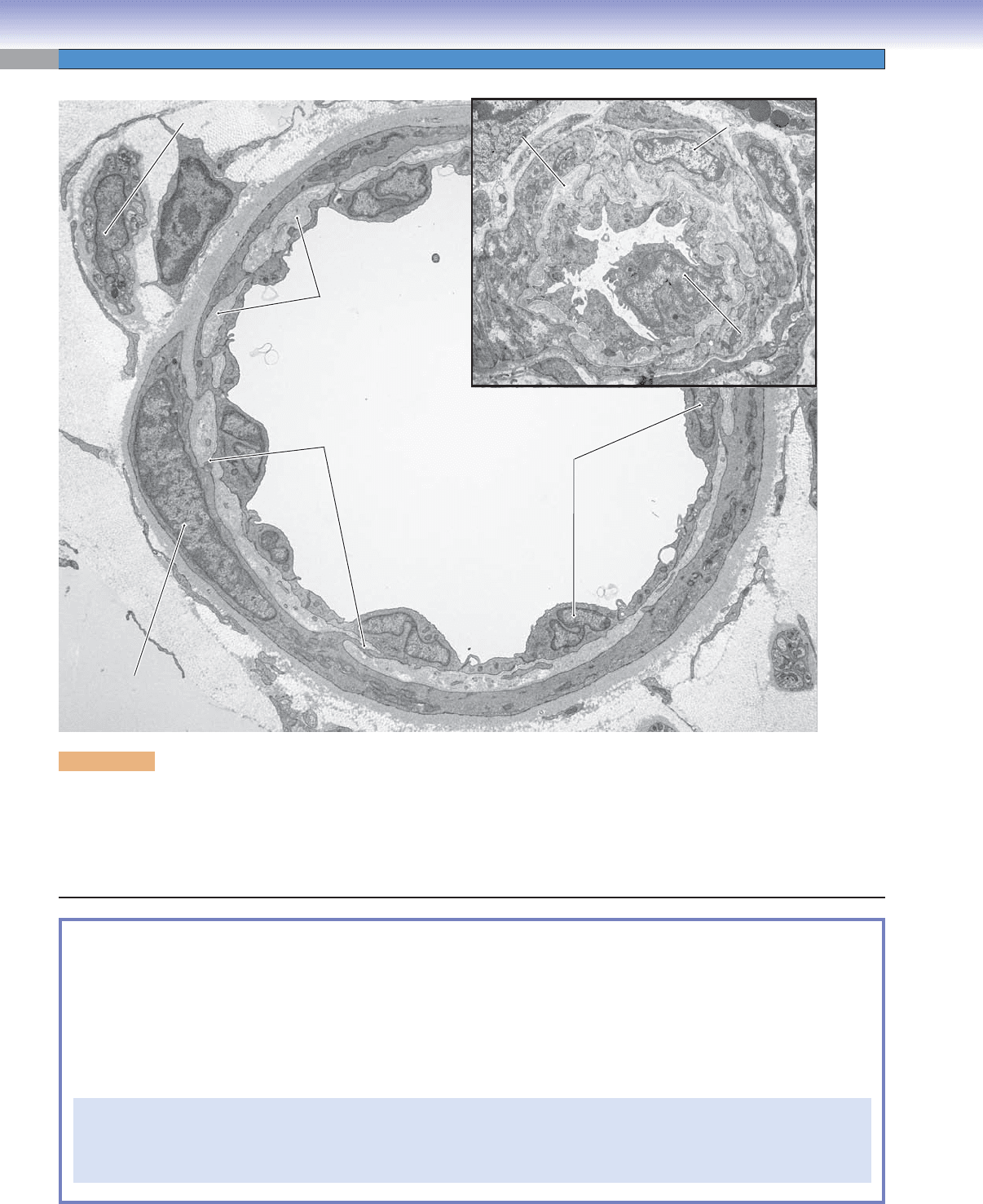
Figure 9-11. Arteriole. TEM, 5, 800; inset 3,800
The arteriole in the larger image was fi xed in a dilated state, whereas the inset shows a slightly smaller arteriole that was fi xed in a
contracted state. In both vessels, a thin elastic lamina separates the endothelium from the smooth muscle cells of the tunica media. The
state of contraction of the smooth muscle cells is regulated largely by signals from the endothelial cells. In addition to chemical messen-
gers, such as nitric oxide and endothelin, signaling may also involve direct contacts between endothelial and smooth muscle cells. The
cell in the upper left corner of the larger micrograph is a Schwann cell with several unmyelinated axons embedded in its cytoplasm.
Nucleus of smooth
Nucleus of smooth
muscle cell
muscle cell
Nucleus of
Nucleus of
Schwann cells
Schwann cells
Endothelium-smooth muscle
Endothelium-smooth muscle
cell junctions
cell junctions
Internal
Internal
elastic
elastic
lamina
lamina
Internal elastic
Internal elastic
lamina
lamina
Nucleus of smooth
Nucleus of smooth
muscle cell
muscle cell
Nuclei of
Nuclei of
endothelial
endothelial
cells
cells
Nucleus of
Nucleus of
endothelial
endothelial
cell
cell
Endothelium–smooth muscle
cell junctions
Internal
elastic
lamina
Internal elastic
lamina
Nucleus of smooth
muscle cell
Nucleus of
Schwann cell
Nuclei of
endothelial
cells
Nucleus of
endothelial
cell
Nucleus of smooth
muscle cell
SYNOPSIS 9-2 Functions of Endothelium in Blood Vessels
Endothelium provides a permeability barrier and controls the composition of interstitial tissue fl uid. ■
Endothelium allows the movement of leukocytes, fl uid, and immunoglobulins into tissues. ■
Endothelium provides for angiogenesis in the formation and differentiation of new blood vessels. ■
Endothelium provides signals that regulate the tone of adjacent vascular smooth muscle cells that control blood pressure ■
by vasoconstriction (endothelin) and vasodilation (nitric oxide, prostacyclin).
