Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.


PULMONARY DISEASE
557
when used in the setting of venous thromboembolism.
Bleeding is usually not spontaneous but due to some underly-
ing cause. Heparin-induced thrombocytopenia may con-
tribute to bleeding, as may simultaneous administration of
antiplatelet agents such as aspirin or dextran. Warfarin and
other oral anticoagulant agents are also associated with bleed-
ing complications. Bleeding has been demonstrated to be less
common when excessively prolonged coagulation times are
avoided.
The effect of UFH can be quickly counteracted by discon-
tinuing its infusion and administering protamine sulfate.
Approximately 1 mg of protamine will neutralize 100 units of
circulating heparin. The reversal of subcutaneously adminis-
tered UFH may require a prolonged infusion of protamine.
Patients who use a protamine-based insulin preparation, have
undergone a vasectomy, or have known hypersensitivity to fish
are at increased risk of developing adverse allergic reactions to
protamine, including anaphylaxis. The effects of LMWH are
only in part reversed by the administration of protamine.
Nonbleeding patients on warfarin with an elevated INR but
in the less than 5.0 range can safely have warfarin withheld
until the INR falls into the therapeutic range. For INR values
between 5.0 and 9.0, low-dose vitamin K (<5 mg oral phy-
tonadione) is indicated if there is bleeding, high risk of bleed-
ing, or need for performing an invasive procedure. If the INR
is greater than 9.0 and associated with bleeding, oral vitamin
K in larger doses (5–10 mg) is necessary. For serious bleeding
at any elevation of INR, treatment is a 10 mg slow intra-
venous infusion of vitamin K supplemented with factor
replacement (eg, fresh-frozen plasma or prothrombin com-
plex concentrate). Restoration of the desired anticoagulated
state may be difficult and prolonged if too much vitamin K is
administered. Reversal of the effects of warfarin with oral or
intravenous vitamin K can take several hours to correct the
INR, whereas fresh-frozen plasma, which contains the vitamin
K–dependent factors inhibited by warfarin, can be given to
reverse the prothrombin time relatively quickly.
An important complication of heparin use is heparin-
induced thrombocytopenia syndrome, an immune-mediated
disease that is associated with both bleeding and venous and
arterial thrombotic complications. This syndrome should be
suspected when the platelet count falls precipitously in a
patient receiving any form of heparin. It is seen in approxi-
mately 3–4% of patients receiving UFH and fewer patients
receiving LMWH. Treatment of this syndrome includes
immediate discontinuation of all forms of heparin adminis-
tration, including intravenous flushes. If anticoagulation is
still necessary for the patient’s primary disease process, direct
thrombin inhibitors (eg, lepirudin, bivalirudin, and arga-
troban) or heparinoids (eg, danaparoid) can be used. Case
reports of using fondaparinux, a synthetic pentasaccharide
anticoagulant, in cases of heparin-induced thrombocytope-
nia are also in the literature. However, this drug is not currently
FDA approved for this indication, but may play a role in the
future as more evidence becomes available. Warfarin should
not be used alone.
B. Thrombolytic Therapy—Thrombolytic agents currently
approved for use in venous thromboembolic disease in the
United States are urokinase, streptokinase, and alteplase (ie,
recombinant tissue plasminogen activator [tPA]). Deep
venous thrombosis, especially in patients with extensive
iliofemoral thrombosis with limb threat owing to vascular
occlusion, is an approved indication for the use of throm-
bolytic agents according to the 2004 American College of
Chest Physician guidelines. In studies in which thrombolytic
therapy was given for pulmonary embolism the associated
deep vein thrombosis resolved more rapidly, and there was
evidence that destruction of venous valves was lessened,
decreasing the pain, swelling, and potential for postphlebitic
venous insufficiency. However, thrombolytic therapy should
be individualized and is not currently recommended as rou-
tine therapy for deep vein thrombosis.
In short-term studies of pulmonary embolism, throm-
bolytic therapy was associated with faster clot lysis than
heparin, decreased pulmonary hypertension, improved pul-
monary perfusion, and subsequent higher pulmonary capil-
lary blood volume, as assessed by carbon monoxide diffusing
capacity. A trend toward lower death rates in patients with pul-
monary embolism treated with urokinase followed by heparin
compared with those given heparin alone was seen in one trial;
in the first 2 weeks of treatment, 7% died in the urokinase
group compared with 9% in the heparin group. Lower num-
bers of recurrent pulmonary emboli in the urokinase-treated
group also were found. Despite these results, many physicians
believe that the benefits of thrombolytic therapy over antico-
agulation alone are not clear for patients with pulmonary
embolism. Thus the vast majority of patients are treated with
heparin and oral anticoagulation alone.
Thrombolytic therapy has been considered most often in
the setting of “massive”pulmonary embolism, described in ear-
lier studies based on the radiographic finding of a clot occupy-
ing over 50% of the pulmonary vascular bed. Occlusion of
much smaller amount of the pulmonary vascular bed may be
considered “massive” in a patient with significant underlying
cardiopulmonary disease. Rather than the size of the radio-
graphic occlusion itself defining a massive pulmonary
embolism, this syndrome is now defined by the presence of
severe hemodynamic compromise with hypotension, shock,
syncope, or severe gas-exchange abnormalities. Several small
clinical trials of patients with severe large pulmonary emboli
have shown faster lysis of clot in the pulmonary circulation,
reduction of pulmonary artery pressure, and improved cardiac
output with the combination of thrombolytic agent and
heparin compared with heparin alone. However, a survival
benefit has not been clearly established with this therapy and
the risk of bleeding is higher than when heparin is used alone.
At present, thrombolytic therapy should be considered in
patients with acute massive embolism who are hemodynami-
cally unstable and who appear to be able to tolerate throm-
bolysis. It may also be a consideration in patients with
“submassive” embolism who show evidence of right ventric-
ular (RV) dysfunction, but this area remains controversial.

CHAPTER 24
558
RV dysfunction appears to identify normotensive patients
who have a significantly higher risk of recurrent pulmonary
embolism and death, and therefore, thrombolysis may bene-
fit this subgroup of patients. Mortality rates between 4.3%
and 12.8% have been seen in patients with an acute pul-
monary embolism with evidence of RV dysfunction as com-
pared with rates between 0% and 0.9% in patients with
normal right-sided heart function. Echocardiography has
become a key tool used to evaluate right-sided heart function
in these patients. Echocardiographic findings suggestive of
RV dysfunction acutely related to a pulmonary embolism
include qualitative findings such as RV hypokinesis and
quantitative finding such as enlarged RV to LV end-diastolic
diameter greater than 1 mm, RV end-diastolic diameter
greater than 30 mm, and pulmonary artery systolic pressure
greater than 30 mm Hg. Another echocardiographic finding
that has been found to have a high specificity in the diagnosis
of an acute pulmonary embolism is the McConnell sign in
which the RV fee wall is hypokinetic in the face of preserved
contractility of the apical segment.
