Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.


ENDOCRINE PROBLEMS IN THE CRITICALLY ILL PATIENT
567
Although the signs and symptoms of hyperthyroidism
suggest sympathetic overactivity, plasma levels and secretion
rates of epinephrine and norepinephrine are actually normal
in patients with thyroid storm. Because of this, increased
sensitivity to catecholamines has been suggested, and ele-
vated cAMP levels in these patients have been cited as evi-
dence of increased adrenergic activity.
The mechanisms that lead to the decompensated state
characteristic of thyroid storm have not been well studied.
Higher levels of cytokines and immune dysregulation have
been implicated, but without conclusive data. The basal
metabolic rate and thermogenesis are increased, and there is
a net degradation of proteins. Although both protein synthe-
sis and degradation are increased, hyperthyroidism results in
negative nitrogen balance, muscle wasting, and reduced
albumin concentrations. Although cortisol clearance is
increased, its production rates are also increased, so the cor-
tisol levels remain essentially unchanged. Thyroid hormones
have direct cardiostimulatory effects, resulting in tachycardia
and increased contractility. Increased thermogenesis results
in vasodilatation as part of the compensatory response to
increased body temperature.
Clinical Features
Thyroid storm is usually seen in patients with known hyper-
thyroidism but may be the presenting feature in a patient with
previously undiagnosed thyrotoxicosis. Thyroid storm is seen
often in association with one of a long list of precipitating
conditions, but the two most common conditions are surgical
procedures of any kind—but particularly thyroid surgery in
an uncontrolled or poorly prepared hyperthyroid patient—
and infections. Thyroid storm is now quite uncommon fol-
lowing thyroid surgery because of preoperative preparation
and control of hyperthyroidism with antithyroid drugs.
Other potential precipitating factors include cardiovascu-
lar disease (including acute myocardial infarction), systemic
illness, trauma, diabetic ketoacidosis, vigorous palpation of
an untreated hyperthyroid gland, administration of iodi-
nated contrast material, stroke, and preeclampsia or eclamp-
sia. Rare cases of thyroid storm have been seen after
amiodarone administration. Exacerbation of hyperthy-
roidism may occur following radioactive iodine treatment of
Graves’ disease, but thyroid storm is unusual because most
hyperthyroid patients are well controlled by antithyroid drug
therapy. In contrast, thyroid storm may occur in hyperthy-
roid patients who discontinue antithyroid medications pre-
maturely or inadvertently. Patients who accidentally or
deliberately ingest an excessive amount of thyroid hormone
may present with severe hyperthyroidism but usually with-
out the complete picture seen in thyroid storm.
A. Symptoms and Signs—Thyroid storm is characterized
by clinical features of severe thyrotoxicosis with fever and
altered mental status. In one series of patients hospitalized
for complicated thyrotoxicosis, cardiovascular complications
and neuropsychiatric syndromes were the two most frequent
indications for admission. Mental status changes may
include confusion, agitation, overt psychosis, and in extreme
cases, even coma. Common cardiovascular manifestations
include tachycardia that is out of proportion to fever, cardiac
arrhythmias (sinus or supraventricular tachycardia, includ-
ing atrial fibrillation), and congestive heart failure. Patients
presenting with congestive heart failure are usually elderly
and have an underlying history of heart disease. However, it
is well documented that hyperthyroidism can cause conges-
tive heart failure even in the absence of underlying heart dis-
ease. Hypotension and shock may be late manifestations. GI
manifestations include nausea, vomiting, diarrhea, and
abdominal pain. Weight loss and cachexia are common.
Goiter is almost always present and may be diffuse or
multinodular. Since many of these patients have Graves’ dis-
ease, the goiter is more often diffuse and nontender. Patients
often have marked muscle weakness owing to proximal
myopathy and generalized cachexia. Tremor is present. The
skin is warm, moist, flushed, soft, and “velvety.” The reflexes
may be brisk. Graves’ disease patients also may have ophthal-
mopathy and dermopathy. Burch and Wartofsky have pro-
posed a point scale to facilitate the diagnosis of thyroid
storm, assigning points based on the severity of thermoregu-
latory dysfunction (temperature), cardiovascular dysfunc-
tion, CNS effects, GI-hepatic dysfunction, and precipitating
factors. That is, thyrotoxic patients with fever and dysfunc-
tion of one or more organ systems, particularly cardiovascu-
lar and CNS, are more likely to have severe thyrotoxicosis and
need hospitalization for aggressive treatment.
B. Laboratory Findings—Elevated aminotransferases,
hyperbilirubinemia, and hepatomegaly are common.
Alkaline phosphatase levels are also increased, but this usu-
ally represents an increase in the bone fraction rather than
the liver fraction. Serum calcium may be elevated as a reflec-
tion of increased bone resorption. Other laboratory abnor-
malities observed in patients hospitalized for complicated
thyrotoxicosis include hypo- or hypernatremia, hyper-
glycemia, and anemia.
The diagnosis of thyroid storm is essentially a clinical
one. The presence of high fever and altered mental status in
a severely ill patient with hyperthyroidism should warrant
aggressive treatment for thyrotoxic crisis. Laboratory tests of
thyroid function confirm the presence of hyperthyroidism,
that is, high total and free thyroxine (T
4
) and triiodothyro-
nine (T
3
) and a reduced and nearly undetectable thyrotropin
(TSH) level. However, T
3
and T
4
levels may be decreased by
concurrent nonthyroidal illness. Therefore, levels of T
4
and
T
3
may not correlate with the patient’s clinical picture.
Treatment
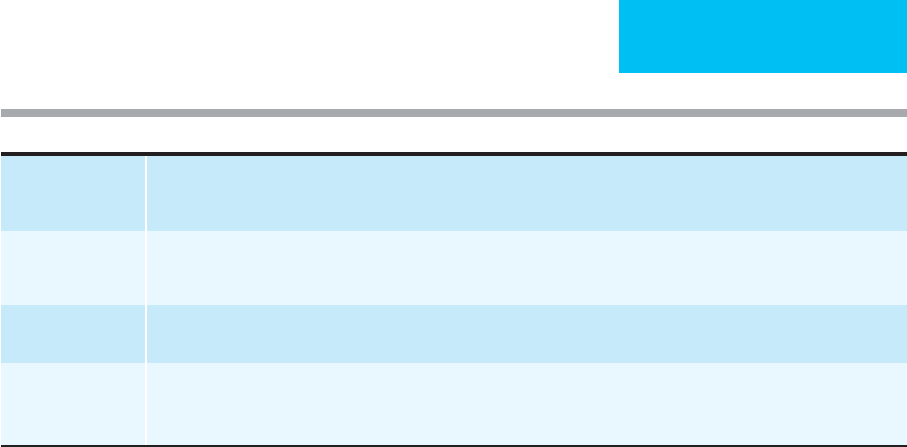
The management of thyroid storm can be discussed under
three broad categories: (1) control of hyperthyroidism,
(2) treatment of the precipitating illness, and (3) other
supportive measures. Treatment is summarized in Table 25–1.
CHAPTER 25
568
A. Control of Hyperthyroidism—Several therapeutic
agents that act by different mechanisms to block the synthe-
sis, secretion, activation, or action of thyroid hormones can
be used together for rapid control of hyperthyroidism.
1. Thioureas—Propylthiouracil, methimazole, and car-
bimazole inhibit thyroid hormone synthesis primarily by
inhibiting reactions catalyzed by the thyroid peroxidase
enzyme. These reactions include oxidation, organification,
and iodotyrosine coupling. Propylthiouracil is also a weak
inhibitor of peripheral conversion of T
4
to T
3
. Methimazole is
generally considered to be more potent than propylthiouracil.
In comatose patients with thyroid storm, propylthiouracil or
methimazole may be given through a nasogastric tube because
these drugs are not available in parenteral formulations.
There is no agreement about the optimal dosage of
antithyroid drugs. One regimen is to start propylthiouracil at
an initial dose of 600–1200 mg/day in four divided doses.
Alternatively, 60–120 mg/day methimazole can be given in
four divided doses. Should the patient be unable to take med-
ication orally, these medications can be administered rectally.
Others have advocated giving a loading dose of 600–1200 mg
propylthiouracil followed by 200–300 mg every 8 hours.