Endothelium provides anticoagulant signals (thrombomodulin, nitrous oxide, and prostacyclin) that inhibit platelet attach-
■
ment and aggregation to prevent blood clotting and allow unobstructed fl ow of blood in normal conditions.
When endothelial cells are injured, they reduce the production of platelet inhibitors and increase the release of stimulators
of platelet activation (e.g., von Willebrand factor, tissue thromboplastin). Exposure of the underlying basal lamina and con-
nective tissue further stimulates platelets to adhere and aggregate. Damage to the endothelium will slow down oxidation and
clearance of low-density lipoprotein, leading to many cardiovascular diseases such as atherosclerosis.
CUI_Chap09.indd 168 6/17/2010 10:22:57 AM
CHAPTER 9
■
Circulatory System
169
SYNOPSIS 9-3 Pathological and Clinical Terms for the Circulatory System
Vasculitis ■ : Infl ammation and damage to blood vessels often resulting in ischemia of the tissue served by the affected vessels;
may be related to infection, medications, and various autoimmune disorders.
Angina
■ : Chest pain associated with ischemia of the myocardium, most often due to severe atherosclerosis of the coronary
arteries; the pain of angina, often described as pressure, is typically substernal but may radiate to the arms or neck.
Myocardial infarction
■ : Necrosis of cardiac muscle due to interruption of its blood supply, most often due to coronary
artery atherosclerosis.
Atherosclerosis
■ : The most clinically signifi cant form of arteriosclerosis (“hardening of the arteries”), characterized by the
accumulation of lipid within the intima of arteries producing plaques that cause narrowing, or “stenosis,” of the artery.
Arteriosclerosis
■ : A general term referring to any hardening (loss of elasticity) of arteries, especially small arteries. High
blood pressure is the most common cause. Atherosclerosis is one form of arteriosclerosis.
Thrombus
■ : A blood clot formed within an artery or vein as a result of endothelial injury, abnormal blood fl ow, or an
increased tendency to form clots (hypercoagulability); rupture of an atherosclerotic plaque in a coronary artery promotes
the formation of a thrombus.
CLINICAL CORRELATIONS
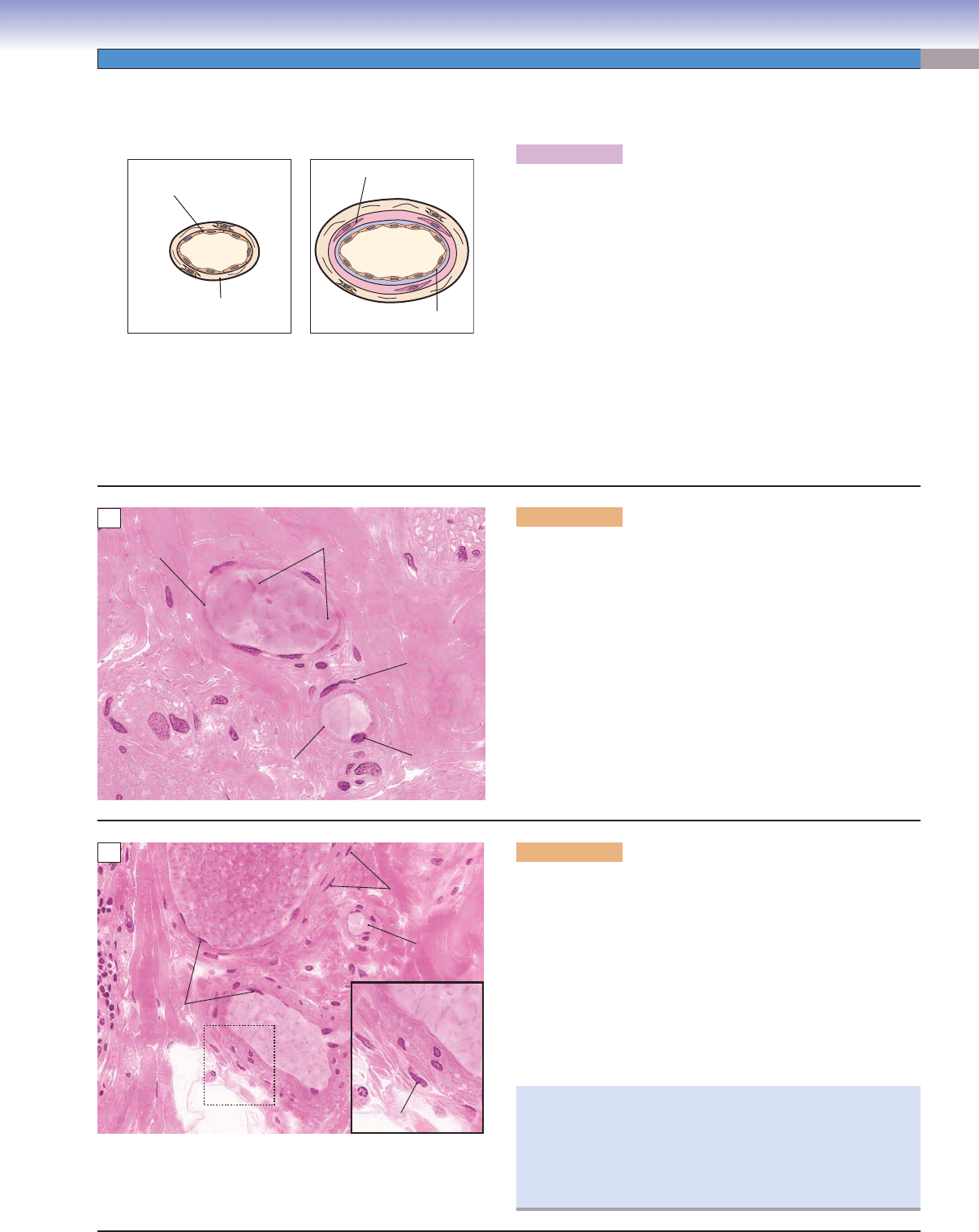
Figure 9-12A.