Most investigators previously recommended that pul-
monary angiography be used to confirm the diagnosis of
pulmonary embolism prior to the administration of throm-
bolytic therapy. However, one analysis found that the fre-
quency of major bleeding averaged 14% in patients who
received tissue plasminogen activator after pulmonary
angiography, whereas it was estimated from thrombolytic
trials in acute myocardial infarction patients that a noninva-
sive diagnosis of pulmonary embolism would be associated
with only a 4.2% risk of bleeding. These authors suggested
that it would be safer to avoid pulmonary angiography for
patients chosen to receive thrombolytics who have positive
findings on a CT pulmonary angiogram, a high-probability
lung scan, an intermediate-probability scan plus high clinical
suspicion, or evidence of significant RV dysfunction by
echocardiography. A comparison of relative risks may prove
useful in making decisions about pulmonary angiography
and thrombolytic therapy.
Contraindications to thrombolytic therapy include sur-
gery in the past 10 days, recent puncture or invasion of non-
compressible vessels, recent intracerebral hemorrhage or
stroke, uncontrolled hypertension, recent trauma, preg-
nancy, hemorrhagic retinopathy, other sites of potential
bleeding, and infective endocarditis. In addition, streptoki-
nase has been associated with allergic reactions given its anti-
genic properties and cannot be administered more than once
in a 6-month period. Customary invasive vascular proce-
dures such as arterial blood gas measurements and catheter-
ization sites where bleeding cannot be easily controlled
should be avoided. Pulmonary angiography, if done, should
be approached from the brachial vein rather than from the
femoral vein. Heparin should be discontinued before starting
thrombolytic agents; antiplatelet agents should not be given
simultaneously.
Streptokinase, urokinase, and alteplase have been used
in pulmonary embolism. Urokinase and streptokinase are
given as a loading dose (streptokinase: 250,000 units over
30 minutes; urokinase: 4400 units/kg over 10 minutes), followed
by continuous infusion (streptokinase: 100,000 units/h for
24 hours; urokinase: 4400 units/kg per hour for 12–24
hours). Alteplase usually has been administered as a contin-
uous peripheral infusion of 100 mg over 2 hours.
After completion of thrombolytic therapy with any of
these agents, the continuous infusion of heparin is reinsti-
tuted once the measured aPTT is less than 2.5 times control.
Streptokinase and urokinase activate plasminogen bound to
both fibrinogen and fibrin, but alteplase or tissue plasmino-
gen activator, a genetic recombinant product, is somewhat
more specific for activation of plasminogen bound to fibrin.
This difference suggestes that alteplase may be associated
with fewer bleeding complications than urokinase or strep-
tokinase, but clinical bleeding so far has been found to be
similar for all three agents.
C. Inferior Vena Cava Interruption—There are no data
supporting the routine use of inferior vena cava (IVC) inter-
ruption with a filter in patients with deep venous thrombosis
or pulmonary emboli. A study comparing anticoagulation
with anticoagulation plus placement of an IVC filter demon-
strated a slight reduction in early symptomatic or asympto-
matic pulmonary embolism. There was no effect on
mortality. After 3 years, a significant increase in recurrent
deep venous thrombosis was found in the IVC filter group.
These data, however, support the effectiveness of IVC
interruption in reducing early embolization. Therefore, three
main indications have evolved for interruption of the infe-
rior vena cava in patients with deep venous thrombosis and
pulmonary embolism. First, patients who are at high risk for
pulmonary embolism (proximal deep venous thrombosis) in
whom heparin is contraindicated should be strongly consid-
ered for the procedure. The contraindication may be a strong
likelihood of bleeding prior to anticoagulation or moderate
to severe bleeding during heparin therapy. For example, in
trauma patients admitted to the ICU who were treated for
deep venous thrombosis or pulmonary embolism with
heparin, 36% developed complications requiring termina-
tion of the drug, whereas no serious complications or deaths
were reported in 34 other patients who underwent place-
ment of an IVC filter. A second indication is failure of anti-
coagulation to prevent recurrent pulmonary embolism
despite an adequate dose and duration of therapy. However,
early embolism after initiation of heparin generally should
not be considered as necessitating IVC interruption because
poorly organized thrombi may detach themselves from the
venous wall or from other parts of the clot regardless of
heparin therapy. Finally, a clinical indication for IVC inter-
ruption is identified in the rare patient whose cardiac and
pulmonary reserves are so low that even a single small pul-
monary thromboembolus may be life-threatening.
The decision to proceed with interruption of the IVC
should be based on evidence that the thromboemboli are
coming from deep veins that flow into that vessel. The right

PULMONARY DISEASE
559
atrium and ventricle and the upper extremities should be
excluded as sources. If an upper extremity is identified as the
continued source of emboli, some centers are capable of
placing superior vena cava filters. Contrast venography or
other proof of existing clot below the site of planned inter-
ruption should be obtained.
The Greenfield filter or other types of intravenous
devices is used most often, while surgical ligation of the IVC
is rarely needed. The filter can be placed via percutaneous
venous access under fluoroscopic guidance either from an
internal jugular vein or from a femoral vein. The filter usu-
ally is positioned below the level of the renal veins, but there
are reports of its being placed above the renal veins in
patients with IVC and renal vein thrombosis. If the filter is
placed because of recurrent pulmonary emboli during anti-
coagulation, anticoagulation usually is continued to prevent
additional thrombi from forming on the filter and else-
where. If the filter is placed because of a contraindication
for or adverse reaction to anticoagulation, anticoagulation
therapy is not given. The risk of recurrent pulmonary
emboli after interruption of the vena cava with this device
is low (2–3%). Other reported problems include procedural
complications, filter malposition and migration, caval
occlusion, and sepsis owing to device infection.
D. Other Treatment—In some centers, emergent pul-
monary embolectomy can be performed in selected patients.
Mortality is high (up to 30% in some series), and special
experience and expertise are needed. Other modalities cur-
rently being investigated include local instillation of throm-
bolytics directly into the embolus; intravascular catheter
disruption systems, including fragmentation, rotor devices,
and rheolytic therapy that break the clot into smaller pieces
that then can be removed; suction catheter removal of the
clot; and balloon angioplasty of the embolus.
