Caballero B. (ed.) Encyclopaedia of Food Science, Food Technology and Nutrition. Ten-Volume Set
Подождите немного. Документ загружается.


number of factors, especially the climatic conditions.
Intensive livestock production has created problems
of excreta disposal. The number of animals per unit
area of land has vastly increased in many countries
and it has been necessary to increase application
rates of animal waste on to the land. One survey
found that 10% of cattle slurry samples contained
Salmonella, with survival periods ranging from 11
to 12 weeks.
0025 Biological treatment of human sewage removes
most of the suspended and dissolved organic matter,
but it does not necessarily remove pathogenic bac-
teria. Where sewage sludge is used as a fertilizer,
many samples have been found to be contaminated
with Salmonella. There are numerous reports of the
isolation of Salmonella from rivers and streams and
of their pollution by sewage effluent and slurry run-
off. Further spread from contaminated environments
may also take place by wild animals and birds.
Transmission to Humans
0026 Typhoid fever usually follows the ingestion of drink-
ing water contaminated by human carriers of S. typhi
or food prepared or handled by such carriers who do
not take adequate hygienic precautions.
0027 In contrast, acute gastroenteritis (foodborne dis-
ease/poisoning) is usually acquired from consumption
of foods which may be directly or indirectly contam-
inated with Salmonella. A wide variety of animal
species have been shown to be capable of harboring
the organisms, and in the developed world turkeys,
chickens, swine, and cattle have often been found to
be infected in abattoir studies. Cross-contamination
may readily occur during transport to the abattoir
and during slaughter. Modern poultry-processing
plants are designed with emphasis on speed, and
during the slaughtering process there are many points
where cross-contamination may occur. Recent
surveys have found that up to 30% of chicken car-
casses may be contaminated with Salmonella. Table
eggs have been found to be an important vehicle for
the transmission of S. enteritidis to humans and
undercooked or raw eggs or dishes made from them,
such as mayonnaise or mousse, have been responsible
for many outbreaks of food poisoning.
0028 The progressive trend toward mass processing and
distribution of food products has been an important
factor in the increased incidence of Salmonella food-
borne disease. Milk has also been shown to be an
important source of infection and has been associated
with massive outbreaks of human salmonellosis.
Most outbreaks have been associated with the con-
sumption of raw milk, although pasteurization plant
failure has also resulted in large outbreaks. Salads and
other vegetables which have been contaminated in
washing or ‘freshening’ with polluted water have
also been shown to be associated with human sal-
monellosis. Many other products, e.g., beansprouts,
chocolate, have been found to be the source of Sal-
monella infection and dried milk became contamin-
ated with Salmonella when the production machinery
was contaminated. Whatever the source, many out-
breaks occur as a consequence of the delay between
preparation/cooking and consumption of the food,
which allows the numbers of Salmonella to increase
rapidly. The important food-associated risk factors
are inadequate cooking or reheating, storage at
inappropriate temperatures, and cross-contamination
from raw to cooked food.
0029Person-to-person spread has been demonstrated on
many occasions and may be of importance in young
children and groups living under poor socioeconomic
conditions where effective sanitation is lacking. In
these situations, flies may serve as vectors for Salmon-
ella transmission. Dog and wild animal feces on
footwear have been implicated as a route by which
infection can be carried into households. Person-
to-person spread may also occur in hospitals, nursing
homes, and mental institutions, where a number of
large outbreaks have occurred. Amplification of in-
fection in these institutions may occur from contam-
inated food or from asymptomatic carriers; babies are
at special risk. Likewise, contaminated equipment
has been shown to be vehicles of infections.
Causation of Disease
0030Salmonella cause disease by invading the intestinal
mucosa and multiplying in the gut-associated lymph-
oid tissue. From the infected tissue the organisms are
drained to the regional lymph nodes, where further
spread is usually prevented if the host defense
mechanisms are successful. In humans nontyphoidal
Salmonella serovars usually cause a localized disease
which is manifest as an acute gastroenteritis. If, on
the other hand, the host’s defense mechanisms are
unable to prevent the spread of the organism, sys-
temic disease results, as commonly occurs with
typhoid. The etiology of diarrheal disease is poorly
understood, and although several putative toxins,
e.g., enterotoxins, cytotoxins, have been described,
their significance is far from clear. (See Salmonella:
Salmonellosis.)
0031Whether infection follows exposure to any patho-
genic microorganisms depends in part on the number
of organisms that enter the host’s tissues. From vol-
unteer studies in humans, it has been suggested that
large inocula of Salmonella are necessary to cause
illness. However, investigations of outbreaks of Sal-
monella foodborne disease have suggested that the
SALMONELLA
/Properties and Occurrence 5077

infective dose is often low; in six of the 11 outbreaks
the actual dose ingested was calculated as < 10
3
organisms. However, many factors may affect the
infective dose, not least of which are strain variations,
e.g., S. choleraesuis, although a rare cause of human
infection, may cause serious disease. Children and
older people are more susceptible; other concurrent
illnesses (e.g., acquired immune deficiency syndrome
(AIDS)) may increase susceptibility. The use of anti-
biotics for other indications may predispose to food-
borne salmonellosis, even when the Salmonella are
sensitive to that antibiotic. There is a fivefold increase
in risk when the Salmonella are resistant.
Prevention of Transmission
0032 The overall quality of meat and edible byproducts
depends heavily on their microbiological quality.
This is very dependent on the contamination level of
the production equipment, as well as on the skin
and intestinal microflora of animals and on the
technology and techniques used in slaughtering and
processing. The fecal microflora of animals is the
predominant source of pathogens on the final dressed
carcass, and the modern slaughter line offers many
risks of cross-contamination. In general, such cross-
contamination is much less pronounced with car-
casses of beef and sheep than with pork and poultry
carcasses. A system to insure quality and safety must
be designed for the entire chain of operations, from
the farm to the consumer. This system must include
the identification of potential microbiological prob-
lems and control measures at all stages of the entire
meat production chain, as well as the development of
Hazard Analysis Critical Control Point procedures.
