Townsend Courtney M.Jr., Evers B. Mark. Atlas of General Surgical Techniques: Expert Consult
Подождите немного. Документ загружается.

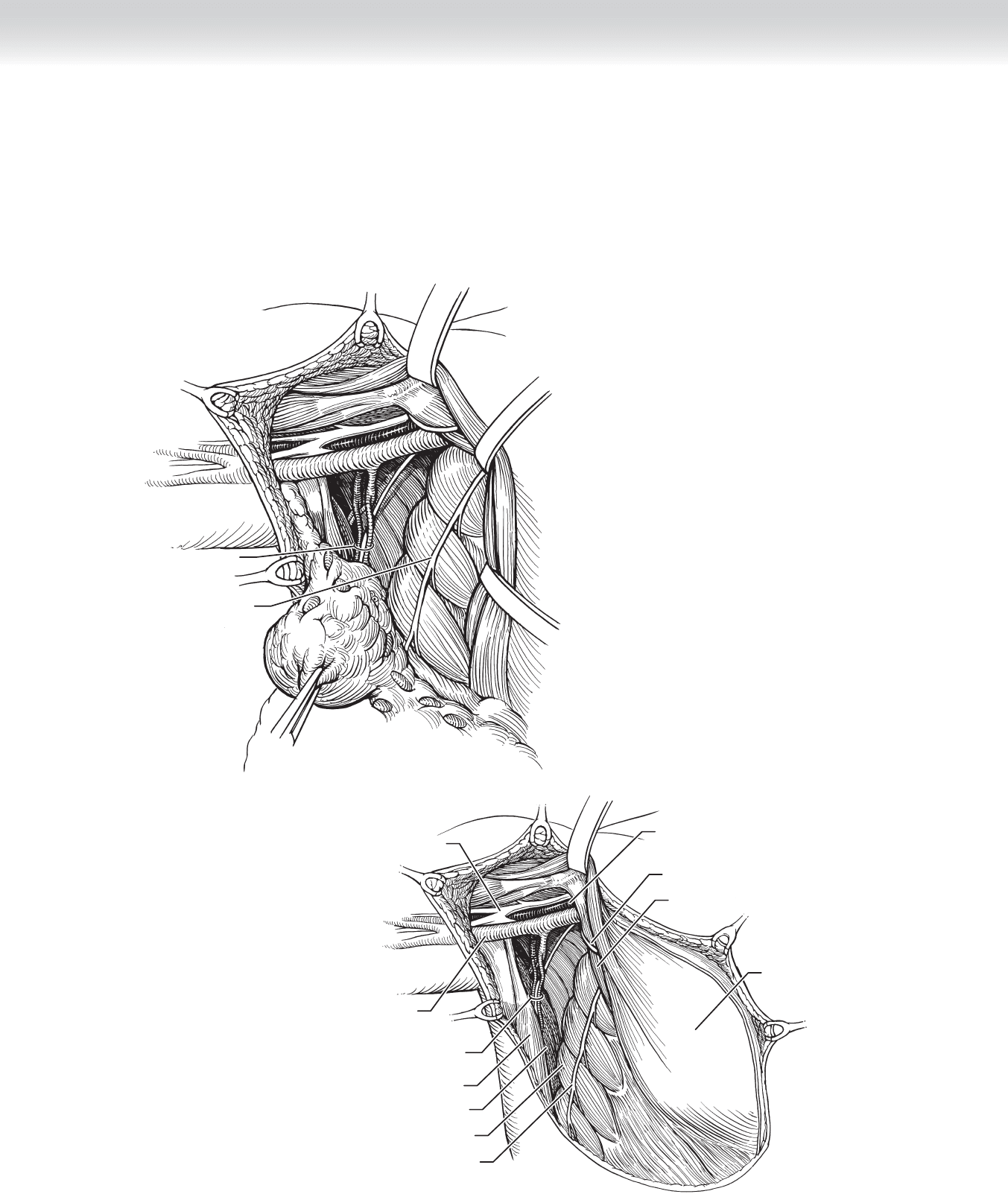
Thoracodorsal
artery, nerve, and vein
Long thoracic nerve
FIGURE 10 –10
Axillary vein
Long thoracic nerve
Brachial plexus
Axillary artery
Medial anterior thoracic nerve
Pectoralis major muscle
Pectoralis minor muscle
Serratus anterior muscle
Teres major muscle
Latissimus dorsi muscle
Thoracodorsal
artery, nerve, and vein
FIGURE 10 –11
◆ The axilla and breast are removed and identifi ed with sutures that distinguish the apex of
the axilla and the orientation of the breast. The axilla and the chest wall are visualized
(see Figure 10-11). The cavity is irrigated with warm saline. Any residual bleeding vessels
are cauterized or ligated.
