Caballero B. (ed.) Encyclopaedia of Food Science, Food Technology and Nutrition. Ten-Volume Set
Подождите немного. Документ загружается.

boiling vegetables and discarding the water. It is not
possible to state an absolute amount for the advised
intake; 0.6–1 mmol kg
1
IBW will help to keep
the plasma levels below 5.5 mmol l
1
. The use of
potassium-losing diuretics and calcium resonium – a
potassium binder – may be appropriate.
Sodium and Water
0015 Kidney diseases such as diabetic nephropathy and
some forms of glomerular nephritis are characterized
by retention of sodium and water with resulting
hypertension and edema. However, interstitial neph-
ritis, e.g., chronic pyelonephritis, may initially pre-
sent with a failure to concentrate urine, leading to
sodium and water loss and potential dehydration.
The nonpharmacological approaches that have been
used to treat hypertension in the nonrenal population
may be of some benefit in the renal population: diet-
ary sodium restriction, weight control, and control of
other risk factors for coronary heart disease. Sodium
restriction also potentiates the action of ACE inhibi-
tors, diuretics, and b blockers. As the kidney loses its
ability to respond rapidly to changes in sodium
intake, any restrictions should be implemented grad-
ually. The dietary changes would include not adding
salt to cooking or at the table and reduction of
processed, tinned, or convenience foods. Comprom-
ises have to be made for the elderly patient who relies
on these foods as dietary staples. To improve the
palatability of the diet, a wide range of herbs and
spices can be used. The recommended level of restric-
tion is usually 80–100 mmol (1.8–2.3 g) of sodium
per day.
0016 Table 5 gives a summary of dietary advice for
conservative management (prior to starting RRT).
Other Nutritional Concerns
0017 Malnutrition A spontaneous decline in nutritional
intake has been recorded in patients approaching
ESRF. Unfortunately, loss of body weight is often
masked by increasing levels of fluid, giving the im-
pression that the weight is stable. A poor nutritional
state when the patient enters the dialysis program will
have a negative affect on morbidity and mortality,
so it is important to monitor these patients as they
approach ESRF irrespective of whether any dietary
restrictions have been advised.
0018Anemia The anemia of CRF has many causes, in-
cluding (1) decreased production of EPO, (2) poor
iron, folate or B
12
intake due to a low protein diet
or a poor appetite, (3) poor iron absorption due to
drug interactions, and (4) chronic blood loss due
to disturbed clotting mechanisms. Anemia contrib-
utes to extreme fatigue, loss of appetite, and taste
changes. Plasma levels of ferritin, hemoglobin, vita-
min B
12
, and red blood cell folate help determine the
need for iron, folate and B
12
supplements, and EPO
injections.
0019Hyperlipidemia Hyperlipidemia (raised cholesterol
and triglycerides) is a common complication of renal
failure. There is evidence in animal models that it may
increase the rate of progression of the disease, but this
has not been shown in humans except in the progres-
sion of diabetic nephropathy. There is, however, a
greatly increased risk of cerebro- and cardiovascular
disease, which accounts for 60% of deaths in renal
patients. HMG CoA (3 hydroxy, 3 methyl giutaryl
coenzyme A) reductase inhibitors are being used to
reduce cholesterol levels, and trials of fish oil supple-
ments are promising. Although diet and drug inter-
ventions have been shown to reduce risk factors,
including improving the lipid profile, as yet, there
have been no studies to show that this actually results
in decreased mortality in renal patients. Extrapolating
from the nonrenal population, it seems wise to en-
courage the principles of healthy eating, weight loss if
the body mass index is higher than 30, and regular
exercise.
tbl0005 Table 5 CRF diet (conservative management prior to ESRF)
Nutrient (recommended daily intake) Rationale
Protein 0.6–1.0 g kg
1
IBW As described in the text. With the lower-protein diet, the patient is given a meal
plan comprising HBV (60%) and LBV (40%) protein foods: to insure all the
amino acid requirements are met
Energy 35 kcal kg
1
IBW or use Schofield
equations, for example
Normal adult requirements. Calorie sources should not exacerbate
hyperlipidemia, i.e., total fat 30% of energy, low saturated fat. Encourage
good glycemic control in diabetics. NB: Monitor for signs of malnutrition
Phosphate 0.3–0.5 mmol kg
1
IBW Plasma levels should be maintained between 0.8 and 1.5 mmol l
1
.
Sodium 80–100 mmol per day. Fluid – no restriction
usually required
Salt restriction will help potentiate action of antihypertensives
Potassium 0.6–1 mmol kg
1
Levels should be maintained between 3.5 and 5.5 mmol l
1
. Restriction may not
be necessary until patient has reached ESRF
Vitamins and minerals May be required with lower protein diets and if potassium restriction is advised
4946 RENAL FUNCTION AND DISORDERS/Nutritional Management of Renal Disorders

Nephrotic Syndrome (NS)
0020 NS is characterized by proteinuria > 3 g per day,
hypoalbuminemia, edema, and hyperlipidemia. It is
usually also associated with hypertension. NS appears
as an additional complication in a number of types of
kidney disease (Table 6). Treatment involves antihy-
pertensive agents, immunosuppressants, diuretics,
salt-poor albumin, and dietary modifications.
Protein
0021 Historically, a high protein diet was advised on the
grounds that protein losses in the urine needed to be
replaced. However, studies comparing low (0.8 g
kg
1
) and high protein (1.5 g kg
1
) diets showed
that proteinuria was reduced with the lower protein
diets, although not all studies showed a correspond-
ing increase in plasma albumin levels. It has been
shown that a high protein intake causes increased
permeability and hyperfiltration in the basement
membrance of the kidney glomeruli, and this may be
the mechanism that explains the poor results of high
protein diets in NS. In addition, phosphate, lipid and
renin levels tended to improve on the lower protein
diets. An intake of 0.8–1 g of protein per kilogram per
day has been recommended.
Salt
0022 The kidneys tend to retain sodium and water in NS,
and patients benefit from a moderate dietary sodium
restriction: 80–100 mmol per day, and if edema is
present, a fluid restriction is also necessary. Sodium
restriction can potentiate the antihypertensive and
antiproteinuric effects of ACE inhibitors.
