Townsend Courtney M.Jr., Evers B. Mark. Atlas of General Surgical Techniques: Expert Consult
Подождите немного. Документ загружается.

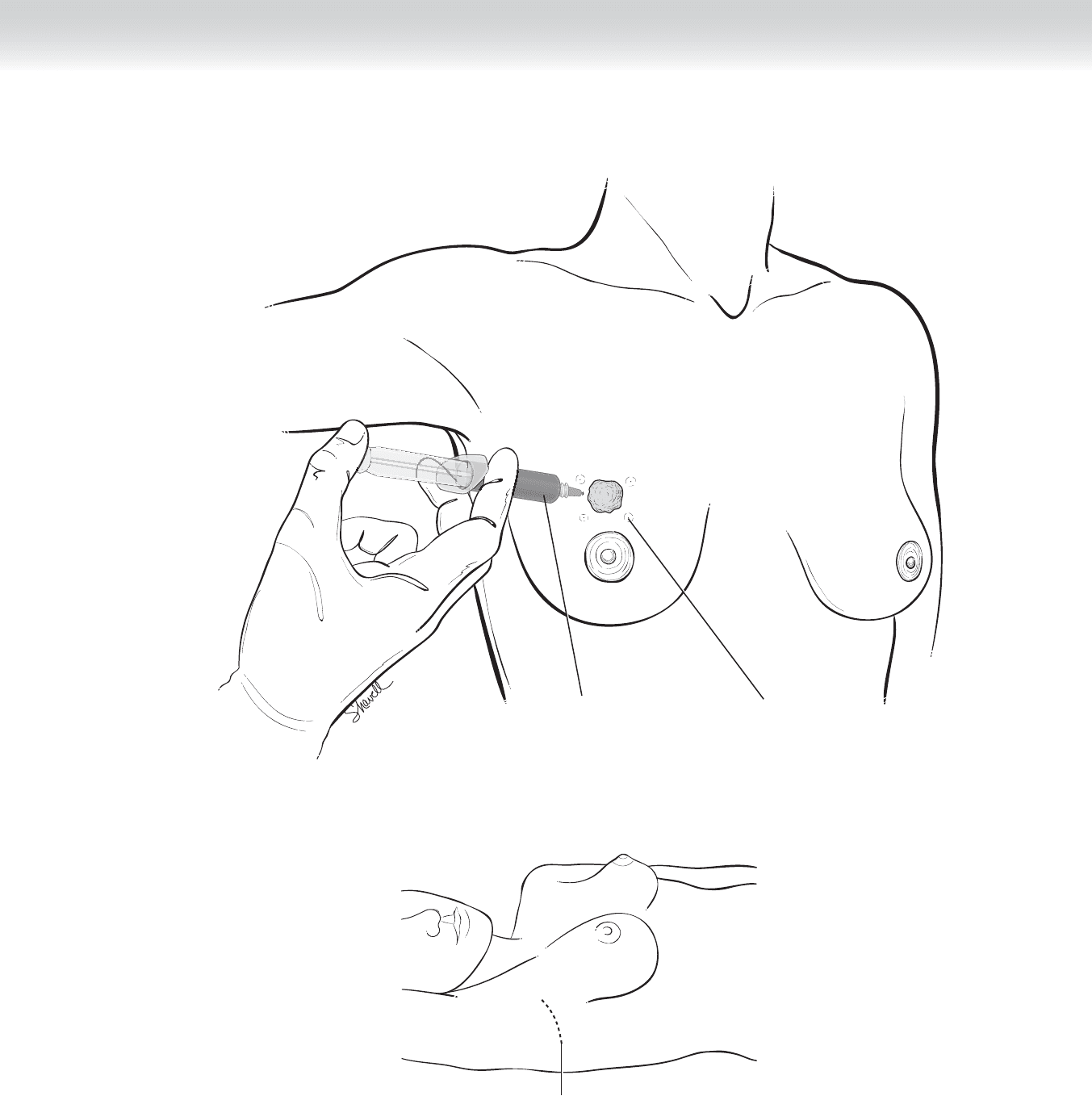
CHAPTER 11 • Sentinel Lymph Node Biopsy 137
Welts from radioactive
injections
Injection of blue dye
FIGURE 11 –3
Incision line
FIGURE 11 –4

138 Section II • The Breast
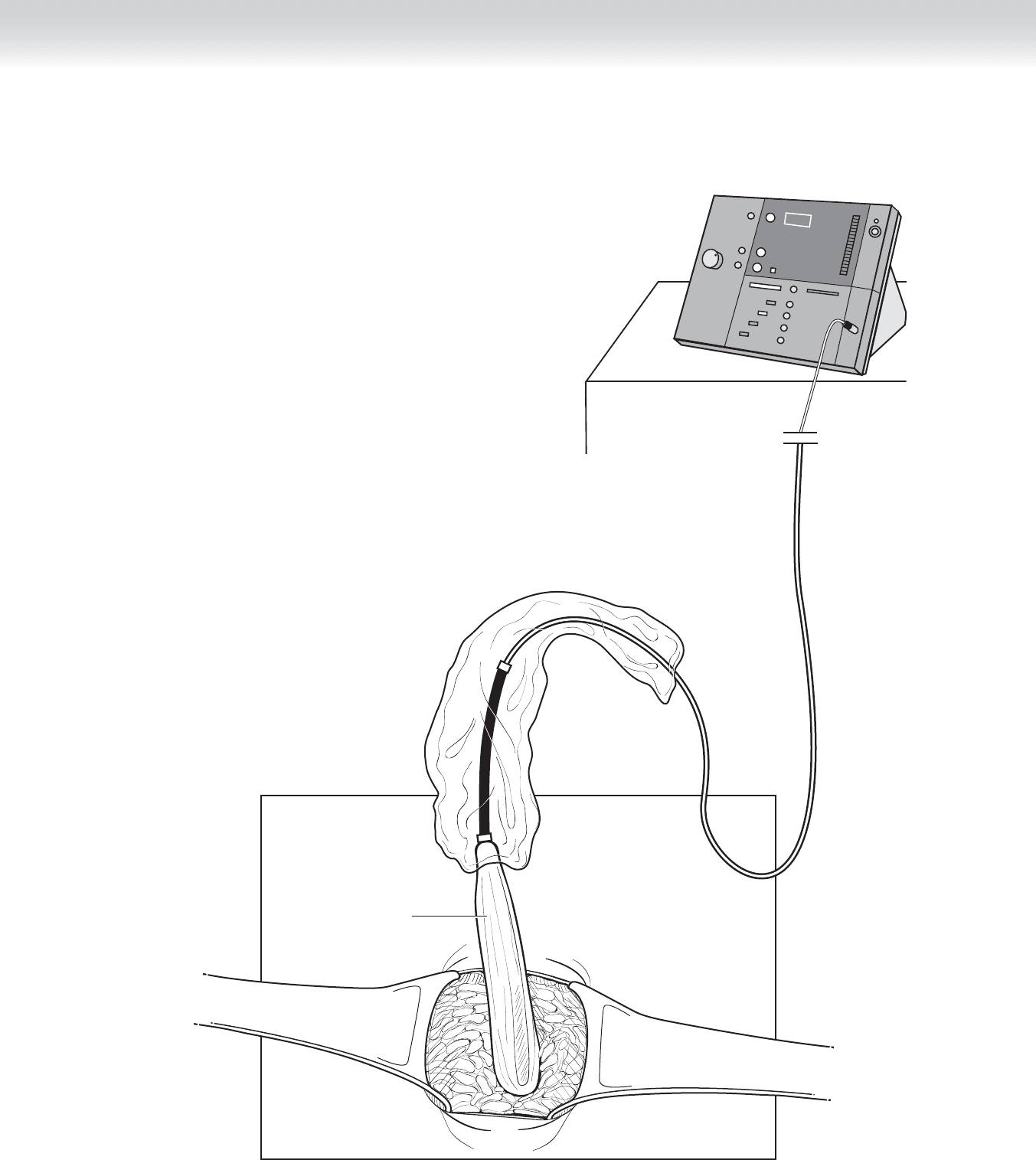
2. DISSECTION
◆ After dissecting through the subcutaneous tissue, the surgeon divides the clavipectoral
fascia to gain exposure to the axillary contents. The gamma counter is used to help locate
the SLN. As the dissection continues, the signal from the probe should increase in intensity
(Figure 11-5). If there is diffi culty in identifying an SLN, the clavipectoral fascia along the
lateral border of the pectoralis major and minor muscles should be divided to easily access
the entire axilla. This is accomplished by elevating and rotating the arm (which has been
incorporated in the sterile fi eld) medially.
