Townsend Courtney M.Jr., Evers B. Mark. Atlas of General Surgical Techniques: Expert Consult
Подождите немного. Документ загружается.

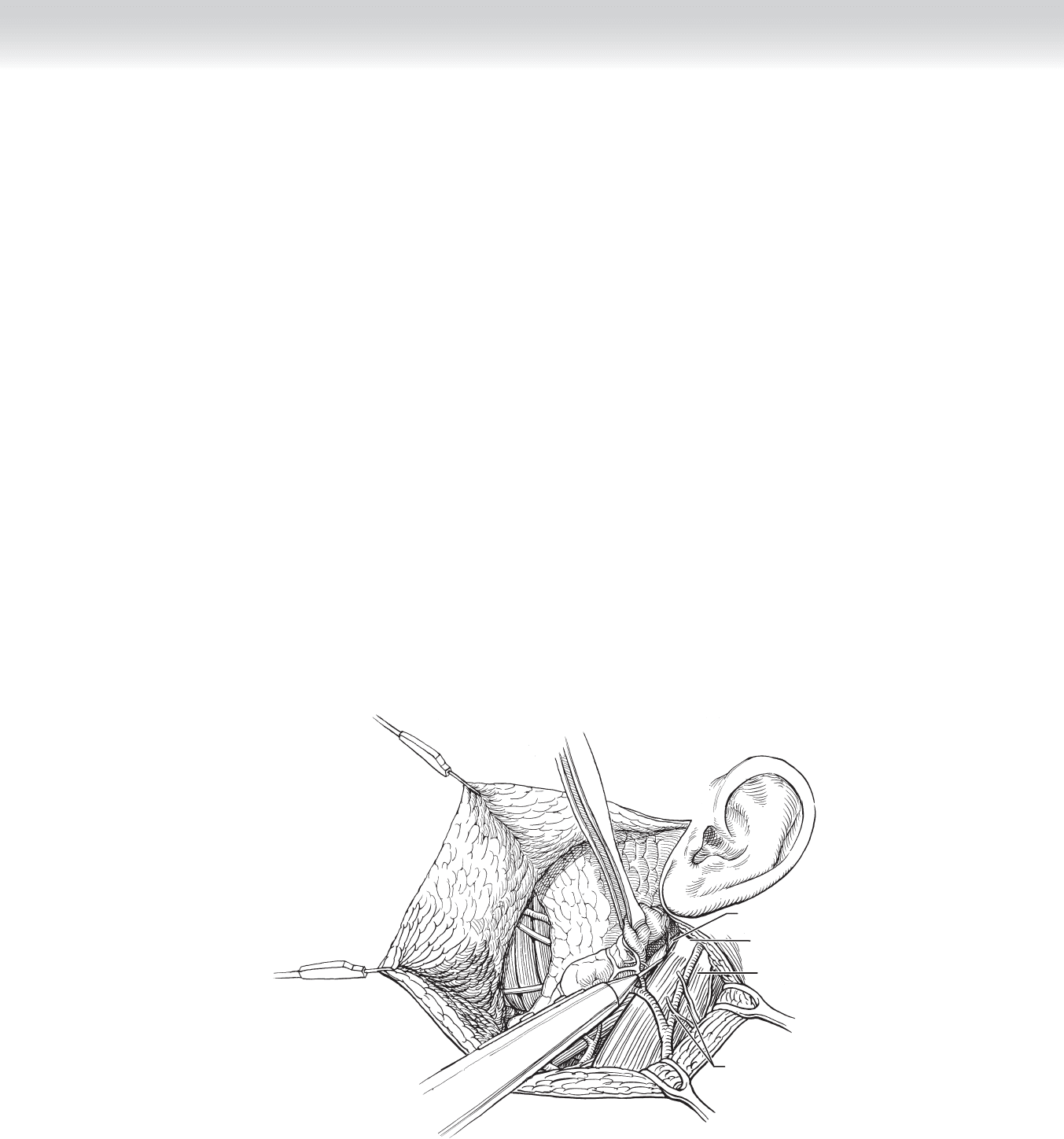
Sternocleidomastoid muscle
Great auricular nerve branches
Digastric muscle (posterior belly)
Mastoid tip
FIGURE 4 –3
55
CHAPTER 4 • Parotidectomy
2. DISSECTION
◆ For a parotidectomy to be performed safely, wide exposure and knowledge of important
anatomic landmarks are key.