CHAPTER 10 • Modifi ed Radical Mastectomy 127
128 Section II • The Breast
3. CLOSING
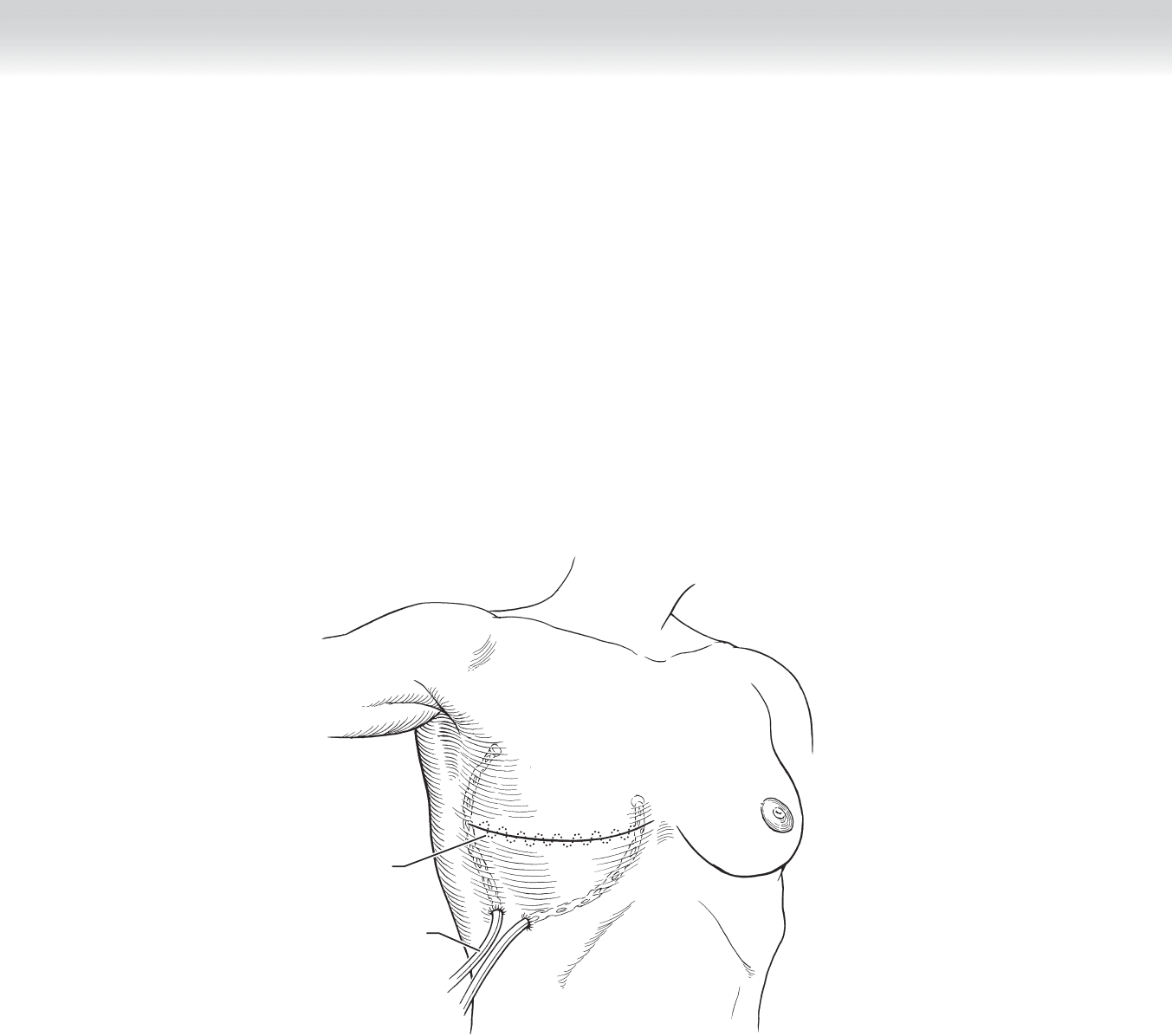
◆ Two closed suction drains, such as #10 Jackson-Pratt drains, are inserted through separate
small stab incisions inferior and lateral to the skin incision, one oriented toward the axilla
and the second anteriorly beneath the skin fl aps. The drains are secured in place with 2-0
silk sutures.