CHAPTER 11 • Sentinel Lymph Node Biopsy 139
Geiger counter
Probe
1081
FIGURE 11 –5
140 Section II • The Breast
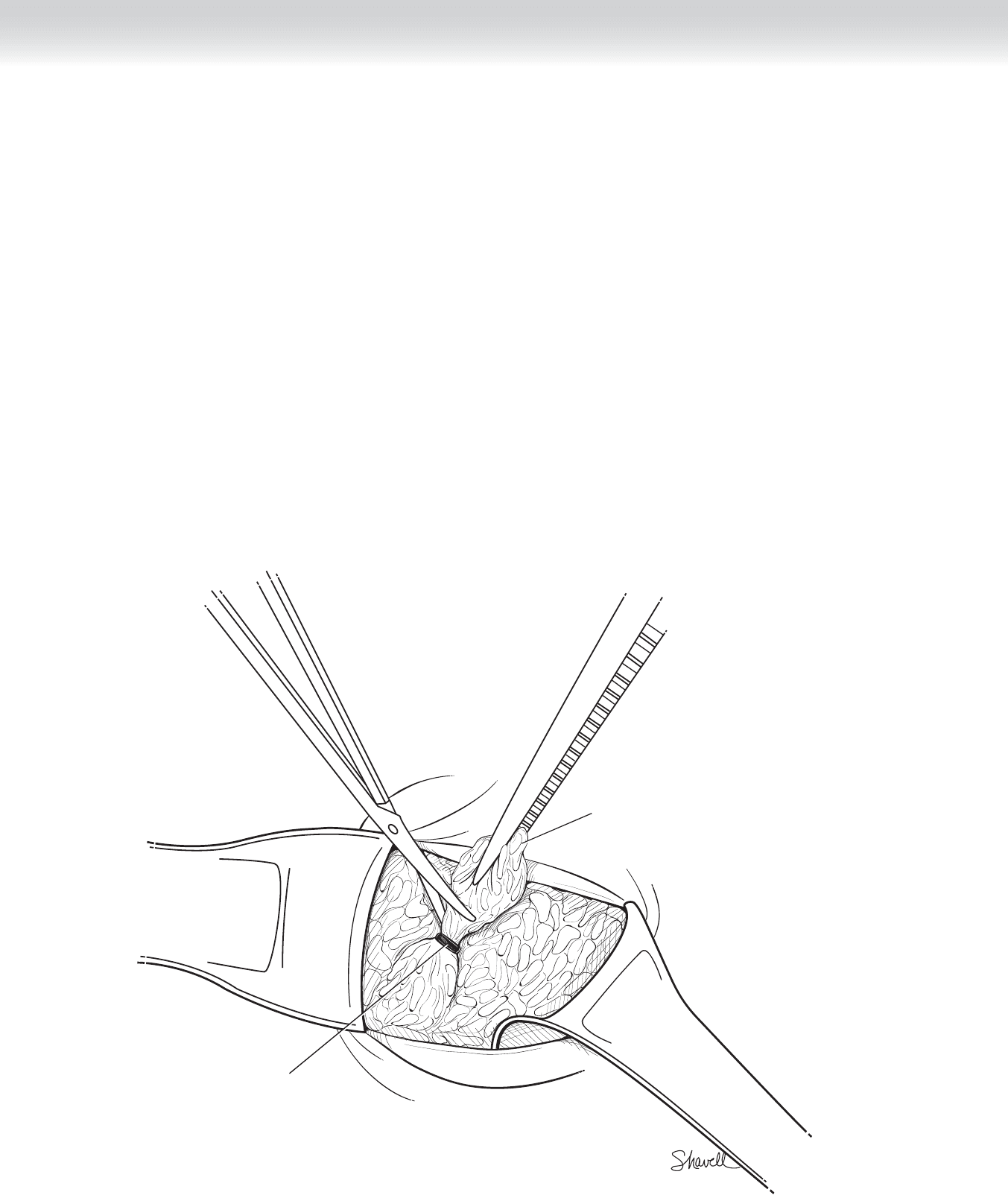
◆ Using a combination of the visualization of blue dye in the afferent lymphatics and lymph
nodes themselves, as well as the hand-held gamma probe, the location of the SLN is pin-
pointed (Figure 11-6). Care should be taken not to disrupt the capsule of the lymph node.
Hemoclips are used for hemostasis and to clip the afferent lymphatic channels. Meticulous
clipping of the lymphatics will prevent postoperative lymphocele formation. This is impor-
tant because a closed suction drain is not placed for SLN biopsy.
◆ After the SLN is removed, ex vivo radioactive counts are obtained, and the node may be sent
to pathology for frozen section analysis if it was harvested for breast cancer (see “Pearls and
Pitfalls”). The background radioactivity in the axilla is then surveyed. False-negative rates are
lowest if all blue nodes, blue-stained afferent lymphatic channels leading to an SLN, and
nodes greater than 10% of the ex vivo count of the hottest SLN are harvested (the 10% rule).
That is, if there is focal activity of 10% or greater of the ex vivo counts of the hottest SLN, a
diligent search should be made for another SLN. The node is placed on the gamma probe
(pointing away from the breast and up toward the ceiling) to obtain an ex vivo radioactive
count. If the highest reading (“hottest node”) recorded is 7099 counts per second, then any
additional lymph node remaining in the axilla with counts greater than 710 (10% of the