E. Supportive Care—Abnormal pulmonary gas exchange
may require supplemental oxygen. Severe respiratory dis-
tress, because of involvement of large portions of the lungs
or because of underlying heart or lung disease, may necessi-
tate mechanical ventilatory support. Some patients may have
bronchospasm that benefits from bronchodilators.
Hemodynamic compromise in pulmonary embolism usually
indicates severe obstruction of the pulmonary circulation
with failure of the right ventricle. Volume loading of the right
ventricle may be helpful. However, volume overexpansion
can lead to increasing right ventricular myocardial oxygen
consumption and subsequent ischemia and deterioration of
function. Inotropic and vasoactive drugs generally are of
little value in severe hemodynamic compromise, but
dopamine, dobutamine, and norepinephrine may be tried.
Prevention
Prevention of deep venous thrombosis and thereby of pul-
monary embolism has become a major goal in the manage-
ment of critically ill patients who are at high risk of
development of deep venous thrombosis as a consequence of
bed rest, immobility, central venous catheterization, critical
illness, or trauma. It has been pointed out, however, that
many ICU patients are not receiving thromboembolism pro-
phylaxis despite this high risk.
The risk of developing a deep vein thrombosis varies with
the clinical scenario and the patient’s underlying medical
condition. Patients with hip fracture, total hip replacement,
or total knee replacement have a 40–70% chance of develop-
ing deep venous thrombosis. Other surgical and medical
patients have approximately a 15–50% risk. It is estimated
that patients with myocardial infarction have about a 24%
overall incidence of deep venous thrombosis, and patients
with stroke may have up to a 55% risk.
Prevention of deep venous thrombosis depends on rever-
sal of predisposing conditions (eg, the local hypercoagulable
state and venous stasis). Antithrombotic therapy can interfere
with thrombus formation either by preventing the platelet
nidus from forming or by preventing activation of the coagu-
lation cascade. The type of preventive therapy is closely linked
to the underlying condition and the bleeding risk. For exam-
ple, patients at moderate risk (eg, minor surgery with additional
risk factors or aged 40 to 60 years with no additional risks)
will benefit from low-dose UFH, LMWH, or intermittent
pneumatic compression of the legs. On the other hand, high-
risk patients including hip fracture or total knee replacement
patients must be treated with LMWH, fondapariunux (2.5
mg started 6–8 hours after surgery), or adjusted-dose war-
farin with a target INR of 2.5. A summary of recommenda-
tions is presented in Table 24–9.
Low-dose UFH, 5000–7500 units subcutaneously every
8–12 hours, has been shown to be effective and safe in several
groups of patients, including those immediately postopera-
tive from general or gynecologic surgery and medical
patients with heart failure, myocardial infarction, respiratory
failure, and stroke. At these doses, the aPTT is not usually
prolonged, and there is little increased risk of bleeding.
LMWH also has been shown to have reliably favorable dose-
response properties and turns out to be superior for prophy-
laxis of deep venous thrombosis in a number of clinical
settings. Warfarin is effective in certain clinical situations
and, for example, is one of the choices for prophylactic treat-
ment for patients with hip fractures as well as elective hip
and knee replacement surgeries. Fondaparinux, a synthetic
pentasaccharide that selectively inhibits factor Xa activity,
has been shown to be highly efficacious in the prevention of
deep vein thrombosis primarily in large orthopedic surgical
trials. Finally, mechanical methods of prophylaxis with grad-
uated compression stockings or external compression of the
legs can be provided by rhythmic intermittent pneumatic
compression devices and have been shown to have compara-
ble effectiveness in preventing deep venous thrombosis with
no risk of hemorrhage. These devices can be combined with
pharmacologic means of prophylaxis in very high-risk
patients or used alone in patients at risk of bleeding compli-
cations from medical therapy.
CHAPTER 24
560
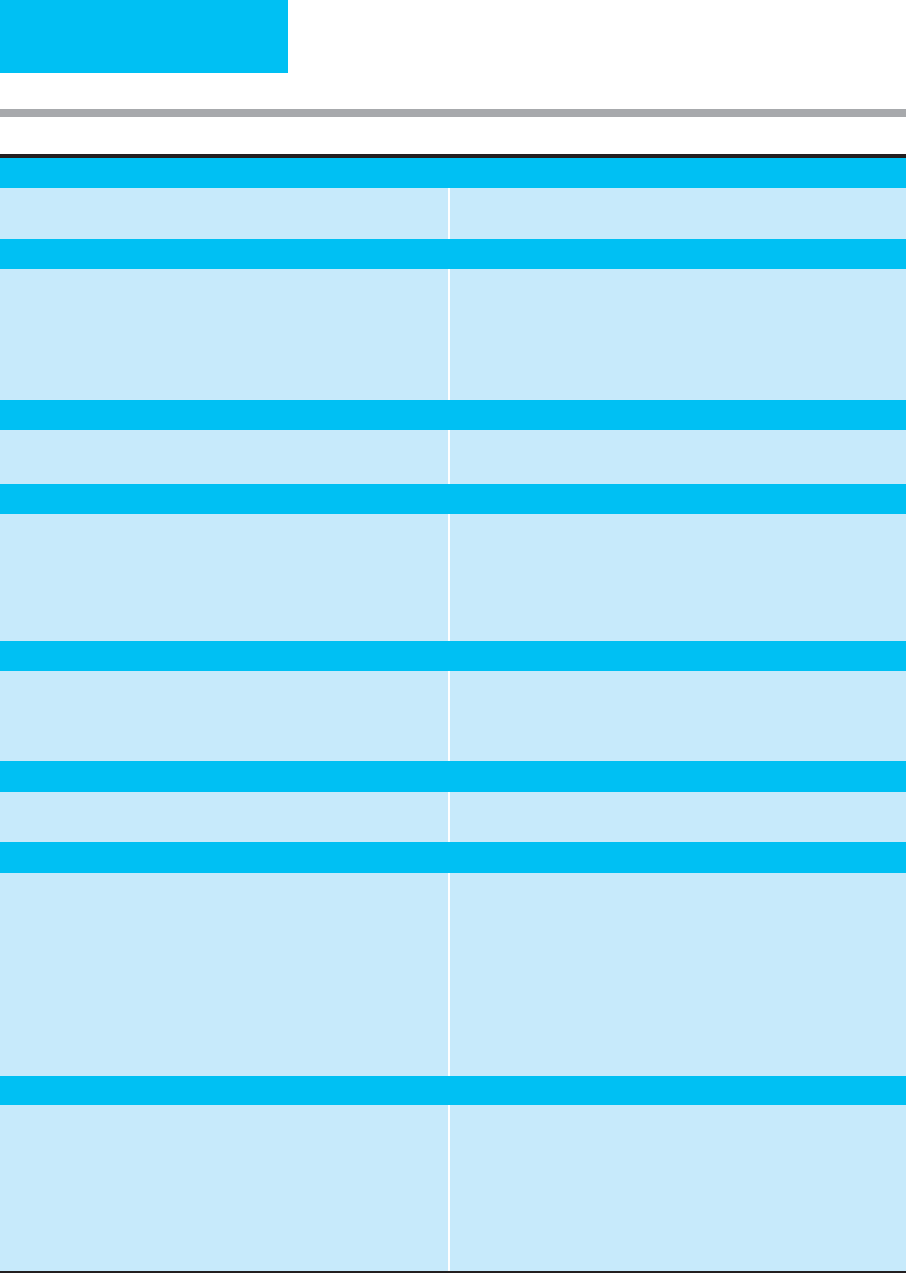
Medical Conditions
Critically ill patients with high bleeding risk
Critically ill patients without high bleeding risk
Mechanical prophylaxis (ES or IPC) until risk diminishes
LDUH or LMWH with or without mechanical prophylaxis
General Surgery
Low risk (minor procedure, age <40, no risk factors)
Moderate risk (40–60 years, major procedure and <40 years
with no risk factors)
High risk (not low or moderate risk) and highest risk (multiple
risk factors)
High risk of bleeding
Early and persistent ambulation
LDUH, 5000 units bid or LMWH <3400 units once/day
LDUH, 5000 units tid or LMWH >3400 units once/day or LMWH with
mechanical prophylaxis (higher risk)
Mechanical prophylaxis (ES or IPC) until risk diminishes
Vascular Surgery
Low-risk procedure
High-risk procedure
No routine prophylaxis
LDUH or LMWH
Gynecologic Surgery
