Caballero B. (ed.) Encyclopaedia of Food Science, Food Technology and Nutrition. Ten-Volume Set
Подождите немного. Документ загружается.


consumption, and there is no evidence that if such
food is primarily contaminated, illness ensues. How-
ever uncooked soft fruits such as strawberries and
raspberries have been implicated in a number of out-
breaks when contamination is assumed to have oc-
curred at the growing site. Salad items are commonly
implicated in outbreaks, although in many of these
incidents, contamination is believed to have origin-
ated from infected food handlers at the time of prep-
aration.
Secondary Contamination: Food Handlers
0026 Viruses causing gastroenteritis and hepatitis A are
infectious in very low doses, and thus are spread
very readily from infected persons. It is now recog-
nized that outbreaks arising from infected food hand-
lers are common occurrences. The foods that pose the
greatest risk to the consumer are cold items, such as
sandwiches and salads, that require much handling
during preparation. Without meticulous attention to
personal hygiene and thorough and frequent hand
washing, fecally contaminated fingers can contamin-
ate foods and work surfaces. Viral gastroenteritis can
be very sudden in onset and commence with projectile
vomiting. The virus can be disseminated over a wide
area in aerosol droplets so that, in food preparation
areas, exposed foods, working surfaces, and door
handles are likely to be contaminated.
Virus Survival
0027 Gastroenteritis viruses and hepatitis viruses are
robust viruses and survive extremely well in the en-
vironment. It is the NLVs and HAV that are the most
resistant to inactivation. There is little precise infor-
mation on the stability of NLVs, since they cannot be
cultured in the laboratory. Most information on sur-
vival and inactivation has come from epidemiological
observations in outbreaks and limited studies of infec-
tivity in volunteers. Some strains of HAV and rota-
virus can be cultured, and there have been a small
number of experimental studies on their stability.
Gastroenteritis and hepatitis viruses have been
detected in food, water, and other environmental
samples by PCR assays, but such assays only detect
the viral genome and do not necessarily correlate with
infectivity.
0028 Viruses that infect via the gastrointestinal tract are
acid-stable. Both NLVs and HAV retain infectivity
after exposure to acidity levels below pH 3. Hence,
they are often able to survive the food-processing and
preservation conditions used to inhibit bacterial and
fungal spoilage of foods, such as pickling in vinegar
and fermentation processes to produce foods such as
yogurt. Alcohol and high sugar concentrations are
unlikely to have any adverse effect on survival. Re-
frigeration and freezing are routinely used to preserve
viruses and have no effect on viability. Frozen foods
that are not subsequently cooked, such as soft fruits,
have been implicated in a number of incidents of both
viral gastroenteritis and hepatitis A.
0029The viruses are destroyed by normal cooking pro-
cesses. For foods that only undergo partial cooking in
special heat processes, such as the treatment of shell-
fish and other pasteurization procedures, care must
be taken to ensure that inactivation of virus is
achieved. Both NLVs and HAV retain infectivity
after heating to 60
C for 30 min.
0030Gastroenteritis viruses and hepatitis viruses appear
to survive in the environment for long periods. They
survive on inanimate surfaces, on hands and in dried
fecal suspensions. Lingering outbreaks have occurred
in hospitals, residential homes and on cruise ships,
probably as a result of environmental contamination.
NLVs have been detected by PCR in swabs from
hospital lockers and hotel carpets supposedly cleaned
after incidents of vomiting.
0031There is conflicting evidence on the efficacy of
disinfectants. Chlorine-based disinfectants are usu-
ally considered the most effective against enteric vir-
uses and the most suitable in food preparation areas.
However, NLVs and HAV are resistant to a level of
0.5–1 mg per liter of free residual chlorine, which is
consistent with that present in drinking water. NLVs
are inactivated by 10 mg per liter of chlorine. In the
USA, a level of 5 mg per liter of chlorine with a
contact time of 1 min is recommended for inactiva-
tion of HAV. Infectivity of HAV is reduced by sodium
hypochlorite, 2% glutaraldehyde, and quarternary
ammonium compounds, but there are no compara-
tive data for NLVs.
Virus Detection
In Food
0032It is not feasible to examine food samples routinely
for the presence of viruses. Although it has been
possible to culture HAV since 1980, primary isolation
is a lengthy and unreliable procedure, and there have
been very few isolations of virus from food or water
samples. Virus was isolated from a drinking water
supply responsible for a large outbreak in the USA,
but this involved culture of highly concentrated water
samples for up to 21 weeks. There have been several
studies involving recovery of virus from artificially
contaminated foods, particularly shellfish, but these
have used highly adapted laboratory strains of virus.
Viruses stick avidly to shellfish meat, and complex
extraction techniques are required. Even with the best
6008 VIRUSES

of these methods, virus recovery rates are poor. NLVs
cannot be cultured in the laboratory. Culture of rota-
viruses and astroviruses is complex and unreliable,
and the problems of avidity similarly apply. Rapid
solid-phase immunoassays are available for the detec-
tion of hepatitis and gastroenteritis viruses. These are
not sufficiently sensitive, however, to detect the very
small numbers of virus particles likely to be present in
contaminated foods. Similarly, electron microscopy is
insufficiently sensitive for the detection of virus in
food samples.
0033 There is considerable interest in the application of
PCR assays to the detection of viruses in food and
water samples. PCR is an extremely sensitive tech-
nique. However, extraction of viral RNA from
samples and removal of PCR inhibitors is a fairly
complex and time-consuming procedure. Hence,
such assays cannot be used for routinely screening
food samples. Furthermore, unlike culture, a positive
PCR result only indicates the presence of viral nucleic
acid and does not necessarily confirm the presence of
viable infectious virus. These tests do have an import-
ant role in the epidemiological investigation of out-
breaks and assessing the efficacy of treatment
procedures.
In Patients
0034 HAV is excreted in feces, but it is not usually appro-
priate to examine fecal specimens for virus as the
main excretion period precedes illness. The usual
diagnostic test is detection of anti-HAV specific im-
munoglobulin M (IgM) antibody in serum, for which
there are a number of commercially available solid-
phase immunoassays. The presence of IgM antibody
is indicative of recent infection. If the fecal specimens
are collected at the appropriate time, it is quite feas-
ible to detect viral antigen by various techniques, the
most rapid and straightforward being the solid-phase
immunoassays and PCR tests.
