Townsend Courtney M.Jr., Evers B. Mark. Atlas of General Surgical Techniques: Expert Consult
Подождите немного. Документ загружается.


65
MC
Hyoid bone
Anterior jugular vein
Cricoid cartilage
Trachea
Thyroid isthmus
Omohyoid muscle
Thyroid cartilage
Thyroid notch
Sternocleidomastoid
muscle
Thyroid gland
Sternohyoid muscle
Sternal notch
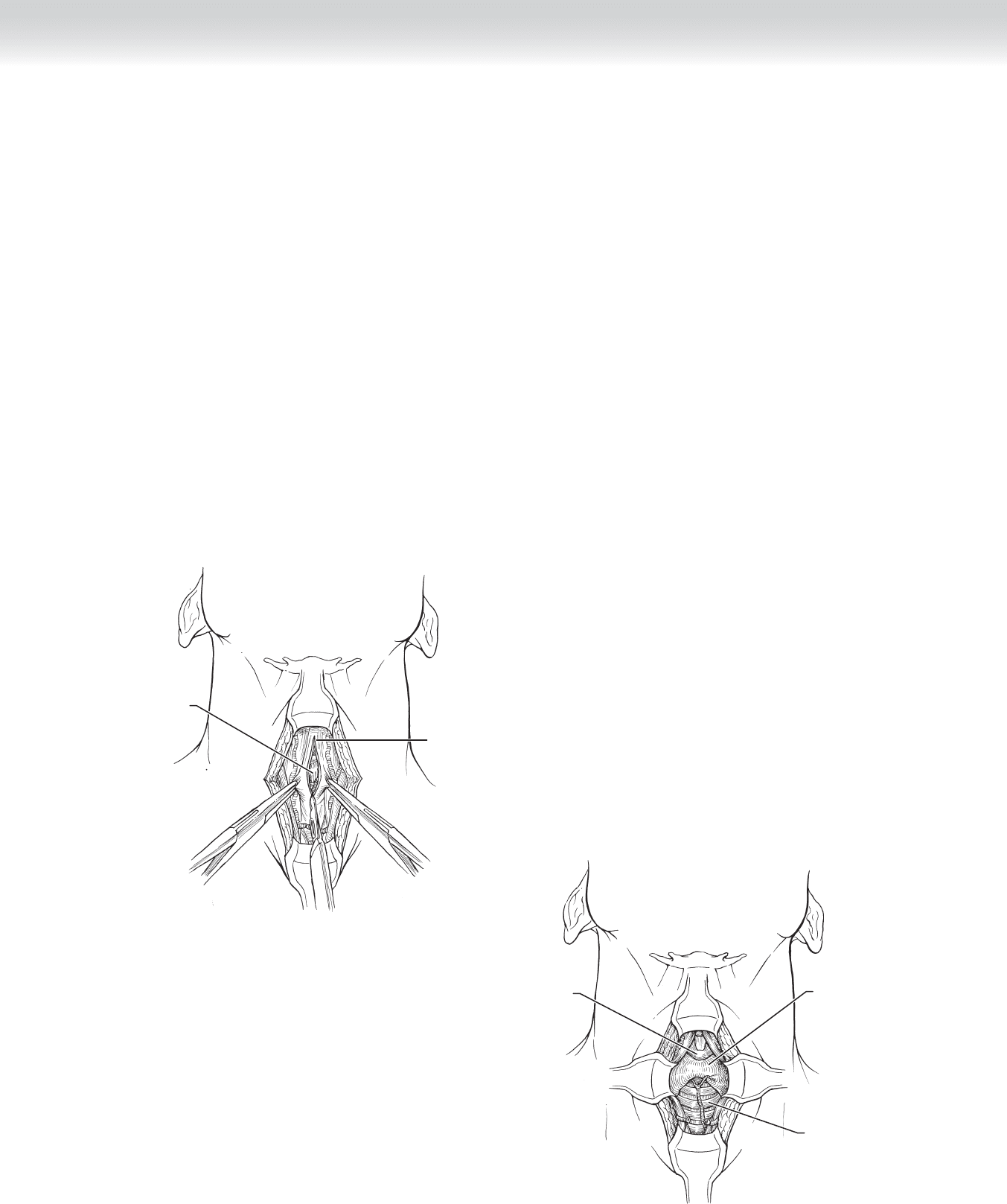
FIGURE 5 –1
STEP 1: SURGICAL ANATOMY
◆ The following landmarks are useful in performing a tracheotomy or cricothyroidotomy
(Figure 5-1):
◆ Hyoid bone
◆ Thyroid notch
◆ Cricoid cartilage
◆ Sternal notch
◆ The thyroid isthmus overlies the anterior trachea at the level of the fi rst tracheal ring.
◆ See Figure 1-2 for demonstration of the relationship of the trachea to the thyroid gland,
esophagus, and great vessels in the neck.
CHAPTER
5
Tracheotomy
Anna M. Pou