hottest node) should be removed as another SLN.
Node being removed
Clip
FIGURE 11 –6

CHAPTER 11 • Sentinel Lymph Node Biopsy 141
◆ After removal of blue and/or hot nodes, palpation of the surgical bed for enlarged, fi rm, or
otherwise suspicious lymph nodes should be performed. A pathologic lymph node may
not be hot or blue for two reasons: (1) the lymph node is completely replaced with tumor
and the lymphatics are “blocked” from uptake of any tracer, and (2) unexplainable false-
negative results do occur. A tumor-positive, nonradioactive or nonblue node should still
be considered a “sentinel” node when removed because it accurately staged the axilla of
that patient. If no SLN can be identifi ed, then a default level I/II axillary dissection must
be performed. On average, two to three SLNs are removed per case for breast cancer, and
one to two for melanoma.
◆ SLN biopsy is followed by either breast-conserving therapy or mastectomy. If mastectomy is
planned, it is helpful to perform the SLN biopsy fi rst by opening a small portion of the axil-
lary portion of the mastectomy incision before raising the fl aps. Depending on the tumor
location, raising the entire superior fl ap may result in blue dye spillage into the axilla,
which can make identifi cation of the SLN diffi cult.
3. CLOSING
◆ The axilla is irrigated and hemostasis is achieved. The wound is closed in two layers: an
interrupted watertight layer with absorbable sutures that reapproximates the clavipectoral
fascial layer and a subcuticular layer to close the skin edges.