◆ The skin is closed in two layers with absorbable sutures, a deep layer of 3-0 Vicryl sutures,
and a subcuticular closure with 4-0 Monocryl sutures (Figure 10-12). Steri-Strips or
Dermabond may be used for skin approximation. A light dressing or special mastectomy
bra is applied with loose fl uff gauze dressings.
Incision closed
with subcuticular
running suture
Drainage catheters
FIGURE 10 –12

CHAPTER 10 • Modifi ed Radical Mastectomy 129
STEP 4: POSTOPERATIVE CARE
◆ Drains are emptied 2 to 3 times per day and drain output is recorded on a log.
◆ Drainage may be sanguinous immediately postoperatively, but should be dilute.
◆ Continued postoperative frank bloody output indicates ongoing bleeding and warrants
return to the operating room.
◆ Drainage clears to serosanguinous, then clear and straw-colored.
◆ Cloudy fl uid may indicate bacterial infection and should be cultured.
◆ Drains are removed when the output is less than 30 mL for 2 consecutive days.
◆ Drains usually remain for 7 to 10 days.
◆ Seroma may form after drain removal.
◆ Aspirate in clinic if large, suspicious for infection, or uncomfortable.
◆ Multiple aspirations may be required.
◆ Compression dressing may reduce likelihood of seroma reaccumulation.
◆ Some seromas reabsorb without aspiration if they are small.
◆ Dressings are removed after 48 hours.
◆ Pain out of proportion to the procedure may indicate a signifi cant hematoma, for which
dressings should be removed earlier.
◆ Other indications include fever and excessive drainage.
◆ Shower may be acceptable after 48 hours when dressings are removed.
◆ The surgical site is bathed with mild soap and water, patted dry, and redressed around
the drain site.
◆ The incision may be left open according to individual preference.
◆ Tub baths are usually not advised while drains are in place.
◆ Antibiotics are usually not needed but may be considered on an individual basis for the
following:
◆ Previous surgical biopsy
◆ Immunocompromised individuals
◆ Local wound conditions
◆ Limited exercises are initiated on postoperative day 1 and increased to range-of-motion and
strengthening exercises after the drains are removed.
◆ Consultation with American Cancer Society for Reach to Recovery is helpful.
◆ Consultation with occupational therapy for rehabilitation is useful.
◆ Individuals are monitored for lymphedema.

130 Section II • The Breast
◆ Patient education about long-term precautions for protection of the affected extremity
include the following:
◆ Avoidance of blood pressure measurements and phlebotomy sticks on the affected
extremity
◆ No intravenous infusion lines
◆ No constrictive clothing
◆ Electric razors for shaving
◆ Protective gloves for tasks that may lacerate the skin and lead to infection
◆ Early intervention with antibiotics for a hand or arm infection, often requiring hospital-
ization for parenteral antibiotics
◆ Compression sleeve and glove may be indicated for cases of extensive nodal disease,
combination surgery and radiotherapy, and evidence of lymphedema, as well as for
prophylaxis for air travel.