◆ The operation begins in the plane deep to the tail of the parotid. The fascia along the
anterior border of the SCM muscle is incised, exposing the muscle toward the level of the
mastoid process. Electrocautery can be used in this dissection (Figure 4-3).
◆ The great auricular nerve and external jugular vein are identifi ed at this time. If the nerve
has multiple branches, the posterior branch is preserved to maintain sensation to the
external ear. Maximal nerve length is dissected in the event that it is needed for a facial
nerve graft (see Figure 4-3).
◆ As the dissection proceeds anteriorly, the tail of the parotid is dissected from the SCM
muscle and mastoid process, and the posterior belly of the digastric muscle is exposed. The
gland is retracted using an Allis clamp or hemostats (see Figure 4-3).
◆ The posterior belly of the digastric muscle is further exposed toward its origin by retracting
the SCM muscle posteriorly and both sharply and bluntly dissecting the tissue overlying the
muscle (see Figure 4-3).

56 Section I • Head and Neck and Endocrine Procedures
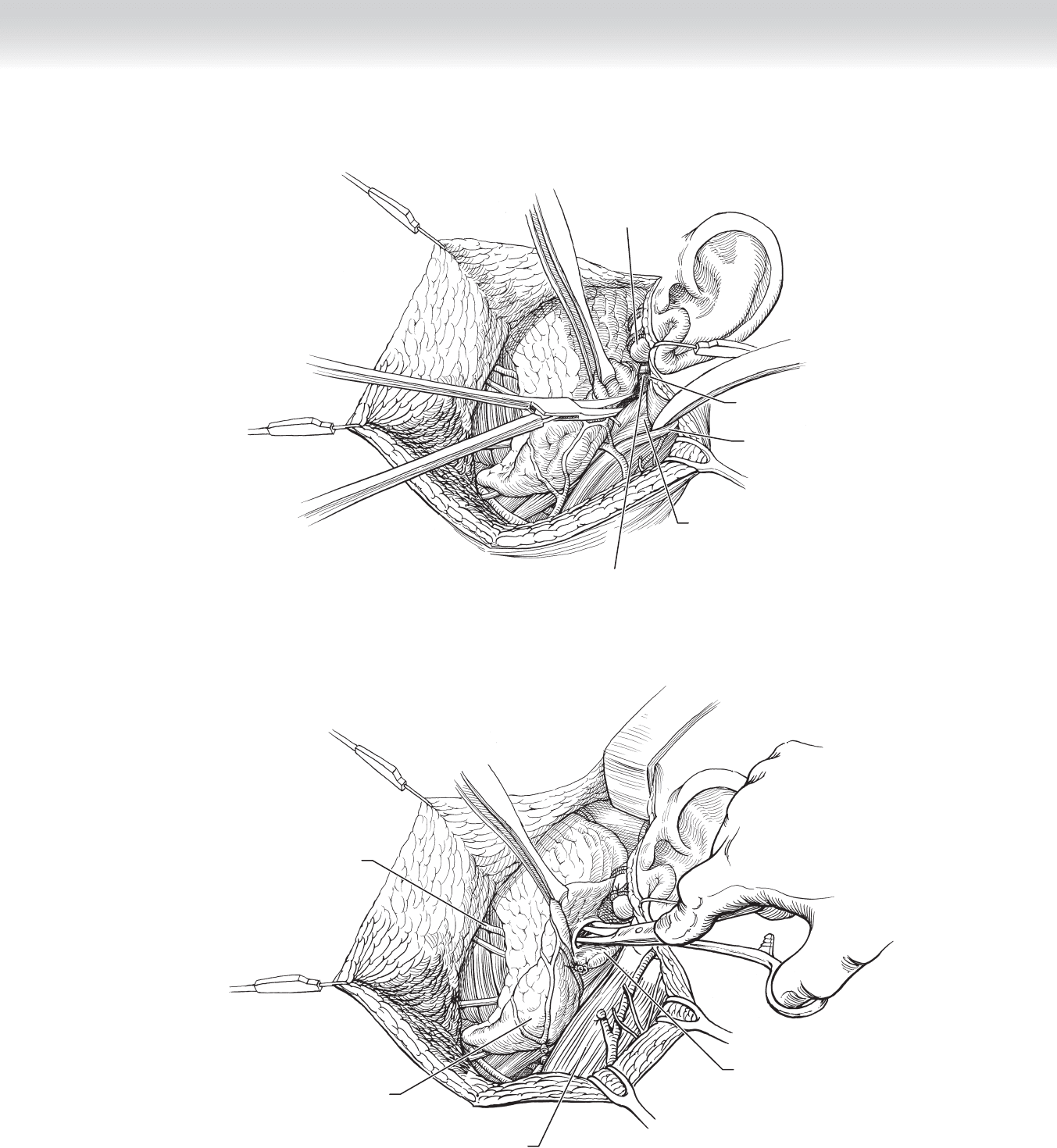
◆ The posterior aspect of the gland is now dissected from the external auditory canal. The
parotid tissue is carefully bluntly and sharply dissected from the ear canal using a fi ne curved
hemostat or scissors and bipolar cautery to maintain hemostasis. It is critical to maintain abso-
lute hemostasis in order to identify the facial nerve trunk without injury (Figure 4-4).