Procedure <30 min for benign disease
Laparoscopic procedure, risk factors present
Major surgery for benign disease
Extensive surgery for malignancy
Early and persistent ambulation
LDUH, LMWH, and/or mechanical prophylaxis
LDUH, 5000 units bid; LDUH, 5000 units tid if VTE risk factors; continue
until discharge; if age >60, continue for 2–4 weeks after discharge
LDUH 5000 units tid or LMWH >3400 units/day; continue for 2–4 weeks
after discharge
Urologic Surgery
Minor, transurethral procedure
Major open procedure
Bleeding or high risk of bleeding
Early and persistent ambulation
LDUH twice or three times daily; with multiple risk factors, add
mechanical prophylaxis
Mechanical prophylaxis (ES or IPC) until risk diminishes
Laparoscopic Surgery
Laparoscopic surgery Early and persistent ambulation, unless risk factors present, then LDUH,
LWMH, and/or mechanical prophylaxis
Orthopedic Surgery
Elective total hip replacement
Elective total knee replacement
Hip fracture surgery
LMWH at high-risk dose, 12 h before surgery or 12–24 h after surgery, or
4–6 h after surgery at half the high-risk dose; increase to high-risk dose
the next day
or
fondaparinux 2.5 mg beginning 6–8 h after surgery
or
adjusted-dose warfarin started the evening after surgery (INR target 2.5)
Continue prophylaxis for 28–35 days after surgery
LMWH at high-risk dose, fondaparinux, or adjusted-dose warfarin (INR
target 2.5)
Fondaparinux, LMWH at high-risk dose, adjusted-dose warfarin (INR target
2.5), or LDUH; continue for 28–35 days after surgery
Table 24–9. Prophylaxis of deep vein thrombosis and pulmonary embolism for patients.
Neurosurgery, Trauma, Spinal Cord Injury
Elective spine procedure (elderly, malignancy, neurologic deficit, prior
to VTE, or anterior surgical approach)
Trauma, identifiable risk factor
Acute spinal cord injury
Postoperative LDUH, LMWH, or IPC alone; if multiple risk factors, combine
LDUH or LMWH with mechanical prophylaxis
LMWH, when safe; mechanical prophylaxis if LMWH is delayed or
contraindicated because of high bleeding risk; consider screening with
ultrasound for those at highest risk; continue LMWH or warfarin (INR
target 2.5) after discharge if impaired mobility
Mechanical prophylaxis; add LDUH or LWMH started when safe (hemostasis
achieved)

PULMONARY DISEASE
561
However, in patients with trauma—especially to the brain
or spinal cord—or those undergoing surgical procedures of
the eye, brain, or spinal cord, even low-dose heparin may be
contraindicated because of the increased risk of bleeding at
these operative sites. External pneumatic compression of the
legs is effective in these patients. Neurosurgical patients and
patients with heparin-induced thrombocytopenia also
should be considered for prevention of deep venous throm-
bosis by pneumatic compression devices. This therapy gener-
ally is well tolerated, but patients may require sedation owing
to discomfort from the cyclic compression or heat generated
by the apparatus.
Hip fractures, major orthopedic surgery, and some types
of urologic surgery enhance the thrombogenic state, prob-
ably by increased contact with and release of tissue throm-
boplastin. While low-dose UFH does decrease the risk of
deep venous thrombosis in some of these patients, it is less
effective than LMWH and the newer anticoagulant fonda-
parinux. Current guidelines recommend the use of LMWH,
fondaparinux, or adjusted-dose warfarin (goal INR 2.5) in
these high-risk orthopedic patients. Adjunctive prophylaxis
with mechanical devices such as elastic stockings and inter-
mittent pneumatic compression devices can add additional
benefit with little risk. The duration of prophylaxis, espe-
cially in this orthopedic patient population, is being inves-
tigated. There is some evidence that extending the period of
prophylaxis to 28–35 days postoperatively has reduced the
incidence of deep venous thrombosis and subsequent pul-
monary embolism. The 2004 ACCP consensus guidelines
recommend extending prophylaxis into the outpatient set-
ting with LMWH, fondaparinux, or warfarin for a total of
4–5 weeks after surgery for these high-risk postoperative
patients.
IVC filters also have been studied for their use in the pre-
vention of complications from deep venous thrombosis, pri-
marily in the surgical population. Four studies evaluating
high-risk surgical patients without current evidence of deep
venous thrombosis using historical controls found a decreased
incidence of pulmonary emboli in the following patients who
had an IVC filter placed: those with high injury severity scores,
head or spinal cord trauma, pelvic or lower extremity frac-
tures, prolonged immobility, and mechanical ventilatory sup-
port. This means of prophylaxis has not been studied in direct
comparison with heparin or mechanical devices. Other patient
populations that may benefit from prophylactic filter place-
ment include patients with advanced malignancy, orthopedic
surgical patients, and patients with limited cardiopulmonary
reserve such as those with severe COPD. The use of these fil-
ters as prophylaxis remains controversial and requires larger
studies to determine their exact role.