Although the hazards may differ from country to
country and vary with animal health, slaughter
procedures, type of meat products, and storage
and distribution, the main areas of focus are the
slaughter process itself and disinfection of tools and
equipment.
0033 Pasteurization will prevent milk-borne salmonel-
losis, although outbreaks have occurred on a number
of occasions when faults have developed in plants.
One of the most effective end-product treatments is
gamma-irradiation, which can destroy Salmonella
on poultry carcasses and prolong shelf-life, although
possible changes in flavor and texture may occur.
There may be some consumer resistance toward the
use of nuclear energy.
0034 Equally important is the education of caterers and
domestic consumers in all aspects of hygienic prepar-
ation of food. Cross-contamination may occur
readily in kitchens, especially when raw and cooked
foods are prepared on the same surfaces.
Public Health Aspects
0035In many countries the results of tests which identify
the presence of Salmonella in animals have to be
reported to the appropriate government department
and, in addition, separate orders may relate to animal
feeds.
0036Likewise, on the human side, it may be necessary to
report if a patient is suffering from or is suspected of
having foodborne disease. Following the reporting of
Salmonella incidents in both humans and animals,
further investigations may be carried out. Regulations
may also apply to the production and sale of food.
Economic and Social Impact
0037The financial costs of Salmonella infections are not
only associated with investigations, treatment, and
prevention of human illness; they may also affect the
whole food production chain.
0038In the public sector, resources are necessary for
surveillance, treatment of patients, and investigations
of outbreaks. Financial burdens may be imposed on
industry, especially the food industry. Likewise, the
cost to affected individuals may be extremely high,
especially should death result from Salmonella infec-
tions. The costs associated with Salmonellosis may be
subdivided into tangible costs, which can be meas-
ured in monetary terms (e.g., medical costs and loss of
work), and intangible costs, such as loss of leisure,
pain, discomfort, etc., which cannot be readily
costed. A study of infectious intestinal disease in
England between 1993 and 1996 suggested that the
true rate of salmonellosis in the community was 220/
100 000 population and the estimated cost per human
case was £660.
0039An analysis of five Salmonella outbreaks in North
America gave direct costs which ranged from $36 400
to $62 million. In the UK, an outbreak of S. ealing
infection associated with powdered milk was esti-
mated to have cost £14.6 million in the late 1980s.
0040There have been few studies into the costs and
benefits of preventing Salmonella infection, but it
has been suggested that for every £1 spent on investi-
gation and curtailment of an outbreak, there is a
saving of £5.
See also: Food Poisoning: Classification; Salmonella:
Detection; Salmonellosis
Further Reading
Doyle MP (ed.) (1989) Foodborne Bacterial Pathogens.
New York: Marcel Dekker.
Ewing WH (ed.) (1986) Edwards and Ewing’s Identifica-
tion of Enterobacteriaceae, 4th edn. New York: Elsevier.
5078
SALMONELLA
/Properties and Occurrence

Guinee PAM and van Leeuwen WY (1987) Phage typing
of Salmonella. In: Methods in Microbiology, vol. 11,
pp. 158–190. New York: Academic Press.
Le Minor L and Popoff MY (1987) Request for an opinion.
Designation of Salmonella enterica sp. nov. as the type
and only species of the genus Salmonella. International
Journal of Systemic Bacteria 37: 465–468.
Reeves MW, Ewins GM, Heiba AA et al. (1989) Clonal
nature of Salmonella typhi and its genetic relatedness
to other salmonellae as shown by multilocus enzyme
electrophoresis and proposal of Salmonella bongori
comb. nov. Journal of Clinical Microbiology. 27:
313–320.
Saeed AM (1999) Salmonella enterica Serovar enteritidis in
Humans and Animals: Epidemiology, Pathogenesis and
Control. Ames, Iowa: Iowa State University Press.
Varnam AH and Evans MG (1991) Foodborne Pathogens:
An Illustrated Text. London: Wolfe.
WHO Collaborating Centre for Reference and Research on
Salmonella (1997) Antigenic formulas of the Salmonella
Serovars. Paris: Institut Pasteur.
Wray C and Wray A (eds) (2000) Salmonella in Domestic
Animals. Wallingford, Oxon: CABI Publishing.
Detection
T Humphrey, PHLS Food Microbiology Research Unit,
Heavitree Exeter, Devon, UK
P Stephens, Oxoid Limited, Basingstoke, Hampshire,
UK
Copyright 2003, Elsevier Science Ltd. All Rights Reserved.
Detection
0001 In the developed world, the majority of cases of
human salmonellosis is zoonotic and results from
the colonization/infection of food animals and result-
ant contamination of products derived from them.
Salmonella are also ubiquitous, and a diverse range
of foodstuffs – including dried milk, fermented saus-
age, beansprouts, chocolate, and yeast-based flavoring
– have been implicated as vehicles for human salmon-
ellosis. In the UK, and elsewhere in the last decade,
most cases or outbreaks of Salmonella infection have
resulted from the consumption of contaminated eggs
or poultry meat. Natural water systems, particularly
those receiving human and animal waste, are also
frequently contaminated.
0002 The ubiquity of Salmonella and the wide range of
materials with which they have been associated have
meant that numerous media and techniques have
been developed for their isolation. It is not the inten-
tion in this chapter to go into detail on the possible
virtues or disadvantages of individual methods.
Attention is focused instead on the fundamental
aspects of the isolation and detection of Salmonella,
particularly from food and environmental samples.