◆ Postoperative radiotherapy or chemotherapy is not initiated for 2 to 3 weeks.
◆ Skin fl ap loss may require local care with wet to dry dressings or silver sulfadiazine
(Silvadene) cream if limited or surgical revision if skin loss is extensive.
◆ A bra and prosthesis are measured and fi tted for long-term symmetry or for a short interval
while the patient is awaiting autologous or implant reconstruction.
◆ Scarring maybe reduced with application of a silicone sheet, such as Biodermis.
STEP 5: PEARLS AND PITFALLS
◆ Discussion with the interdisciplinary team will sequence treatment in the most appropriate
manner.
◆ Surgical planning in conjunction with the plastic surgeon will result in optimal cosmetic
outcome.
◆ Skin-sparing mastectomy leads to the best cosmetic appearance of the reconstructed breast.
◆ Gentle handling of the skin fl aps reduces the risk of fl ap loss.
◆ Preservation of the fascia of the serratus anterior muscle on the chest wall and identifi cation
of the long thoracic nerve underlying it on the chest wall will reduce the risk of transection
and the winged scapula deformity.

CHAPTER 10 • Modifi ed Radical Mastectomy 131
◆ Dissection along the lateral aspect of the latissimus dorsi muscle reduces the likelihood of
injury to the thoracodorsal trunk and weakened shoulder adduction.
◆ Preservation of the medial pectoral nerve prevents atrophy of the pectoralis major muscle
and chest wall contour.
◆ Preservation of the intercostal brachial cutaneous nerves maintains sensation to the medial
aspect of the upper extremity and prevents bothersome dysesthesias.
◆ Preservation of fatty tissue and lymphatic channels from the arm around the axillary vein
reduces the risk of lymphedema.
◆ In obese patients, anatomic boundaries may be more diffi cult to identify and require
wider exposure, increased operative time, and patience during the procedure.
◆ The pulse in the axillary artery is a landmark that can help orient the surgeon to stay
inferior.
SELECTED REFERENCES
1. Fisher B, Anderson S, Bryant J, et al: Twenty-year follow-up of a randomized trial comparing total
mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer.
N Engl J Med 2002;347:1233-1241.
2. Iglehart JD, Kaelin CM: Diseases of the breast. In Townsend C Jr , Beauchamp R, Evers B, Mattox K (eds):
Sabiston Textbook of Surgery. Philadelphia, Elsevier Saunders, 2004, pp 867-927.
3. Staradub VL, Morrow M: Modifi ed radical mastectomy with knife technique. Arch Surg 2002;137:
105-110.
4. Stolier AJ, Grube BJ: Areola-sparing mastectomy: Defi ning the risks. J Am Coll Surg 2005;201:118-124.
5. Veronesi U, Cascinelli N, Mariani L, et al: Twenty-year follow-up of a randomized study comparing
breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med 2002;347:
1227-1232.