Coronary Artery Atherosclerosis. H&E, 21
Coronary artery atherosclerosis, also known as CAD, is
characterized by the presence of atherosclerotic changes
within the walls of the coronary arteries (see Fig. 3-3C).
These changes include accumulation of lipid, formation of
atherosclerotic plaques, and thickening of arterial tunica
intima. Eventually
, normal blood fl ow to the heart muscle is
impaired or obstructed. Rupture of an atherosclerotic plaque
promotes the formation of a blood clot, or thrombus, which
may occlude the lumen of the coronary artery. Angina (car-
diac chest pain), even MI (heart muscle death) (see Fig. 9-4C),
can develop when blood fl ow is reduced below a certain level.
CAD is a progressive disease process that generally begins in
childhood and manifests clinically in mid-to-late adulthood.
Lifestyle changes to lower blood cholesterol and control
hypertension and diabetes are important in preventing the
disease and reducing the severe consequences.
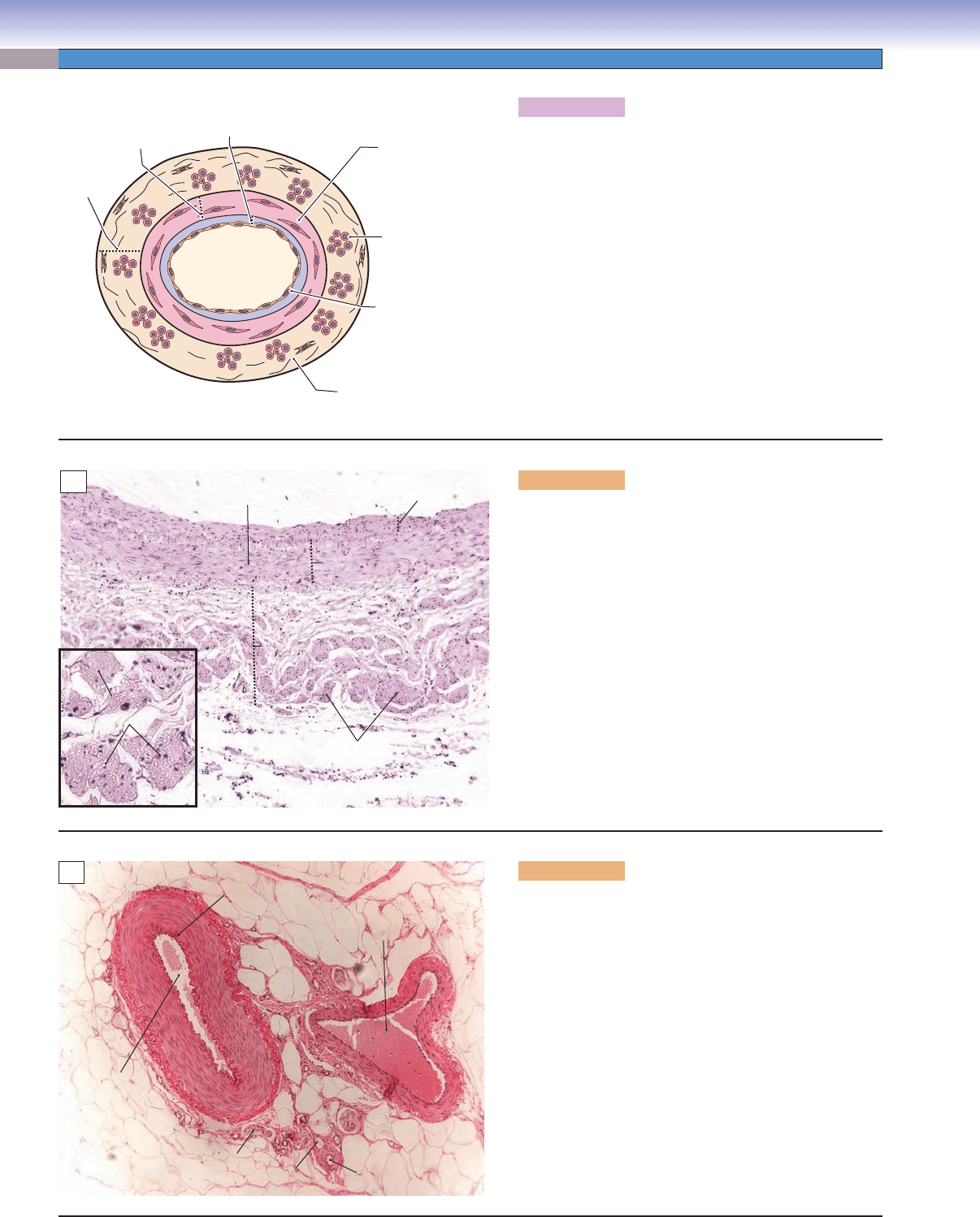
Figure 9-12B.