However, some investigators have questioned whether addi-
tional inhibition of thyroperoxidase is achievable at dosages
of propylthiouracil in excess of 300 mg daily. Methimazole
is given at one-tenth the preceding dosage. The serum half-
life of propylthiouracil is 75 minutes; of methimazole,
240–360 minutes. However, the intrathyroidal residence time
of methimazole is 20 hours, and its duration of action is
believed to be as long as 40 hours. These data have been used to
support once-daily administration of methimazole. However,
in the life-threatening situation of thyroid storm, it may be
preferable to give methimazole three or four times daily.
Propylthiouracil is also a weak inhibitor of 5′-deiodinase, the
enzyme that converts T
4
to T
3
, and this may be a minor advan-
tage over methimazole—although the two drugs have never
been compared directly. Propylthiouracil has been rarely asso-
ciated with pulmonary capillaritis and alveolar hemorrhage.
Resistance to the effects of antithyroid drugs is extremely
uncommon. Most cases of apparent resistance turn out to be
problems of noncompliance. Acute side effects of these drugs
are uncommon, but allergic reactions, leukopenia, and hepa-
totoxicity may occur.
2. Ipodate sodium—Ipodate sodium is an iodine-
containing radiocontrast agent used for gallbladder imaging.
It is one of the most potent inhibitors of 5′-deiodinase.
Clinical studies with ipodate in hyperthyroidism have shown
that the drug has an extremely rapid onset of action, result-
ing in marked lowering of serum T
3
levels within 4–6 hours
and normalization of serum T
3
levels within 24–48 hours.
The mechanism of antithyroid effect of ipodate is complex.
Besides inhibiting conversion of T
4
to T
3
, ipodate also lowers
serum T
4
levels, albeit to a lesser degree, indicating additional
direct effects on thyroid hormone synthesis. Reverse T
3
levels
are higher in ipodate-treated patients, an observation consis-
tent with drug-induced inhibition of 5′-deiodinase.
Although ipodate is an iodine-containing contrast agent,
radioiodine uptake studies in patients with Graves’ disease
treated with ipodate for more than a year revealed normal
uptake a week after discontinuation of ipodate therapy.
Ipodate sodium is administered orally as capsules con-
taining 500 mg. Recommended dosages range from 1–3
g/day. In obtunded patients, ipodate can be administered via
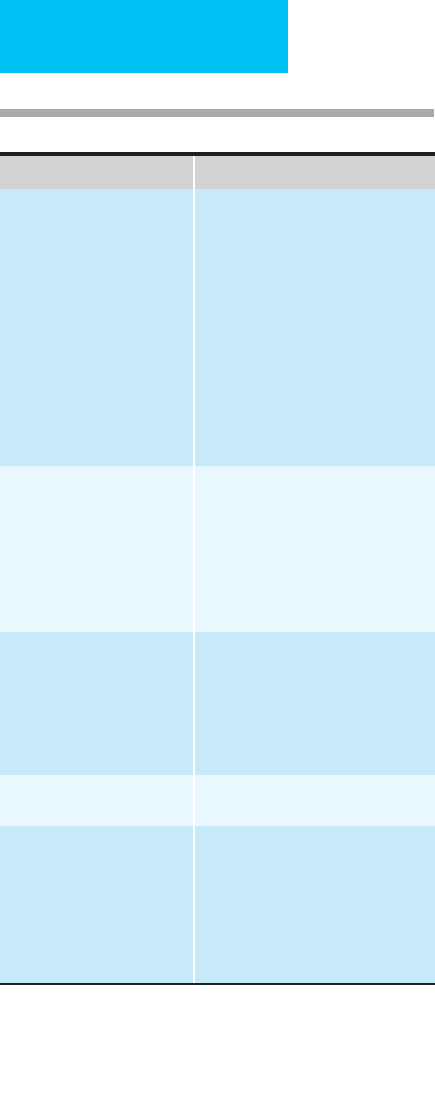
Mechanism of Action Treatment
Measures to reduce thyroid
hormone synthesis or
peripheral conversion of
T
4
to T
3
Propylthiouracil,
∗
200–300 mg orally
or through a nasogastric tube every
6 hours.
or
Propylthiouracil, 600 mg loading dose
orally, followed by 200–300 mg
every 8 hours.
or
Methimazole, 20–30 mg orally or
through a nasogastric tube every
6 hours.
plus
Ipodate,
†
1–1.5 g/d for the first
24 hours, then 500 mg twice daily.
Measures to inhibit the
release of thyroid hormones
Lugol’s solution, 5–10 drops three
times daily, or saturated solution of
sodium iodide, 3 drops three times
daily, after antithyroid therapy
(above) has been instituted.
Lithium carbonate, 300 mg every
8 hours, may be used in patients
with iodine allergy.
Sympathetic blockade Propranolol, 0.5–1 mg IV slowly over
5–10 minutes. Repeat every 3–4 hours
as indicated.
Contraindicated in COPD and asthma;
should be very carefully administered
in patients with congestive heart
failure.
Glucocorticoids Dexamethasone, 2–4 mg IV every
6–8 hours.
Supportive measures Identify and treat the precipitating
event.
Provide fluid and electrolyte replace-
ment as needed.
Hyperpyrexia: Cooling blankets, ice, or
cool sponges as necessary. Other
supportive measures.
∗
Both propylthiouracil and methimazole may be administered rectally.
†
If the patient is allergic to iodine, lithium may be used: lithium
carbonate, 300–400 mg every 8 hours. Serum lithium levels to be
maintained at approximately 1 meq/L.
Table 25–1. Treatment of thyroid storm.

ENDOCRINE PROBLEMS IN THE CRITICALLY ILL PATIENT
569
the intragastric route. It has been recommended that propy-
lthiouracil or methimazole be given prior to administration
of iodine-containing medications to prevent an iodide-
mediated exacerbation of hyperthyroidism.
3. Lithium—Lithium can be used in patients unable to tol-
erate iodine. Lithium is concentrated by the thyroid and
inhibits iodine uptake by the thyroid. It also inhibits thyroid
hormone release. A dosage of 300–400 mg every 8 hours can
be used temporarily to control the thyrotoxic patient who is
allergic to iodine. The dose should be adjusted as necessary
to maintain a serum lithium level of approximately 1 meq/L.
4. Iodide—Iodide blocks the release of thyroid hormones
from the gland. Iodide also has an inhibitory effect on thy-
roid hormone synthesis. High doses of inorganic iodide
decrease the yield of organic iodine within the thyroid
gland—a phenomenon referred to as the Wolff-Chaikoff
effect. However, this inhibitory effect on thyroid hormone
synthesis is transient, and in most patients, an escape from
this inhibition occurs with time.
Iodide should be administered only after synthesis of thy-
roid hormones has been inhibited by prior administration of
thioureas. Intravenous sodium iodide can be administered at
a dosage of 0.25 g every 6 hours. Alternatively, if the patient is
able to take medication orally, Lugol’s solution at a dosage of
5–10 drops three times a day or saturated potassium iodide
solution at a dose of 3 drops three times daily can be used.
Administration of a large dose of inorganic iodide pre-
dictably will reduce radioiodine uptake by the thyroid gland
for several weeks. Therefore, prior administration of inor-
ganic iodide will preclude subsequent treatment with
radioactive iodine for several weeks.
5. Propranolol—β-adrenergic blockers attenuate many of
the peripheral manifestations of hyperthyroidism. Thus
these agents can reverse the thyroid hormone-induced
increases in heart rate, cardiac output, and tremor. However,
weight loss is not affected by β-blockers. Propranolol, in
addition to its antiadrenergic properties, is a weak inhibitor
of 5′-deiodinase and thus lowers T
3
levels. The advantage of
the 5′-deiodinase inhibition property of propranolol is
unclear given the similar action of propylthiouracil and ipo-
date sodium. Other β-adrenergic blocking agents such as
esmolol and labetalol also have been used successfully.
The response to propranolol varies from patient to
patient, and dosages should be titrated to the clinical
response. The initial dose usually is 0.5–1 mg intravenously
given slowly over 5–10 minutes for a total of up to 10 mg.
This can be followed by 40–60 mg orally every 6 hours. If the
patient is unable to take medication orally, propranolol can
be administered intravenously in doses of 1–2 mg every 3–4
hours. These dosage recommendations are only general
guidelines to be used initially. Subsequent dosage adjust-
ments should be dictated by the clinical response.