Fat
0023 Both triglycerides and cholesterol are raised in NS.
The incidence of myocardial infarction has been
reported as 5.5 times greater in NS compared with
normal. Lipid lowering agents are used in conjunc-
tion with standard lipid-lowering advice.
Micronutrients
0024 Iron, copper, zinc, and vitamin D are also lost as a
result of proteinuria. Vitamin D losses can result in
derangements of calcium metabolism, and supple-
mentation may be necessary.
Renal Replacement Therapy
Hemodialysis (HD) and continuous ambulatory
peritoneal dialysis (CAPD)
0025The nutritional problems of renal patients do not stop
once renal replacement therapy is started. Even with
dialysis, it is not possible to maintain body fluid,
potassium, and phosphate levels within the normal
ranges without some degree of dietary restriction. On
the positive side, some of the symptoms of uraemia
such as nausea, taste changes and gastrointestinal
disturbances improve. Usually, there is an increase in
appetite within 1 month of starting dialysis.
0026Dialysis itself has a number of negative effects on
the nutritional state (Tables 7 and 8). In addition,
some global factors affect the patient’s well-being:
.
0027The procedure itself is time-consuming, and travel-
ing to and from hospital for unit HD severely
disrupts the patient’s day, including meal times.
.
0028It is important that the risk of infections from the
procedures be minimized as the catabolic effects of
line infections and peritonitis can have long-term
consequences for the patient’s nutritional status.
.
0029Underdialysis – as measured by urea and creatinine
clearance – leads to impaired nutritional intake.
There are now set standards that describe the
amount of dialysis required in order to minimize
morbidity and mortality.
.
0030Depression can affect the patient for a number of
reasons: inability to keep full-time employment,
financial problems, body-image problems – as the
treatment can be disfiguring, restrictions on travel-
ing, dietary restrictions, and physical weakness due
to the long-term metabolic effects on bone and
muscle metabolism.
.
0031It is important to maintain normal hemoglobin
levels as anemia causes decreased appetite and
poor physical functioning. Injections of EPO and
iron are normally required to achieve this.
A team of professionals is necessary to treat the renal
patient and help them achieve the best quality of life.
In addition to medical and nursing staff, this should
include a dietitian, social worker, physiotherapist,
and counselor.
0032It is estimated that 30 – 70% of dialysis patients fall
into the moderate- to high-risk categories for malnu-
trition. Protocols for routinely assessing the nutri-
tional status of each patient must be in place in
order to identify problems early. Subjective global
assessment has been validated for use in dialysis
tbl0006 Table 6 Renal diseases which may develop nephrotic
syndrome
Glomerulonephritis
Diabetic nephropathy
Amyloidosis
Systemic lupus erythematosus
Vasculitis
Toxic glomerulopathy (gold, penicillamine)
RENAL FUNCTION AND DISORDERS/Nutritional Management of Renal Disorders 4947

patients; this combines medical history, including
dietary assessment, with a physical examination of
fat and muscle stores. There is a wide range of nutri-
tional supplements available for the first-line treat-
ment of malnutrition, and for the more severely
malnourished patient, gastrostomy feeding (HD and
CAPD) and intradialytic parenteral nutrition (IDPN)
in HD patients have been used successfully. An amino
acid containing CAPD solution is available and may
be of use in certain cases of hypoalbuminemia caused
by a persistent low protein intake.
0033 The dialysis diet should be tailored to the individ-
ual patient taking into consideration their medical
treatment and psychosocial factors. It is also guided
by regular monitoring of biochemical profiles that
usually occur monthly for HD and every 2 months
for CAPD patients. For the well-nourished patient,
healthy eating principles should continue to be
encouraged within the constraints of the potassium
restriction.
Transplantation
0034The positive effects of transplantation are to relieve
the patient from dietary and other lifestyle restric-
tions imposed by dialysis, and the patient experiences
a general improvement in well-being. This in itself
can lead to large gains in body weight as the patient
eats more in general. In addition, the immuno-
suppressive therapy can exacerbate the long-term
metabolic effects of CRF such as bone disease, muscle
tbl0007 Table 7 HD diet
Nutrient (recommended daily intake) Rationale
Protein 1.1–1.3 g kg
1
IBW From nitrogen balance studies (although numbers were small and may not
be applicable to all ethnic groups). 8–12 g of amino acids lost per dialysis.
Possible poor intake on dialysis days
Energy 35 kcal kg
1
IBW or use Schofield equations. Normal adult requirements. 25 g of glucose lost if glucose free dialysate is
used
Phosphate 0.5 mmol kg
1
IBW Plasma levels should be maintained between 1.2 and 1.7 mmol l
1
.
Phosphate is not well dialyzed, so restriction is necessary, aided by
phosphate binders
Sodium 80–100 mmol per day. Fluid 500 ml þ previous
day’s urine output
Urine output decreases once dialysis starts. Salt restriction will help
prevent thirst. Maximum of 2 kg interdialytic weight gain recommended.
Fluid overload leads to left ventricular heart disease and hypertension
Potassium 1 mmol kg
1
Plasma levels should be maintained between 3.5 and 6.5 mmol l
1
tbl0008 Table 8 CAPD diet
Nutrient (recommended daily intake) Rationale
Protein 1.2–1.5
a
gkg
1
IBW From nitrogen balance studies (although numbers were small, and
nitrogen balance was achieved at lower levels in some individuals).
9 g of protein/amino acids lost per day.
Energy 25–30 kcal kg
1
IBW þ energy from dialysate or
use, e.g., Schofield equations
Normal adult requirements. 70% of glucose is absorbed from the ‘bag’
of dialysate fluid. This can provide 300–1000 calories per day,
depending on the glucose concentration in the bag. This leads to
hypertriglyceridemia, obesity, and poor glycemic control in diabetics
Phosphate 0.5 mmol kg
1
IBW Plasma levels should be maintained between 1.1 and 1.6 mmol l
1
.
Phosphate is not well dialyzed, so restriction is necessary, aided by
phosphate binders
Sodium 80–100 mmol per day. Fluid 500 ml þ previous
day’s urine output. Additional fluid may be taken if
the patient ultrafiltrates (removes fluid during
dialysis) well
Urine output decreases once dialysis starts. Salt restriction will help
prevent thirst. Overdrinking leads to overuse of the higher sugar
containing bags of dialysis fluid and the problems described above
Potassium *1 mmol kg
1
IBW Levels should be maintained between 3.5 and 5.5 mmol l
1
. As dialysis
is continuous, hyperkalemia is less of a risk than on HD. The diet can
be more varied with respect to high-potassium foods
Vitamins (HD and CAPD) There is no consensus on the routine use of vitamins. Folate, pyridoxine,
and vitamin C levels are reported to be low without supplementation.