Polyarteritis Nodosa (Vasculitis), Small Artery
in Intestine. H&E, 71
Polyarteritis nodosa is a multisystem necrotizing vasculitis of
small and medium-sized muscular arteries in which involve-
ment of renal and visceral arteries is characteristic. Classic
polyarteritis nodosa spares the pulmonary arteries. The cause
of the disease is not clear, but it is associated with hepatitis B
virus infection in 20% to 30% of cases. Symptoms may be
nonspecifi c, making it diffi cult to diagnose. Fever, weight loss,
and malaise are present in more than 50% of cases. Patients
may present with fever, headache, weakness, abdominal pain,
and myalgias. Histologically, affected arteries are characterized
by segmental transmural infl ammation. Internal and external
elastic laminae are disrupted, which may lead to aneurysms
and bleeding. Polymorphonuclear leukocytes and mononu-
clear leukocytes are visible in the cellular infi ltrate. Steroids
are the major drugs used to control disease progression.
Fibrous
thickening of the
tunica intima
Central lipid core
(with cholesterol
clefts)
Tunica media
Tunica adventitia
Narrow lumen
Internal elastic
lamina
A
Inflammatory
Inflammatory
leukocytes
leukocytes
Diminished
lumen
of the
small artery
Inflammatory
leukocytes
Fibrous
thickening of the
tunica intima
Disrupted
internal elastic
lamina
B
CUI_Chap09.indd 169 6/17/2010 10:23:01 AM
170
UNIT 3
■
Organ Systems
The Capillary System
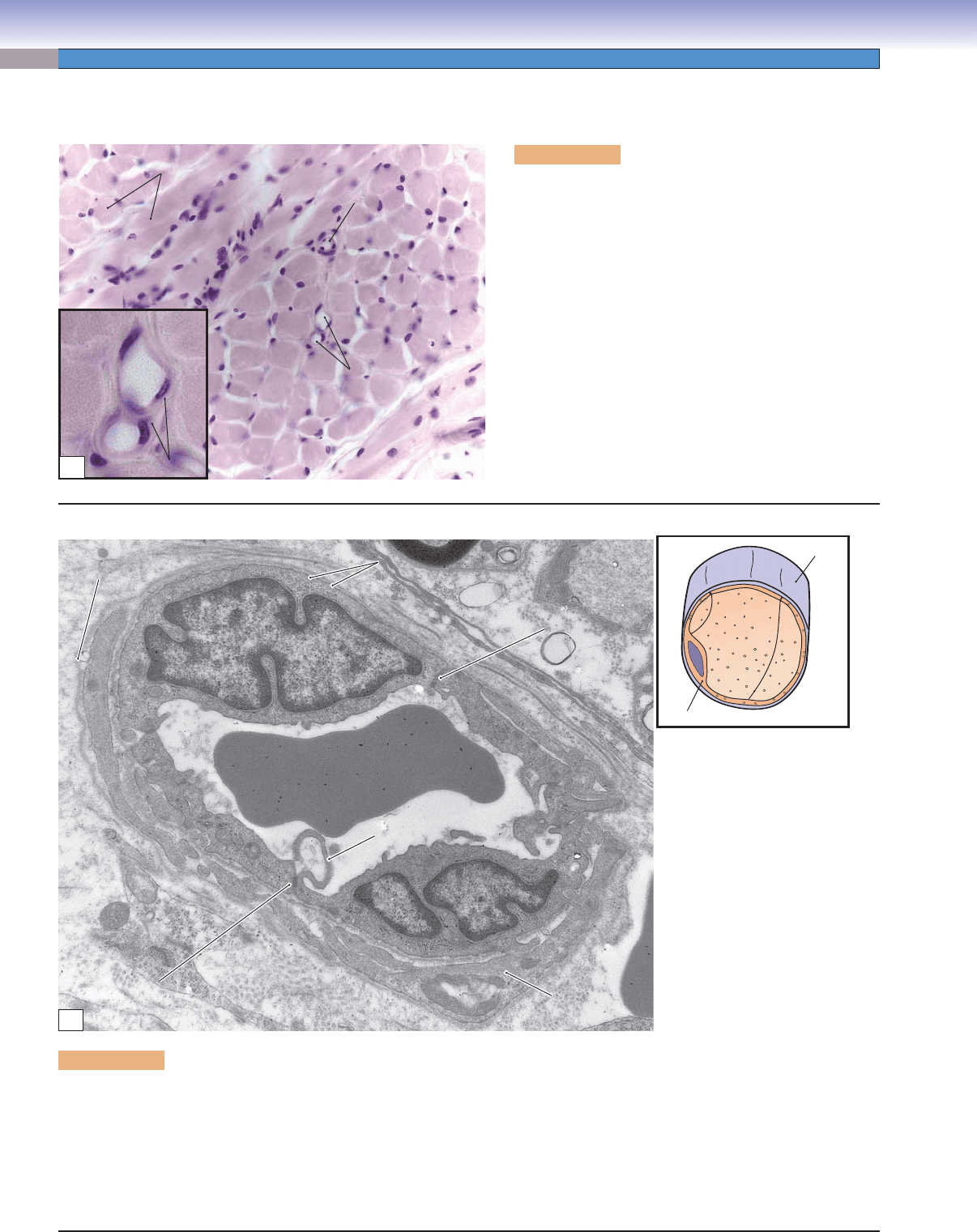
Figure 9-13A. Continuous capillaries, skeletal muscle.