Special emphasis is given to sublethal injury and its
impact on recovery of the bacteria and the possible
inhibition by other organisms. The application of
rapid methods is also discussed. (See Food Poisoning:
Tracing Origins and Testing.)
Sublethal Injury and its Impact on Detection
0003Salmonella are primarily enteric organisms and,
whether in the gut or on contaminated foodstuffs,
they are usually present as part of a mixed microbial
population. Exceptions to this are seen with invasive,
host-specific strains such as S. typhi in humans and
S. enteritidis in poultry. The latter organism, for
example, can be isolated in pure culture from both
the tissues of infected chickens and the contents of
intact shell eggs. It is generally necessary, however, to
apply techniques which selectively encourage the
growth of Salmonella and to use agars which permit
the organism to produce characteristic colonies. The
similarity in antibiotic resistance patterns between
Salmonella and other enterobacteria has largely pre-
cluded the use of antibiotics and selection has relied
upon the use of chemicals such as selenite, tetra-
thionate, and deoxycholate.
0004When microorganisms, particularly Gram-negative
bacteria, are exposed to unfavorable conditions such
as high or low temperature, they may become sub-
lethally injured. This can be defined as ‘a sensitivity to
either selective agents or conditions to which normal
cells are resistant.’ In Salmonella, injury can be mani-
fested by, for example, lowered resistance to the chem-
icals mentioned above. The organisms may also be less
able to grow, particularly in selective media, at ele-
vated incubation temperatures, such as 43
C, which
are used to improve the selectivity of isolation media
when samples like sewage are examined.
0005Techniques used routinely for clinical specimens
when large numbers of the target pathogen may be
present and where it is relatively unaffected by its
environment are not suitable for use with either food
or environmental samples. These might have been
exposed to conditions damaging to bacteria and
they may also contain only low numbers of Salmon-
ella. The direct inoculation of food or environmental
samples into selenite broth or another selective
medium may lead to false-negative results.
0006The principal site of injury in the bacterial cell is
the outer membrane, and alterations in permeability
allow the ingress of selective agents that are normally
excluded. If cells are exposed to more extreme condi-
tions, damage can also be caused to the chromosome
and ribosomes. Much work remains to be done on the
SALMONELLA
/Detection 5079

response of Salmonella to adverse conditions and on
the full impact of the exposure of these bacteria to
different environments and their subsequent ability
to grow in culture media. Salmonella, like other
bacterial cells, are able to repair the lesions causing
sublethal injury, either partially or completely, if they
are incubated in a nonselective medium at 37
C. Two
media, buffered peptone water (BPW) and lactose
broth, are the most commonly used, with the buffer-
ing capacity of BPW giving it an advantage over the
other medium – particularly when foods containing
fermentable substrates are examined.
0007 Studies have demonstrated that the isolation rate
from selective broth cultures is greatly improved if
they are inoculated with an actively growing popula-
tion of Salmonella. It is thus essential that initial
incubation in BPW allows the organism both to over-
come the effects of sublethal injury and to multiply.
0008 The period of recovery or repair is often referred to
as preenrichment. Incubation is usually for 18–24 h,
although some workers have reported improved isol-
ation rates when preenrichment is extended to 72 h.
This is dependent on the material under investigation.
Salmonella do not appear to be able to compete well
with some other bacteria. Recovery media, by neces-
sity, are nonselective and permit the growth of the
majority of aerobic and facultative organisms present
in the sample. Where this encourages the prolifer-
ation of either Proteus or Pseudomonas spp. – as
with liquid raw egg and chicken meat – or lactobacilli
– as with dairy products – Salmonella may be
inhibited. This can be particularly pronounced when
incubation is prolonged (Table 1).
0009 The addition to BPW of novobiocin and cefsulodin,
which inhibit Proteus or Pseudomonas spp., respect-
ively, but have little effect on the growth of Salmon-
ella, was found to improve the isolation rate of
Salmonella from naturally contaminated samples of
raw liquid egg (Table 1). The recovery of Salmonella
from dried milk can also be improved if, after 2–4h
initial incubation, brilliant green at a final concen-
tration of 0.0002% is added to the preenrichment
culture.
0010The presence of any number of Salmonella in a
processed or cooked food is regarded as being poten-
tially hazardous and most microbiological guidelines
suggest an absence of the bacteria in 25 g of product.
There is also evidence that, with some foodstuffs,
particularly those rich in fat, and with certain vulner-
able individuals such as the very young or the elderly,
the infective doses of Salmonella may be low. Recent
studies have also demonstrated that sublethally
injured cells of Campylobacter jejuni are capable of
repair in the intestinal tract. Salmonella may also be
able to do this and it is important that sensitive tech-
niques are used for their detection in the laboratory.
In this respect, the importance of effective preenrich-
ment cannot be overemphasized. As a general rule,
it is prudent, when examining food and environmen-
tal samples from any source, to carry out primary
incubation in BPW at 37
C for a full 24 h. The ratio
of sample to medium should be at least 1:10 and,
where appropriate, the growth of competing flora
may be suppressed by the addition of antibiotics.
Selective Culture
0011The necessity for selective culture techniques in
microbiology has been recognized for over 100 years
and much of the early work was centered upon
Salmonella. Selective isolation is usually in two
stages: growth in an enrichment broth followed by
plating on a selective agar. Selective media make use
of either dyes or chemicals. A formulation much in
use in clinical laboratories is based on selenite. It is
believed that this compound inhibits bacteria either
by reaction with sulfhydryl groups or by the forma-
tion of analogs of sulfur amino acids. Selenite broth
has been used successfully for many years and modi-
fications to improve the isolation rate have included
the addition of cystine and the incorporation of fer-
mentable sugars, such as either mannitol or lactose,
which prevent increases in the pH. Selenite is less
selective at alkaline pH values.
