Cui Dongmei. Atlas of Histology: with functional and clinical correlations. 1st ed
Подождите немного. Документ загружается.

CHAPTER 10
■
Lymphoid System
195
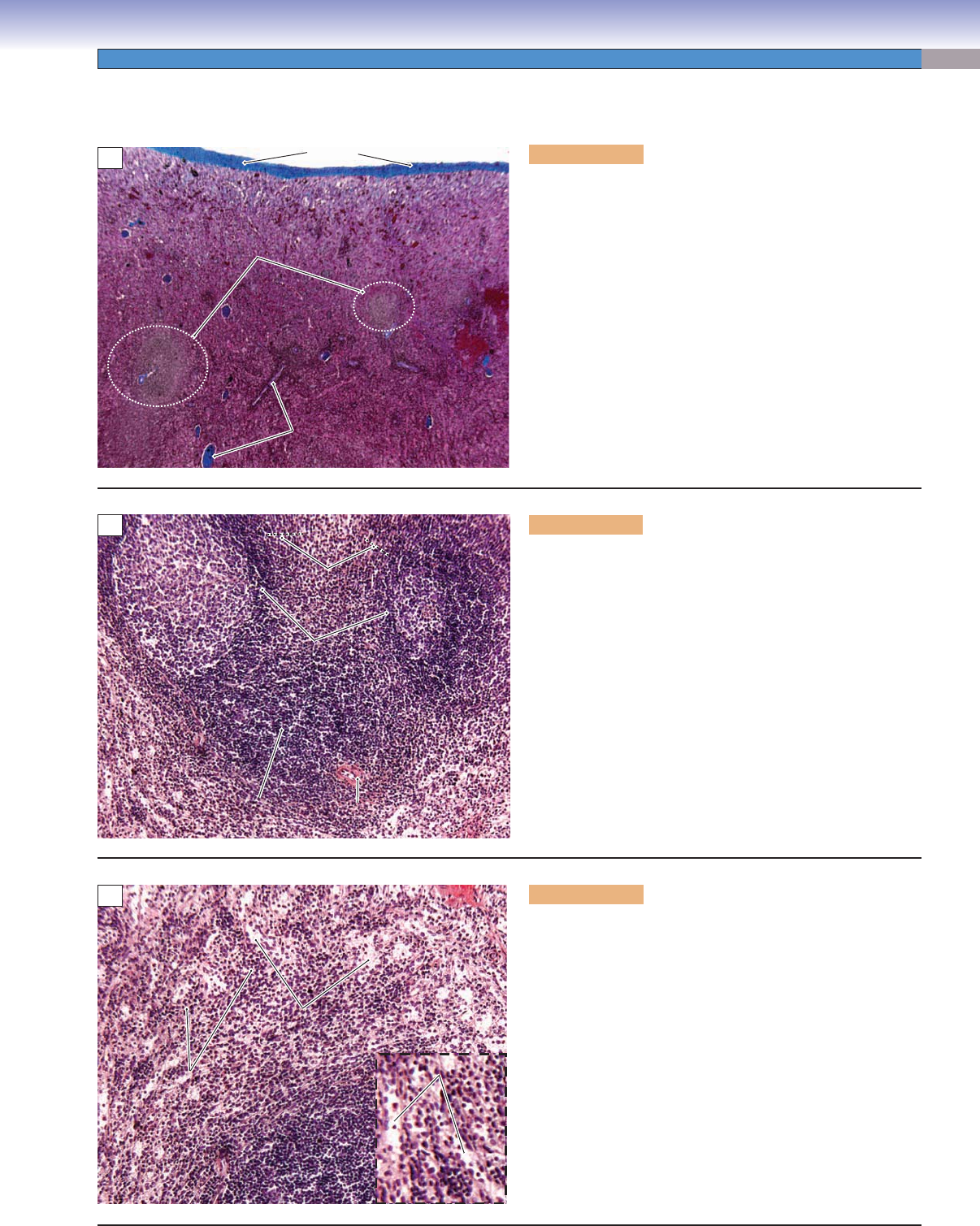
Figure 10-14A. Spleen. H&E, 60
The spleen is a large lymphoid organ (about 140–180 g in
humans) located in the left superior quadrant of the abdomen
(Fig. 10-6). It is covered by a thick, dense connective tissue
(capsule), which extends into the organ to form trabeculae.
Trabeculae provide structural support for arteries and veins,
which supply the compartments (white and red pulp) of the
spleen. The spleen is not organized into a cortex and medulla as
are lymph nodes and the thymus but is divided into white pulp
associated with a central artery and red pulp associated with
a vein and venous sinusoids. Functions of the spleen include
(1) an immune component (white pulp) to activate lymphocytes
and promote antibody production by plasma cells, (2) fi ltration
of blood and destruction of aged erythrocytes in red pulp, and
(3) serving as reservoir for erythrocytes and platelets.