0035 All the gastroenteritis viruses were discovered by
electron microscopy, and this has continued to play
an important role in diagnosis. Viruses from different
groups look different, and it is this characteristic
morphology that is the basis for their identification.
However, electron microscopy is a time-consuming
technique that demands considerable skill and ex-
perience on the part of the operator, and it is not
a technique that lends itself to examining large
numbers of specimens. PCR assays are being used
increasingly for the detection of NLVs, but their use
is mainly confined to specialist virology laboratories.
Although of far greater sensitivity than electron mi-
croscopy, current primers will not detect all strains of
NLVs. Recombinant capsid antigens have been made
from a small number of NLV strains and have been
used to develop ELISA tests. So far, only a very few
NLV types can be detected, and the tests are not yet
widely available. Commercial ELISA and latex agglu-
tination test kits are readily available for the detection
of rotaviruses. Astroviruses are usually detected by
electron microscopy. Some laboratories use in-house
PCR assays or culture combined with immunofluor-
escence.
Prevention and Control
0036Elimination of viral contamination at source is an
ideal that is unlikely to be attained in the near future.
In practice, it would be necessary to prevent the dis-
charge of sewage into rivers and coastal waters,
which not only pollutes water supplies that may be
used for irrigation but also results in the contamin-
ation of shellfish. Sewage sludge provides beneficial
nutrients and is applied to agricultural land as fertil-
izer. In developed countries, increasingly stringent
regulations for the use of untreated or partially treated
sewage are being introduced. Since the end of 1999,
application of all untreated sewage sludge on agricul-
tural land has been prohibited in the UK. Where
treated sewage is applied to land for growing salad
and vegetable crops, permitted time intervals, be-
tween applying the sewage and harvesting the crops,
are specified. Hepatitis A is endemic in underdevel-
oped areas of the world and viral gastroenteritis
more prevalent. Viruses commonly occur in polluted
coastal waters in these areas, and contamination of
shellfish is likely. Standards for the use of sewage in
agriculture are also less satisfactory. Imports of fruits,
salads, vegetables and shellfish could potentially pose
a risk to consumers.
0037It is usual practice to treat shellfish in some way to
remove microbial contamination before they are sold
to the public. In the European Union, conditions for
bivalve molluscs are laid down in the European
Council Directive on Shellfish Hygiene (91/492/
ECC), and there are similar regulations in the USA.
Shellfish, such as oysters and mussels, may be
cleansed, either by relaying in cleaner coastal or estu-
arine waters or by transfer to land-based depuration
facilities. Harmful microorganisms should be washed
out during the natural feeding process. These proced-
ures are remarkably successful in removing bacterial
contamination but do not completely eliminate vir-
uses. These may remain for several weeks in molluscs
held in depuration tanks. Even though molluscs
may appear entirely satisfactory in bacteriological
tests, incidents of viral illness may follow their
consumption.
0038Up to the middle of the 1980s, many outbreaks
of viral illness were recorded, related to the
VIRUSES 6009

consumption of inadequately cooked shellfish such as
cockles. Prolonged cooking results in a tough unpal-
atable product, and thus the aim of treatment must be
to apply the minimum heat necessary to render shell-
fish safe. Studies on the inactivation of hepatitis A
virus in shellfish led to recommendations that the
internal temperature of shellfish meat should be
raised to 90
C and maintained for 1.5 min. These
recommendations were adopted by the UK shellfish
industry and subsequently accepted as a valid method
of treatment by the European Commission. Later
studies, using feline calicivirus as a model, indicated
that these conditions were also adequate for inactiva-
tion of the NLVs. Epidemiological evidence strongly
supports the view that this treatment is effective for
the inactivation of gastroenteritis viruses. Since early
1988, there have been no further reports in England
and Wales of any viral illness, either hepatitis A or
gastroenteritis, from shellfish heat-treated according
to the recommendations.
0039 Foods may be contaminated during preparation
and serving by infected food handlers. Both the gas-
troenteritis viruses and hepatitis A virus are extremely
infectious in low doses and thus are spread easily
from infected persons. Persons with symptoms should
be excluded from handling food. However, food
handlers with very minimal symptoms have been im-
plicated in the transmission of NLVs. There is a little
circumstantial evidence that asymptomatic excretion
of virus occurs, but in the absence of more definitive
data, it is generally recommended that people should
be allowed to resume work 48 h after symptoms have
ceased. That recommendation was based on the rapid
decline in virus shedding observed by electron micro-
scopy and in practice appears to work satisfactorily.
However, NLVs often can be detected by PCR for a
longer period than by electron microscopy and, in
some instances, for up to a week after the onset of
symptoms. It is not clear if persons shedding virus
detectable by PCR are infectious after symptoms
have ceased. Recommendations on how long to ex-
clude people from work need to be kept under review.
0040 Excretion of hepatitis A virus precedes symptoms,
and hence, early exclusion of infectious food handlers
is not usually possible. An effective vaccine is avail-
able. Currently, in the UK, hepatitis A vaccine is used
selectively for persons at high risk, such as travelers.
It is not generally used for food handlers except in
outbreak situations. If exposure is known to have
occurred, the use of normal human immunoglobulin
might be considered in persons at risk of developing
illness.
0041 In the kitchen, prevention of transmission of vir-
uses through foods largely depends on rigorous appli-
cation of normal good hygiene practices, including
frequent hand washing and thorough washing of
fruit and vegetables. Shellfish must be regarded as a
potential source of infection, and uncooked shellfish
should be kept separate from other food items that
are not to be cooked. If vomiting occurs, virus may be
spread over a wide area. Uncovered food should be
discarded. Even food that is to be cooked is a poten-
tial source of cross-contamination. Work surfaces,
door handles, and toilet areas should be cleaned thor-
oughly. Chlorine-based disinfectants are considered
the most effective. Handling of food should be kept
to a minimum. Wearing gloves may prevent fecally
contaminated fingers coming into contact with food
but will not prevent transfer of organisms from con-
taminated work surfaces.