Propranolol blood levels in the range of 50–100 μg/mL have
been shown to provide effective beta blockade. However,
blood levels of propranolol have not been used extensively in
clinical practice; it is much simpler to follow the heart rate
and blood pressure responses. Side effects of β-adrenergic
blockade in patients with thyroid storm include heart failure,
bradycardia, hypotension, and increased airway resistance.
6. Glucocorticoids—The older literature warned that
adrenal insufficiency might ensue in patients with thyroid
storm because of accelerated cortisol degradation. However,
this hypothesis has never been validated, and the routine use
of glucocorticoid replacement has declined. Glucocorticoids
do, however, have several salutary effects on thyroid function
in thyroid storm. In patients receiving thyroxine replace-
ment, glucocorticoids lower serum T
3
concentrations, prob-
ably by inhibition of peripheral 5′-deiodinase. In addition,
glucocorticoids lower serum T
4
levels in patients with
Graves’ disease. Finally, glucocorticoids in pharmacologic
doses inhibit TSH secretion. One recommended regimen is
2–4 mg dexamethasone every 6 hours intravenously. Patients
suspected of having adrenal insufficiency should be treated
accordingly with higher doses of hydrocortisone (see below).
7. Extracorporeal therapy—Exchange transfusion and
plasmapheresis have been advocated as ways of removing
large amounts of thyroid hormones from the circulation.
Experience with these techniques is limited. Furthermore,
with the availability of potent antithyroid drugs, they are not
likely to be needed.
B. General Supportive Measures—General measures
include fluid and electrolyte replacement and control of
hyperpyrexia. The latter may require the use of cooling blan-
kets. Salicylates should be avoided because these drugs can
inhibit T
4
and T
3
binding to the binding proteins and
increase the concentrations of the free T
4
and T
3
. In addition,
specific measures for prompt treatment of the precipitating
illness, cardiac arrhythmias, and congestive heart failure
should be initiated if indicated.
Prognosis
Most data on mortality statistics in thyroid storm are old, and
there are no recent series. Survival figures vary from 24–66%
in older series. The precipitating illness is clearly an important
determinant of prognosis. Many of these patients may require
admission to the ICU, and most require an extended hospital
stay; in one study, the median hospital stay was 12 days.
Basaria S, Cooper DS: Amiodarone and the thyroid. Am J Med
2005;118:706–14. [PMID: 15989900]
Cardenas GA, Cabral JM, Leslie CA: Amiodarone-induced thyro-
toxicosis: Diagnostic and therapeutic strategies. Cleve Clin J Med
2003;70:624–6. [PMID: 12882384]
Cooper DS: Antithyroid drugs. N Engl J Med 2005;352:905–17.
[PMID: 15745981]
Goldberg PA, Inzucchi SE: Critical issues in endocrinology. Clin
Chest Med 2003;24:583–606. [PMID: 14710692]
Nayak B, Burman K: Thyrotoxicosis and thyroid storm.
Endocrinol Metab Clin North Am 2006;3:663–86. [PMID:
17127140]
CHAPTER 25
570
Myxedema Coma
ESSENTIALS OF DIAGNOSIS
Features of severe hypothyroidism (myxedema): dry,
rough, cold skin, nonpitting doughy edema, loss of eye-
brows and scalp hair, and delayed relaxation phase of
deep tendon reflexes.
Hypothermia.
Altered mental status or coma.
Hypercapnic respiratory failure.
General Considerations
Myxedema coma represents a breakdown of the body’s com-
pensatory mechanisms during the course of long-standing
severe hypothyroidism. Development of an intercurrent illness
such as an infection on top of the underlying severe hypothy-
roidism usually leads to this decompensation. Myxedema
coma is primarily a clinical diagnosis. While laboratory tests
confirm hypothyroidism, the diagnosis is based on the con-
stellation of clinical findings of myxedema, altered mental sta-
tus, and hypothermia. The physician must remain alert for the
possibility of myxedema coma because the consequences of
missing the diagnosis can be devastating. In addition, the usual
clinical signs of infection such as fever and leukocytosis may
be masked in patients with severe hypothyroidism. Therefore,
one also must actively search for infection or other precipitat-
ing factors and treat these illnesses aggressively.
Pathophysiology
Hypothyroidism is a common endocrinopathy, but
myxedema coma is encountered much less commonly
because of thyroid hormone replacement therapy.
Myxedema coma is associated with poor outcome. Patients
with myxedema most often have a history of hypothy-
roidism, but the precipitating condition is almost always a
combination of failure to take an adequate amount of thy-
roid replacement therapy and the presence of some comor-
bid condition. Because the serum half-life of T
4
is quite long,
hypothyroidism is a subacute condition characterized by
decreased metabolic rate, accumulation of edema fluid, dete-
rioration of cardiac function from structural and physiologic
changes, hyperlipidemia, and inability to manifest an appro-
priate response to hypothermia. Ventilatory drive is dimin-
ished from central mechanisms and, because of respiratory
muscle weakness and pleural effusions and ascites, can result
in hypercapnia. Hyponatremia is common and results from
the inability to dilute urine maximally.
Clinical Features
Myxedema coma almost always occurs in patients with
known hypothyroidism but rarely can present as the initial
finding in hypothyroidism. A precipitating event usually can
be identified along with absent or inadequate thyroid replace-
ment therapy. The majority of cases of myxedema coma are
reported in winter months in regions with cold climates. Thus
cold exposure appears to be an important antecedent factor.
Other precipitating factors include sedative or anesthetic
drugs, congestive heart failure, cerebrovascular accidents,
trauma, infections, and a variety of other illnesses.
A. Symptoms and Signs—Most patients with myxedema
are elderly women. The classic signs of myxedema are pres-
ent, including puffy, expressionless face; dry, rough, and cold
skin; nonpitting, doughy edema; loss of eyebrows and scalp
hair; delayed relaxation phase of the tendon reflexes; and
enlarged tongue. Hypothermia is a hallmark of myxedema
coma, with core body temperatures as low as 21°C but more
often in the range of 32–35°C. Severe hypothermia (temper-
ature <32°C) is associated with a poor prognosis. However,
hypothermia can be easily overlooked if a thermometer that
can register temperatures below the usual range is not used.
Blood pressure may be normal, high, or low. The heart rate is
classically slow. Respirations may be slow and shallow
depending on the level of ventilatory drive and respiratory
muscle weakness. Mental status changes may include confu-
sion, somnolence, hallucinations, or coma. The thyroid gland
may not be palpable because of idiopathic atrophy, prior
radiation, or surgery.
Drug metabolism is significantly reduced in hypothy-
roidism, and administration of the usual doses of sedatives
may depress ventilation significantly and compromise men-
tal status. In critically ill patients, the diagnosis of hypothy-
roidism sometimes may be hard to make on clinical grounds.
B. Laboratory Findings—Hyponatremia is often present.
Arterial blood gases may reveal respiratory acidosis, hypercap-
nia, and hypoxemia. Hypoglycemia may occur, particularly if
there is deficiency of pituitary hormones as well. Chest x-ray
may reveal an enlarged cardiac silhouette and pleural and peri-
cardial effusions. The ECG may demonstrate low voltage,
sinus bradycardia, diffuse T-wave depression, nonspecific
ST-segment changes, and prolonged QT and PR intervals.
There may be conduction blocks as well. Cerebrospinal fluid
(CSF) pressure and protein concentrations may be increased.
Although myxedema coma is a clinical diagnosis, thyroid
function tests reveal low thyroxine (T
4
), low T
3
resin uptake,
and a high thyrotropin (TSH) level. It may be difficult at times
to distinguish sick euthyroid syndrome from primary hypothy-
roidism by thyroid function tests. Very high serum TSH levels
(>20 μU/mL) favor the diagnosis of primary hypothyroidism.
Moderately elevated TSH levels (up to 20 μU/mL) may be seen
occasionally in the course of sick euthyroid syndrome. Severe
nonthyroidal illness decreases the TSH response, and inappro-
priately low TSH is seen in secondary hypothyroidism owing
to hypothalamic or pituitary disorders.
C. Adrenal Insufficiency—In patients with hypothyroidism,
the manifestations of adrenal insufficiency may be masked.