0012Selenite can be used for direct inoculation with
specimens such as feces or used following preenrich-
ment. It is probably less suitable, however, for the
latter when compared to other media. The medium
can inhibit many bacterial types, but two important
exceptions – Proteus and Pseudomonas spp. – can
cause problems, particularly as they are capable of
preventing the growth of Salmonella and can also
resemble them on selective agars.
0013Salmonella have been shown to possess the enzyme
tetrathionate reductase, which is absent in many
tbl0001 Table 1 The influence of period of preenrichment and the
addition of novobiocin and cefsulodin on the isolation of
Salmonella from samples of liquid raw egg
Culture medium No. of Salmonella-positive
samples
a
after incubation
for
24 h 48 h
Egg/BPW only 32 14
Egg/BPW plus novobiocin (5 mgml
1
),
cefsulodin (10 mgml
1
)
74 70
a
110 samples were examined. Rappaport–Vassiliadis broth was used as
the selective medium.
BPW, buffered peptone water.
Data from Humphrey TJ and Whitehead A (1992).
5080
SALMONELLA
/Detection

other bacteria. This provides a selective advantage
and has been used in the development of another
commonly used enrichment medium, tetrathionate
broth. Tetrathionate is usually employed in combin-
ation with brilliant green and bile salts, the medium
being known as Mu
¨
ller–Kauffman tetrathionate
broth. It is probably more selective than selenite, but
more care may be required in the control of incuba-
tion temperatures.
0014 Malachite green, in combination with high concen-
trations (4%) of magnesium chloride and a medium
pH of 5.0–5.2, has been shown to be effective for the
isolation of Salmonella. The medium was originally
developed for use with feces but modifications in
the last 10–15 years, which have seen a reduction
in the malachite green concentration from 0.012%
to 0.004% and use of soya peptone rather than tryp-
tone, have meant that the formulation, usually known
as Rappaport–Vassiliadis (RV) broth, is more suitable
for selective culture following preenrichment. This
medium is probably the one of choice in the examin-
ation of nonclinical samples and numerous studies,
on many different materials, have confirmed the
superiority of RV broth over both selenite and
tetrathionate.
0015 The selective nature of the above broths is often
finely balanced and can be disturbed by either a large
inoculum, relative to broth volume, or overlong incu-
bation. A change in incubation temperature can also
profoundly affect the toxicity of the medium.
0016 An inoculum-to-broth ratio of 1:10 is recom-
mended for both selenite and tetrathionate broths,
although following preenrichment culture there
would appear to be no reduction in sensitivity if
smaller volumes of BPW are used. The size of the
inoculum is critical with RV broth and its ratio to
the medium should be at least 1:100. With this
medium, studies have indicated that more samples
are Salmonella-positive after 48 h rather than 24 h
incubation, although the differences are often not
significant. In contrast, extended incubation signifi-
cantly reduces the effectiveness of tetrathionate and
selenite broths and, with the latter, overgrowth of
competing flora occurs frequently. These media
can also become more toxic to the target organism
and Salmonella may die if incubation is continued
much beyond 24 h. Care also has to be taken in
controlling incubation temperature. Selenite and
tetrathionate can be used at either 37
Cor43
C
and are more selective at the higher temperature.
Some studies have shown, however, that Salmonella
will not always survive in these media at 43
C. Initial
studies on RV broth recommended 43
C but it is
now accepted that incubation at 41+0.5
C increases
sensitivity.
0017Studies with particular samples or in particular
situations have demonstrated that one selective
medium may be superior to another. No one medium,
however, can be relied upon always to maximize the
isolation rate with all samples. There may thus be
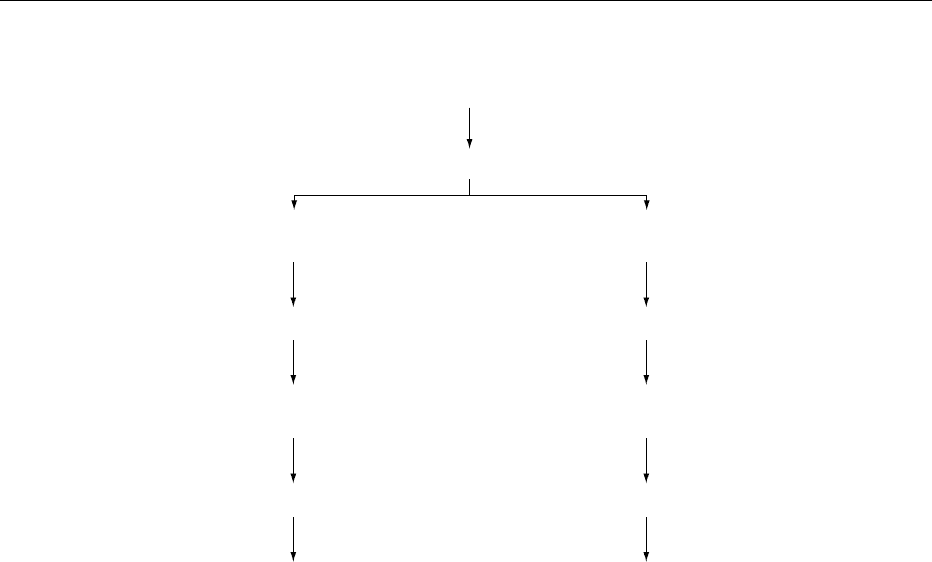
advantages in using two selective broths (Figure 1).
0018An important disadvantage with traditional culture
techniques is the time taken to confirm whether a
food sample is Salmonella-positive or -negative.
There have been many attempts to make Salmonella
testing more rapid and some of the newer methods
are discussed below.
0019At first sight, it would seem possible to reduce the
length of either preenrichment or selective broth cul-
ture, but in the past this approach has been largely
unsuccessful. A number of publications have stated
that recovery from injury is complete within 8 h at
37
C. This is dependent on the culture medium used
and the degree of cellular damage. In some systems,
lag times of up to 72 h have been reported, and other
studies have indicated that repair of damaged cells is
not complete until some hours after growth has begun.