See also: Contamination of Food; Food Poisoning:
Statistics; Shellfish: Contamination and Spoilage of
Molluscs and Crustaceans; Zoonoses
Further Reading
Advisory Committee on the Microbiological Safety of Food
(1998) Report on foodborne viral infections. London:
The Stationery Office.
Appleton H (2000) Control of foodborne infections. British
Medical Bulletin 56: 172–183.
Cliver DO (1997) Foodborne viruses. In: Doyle MP, Beu-
chat LR and Montville TJ (eds) Food Microbiology:
Fundamentals and Frontiers, pp. 437–446. Washington,
DC: ASM Press.
Desslberger U (2000) Viruses associated with acute diar-
rhoeal disease. In: Zuckerman AJ, Banatvala JE and
Pattison JR (eds) Principles and Practice in Clinical Vir-
ology, 4th edn., pp. 235–252. Chichester, UK: John
Wiley.
Evans HS, Madden P, Douglas C et al. (1998) General
outbreaks of infectious intestinal disease in England
and Wales: 1995 and 1996. Communicable Disease
and Public Health 1: 165–171.
Food Standards Agency (2000) A report of the study of
infectious intestinal disease in England. London: The
Stationery Office.
Harrison TJ, Dusheiko GM and Zuckerman AJ (2000)
Hepatitis viruses. In: Zuckerman AJ, Banatvala JE and
Pattison JR (eds) Principles and Practice in Clinical Vir-
ology, 4th edn., pp. 187–233. Chichester, UK: John
Wiley.
Hui YH, Sattar SA, Murrell KD, Nip W-K and Stanfield PS
(eds) (2000) Foodborne Disease Handbook, Volume 2:
Viruses, Parasites, Pathogens, and HACCP, 2nd edn.
Chapters 2–9. New York: Marcel Dekker.
Lees D (2000) Viruses and bivalve shellfish. International
Journal of Food Microbiology 56: 81–116.
Millard J, Appleton H and Parry JV (1987) Studies on
heat inactivation of hepatitis A virus with special refer-
ence to shellfish. Epidemiology and Infection 98:
397–414.
6010 VIRUSES
Public Health Laboratory Service Viral Gastroenteritis Sub-
Committee (1993) Outbreaks of gastroenteritis associ-
ated with SRSVs. PHLS Microbiology Digest 10: 2–8.
Seymour IJ and Appleton H (2001) A review: Foodborne
viruses and fresh produce. Journal of Applied Microbiol-
ogy 91: 759–773.
Slomka MJ and Appleton H (1998) Feline calicivirus as a
model system for heat inactivation studies of small
round structured viruses in shellfish. Epidemiology and
Infection 121: 401–407.
Wheeler JG, Sethi D, Cowden JM et al. (1999) Study of
infectious intestinal disease in England: rates in the com-
munity, presenting to general practice, and reported to
national surveillance. British Medical Journal 318:
1046–1050.
Visible Spectroscopy See Spectroscopy: Overview; Infrared and Raman; Near-infrared;
Fluorescence; Atomic Emission and Absorption; Nuclear Magnetic Resonance; Visible Spectroscopy and
Colorimetry
Vitamin A See Retinol: Properties and Determination; Physiology
Vitamin B
1
See Thiamin: Properties and Determination; Physiology
Vitamin B
12
See Cobalamins: Properties and Determination; Physiology
Vitamin B
2
See Riboflavin: Properties and Determination; Physiology
VIRUSES 6011
VITAMIN B
6
Contents
Properties and Determination
Physiology
Properties and Determination
J A Driskell, University of Nebraska, Lincoln, NE, USA
Copyright 2003, Elsevier Science Ltd. All Rights Reserved.
Vitamin B
6
: Properties and Analysis
0001 Vitamin B
6
is a B-complex vitamin. Vitamin B
6
is the
generic descriptor for all 3-hydroxy-2-methylpyridine
derivatives possessing the biological activity of pyrid-
oxine.
0002 Gyu
¨
rgy, in 1934, identified vitamin B
6
as a curative
factor for a characteristic dermatatis in the laboratory
rat. The first naturally occurring form of the vitamin
was isolated in 1938; its structure was confirmed
by chemical synthesis as 3-hydroxy-4,5-bis(hydroxy-
methyl)-2-methylpyridine in 1939. ‘Pyridoxine’ was
the trivial name of this compound, and ‘pyridoxine’
and ‘vitamin B
6
’ were synonyms. Other compounds
having vitamin B
6
activity were detected and isolated.
In the 1960 IUPAC Definitive Rules for the Nomen-
clature of Vitamins, ‘pyridoxine’ was recommended
as the generic descriptor of the B
6
vitamers and ‘pyr-
idoxol’ as the trivial name of the alcohol form of the
vitamin. In the 1966 IUPAC-IUB Tentative Rules, the
suggestion was made that ‘pyridoxol’ should be
designated as ‘pyridoxine.’ In 1968, the IUPAC-IUB
Commission on Biochemical Nomenclature decided
to publish a special document regarding vitamin B
6
nomenclature, which clearly stated that ‘pyridoxine
should not be used as a generic name synonymous
with vitamin B
6
’; this document, published in 1973,
also designated the composition of the six forms of
the vitamin and oxidized metabolites, 4-pyridoxic
acid and 4-pyridoxolactone. However, confusion
still exists in the literature regarding usage of the
term ‘pyridoxine.’