STEP 4: POSTOPERATIVE CARE
◆ Should the patient require a completion axillary lymph node dissection, the previous SLN
biopsy scar should be removed en bloc with the specimen.
STEP 5: PEARLS AND PITFALLS
◆ Unless formally trained during residency or fellowship, all surgeons must climb the learning
curve and begin to learn this procedure by offering SLN biopsy with planned backup axillary
dissection. This will allow the individual surgeon to calculate his or her own identifi cation
and false-negative rates. Surgeons who wish to adopt this technology must ensure that in
their own hands, a false-negative rate of 5% or lower and an identifi cation rate of 95% or
higher are achieved. The false-negative rate signifi cantly decreased from 9% for surgeons
who performed 20 or fewer procedures to a rate of 1.9% for those who performed more
than 20 procedures. It must be emphasized, however, that false-negative results and non-
identifi cation of the SLN can occur even after appropriate surgical training. Patients must be
told of the small risk of a false-negative result and balance this against the benefi ts of a less
invasive procedure. If staged to be SLN negative, the patient may have a small lifetime risk of
axillary recurrence due to the potential of a false-negative result.

142 Section II • The Breast
◆ Although limited data suggest that SLN biopsy may be feasible following previous SLN
biopsy, previous neoadjuvant chemotherapy, or radiotherapy, if successful mapping is not
achieved by the technical criteria defi ned previously, the standard levels I and II axillary
dissection should be performed. Many studies demonstrate adequate identifi cation rates,
but few report false-negative rates in these clinical circumstances.
◆ The role for SLN biopsy in infl ammatory breast cancer has not been defi ned.
◆ Some surgeons advocate frozen section analysis of the SLN, whereas others never use frozen
section analysis because of the issue of sampling error in this setting. The decision to
incorporate frozen section evaluation into one’s program depends on the comfort level of
the pathologist and surgeon. Patients are informed preoperatively that frozen section
analysis may miss some positive SLNs, which subsequently will be found on fi nal patho-
logic sections. The sensitivity of frozen section analysis decreases with micrometastatic
deposits, defi ned as tumor 2 mm or smaller in the SLN. If there is a positive SLN found on
frozen section examination, this is an indication for completion axillary dissection under
the same anesthetic setting. If frozen section evaluation is not used, the patient can return
to the operating room (1 or 2 weeks later) for completion level I/II node dissection after
fi nal sections have been confi rmed to be tumor-positive.
◆ For melanoma, frozen section analysis is never recommended. Because both serial section-
ing and immunohistochemistry for tumor markers (e.g., S-100, MART-1) are required, per-
manent sections are necessary for accurate histopathologic diagnosis.
◆ Injection technique: Many centers perform peritumoral injection of both blue dye and
radioactive colloid. However, peritumoral injection of radioactive colloid results in a large
zone of diffusion that can obscure the objective of locating the axillary SLN, especially for
upper outer quadrant tumors. To minimize this “shine-through” effect, some centers use a
sterile lead shield to block the radioactive interference from the upper outer quadrant of the
breast. Furthermore, peritumoral injection results in relatively little uptake of the tracer
from the breast tissue compared with dermal injection. Studies have shown that dermal in-
jection of radioactive colloid signifi cantly improves SLN identifi cation rate and minimizes
the false-negative rate. For instance, dermal injection of radioactive colloid is associated
with SLNs that are fi vefold to sevenfold more radioactive, or hot, than with the peritumoral
injection method. When the dermal injection is used, the skin overlying the tumor can be
retracted medially, away from the axilla, to facilitate accurate gamma probe localization.
STEP 6. CONCLUSION
◆ Implementation of SLN biopsy requires multidisciplinary cooperation and high standards of
quality control. Ongoing studies, such as the American College of Surgeons Oncology
Group Trials Z0010 and Z0011 and the NSABP trial B-32, should provide answers to many
of the remaining clinically relevant questions.