Capsule
Capsule
Capsule
White pulp
White pulp
Red pulp
Red pulp
White pulp
Red pulp
Red pulp
Red pulp
Red pulp
Trabeculae
Trabeculae
Red pulp
Red pulp
Trabeculae
Red pulp
A
Germinal
Germinal
center
center
Germinal
center
Marginal zone
Marginal zone
Marginal zone
G
G
G
Mantle
Mantle
zone
zone
Mantle
zone
Central
Central
artery
artery
Central
artery
Primary
Primary
follicle
follicle
Primary
follicle
PALS
PALS
PALS
PALS
PALS
PALS
B
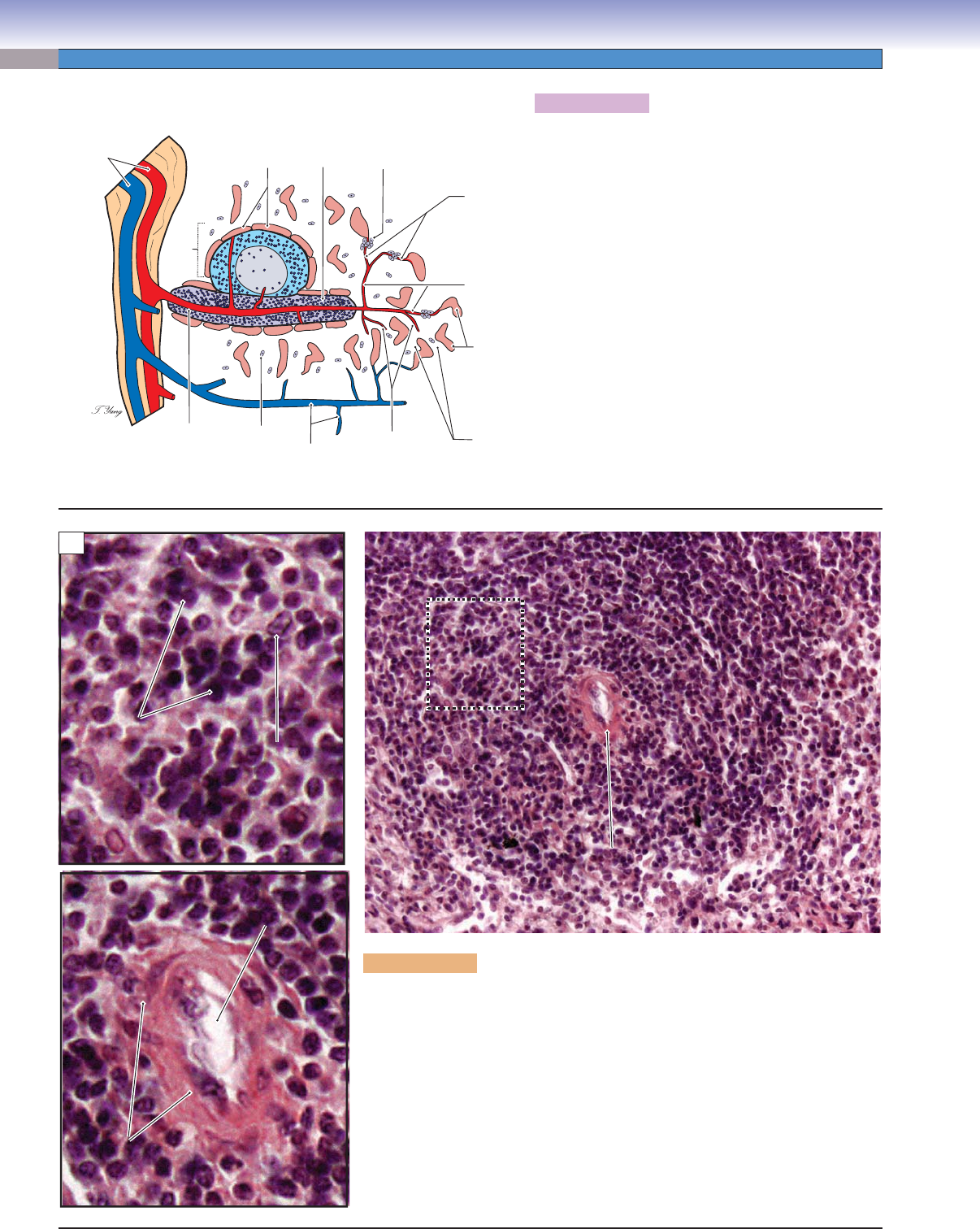
Figure 10-14B. White pulp, spleen. H&E, 194; inset
748
White pulp and red pulp are the two basic components of the
spleen. White pulp is composed of a central artery, a PALS,
and a lymphatic nodule. The nodules with germinal centers are
secondary nodules (follicles) where B cells actively differentiate
into large cells (lymphoblasts and lymphocytes). The dark ring
region around the germinal center is the mantle zone where
small inactive B cells are hosted. The mantle zone stains dark
because of densely packed lymphocytes. The nodules without
the germinal centers are primary nodules, which contain most
of the inactive B cells. The region that surrounds the white
pulp is the marginal zone, which contains marginal sinuses.
(G, germinal center.)
Splenic
Splenic
cord
cord
Lymphatic
Lymphatic
nodule
nodule
Splenic
cord
Lymphatic
nodule
Venous
Venous
sinuses
sinuses
Venous
sinuses
Splenic
Splenic
cord
cord
Splenic
cord
Venous sinuses
Venous sinuses
Venous sinuses
C
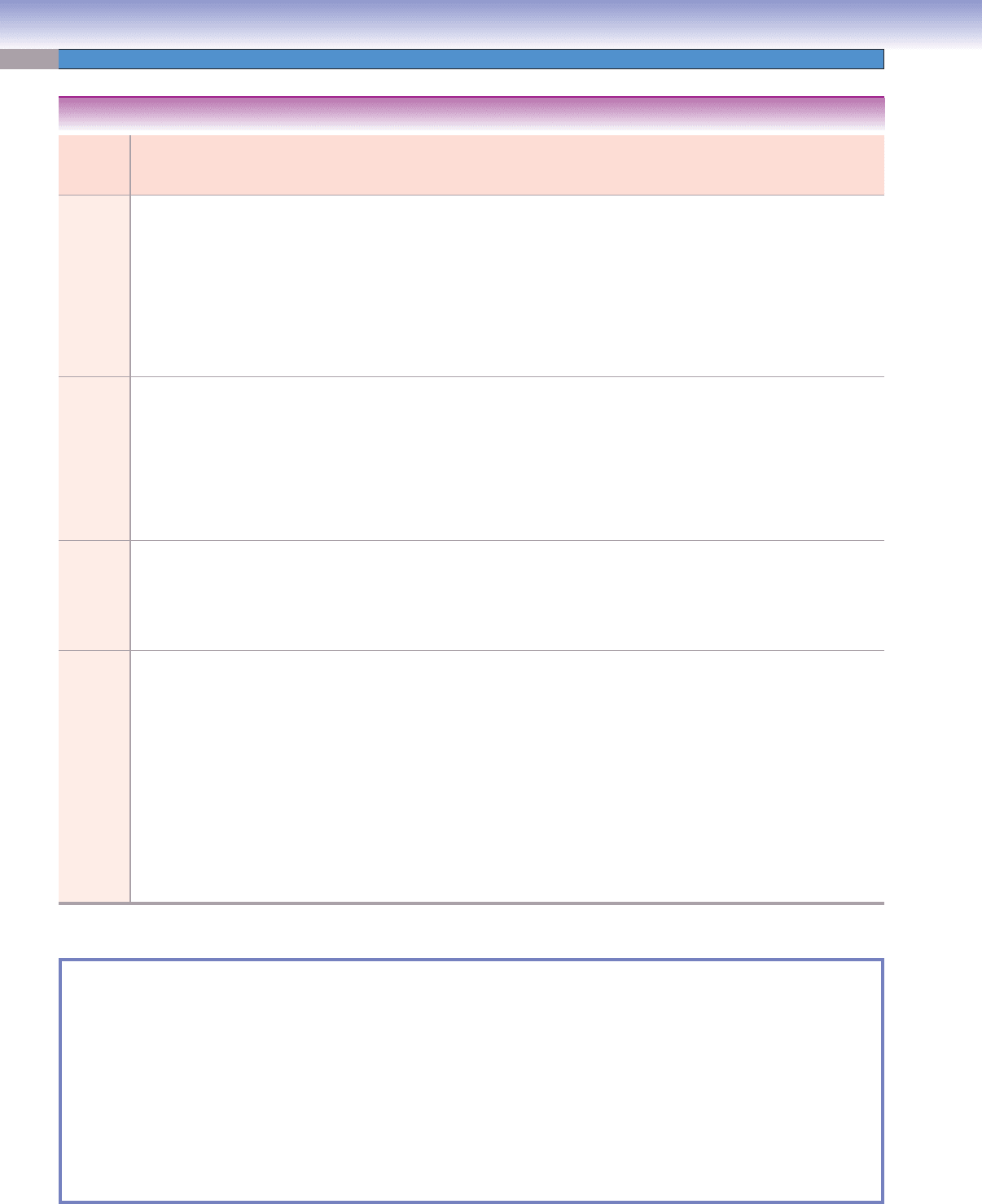
Figure 10-14C. Red pulp, spleen. H&E, 256; inset 385
Red pulp (red because it is rich in blood) stains light and con-
tains splenic cords and venous sinuses that are fi lled with blood.