Thus, subculture of preenrichment broths after 6 h
rather than 24 h incubation was found to reduce the
isolation rate. Newer work, however, has suggested
that it may be possible to shorten traditional culture
methods without any loss of sensitivity by using a
combination of delayed release of selective agents
into an optimized recovery medium. The new method
makes use of a peptone-based medium that contains
oxygen-consuming sterile outer membrane fragments
from Escherichia coli, which protect bacteria by
reducing oxidative stress. This allows damaged
Salmonella cells to recover more rapidly than with
conventional media. The method also makes use of
delayed release capsules that release the selective
components of RV broth after about 5 h at 42
C.
Trials to date indicate that this method is at least
equivalent in performance to standard methods.
0020Selective agars should be so formulated that the
competing flora is suppressed while the target organ-
ism is able to form discrete, characteristic colonies. A
degree of selectivity is achieved by the addition of
either dyes like brilliant green or chemicals such as
sodium deoxycholate. The resistance of Salmonella to
selective agents is similar to that of many other bac-
teria and this can create difficulties in media formula-
tion. Thus, the detection of Salmonella on selective
agars relies heavily on diagnostic aspects. Principal
among these is the inability of most strains to ferment
lactose and the production of hydrogen sulfide from
thiosulfate at a neutral pH (leading to black colonies).
More recently, the advent of affordable chromogenic
substrates has led to the development of a number of
new selective differential media for Salmonella. These
SALMONELLA
/Detection 5081
new media often utilize a combination of traditional
diagnostic markers with new substrates for the detec-
tion of galactosidase, glucoronidase, and esterase ac-
tivities. Additionally, old diagnostic tools such as acid
production from carbohydrate utilization have been
applied to new substrates, e.g., propylene glycol util-
ization by Salmonella.
0021 As with enrichment broths, many selective agars
are available, but none has been shown definitively to
be suitable for all applications and the best course of
action would be to use two agars in parallel. The most
commonly used media appear to be bismuth sulfite,
xylose lysine deoxycholate (XLD), and brilliant green
agar (BGA).
0022 Many workers have attempted to improve selectiv-
ity by the incorporation of antibiotics and/or other
selective agents. Of these, novobiocin, which prevents
the growth of Proteus spp., seems to be the most
useful.
Confirmatory Tests
0023 Other organisms, particularly members of the family
Enterobacteriaceae, can resemble Salmonella on
selective agars and confirmation of ‘Salmonella-like’
colonies is necessary. Tests take the form of biochemical
confirmation, which usually involves assessment of
urease and lysine decarboxylase activity, fermentation
of dulcitol, indole production, growth in the presence
of potassium cyanide, utilization of sodium malonate
and, more recently, pyrrolindonylarylamidase (PYR)
activity. These reactions, in combination with sero-
logical tests, are usually sufficient for identification,
but additional tests may sometimes be necessary. If
these are to form part of a laboratory routine, the use
of commercial kits may be cost-effective. Antibodies
against somatic (O) and flagella (H) antigens are used
to confirm/identify Salmonella-like isolates. Somatic
antigens are composed of polysaccharide, while those
from the flagella are proteinaceous. Testing will usually
comprise slide agglutinations with polyvalent O and H
antisera, followed by the use of sera raised against
specific antigens.
Rapid Methods
0024The time taken to confirm or deny the presence of
Salmonella, especially in food and environmental
samples, can create difficulties and, with perishable
foods, can mean that products may be distributed
and consumed before test results are known. It
is not surprising that considerable attention has
Test portion (1 part, typically 25
g)
+
Buffered peptone water (9 parts)
Incubate at 37
C for 18
h 2
h
Sub-culture 1
ml into 10
ml
MKTTnmedium
Incubate at 37
C for 24
h 3
h
Plate onto: XLD agar + second
agar
Sub-culture 0.1 ml into 10 ml
Rappaport-Vassiliadis medium
Incubate at 41.5
C for 24
h 3
h
Plate onto: XLD agar + second
agar
Incubate at 37
C for 24
h 3
h
Select 5 typical colonies from
each
p
late for confirmation
Incubate at 37
C for 24
h 3
h
Select 5 typical colonies from
each
p
late for confirmation
fig0001 Figure 1 International Standards Organization (ISO) standard method for Salmonella isolation (ISO 6579:1997). BGA, brilliant green
agar; XLD, xylose lysine deoxycholate.
5082
SALMONELLA
/Detection

been paid to the development of rapid methods of
detection.
0025 The new methodologies can be divided into two
broad categories. There are those designed to detect
or isolate viable cells and those that detect cellular
components such as DNA. There are concerns that
the latter methods may detect either dead cells or
DNA released from them and that cultural techniques
may lack the required sensitivity.
0026 Conventional culture techniques, as discussed
earlier, can be long-winded, cumbersome, and expen-
sive. How much better it would be if it were possible
to detect pathogenic bacteria by the direct application
of a test to a food sample. Salmonella spp., and pre-
sumably other foodborne pathogens, appear to have
unique DNA sequences that could allow detection.
Salmonella-specific DNA probes and polymerase
chain reaction (PCR) methods have been developed.
0027 These techniques compare well to conventional
culture when used on enrichment broths. The above
studies were designed to obviate the need for selective
culture and serological/biochemical identification.
There are other examples, and various automated
PCR-based systems are now available. Most of them
require an enrichment period which delays results but
sensitivity can be of the order of 3 CFU per 25 g of
food.
0028 Other new approaches include flow cytometry.
These methods have faced the criticism that they are
still too slow for the rapid pace of modern processed-
food production methods. Tests would be much
easier to perform and much more rapid if the modern
technologies could be applied directly to samples.