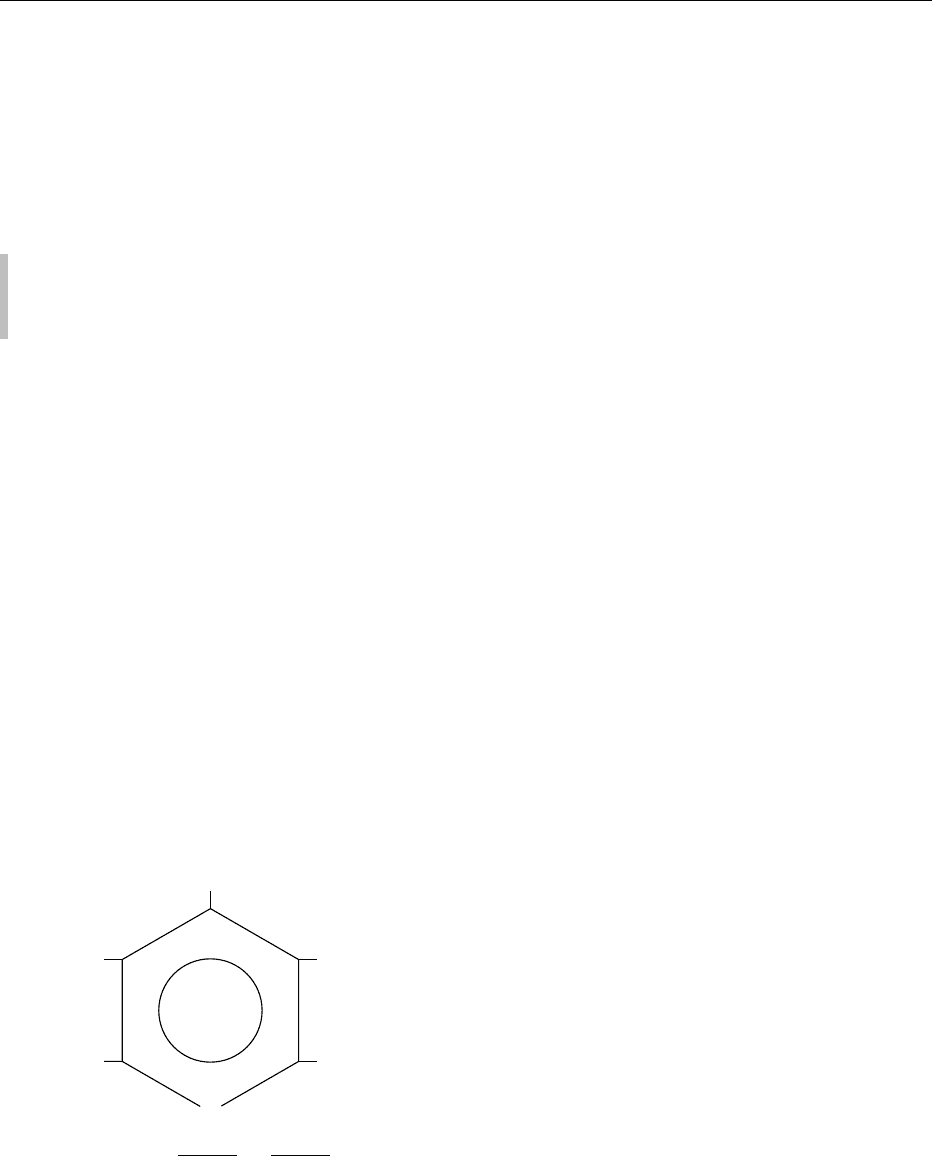
0003The chemical structures of the vitamin B
6
com-
pounds and the accepted ring numbering system are
shown in Figure 1. The vitamin B
6
congeners are
pyridoxine (PN), pyridoxal (PL), and pyridoxamine
(PM) – alcohol, aldehyde, or amine groups are at
the #4 position of the pyridine ring. Each of these
three forms also has a corresponding 5
0
-phosphate
(P), i.e., pyridoxine 5
0
-phosphate (PNP), pyridoxal
5
0
-phosphate (PLP), and pyridoxamine 5
0
-phosphate
(PMP). The various forms of the vitamin are bio-
chemically interconvertible, as shown in Figure 2.
They can also be chemically interconverted. The
major excretory form of the vitamin is 4-pyridoxic
acid (4-PA), which is eliminated in the urine.
Physical and Chemical Properties
0004In general, the various vitamin B
6
compounds are
white crystals that are very soluble in water, slightly
soluble in alcohol, and often insoluble in ether. They
melt, usually with decomposition. Aqueous solutions
of the various vitamin B
6
compounds are relatively
sensitive to light and often are destroyed by heating.
The light sensitivity of the vitamers is affected by pH.
The nonphosphorylated vitamers are relatively stable
to heat at an acidic pH but not at an alkaline pH.
According to Ang, stability values of PNHCl,
PLHCl, and PM2HCl at pH 4.5 to white light
for 8 h are 97, 97, and 81%, respectively, which
decreases with increasing pH. For example PNHCl
stability is 88% pH 7; at PLHCl, 81% at pH 6;
and PM2HCl, 74% at pH 8. Overall, PN is the
most stable, followed by PL and then PM. Greater
H
3
CH
62
N
R
1
4
1
HO
35
CH
2
OR
2
PN
PL
PM
4-PA
CH
2
OH
R
1
CHO
CH
2
NH
2
COOH
H
R
2
H
H
H
PNP PO
3
−
*When -CH
2
O
.
PO
3
, then is PNP, PLP, or PMP.
=
*
fig0001 Figure 1 Stuctural formulae of vitamin B
6
compounds.
6012 VITAMIN B
6
/Properties and Determination
decomposition of the vitamin B
6
compounds is ob-
served with ultraviolet and near-ultraviolet radiation.
Researchers working with this nutrient generally per-
form their analyses in darkened laboratories (red or
yellow lights may be used); in addition, media con-
taining the vitamin are kept at temperatures of 5
C
or less.
0005 The physical properties of the vitamin B
6
com-
pounds are summarized in Table 1. The ultraviolet
absorption spectra of these compounds are dependent
upon the pH because of changes to the electronic
structure. The pyridine ring of the vitamin B
6
com-
pounds is zwitterionic at neutral pH with ionized
phenolate and pyridinium groups. The physical prop-
erties of the B
6
compounds are useful with regard to
detection and quantitation of the vitamin.