Venous sinuses are discontinuous capillaries, which have large
lumens, incomplete basal laminae, and gaps between endothe-
lial cells. These special features allow blood cells to pass
through the capillary wall (see Fig. 9-14A,B). The splenic cord
is a framework of reticular tissue that contains B cells, T cells,
plasma cells, macrophages, and other blood cells. Macrophages
in the splenic cord often extend their processes into the lumen
of the sinuses to reach and engulf foreign substances, microbes,
and aged erythrocytes. The red pulp of the spleen also serves as
a reservoir for platelets (Fig 10-16).
Spleen
CUI_Chap10.indd 195 6/2/2010 4:12:14 PM
196
UNIT 3
■
Organ Systems
Lymphocytes
Lymphocytes
Macrophage
Macrophage
Lymphocytes
Macrophage
Luman of
Luman of
central artery
central artery
Lumen of
central artery
Endothelial
Endothelial
cells
cells
T cells
T cells
T cells
Endothelial
cells
Central artery
Central artery
PALS
PALS
Central artery
PALS
PALS
PALS
PALS
PALS
PALS
PALS
B
Figure 10-15B. Periarterial lymphatic sheath, spleen. H&E stain, 564; insets
1,727
The central artery, which helps to maintain the lymphatic sheath, continues through
the white pulp and branches before supplying the marginal sinuses (capillaries). Its
distal branches supply the red pulp. The central artery carries lymphocytes into
the marginal sinuses in the marginal zone, where B cells encounter antigens. Naive
B cells become memory B cells and plasma cells, which produce antibodies. T cells
migrate to the central artery region and form multiple layers that surround that
artery to form the PALS. T cells interact with antigen-presenting cells (inset shows a
macrophage) and receive antigens. Active T cells undergo proliferation to increase
their population (Fig. 10-5A).
Figure 10-15A. Splenic circulation.
The splenic artery enters the spleen at the hilum and
branches into trabecular arteries, which follow the
trabeculae into the white pulp where they become the cen-
tral artery. Lymphatic tissue that immediately surrounds
the central artery is called the PALS. The central artery
passes through the white pulp and gives rise to two routes
of capillaries: (1) those which supply sinuses (marginal
sinuses) around the lymphatic nodule; (2) those which
supply sinuses in the red pulp. The central artery leaves
the white pulp and forms several penicillar arterioles (not
surrounded by PALS). The branches of the penicillar arte-
rioles are called terminal arterial capillaries, which either
give rise directly to the splenic sinuses (closed circulation)
or terminate as open-ended vessels within the splenic
cord of the red pulp (open circulation). Open circula-
tion allows blood passing through the splenic cord to be
fi ltered by macrophages before the blood cells enter the
sinuses. The aggregation of the macrophages surround-
ing the terminal arterial capillaries is called the sheath of
macrophages or the Schweigger-Seidel sheath.
Open
circulation
Pulp
vein
Sheath of
macrophages
Macrophage
Splenic
cord
Splenic
sinuses
Penicillar
arterioles
Closed
circulation
Central
artery
Marginal
sinuses
Splenic nodule
Trabecular
artery and vein
Germinal
center
PALS
A
CUI_Chap10.indd 196 6/2/2010 4:12:21 PM

CHAPTER 10
■
Lymphoid System
197
Figure 10-16. Red pulp of the spleen. TEM, 7,100.
Part of the wall and lumen of a red pulp sinusoid is shown here along with some adjacent red pulp cord (cord of Billroth) on the left.
The plane of section through the sinusoid appears to be transverse to its long axis as indicated by the varying shapes and sizes of the
many profi les of endothelial cells that make up this part of its wall. These cells have a fusiform three-dimensional shape, and their
long axis parallels that of the vessel. A few endothelial cells are cut through the nucleus, but many more show only small profi les of
cytoplasm. The basement membrane of the endothelium is incomplete, and only a couple of pieces are visible here. In life, the formed
elements of blood squeeze between endothelial cells to move into and out of the red pulp cords. Macrophages, plasma cells, and all
types of blood cells and platelets are suspended in the reticular framework of the red pulp cord tissue.
Plasma cell
Plasma cell
Sinusoid
Sinusoid
lumen
lumen
Plasma cell
Sinusoid
lumen
Endothelial cells
Basement
membrane
Erythrocyte
Platelet
Macrophage
Macrophage
Macrophage
Lymphocyte
Lymphocyte
Lymphocyte
CUI_Chap10.indd 197 6/2/2010 4:12:27 PM
198
UNIT 3
■
Organ Systems
Organ Epithelium/
Capsule
Covering
Cortex and
Medulla
Cords and
Sinuses
B-cell Main
Region
T-cell Main
Region
Special Features (1)
and Functions (2)
Tonsils Incomplete
epithelium
and capsule
No No Primary and
secondary nodules
Outside of
the lymphatic
nodules
1. Epithelial covering
2. Promotes B cells to
proliferate and to
produce IgA; immune
defense against upper
respiratory infections,
where B and T cells
encounter foreign
antigens and initiate
immune response
Lymph
nodes
Capsule
(thin)
Cortex, paracortex,
and medulla
Medullary
cords and
medullary
sinuses
Primary and
secondary nodules
(most nodules
are secondary);
medullary cords
Paracortex 1. Afferent lymphatic
vessels and
subcapsular sinuses
2. Filter lymph and
recirculate both B
and T cells; provide
place for lymphocytes
to meet antigens and
start immune response
Thymus Capsule
(thin)
Cortex (without
lymphatic nodules);
medulla (with
Hassall corpuscles)
No No Cortex and
medulla
1. Epithelial reticular
cells and Hassall
corpuscles; no
lymphatic nodules
2. Development and
maturation of T cells
Spleen Capsule
(thick)
No, arranged in
white pulp and red
pulp
Splenic cords
and venous
sinuses
Secondary nodules
(splenic nodules)
PALS 1. Central arteries and
PALS
2. Red pulp fi lters
blood, removes aged
erythrocytes, and
acts as a reservoir
for erythrocytes and
platelets; the white
pulp hosts B and T
lymphocytes, where
they meet antigens,
mature and prolif-
erate, and initiate
immune response
TABLE 10-2 Lymphoid Organs
SYNOPSIS 10-3 Pathological and Clinical Terms for the Lymphoid System
Lymphadenopathy ■ : Enlarged lymph nodes due to a variety of causes including lymphoma, infection, autoimmune disease,
medications, and metastatic disease (Fig. 10-9C).