◆ Once the parotid gland is freed from its fi brous attachments, blunt dissection along the ear
canal perichondrium using a fi nger will allow the surgeon to palpate the bony-cartilaginous
junction of the ear canal, the tympanomastoid fi ssure, and the tragal pointer (see Figure 4-4).
◆ The main trunk of the facial nerve is now close by. It is approximately 1 cm deep to the tip
of tragal pointer (anterior and inferior), 6 to 8 mm below the end of the tympanomastoid
fi ssure (groove palpated separating the mastoid tip from the tympanic portion of the
temporal bone), and just above and on the same plane as the attachment of the digastric
muscle in the digastric groove.
◆ The remaining bridge of parotid tissue located between the superior border of the posterior
belly of the digastric muscle and the external auditory ear canal is now dissected. The
mobilized portions of the parotid gland are retracted anteriorly, putting the residual parotid
tissue on stretch. A retractor is placed so that the posterior belly of the digastric muscle is
also exposed during this dissection. This tissue is bluntly and sharply dissected, layer by
layer, to expose the junction of the superior aspect of the posterior belly of the digastric
muscle and the tympanomastoid fi ssure. The tips of the dissecting instrument face upward
and dissection is done along a broad front (see Figure 4-4).
◆ Once the temporoparotid fascia, which runs from the tympanomastoid fi ssure to the
gland, is transected, the parotid tissue is released and the facial nerve will be easily
identifi ed (see Figure 4-4).
◆ The nerve stimulator should be used only if there is a question as to the identity of the
main trunk of the facial nerve (see Figure 4-4).
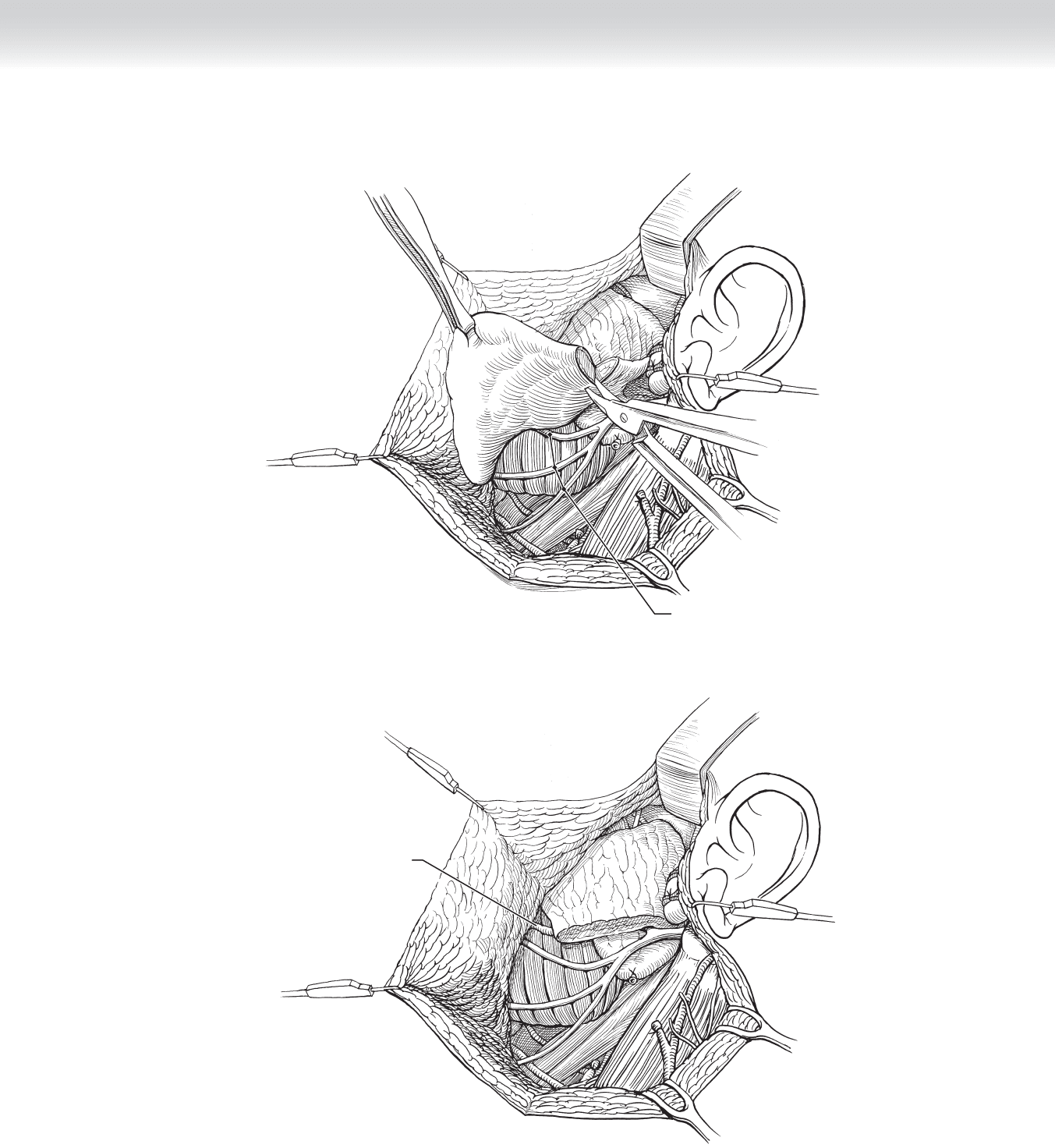