Folic acid supplements may also reduce homocysteine (risk factor for
CVD). Fat-soluble vitamins are not supplemented, except vitamin D,
as discussed earlier.
a
Larger protein requirements applicable during peritonitis.
4948 RENAL FUNCTION AND DISORDERS/Nutritional Management of Renal Disorders

wasting, and cardiovascular disease. The main aims
of dietary therapy are to reduce the risk factors for
cardiovascular disease, which is the cause of 60% of
deaths in transplant patients. All the aspects of
‘Healthy Eating’ should be encouraged. Patients may
be reluctant at first to increase their intake of fruits
and vegetables and even oily fish, as these would have
been restricted on the dialysis diet. Intensive dietary
counseling prior to discharge with regular follow up
in outpatient clinics has been shown to reduce the
average weight gain from 12 to 6 kg in the first year.
Lipid levels can also be improved with advice on
appropriate fat and sugar intake. An increasing
amount of literature is showing that encouraging
exercise at all stages of renal disease helps to improve
physical mobility, and extrapolating from the nonre-
nal population may further reduce risk factors for
CVD.
Acute Renal Failure (ARF)
0035 ARF can be defined as an abrupt decline in renal
function. Initially, there is oliguria (< 400 ml per day)
or anuria, retention of the end products of protein
metabolism, acidosis, and electrolyte imbalance. Bio-
chemical profiles show a rapid increase in urea and
creatinine, and also potassium and phosphate levels
can increase. ARF is usually reversible, and as renal
function returns, there may be polyuria to an extent
where potassium and phosphate levels can drop
below normal, and salt and water depletion can
occur. As the causes of ARF are so varied, the effect
on nutritional requirements may be negligible or, in
the case of severe trauma or sepsis, cause a hypercata-
bolic state. Protein and energy requirements are cal-
culated using standard formulae and stress factors
and are related to the underlying causes. ARF in itself
has specific effects on protein, fat, and carbohydrate
metabolism, but the literature is less clear about how
this impacts on the final nutrient prescription. ARF
can be divided into three categories:
1.
0036 Noncatabolic: nontraumatic causes such as
obstruction and interstitial nephritis from drugs.
2.
0037 Catabolic: postsurgery, rhabdomyolysis, and
hemolytic uremic syndrome.
3.
0038 Hypercatabolic: major trauma (road traffic acci-
dent), burns, and sepsis.
Noncatabolic ARF
0039 As in CRF, the aims of treatment are to slow down the
build-up of uremic toxins and fluid overload in order
to prevent or alleviate symptoms, to maintain good
nutritional status, and to prevent weight loss. Dialysis
may or may not be necessary. Nausea and lack of
appetite are common features, and the main concern
is insuring the patient is meeting their nutritional
requirements sometimes with the help of dietary sup-
plements. Restriction of dietary protein < 0.8 g protein
per kilogram is not recommended. It is usually accept-
able to aim for a ‘normal’ protein intake of 1 g per
kilogram IBW per day. Advice on salt intake – aiming
for 80–100 mmol per day, fluid restriction – 500 ml
plus PDUO (previous days urine output) and potas-
sium restriction < 1 mmol kg
1
may be necessary.
In practice, all that is usually required is a simple
diet sheet advising the patient and their relatives on
suitable snacks and drinks. The usual ‘treats’ that
people receive in hospital, i.e., fruit juice, fruit, and
chocolate, may not be acceptable. High plasma
phosphate levels can be controlled by phosphate
binders.
Catabolic and Hypercatabolic ARF
0040The patient will almost certainly require dialysis
treatment as the rate of production of waste products
will otherwise cause severe and potentially fatal
uremia. The type of dialysis will also affect nutrient
requirements and the ability to provide them through
nutritional support. Intermittent HD may be suf-
ficient in noncatabolic or moderately catabolic
patients, but as the severity of catabolism increases,
continuous dialysis may be required, e.g., continuous
arteriovenous HD (CAVHD). Losses of 9–13 g of
protein per day can occur with this therapy. With
1.5% glucose in the dialysate solution, there is a net
gain of glucose of 6 g h
1
, which represents an energy
intake from dialysis of 550 kcal per day. The effects
of dialysis on nutrient losses and gains should be
taken into consideration when prescribing the feeding
regimen.
0041Protein requirements Catabolic patients require in
the region of 9–14 g of nitrogen (56–87 g of protein)
per day. Hypercatabolic patients may break down up
to 40 g of nitrogen (235 g of protein) per day, but the
liver cannot deaminate more than 20 g of nitrogen
(117 g of protein) per day, so this is the maximum
that can be replaced by nutritional support.
0042Carbohydrate Glucose utilization is limited by ARF,
and excessive amounts can cause lipogenesis, fatty
liver, and increased carbon dioxide production. Pro-
vision of carbohydrate should not exceed the max-
imum oxidation rate of 4 mg per kilogram IBW per
minute.
0043Fat As the metabolism of fat is impaired in ARF, an
upper limit of 1 g of fat per kilogram per day is
recommended.
RENAL FUNCTION AND DISORDERS/Nutritional Management of Renal Disorders 4949

0044 Fluid and electrolytes With intermittent HD, a feed-
ing regimen containing reduced fluid, sodium, and
potassium may be necessary and may limit the macro-
nutrient provision from an enteral or parenteral
feed. Continuous dialysis and ultrafiltration obviate
the need for a fluid (and usually also electrolyte)
restriction.
0045 Phosphate Hyperphosphatemia is a common fea-
ture of ARF, and initially, TPN (total parenteral nu-
trition) regimens can be phosphate-free. Anabolism
and dialysis will lower serum phosphate, and the
requirements would be reassessed at this stage.
0046 Vitamins and minerals Requirements for micro-
nutrients are not well documented. Water-soluble
vitamins tend to be given daily in the standard
amounts and trace elements given only once or
twice a week. Fat-soluble vitamins are not required
in the short term.