H&E, 272; inset 870
Capillaries, the smallest vessels (5–10 μm in diameter) in the
blood circulatory system, connect arterioles to venules. Capil-
laries contain one layer of endothelial cells with a basal lamina
sometimes wrapped by pericytes. According to the structure
of the endothelial cells and the continuity of the basal lamina,
capillaries can be classifi ed into three types: (1) continuous
capillaries, (2) fenestrated capillaries, and (3) discontinuous
(sinusoidal) capillaries. Continuous capillaries have complete
endothelial cells (no pores), interrupted only by intercellular
clefts between the cells, and a continuous basal lamina with
no breaks in the endothelial barrier between the vascular
compartment and the surrounding tissues. Such structures
in the continuous capillaries allow very limited amounts of
materials to pass through their walls. Continuous capillaries
can be found in muscles, connective tissues, nervous tissues,
lungs, exocrine glands, and the thymus.
Arteriole
Muscle fibers
Capillaries
Endothelial cells
A
Figure 9-13B. Continuous capillary, loose connective tissue. EM 5,100
The caliber of this continuous capillary can be inferred from the erythrocyte that occupies the lumen. Nuclei of two endothelial cells
are prominent, and portions of pericytes can be seen external to the endothelial cells. A continuous layer of endothelial cell cyto-
plasm forms a barrier between the capillary lumen and the surrounding tissue compartment. Junctions between adjacent endothe-
lial cells can be of both the occludens and the adherens types. Marginal folds, such as the one beneath the erythrocyte, are typical
features at the junctions between capillary endothelial cells. Each endothelial cell has numerous caveolae beneath its plasmalemma,
although these structures are diffi cult to discern at this magnifi cation. The caveolae are a manifestation of active transcytosis of
materials between the plasma and the tissue space.
T. Yang
Basal lamina
Endothelial cell
Caveolae
Caveolae
Erythrocyte
Erythrocyte
Marginal fold
Marginal fold
Pericyte
Pericyte
Intercellular
Intercellular
junction
junction
Intercellular
Intercellular
junction
junction
Basal lamina of
Basal lamina of
pericyte
pericyte
Erythrocyte
Marginal fold
Pericyte
Intercellular
junction
Caveolae
Intercellular
junction
Basal lamina of
pericyte
B
CUI_Chap09.indd 170 6/17/2010 10:23:03 AM
CHAPTER 9
■
Circulatory System
171
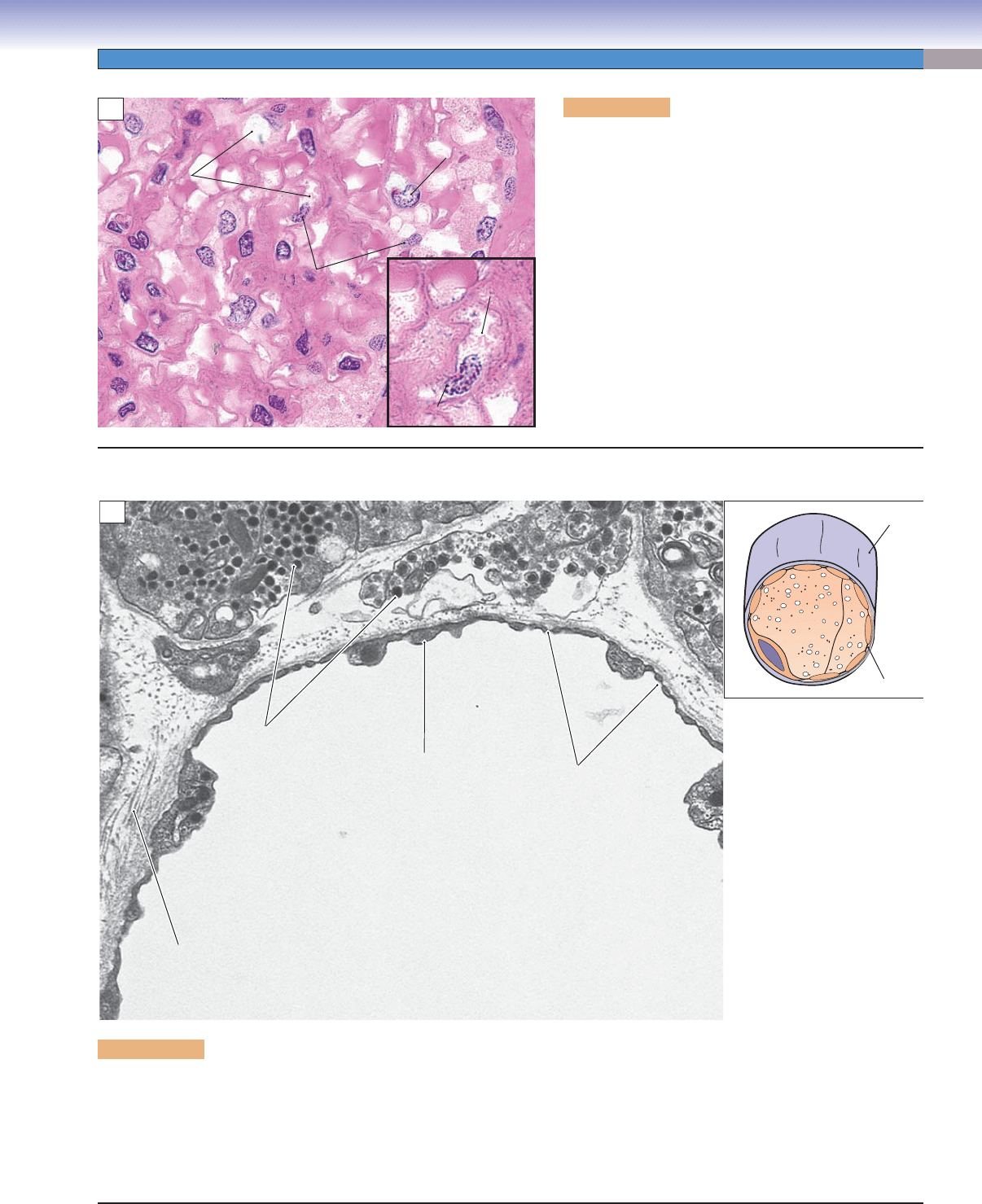
Figure 9-14A. Fenestrated capillaries, kidney. H&E,
680; inset 1,405
Fenestrated capillaries have endothelial cells that are
perforated by small pores, often bridged by diaphragms
(the glomerulus of the kidney is an exception). The basal
laminae beneath the endothelial cells are continuous. This
type of capillary allows a greater range of substances to