◆ Following identifi cation of the main trunk, dissection proceeds in a plane superfi cial to the
nerve. A curved hemostat or scissors, with tips facing upward, is used to spread the tissue
immediately superfi cial to the nerve, keeping the nerve under direct vision at all times. The
main trunk is dissected anteriorly until the pes anserinus is reached. The upper (zygomati-
cotemporal) and lower (cervicofacial) divisions are identifi ed (Figure 4-5).
CHAPTER 4 • Parotidectomy
57
Deep lobe of
parotid gland
Tumor in tail of
superficial parotid lobe
Parotid duct
Sternocleidomastoid muscle
FIGURE 4 –5
Sternocleidomastoid
muscle
Main trunk facial nerve
Digastric muscle (posterior belly)
Cartilage of
external
auditory canal
Tympanomastoid
suture line
FIGURE 4 –4

58 Section I • Head and Neck and Endocrine Procedures
◆ Dissection of individual facial nerve branches to the periphery of the gland is performed in
an orderly fashion. Dissection can proceed from inferior to superior or superior to inferior,
depending on tumor location (Figure 4-6).
◆ A fi ne curved hemostat or scissors is used to dissect just on top of the nerve, elevating the
parotid tissue off the nerve. The instrument is opened, spreading the parotid tissue and ex-
posing the nerve. The tissue is cut in a horizontal plane parallel to the nerve. If the nerve is
not visualized, do not cut the tissue! Once a nerve branch is completely exposed, the sur-
geon again returns to the major division where he or she was working and the next nerve
branch in sequence is exposed. This is done until all the branches are exposed and the
gland is removed. The parotid tissue is retracted forward using Allis clamps and other
retractors during this dissection (see Figure 4-6).