Myalgia
■ : Muscle pain that may be caused by a variety of conditions including exercise, autoimmune disease, medications,
infections, and neoplasms (Fig. 10-9C).
Lymphoid hyperplasia
■ : A reactive proliferative process of lymphoid tissues, particularly lymph nodes, characterized by
enlarged follicles with abundant macrophages within the germinal center (Fig. 10-9C).
Reed-Sternberg cell
■ : Characteristic cell of classical Hodgkin lymphoma containing two nuclei or nuclear lobes, each with
a prominent nucleolus (Fig. 10-12C).
Waldeyer ring
■ : Lymphoid tissues of the nasopharynx including the palatine tonsils and pharyngeal tonsils (adenoids) that
may be an extranodal site of lymphoma development (Fig. 10-9B).
CUI_Chap10.indd 198 6/2/2010 4:12:30 PM
199
11
Respiratory System
Introduction and Key Concepts for the Respiratory System
Figure 11-1 Overview of the Respiratory System
Figure 11-2 Orientation of Detailed Respiratory System Illustrations
Conducting Portion
Upper Respiratory Airway
Figure 11-3A Nasal Vestibule, Nose
Figure 11-3B,C Nasal Mucosa, Nose
Figure 11-4A,B Olfactory Mucosa, Nose
Figure 11-5A,B Epiglottis, Larynx
Figure 11-5C Clinical Correlation: Age Impact on the Epiglottis
Lower Respiratory Airway
Figure 11-6A,B Trachea
Figure 11-6C Trachealis Muscle, Trachea
Figure 11-7A,B Respiratory Epithelium
Figure 11-8A,B Secondary Bronchi
Figure 11-8C Tertiary Bronchus
Figure 11-9 Overview of the Bronchioles and Alveoli
Figure 11-10A,B Bronchioles, Lung
Figure 11-10C Clinical Correlation: Small Cell Neuroendocrine Carcinoma
Figure 11-11A Clara Cells, Terminal Bronchioles
Figure 11-11B Terminal Bronchiole, Lung
Respiratory Portion
Figure 11-11C Respiratory Bronchioles, Lung
Alveolar Ducts and Alveoli
Figure 11-12A Alveolus and Gas Exchange
Figure 11-12B Blood-Air Barrier
CUI_Chap11.indd 199 6/16/2010 7:34:38 PM
200
UNIT 3
■
Organ Systems
Figure 11-13A,B Type I Pneumocytes
Figure 11-14A,B Type II Pneumocytes
Figure 11-15A,B Alveolar Macrophages
Figure 11-16A Clinical Correlation: Acute Respiratory Distress Syndrome
Figure 11-16B Clinical Correlation: Emphysema
Synopsis 11-1 Pathological and Clinical Terms for the Respiratory System
Table 11-1 Respiratory System
Synopsis 11-2 Structural Differences (from Upper to Lower Airway) in the Respiratory System
Introduction and Key Concepts
for the Respiratory System
The primary function of the respiratory system is to supply the
body’s need for oxygen and to give off carbon dioxide. Other
functions include maintaining homeostasis and a normal pH
and participating in the body’s immune defense against bacte-
rial and viral infections. Anatomically, the respiratory system
can be divided into an upper respiratory airway and a lower
respiratory airway. Functionally, the respiratory system can
be divided into a conducting portion for the transportation
of gases and a respiratory portion for gas exchange. The con-
ducting portion includes the upper respiratory airway and the
lower respiratory airway. These conducting airways include
the nasal cavity, pharynx, larynx, trachea, extrapulmonary and
intrapulmonary bronchi, bronchioles, and terminal bronchi-
oles. The respiratory portion includes the respiratory bronchi-
oles, alveolar ducts, alveolar sacs, and alveoli. The respiratory
muscles (skeletal muscles: external intercostal muscle and the
diaphragm) play an important role in producing the movement
of air into and out of the lungs. The sympathetic and para-
sympathetic nervous systems innervate the smooth muscle of
the bronchial tree as well as the mucous membranes and blood
vessels in the lungs. Sympathetic fi bers cause bronchodilation
(relaxation of bronchial smooth muscles), whereas parasym-
pathetic fi bers cause bronchoconstriction (contraction of bron-
chial smooth muscles).
Conducting Portion
Upper Respiratory Airway
The upper respiratory airway functions as a part of the con-
ducting portion; it consists of the nasal cavity, nasopharynx,
oropharynx, and larynx. In general, the conducting airway is
composed of bone, cartilage, and fi brous tissue and is lined
with stratifi ed squamous and ciliated pseudostratifi ed columnar
epithelia moistened with mucus and other glandular secretions.
Cilia on the surface of the pseudostratifi ed columnar epithelia
sweep particles out of the respiratory airway.
THE NASAL CAVITY is the fi rst portion of the upper respira-
tory airway. It can be divided into three regions based on the
types of epithelial coverings. (1) The nasal vestibule is the most
anterior part of the nasal cavity and is covered by a keratinized
stratifi ed squamous epithelium and vibrissae (stiff hairs); it is
continuous with a mucosa of nonkeratinized stratifi ed squamous
epithelium (Fig. 11-3A). (2) The nasal mucosa region is covered
by pseudostratifi ed ciliated epithelium (respiratory epithelium),
which contains ciliated columnar cells, goblet cells, basal cells,
and, occasionally, neuroendocrine cells (Figs. 11-3B and 11-7).