Renal Stone Disease (Nephrolithiasis)
0047 Renal stone formation occurs as a result of increased
urinary concentration of promotor substances and
decreased concentration of inhibitor substances
(Table 9). This is partly influenced by dietary factors
but can also be linked to congenital abnormalities, as
seen in polycystic kidneys, horseshoe kidneys, and
medullary sponge kidney or to short bowel syn-
dromes such as Crohn’s disease. The stones vary in
composition, but the main types include combin-
ations of calcium, oxalate, and phosphate. The size
of the stones can vary from microscopic to the large
‘staghorn’ calculi, and can lead to kidney failure if the
kidney or urinary tract becomes obstructed.
0048 A number of dietary factors can contribute to the
management of stone disease.
Fluid
0049 An adequate fluid intake of 2–3 l a day is encouraged
to ensure a minimum urine output of 2 l per day.
Specifically, patients are told to drink 250 ml every
four waking hours, with 250 ml at meals. Compliance
with this single measure has been shown to reduce
new stone formation by diluting the concentration of
stone-forming salts, and may prevent new stone for-
mation in up to 60% of patients with ideopathic
calcium urolithiasis.
Calcium
0050Forty to 50% of people who develop stones have a
higher level of calcium in the urine (daily excretion
> 4 mg kg
1
, although absolute amounts are also
relevant).
0051There are a number of dietary factors that can
cause hypercalcuria:
.
0052excessive intake of calcium or vitamin D particu-
larly as supplements;
.
0053high salt intake; and
.
0054high protein intake, particularly from animal
protein.
The ideal level of calcium intake has not been ascer-
tained – what is known is that a low dietary intake of
calcium will exacerbate intestinal absorption of oxal-
ate and promote stone formation. In a number of
patients, a low calcium diet will also escalate an
underlying tendency to osteoporosis. Intake of cal-
cium supplements, however, is associated with an
increased risk of stone formation, and therefore, on
balance it is advisable to aim for the normal reference
nutrient intake for calcium (700–800 mg per day)
from diet, not supplements. There is also evidence
showing that calcium excretion increases with
sodium intake and protein intake. A moderate intake
of no more than 100 mmol of sodium per day is
recommended, and 1 g of protein per kilogram of
body weight is thought to be appropriate.
Oxalate
0055Calcium oxalate stones account for up to 75% of
stones formed. Oxalate is mostly formed endogen-
ously; only 10% comes from the diet, although the
proportional change in excretion is quite significant
if calcium intake is decreased or oxalate intake
increases. Therefore, it still helps to avoid or reduce
intake of high oxalate foods such as tea, rhubarb,
beetroot, chocolate, cocoa, nuts, spinach, and straw-
berries. American sources also name gooseberries,
sweet potato, leek, parsley, okra, and wheat bran.
Unfortunately, there are no comprehensive lists of
oxalate-containing foods and their bioavailability.
High vitamin C intake increases oxalate production,
although the doses stated are in excess of 1 g per day.
0056Other dietary factors that may have a role are
dietary fiber and phytates, which reduce the amount
of calcium absorbed by the gut, but this may then
increase the amount of oxalate absorbed.
tbl0009 Table 9 Risk factors for renal stones
Low urine volume particularly < 1000 ml per day
High urinary concentrations of:
Calcium
Oxalate
Low urinary concentrations of:
Citrate
Urine acidity
4950 RENAL FUNCTION AND DISORDERS/Nutritional Management of Renal Disorders
Uric Acid
0057 Uric acid excretion is involved in calcium and also uric
acid stone formation. Uric acid is an end product of
purine metabolism, and dietary restriction of purines
and animal protein will reduce its urinary excretion.
Purine-rich foods include liver, kidney, brain, ancho-
vies, sardines, herring, mackerel, mussels, scallops,
goose, partridge, and yeast.
0058 In summary, stone formation is multifactorial, so in
order to give appropriate dietary advice, it is neces-
sary to have an analysis of the stone composition and
urinary concentrations of the risk factors (Table 9). It
is then necessary to take a detailed diet history in
order to identify excesses or deficiencies or general
trends in dietary intake.
See also: Calcium: Physiology; Energy: Intake and Energy
Requirements; Hyperlipidemia (Hyperlipidaemia);
Malnutrition: The Problem of Malnutrition; Phosphorus:
Physiology; Potassium: Physiology; Protein:
Requirements; Sodium: Properties and Determination;
Vitamins: Overview; Water: Physiology
Further Reading
Brown MA and Whitworth JA (1992) Hypertension in
human renal disease. Journal of Hypertension 10:
701–712.
Engel B et al. (1998) Setting Standards and Achieving
Optimal Nutritional Status. Birmingham, UK: British
Dietetic Association.
Giovannetti S (1989) Nutritional Treatment of Chronic
Renal Failure. Dordrecht: Kluwer Academic.
Greenberg A (1994) Primer on Kidney Diseases. London:
Academic Press.
K/DOQI (2000) Clinical practice guidelines for nutrition in
chronic kidney failure. American Journal of Kidney
Diseases 35(6) (supplement 2): s1–s137.
Lazarus JM (1993) Nutrition in haemodialysis patients.
American Journal of Kidney Diseases 21(1): 99–105.
Levey AS (1998) Controlling the Epidemic of CVD in CRD.
USA: National Kidney Foundation.
Levey AS, Adler S, Gaggiula AW et al. (1996) Effects of
dietary protein restriction on the progression of ad-
vanced renal disease in the modification of diet in renal
disease study. American Journal of Kidney Diseases
27(5): 652–663.
McCann L (1996) Subjective global assessment as it
pertains to the nutritional status of dialysis patients.
Dialysis and Transplantation 25(4): 190–225.
Massy ZA, Jennie Z et al. (1995) Lipid lowering therapy in
patients with renal disease. Kidney International 48:
188–198.
Mitch W and Klahr S (1998) Handbook of Nutrition and
the Kidney, 3rd edn. Philadelphia, Pennsylvania, USA:
Lippincott-Raven.
RCP and Renal Association (1997) Treatment of Adult
Patients with Renal Failure: Recommended Standards
and Audit Measures 2nd edn. UK: Royal College of
Physicians and Renal Association, Lavenham Press.