◆ In this example, the benign tumor is located in the tail of the parotid. The branches of the
lower division are dissected and the tumor is removed with a large cuff of parotid tissue. Care
should be taken to avoid injury to the marginal mandibular branch when ligating the posterior
facial vein. In addition, the “fl anking maneuver” (swinging around the tail of the parotid)
should also be avoided because it may also result in injury to the marginal mandibular branch
(most common site of injury). A complete superfi cial parotidectomy with dissection of all of
the upper division nerve branches is unnecessary in this case (Figure 4-7).
CHAPTER 4 • Parotidectomy
59
Parotid duct
FIGURE 4 –7
Buccal, mandibular, and cervical
branches of facial nerve
FIGURE 4 –6

60 Section I • Head and Neck and Endocrine Procedures
3. DEEP LOBE PAROTIDECTOMY
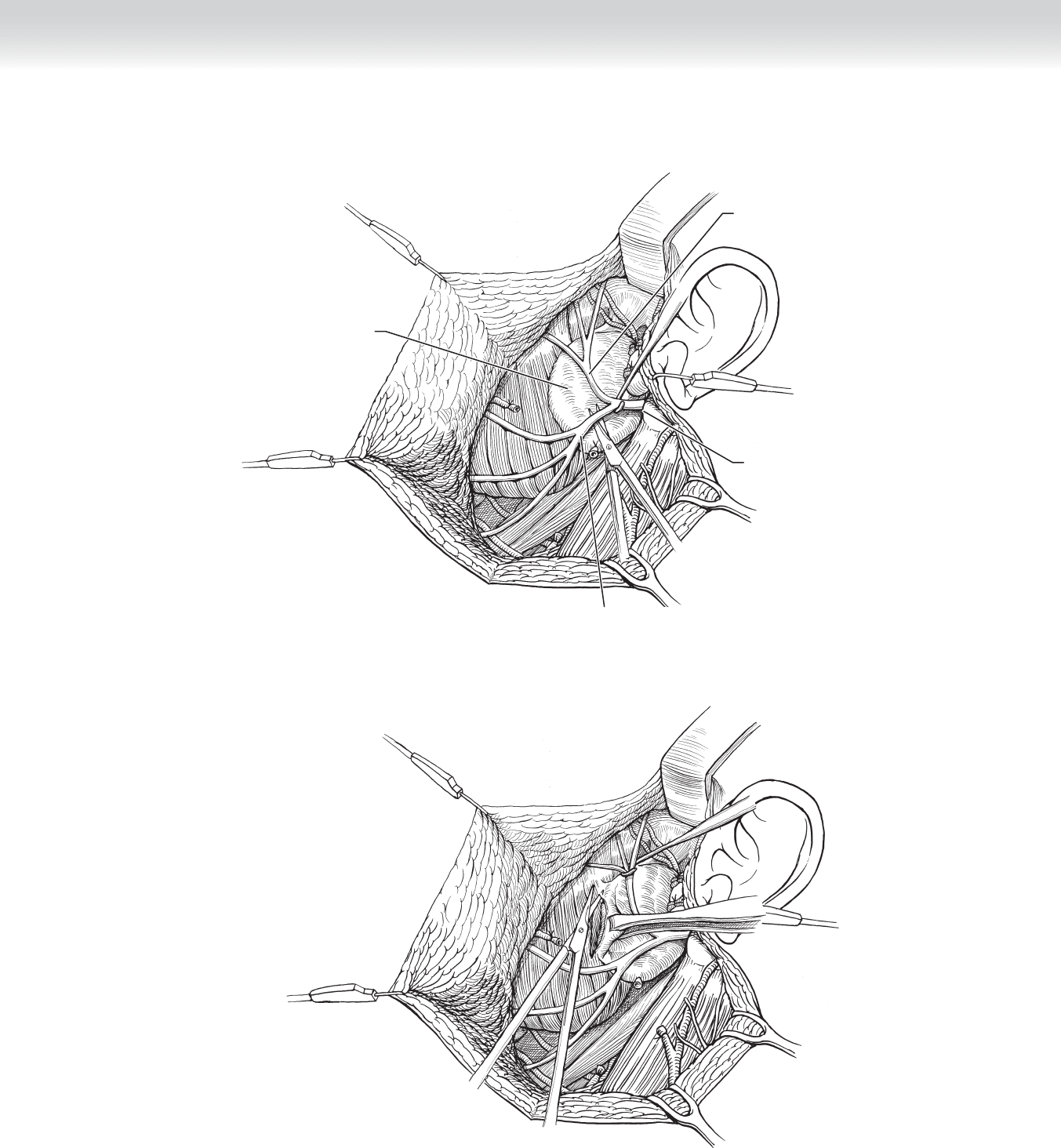
◆ All branches of the upper and lower divisions of the facial nerve are systematically dissected,
and the entire lateral lobe of the parotid is removed when the tumor located in the lateral
lobe dictates it and in cases in which a total parotidectomy is required (deep lobe tumor, ma-
lignancy, chronic parotitis). The superfi cial lobe is sent as a separate specimen (Figure 4-8).