The goblet cells manufacture mucus, which traps particles
of dust and bacteria and moves them out of the nasal fossa,
sinuses, and the nasopharynx, with the help of the ciliary action
of the epithelium. Nasal mucosa fi lters, warms, and moistens
the inhaled air. Mucus serves as a protective mechanism for pre-
venting pathogens and irritants from entering the respiratory
airway (Fig. 11-3B,C). There is a special vascular arrangement
in the lamina propria of the nasal conchae called swell bodies
(venous plexuses), which alternately fi ll with blood from the
small arteries directly into the venous plexuses on each side of
the nasal cavity to help reduce air fl ow and increase air contact
with nasal mucosa. (3) The olfactory mucosa region is located
in the roof of the nasal cavity and is covered by pseudostratifi ed
columnar epithelium, which is composed of ciliated olfactory
cells (olfactory receptor neurons), nonciliated columnar cells,
and basal cells. It functions as a site for odorant chemorecep-
tion (Fig. 11-4A,B).
THE NASOPHARYNX AND OROPHARYNX conduct
air from the nasal cavity and oral cavity to the larynx. The
oropharynx is lined by stratifi ed squamous epithelium, and the
nasopharynx is lined by respiratory (pseudostratifi ed columnar)
epithelium (see Table 11-1). The nasopharynx contains sero-
mucous glands in the lamina propria. The pharyngeal tonsil, an
unencapsulated patch of lymphoid tissue, is located in the pos-
terior aspect of the nasopharynx (see Fig. 10-8A). The palatine
tonsils are located at the junction of the oral cavity and the oral
pharynx, between the palatoglossal and the palatopharyngeal
folds, which indicate the posterior boundary of the oral cavity
(see Fig. 10-8B). Tonsils, rich in lymphoid tissue, are the fi rst
line of defense against many airborne pathogens and irritants.
Streptococcal pharyngitis is the most frequent bacterial upper
respiratory infection in children.
THE LARYNX conducts air from the pharynx to the trachea.
It is supported by a set of cartilages of complex shape and cov-
ered by a ciliated, pseudostratifi ed respiratory epithelium. This
mucosa continues from that of the pharynx and extends to the
trachea. The larynx contains several structures, including the
epiglottis, vocal cords, and nine pieces of cartilage located in its
wall. The epiglottis is a thin leafl ike plate structure; its central
cord contains a large piece of elastic cartilage. This cartilage is
attached to the root of the tongue and projects obliquely upward
behind the tongue and the hyoid body. The epiglottis stands in
front of the laryngeal inlet and bends posteriorly to cover the
inlet of the larynx when food is swallowed. The upper anterior
CUI_Chap11.indd 200 6/16/2010 7:34:42 PM
CHAPTER 11
■
Respiratory System
201
surface of the epiglottis is covered by nonkeratinized stratifi ed
squamous epithelium. In children, the epiglottis will occasion-
ally become infected with Haemophilus. In elderly individu-
als, the elastic cartilage of the epiglottis is often reduced in size
and is replaced by adipose tissue (Fig. 11-5C). The vocal cords
(folds), which contain striated skeletal muscle and ligaments
(mainly elastic fi bers), are lined by thin nonkeratinized stratifi ed
squamous epithelium, which is fi rmly attached to the underlying
vocal ligaments. The stratifi ed squamous epithelium protects the
vocal cords from mechanical stress. The main functions of the
vocal cords are to control airfl ow and facilitate speaking.
Lower Respiratory Airway
The lower respiratory airway includes the trachea, bronchi,
bronchioles, and terminal bronchioles. Each portion of the
lower respiratory airway has unique tissue components, which
facilitate oxygen delivery, gas exchange, and immune defense
mechanisms. Individual airways decrease in diameter as they
continue branching.
THE TRACHEA is a tube formed of cartilage and fi bromus-
cular membrane, 10 to 12 cm long, with a diameter of 2 to
2.5 cm. It extends from the larynx, at the cricoid cartilage, to
the bifurcation of the bronchi. The trachea is lined by pseu-
dostratifi ed ciliated columnar epithelium and reinforced by 10
to 12 C-shaped hyaline cartilage rings (Fig. 11-6). A band of
smooth muscle is located between the two ends of the C-shaped
cartilage. The epithelium is composed of several cell types
including goblet cells, ciliated columnar cells, basal cells, and,
occasionally, neuroendocrine cells, which are also called dif-
fuse neuroendocrine system (DNES) cells (Fig. 11-7A). Chronic
irritation of the epithelium will lead to an increase in goblet
cells and a transformation to a stratifi ed squamous epithelium,
known as squamous metaplasia.
EXTRAPULMONARY BRONCHI are the primary bronchi,
which begin at the bifurcation of the trachea and lead to the
right and left lungs. They are called “extrapulmonary” bronchi
because they are positioned outside the lungs. They are structur-
ally similar to the trachea, are lined by respiratory epithelium
(pseudostratifi ed columnar epithelium), and have C-shaped
hyaline cartilage. The left primary bronchus is narrower and
less vertical than the right one and gives rise to two second-
ary (lobar) bronchi. The right primary bronchus is wider and
shorter and more vertical than the left one; it gives rise to three
secondary (lobar) bronchi. That is the reason foreign body aspi-
ration occurs more often to the right lung.
INTRAPULMONARY BRONCHI are secondary and tertiary
bronchi. As the primary (extrapulmonary) bronchi enter the
hiluses of the lungs they become the secondary (lobar) bronchi,
which eventually divide into the tertiary (segmental) bronchi
(Figs. 11-1 and 11-8C). They are lined by respiratory epithe-
lium, and the bronchial glands (seromucous glands) are found
in the submucosa. A band of spiral smooth muscle separates
the lamina propria and submucosa of the intrapulmonary bron-
chi. The skeletal support for each intrapulmonary bronchus is
provided by several hyaline cartilage plates instead of C-shaped
cartilage rings. As the bronchi continue branching, there is a
decrease in airway diameter and in the amount of cartilage in
their walls. The number of goblet cells, glands, and the height
of epithelial cells also decrease. However, the airways tend to
have increased amounts of smooth muscle and elastic tissues.
Smooth muscle in the bronchi is innervated by the sympathetic
and parasympathetic nervous systems. In patients with asthma,
this smooth muscle thickens with hyperplasia and hypertrophy
and undergoes extensive and prolonged contraction causing
reduction in airway luminal diameter and diffi culty in exhaling
and inhaling. Bronchial branches are accompanied by branches
of the pulmonary arteries, pulmonary veins, nerves, and lymph
vessels. These structures usually travel in intersegmental and
interlobar layers of connective tissue.