132
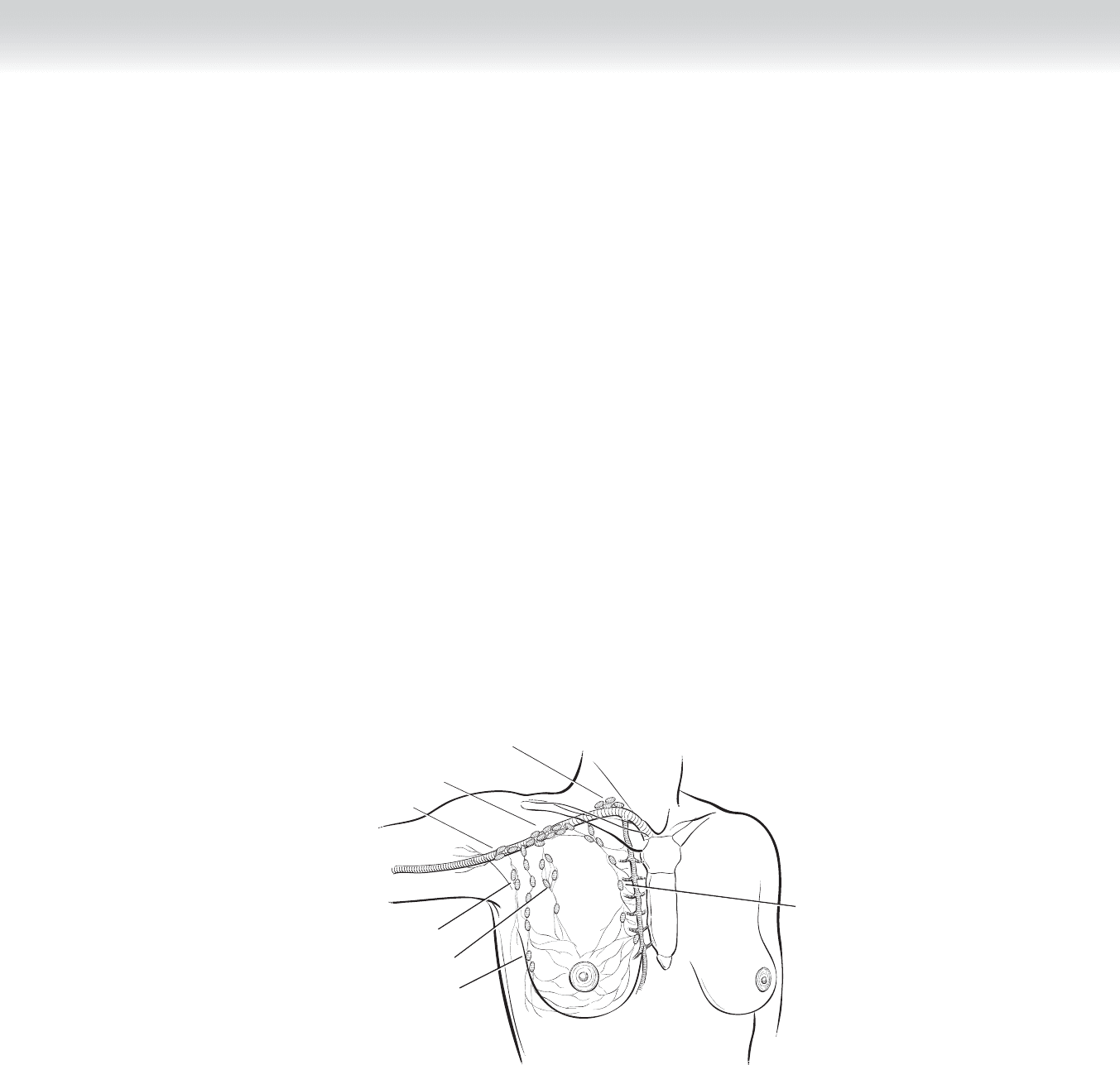
INTRODUCTION
Regional lymph node status is the most powerful predictor of recurrence and survival in
patients with breast cancer and melanoma. Nodal staging remains an essential component in
the decision-making process to offer adjuvant therapy for both breast cancer and melanoma.
Over the last century, experience with surgical clearance of a nodal basin has shown that this
procedure can result in signifi cant morbidity: pain, paresthesias, seroma, infection, limitation
of limb motion, lymphedema, and lymphangitis. Sentinel lymph node (SLN) biopsy has
proven to be a highly accurate technique with minimal morbidity. The development and adap-
tation of SLN biopsy has revolutionized the staging of melanoma and breast cancer.
STEP 1: SURGICAL ANATOMY
◆ SLN biopsy is most commonly performed for breast cancer. Although the same principles
and techniques apply to SLN biopsy for primary malignant melanoma, this chapter
describes in detail SLN biopsy for breast cancer. Figure 11-1 demonstrates the lymphatic
drainage of a breast cancer to the axillary lymph nodes.