◆ Stensen’s duct is transected at the anterior border of the gland and ligated. Care is taken not
to injure the buccal branch of the nerve that runs parallel to Stensen’s duct (see Figure 4-8).
◆ To remove the deep lobe of the parotid, the surgeon very delicately and meticulously
dissects the main trunk of the facial nerve and its branches to free them from the deep lobe.
◆ After each branch is completely freed from the deep lobe, the surgeon uses gentle retraction
using a vein retractor, nerve hook, or very small vessel loops to lift the nerves, allowing
blunt and sharp dissection and mobilization of the deep lobe. Excessive retraction of the
nerves will result in a stretch injury (see Figure 4-8).
◆ The gland may be dissected from the stylohyoid and stylopharyngeus muscles. During dis-
section of the deep lobe the following vessels may be encountered: the superfi cial temporal
vessels, the internal maxillary artery (running deep to mandibular ramus), the occipital
artery, the posterior auricular artery, and the pterygoid plexus of veins. Bleeding can be
substantial, and patience must be used in identifying and controlling the bleeding vessel to
avoid inadvertent injury to the nerve (Figure 4-9).
◆ Removal of the deep lobe may be accomplished inferior to, superior to, or between facial
nerve branches (see Figure 4-9).
CHAPTER 4 • Parotidectomy
61
FIGURE 4 –9
Main trunk facial nerve
Deep lobe of
parotid gland
Upper division facial nerve
Lower division facial nerve
FIGURE 4 –8

62 Section I • Head and Neck and Endocrine Procedures
◆ A thin layer of masseter muscle (margin) is removed when dealing with recurrent benign tumors,
and a larger margin or the entire muscle is removed if the lesion is malignant (Figure 4-10).
◆ Stensen’s duct is followed through the buccinator muscle to the mucosa in cases of chronic
and recurrent sialadenitis associated with sialolithiasis (stones).
4. RADICAL PAROTIDECTOMY
◆ Radical parotidectomy (total parotidectomy with facial nerve sacrifi ce) is indicated in cases
of malignant involvement of the main trunk of the facial nerve. Sacrifi ce of one or all of the
peripheral nerve branches without sacrifi ce of the main trunk is indicated when the nerve
branches are involved but the main trunk is not.
◆ Intraoperative frozen section analysis are performed on all proximal and distal nerve stumps
to ensure negative margins. The branches are tagged with a fi ne suture so that they may be
easily located intraoperatively for facial nerve grafting.
◆ Mastoidectomy may be necessary to obtain clear proximal facial nerve margins.
◆ The great auricular or sural nerve can be used to reconstruct the facial nerve. The main
trunk and the marginal mandibular, buccal, and temporal branches are reconstructed to re-
store oral competency and eye closure. However, reconstruction of the facial nerve branches
anterior to lateral canthus is not required.
Masseter muscle
FIGURE 4 –10

CHAPTER 4 • Parotidectomy
63
5. CLOSING
◆ The main trunk of the facial nerve is stimulated (0.5 mA) to prove that all branches are
intact before the wound is closed. If some or all of the branches do not respond to stimu-
lation, careful inspection to ensure anatomic integrity of nerve is performed.
◆ The skin is closed in two layers using fast absorbing versus monofi lament suture. Care is
taken to accurately reapproximate the lobule.
◆ A 10-mm Jackson-Pratt drain is placed via a separate stab incision in the postauricular area.