This is important because adrenal insufficiency can coexist
ENDOCRINE PROBLEMS IN THE CRITICALLY ILL PATIENT
571
with hypothyroidism in two clinical situations. First, in
patients with autoimmune thyroid disease, there is a higher
incidence of autoimmune adrenalitis and adrenal insufficiency
than in the general population. Second, patients with panhy-
popituitarism may have absence of both TSH and adrenocor-
ticotropin (ACTH). These patients with secondary adrenal
insufficiency lack the skin and mucosal hyperpigmentation
that is characteristic of primary adrenal insufficiency. For
these reasons, it is easy to miss adrenal insufficiency in this set-
ting, and the clinician must keep alert to the possibility of con-
comitant adrenal insufficiency. A rapid ACTH stimulation test
should be performed in patients with myxedema. However, it
should be recognized that the cortisol response to ACTH may
be attenuated by hypothyroidism.
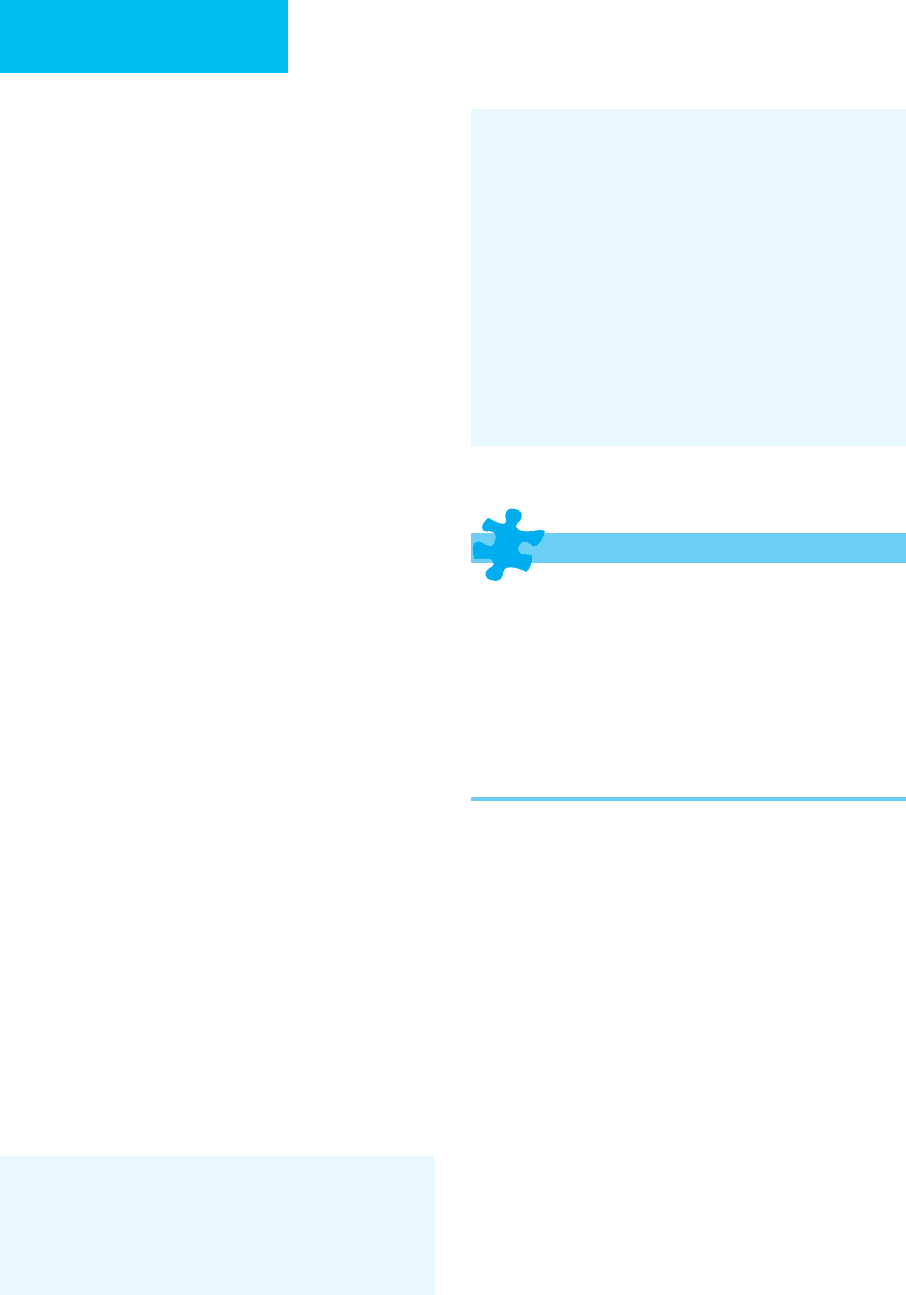
Treatment
Treatment consists of thyroid hormone replacement,
replacement of other necessary hormones, and supportive
measures (Table 25–2), including treatment of hypothermia
and of the precipitating illness.
A. Thyroid Hormone Replacement—While all commenta-
tors assert the need for prompt thyroid hormone replacement
in myxedema coma, there is disagreement about what consti-
tutes an optimal regimen. The major controversy relates
to which regimen of thyroid hormone replacement to use:
T
4
alone, T
3
alone, or a combination of T
4
and T
3
. The use of
T
3
alone has been advocated by some on physiologic grounds.
This is so because the activity of 5′-deiodinase is diminished
in hypothyroidism, and the conversion of T
4
to T
3
may be
limited. On the other hand, a rapid increase in T
3
may be
detrimental to the patient because of cardiac arrhythmias and
too rapid an increase in myocardial oxygen demand. Large
doses of T
3
(>75 μg) have been associated with increased
mortality. Because of its potential adverse effects, the use of
this regimen has been discouraged by some.
Intravenous administration of T
4
is considered safe and has
been the standard for the past three decades. One traditional
regimen consists of 500 μg of levothyroxine (T
4
) given slowly
intravenously, followed by 100–150 μg every 24 hours. The
rationale for the large initial dose is that it restores the total thy-
roxine pool. However, it is not clear if this regimen is any bet-
ter than 150 μg given intravenously daily. The rate of fall in
serum TSH levels is not significantly different between the two
regimens. In fact, a dose of 100–150 μg levothyroxine given
intravenously daily would correct the thermoregulatory, respi-
ratory, cardiac, and mental status changes over 24–48 hours.
A third regimen consists of a combination of both T
4
and
T
3
. It is suggested that 200–300 μg T
4
be given simultane-
ously with 25 μg T
3
intravenously. This is followed by admin-
istration of another 25 μg T
3
12 hours later and 100 μg T
4
at
24 hours. Starting the third day, 100 μg T
4
is given daily until
the patient regains consciousness.
Recent literature has witnessed conflicting reports on the
effectiveness of combined regimens of levothyroxine and
triiodothyronine. The rates of conversion of thyroxine to
triiodothyronine do vary in different tissues; animal studies
suggest that T
3
concentrations in some tissues of thyroidec-
tomized rats replaced with levothyroxine alone are lower
than those observed in euthyroid animals. Similarly, circulat-
ing levels of T
3
in hypothyroid patients treated with levothy-
roxine alone are lower than those in euthyroid individuals.
Objective differences between thyroxine replacement com-
pared with combined thyroxine plus triiodothyronine
replacement have not been found.
There is no strong basis for advocating any one regimen.
The rapid restoration of thyroid hormone levels is desirable.
Most authorities agree that expeditious thyroid hormone
replacement is a more important objective than the exact
regimen of thyroid hormone replacement and that high-dose
levothyroxine administered intravenously is a reasonable and
safe choice.
B. Glucocorticoids—As discussed earlier, signs of adrenal
insufficiency may be masked in hypothyroid patients. On the
other hand, initiation of levothyroxine therapy without con-
comitant glucocorticoid replacement may precipitate adre-
nal crisis if the patient has adrenal insufficiency. Therefore,
one must be on guard against the possibility of adrenal insuf-
ficiency in appropriate patients. If in doubt, it is better to err
on the side of treatment with corticosteroids (see “Adrenal
Insufficiency” next) because the consequences of delayed or
no replacement can be serious.