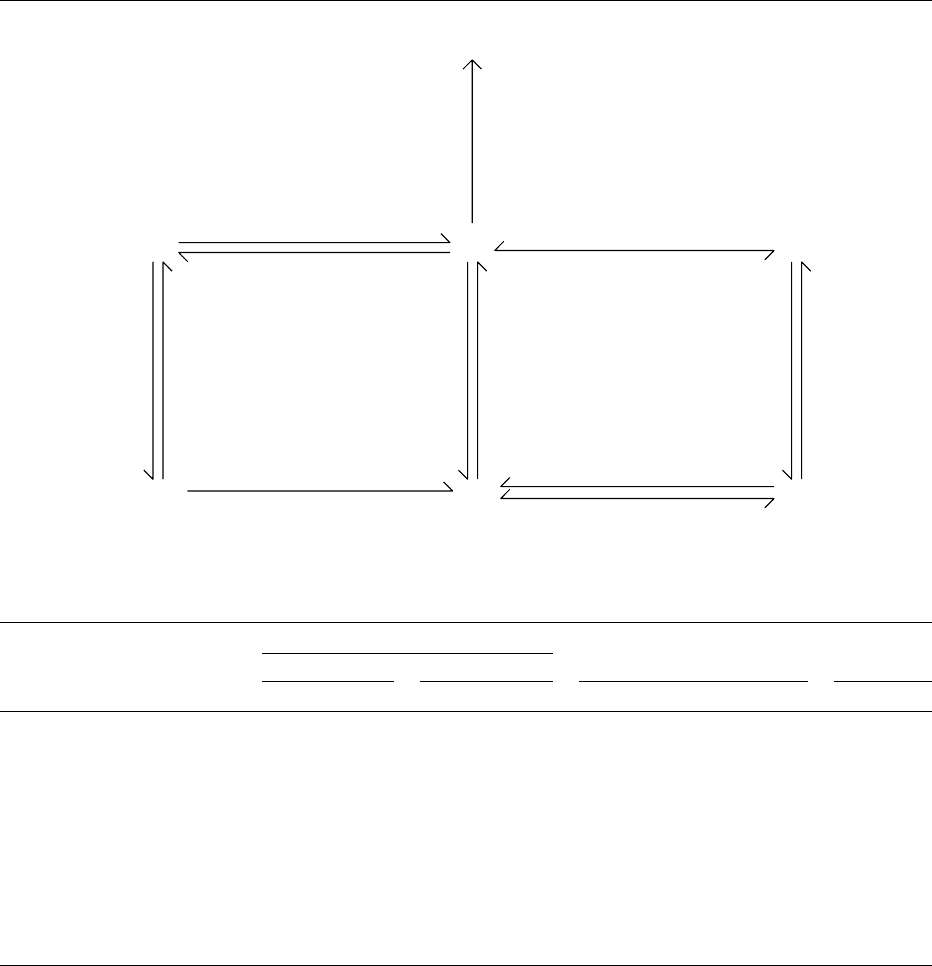
0006As mentioned previously, the various forms of vita-
min B
6
are interconvertible. The various B
6
vitamers
4-PA
Pyridoxine dehydrogenase (NADP)
[EC 1.1.1.65]
Pyridoxaminephosphate oxidase (FMN)
[EC 1.4.3.5]
Pyridoxaminephosphate oxidase (FMN)
[EC 1.4.3.5]
an Aminotransferase (PLP)
an Aminotransferase (PLP)
PM
Phosphatase
(perhaps Zn)
[EC 3.1.3.2]
Phosphatase
(perhaps Zn)
[EC 3.1.3.2]
Phosphatase
(perhaps Zn)
[EC 3.1.3.2]
Pyridoxal
kinase
(ATP, Zn)
Pyridoxal
kinase
(ATP, Zn)
PL
PLP PMP
PN
PNP
Aldehyde oxidase (FAD)
[EC 1.2.3.1]
Aldehyde dehydrogenase (NAD)
[EC 1.2.1.3]
or
[EC 2.7.1.35] [EC 2.7.1.35]
Pyridoxal
kinase
(ATP, Zn)
[EC 2.7.1.35]
fig0002 Figure 2 Interconversions of vitamin B
6
compounds.
tbl0001 Table 1 Physical properties of vitamin B
6
compounds
a
Ultraviolet absorptionspectra
0.1 N HCl pH 7.0 Fluorescence maxima, pH 7 pK
Congener Molecular weight (g) l
max
(nm) e
max
l
max
(nm) e
max
Activation (nm) Emission (nm) pK
1
pK
2
PN 169.1 291 8700 254 3760 325 400 5.0 8.9
PL 167.2 288 9100 390 8800 320 385 4.2 8.7
PM 168.1 293 8500 253 4600 325 405 3.4 8.1
325 7700
PNP 249.2 290 8700 253 3700 322 394 – –
325 7400
PLP 247.2 293 7200 388 5500 330 375 <2.5 4.1
334 1300
PMP 248.2 293 9000 253 4700 330 400 <2.5 3.5
325 8300
4-PA 183.2 – – – – 325
b
425
b
––
355
c
445
c
a
Data from Storvick CA, Benson EM, Edwards MA and Woodring MJ (1964) Chemical and microbiological determination of vitamin B
6
. Methods of
Biochemical Analysis XII: 183–276; Harris SA (1968) Pyridoxine. Encyclopedia of Chemical Toxicology 16: 806–824; Brin M (1978) Vitamin B
6
: chemistry,
absorption, metabolism, catabolism, and toxicity. In: Human Vitamin B
6
Requirements, pp. 1–20. Washington, DC: National Academy of Sciences; Ubbink JB
(1992) Vitamin B
6
. In: DeLeenheer AP, Lambert WE, and Nelis HJ (eds) Modern Chromatographic Analysis of the Vitamins, 2nd edn., Chapter 10. New York:
Marcel Dekker.
b
pH 3.4, 0.01 N acetic acid.
c
pH 10.5, 0.1 N NH
4
OH, lactone of 4-PA.
VITAMIN B
6
/Properties and Determination 6013

can change from one form to another during food
processing and food preparation, and in the body.