STEP 2: PREOPERATIVE CONSIDERATIONS
◆ The SLN is defi ned as the fi rst draining lymph node in the axilla to receive lymphatic
drainage from a primary breast tumor. Should regional metastatic disease exist, the SLN is
the node most likely to contain metastases. Conveniently, if the SLN is negative for metastasis,
then the remainder of the nodal basin should also be negative. Therefore, the SLN should
refl ect the histopathologic status of the entire axilla. In 1992, Morton’s group performed
SLN biopsy in more than 500 patients with melanoma, removing the SLN, as well as the
remaining regional lymph nodes. The pathology of the SLN predicted the remaining regional
nodal status with 99% accuracy. His pioneering work was validated by studies at other
institutions with completion lymphadenectomy, histopathologic nodal examination, and
long-term follow-up to identify potential recurrences in undissected nodal basins following
a negative SLN biopsy. Similarly, Giuliano reported initial experience with SLN biopsy for
breast cancer using vital blue dye injection, including validation with histopathologic
examination of the non-SLN.
CHAPTER
11
Sentinel Lymph Node Biopsy
Celia Chao
CHAPTER 11 • Sentinel Lymph Node Biopsy 133
Pectoral nodes
Parasternal
nodes
Supraclavicular
nodes
Subclavian
nodes
Brachial nodes
Axillary nodes
Interpectoral nodes
FIGURE 11 –1
◆ Defi nitions: Successful SLN biopsy is judged by two critical parameters: the SLN identifi cation
rate and the false-negative rate. The SLN identifi cation rate is the frequency of fi nding and
removing an SLN. When the SLN cannot be identifi ed, a standard level I/II axillary dissection
must be performed. The false-negative rate is the proportion of patients with positive lymph
nodes who are incorrectly staged by the SLN biopsy procedure. Understanding that no staging
procedure is 100% accurate, we accept a small false-negative rate (5% or less) to spare most
true-negative patients the morbidity of a full level I and II axillary dissection.
◆ Pathologic examination of the SLN: By examining serial sections, a more thorough evalua-
tion of the nodal specimen is possible. The SLN biopsy identifi es the node(s) that should be
more closely scrutinized. Such a focused examination would be prohibitively costly and
time-consuming if performed on the entire contents of an axillary dissection.
◆ A team approach: Implementation of SLN biopsy requires the cooperative efforts of multi-
ple disciplines: surgeons and the operating room staff and colleagues from the departments
of radiology, nuclear medicine, pathology, and anesthesiology. The “team” must agree on a
protocol: how to perform injections, how to dispose of radioactive waste, what type of
radionuclide to use, and which adaptation of a SLN pathology protocol should be used.

STEP 3: OPERATIVE STEPS
◆ Patient eligibility: SLN biopsy is appropriate for patients with T1-T3 breast cancers without
palpable nodal metastases (clinical N0). SLN biopsy is applicable for patients undergoing either
a breast-conserving operation or mastectomy and is equally accurate after open excisional
breast biopsy or needle biopsy that has been performed for diagnosis. The procedure is most
appropriate for biopsy-proven invasive cancer, including multifocal/multicentric disease. SLN
biopsy can be considered for ductal carcinoma in situ, in which there is a high likelihood of an
invasive component, or if mastectomy is considered. Contraindications include pregnancy, pal-
pable axillary nodal metastases, hypersensitivity to either blue dye or technetium sulfur colloid,
and prior major breast or axillary operations that could interfere with lymphatic drainage.