Smith CL, Davis M and Berkseth RO (1992) Dietary factors
in calcium nephrolithiasis. Journal of Renal Nutrition
2(4): 146–153.
Toigo G, Aparicio M, Altman PO et al. (2000) Expert
Working Group Report on nutrition in adult patients
with renal insufficiency. Clinical Nutrition 19(3):
197–207.
Rennin See Cheeses: Types of Cheese; Starter Cultures Employed in Cheese-making; Chemistry and
Microbiology of Maturation; Manufacture of Extra-hard Cheeses; Manufacture of Hard and Semi-hard Varieties of
Cheese; Cheeses with ‘Eyes’; Soft and Special Varieties; White Brined Varieties; Quarg and Fromage Frais;
Processed Cheese; Dietary Importance; Mold-ripened Cheeses: Stilton and Related Varieties; Surface Mold-
ripened Cheese Varieties
Residue Determination See Antibiotics and Drugs: Uses in Food Production; Residue Determination;
Contamination of Food; Fumigants; Pesticides and Herbicides: Types of Pesticide; Types, Uses, and
Determination of Herbicides; Residue Determination; Toxicology
Resistant Starch See Starch: Structure, Properties, and Determination; Sources and Processing;
Functional Properties; Modified Starches; Resistant Starch
RENAL FUNCTION AND DISORDERS/Nutritional Management of Renal Disorders 4951
RETINOL
Contents
Properties and Determination
Physiology
Properties and Determination
D C Woollard, AgriQuality NZ, Auckland, New Zealand
H E Indyk, Anchor Products, NZMP, Waitoa,
New Zealand
Copyright 2003, Elsevier Science Ltd. All Rights Reserved.
Physical Properties
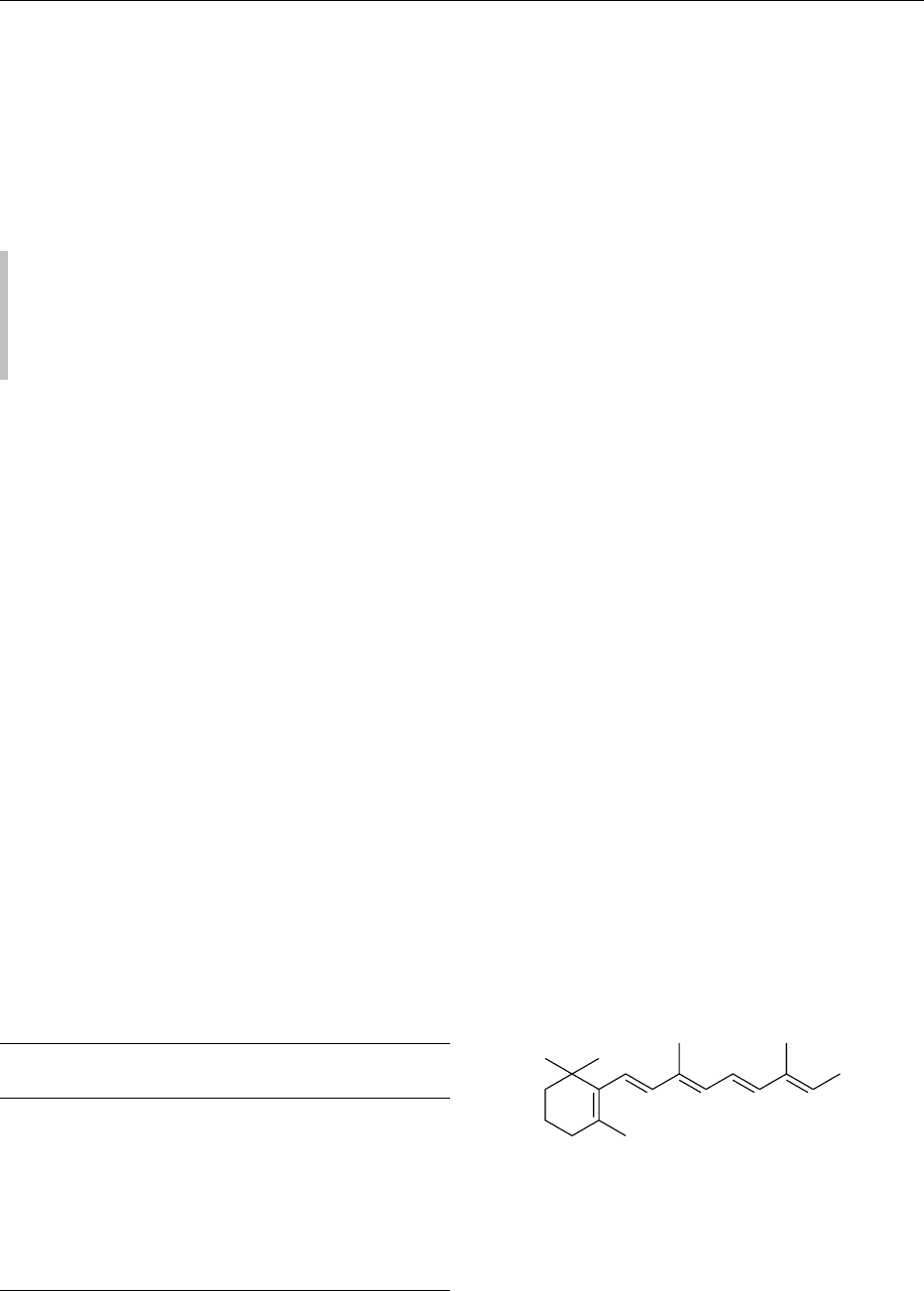
0001 Retinol (9,13-dimethyl-7-[1,1,5-trimethyl-6-cyclo-
hexene-5-yl]-7,9,11,13-nonatetraene-15-ol) is a pale
yellow crystalline powder or oily mass, depending on
purity. It is insoluble in water but readily miscible
with most organic solvents. Its formula, formula
weight, and certain other characteristic physical
properties are summarized in Table 1, along with
those of the two commercially significant ester
derivatives.
Chemical Properties
0002 All-trans retinol, considered the parent compound of
the vitamin A group, is a complex unsaturated alco-
hol. Its trivial name originated with the historical
recognition of its role in vision. This generic structure,
illustrated in Figure 1, shares a common b-ionone
ring, with attached conjugated isoprenoid side chain.