Current Controversies and Unresolved Issues
The diagnosis of pulmonary embolism in the critically ill
patient with multiple preexisting diseases can be very difficult.
The incidence of pulmonary embolism complicating critical
illness is unknown, but 5–10% of deaths may be associated
with unsuspected pulmonary emboli. In a study of patients
with COPD exacerbation, 25% of those without obvious pre-
cipitating cause had pulmonary embolism. Risk was associ-
ated with malignancy, prior venous thromboembolic disease,
and decrease in Pa
CO
2
of at least 5 mm Hg. Abnormal pul-
monary gas exchange and hemodynamic compromise result-
ing from new pulmonary emboli may not be identified in
patients who already have underlying lung or heart disease.
Defects on perfusion lung scans may or may not represent
pulmonary emboli in patients with abnormal chest x-rays,
and ventilation scans cannot be performed without special
arrangements for patients receiving mechanical ventilation.
The helical or spiral CT scan requires administration of con-
trast material and a degree of patient cooperation and breath-
holding to achieve adequate imaging. Again, this may be
difficult for critically ill patients to perform. Finally, treatment
issues are complex, with some patients having relative con-
traindications to anticoagulation and others having diseases
in which adequate anticoagulation is difficult to achieve.
Patients with worsening hypoxemia or increased physio-
logic dead space, increased pulmonary artery pressure (in the
absence of other causes), unexplained tachycardia or
hypotension, or other features of unclear cardiopulmonary
insufficiency should be suspected of having pulmonary
thromboembolic disease until proven otherwise. The use of
end-tidal CO
2
monitors in the ICU may be a noninvasive
means for detecting an acute change in dead space ventila-
tion that may be an early clue for pulmonary embolism.
Ventilation-perfusion scans in patients with COPD gen-
erally are considered to be of limited value because airway
obstruction causes falsely positive perfusion defects. A study
of such patients suspected of having a pulmonary embolism
found that high-probability scans were rare but had a high
predictive value for pulmonary embolism; similarly, a nor-
mal perfusion scan was highly predictive of a normal pul-
monary angiogram. However, 90% of the group had
intermediate-probability (60%) or low-probability (30%)
scans, of which only 17% had pulmonary embolism con-
firmed by angiography. The authors of the study concluded
that ventilation-perfusion lung scans were helpful only if
they were high-probability or normal. In all others, they con-
cluded, sufficient clinical suspicion should lead to pul-
monary angiography.
Ansell J et al: The pharmacology and management of the vitamin
K antagonists. Chest 2004;126:204–33S. [PMID: 15383473]
Augustinos P, Ouriel K: Invasive approaches to treatment of
venous thromboembolism. Circulation 2004;110:I27–34. [PMID:
15339878]
Buller HR et al: Antithrombotic therapy for venous thromboem-
bolic disease. Chest 2004;126:401–28S. [PMID: 15383479]
Carlbom DJ, Davidson BL: Pulmonary embolism in the critically
ill. Chest 2007;132:313–24. [PMID: 17625093]
Chunilal SD et al: Does this patient have pulmonary embolism?
JAMA 2003;290:2849–58. [PMID: 14657070]
CHAPTER 24
562
Dong B et al: Thrombolytic therapy for pulmonary embolism.
Cochrane Database Syst Rev 2006;2:CD004437. [PMID: 16625603]
Fedullo PF, Tapson VF: The evaluation of suspected pulmonary
embolism. N Engl J Med 2003;349:1247–56. [PMID: 14507950]
Geerts WH et al: Prevention of venous thromboembolism. Chest
2004;126:338–400S. [PMID: 15383478]
Hirsh J et al: Heparin and low-molecular weight-heparin. Chest
2004;126:188–203S. [PMID: 15383472]
Hogg K et al: Diagnosis of pulmonary embolism with CT pul-
monary angiography: A systematic review. Emerg Med J
2006;23:172–8. [PMID: 16498151]
Hull RD et al: Low-molecular-weight heparin vs heparin in the
treatment of patients with pulmonary embolism. Arch Intern
Med 2000;160:229–36. [PMID: 10647762]
Kreit JW: The impact of right ventricular dysfunction on the prog-
nosis and therapy of normotensive patients with pulmonary
embolism. Chest 2004;125:1539–45. [PMID: 15078772]
Kruip MJHA et al: Diagnostic strategies for excluding pulmonary
embolism in clinic outcome studies: A systematic review. Ann
Intern Med 2003;138:941–51. [PMID: 12809450]
Kucher N et al: Massive pulmonary embolism. Circulation
2006;113:577–82. [PMID: 16432055]
Kucher N et al: Prognostic role of echocardiography among
patients with acute pulmonary embolism and a systolic arterial
pressure of 90 mm Hg or higher. Arch Intern Med
2005;165:1777–81. [PMID: 16087827]
Kucher N, Goldhaber SZ: Risk stratification of acute pulmonary
embolism. Semin Thromb Hemost 2006;32:838–47. [PMID:
17171598]
Kutinsky I et al: Normal D-dimer levels in patients with pul-
monary embolism. Arch Intern Med 1999;159:1569–72. [PMID:
10421279]
Le Gal G et al: Prediction of pulmonary embolism in the emer-
gency department: The revised Geneva score. Ann Intern Med
2006;144:165–71. [PMID: 16461960]
Levine MN et al: Hemorrhagic complications of anticoagulant
treatment: The Seventh ACCP Conference on Antithrombotic
and Thrombolytic Therapy. Chest 2004;126:287–310S. [PMID:
15383476]
Low-molecular-weight heparin in the treatment of patients with
venous thromboembolism. The Columbus Investigators. N
Engl J Med 1997;337:657–62. [PMID: 9280815]
Moores LK et al: Meta-analysis: Outcomes in patients with sus-
pected pulmonary embolism managed with computed tomo-
graphic pulmonary angiography. Ann Intern Med 2004;141:
866–74. [PMID: 15583229]
Nijkeuter M et al: The natural course of hemodynamically stable
pulmonary embolism: Clinical outcome and risk factors in a
large prospective cohort study. Chest 2007;131:517–23. [PMID:
17296656]
PREPIC Study Group: Eight-year follow-up of patients with per-
manent vena cava filters in the prevention of pulmonary
embolism: The PREPIC (Prevention du Risque d’Embolie
Pulmonaire par Interruption Cave) randomized study.