CHAPTER 11 • Sentinel Lymph Node Biopsy 143
SELECTED REFERENCES
1. Morton DL, Wen DR, Wong JH, et al: Technical details of intraoperative lymphatic mapping for early stage
melanoma. Arch Surg 1992;127:392-399.
2. Giuliano AE, Kirgan DM, Guenther JM, Morton DL: Lymphatic mapping and sentinel lymphadenectomy
for breast cancer. Ann Surg 1994;220:391-401.
3. McMasters KM, Giuliano AE, Ross MI, et al: Sentinel lymph node biopsy for breast cancer: Not yet the
standard of care. N Engl J Med 1998;339:990-995.
4. McMasters KM, Chao C, Wong SL, et al: Sentinel lymph node biopsy in patients with ductal carcinoma-
in-situ: A proposal. Cancer 2002;95:15-50.
5. McMasters KM, Wong SL, Chao C, et al: Defi ning the optimal surgeon experience for breast cancer senti-
nel lymph node biopsy: A model for implementation of new surgical techniques. Ann Surg
2001;234:292-300.

144
STEP 1: SURGICAL ANATOMY
◆ Knowledge of breast anatomy is important. Benign lesions are usually fi broadenomas,
papillomas, or fi brocystic condition.
◆ Fibroadenomas usually occur in younger women, often in their 20s, and often are charac-
terized by a round, smooth, “slippable” mass. Indication for operation is patient concern,
because fi broadenoma is not a premalignant lesion.
STEP 2: PREOPERATIVE CONSIDERATIONS
◆ I favor the patient having general anesthesia for all of these resections for the following reasons:
◆ In young women with dense breast tissue, local anesthetic diffuses poorly. Resecting a
lesion at any depth or size often is much more uncomfortable than one would think.
◆ With fi brocystic condition in premenopausal or postmenopausal women, the fi brous nature
of the reaction sometimes is such that local anesthetic does not diffuse well throughout the
breast. If local anesthetic is chosen, however, I always avoid the use of epinephrine because