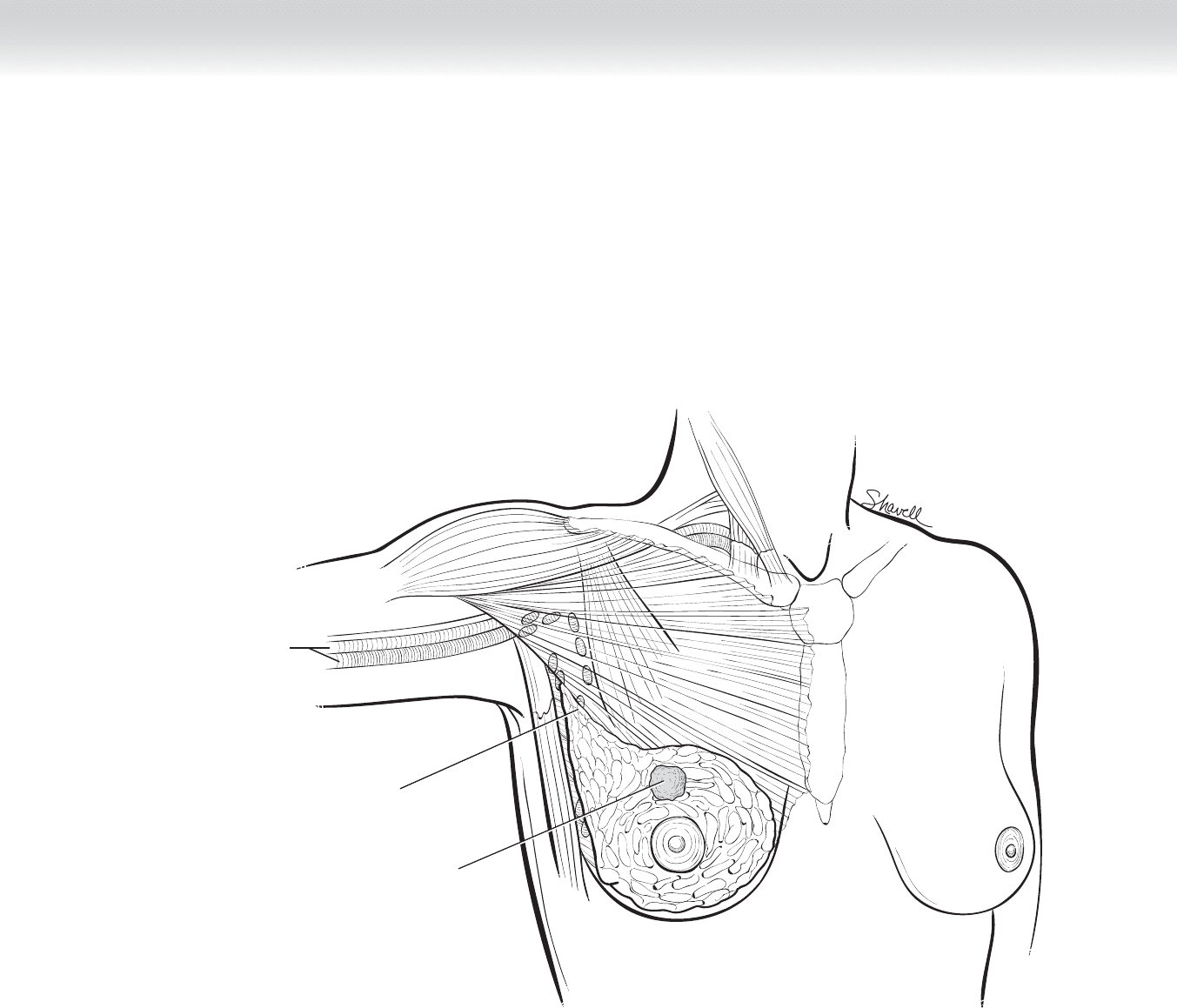
◆ Dual-agent injection technique: Intraoperative lymphatic mapping using vital blue dye,
radioactive colloid, or a combination of both is performed to identify the SLN. I advocate
the use of dual-agent injection to facilitate SLN localization. The combination of the two
techniques—visualization of the blue dye and intraoperative gamma probe detection—
provides overlapping and complementary ability to discriminate the SLN. Some SLNs may
be blue-stained but not radioactive (“blue, not hot”), and others may be radioactive but not
blue (“hot, not blue”); but most SLNs will be both blue and hot. Use of dual agents
provides more accurate nodal staging than the use of either agent alone.