BRONCHIOLES are smaller airways deriving from tertiary
bronchi, which continue to branch into terminal bronchioles
(Fig. 11-9). Bronchioles have no cartilage in their walls. Large
bronchioles are lined with ciliated columnar epithelial cells and
a gradually decreasing number of goblet cells. Small bronchioles
are covered with ciliated cuboidal epithelial cells and with Clara
cells. The number of Clara cells is greatly increased in the ter-
minal bronchioles (Fig. 11-11A). Terminal bronchioles are the
smallest and last of the conducting portion of the respiratory
system and they have no gas exchange function. Terminal bron-
chioles give rise to respiratory bronchioles, which connect to the
alveolar ducts, alveolar sacs, and alveoli (Fig. 11-11A,B).
Respiratory Portion
The respiratory portion of the lungs includes the respiratory
bronchioles, alveolar ducts, alveolar sacs, and alveoli. This por-
tion of the respiratory system does not have cartilage and has
gradually increasing numbers of alveoli.
Respiratory Bronchioles
Respiratory bronchioles are lined by cuboidal epithelium and
are interrupted by pouchlike, thin-walled structures called alve-
oli. Alveoli function in gas exchange. Respiratory bronchioles
continue to branch to become alveolar ducts (Figs. 11-9 and
11-11C).
Alveolar Ducts and Alveoli
Alveolar ducts arise from respiratory bronchioles. They have
more alveoli and some cuboidal epithelium on the walls as
compared to respiratory bronchioles. They terminate as blind
pouches with clusters of alveolar sacs. An alveolar sac is com-
posed of two or more alveoli that share a common opening.
Alveolar ducts and alveoli are rich in capillaries, which make
gas exchange more effi cient. Alveoli are thin-walled pouches,
which provide the respiratory surface area for gas exchange
(Figs. 11-9 and 11-11C). The wall of the alveolus is formed by
a delicate layer of connective tissue with reticular and elastic
fi bers covered by type I and type II pneumocytes. The type I
pneumocytes lie on a basal lamina, which is fused with the basal
lamina surrounding the adjacent capillaries to form a blood-
CUI_Chap11.indd 201 6/16/2010 7:34:42 PM
202
UNIT 3
■
Organ Systems
air barrier. The blood-air barrier is an important structure for
oxygen and carbon dioxide exchange (Fig. 11-12A,B). The
neighboring alveoli are separated by alveolar septa, which con-
tain elastic connective tissue and may have capillaries within
them. The lumina of the neighboring alveoli may be connected