Occurrence and Forms in Foods
0007 Information regarding the vitamin B
6
content of
foods has been obtained primarily via microbiological
assay, although some values are available which were
obtained by high-performance liquid chromatog-
raphy (HPLC) methodologies, which can differenti-
ate between the vitamers. In the microbiological
assay techniques, acid (generally hydrochloric acid)
is used in extracting the vitamin from the food; the
acid hydrolyzes phosphates. Hence, vitamer values
obtained using microbiological methods represent
the sum of the phosphorylated and nonphosphoryl-
ated forms of the vitamin. Frequently, total vitamin
B
6
concentration values are obtained rather than
values for the individual vitamers.
0008 Food composition values are available for the three
forms of the vitamin (PL þPLP, PN þPNP, and
PM þPMP) in various foods. These can be found
in the USDA’s publication Pantothenic Acid. Vitamin
B
6
and Vitamin B
12
in Foods. In some reports, the
individual phosphate and free-base forms are also
available.
0009 A high proportion of the B
6
vitamers in plant-
derived foods is glycosylated PN, primarily as 5
0
-
b-d-glucoside. PL, primarily as the phosphorylated
form, is generally the predominant B
6
vitamer in
animal-derived foods. Different foods vary somewhat
as to which form of the vitamin is predominant.
0010 Vitamin B
6
found in unprocessed foods is mainly
bound to proteins. Table 2 gives the vitamin B
6
content of selected foods. This information can be
obtained by accessing the USDA food composition
website or from a variety of printed formats such as
McCance and Widdowson. Meats, whole-grain prod-
ucts, and nuts are good sources of vitamin B
6
.
Cultured cheeses and other fermented products are
also good sources of the vitamin. Fruits and vege-
tables are generally rather poor sources. PN, PM,
and PL have been reported to have equal potencies
in the rat. In humans, dietary PM and PL are about
10% less effective than PN, as indicated by effects on
plasma PLP and urinary 4-PA levels according to a
previous report. In the human body, the nonpho-
sphorylated forms of vitamin B
6
can be converted to
their respective phosphorylated forms and vice versa
by pyridoxal kinase and pyridoxamine (pyridoxine)
phosphate oxidase (see Figure 2). Recently, these
kinase and oxidase enzymes have been identified as
potential targets for pharmacologic agents.
0011 Glycosylated vitamin B
6
is found in all plant-type
foods. The glycosylated vitamin B
6
contents of
selected foods can be found in various publications.
Gregory indicated that a mixed diet contains about
15% of glycosylated vitamin B
6
, which is about 50%
as available as the other B
6
vitamers. This is often
excluded from food composition data. Bioavailability
is of importance in that it reflects the quantity of a
consumed nutrient that becomes available to the cells
of the body.
Effects of Food Processing and
Preparation Methods upon Vitamin B
6
Content of Foods
0012Vitamin B
6
is one of the more labile nutrients. The
vitamin is stable to dry heat; its stability in moist heat
is largely dependent upon the pH of the media, being
relatively stable to heat in an acidic media but not in
alkaline media. The vitamin is unstable to light, both
visible and ultraviolet. The vitamin undergoes rapid
destruction or loss during cooking procedures.
0013Food processing and subsequent storage may also
have an effect upon the vitamin B
6
content of various
foods. The retention of the vitamin is quite high fol-
lowing the processing of dry foods. Thirty to 50% of
the vitamin B
6
present in whole milk and infant for-
mulas is retained following liquid processing includ-
ing sterilization treatments, whereas the spray drying
of these products results in minor loss. Storage of
canned dairy products shows no degradation over
2–3 years. The same is true with regard to commercial
canning and irradiation of boned chicken, although
the retention is better for the irradiated than the
canned product. Heat processing by retorting results
in vitamin B
6
losses in several products. The stability
of the vitamin in dehydrated foods is affected by
moisture content, water activity, and storage condi-
tions. Food-processing techniques generally result in
losses of 0–50% of the vitamin.
0014Vitamin B
6
aldehydes can bind to food proteins as
e-pyridoxyllysine complexes during thermal process-
ing and low-moisture storage. Gregory has shown
that the protein-bound e-pyridoxyllysine has
antivitamin B
6
effects in rats. This pyridoxyllysine
complex may also affect vitamin B
6
availability to
humans, particularly with regard to the vitamin in
unfortified infant formulas.
0015Much of the vitamin loss is due to cooking and
holding practices of consumers and food service per-
sonnel. The retention of the vitamin in oven-braised
beef rounds prepared in food service establishments
has been reported to range from 45 to 62%; values
for green beans are slightly higher, whereas those for
baking potatoes prepared in the skins are around
80%. The vitamin B
6
content of meats and vege-
tables has been shown to decrease following various
6014 VITAMIN B
6
/Properties and Determination

household cooking procedures, even when foods
were cooked according to standard recipes or
manufacturer’s instructions. The retention of vitamin
B
6
in selected vegetables has been found to be highest
for those steamed in plastic bags, followed by those
boiled in plastic bags, those steamed, and lastly, for
those boiled. Boiling results in degradation and leach-
ing but the retention of the vitamin in vegetables
following microwave steaming or regular microwave
cooking techniques is around 90%. It has been found
that more vitamin B
6
is retained when beef and
pork strips are cooked by stir-frying (*67%) than
tbl0002 Table 2 Vitamin B
6
content of selected foods
Food Edible portion
(mgper100 g)
Food Edible portion
(mgper100 g)
Meats
Bacon 0.270 Ham, cured, roasted 0.310
Beef, ground, broiled, medium 0.270 Herring, Atlantic, cooked, dry heat 0.348
Beef, components, separable lean and fat,
trimmed, choice, cooked
0.320 Lamb, composite, separable lean, choice, cooked 0.160
Bologna, beef 0.180 Liver, chicken, simmered 0.580
Bologna, pork 0.270 Mackerel, Atlantic, cooked, dry heat 0.460
Chicken Oysters, Eastern, raw 0.050
Dark with skin, roasted 0.310 Pork, composite, separable lean, roasted 0.404