bleeding, which occurs some time later, may not be detected at the time of operation.
◆ Many lesions can be reached through an areolar margin incision, even though they
appear initially to be some distance from the areolar margin. However, if a lesion is
too far from the areolar margin, then an incision directly over the lesion in Langer’s
lines paralleling the areolar margin should be used. Radial incisions are to be avoided
(Figures 12-1 and 12-2).
◆ A preoperative mammogram is required for all patients who are to have a breast operation.
◆ Prophylactic antibiotics are given.
CHAPTER
12
Excision of Benign
Breast Lesion
Courtney M. Townsend, Jr.
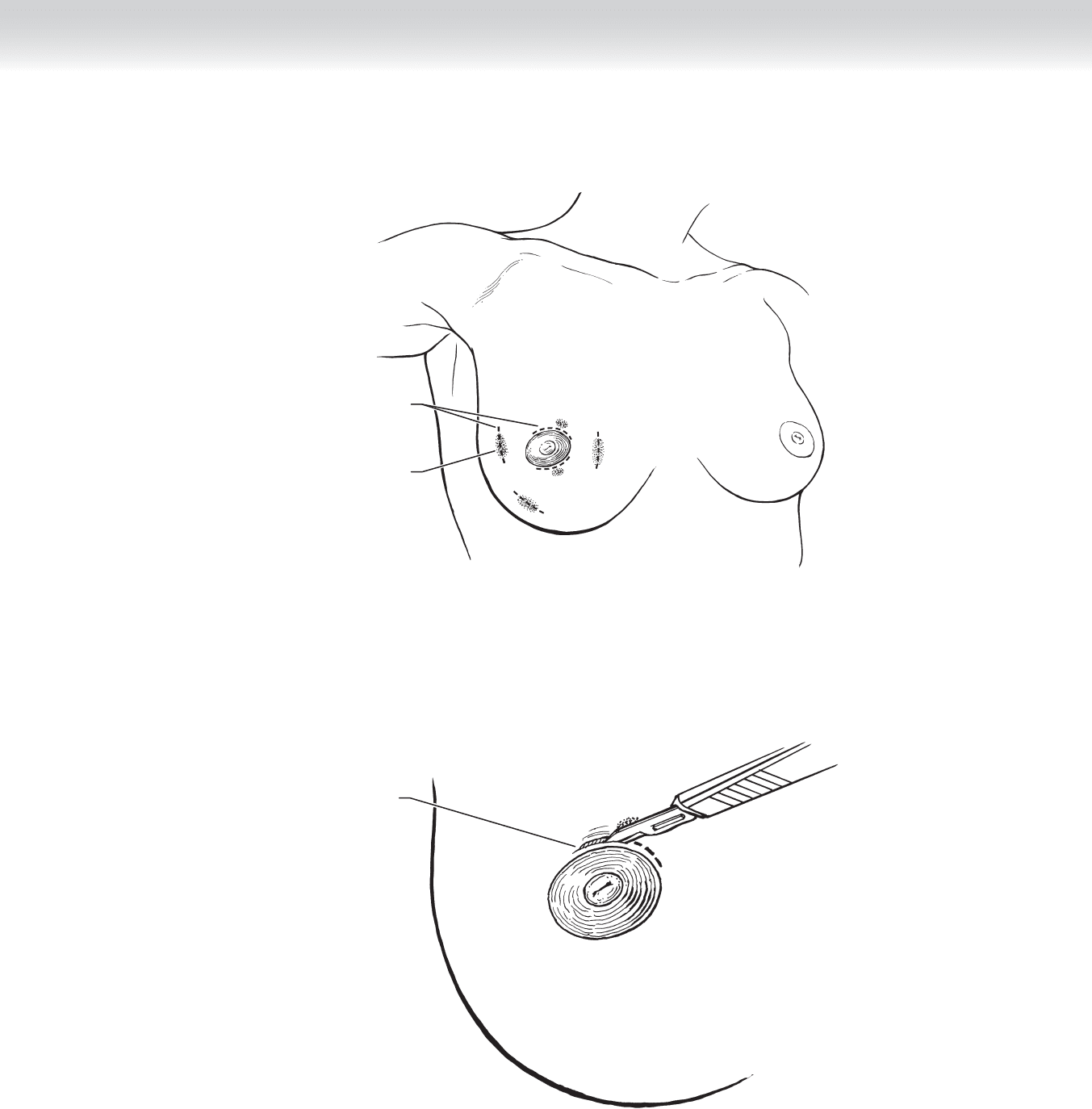
CHAPTER 12 • Excision of Benign Breast Lesion 145
Incision lines
Tumor
FIGURE 12 –1
Incision near
areolar edge
FIGURE 12 –2

146 Section II • The Breast
STEP 3: OPERATIVE STEPS
1. INCISION
◆ Regardless of the size of the incision, fl aps are raised after the skin incision has been carried
down through the intramammary fat.
2. DISSECTION
◆ The lesion is then approached directly or, if it is not a palpable lesion, the area of breast
tissue into which the localizing wire disappears is resected (Figures 12-3 and 12-4).
◆ The portion of tissue into which the wire disappears is excised blindly and the specimen
mammography is required to determine that the lesion has been removed.
◆ For a solid lesion, the margin is easily determined. I use a traction suture placed in a fi gure-
of-eight fashion rather than clamps.
◆ Before fi nal removal of the lesion, the borders are marked. I use a short suture on the
superior margin, a long suture for the lateral margin, and a traction suture of intermediate
length marks the superfi cial margin.
◆ Hemostasis is achieved with coagulating cautery, and the wound is irrigated with hydrogen
peroxide to aid in detection of bleeders.