pass freely through the capillary wall. Examples of fenes-
trated capillaries are the capillary beds in the intestine
(where nutrients are absorbed), the glomerulus of the
kidney (where blood is fi ltered and urine is formed), and
the capillaries in the endocrine organs, such as in the pitu-
itary gland and endocrine pancreas (where hormones are
secreted and released into the capillaries). The glomerular
capillaries in the kidney are shown here.
Lumen of
Lumen of
capillary
capillary
Podocyte
Podocyte
Endothelial cell
Endothelial cell
Endothelial cells
Endothelial cells
Glomerular
Glomerular
capillaries
capillaries
Glomerular
capillaries
Podocyte
Endothelial cell
Endothelial cells
Lumen of
capillary
A
Figure 9-14B. Fenestrated capillary, pituitary. EM, 14,000
The wall of this fenestrated capillary consists of a thin layer of cytoplasm interrupted at frequent intervals by circular pores, termed
fenestrations, of fairly consistent diameter (about 70 nm). This permits freer movement than occurs in continuous capillaries for
some molecules such as peptide hormones. In order to pass between the vascular compartment and the interstitial tissue compart-
ment, dissolved molecules still must pass through the diaphragms that bridge the pores, and the endothelial cells still produce a
complete basal lamina at the interface with the surrounding tissue. Fenestrated capillaries are found in the gastrointestinal tract, the
kidney, and in endocrine glands. The vessel shown here is located in the anterior pituitary.
T. Yang
Diaphragm
Basal lamina
Lumen of a
Lumen of a
fenestrated capillary
fenestrated capillary
Secretory granules
Secretory granules
containing hormones
containing hormones
Collagen
Collagen
fibers
fibers
Diaphragm of
Diaphragm of
fenestration
fenestration
Endothelial cell
Endothelial cell
cytoplasm
cytoplasm
Collagen
fibers
Diaphragm of
fenestration
Lumen of a
fenestrated capillary
Endothelial cell
cytoplasm
Secretory granules
containing hormones
B
CUI_Chap09.indd 171 6/17/2010 10:23:07 AM
172
UNIT 3
■
Organ Systems
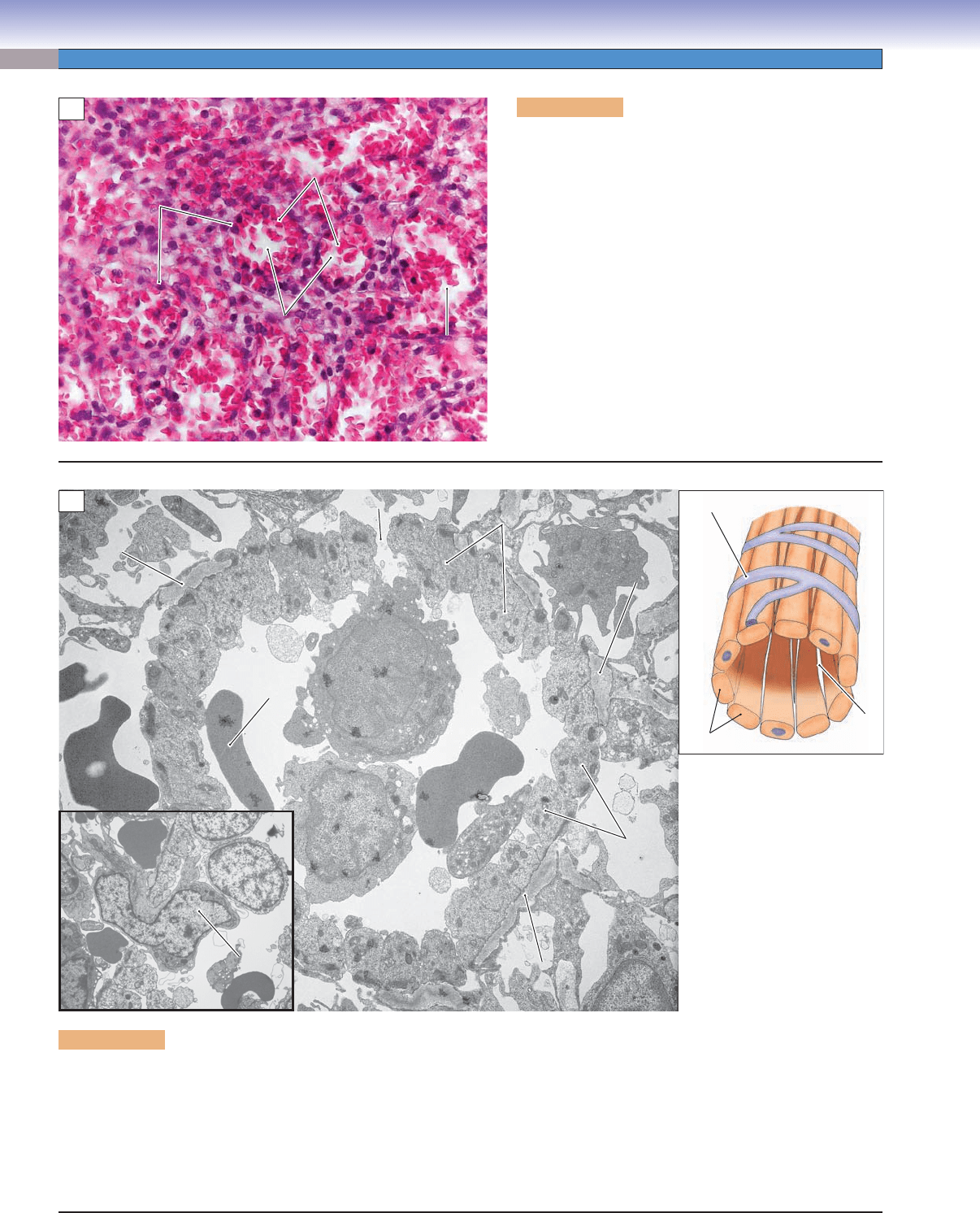
Figure 9-15A. Discontinuous capillaries, spleen. H&E,
274
Discontinuous capillaries, also called sinusoidal capillaries
(or sinuses), are characterized by large pores, which per-
forate the cytoplasm of endothelial cells, and incomplete
or missing basal laminae. In addition, the sinusoids have
large intercellular clefts (gaps between endothelial cells).
These structures permit free movement of proteins, plasma
constituents, and other materials. In some cases, even cells
can pass through the capillary wall. This type of capillary
has a large diameter (30–60 μm) and may have an irregular
shape due to an incomplete basal lamina, spindle-shaped
endothelial cells, and fenestrated structures. Discontinu-
ous capillaries can be found in the liver, spleen, bone mar-
row, and lymph nodes.