Such an approach, which continues to be investi-
gated, is not without problems. One is due to the
fact that DNA is heat-stable. Thus, intact DNA will
be present in processed foods. DNA in both a free
form and within dead cells of Salmonella can also
survive for considerable periods in sea water. One
possible way to overcome this problem is to include
a culture step as a means of detecting viable cells. Not
only will this increase the length of the test but it may
not be sufficient to allow the growth of more severely
damaged cells, as discussed earlier.
0029 An alternative nucleic acid target to determine via-
bility would be an RNA molecule that exists as many
copies in a cell and which exhibits rapid turnover.
Messenger RNA (mRNA) may prove to be a suitable
target as it has a reported half-life of 2 min or less,
and PCRs have been published for the detection of
viability in Escherichia coli and the thermophilic
Campylobacter spp. The rate of degradation of the
mRNA is influenced by the method of inactivation,
however, and this has to be considered when assessing
food-processing conditions.
0030‘Rapid’ methods clearly have a place for the detec-
tion of Salmonella spp. in food samples. With many
of the current tests, time is saved because selective
plating and biochemical and/or serological confirma-
tory tests are not necessary. ‘Rapid’ tests would
appear to offer advantages over traditional culture
systems. It is likely that improvements will be made
in both speed and sensitivity. This may encourage
a wider use of the new technologies. If this is
the case, it is to be hoped that people continue to
bear in mind the vital roles of proper sample handling
and the importance of using initial culture systems,
which facilitate the recovery and growth of injured
organisms.
See also: Escherichia coli: Occurrence; Detection; Food
Poisoning; Occurrence and Epidemiology of Species
other than Escherichia coli; Food Poisoning by Species
other than Escherichia coli; Food Poisoning: Tracing
Origins and Testing
Further Reading
Bailey JS, Cox NA and Blankenship LC (1991) Comparison
of an enzyme immunoassay, DNA hybridisation, anti-
body immobilisation and conventional methods for re-
covery of naturally occurring Salmonella from processed
broiler carcases. Journal of Food Protection 54: 354–
356.
Barrow GI and Feltham RKA (1993) Cowan and Steel’s
Manual for the Identification of Medical Bacteria, 3rd
edn. Cambridge: Cambridge University Press.
Candish AAG (1991) Immunological methods in food
microbiology. Food Microbiology 8: 1–14.
Cudjoe KS and Krona R (1997) Detection of Salmonella
from raw food samples using Dynabeads anti-Salmon-
ella and a conventional reference method. International
Journal of Food Microbiology 17: 55–62.
de Boer E (1998) Update on media for isolation of entero-
bacteriaceae from foods. International Journal of Food
Microbiology 45: 43–53.
Fierens H and Huyghebaert A (1996) Screening of Salmon-
ella in naturally contaminated feeds with rapid methods.
International Journal of Food Microbiology 31:
301–309.
Howie A (1999) A new development in Salmonella
testing. European Food and Drink Review, winter
issue, 53–56.
Mansfield L and Forsythe S (1996) Collaborative ring-trial
of Dynabeads anti-Salmonella for immunomagnetic
separation of stressed Salmonella cells from herbs and
spices. International Journal of Food Microbiology 29:
41–47.
Reissbrodt R, Vielitz E, Kormann E, Rabsch W and Kuhn H
(1996) Ferrioxamine E-supplemented pre-enrichment
and enrichment media improve various isolation
methods for Salmonella. International Journal of Food
Microbiology 29: 81–91.
SALMONELLA
/Detection 5083
Saeed AM (ed.) (1999) Serovar Enteritidis in Humans and
Animals: Epidemiology, Pathogenesis and Control.
Ames, Iowa: Iowa State University Press.
Speck ML (1984) Compendium of Methods for the Micro-
biological Examination of Foods, 2nd edn. Washington,
DC: American Public Health Association.
Salmonellosis
C Wray, Greendale Veterinary Laboratories Ltd,
Knaphill, Woking, UK
C A Hart, University of Liverpool, Liverpool, UK
Copyright 2003, Elsevier Science Ltd. All Rights Reserved.
Introduction
0001 Salmonellosis is the general term for human illness
caused by members of the genus Salmonella; however
from the epidemiological point of view it is necessary
to differentiate the enteric fevers caused by S. typhi
and paratyphi, A, B, and C from foodborne gastro-
enteritis caused by any of the other Salmonella sero-
vars. The infectious nature of typhoid fever has been
known for more than a century and the causative
organism was one of the earliest to be isolated and
characterized. The transmission of S. typhi occurs
most often by water which has been contaminated
by feces or urine from infected human carriers or food
prepared and handled by such carriers who do not
take adequate hygienic precautions. The organism
appears to be only a parasite of humans and the
higher apes and the link between poor sanitation
and other epidemiological aspects of the disease was
elucidated by William Budd before the opening of the
bacteriological era.
0002 In contrast, gastroenteritis (foodborne disease) is
usually acquired from consumption of foods which
may be directly or indirectly contaminated with Sal-
monella. Whether infection follows exposure to any
pathogenic microorganism depends in part on the
number of organisms (infective dose) that enter the
host’s tissues. Factors that may predispose to human
salmonellosis are given in Table 1 and the following
section. There are four main clinical patterns of
Salmonella infection in humans: (1) typhoid (enteric
fever); (2) acute gastroenteritis; (3) septicemia, with
or without localized infection; and (4) asymptomatic
infection.