to each other by small alveolar pores.
TYPE I PNEUMOCYTES are also called type I alveolar cells.
These cells cover 95% to 97% of the alveolar surface, whereas
type II pneumocytes cover the rest of the surface. Type I pneu-
mocytes are squamous cells with a fl at, dark, oval nucleus.
Tight junctions between type I pneumocytes help prevent move-
ment of extracellular fl uid into the alveolar sacs. Type I pneu-
mocytes are unable to divide; however, they can be regenerated
from type II pneumocytes (Fig. 11-13A,B).
TYPE II PNEUMOCYTES cover about 3% to 5% of the alve-
olar surface and form tight junctions with type I pneumocytes.
Their cytoplasm contains numerous characteristic secretory
lamellar bodies, which are mainly composed of phospholipids
and proteins. These components can be released by exocytosis
into the alveolar lumen to form a thin fi lm of pulmonary sur-
factant. The function of the pulmonary surfactant is to increase
pulmonary compliance and decrease surface tension of the alve-
oli to prevent them from collapsing. Type II pneumocytes can
undergo mitosis to regenerate and also can form type I pneumo-
cytes. The pulmonary surfactant is recycled by type II pneumo-
cytes or cleared by alveolar macrophages (Fig. 11-14A,B).
ALVEOLAR MACROPHAGES are also called dust cells. They
originate in bone marrow and circulate in blood as monocytes.
They become mature and migrate into the connective tissue of
the alveolar septa and into the lumina of the alveoli from blood
capillaries. They move around on the epithelial surfaces and
help to clear particles, as well as excessive surfactant, out of the
respiratory spaces (Fig. 11-15A,B).
CUI_Chap11.indd 202 6/16/2010 7:34:42 PM
CHAPTER 11
■
Respiratory System
203
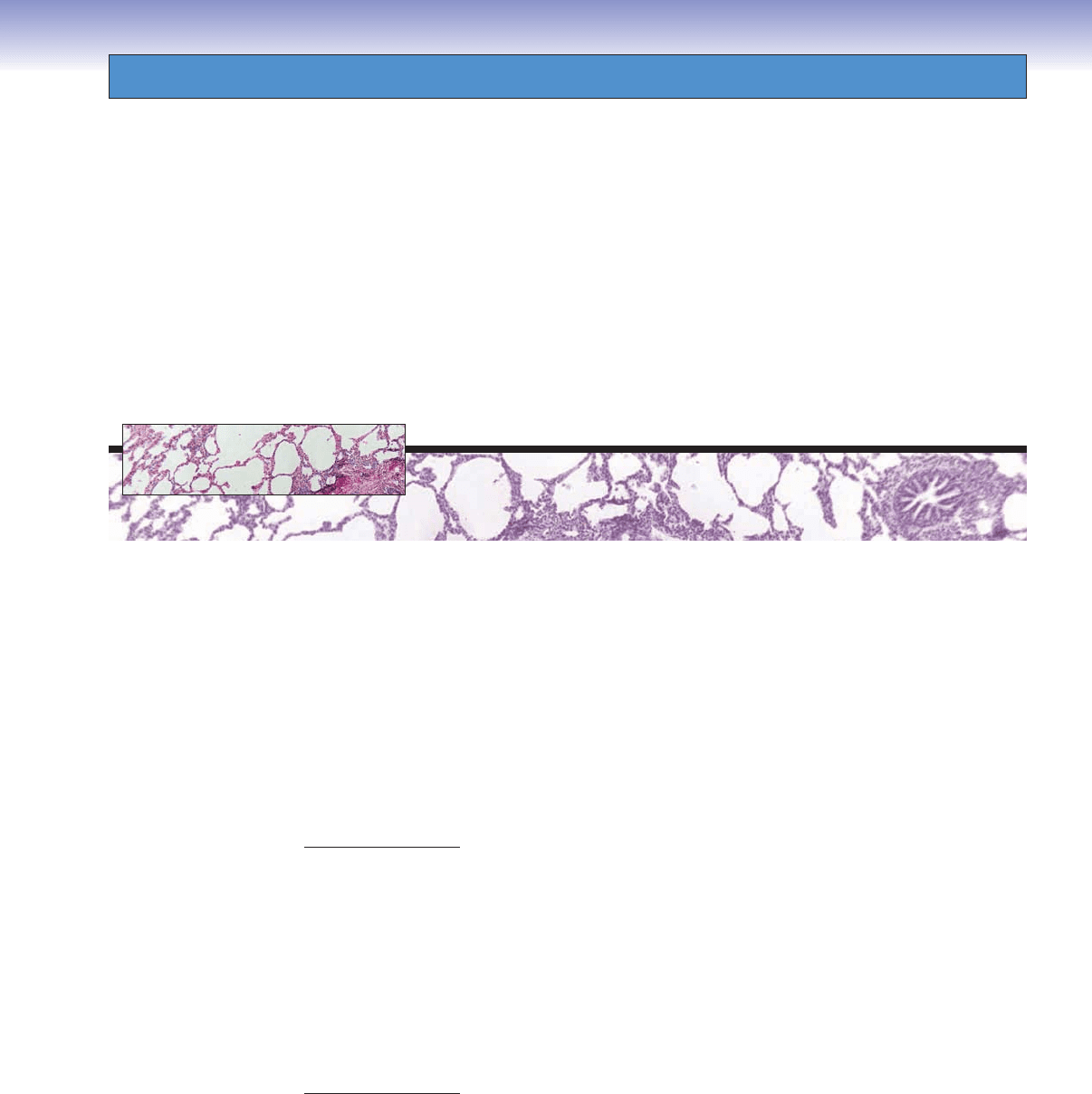
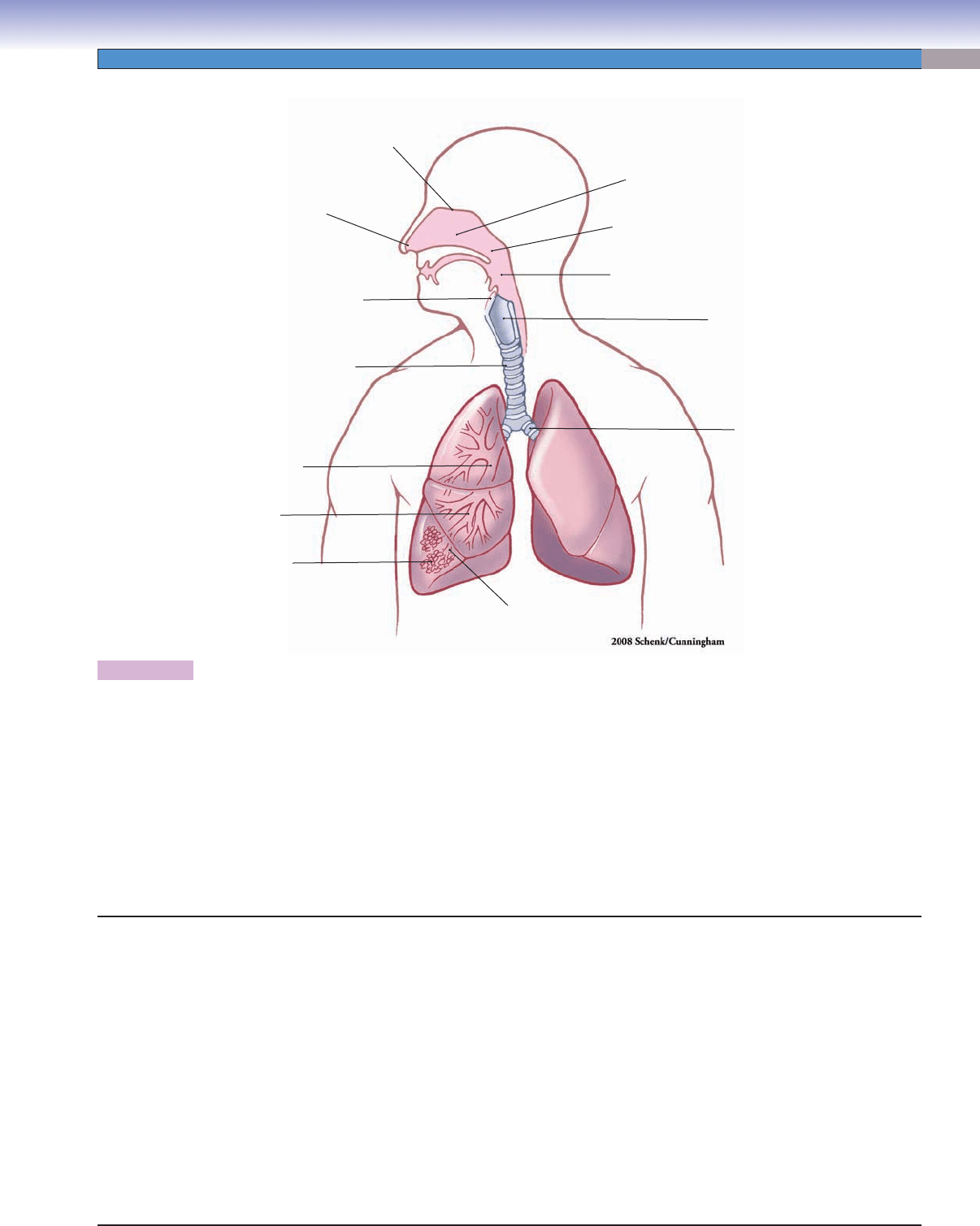
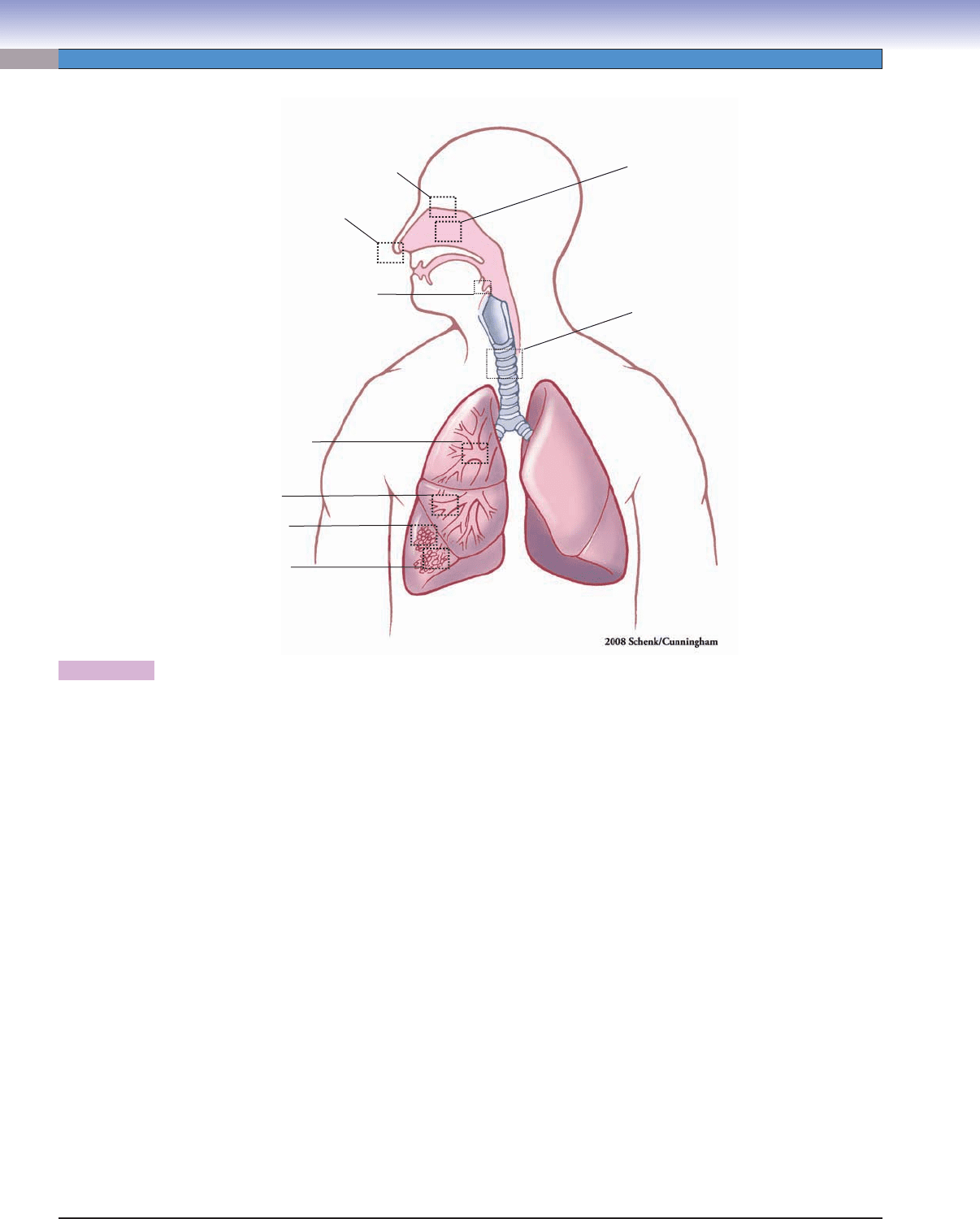
Figure 11-1. Overview of the respiratory system.
The respiratory system plays the essential role of supplying oxygen to the body. It can be divided into the upper respiratory airway
and lower respiratory airway; functionally, the respiratory system can also be divided into a conducting portion and respiratory por-
tion. Upper respiratory airway infection is a common term in clinical diagnosis. The upper respiratory airway consists of the nasal
cavity, nasopharynx, oropharynx, and larynx. There are three regions in the nasal cavity classifi ed according to types of epithelial
covering: the nasal vestibule (stratifi ed squamous epithelium), the nasal mucosa (ciliated pseudostratifi ed columnar epithelium), and