66 Section I • Head and Neck and Endocrine Procedures
STEP 2: PREOPERATIVE CONSIDERATIONS
◆ Indications:
◆ Respiratory failure with ventilator dependence
◆ Airway obstruction: edema, trauma, tumor, hematoma
◆ Status of cervical spine:
◆ If status of cervical spine is in question, seek neurosurgical clearance before extending
the neck.
◆ In patients with a cervical spine injury, the neck remains in a neutral position and the
head and neck are stabilized with sandbags.
◆ If the patient has had a previous tracheotomy, the operative report is reviewed with atten-
tion to the level of the tracheotomy and the presence of anatomic abnormalities.
◆ A vertical, rather than horizontal, skin incision is useful in the following cases: (1) redo trache-
otomies, because it gives a larger area of exposure, which is helpful when dealing with scar
tissue; (2) in patients whose landmarks are not easily palpated; and (3) in infants and children.
◆ Local, awake tracheotomy should be considered in patients with laryngeal obstruction
(edema, tumor) who are not in acute airway distress and who are determined to be diffi cult
fi ber-optic intubations.
◆ “High” tracheotomies are performed in patients with laryngeal carcinoma so that maximal
tracheal length can be preserved for stoma construction in the event a total laryngectomy is
required for treatment.
◆ The size of the tracheotomy tube is decided preoperatively (a size 6 cuffed tube is usually
placed in a woman, and a size 8 cuffed tube is usually placed in a man). An extended-
length tracheotomy tube may be necessary in patients with large necks and should be
available in the operating room before the tracheotomy is performed.
◆ The cuff of the tracheotomy tube is tested before use.
◆ The surgeon and anesthesiologist discuss the surgical plan preoperatively; the airway is
shared by both parties.

STEP 3: OPERATIVE STEPS
1. INCISION
◆ The patient is placed supine. The neck is extended using a shoulder roll and the head is
stabilized using a doughnut cushion.
◆ The anesthesiologist should be at the head of the table to maintain control of the airway.
◆ The surgical site is sterilely prepped with betadine and draped in such a manner that the
anesthesiologist has easy access in the event reintubation becomes necessary.
◆ Using a sterile marking pen, the surgeon outlines the previously mentioned landmarks on
the neck and a 2-cm horizontal skin incision 2 fi ngerbreadths above the sternal notch
(Figure 5-2).
◆ The skin incision and subcutaneous tissues are injected with 1% lidocaine with
1:100,000 epinephrine.
◆ The skin incision is made using a no.10 scalpel blade and extends through the underlying
subcutaneous tissues (see Figure 5-2).
FIGURE 5 –2
Incision
Thyroid gland
CHAPTER 5 • Tracheotomy 67
68 Section I • Head and Neck and Endocrine Procedures
2. DISSECTION
◆ The superior and inferior skin fl aps are retracted (Figure 5-3).
◆ A vertical incision is made in the midline fascia between the strap muscles. This is usually a
bloodless plane (see Figure 5-3).
◆ The strap muscles and, typically, the anterior jugular veins are retracted laterally
(see Figure 5-3).
◆ The dissection proceeds vertically in the midline through the pretracheal tissue and fat. The
lateral retractors are placed deeper in the wound as the dissection proceeds to a deeper level.
◆ The cricoid cartilage and thyroid isthmus are encountered (Figure 5-4).
MC
Thyroid gland
Infrahyoid fascia
FIGURE 5 –3
Cricoid cartilage
Trachea
Thyroid gland
FIGURE 5 –4

CHAPTER 5 • Tracheotomy 69
MC
Third tracheal ring
A
Thyroid isthmus
B
FIGURE 5 –5
◆ The isthmus is retracted superiorly using an Allis clamp (Figure 5-5, A).
◆ If the isthmus is diffi cult to retract, it is transected. A horizontal incision is made in the
anterior suspensory ligament of the thyroid, which is between the inferior edge of the
cricoid cartilage and the isthmus. A curved hemostat is used to dissect the thyroid isthmus
from the anterior surface of the trachea (Figure 5-5, B), and the thyroid isthmus is tran-
sected using electrocautery. Care is taken to not violate the anterior surface of the trachea or
to pass the hemostat deep to the cricoid cartilage.
◆ The pretracheal tissue is palpated in this area for a “high-riding” innominate artery before
the tracheotomy incision is made.