Enteric Fevers
0003 Typhoid and paratyphoid fevers usually follow inges-
tion of drinking water contaminated with feces
containing S. typhi/paratyphi A, B, or C, or food
prepared or handled by a person who is a carrier of
the organism. Direct transmission from one individ-
ual to another may occur via the fecal–oral route,
especially in children, because of their poor attention
to personal hygiene. While large-scale epidemics of
typhoid fever have been traced to human fecal con-
tamination of food, poor sanitary practice resulting in
contamination of drinking water by fecal material
containing S. typhi appears to be a major factor in
many countries. Of foodborne outbreaks, 504 cases
of typhoid occurred in Aberdeen; this was caused
by the ingestion of tinned corned beef from Argen-
tina. The meat was contaminated in Argentina, where
river water containing unprocessed sewage was used
to cool the containers after sterilization. The water
seeped through the seams of the cans and reached
the contents. In Aberdeen, infection developed in
individuals who ate the corned beef, but also in those
who ate meat that became contaminated by the
machine that had been used to slice the corned beef.
0004In Mexico, in the early 1970s a large outbreak of
typhoid was caused by a chloramphenicol-resistant
strain of the organism, which had contaminated
water. The lack of susceptibility of the organism to
chloramphenicol was responsible for the death of
many patients who were infected with it. The resist-
ance determinant was a useful epidemiological
marker when the organism caused disease in the
USA, and a number of European countries.
Clinical Findings: Typhoid Fever
0005Typhoid fever is the best-studied form of salmonel-
losis and is well-described in the literature. It is po-
tentially fatal for young children, particularly during
the first year of life, and for the elderly, but in endemic
areas a degree of immunity may develop in the popu-
lation. Clinically, paratyphoid tends to be less severe
than typhoid.
tbl0001Table 1 Factors affecting the infectious dose of Salmonella
Bacteria-associated factors
Serovar, genotype
State and nature of contaminated material ingested (dry, moist,
liquid, and does it allow bacterial multiplication?)
Resistance to antibacterials
Stress status of the bacteria
Host-associated factors
Age of host (very young and aged are most susceptible)
Effect of therapy (prior treatment with antibacterials,
antacids, etc.)
Presence of other disease (malaria, human immunodeficiency
virus (HIV), etc.)
Immune status of the host
Genetic status of the host
5084
SALMONELLA
/Salmonellosis

0006 Illness usually occurs 7–10 days after consumption
of infected water or food, and the initial symptoms
tend to be both vague and variable. Headaches tend
to be common, as does a general feeling of lethargy,
along with abdominal pain/discomfort, and constipa-
tion is more usual than diarrhea. The fever increases
progressively during the first week, and then de-
creases, although a biphasic response may be seen.
Rose spots representing cutaneous vasculitis may be
seen on the abdomen and enlargement of the spleen
may be felt on abdominal palpation. The initial symp-
toms resemble those of acute gastroenteritis and Sal-
monella may be isolated from the feces. Then for a
week or more the organism may not be isolated from
the feces, although blood cultures are positive. This is
then followed by further fecal shedding. In about
25% of patients Salmonella may be isolated from
the urine. Fatalities usually arise from perforation
of the intestine after the bacteria have been localized
in the Peyer’s patches, and/or pneumonia, but other-
wise the disease runs a slow course over 5–6 weeks
and then leaves the patient in a longer period of
gradual convalescence.
0007 The pathogenesis of the disease is of interest. From
the small intestine the organisms pass via the lympha-
tics to the mesenteric lymph nodes, where, after a
period of multiplication, they invade the blood
stream via the thoracic duct and the liver, gall bladder,
spleen, kidney, and bone marrow become infected
during this bacteremic phase in the first 7–10 days of
the disease. From the gall bladder a further invasion
of the intestine occurs and lymphoid tissue, particu-
larly Peyer’s patches, are involved in an acute inflam-
matory reaction, followed by necrosis, sloughing, and
the formation of the characteristic typhoid ulcers.
Hemorrhage of varying degree may occur and, less
frequently, perforation through a necrotic Peyer’s
patch may complicate the illness and result in death.
S. typhi is present in large numbers in the inflamed
tissues in the ulcers and it may localize in the kidneys
and be found in other lesions that occur as a com-
plication or sequela of typhoid fever, e.g., acute sup-
purative periosteitis, renal and hepatic abscesses,
bronchopneumonia, and ulcerative endocarditis.
0008 In 2–5% of convalescents the organism persists in
the body, sometimes for an indefinite period, and in
such chronic carriers the organism is most commonly
found in the gall bladder or, more rarely, in the urin-
ary tract.
Diagnosis
0009 Typhoid fever should be suspected in any patient who
has visited an endemic area; the diagnosis is con-
firmed by recovering the organism from the feces,
urine, blood, or other tissues. Blood cultures are
positive in about 80% of patients and in the early
stages of illness, i.e., 7–10 days, it is the most reliable
diagnostic test. Bone marrow cultures and skin biop-
sies of rose spots are, however, more likely to be
positive for S. typhi than blood cultures. S. typhi
and paratyphi can be isolated from the feces through-
out the illness but are most frequently found during
the second and third weeks. Repeated examination of
the feces may be required before isolation is success-
ful. The tube agglutination test (Widal reaction) for
detecting antibodies to the somatic, flagellar H and
the envelope Vi antigen has been used for the sero-
logical diagnosis and positive titers occur about day
7–10 after infection. Occasionally positive titers de-
velop earlier, but they may be delayed and a negative
result at an early stage of the illness therefore may be
inconclusive (cross-reactions with other bacteria and
previous typhoid may give false-positive results).
Other serological tests, such as enzyme-linked immu-
nosorbent assays (ELISAs) have also been developed
to detect different antigens of the bacillus. Vaccin-
ation may give rise to false-positive serological reac-
tions and, if the patient has a history of vaccination, it
is advisable to take a second sample a week or so later
to determine whether there is a rising titer.