the olfactory mucosa (specialized olfactory epithelium). The nasopharynx is continuous with the oropharynx and extends to the
larynx. The larynx is composed of the epiglottis, vocal cords (folds), and a set of cartilages of complex shape. The lower respiratory
airway consists of the trachea, bronchi, bronchioles, and alveoli in the lungs. The skeletal support changes from C-shaped hyaline
cartilage in the trachea and primary bronchi to cartilage plates in secondary and tertiary bronchi. Bronchioles have no cartilage
support. Terminal bronchioles give rise to respiratory bronchioles. which have the function of gas exchange along with the alveoli
(see Fig. 11-9).
Structures of the Respiratory System
I. Conducting portion
A. Upper respiratory airway
1. Nasal cavity
a. Nasal vestibule
b. Nasal mucosa
c. Olfactory mucosa
2. Nasopharynx
3. Oropharynx
4. Larynx
a. Epiglottis
b. Vocal cords (folds)
B. Lower respiratory airway
1. Trachea
2. Extrapulmonary bronchi (primary bronchi)
3. Intrapulmonary bronchi
a. Secondary bronchi
b. Tertiary (segmental) bronchi
c. Bronchioles
d. Terminal bronchioles
II. Respiratory portion
A. Respiratory bronchiole (respiratory portion begins)
B. Alveolar ducts and alveoli
C. Type I and II pneumocytes
D. Alveolar macrophages
Vestibule
Bronchioles
Nasal mucosa
Nasopharynx
Oropharynx
Extrapulmonary
(primary) bronchus
Larynx
Intrapulmonary
(secondary) bronchus
Intrapulmonary
(tertiary) bronchus
Alveoli
Epiglottis
Trachea
Olfactory
mucosa
CUI_Chap11.indd 203 6/16/2010 7:34:42 PM
204
UNIT 3
■
Organ Systems
Figure 11-2. Orientation of detailed respiratory system illustrations.
Fig. 11-6A,B,C
Fig. 11-7A,B
Fig. 11-3A
Fig. 11-5A,B,C
Fig. 11-4A,B
Fig. 11-3B,C
Fig. 11-8A,B
Fig. 11-8C
Fig. 11-9
Fig. 11-10A to
Fig. 11-15B
Structures of the Respiratory System with Figure Numbers
Nasal vestibule
Figure 11-3A
Nasal mucosa
Figure 11-3B
Figure 11-3C
Olfactory mucosa
Figure 11-4A
Figure 11-4B
Epiglottis
Figure 11-5A
Figure 11-5B
Figure 11-5C
Trachea
Figure 11-6A
Figure 11-6B
Figure 11-6C
Figure 11-7A
Figure 11-7B
Bronchi
Figure 11-8A
Figure 11-8B
Figure 11-8C
Overview of bronchioles and alveoli
Figure 11-9
Bronchioles
Figure 11-10A
Figure 11-10B
Figure 11-10C
Figure 11-11A
Figure 11-11B
Figure 11-11C
Alveoli, type I and II pneumocytes, and macrophages
Figure 11-12A
Figure 11-12B
Figure 11-13A
Figure 11-13B
Figure 11-14A
Figure 11-14B
Figure 11-15A
Figure 11-15B
Figure 11-16A
Figure 11-16B
CUI_Chap11.indd 204 6/16/2010 7:34:43 PM