◆ I recommend preoperative dermal radioactive colloid injection using 0.5 mCi of 0.2 m
technetium-99 sulfur colloid in a volume of 0.2 to 0.5 mL at least 30 minutes before opera-
tion. The use of fi ltered or unfi ltered colloid has been shown to be equivalent in terms of
identifi cation rates and false-negative rates. Equal injections into the dermis (intradermally)
are accomplished using a tuberculin syringe with a 25- to 30-gauge needle (raising a wheal)
immediately anterior (superfi cial) to the tumor site, using four to fi ve separate injections
(Figure 11-2). The use of routine lymphoscintigraphy has been shown to be neither neces-
sary nor helpful in SLN biopsy for breast cancer. However, because of less predictable
drainage patterns, such as bilateral drainage basins, or the possibility of interval node
involvement, a lymphoscintigram is recommended routinely for melanoma.
◆ Injection in the areolar border has been shown to be accurate for breast cancers located in
any quadrant or centrally. Embryologically, all the lymphatic drainage of the breast con-
verges in the periareolar or subareolar plexus of lymphatics. Therefore injection of the are-
ola will accurately refl ect the drainage of tumors in any part of the breast. This technique
has been advocated for patients with multicentric or multifocal breast cancer.
◆ Following radioactive colloid injection, the patient is taken to the operating room. For patient
comfort, I perform almost all SLN biopsies with the patient under general anesthesia, without
muscle relaxant, although it is possible to use local anesthesia. Patients should be counseled
preoperatively that the blue dye injection will impart a change to the color of their urine and
that there is a small chance of allergic reaction to the dye (approximately 1 in 10,000).
Adverse reactions, including anaphylactic reactions, to vital blue dye are rare but have been
documented. Allergic reaction to the blue dye may manifest as blue-colored hives.
Section II • The Breast134
CHAPTER 11 • Sentinel Lymph Node Biopsy 135
Axillary lymph nodes
Tumor
Axillary artery
and vein
FIGURE 11 –2
◆ Patients will occasionally have a noticeably blue tattoo on the skin after the procedure.
They should be told that this color will fade and disappear with time. The anesthesiologist
should be aware that pseudohypoxia is often seen intraoperatively as a result of the blue
dye, which interferes with pulse oximetry, falsely lowering oxygen saturation readings. The
use of radioactive colloid is safe, and numerous reports have documented the relatively low
amount of radiation exposure associated with its use.

136 Section II • The Breast
◆ For beginners, I recommend that the entire arm (limb) be prepped and draped into the
operative fi eld. This allows for mobility of the arm and offers potentially easier access to the
SLN(s). After the patient is prepped and draped, 5 mL of Lymphazurin (1% isosulfan blue)
dye can be injected peritumorally, in a subareolar location, or subdermally (deeper than
intradermal, no wheal), taking care to disperse the dye around the tumor (Figure 11-3).
For melanoma, 1 mL of blue dye intradermally (raising a wheal) is suffi cient. A 5-minute
massage of the area following blue dye injection helps stimulate lymphatic uptake toward
the axilla or nodal basin of interest. Peritumoral injection of isosulfan blue dye is performed
by injecting 1 mL in each of four corners intraparenchymally around the tumor, with the
fi nal 1 mL injected superfi cial to the tumor (between the tumor and the skin). For palpable
tumors, the injection is easily accomplished. For nonpalpable tumors, the injection is
guided by ultrasound or by judging the depth and direction of the imbedded wire following
standard needle localization. It is helpful for the radiologist to mark on the skin anterior to
the tumor with an indelible marker at the time of needle localization. It is not advisable to
inject all of the blue dye or radioactive colloid down the localization needle, because this
does not disperse the blue dye well and may concentrate the dye deep within the breast
tissue. For patients who previously have undergone excisional biopsy, injection should be
made around the biopsy cavity, avoiding the seroma cavity.
1. INCISION
◆ The hand-held gamma counter is used to locate the SLN transcutaneously, and a 3-cm
incision is made in line with the usual axillary dissection incision, usually just lateral to the
pectoralis muscle edge and just below the hairline (Figure 11-4). The localization of the
“hot spot” allows for planning of a small incision over the suspected site of the SLN. If a hot
spot is not identifi ed, a curved transverse incision in the lower axilla just below the hairline
provides excellent exposure.