Light with skin, roasted 0.520 Pork sausage, fresh, cooked 0.330
Frankfurters, beef 0.110 Salmon, Sockeye, cooked, drained 0.219
Haddock, cooked, dry heat 0.346 Shrimp, breaded, fried 0.098
Halibut, cooked, dry heat 0.397 Tuna, canned in water, drained 0.350
Dairy products
Butter 0.003 Eggs 0.139
Buttermilk 0.034 Milk
Cheese Whole 0.042
Cottage, creamed 0.067 2% 0.043
Cheddar 0.074 Skim 0.040
Swiss 0.083 Yogurt 0.032
Cereal and grain products
Bread Rice
White 0.064 White, short-grain, cooked 0.059
Whole wheat 0.097 Brown, medium-grain, cooked 0.149
Pumpernickel 0.126 Wheat, germ, toasted, plain 0.978
Vegetables
Asparagus, solids, drained 0.122 Collards, boiled, drained 0.128
Beans Corn, sweet, boiled, drained 0.060
Lima, boiled, drained 0.193 Lettuce, looseleaf, raw 0.055
Snap, green, boiled, drained 0.056 Mushrooms, raw 0.102
Beets, boiled, drained 0.067 Onions, raw 0.116
Broccoli, boiled, drained 0.143 Peas, green, boiled, drained 0.216
Brussels sprouts, boiled, drained 0.178 Potatoes, boiled, without skin 0.269
Cabbage, boiled, drained 0.113 Potatoes, flesh 0.301
Carrots, raw 0.147 Potatoes, French-fried, restaurant-prepared 0.243
Cauliflower, boiled, drained 0.173 Spinach, boiled, drained 0.242
Celery, raw 0.087 Tomatoes, red, ripe, raw 0.080
Fruits
Apples, raw 0.048 Orange, raw 0.060
Avocados, raw 0.280 Orange juice, fresh 0.040
Blueberries, raw 0.036 Peaches, raw 0.018
Cherries, sour, red raw 0.044 Pears, raw 0.018
Grapefruit, raw 0.042 Raisins, seedless 0.249
Grapes, American type, raw 0.110 Strawberries, raw 0.059
Nuts and seeds
Almonds, dry roasted, unblanched 0.126 Peanuts, dry roasted 0.296
Cashew nuts, dry roasted 0.256 Pecans, dried 0.187
Coconut meat, dried, unsweetened 0.300 Walnuts, dried 0.537
Mixed nuts, dry roasted, with peanuts 0.296
Alcoholic beverages
Beer 0.050 Wine, table 0.024
Data from US Department of Agriculture, Agricultural Research Service (1999) USDA Nutrient Database for Standard Reference, Release 13.
VITAMIN B
6
/Properties and Determination 6015

by microwaving (*60%) or by broiling (*58%).
More vitamin B
6
is retained when pork roasts are
cooked to an internal temperature of 71
C (62%)
than 82
C (54%) and this retention is greatest when
pork is cooked in a bag than roasted or braised.
Vitamin B
6
retention has been found to be similar
(68%) in bison patties cooked by grilling and by
broiling. In summary, loss of some vitamin B
6
is inev-
itable during all household/food service preparation,
to a greater or lesser extent.
Fortification of Foods with Vitamin B
6
0016 PNHCl is listed on the generally recognized as safe
(GRAS) list of the US Food and Drug Administration
and is used in the fortification of foods, particularly
various cereal and dairy products. This form of the
vitamin is also used in dietary supplements and
pharmaceutical products. PNHCl is resistant to
destruction by heat as well as by other factors but
should be protected from light and moisture. Pharma-
ceutical products containing this vitamin have been
reported to have less than 10% loss in vitamin activ-
ity after storage at room temperature for 1 year.
Methods of Analysis
0017 There are two basic stages in procedural methods
dealing with quantitation of vitamin B
6
components
– preparative or extraction techniques and determina-
tive methods. Several excellent reviews have been
published on methods of vitamin B
6
analysis in-
cluding chromatographic techniques. Many methods
have been utilized in quantitating the vitamin B
6
components in foods. These include animal and
microbiological growth, enzymatic, fluorometric, im-
munologic, gas chromatographic (GC), and HPLC
assays.
Extraction Techniques
0018 The major problem encountered in quantitating
vitamin B
6
in plant or animal products is extraction.
Vitamin B
6
compounds must be extracted from food
products before being analyzed by microbiological,
chromatographic, and other methods. Vitamin B
6
frequently occurs in biological materials in associ-
ation with proteins. The most common bond for PLP
is the Schiff base linkage with the e-amino group of
lysine. The Schiff base linkage is easily hydrolyzed by
deproteinizating agents.
0019 Great care must be taken during sample handling
and extraction and with relation to the stability of the
different vitamers as well as their interconversions.
The samples must be homogenous and representative
of the bulk product.
0020Conventional methods for extracting vitamin B
6
compounds from foods entail the use of high tem-
perature and acidic media to denature the protein
and disrupt the sample matrix. The phosphate esters
of PNP, PLP, and PMP are hydrolyzed by autoclaving
in acidic media. The microorganisms used in micro-
biological assays lack response to the phosphates.
Efficient extraction of vitamin B
6
compounds is
obtained using a sample size containing 2–4 mgof
the vitamin and hydrolyzing in 180 ml of 0.055 N
H
2
SO
4
for 1 h at 128
C (20 psi, 138 kPa); 0.44 N
sulfuric acid under the same conditions is essential for
all plant products. Thermal extractions of pH 1.7–1.8
have been found to be optimally effective for most
samples; this pH range corresponds closely to the
0.055 N sulfuric acid, which was recommended
earlier. Hydrochloric acid is also used in thermal ex-
tractions of the vitamin. Complete hydrolysis of PLP
is achieved after autoclaving the sample in 0.055 N
hydrochloric acid at 121
C (15 psi, 103 kPa) for 1 h;
however, 5 h are required for extraction of the
vitamin from dried yeast and liver powder. Complete
hydrolysis of PMP requires 3 h at 125
C in 0.055 N
hydrochloric acid, whereas PLP is hydrolyzed com-
pletely in 30 min. The B
6
vitamers in rice bran are best
hydrolyzed using 2 N hydrochloric acid. The AOAC
method of thermal hydrolysis for B
6
vitamers is as
follows: use 1–2 g of dry product; add 200 ml of 0.44
N hydrochloric acid for plant products followed
by autoclaving at 121
C for 2 h and for animal
products, add 200 ml of 0.055 N hydrochloric
acid, and autoclave at 121
C for 5 h; after the
solution has cooled to room temperature, adjust
the pH to 4.5 with 6 N or saturated potassium hy-
droxide; then dilute to 250 ml with water and filter,
using Whatman No. 40 paper. Complete release of
both protein-bound and phosphorylated forms of the
vitamin is essential for quantitative assay using
microorganisms.