Care is taken to avoid placement of the drain next to the nerve.
◆ A fi gure-of-eight pressure dressing is placed around the neck, face, and head.
STEP 4: POSTOPERATIVE CARE
◆ Facial nerve function is evaluated as soon as the patient is awake and cooperative.
◆ If facial nerve paresis or paralysis is noted, steroids may be given only if the facial nerve is
known to be intact. If it is possible that the main trunk or nerve branch was transected
during surgery, immediate exploration and repair of nerve must be performed.
◆ Pressure dressing is removed the next morning.
◆ Closed suction drain is removed when output is less than 15 to 30 mL over 24 hours.
◆ If eye closure is poor (neuropraxia, nerve sacrifi ce), saline drops are used multiple times
per day, and Lacri-Lube and eye taping are prescribed nightly to prevent exposure keratitis.
STEP 5: PEARLS AND PITFALLS
◆ A nerve integrity monitor and magnifi cation (loupe or microscope) may be used to aid in
facial nerve identifi cation and preservation, particularly in reoperations and cases of chronic
infection with scarring.
◆ Overuse of the facial nerve stimulator can cause neuropraxia.

64 Section I • Head and Neck and Endocrine Procedures
◆ If the tumor location precludes identifi cation of the main trunk of the facial nerve using
standard techniques, the main trunk can be identifi ed using retrograde dissection along the
temporal, buccal, or marginal mandibular branch (most common) or via mastoidectomy.
◆ Parotid specimen and/or lymph nodes are sent for intraoperative frozen section analysis if
malignancy is suspected.
◆ The posterior auricular artery or its branch can cross the main trunk of the facial nerve and
cause signifi cant bleeding and inadvertent injury to the nerve if not properly identifi ed and
ligated.
◆ Facial paralysis or paresis can result from aggressive dissection or inadvertent injury of the
nerve. Recovery of facial nerve paresis/paralysis can occur over 3 to 4 weeks if neuropraxic
injury and up to 1 year if axon death has occurred.
◆ Hematoma formation, manifested by acute postoperative pain, swelling of fl ap, and oozing
from wound, demands reexploration and evacuation. Hematoma can cause airway compres-
sion if signifi cant. Extreme care must be taken to avoid injury to the exposed facial nerve.
◆ Skin fl ap necrosis is rare but can occur in heavy smokers and in the postauricular area
when the skin fl ap is too thin and the skin incision is made at an acute angle.
◆ Frey’s syndrome (gustatory sweating) is associated with sweating in the area of skin overlying
the parotid bed. Most patients have this to some degree, and it is typically subclinical. It
occurs because of the aberrant regrowth of parasympathetic motor fi bers from the auriculo-
temporal nerve into the sympathetic nerve fi bers controlling sweat glands. Raising thicker
subcutaneous fl aps may reduce its occurrence. Medical therapy includes topical
scopolamine. Surgical remedies are rarely successful (dermal graft, tympanic neurectomy).
◆ Postoperative sialocele or salivary fi stula (salivary drainage from wound) is rare and can
usually be successfully managed with aspiration and compression dressings. Atropine-like
drugs may be benefi cial.
SELECTED REFERENCES
1. Johnson JT: Parotid. In Myers EN, Carrau RL (eds): Operative Otolaryngology: Head and Neck Surgery,
1st ed. Philadelphia, Saunders, 1997, pp 504-518.
2. Olsen KD: Parotid superfi cial lobectomy. In Bailey BJ, Calhoun KH, Coffey AR, Neely JG: Atlas of Head &
Neck Surgery—Otolaryngology. Baltimore, Lippincott-Raven, 1996, pp 2-11.
3. Lore JM, Medina J: The parotid salivary gland and management of malignant salivary gland neoplasia. In
Lore JM, Medina J (eds): An Atlas of Head and Neck Surgery, 4th ed. Philadelphia, Saunders, 2005,
pp 861-891.
4. Olsen KD: Superfi cial parotidectomy. Oper Tech Gen Surg 2004;6:102-114.
5. Shah JP, Patel SG: Salivary glands. In Shah JP, Patel SG (eds): Head and Neck Surgery and Oncology,
3rd ed. Edinburgh, Mosby, 2003, pp 439-474.