C. Supportive Measures—Patients with myxedema coma
may need transient endotracheal intubation and mechanical
ventilation for hypercapnic respiratory failure. Intravenous
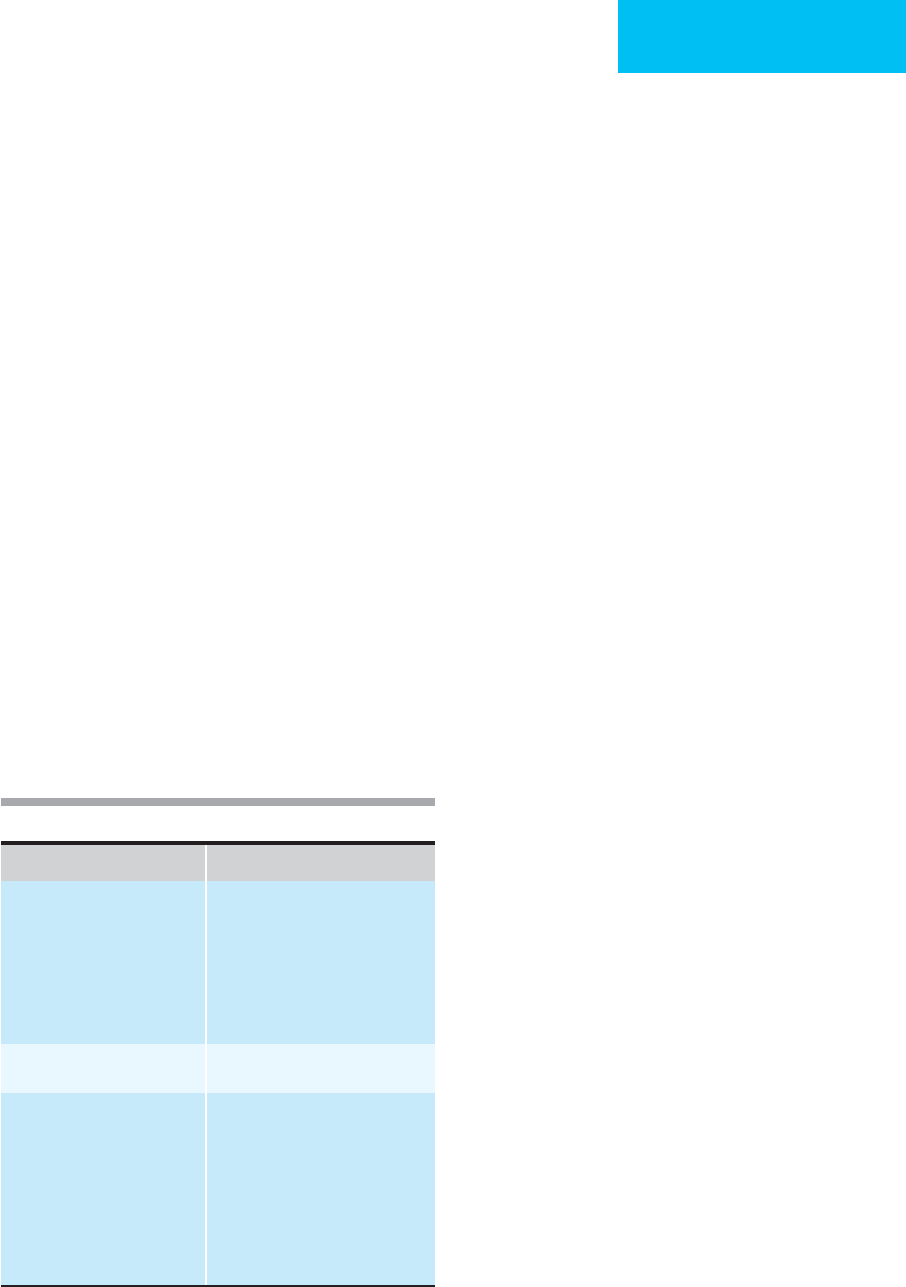
Mechanism of Action Treatment
Thyroid hormone replacement Levothyroxine (T
4
), 500 μg by slow
intravenous infusion, followed by
100–150 μg every 24 hours.
or
T4, 200–300 μg, and triiodothyronine
(T
3
), 25 μg IV; 25 μg of T
3
12 hours
later; and 100 μg of T
4
at
24 hours.
Glucocorticoid Hydrocortisone, 100 mg IV every
8 hours.
Supportive measures Maintain adequate ventilation.
Institute endoctracheal intubation
and mechanical ventilation if
necessary.
Identify and treat the precipitating
event.
Provide fluid and electrolyte
replacement as needed.
Correct core body temperature.
Table 25–2. Treatment of myxedema coma.
CHAPTER 25
572
fluids, electrolytes, and vasopressors may be needed to maintain
blood pressure. Rapid rewarming through the use of heating
blankets is not generally recommended because it may provoke
or worsen peripheral vasodilation and hypotension. However,
in patients with severe hypothermia, thermogenic shivering
mechanisms may become impaired, and these patients may not
be able to raise their body temperatures. Therefore, gradual but
active rewarming may be required in some patients. In most
patients with mild hypothermia, wrapping the patient in blan-
kets in a warm room is sufficient to restore body temperature,
provided that thyroid replacement therapy has been initiated.
Treatment of hypothermia is discussed in Chapter 38. A search
for infection or other precipitating factors should be mounted.
In many instances, empirical antibiotic therapy may be justified.
Because of decreased metabolic rate, many drugs are cleared
more slowly in patients with severe hypothyroidism.
Prognosis
Myxedema coma may be fatal if unrecognized and left
untreated. Poor prognostic indicators include severe hyper-
capnia and hypothermia. If infection or other precipitating
illness is present, outcome depends on treatment and
response to these problems. Complications of thyroxine (T
4
)
and triiodothyronine (T
3
) replacement therapy may include
serious cardiac morbidities, such as acute coronary syn-
drome and cardiac arrhythmias.
Escobar-Morreale HF et al: Thyroid hormone replacement therapy
in primary hypothyroidism: A randomized trial comparing
L
-
thyroxine plus liothyronine with
L
-thyroxine alone. Ann Intern
Med 2005;142:412–24. [PMID: 15767619]
Fliers E, Wiersinga WM: Myxedema coma. Rev Endocr Metab
Disord 2003;4:137–41. [PMID: 12766541]
Goldberg PA, Inzucchi SE: Critical issues in endocrinology. Clin
Chest Med 2003;24:583–606. [PMID: 14710692]
Rodriguez I et al: Factors associated with mortality of patients with
myxoedema coma: Prospective study in 11 cases treated in a sin-
gle institution. J Endocrinol 2004;180:347–50. [PMID: 14765987]
Wartofsky L: Myxedema coma. Endocrinol Metab Clin North Am
2006;35:687–98. [PMID: 17127141]
Acute Adrenal Insufficiency
ESSENTIALS OF DIAGNOSIS
Hypotension, volume depletion, hypovolemic shock.
Hyperkalemia, hyponatremia.
Weakness, abdominal pain, nausea, vomiting, fever.
Acute infectious illness or trauma, recent cessation of
corticosteroid therapy, or inadequate replacement in
chronic adrenal insufficiency.
Abnormal ACTH stimulation test.
General Considerations
Critical illness, whether from sepsis, trauma, surgery, or any
condition associated with hemodynamic compromise, stim-
ulates the hypothalamic-pituitary-adrenal axis causing an
increased production of cortisol. This hormone, synthesized
in the adrenal cortex under the influence of ACTH, main-
tains vascular integrity and tone, stimulates neoglucogenesis
and free water clearance, and influences fluid and electrolyte
balance. Lack of aldosterone—a mineralocorticoid—is asso-
ciated with inability to conserve sodium in the face of hypo-
volemia and hyperkalemia. Deficiency of cortisol—a
glucocorticoid—on the other hand, is associated with inabil-
ity to clear free water and with hemodynamic compromise
mimicking hypovolemic or septic shock. Hyponatremia, a
hallmark of adrenal insufficiency, is typically due to the
inability of these patients to clear free water owing to corti-
sol deficiency and dysregulated antidiuretic hormone (ADH)
secretion. Patients with adrenal insufficiency become
hypotensive owing to a combination of factors, including
hypovolemia and impaired vascular response to cate-
cholamines and also to loss of a direct inotropic effect of cor-
tisol. Cortisol stimulates hepatic neoglucogenesis, and it is
therefore not surprising that patients with adrenal insuffi-
ciency may present with hypoglycemia. Serum cortisol levels
in acutely ill patients are usually increased.