0003 Chemical and structural modifications to the ring,
side chain, or polar functional group generate many
retinoids possessing a wide spectrum of properties. In
nature only relatively few of these compounds exhibit
significant vitamin A activity. These include the pre-
dominant all-trans forms of retinol (originally desig-
nated vitamin A
1
) and its esters, retinal, retinoic acid,
and their associated 9-, 11-, and 13-cis isomers. The
cis-isomers are selectively interconvertible with the
trans-forms in the body and thereby express frac-
tional biological activities of approximately 0.25,
0.50, and 0.75, respectively, relative to the all-trans
vitamer. Some marine and fresh-water fish contain
significant quantities of the cyclic diene 3-dehydro-
retinol (originally designated vitamin A
2
), which
possesses approximately 40% of the bioactivity of
all-trans retinol.
0004Vitamin A activity is commonly expressed in inter-
national units (1 IU is equivalent to 0.300 mg all-trans
retinol, 0.344 mg retinyl acetate, or 0.549 mg retinyl
palmitate), or, more recently, retinol equivalents
(1 RE is equivalent to 1.0 mg all-trans retinol). Such
units have been useful in nutritional studies where
contributions from numerous vitamin A active con-
geners may be combined to yield a single value. For
the food scientist, it is probably more appropriate to
express vitamin A content as the summation of each
retinoid, in absolute mass units (usually mg).
0005The dominant structural feature of retinol is the
extensive conjugated double-bond system, to which
many of the physicochemical and biological proper-
ties may be attributed. It is also the principal factor
in the lability of vitamin A. Thus, retinol and its
derivatives are particularly sensitive to oxidizing
conditions and are rapidly destroyed by heat, light,
tbl0001 Table 1 Physical properties of retinol (all-trans) and its esters
Property Retinol Retinyl
acetate
Retinyl
palmitate
Formula C
20
H
30
OC
22
H
32
O
2
C
36
H
60
O
2
Formula weight 286.46 328.50 524.88
Melting point (
C) 63–64 57–59 28–29
l
max
(nm)
a
325 326 326
Extinction coefficient, E
1%
1cm
1820 1530 960
Molar absorptivity, e 52 140 50 260 50 390
Fluorescence
Excitation max. (nm) 325 325 325
Emission max. (nm) 470 470 470
a
In 2-propanol. Spectral properties vary slightly between protic and
aprotic solvents.
17 16
19 20
11 13 R97
1
4
2
3
6
18
1081214
15
5
fig0001Figure 1 Structures of the basic retinoids. The cis-isomer
positional variants are indicated by the side-chain numbering
system.
R¼CH
2
OH all-trans retinol
CH
2
OCOCH
3
all-trans retinyl acetate
CH
2
OCO(CH
2
)
14
CH
3
all-trans retinyl palmitate
CHO all-trans retinal
COOH all-trans retinoic acid
4952 RETINOL/Properties and Determination
and acids when in solution. Isomerization, oxidation
and, ultimately, molecular cleavage may all occur
concurrently, depending on the extent of environ-
mental stress. Cleavage may result in the formation
of volatile b-ionone fragmentation products which
have importance in the development of off-flavor in
some foods. Retinol is, however, relatively resistant
towards alkali, and most degradation processes are
minimized if it is maintained under inert gas at low
temperature and in the absence of short-wavelength
light.
0006 In solution, several fat-soluble antioxidants offer
protection, while in foods and food extracts, accom-
panying lipids and endogenous antioxidants such
as phospholipids, tocopherols, and carotenes act
to stabilize retinol until they are sacrificially depleted.
Both thermal processing and storage expose vitamin
A in foods to the risks of considerable loss (5–40%),
although published data are often highly variable.
(See Antioxidants: Natural Antioxidants.)
0007 Retinyl esters are considerably more stable than
the parent alcohol, a feature which is exploited in the
principal commercial formulations available to the
food industry. Although minor differences in absorp-
tion efficiency have been reported, dietary retinyl
esters are considered to exhibit identical biological
activities as a result of their conversion to retinol in
the intestinal wall.
Occurrence and Forms in Foods
0008 All forms of vitamin A found in foods ultimately
derive from the provitamin A carotenoids, which are
ubiquitous in the higher plants and lower animal
organisms. Humans obtain preformed vitamin exclu-
sively from animal sources, while carotenoids are
gained from foods of both plant and animal origin.
0009 Retinol and its derivatives are not widely distrib-
uted in foods. Fish liver oils are by far the most
concentrated natural source, while animal liver, milk
(and dairy products), and eggs contain significant
quantities. The average western diet is generally
assessed as satisfying the recommended daily intake
level of 1000 RE total vitamin A, with about 25%
supplied by b-carotene. (See Carotenoids: Occur-
rence, Properties, and Determination; Physiology.)
0010 Retinoids in foods occur mainly as mixtures of
retinyl esters, with lesser contributions from retinol
itself. The predominant forms are long-chain esters,
notably palmitate, with contributions from stearate
and oleate. However, eggs are an exception, where
unesterified retinol is the major form. Certain foods
also contain contributions from retinal (eggs and
fish roe) and cis-isomers (mainly 13-cis), the latter
particularly in foods subjected to processing.
0011Vitamin A deficiency is one of the prevalent diet-
related issues and has received global attention.
Consequently, nutritional tables are replete with
information regarding retinol distribution in foods.
Table 2 lists the vitamin A content of a few represen-
tative foods. Carotenoid-rich vegetable sources are
not included. Refer to individual foods.
Use in Food Fortification
0012Increasing the vitamin A intake amongst populations
at risk of retinol deficiency is a simple expediency and
has been employed for several decades, both prophyl-
actically and therapeutically. Many of the specific
symptoms of severe deficiency (e.g., xerophthalmia,
keratomalacia) are usually reversible, provided other
nutritional criteria are similarly satisfied. In the
developed nations, potential risks of subclinical defi-
ciency are also avoided through food enrichment,
thereby insuring satisfactory intake. (See Food
Fortification.)
0013Fat-based foods such as margarine, milk, and
infant formula provide an ideal carrier in which to
supply supplemental vitamin A. Dried milk, by
reason of cost and convenience, is globally the pre-
ferred foodstuff and additionally offers a high-quality
protein and mineral enrichment medium appropriate
to nutritional rehabilitation programs. An increasing
range of alternative food items are being used as
carriers, ranging from specialized dietary beverages
to breakfast cereals.