0021Perchloric acid, trichloroacetic acid, and sulfo-
salicylic acid may be used as deproteinating agents.
These acids are particularly useful when one desires
to quantitate phosphorylated, nonphosphorylated,
and glycosylated forms of the vitamin individually,
as use of these agents does not result in dephosphoryl-
ation or deconjugation. If so desired, trichloroacetic
acid may be removed from the extract by extraction
with diethyl ether or freon amine. Perchloric acid can
also be removed from the extract by precipitation
with potassium hydroxide; and sulfosalicylic acid
can be removed via ion-exchange chromatographic
techniques. Metaphosphoric acid has been used in
extraction of the vitamin from brain tissue. This
acid does not need removal from the extract prior to
many of the HPLC techniques for vitamin B
6
assay.
6016 VITAMIN B
6
/Properties and Determination

0022 Extraction procedures must solubilize the vitamers
for subsequent quantitation. The effectiveness of the
extraction procedures may be determined by evalu-
ation of recoveries of B
6
vitamers added during
sample homogenization or, even better, by incorpor-
ation of radiolabeled forms of the vitamin into the
sample, called intrinsic labeling.
Animal Growth Assays
0023 Bioassays are based on the growth response of
animals, usually rats or chicks, to purified diets con-
taining graded levels of a standard vitamin to the
sample being tested. An advantage of the method is
that the vitamin in the sample does not have to be
extracted. Animal assays are not used very frequently
because of their lack of specificity as well as their
expense and time requirement. The intestinal micro-
flora of these animals may affect the data; efforts to
prevent coprophagy or the use of antibiotics are not
completely effective.
Microbiological Assays
0024 The vitamin B
6
composition of plant and animal
products is generally determined using microbio-
logical assays. These assays are tedious, and none
are without problems. The most widely used micro-
biological assay is a growth assay using the yeast
Saccharomyces uvarum (ATCC 9080; formerly S.
carlsbergenesis). Growth is measured via turbidity
using a spectrophotometer. Unfortunately, the re-
sponse of many cultures of the yeast to PM is fre-
quently 60–80% of that to PN and PL. It is
advisable to evaluate the magnitude of the response
differences under the conditions of each assay. PL,
PN, and PM can be separated by subjecting the acid
extractant to cation-exchange chromatography on
Dowex AG 50W-X8 resin using KOAc solutions of
three different pHs; each form of the vitamin is then
analyzed, utilizing its respective calibration curve.
Care must be taken to assure proper separation of
the vitamers and avoid cross-contamination of the
three fractions.
0025 The yeast Kloeckera brevis (ATCC 9774; formerly
K. apiculata) may be used in quantitating total vita-
min B
6
. Some researchers indicate that K. brevis
has an equal growth response to PL, PN, and PM,
whereas others indicate that it has an even lower
relative response to PM than S. uvarum. The K. brevis
assay has been adapted to radiometric quantitation.
0026 The total, as well as the three nonphosphorylated
vitamers, may also be determined by a differential
microbiological technique. S. uvarum responds to PL,
PN, and PM, whereas Streptococcus faecalis R (ATCC
8043) responds to PL and PM, and Lactobacillus
casei (ATCC 7469) responds to only PL. Tetrahy-
mena pyriformis, a protozoan, has also been used as
an assay organism.
0027Saccharomyces uvarum is the microorganism used
in the AOAC method. The concentrations of the three
nonphosphorylated B
6
vitamers are quantitated in
this method.
0028Assays for glycosylated vitamin B
6
compounds in
foods have been developed utilizing S. uvarum and
differential hydrolytic procedures. This method does
have a tendency to underestimate the quantity of
the glycosylated vitamin in raw plant foods having
p-glycosidase activity.
0029Values given in food composition tables have
been derived primarily using S. uvarum as the test
organism. These tables generally list total vitamin B
6
concentrations but may list PL, PN, and PM con-
centrations. The Center for Nutrient Analysis of
the US Food and Drug Administration uses S.
uvarum for quantitating vitamin B
6
in foods. Data
obtained microbiologically using S. uvarum do not
always agree with those obtained by animal growth
assays.
Enzymatic Assays
0030Several enzymatic methods are available that quanti-
tate PLP, the main circulating form of vitamin B
6
.
These methods are frequently utilized as parameters
for the assessment of vitamin B
6
status of animals,
including humans but are not utilized in the analysis
of food samples. The enzymatic methods that have
been more commonly used include the following:
the cleavage of tryptophan using apotryptophanase
(EC 4.1.99.1), the measurement of aspartate amino-
transferase (EC 2.6.1.1; formerly referred to as
glutamic-oxaloacetic transaminase), and alanine
aminotransferase (EC 2.6.1.2; formerly referred to
as glutamic-pyruvic transaminase) activities, and the
radiomonitored decarboxylation of [
14
C]tyrosine
using the apoenzyme of tyrosine decarboxylase (EC
4.1.1.25). Currently, the most acceptable enzymatic
method of quantitating PLP is the tyrosine apode-
carboxylase technique.
Fluorometric Assays
0031Direct fluorometric analysis of vitamin B
6
in extracts
of plant and animal products is generally unsatisfac-
tory. This is due to the presence of many potentially
interfering compounds that fluoresce, as well as the
varying spectral characteristics of the B
6
vitamers. As
a result, the total vitamin B
6
content of selected foods
is higher when measured by fluorometry following
open-column chromatography than published values
based on microbiological assay.
VITAMIN B
6
/Properties and Determination 6017