Circulation 2005;112:416–22. [PMID: 16009794]
Rocha AT et al: Venous thromboembolism in intensive care
patients. Clin Chest Med 2003;24:103–22. [PMID: 12685059]
Roongsritong C et al: Common causes of troponin elevations in
the absence of acute myocardial infarction: Incidence and clin-
ical significance. Chest 2004;125:1877–84. [PMID: 15136402]
Snow V et al: Management of venous thromboembolism: A clini-
cal practice guideline from the American College of Physicians
and the American Academy of Family Physicians. Ann Intern
Med 2007;146:204–10. [PMID: 17261857]
Stein PD et al: Multidetector computed tomography for acute pul-
monary embolism. N Engl J Med 2006;354:2317–27. [PMID:
16738268]
Streiff MB: Vena caval filters: A review for intensive care specialists.
J Intensive Care Med 2003;18:105–7. [PMID: 15189653]
Tillie-Leblond I et al: Pulmonary embolism in patients with unex-
plained exacerbation of chronic obstructive pulmonary disease:
Prevalence and risk factors. Ann Intern Med 2006;144:390–6.
[PMID: 16549851]
Value of the ventilation-perfusion scan in acute pulmonary
embolism: Results of the prospective investigation of pul-
monary embolism diagnosis (PIOPED). The PIOPED
Investigators. JAMA 1990;263:2753–59. [PMID: 2332918]
van Belle A et al: Effectiveness of managing suspected pulmonary
embolism using an algorithm combining clinical probability, D-
dimer testing, and computed tomography. JAMA 2006;295:
172–9. [PMID: 16403929]
Weitz JI, Linkins LA: Beyond heparin and warfarin: the new gener-
ation of anticoagulants. Exp Opin Investig Drugs 2007;
16:271–82. [PMID: 17302522]
Wood KE: Major pulmonary embolism: Review of a pathophysio-
logic approach to the golden hour of hemodynamically signifi-
cant pulmonary embolism. Chest 2002;121:877–905. [PMID:
11888976]
Anaphylaxis
ESSENTIALS OF DIAGNOSIS
Follows reexposure to foreign antigens such as food,
drug, nonhuman protein, or other substances.
Respiratory tract: rhinitis, edema, laryngeal edema,
asthma.
Hypotension, lightheadedness, collapse.
Generalized erythema, pruritus, and urticarial skin
lesions with or without angioedema.
General Considerations
Anaphylaxis is a severe allergic reaction that occurs after reex-
posure to a foreign substance such as food, a drug, serum, ven-
oms, or nonhuman proteins but also occurs occasionally after
exercise. Approximately 72 hours after initial exposure to a
foreign antigen, IgE antibody synthesis begins. Reexposure to
the antigen promotes cross-linking of mast cell and basophil-
bound IgE molecules and causes the subsequent release of
stored mediators of anaphylaxis such as histamine and other
substances. These factors cause increases in capillary perme-
ability, mucosal edema, and smooth muscle contraction; acti-
vate the classic complement pathway and components of the
clotting cascade; and cause the release of other mediators.

PULMONARY DISEASE
563
Anaphylactoid (ie, anaphylaxis-like) reactions are clini-
cally similar to anaphylaxis but are not mediated by
antigen-antibody interactions. Many of the same mediators
are involved, so treatment is identical to that for anaphy-
laxis. Mechanisms include (1) activation of the comple-
ment cascade by immune complexes or other substances
that cause release of anaphylatoxins (eg, C3a and C5a),
resulting in mediator release from mast cells and
basophils, and (2) direct activation by certain agents of
mast cells and basophils resulting in mediator release (eg,
effect of hyperosmolar solutions such as mannitol and
radiocontrast media).
Patients with anaphylaxis may be admitted to the ICU
because of severe respiratory or cardiovascular compromise,
or they may develop anaphylaxis in the ICU from exposure
to blood products or drugs.
Clinical Features
The onset of a systemic anaphylactic reaction, which may
develop over minutes to 1–2 hours, depends on the sensitiv-
ity of the person as well as the route, rate, and quantity of the
precipitating agent. The clinical signs and symptoms can dif-
fer greatly depending on the severity of the anaphylactic
reaction, and clinical findings may be present in various
combinations. Severe systemic reactions are characterized by
respiratory failure and cardiovascular collapse. Recurrence of
symptoms can occur 2–24 hours after onset despite initial
stabilization and treatment.
A. History—A history of recent use of medication, ingestion
of new or unusual foods (notably peanuts and other nuts and
shellfish), and exposure to toxic products such as venoms or
insect bites should be sought, but treatment should be initi-
ated immediately if necessary. An increasingly recognized
cause of allergy and anaphylaxis is exposure to latex rubber.
About half of patients will have a history of atopy, and only
about 70% of patients who develop anaphylaxis outside
the hospital will have an identifiable precipitating cause. In
the ICU, intravenous contrast agents, antibiotics, NSAIDs,
aspirin, and other drugs are the most likely causes.
B. Symptoms and Signs—Anaphylaxis is often associated
with severe anxiety and apprehension. Patients may experi-
ence any combination of the following symptoms: itching of
skin and mucosal surfaces, swelling of the lips and tongue,
hoarseness, coughing, shortness of breath, wheezing, vomit-
ing, abdominal cramps, diarrhea, and palpitations.
Physical findings in severe systemic reactions include
hypotension, upper airway obstruction resulting in stridor,
and bronchospasm with impaired gas exchange, hypercap-
nia, and wheezing. Loss of consciousness may result from
poor cerebral perfusion. Urticaria may be present, and there
may be evidence of angioedema.
Allergens injected systemically—for example, insect
stings, intravenous drugs, blood products, and allergy desen-
sitization treatments—often cause a predominantly
cardiovascular reaction with hypotension. Food and inhaled
allergens may cause more facial and respiratory edema, asso-
ciated with respiratory problems.
Differential Diagnosis
Anaphylaxis may be confused with syncopal episodes associ-
ated with metabolic or vascular disturbances, acute respira-
tory failure secondary to epiglottitis, status asthmaticus,
obstruction owing to foreign-body aspiration, and pulmonary
embolism. Similar disorders with cutaneous and respiratory
manifestations—for example, mastocytosis, carcinoid syn-
drome, hereditary angioedema, and other specific adverse
pharmacologic (allergic and nonallergic) reactions to
drugs—should be considered if appropriate.
Treatment
Treatment is based on early recognition of features of ana-
phylaxis combined with a history of exposure to an inciting
agent. The suspected agent should be discontinued if possi-
ble (eg, a drug, blood products, or contact with latex rubber),
the extent and severity of the reaction should be assessed,
and treatment should be initiated as soon as anaphylaxis is
suspected.