A
Endothelial
Endothelial
cells
cells
Erythrocytes
Erythrocytes
Capillaries
Capillaries
(sinusoids)
(sinusoids)
Capillaries
Capillaries
(sinusoids)
(sinusoids)
Endothelial
cells
Erythrocytes
Capillaries
(sinusoids)
Capillaries
(sinusoids)
Figure 9-15B. Discontinuous (sinusoidal) capillary. EM, 5,200; inset 3,400
Sinusoidal capillaries vary greatly in appearance, but they all have as common features, lumens of large diameter and gaps or
potential gaps between and sometimes even within endothelial cells. Objects as large as cells can pass through these discontinuities.
The sinusoidal capillary shown here is located in the red pulp of the spleen, and it is termed a red pulp sinusoid. The endothelial
cells are elongated with the long axis parallel to the long axis of the vessel. In cross section, as seen here, the endothelial cells are
nearly circular in shape. There are gaps between cells, such as the one seen at the top edge of this example, but many neighboring
endothelial cells are in close contact. Nevertheless, as seen in the inset, motile blood cells and macrophages can pass readily between
adjacent endothelial cells because of sparseness of intercellular junctions and the incomplete basement membrane.
T. Yang
Migrating cell
Migrating cell
Gap
Gap
Red pulp
Red pulp
cord
cord
Erythrocyte
Erythrocyte
Monocyte
Monocyte
Basement
Basement
membrane
membrane
Basement
Basement
membrane
membrane
Lumen
Lumen
Basement
Basement
membrane
membrane
Endothelial
Endothelial
cells
cells
Endothelial
Endothelial
cells
cells
Erythrocyte
Migrating cell
Monocyte
Basement
membrane
Basement
membrane
Lumen
Basement
membrane
Endothelial
cells
Endothelial
cells
Gap
Red pulp
cord
Endothelial cells
Gap
Incomplete basal lamina
Incomplete basal lamina
Incomplete basal lamina
B
CUI_Chap09.indd 172 6/17/2010 10:23:10 AM
CHAPTER 9
■
Circulatory System
173
The Venous System
Figure 9-16B. Venule and arteriole, colon. H&E, 680
This venule (muscular venule) and companion arteriole were taken
from the colon of the large intestine. Venules have larger lumens
than arterioles. In histological sections, they often have blood
cells remaining inside the lumen. Venules are the smallest veins;
they drain blood from capillaries into the small veins. They are
also involved in exchange of metabolites with tissues and allow
blood cells to migrate from the vessels into the tissues (diapedesis).
The postcapillary venules are the primary sites involved in the
infl ammatory response; they allow leukocytes (white blood cells)
to migrate into the affected tissues in cases of infl ammation or
infection. Note that the companion artery has a small, round
lumen and a single layer of smooth muscle cells. There are fewer
or no blood cells in the lumen of an arteriole specimen, because of
the higher pressure and stronger contraction of the arteriole wall.