0014In most cases, supplementation is performed with
synthetic all-trans retinyl acetate or palmitate. The
esters in the case of margarine are usually added
directly in an oil carrier, often in the presence of
appropriate antioxidants. Where additional stability
is required, or when dried food products are involved,
it is common practice to use a powder preparation
in which vitamin A (and stabilizer) is deposited in
a suitable carrier, such as gelatin carbohydrate,
although alternatives (e.g., acacia gum) have re-
cently been developed. However, uneven vitamin
tbl0002Table 2 Preformed vitamin A content of selected foods,
expressed as retinol
Food Retinolcontent (range) of
edibleportion (mg100g
1
)
a
Milk 32–45
Butter 800–1000
Eggs 140–250
Beef 2–5
Liver (lamb) 7000–10 000
Mackerel 25–50
Cod liver oil 15 000–30 000
a
To convert to IU per 100 g, multiply by 3.33.
RETINOL/Properties and Determination 4953

distribution is a common problem when dry-blending
food products.
0015 Water-miscible vitamin A powders have been de-
veloped containing emulsifiers that facilitate reconsti-
tution into aqueous solution. These solutions can
then be processed directly into fluids such as milk
prior to drying. Using the wet-blending technique,
the protective environment of the additive is hope-
fully substituted by intimate interaction with the lipid
phase of the finished food. The principal advantage of
this supplementation route is an enhanced vitamin
homogeneity in the finished product. However, the
added ingredients are generally found to be less stable
than their endogenous counterparts. (See Emulsifiers:
Uses in Processed Foods.)
0016 During food storage there are significant advan-
tages in using packaging which provides effective
oxygen and light protection. The use of cans allows
nitrogen purging of the head space, thereby greatly
enhancing the oxidative stability of the food and
extending its shelf-life, particularly in developing
countries with extreme climates.
Extraction and Clean-up
0017 During analytical procedures, precautions are man-
datory to exclude exposure of vitamin A to ultraviolet
radiation, thermal, and oxidative stresses. Protective
antioxidants and exclusion of air are essential to the
success of the analysis. Purity of vulnerable retinoid
standards is important during quantitative investiga-
tions, and spectrophotometric procedures are gener-
ally necessary to ascertain accurately their purity
concentration.
0018 Alkaline digestion (saponification) is most com-
monly employed as the first stage during analysis of
retinol in foods. A representative sample is homogen-
ized and digested in ethanolic potassium hydroxide or
similar media. Saponification has the threefold effect
of eliminating the bulk of lipid materials, releasing
the vitamin from within the sample, and converting
the various esters into free retinol. The procedure can
be performed under reflux temperatures, or at ambi-
ent temperature (for longer periods), the details of
which are determined by the sample matrix. In some
food samples where the vitamin A concentration may
be low, a preliminary fat extraction step will assist in
achieving the required assay sensitivity.
0019 Retinol is partitioned from the digest into a binary
organic solvent, commonly consisting of hexane and
a polar modifier such as an ether. The solution is
washed with water, dried, and usually concentrated
by evaporation, to provide a crude extract. Direct
spectrophotometric or fluorometric assay of retinol
may be impractical in poorly characterized foods,
owing to interfering coextractives, and further clean-
up is often necessary. Traditionally this has been
achieved by open-column or thin-layer chromatog-
raphy, using silica or alumina stationary phases,
while gel-permeation chromatography has also been
advocated. The laborious nature of these clean-up
techniques has largely been overcome through the
online automated use of prepacked, solid-phase
extraction columns.
0020As the majority of native and supplementary
retinol in foods exists in esterified form, there are
analytical advantages to be gained through avoiding
preliminary saponification, providing the nature of
the food allows such simplified methodology. The
total lipid fraction of such foods may therefore be
directly extracted into organic solvent, which is then
ready for analysis of the intact esters. Advantages
include a reduction in the number of manipulative
steps and the decreased risk of analyte loss through
retinol degradation.
Chromatographic and Other Methods of
Determination
0021The detection of retinol is based on its extensive
conjugated double-bond functionality, which pro-
vides an intense and relatively specific chromophore
in the long-wavelength ultraviolet region. The sensi-
tivity and selectivity of spectral analysis are conse-
quently enhanced, irrespective of the separation
techniques used. In addition, retinol exhibits a strong
fluorescence which offers selectivity advantages and
often reduces the need for preliminary clean-up. In
situations involving well-characterized foods, and
where discrimination between retinol and related
compounds is unnecessary, spectrophotometric or
fluorometric measurement of the crude extracts can
often supply a reliable estimate, providing the limita-
tions of such strategies are recognized. (See Spectros-
copy: Fluorescence.)
0022The traditional Carr–Price method for determin-
ation of retinol in foods has exploited the reaction
with antimony trichloride to produce a blue complex
in direct proportion to vitamin A concentration. Al-
though the color is transient and difficult to control,
the reaction is still employed in laboratories with
limited access to modern chromatographic instru-
mentation. Other Lewis acids, notably trifluoroacetic
acid, will react in a similar way and offer some ma-
nipulative advantages over the Carr–Price approach.
0023It is now accepted that a reliable estimate of vitamin
A content in foods is best achieved through exploiting
chromatography to separate coextracted substances
and, in particular, to differentiate the active retinoid
species. Most variants of chromatography have been
4954 RETINOL/Properties and Determination
used during attempts to separate and quantify the
retinoids. Thin-layer chromatography (TLC) and
low-pressure liquid chromatography, while reason-
ably successful, have traditionally lacked the resolv-
ing power for reliable quantitative measurements,
although high-performance TLC shows potential.
Gas-liquid chromatography has not been widely util-
ized, as retinol (and its esters) degrades at elevated
temperatures. The use of high-performance liquid
chromatography (HPLC) has dominated vitamin
A measurement over the last 20 years and has been
largely responsible for the rapid proliferation
of knowledge regarding this vitamin. This non-
destructive technique facilitates a rapid analysis with
minimum sample preparation. Recently, variants of
micellar capillary electrophoresis (CE) have been
applied to fat-soluble vitamin separations. Although
representing an alternative to HPLC techniques,
the application of CE to the hydrophobic vitamins
iscurrently in its infancy. (SeeChromatography: High-
performance Liquid Chromatography; Thin-layer
Chromatography; Gas Chromatography.)