Acute adrenal insufficiency is the result of inadequate
cortisol production with life-threatening cardiovascular col-
lapse and potentially severe electrolyte and fluid abnormali-
ties. Acute insufficiency can occur as a result of an acute
insult to the adrenal glands from infection or trauma or may
be seen in a patient with chronic adrenal insufficiency who
develops critical illness. Patients who receive corticosteroids
for treatment of inflammatory diseases will have chronic
suppression of pituitary-adrenal function, and abrupt cessa-
tion of therapy may precipitate acute adrenal insufficiency,
especially if there is intercurrent illness. A high index of sus-
picion for the diagnosis of adrenal crisis is the key. Because
delay in instituting treatment can be fatal, acute adrenal
insufficiency should be suspected in any patient presenting
with hypotension, fever, abdominal pain, hyponatremia, or
hyperkalemia, especially if hyperpigmentation is present. In
many clinical situations, empirical therapy may be appropri-
ate, even before a definitive diagnosis has been made.
Pathophysiology
Idiopathic or autoimmune adrenalitis accounts for about
80% of cases of chronic adrenal insufficiency in outpatients.
Tuberculosis used to be a major cause of adrenal insuffi-
ciency, but that disease is relatively uncommon now in devel-
oped countries. Other less common causes include adrenal
hemorrhage; fungal infections such as histoplasmosis, coc-
cidioidomycosis, blastomycosis, and candidiasis; hemochro-
matosis; irradiation; surgical removal of the adrenal glands;
drug toxicity; and congenital disorders such as synthetic

ENDOCRINE PROBLEMS IN THE CRITICALLY ILL PATIENT
573
enzyme deficiencies. Patients with HIV infection often have
abnormalities in the adrenal glands at autopsy but appear to
have only a slightly increased incidence of adrenal insuffi-
ciency (about 5–10%). The impaired immune status result-
ing from HIV infection increases the likelihood of adrenal
involvement with cytomegalovirus (the most common find-
ing), fungi (eg, Cryptococcus and Histoplasma), or mycobac-
teria (both tuberculous and nontuberculous). HIV, however,
directly affects the adrenal glands only in a small number of
patients. Secondary adrenal insufficiency can occur in HIV-
infected patients because of direct involvement of the hypo-
thalamus or the pituitary gland, opportunistic infections
(eg, tuberculoma or histoplasmosis), or lymphoma.
Other causes of adrenal insufficiency include metastatic
cancer and hemorrhage. Although metastases to the adrenal
gland are relatively common, adrenal insufficiency as a result
of metastatic disease is uncommon. Adrenal hemorrhage may
occur during the course of sepsis, excessive anticoagulation,
trauma, pregnancy, or surgery. Adrenal infarction may occur
as a result of thrombosis, embolism, or arteritis. Infiltrative
disorders include amyloidosis, sarcoidosis, and hemochro-
matosis. Congenital disorders leading to adrenal insufficiency
include congenital adrenal hyperplasia. This is due to a genetic
defect in one of the steroidogenic enzymes or hypoplasia.
A number of drugs directly inhibit the enzymes involved in
steroidogenesis. Etomidate is frequently used during endotra-
cheal intubation; it suppresses adrenocortical function for up
to 24 hours. Metyrapone inhibits β-hydroxylase, aminog-
lutethimide inhibits side-chain cleavage enzymes, ketoconazole
inhibits a number of cytochrome P450-linked steroidogenic
enzymes, and mitotane is an adrenolytic cytotoxic agent.
Fluconazole also has been implicated. Relatively common med-
ications such as rifampin and seizure medications (eg, pheny-
toin and carbamazepine) increase hepatic cytochrome P450
activity, thus increasing cortisol metabolism. These medica-
tions should be used with caution in patients with limited adre-
nal reserve.
In patients with autoimmune adrenalitis, there is an
increased incidence of other endocrinopathies. For example,
Hashimoto’s thyroiditis, Graves’ disease, pernicious anemia,
hypoparathyroidism, premature ovarian or testicular failure,
and type 1 diabetes occur with a greater frequency than in
the general population. It is now clear that multiple
endocrine organs may be affected by organ-specific autoim-
mune disease. These polyendocrine autoimmune syndromes
are classified into two major groups: type I and type II. Type
I patients usually present in early childhood with
hypoparathyroidism and mucocutaneous candidiasis; adre-
nal insufficiency may develop later. Disease is usually limited
to one generation of siblings. Genetic analyses of families are
consistent with an autosomal recessive inheritance in a single
gene. Mutations in an autoimmune regulator gene (AIRE)
have been described in association with polyendocrine
autoimmune syndrome type I. In contrast, type II patients
usually present with adrenal insufficiency in the third or
fourth decade. Type 1 diabetes mellitus occurs in almost
half of patients. There is a strong association with HLA-DR3
or -DR4 haplotypes. Hyperthyroidism (Graves’ disease),
Hashimoto’s thyroiditis, primary ovarian failure, myasthenia
gravis, celiac disease, and pernicious anemia occur much more
commonly in patients with type II polyendocrine autoimmune
syndrome than in the general population. Multiple generations
in the same family are usually affected. The genetic analyses of
families suggest that it is a polygenic disorder with autosomal
dominant inheritance. Autoantibodies against at least three
cytochrome P450 enzymes that are involved in cortisol synthe-
sis have been reported in association with Addison’s disease
as part of both type I and type II syndromes.
Acute Adrenal Crisis
Acute adrenal crisis refers to the collapse and shock syndrome
that occurs in a patient with inadequate adrenal cortical
function. This can occur in chronic adrenal insufficiency
because of stress imposed by a serious illness such as infec-
tion, trauma, or surgery without adequate replacement. In
other patients, acute bilateral adrenal hemorrhage (ie,
Waterhouse-Friderichsen syndrome), originally described in
association with meningococcemia, is the cause of acute adre-
nal insufficiency. Acute adrenal hemorrhage can complicate the
course of systemic sepsis from other pathogens as well. In fact,
Pseudomonas aeruginosa is a common organism in children
dying with sepsis and adrenal hemorrhage. Other common
acute antecedent factors include anticoagulant therapy, dissem-
inated intravascular coagulation, and the perioperative state.
Clinical Features
The clinical manifestations of adrenal insufficiency depend
(1) on whether the patient has primary or secondary adrenal
failure, (2) on the presence or absence of other endocrinopathies
(eg, coexistence of hypothyroidism may significantly attenu-
ate the manifestations of adrenal insufficiency), and (3) on the
presence of superimposed nonendocrinologic illness or stress.
In the ICU, symptoms and signs of the acute illness may
overshadow the features of concomitant adrenal insuffi-
ciency, making clinical suspicion the key to diagnosis.
A. Symptoms and Signs—Patients with chronic adrenal
insufficiency may not come to medical attention for some
time because of the nonspecific nature of symptoms, such as
fatigue, anorexia, weight loss, nausea, and vomiting. Other
manifestations include weakness, salt craving, and postural
dizziness. Patients with primary adrenal insufficiency usually
have hyperpigmentation of the skin and mucous membranes
because of increased ACTH production by the pituitary.
Patients often develop a “tan” in both sun-exposed and non-
exposed parts, especially in areas that suffer chronic friction
and trauma, such as elbows, knees, knuckles, and the belt-
line. The buccal mucosa may show hyperpigmentation,
especially along sites of dental occlusion. The “tan” appear-
ance of these patients often conveys a misleading impression
of good health. Scars acquired during the course of adrenal

CHAPTER 25
574
insufficiency also become hyperpigmented, whereas those
acquired before or after remain unpigmented.
The hallmarks of acute adrenal insufficiency (ie, adrenal
crisis) include severe hypotension and vascular collapse, nau-
sea, vomiting, abdominal pain, and fever. Hypotension is due
largely to volume depletion, and there may be other evidence
of volume depletion. Abdominal symptoms may lead to an
erroneous diagnosis of acute abdomen, resulting in unwar-
ranted and potentially catastrophic surgical exploration.
Confusion and altered mental status also may occur.