A. General Measures—The patient should be positioned
supine or head down with the feet elevated. The airway must
be maintained by proper positioning. If necessary, endotra-
cheal intubation, tracheostomy, or cricothyroidotomy
should be performed. Because of the need for intravenous
fluid infusion and medications, a large-bore intravenous
catheter should be inserted.
B. Initial Treatment—Epinephrine should be given first in
a dosage of 0.3–0.5 mL of 1:1000 dilution (0.3–0.5 mg)
intramuscularly deep into the thigh every 10–20 minutes as
needed. The subcutaneous route is no longer recom-
mended. In severe anaphylaxis with suspicion of poor per-
fusion, slow intravenous injection (5 mL of 1:10,000
dilution) should be considered. Other initial treatment
includes oxygen, inhaled β-adrenergic agonists for bron-
chospasm, and airway management.
C. Other Medications—Medications are directed toward
blocking further mediator action on target organs, preventing
further release of mediators, reversing the physiologic effects
of the mediators, and supporting vital functions.
Antihistamines (histamine H1-antagonists) such as
diphenhydramine hydrochloride, 25–50 mg intra-
venously every 6 hours, are useful. Some studies show
additional benefit of histamine H2-receptor antagonists, so
cimetidine or ranitidine may be given as well. Excessive
antihistamine dosages may cause impaired CNS function,
anticholinergic symptoms (eg, dry mouth or urinary reten-
tion), and drowsiness, especially in elderly patients.
Hydrocortisone, 100 mg intravenously every 8 hours for
CHAPTER 24
564
several doses, is recommended, especially if there is bron-
chospasm or airway compromise. Patients who are receiving
β-blockers may have a poor response to treatment directed at
hypotension. These patients may have some response to
glucagon, which has both inotropic and chronotropic effects
on the heart.
D. Intravenous Fluids—Adults should receive 0.9% NaCl
solution, 0.5–1 L intravenously over 30 minutes, if hypoten-
sive. Additional fluid therapy depends on blood pressure,
heart rate, urine output, and clinical response.
E. Prevention of Anaphylaxis—The patient should be
instructed to avoid the offending agent in future, if possible.
For patients who have a likelihood of reexposure to an
identified antigen, a kit containing epinephrine for self-
administration should be considered.
Angioedema
ESSENTIALS OF DIAGNOSIS
Subcutaneous swelling of skin or mucous membranes,
possibly with laryngeal or lower airway compromise.
May present with urticaria.
Acute angioedema: may have history of ACE inhibitor,
aspirin, or NSAID therapy or a history of allergies.
History of recurrent transient episodes of swelling may
be present in allergic or hereditary forms.
General Considerations
Angioedema is produced by mechanisms similar to those
that cause anaphylaxis and anaphylactoid reactions. In addi-
tion, these mechanisms can be triggered by various physical
forces, exercise, and other medical conditions such as
endocrine disorders, infections, malignancies, allergic phe-
nomena, and collagen vascular diseases. Severe angioedema
involving the upper or lower airways is a medical emergency
similar to anaphylaxis.
Acute angioedema, which may occur once or on multiple
occasions, is often idiopathic or associated with allergic phe-
nomena. Among identified causes, the most common are
related to ACE inhibitor therapy, aspirin, and NSAIDs.
Hereditary angioedema is caused by an autosomal domi-
nant inherited deficiency or functional abnormality of C1
esterase inhibitor. Without this inhibitor, the complement
cascade is activated, and a kinin-like fragment and other
mediators are released that produce the angioedema.
Acquired C1 esterase inhibitor deficiency is very rare and
seen in adults with autoimmune or lymphoproliferative
disorders. Patients have unexplained recurrent angioedema,
and the diagnosis is confirmed by low levels of C1q and low
C1 esterase inhibitor activity.
Clinical Features
A. Symptoms and Signs—Angioedema is characterized by
the presence of nonpruritic subcutaneous swelling of the skin
and mucous membranes. Lesions of the skin are poorly
demarcated and reddish. These may occur in conjunction with
urticarial lesions. Involvement of the upper airway can result
in hoarseness, stridor, shortness of breath, and even death.
Likewise, GI involvement is associated with abdominal pain,
nausea, and diarrhea. Patients may or may not have associated
urticaria, characterized by evanescent pruritic lesions.
Because of widespread use of ACE inhibitors for hyperten-
sion, diabetic proteinuria, and congestive heart failure, these
agents are a common cause of acute angioedema. This disor-
der may present after recent initiation of ACE inhibitor ther-
apy but may occur even after prolonged use. It is said that
urticaria is unusual in ACE inhibitor–induced angioedema.
Angiotensin-receptor blockers, sometimes given to patients
instead of or in addition to an ACE inhibitor, rarely have
been associated with angioedema, but some experts have
cautioned against use of these agents in patients with ACE
inhibitor–induced angioedema. Hereditary or acquired
angioedema has been precipitated by ACE inhibitors.
In hereditary angioedema, episodes can be precipitated
by trauma, emotional upset, infections, and exposure to sud-
den temperature changes. The disorder usually is apparent in
childhood, and attacks tend to be recurrent and usually are of
2–4 days duration. The physical findings are similar to those
described earlier. Similar features are present in acquired
forms of angioedema.
B. Laboratory Findings—In patients with angioedema or
urticaria, investigation should include a complete blood
count, erythrocyte sedimentation rate, and urinalysis. Other
laboratory tests should be ordered depending on the under-
lying medical condition. In patients with abdominal symp-
toms, edema of the bowel wall may be seen on CT scan.
When hereditary angioedema is suspected, C4, C3, CH50
or total complement, and C1 esterase inhibitor (by immuno-
chemical and functional assay) should be measured. Levels of
C4 and C2 are always low, and CH50 is usually diminished or
absent during an attack. C1 esterase will be reduced but may
be normal in persons with a functional abnormality.
Acquired angioedema (acquired C1 inhibitor deficiency) is
due to increased catabolism of C1 esterase inhibitor and C1q.
Laboratory findings in allergic angioedema and that induced
by ACE inhibitors and NSAIDs are rarely specific or helpful.
Treatment
Patients may require long-term treatment and should avoid
precipitating conditions and situations. In some patients, the
underlying cause may not be identifiable.

PULMONARY DISEASE
565
A. General Measures—Acute angioedema is treated ini-
tially much the same way as anaphylaxis. The underlying
cause should be treated or removed, especially if ACE
inhibitors have been implicated. Hypotension and shock
should be treated with intravenous fluids. The airway
should be protected, and endotracheal intubation may
become necessary. If there is severe upper airway obstruction,
tracheostomy should be considered.