Chemotherapy
0010The treatment of enteric fevers necessitates the use
of antibacterial drugs. Chloramphenicol, ampicillin/
amoxicillin, trimethoprim/sulfamethoxazole are the
drugs of choice against sensitive Salmonella. Multiple
drug-resistant (MDR) isolates of S. typhi, resistant to
the first three antimicrobials (chloramphenicol, ampi-
cillin, and co-trimoxazole) have emerged in South-
east Asia and in 1998 in Kenya. Therapeutic options
include fluoroquinolones or azithromycin. Thus,
because MDRs of S. typhi have been reported, all
isolates should be tested for their antimicrobial sus-
ceptibility. Proper management of the fluid and elec-
trolyte balance is important in all patients, especially
the young and the old.
Immunoprophylaxis
0011Vaccines have been available for the prevention of
enteric fevers for many years. The classic inactivated
vaccine TAB protects against both typhoid and para-
typhoid A and B and extensive field trials in endemic
areas have shown a good degree of protection, al-
though a high percentage of vaccinates develop local
and systemic reactions.
0012In recent years, two new typhoid vaccines have
become available. A vaccine prepared from the Vi
capsular polysaccharide antigen has given good results
in field trials. One dose protects for 3 years and it has
a low incidence of side-effects. It is not licenced for
SALMONELLA
/Salmonellosis 5085

children less than 18 months of age because they may
have a suboptimal response.
0013 A live oral preparation produced from an attenu-
ated strain (Ty 21a) of S. typhi is available in enteric-
coated capsules; it is administered in three doses on
alternate days. Significant side-effects have not been
reported, but transient mild nausea, vomiting, ab-
dominal cramps, diarrhea, and urticaria may occur
in less than 1% of vaccinates. In mass trials it has not
proved as effective as the previous vaccines.
Acute Gastroenteritis
0014 Acute gastroenteritis is usually acquired from con-
sumption of foods which may have been directly or
indirectly contaminated with Salmonella. A wide
variety of animal species have been shown to be
capable of harboring the organisms without showing
clinical signs, and in the developed world, turkeys,
swine, chickens, and cattle have often been found to
be infected in abattoir studies. Animal products such
as milk and eggs have also been shown to be import-
ant vehicles of infection. Many other foodstuffs, in-
cluding vegetables and salads, have also been found
to be associated with Salmonella outbreaks. It should
also be remembered that person-to-person spread
may also be of importance.
Clinical Findings
0015 The incubation period ranges from 8 to 48 h
following the ingestion of contaminated food. The
most common symptoms are diarrhea, abdominal
pain, fever, and headache. Extremely fluid stools per-
sist for 3–4 days, and these may contain mucus and
occasionally blood. The temperature may be slightly
elevated in most patients but usually returns to
normal within 1–2 days. In the young and the elderly
the symptoms may be more severe and last for a week
or more.
0016 Salmonella gastroenteritis is usually a self-limiting
illness and fatalities are uncommon. Sigmoidoscope
and biopsy examinations have demonstrated that the
colon is the major site of infection. The changes in the
colon range from edema of the lamina propria with
a focal or diffuse inflammatory infiltrate to a more
intense inflammation with disruption of the surface
epithelium and multifocal microabscesses. In more
severe cases, edema, vascular congestion, infiltration
of the lamina propria with polymorphonuclear leuko-
cytes, and abscess formation have been recorded.
Chemotherapy
0017 Although Salmonella are usually sensitive in vitro to
many antibiotics, their use for the treatment of un-
complicated gastroenteritis until recently has generally
been contraindicated by the lack of favorable effect on
the course of disease and by a prolongation of Salmon-
ella shedding. Following the introduction of the fluor-
oquinolones, a number of clinicians have advocated
their use for the treatment of Salmonella gastroenter-
itis because of their efficacy in reducing the severity of
symptoms, the duration of illness, and Salmonella
shedding. However, this has been followed by increas-
ing development of resistance.
Salmonella Bacteremia (Septicemia)
0018A transient bacteremia may occur in patients with
gastroenteritis caused by Salmonella, although
periods of longer persistence occur in the blood of
individuals with one of the forms of enteric fevers or
those suffering from underlying disorders. Chronic
bacteremia is commonly associated with S. cholerae-
suis infection, and the fatality rate is usually two to
three times that caused by typhoid fever. Metastatic
infectious foci, of which the most important are intra-
vascular lesions, osteomyelitis, and meningitis, are
common complications of disease caused by S. cho-
leraesuis. This organism may lie dormant in some
tissues, usually bone marrow, and then later become
activated.
0019The serovar most commonly associated with bacter-
emia is S. typhimurium. This is perhaps not surprising
because it is the most frequent cause of salmonellosis
in humans and other animals. The high-grade bacter-
emia suggests the presence of focal intravascular infec-
tions in either the large arteries or the endocardium,
but whether this is a primary or secondary effect is
not certain. In sub-Saharan Africa, non-typhi Sal-
monella (NTS) are the most common isolates from
blood culture in children (< 50% of isolates). This is
not related to human immunodeficiency virus (HIV)
infection but occurs in the malaria season and espe-
cially in children with severe malarial anemia. In
HIV-infected adults NTS bacteremia is an early ac-
quired immunodeficiency syndrome (AIDS)-defining
illness: relapse after therapy commonly occurs.
0020Focal infections, such as osteomyelitis, arthritis,
and meningitis, are not uncommon sequelae to Sal-
monella infections. Any area of the skeleton, espe-
cially the long bones, may be invaded. Two types of
arthritis have been described: bacteremia may give
rise to suppurative arthritis with the organism in the
joint fluid, or a sterile inflammatory reaction involv-
ing the synovia may occur as a sequel in about 2.5%
of cases of gastroenteritis.
Chemotherapy
0021Chemotherapy is usually similar to that for typhoid
fever, although prolonged antibiotic therapy for
5086
SALMONELLA
/Salmonellosis