0024 Since isomerization can be a common phenomenon
during food production, cis and trans differentiation
may be required, with the application of appropriate
factors to account for their selective bioactivities.
In addition, inactive oxidation products such as
oxyretinoids, epoxyretinoids, and their fragmentation
products, as well as various retroretinoids, can exist in
many food samples. Published literature is available
for the determination of retinol isomers and esters,
3-dehydroretinol, retinal, and retinoic acid in a wide
variety of foods. These analyses are accomplished
using normal- or reversed-phase HPLC, often with
simple isocratic solvent systems. Normal-phase is
generally the more efficient mechanism for isomer
separations, while esters are best resolved under re-
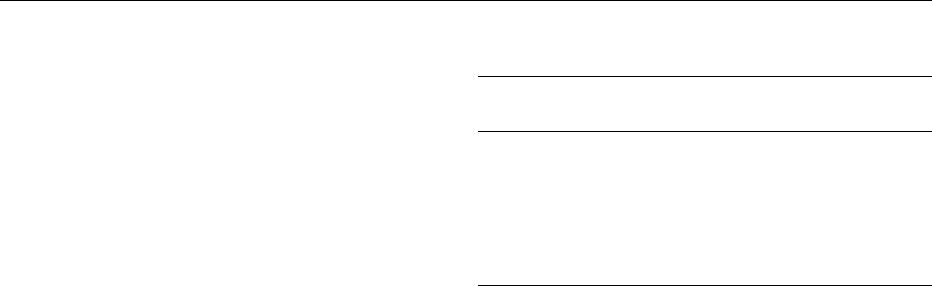
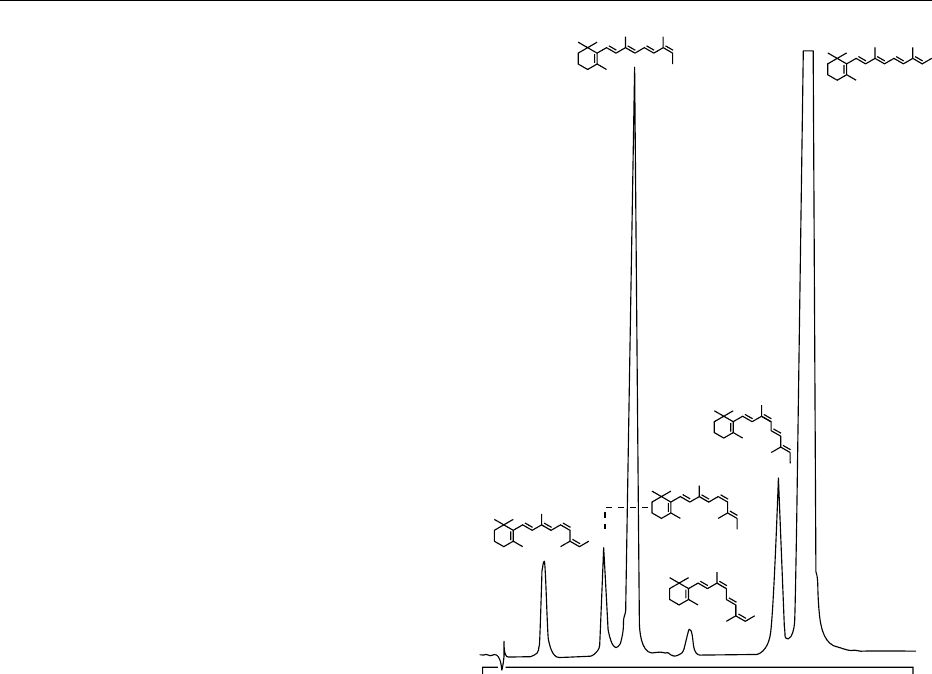
versed-phase conditions. Figure 2 illustrates the iso-
meric distribution in a saponified sample of cod liver
oil utilizing normal-phase conditions.
0025 The estimation of retinal and retinoic acid in foods
is not frequently required. They exist in some foods as
metabolites of the live animal but their contribution
to the vitamin A pool is negligible compared to that of
retinol. Despite the occurrence of 3-dehydroretinol in
fish and particularly fish liver oils, retinol remains the
primary source of vitamin A owing to its higher bio-
potency. Thus retinol, and its esters, are generally the
retinoids of major interest during routine food
analysis.
0026 The specific details of HPLC procedures used
for retinol analysis are too numerous to cover
comprehensively. However, there are several features
common to most schemes, notably the almost
universal use of ultraviolet (either dual-wavelength
or photodiode array) or fluorescence detection. Both
electrochemical and mass spectrometric detection
techniques have been reported but are not currently
in widespread use. Normal-phase separations are
generally performed on 5–10-mm particulate silica
columns, replacing the earlier use of alternative ad-
sorbents (alumina, keiselguhr, etc.). Amino-, cyano-
and diol-bonded silica is sometimes advocated to
circumvent the problems associated with moisture
on underivatized silica. The primary mobile-phase
component is usually a hydrocarbon in binary com-
bination with a polar organic modifier, although
ternary systems are sometimes recommended. Re-
versed-phase separations are usually confined to C
18
bonded-phase columns, although other hydrophobic
derivatives are sometimes used (C
2
,C
8
,C
30
,and
phenyl). Mobile phases are often a simple binary
1
3
6
2
4
5
0
Time (min)
15
fig0002Figure 2 A 1-g sample of commercially refined cod liver oil was
saponified with alcoholic potassium hydroxide and extracted into
hydrocarbon. A portion was analyzed by normal-phase high-
performance liquid chromatography using a Waters Radial-PAK
silica column with a mobile phase of hexane:2-propanol (96:4 v/v)
at 1.5 ml min
1
. Measurement was by fluorescence detection at
325 nm (excitation) and 470 nm (emission). Peak identification: 1,
11,13-di-cis-retinol; 2, 11-cis-retinol; 3, 13-cis-retinol; 4, 9,13-di-cis-
retinol; 5, 9-cis-retinol; 6, all-trans-retinol.
RETINOL/Properties and Determination 4955