70 Section I • Head and Neck and Endocrine Procedures
◆ The anterior surface of the trachea is further cleaned; the tracheal fascia is incised vertically
in the midline and bluntly dissected laterally.
◆ A 2-mL injection of 4% lidocaine plain is given intraluminally. This is especially important
in awake patients to prevent coughing and anxiety while placing the tracheotomy tube.
◆ Before entering the airway, the surgeon notifi es the anesthesiologist and the scrub nurse so
that the remainder of the procedure can proceed in a highly organized fashion. All neces-
sary instruments and the previously tested tracheotomy tube should be readily available
and placed in the order of need on the Mayo stand.
◆ The anesthesiologist untapes the endotracheal tube (ETT), holds it in place, and waits for
instructions from the surgeon. All extraneous noise in the room should cease.
◆ A horizontal incision (5 to 8 mm in length) is made directly above the tracheal ring of
choice (second, third, or fourth) using a no. 15 scalpel blade, taking care not to puncture
the cuff on the ETT (Figure 5-6, A).
◆ The incision continues in a manner necessary to remove an anterior portion of the ring
(Figure 5-6, B). An alternative method is to perform a broad, inferiorly based,
U-shaped
fl ap extending the length of one tracheal ring (Figure 5-6, C).

CHAPTER 5 • Tracheotomy 71
Third tracheal ring
A
MC
B
Third tracheal ring
Tracheal ring flap
Thyroid gland
C
FIGURE 5 –6

72 Section I • Head and Neck and Endocrine Procedures
◆ The trachea is delivered into the wound and stabilized using the retractors already in place
or a cricoid hook (Figure 5-7). (The thyroid isthmus was removed in the fi gure for
visualization of the underlying cricoid cartilage.)
◆ A 2-0 silk suture is placed through the inferior and superior tracheal rings, from outside to
inside the lumen. The needles are removed and the sutures are not cut; the ends are
brought out through the wound and can be used for retraction (Figure 5-8).
◆ The ETT is now withdrawn under direct visualization. The cuff is defl ated and ventilation is
stopped. The surgeon instructs the anesthesiologist to slowly withdraw the ETT until the
tip is seen immediately above the tracheotomy incision and no farther.
Third
tracheal ring
FIGURE 5 –7
MC
Superior
stay suture
Placing lower/
inferior stay suture
FIGURE 5 –8

CHAPTER 5 • Tracheotomy 73
◆ The surgeon places the tracheotomy tube (with obturator in place) into the airway under direct
visualization. The tube is introduced at a right angle and then turned inferiorly (Figure 5-9).
◆ Once the tube is in place, the obturator is removed, the inner cannula is placed, the cuff is
infl ated, and the anesthesia circuit is hooked to the tracheotomy tube. The return of carbon
dioxide following ventilation is confi rmed, and the chest is auscultated for the presence of
bilateral breath sounds. Confi rmation is required before completely removing the ETT from
the airway.
◆ Tracheotomy ties are placed around the neck, and the fl anges of the tracheotomy tube are also
sewn to the skin as an extra precaution to prevent accidental decannulation (Figure 5-10).
Tube in place
Stitch
FIGURE 5 –10
FIGURE 5 –9
Opening in trachea
Tube being introduced
MC

74 Section I • Head and Neck and Endocrine Procedures
3. CLOSING
◆ Not applicable.
STEP 4: POSTOPERATIVE CARE
◆ The “stay sutures” are taped to the inferior and superior skin fl aps, respectively. The pieces
of tape have “Do Not Remove” written on them so that these sutures can be used to retract
the trachea in the event of accidental decannulation.
◆ Postoperative orders should include the following:
◆ Tracheal suctioning every shift and as needed (prn). Patient may require tracheal
suctioning every hour in the immediate postoperative period. Preoxygenation with
100% oxygen may be necessary.
◆ Saline irrigation is used before suctioning to lubricate the trachea and suction catheter
and to thin secretions in selected patients (copious, thick secretions).
◆ The inner cannula must be changed/cleaned every shift and prn.
◆ Continual humidifi cation via a tracheotomy collar to prevent mucous plug and obstruc-
tion of inner cannula with dried secretions.
◆ Gauze dressing is placed under the tracheotomy fl ange to keep the area clean. Care is taken
not to dislodge the tube when changing this dressing.
◆ Regarding ventilator-dependent patients, the tracheotomy tubing is stabilized to prevent
subglottic and/or tracheal stenosis and accidental dislodgment of the tube.
◆ The cuff pressure should be minimal to prevent tracheal necrosis and resultant subglottic
and/or tracheal stenosis.
◆ Tracheotomy care is taught to the patient and his or her caregiver(s) as soon as possible.
◆ The “stay sutures” are removed on postoperative day 5.
◆ Speech pathology is consulted to address speech and swallowing problems associated with
tracheotomy.
STEP 5: PEARLS AND PITFALLS
◆ Complications include the following:
◆ Injury to the esophagus or great vessels intraoperatively. This is rare but can occur in
operative fi elds fi lled with scar tissue or tumor and in emergent cases.
◆ Pneumothorax