Venule
Blood cells
Arteriole
Endothelial cell
Smooth
muscle
cells
B
Figure 9-16C. Small vein, colon. H&E, 272; inset 527
Small veins have one to three layers of isolated smooth muscle cells
in the walls. The tunica adventitia of small veins is a little thicker
than that of venules. Small veins have a thinner wall and less dis-
tinguishable smooth muscle layers than do small arteries (also
see Fig. 9-10B). Small veins gradually increase in size to become
medium veins. Microvessels include arterioles, capillaries, and
venules and play a key role in the response to infl ammation. During
infection or tissue injury, immune cells (such as mast cells and
basophils) release histamine and heparin. In response, the endothe-
lium of microvessels allows fl uid leakage (edema) and relaxation of
smooth muscle cells, leading to vessel dilation (redness and heat).
Endothelial
cell
Lumen of a
small vein
Lumen of a
small vein
Arteriole
Smooth
muscle
nuclei
Smooth muscle nucleus
C
Exudation is the escape of blood fl uid and protein from the
lumen of the vessel into the interstitial tissue when the cell-to-
cell junctions of the endothelium loosen. Transudation is move-
ment, due to hydrostatic imbalance, of the blood plasma fl uid
from the lumen to the interstitial tissue, with large protein and
cells fi ltered out by the normal endothelial wall.
Figure 9-16A. A representation of a venule and small vein.
The venous system is composed of venules, small veins, medium
veins, and large veins. These vessels carry blood from capillar-
ies in the tissues back to the heart. Small veins and venules are
very similar in structure and are sometimes diffi cult to distinguish
from one another. In general, small veins have larger lumens
and more visible smooth muscle cells than venules. Venules, the
smallest veins, receive blood from the capillary network. Venules
have small lumens and very thin walls, with only a single layer
of endothelium and a small amount of underlying connective
tissue (similar to large capillaries). They may have a few scat-
tered smooth muscle cells in the vessel walls. Venules gradually
increase in size to form small veins. They can be categorized as
postcapillary venules (10–30 μm in diameter), collecting venules
(30–50 μm) and muscular venules (50–100 μm). Postcapillary
venules connect directly to capillaries and drain blood into the
collecting venules. Muscular venules often accompany arterioles.
D. Cui /T. Yang
D. Cui /T. Yang
Smooth muscle cell
Venule Small vein
Endothelial
cell
Endothelium
Connective tissue
A
CUI_Chap09.indd 173 6/17/2010 10:23:15 AM
174
UNIT 3
■
Organ Systems
Figure 9-17A. A representation of a medium vein.
In general, the tunica media of veins is thinner than the
tunica adventitia, and smooth muscle cells in this layer are
not as well organized as in arteries. The tunica adventitia
of medium veins is more prominent and much thicker than
the tunica media. Medium veins have various sizes and
structural features depending on their location. The tunica
intima consists of an endothelium and a thin subendothe-
lial layer. The tunica media contains a few layers of circu-
larly arranged smooth muscle cells, which usually do not
form a distinct sheet. In some areas, large-sized medium
veins have a structure similar to that of large veins. Their
tunica intima is thinner, and the tunica adventitia contains
fewer bundles of longitudinal smooth muscle than large
veins. However, this characteristic is not prominent in
small segments of the medium veins. Valves are prominent
in medium veins, especially in the extremities of the body.
D. Cui /T. Yang
Tunica
adventitia
Tunica
media
Tunica
intima
Connective tissue
Longitudinal smooth
muscle bundle
Circular smooth
muscle layer
Endothelium
A
B
Smooth
Smooth
muscle bundles
muscle bundles
Smooth
muscle bundles
Longitudinal smooth
muscle bundles
Circular smooth
muscle layer
Tunica
intima
Tunica
media
Tunica
adventitia
Figure 9-17B. Medium vein, large segment of medium
vein. H&E, 68; inset 182
This sample of a large segment of medium vein has a
similar structure to a large vein but has fewer longitudi-
nal smooth muscle bundles in the tunica adventitia (Fig.
9-18B). The tunica intima is thinner than in the large veins,
and the tunica media contains several layers of circular
smooth muscle. The tunica adventitia is the thickest and
the most prominent layer in most medium veins. There are
some longitudinal smooth muscle bundles (inset) and con-
nective tissue in the tunica adventitia. In the extremities,
such as the legs and arms, there are many valves at vary-
ing intervals in the innermost layer of veins. They prevent
blood backfl ow against gravity. Veins carry blood toward
the heart under lower pressure than arteries and have a
great capacity for housing blood (about 65% of blood is
in the venous system); for this reason, they are sometimes
called capacitance vessels.
C
Internal
elastic
lamina
Lumen of the
medium artery
Lumen of the
medium vein
Arteriole
Venule
Nerve
fibers
Figure 9-17C. Medium vein, small segment of medium
vein. H&E, 68
Veins accompanying companion arteries are often found
in the tissues and organs. Structurally, medium arteries
have relatively smaller lumens, thicker walls, and more
prominent IEL than medium veins. The IEL is usually
absent in medium veins. In this example, a small segment
of a medium vein with a companion medium artery, the
vein has a larger lumen and a thinner wall than a compan-
ion artery. This medium vein does not show the promi-
nent tunica adventitia or the longitudinal smooth muscle
bundles usually seen in medium veins.
CUI_Chap09.indd 174 6/17/2010 10:23:18 AM