Petechiae may be found if meningococcemia is the cause of
acute adrenal hemorrhage. Hyperpigmentation, if present,
indicates chronic primary adrenal insufficiency. Infection,
surgical stress, and trauma may precipitate acute adrenal cri-
sis in patients with chronic adrenal insufficiency. Patients
should be questioned about receiving chronic corticosteroid
therapy, especially if they have a history of asthma, interstitial
lung disease, rheumatologic diseases such as systemic lupus
erythematosus, or lymphoproliferative disorders. Patients
with HIV infection and autoimmune endocrinopathies
should be suspected of adrenal insufficiency if they present
with intractable hypotension and hyponatremia.
A degree of clinical suspicion may be necessary in evalu-
ating critically ill patients who may present in atypical fash-
ion. Patients with hemodynamic instability that cannot be
explained easily—in association with fever with no identified
source and alteration in mental status—should be consid-
ered for adrenal insufficiency. These patients may benefit
from empirical adrenal replacement therapy.
B. Laboratory Findings—Laboratory data may reveal
hyponatremia, hyperkalemia, and azotemia. Hypoglycemia
occurs more often in children but may be seen in adults as
well, especially in those who have been vomiting.
Corticosteroids play an important role in regulating gluco-
neogenesis and have potent anti-insulin actions.
Hypercalcemia and eosinophilia also may be found.
Hyponatremia is usually multifactorial. Patients with pri-
mary adrenal insufficiency are unable to conserve sodium
because of mineralocorticoid deficiency. However, these
patients become hyponatremic even in the face of positive
sodium balance. This is so mainly because of inability to
clear free water due to glucocorticoid deficiency. The exact
pathophysiology of the defect in free water clearance in pri-
mary adrenal insufficiency is not known, but there is lack of
adequate suppression of ADH levels in the face of hypona-
tremia. In addition, glucocorticoids also exert a permissive
effect of ADH directly at the kidney level. In the evaluation
of volume depletion and hyponatremia, low urinary sodium
and fractional excretion of sodium usually reflect volume
depletion; in adrenal insufficiency, however, both urinary
indices may be elevated because of the inability of the kid-
neys to conserve sodium maximally in the absence of cortisol
and aldosterone.
C. Adrenal Function Tests—A patient in whom acute adre-
nal insufficiency is suspected should be treated immediately.
However, diagnosis can be made rapidly and reliably by an
ACTH stimulation test. In addition, a random serum cortisol
level greater than 20 μg/dL makes the diagnosis of adrenal
insufficiency unlikely.
The traditional protocol for the rapid ACTH stimulation
test is as follows: 250 μg cosyntropin (containing amino acids
1–24 of ACTH) is administered intravenously, and plasma
samples are obtained at 0, 30, and 60 minutes for measure-
ment of cortisol. In addition, it is helpful to save contingency
samples for plasma aldosterone measurement. Earlier stud-
ies had suggested that an increment of more than 7 μg/dL
after cosyntropin administration or peak levels greater than
17 μg/dL would exclude adrenal insufficiency. However,
other data indicate that any cortisol value greater than or
equal to 20 μg/dL before or after the cosyntropin test is con-
sistent with normal adrenal function. A normal response
excludes primary adrenal insufficiency. Concern about adre-
nal insufficiency should be raised if any of these criteria are
not met. A small incremental increase in plasma cortisol
after cosyntropin despite a baseline value in the normal
range may be associated with a poor outcome and increased
mortality.
Some studies have suggested that the supraphysiologic
dose of corticotropin used may cause false-negative readings
in patients with partial or secondary adrenal insufficiency.
This is so because patients with adrenal insufficiency may
have some reserves left, and using the relatively large dose of
corticotropin might lead to a normal response. Some have
advocated using instead a low-dose ACTH stimulation test
with 1 μg corticotropin. A normal response is a rise in corti-
sol level to 20 μg/dL or more at 30 or 60 minutes.
If the cortisol response to cosyntropin is subnormal, the
contingency samples can be used to measure aldosterone and
endogenous ACTH to distinguish primary from secondary
adrenal insufficiency. Aldosterone responses to cosyntropin
are impaired in primary adrenal insufficiency but are pre-
served in secondary adrenal insufficiency (due to decreased
endogenous ACTH secretion). ACTH is elevated in primary
adrenal insufficiency and low normal or below normal in
secondary adrenal insufficiency. Certain clinical features also
can be useful in distinguishing primary from secondary
adrenal insufficiency. For example, hyperpigmentation and
hyperkalemia are observed in primary but not in secondary
adrenal insufficiency. The presence of other endocrine hor-
mone deficiencies does not necessarily indicate panhypopi-
tuitarism because these also could be a consequence of
autoimmune polyendocrinopathy.
Treatment
Once the diagnosis of adrenal insufficiency has been made,
treatment is relatively straightforward (Table 25–3).
A. Corticosteroid Replacement—Promptness in institut-
ing corticosteroid therapy is very important. Corticosteroid
replacement can be given as hydrocortisone sodium succinate,
75–100 mg intravenously every 6–8 hours. If the patient is
ENDOCRINE PROBLEMS IN THE CRITICALLY ILL PATIENT
575
hypotensive, performance of the diagnostic ACTH stimula-
tion test may unduly delay institution of therapy. Under
these circumstances, an equivalent dose of dexamethasone
(3–4 mg every 6–8 hours) can be given intravenously con-
temporaneously with ACTH administration. Dexamethasone
does not crossreact in the cortisol assay, and the diagnostic
procedure therefore can be done without concern about the
delay in instituting replacement therapy. The dose of hydro-
cortisone sodium succinate can be reduced to the replace-
ment level (10–20 mg in the morning and 5–10 mg in the
evening) as the patient’s condition improves.
Some studies cast doubt on the need for large pharmaco-
logic doses of corticosteroids during surgery. Studies in
adrenalectomized monkeys suggest that physiologic replace-
ment doses of corticosteroids are sufficient in this primate
model to tolerate the stress of surgical laparotomy.
Supraphysiologic doses of corticosteroids conferred no sur-
vival advantage on these adrenalectomized monkeys over
physiologic replacement doses during the period of surgical
stress. Other studies have shown that patients receiving
steroids prior to undergoing surgery did not require addi-
tional glucocorticoids during the perioperative period.
Empirical recommendations for glucocorticoid adminis-
tration in surgical patients are to estimate the degree of stress
and give 25 mg/day of hydrocortisone for mild stress, 50–75
mg/day for 2–3 days for moderate stress, and 100–150
mg/day for 2–3 days for severe stress. After recovery from
acute illness, patients with adrenal insufficiency should be
placed on chronic replacement therapy with hydrocortisone.
Traditionally, a dose of 30 mg hydrocortisone administered
in two divided doses—20 mg in the morning and 10 mg in
the evening—has been used widely. However, recent assess-
ments using more accurate isotope dilution and mass spec-
trometric methods suggest that daily cortisol production
rates are 5–6 mg/m
2
of body surface area rather than the
12–15 mg/m
2
of body surface area, as was thought previously.
Therefore, the traditional regimen of 30 mg hydrocortisone
daily possibly represents excessive glucocorticoid replace-
ment and may increase the risk of osteoporosis. A more
appropriate regimen may be 15 mg hydrocortisone adminis-
tered in two divided doses: 10 mg in the morning and 5 mg
in the afternoon. Although hydrocortisone traditionally has
been administered in a twice-daily regimen, some authors
have suggested that a thrice-daily regimen (10, 5, and 5 mg)
might provide more physiologic cortisol levels.
B. Mineralocorticoid Replacement—Most patients with
primary adrenal insufficiency require mineralocorticoid
replacement. In chronic adrenal insufficiency, this can be
administered as fludrocortisone acetate. The usual starting
dosage is 0.05–0.1 mg by mouth daily. Some patients may
develop leg edema on initiation of therapy. This usually will
abate if the dose is reduced. Hydrocortisone by itself has
some mineralocorticoid activity, so when patients are receiv-
ing more than 50–60 mg/day of hydrocortisone, no addi-
tional mineralocorticoid replacement is necessary. However,
if dexamethasone, which has little or no mineralocorticoid
activity, is used instead of hydrocortisone, a mineralocorti-
coid should be added.
C. Fluid and Electrolytes—Patients with adrenal insuffi-
ciency often have an enormous salt and water deficit. It is
important to correct these deficits aggressively by adminis-
tration of 0.9% NaCl solution intravenously. However,
patients with adrenal insufficiency may continue to be
hypotensive even after adequate fluid and electrolyte
replacement. Blood pressure may be restored only by cor-
ticosteroid administration. It is often not recognized that
corticosteroids have an inotropic effect on the myocardium.