B. Specific Treatment
1. Epinephrine—Epinephrine is indicated for patients with
severe acute urticaria or angioedema with airway involve-
ment. It can be given subcutaneously or intravenously. One
recommendation is to give 0.3–0.5 mL of 1:1000 solution
subcutaneously and repeat every 10–20 minutes as necessary.
Epinephrine may be lifesaving in angioedema, but it should
be noted that many patients with ACE inhibitor–induced
angioedema are elderly or have heart disease or hyperten-
sion. Epinephrine may cause excessive tachycardia, may
increase myocardial oxygen demand, may provoke myocar-
dial ischemia, and may raise blood pressure excessively.
2. Antihistamines—Antihistamines usually are effective
against urticaria and can be helpful for some forms of
angioedema. H1-blockers such as diphenhydramine, 50 mg
orally or intravenously every 6 hours, are helpful for an acute
episode of urticaria. Patients may have dry mouth, drowsi-
ness, and excessive sedation with these agents. In patients
with angioedema, in addition to H1-blockers, an H2-blocker
such as ranitidine, 50 mg intravenously two or three times
daily or 150 mg orally twice daily, or cimetidine, 300 mg
orally or intravenously every 6 hours, may be helpful.
3. Corticosteroids—Corticosteroids usually are not nec-
essary for acute urticaria alone but can be very helpful in
refractory acute urticaria or chronic urticaria. A recom-
mended initial dosage is prednisone, 2 mg/kg per day
orally, or methylprednisolone, 60 mg intravenously every
6 hours.
C. Hereditary Angioedema—Clinical trials of recombinant
C1 inhibitor concentrate for acute hereditary angioedema
are under way. C1 inhibitor concentrates from pooled
plasma are available in Europe but not in the United States.
Fresh frozen plasma may be given (2 units) as treatment to
prevent angioedema or in preparation for surgery. Long-
term preventive treatment of angioedema can be tried using
androgen derivatives such as danazol, 200 mg orally three
times daily, or stanozolol, 2–4 mg/day.
Bochner BS, Lichtenstein LM: Anaphylaxis. N Engl J Med
1991;324:1785–90. [PMID: 1789822]
Bork K, Barnstedt SE: Treatment of 193 episodes of laryngeal
edema with C1 inhibitor concentrate in patient with hereditary
angioedema. Arch Intern Med 2001;161:714–8. [PMID:
11231704]
Kleiner GI et al: Unmasking of acquired autoimmune C1-inhibitor
deficiency by an angiotensin-converting enzyme inhibitor. Ann
Allergy Asthma Immunol 2001;86:461–4. [PMID: 11345293]
Lieberman P: Use of epinephrine in the treatment of anaphylaxis.
Curr Opin Allergy Clin Immunol 2003;3:313–8. [PMID:
12865777]
Lin RY et al: Improved outcomes in patients with acute allergic
syndromes who are treated with combined H
1
and H
2
antago-
nists. Ann Emerg Med 2000;36:462–8. [PMID: 11054200]

566
00
Several endocrine problems may require management in the
ICU, including severe thyroid disease, acute adrenal insuffi-
ciency, and diabetic ketoacidosis. While these problems usu-
ally are encountered in patients in whom a diagnosis of
endocrine dysfunction has already been made, they are occa-
sionally the presenting manifestation in an undiagnosed
patient. If these endocrine disorders are not identified, spe-
cific treatment such as endocrine replacement therapy may be
delayed, and significant complications or death may ensue.
In this chapter, severe thyrotoxicosis (eg, thyroid storm or
decompensated hyperthyroidism), severe hypothyroidism
(eg, myxedema coma), and acute and chronic adrenal insuffi-
ciency are discussed. Diabetic ketoacidosis and other manifes-
tations of severe diabetes mellitus are covered in Chapter 26.
In this chapter we also discuss the problem of assessing thy-
roid function in severe nonthyroidal illness (ie, sick euthyroid
syndrome).
Thyroid Storm
ESSENTIALS OF DIAGNOSIS
Long-standing hyperthyroidism, uncontrolled or poorly
controlled.
Breakdown of the body’s thermoregulatory mechanisms,
resulting in hyperpyrexia.
Altered mental status.
Precipitating illnesses or events such as thyroid sur-
gery, infection, trauma, acute abdominal problems, or
anesthesia.
Signs and symptoms of severe hyperthyroidism—usually
marked wasting.
General Considerations
Thyroid storm—or thyrotoxic crisis—results from the even-
tual failure of the body’s compensatory mechanisms in
severe hyperthyroidism. Clinically, thyroid storm has been
defined as “a life-threatening augmentation of the manifesta-
tions of hyperthyroidism.” There are no pathognomonic lab-
oratory markers of thyroid storm. However, because of its
high mortality rate, one should be vigilant for its diagnosis
and provide aggressive and prompt management. This is
especially true because the features of thyroid storm are com-
mon findings in other critically ill patients.
A. Incidence—The incidence of thyroid storm has decreased
markedly since the advent of antithyroid drugs. Some studies
suggest that the incidence is 2–8% of all patients admitted to
the hospital for management of hyperthyroidism. However, a
recent evaluation at a major teaching hospital revealed that
severe complicated thyrotoxicosis is a rare syndrome,
accounting for only 0.01% of hospital admissions over a
14-year period. Thyroid storm occurs nine to ten times more
commonly in women than in men, probably a reflection of
the higher incidence of thyroid diseases in women in general.
No race- or age-related differences in incidence have been
reported. An association between thyroid storm and med-
ically underserved, socially disadvantaged populations has
been suggested. In one study, patients admitted because of
complicated thyrotoxicosis were more likely to be uninsured,
poorer, unmarried, and African-American than uncompli-
cated thyrotoxic controls. One explanation is that control of
chronic hyperthyroidism with antithyroid drugs is very effec-
tive in preventing decompensation, but poorer populations
may be less likely to receive adequate treatment.
Pathophysiology
The pathophysiology of thyrotoxic crisis is not well under-
stood. Indices of thyroid gland overactivity (levels of total
and free thyroxine or triiodothyronine) are not significantly
higher than in usual cases of hyperthyroidism.
25
Endocrine Problems in the
Critically Ill Patient
∗
Shalender Bhasin, MD
Piya Ballani, MD
Ricky Phong Mac, MD
∗
Shalender Bhasin, MD, Laurie K. S. Tom, MD, and Phong Mac, MD,
were the authors of this chapter in the second edition.
Copyright © 2008 by The McGraw-Hill Companies, Inc. Click here for terms of use.