Patients with adrenal insufficiency may present with
hyperkalemia; therefore, routine potassium replacement
should be postponed until serum potassium measure-
ments are obtained.
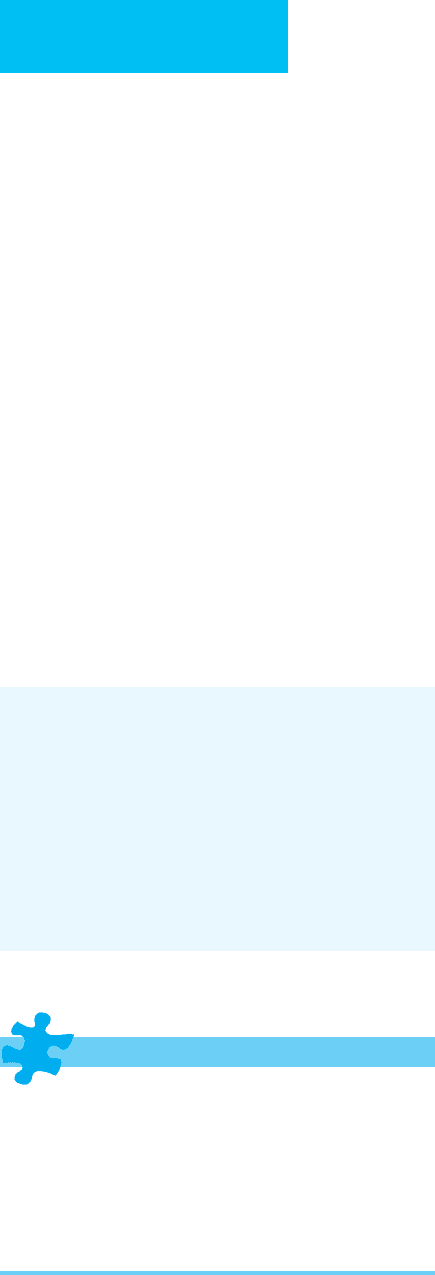
Diagnostic testing If you are considering a diagnosis of acute adrenal insufficiency, perform a rapid ACTH test (see text) immediately and initiate
treatment pending return of laboratory results. If a patient is highly likely to have adrenal insufficiency, give dexamethasone
immediately while the ACTH test is being conducted.
Glucocorticoid Hydrocortisone sodium succinate, 75–100 mg IV immediately and then every 6–8 hours.
or
Dexamethasone, 3–4 mg IV every 6–8 hours.
Mineralocorticoid Not required when large doses of hydrocortisone (>50–60 mg/d) are used. Consider adding fludrocortisone acetate, 0.05–0.1 mg
orally daily if dexamethasone is used.
Supportive measures Identify and treat the precipitating illness.
Correct fluid and electrolyte abnormalities. Intravenous NaCl 0.9% is usually given initially.
Monitor blood glucose and electrolytes and administer glucose if necessary.
Table 25–3. Management of acute adrenal insufficiency (adrenal crisis).
CHAPTER 25
576
D. Glucose—Corticosteroids are important regulators of
gluconeogenesis. Although in adults, unlike children, hypo-
glycemia is not a common manifestation of adrenal insuffi-
ciency, patients who have been vomiting for a few days may
present with hypoglycemia or develop hypoglycemia during
the course of evaluation or treatment. Therefore, plasma glu-
cose levels should be monitored and glucose given intra-
venously to correct or prevent hypoglycemia.
E. Other Treatment—It is crucial to identify and treat the
antecedent illness precipitating acute adrenal insufficiency.
This may include administration of antibiotics to treat an
infection. Many patients with adrenal insufficiency have one
or more endocrinopathies. It is important to recognize and
treat these when identified.
Current Controversies and Unresolved Issues
Serum cortisol is measured as the total rather than free cor-
tisol, and more than 90% of cortisol is protein-bound. In
critically ill patients, low serum albumin and serum proteins
may cause lower serum total cortisol but normal free corti-
sol. Therefore, some patients might be labeled incorrectly as
having cortisol deficiency. In a recently published study,
baseline and postcosyntropin total cortisol were lower in
patients with serum albumin levels of less than 2.5 g/dL com-
pared with those with higher serum albumin levels. Despite
this finding, baseline and postcosyntropin free cortisol meas-
urements were often not different. Thus, in this study, almost
40% of patients with low serum albumin levels had low total
cortisol levels, but all had normal adrenal function. Because
free cortisol measurements are not widely available, it is not
clear how to interpret low serum total cortisol in the face of
hypoproteinemia. The safest course would be to continue to
give these patients glucocorticoid replacement but recognize
that some of the patients may be treated unnecessarily.
Another controversial issue has been the use of corticos-
teroids in patients with septic shock. Some studies suggest
that hydrocortisone at dosages similar to replacement for
adrenal insufficiency improves outcome in septic shock.
Benefit was seen almost exclusively in those with an increase
in serum cortisol level of less than 9 μg/dL in response to cor-
ticotropin, despite some patients having supraphysiologic
baseline serum cortisol levels. A cytokine-induced “relative”
adrenal insufficiency has been postulated, but it is not clear
that patients with high cortisol levels require replacement.
However, a recent study did not find that corticosteroids
benefit septic shock patients, and one recommendation is to
use corticosteroids only if baseline cortisol levels are very low
or if etomidate had been given within 24 hours.
Alonso N et al: Evaluation of two replacement regimens in primary
adrenal insufficiency patients: Effects on clinical symptoms,
health-related quality of life and biochemical parameters.
J Endocr Invest 2004;27:449–54. [PMID: 15279078]
Annane D et al: Diagnosis of adrenal insufficiency in severe sepsis
and septic shock. Am J Respir Crit Care Med 2006;174:1319–26.
[PMID: 16973979]
Cooper MS, Stewart PM: Corticosteroid insufficiency in acutely ill
patients. N Engl J Med 2003;348:727–3. [PMID: 12594318]
Dittmar M, Kahaly GJ: Polyglandular autoimmune syndromes:
Immunogenetics and long-term follow-up. J Clin Endocrinol
Metab 2005;88:2983–92. [PMID: 12843130]
Hamrahian AH, Oseni TS, Arafah BM: Measurements of serum
free cortisol in critically ill patients. N Engl J Med 2004;350:
1629–38. [PMID: 15084695]
Ho JT et al: Septic shock and sepsis: A comparison of total and free
plasma cortisol levels. J Clin Endocrinol Metab 2006;91:105–14.
[PMID: 16263835]
Minneci PC et al: Meta-analysis: The effect of steroids on survival
and shock during sepsis depends on the dose. Ann Intern Med
2004;141:47–56. [PMID: 15238370]
Sprung CL, Annane D, Keh D et al. Hydrocortisone therapy for
patients with septic shock. N Engl J Med 2008;358:111–24.
[PMID: 18184957]
Sick Euthyroid Syndrome
ESSENTIALS OF DIAGNOSIS
Low T
3
and/or low total T
4
suggestive of hypothy-
roidism in a patient with acute or chronic nonthyroidal
illness.
But patient is euthyroid, as shown by clinical appear-
ance, normal TSH, usually normal TSH response to
thyrotropin-releasing hormone (TRH), and normal free
T
4
by equilibrium dialysis.
In extremely ill patients, free T
4
may fall to subnormal
levels.
General Considerations
Alterations in thyroid function occurring with nonthyroidal
illness are usually associated with changes in other hormonal
systems and can be thought of as part of a complex and mul-
tifaceted response of the endocrine system to illness. A num-
ber of nonthyroidal illnesses produce alterations in thyroid
function in patients in whom no intrinsic thyroid disease is
present and the patient is judged to be euthyroid. These low
T
3
and low T
3
-T
4
syndromes seen with nonthyroidal illness
represent a continuum probably reflecting severity of the dis-
ease process rather than discrete conditions. The syndromes
must be distinguished from hypothyroidism because their
treatment requires correction of the underlying disorder
rather than thyroid hormone replacement.
Pathophysiology
The sick euthyroid syndrome is essentially a laboratory diag-
nosis (Table 25–4). Patients are clinically euthyroid, but
because they have acute or chronic nonthyroidal illness, the
underlying disease may make assessment of thyroid status
difficult or unclear. The syndrome may be divided into three
