Nof S.Y. Springer Handbook of Automation
Подождите немного. Документ загружается.


Automation in Hospitals and Healthcare 77.3 Applications 1395
a National Health Information Network (NHIN) to
connect these RHIOs. Unfortunately, even at an insti-
tutional level there are numerous clinical and financial
applications that have difficultly communicating and
thus there are significant unmet needs even within a sin-
gle organization. Many countries across the globe are
issuing tenders to seek solutions for health information
exchange on national levels.
Putting aside the complex business model and or-
ganizational barriers that have been significant barriers
towards significant national and local information ex-
change, there continues to be significant technology
barriers. One of the fundamental challenges resides in
the prime directive of medical informatics in that most
systems store data rather than knowledge and as a re-
sult haveno external references to establish the meaning
of data that needs to be exchanged. For example, con-
sider allergies. Allergies represent one of the most acute
life threatening risks to an individual whenever he en-
counters a healthcare system, especially if he enters the
system unconscious. Surprisingly, there is no common
dictionary for allergies, and as a result most systems
have no method to exchange allergies in a form be-
yond simple free text. With free text allergies there is
no method to perform simple allergy checking before
prescribing or administering a drug.
Today organization such as Health Language 7
(HL7), Integrating the Healthcare Enterprise (IHE),
Healthcare Information Technology Standards Panel
(HITSP), and the Center for Healthcare Information
Technology are all working on establishing standards to
facilitate interoperability across institutions and across
vendors. Although there are emerging standards for
rudimentary exchange of information today there are
surprisingly few examples of information exchange
even at the level we have come to expect in the banking
industry. With patients continually changing healthcare
environments due to changes in health and changes
in insurance, the challenge of interoperability must be
solved to ensure that information technology has a sig-
nificant impact on the quality of care.
77.3.7 Enterprise Systems
Historically, patient access and financial systems were
the first to gain a foothold in healthcare. Driven by the
bottom line, these supported the back office and had no
access to (or need for) clinical data. Clinical systems
followed, designed to address specific needs in individ-
ual care areas such as labor and delivery, where there
was a need to record and store the massive amounts
of information generated by fetal heart monitors and
other devices. For the past two decades, lab systems
built around the workflow of technicians and pathol-
ogists have had the capability to collect results from
a wide array of tests and presentphysicians with a single
view of all the data for each patient (although in most
physician’s offices that information is still presented on
paper rather than electronically).
Because these systems were developed for specific
care areas, each tightly adhered to the workflow in one
particular area. Many healthcare organizations adhered
to a best-of-breed approach, buying a lab system from
one vendor, a pharmacy system from another, a peri-
operative system from a third, and so on. These care
area-specific systems can be more nimble, and can be
installed in a matter of weeks, but require complex in-
terfaces in order to share data with each other. As time
passed, clinicians recognized the need for enterprise-
wide systems, so some vendors of area-specific systems
began broadening their scope.
Other vendors took the approach of developing
enterprise-wide systems that allow information to eas-
ily cross the boundaries between care areas. Consider,
for example, what happens when a physician orders
medication for a hospital patient: the provider needs
to know whether the patient is allergic to that drug, or
has been given any other medication that should not
be combined with the new one, formularies must be
consulted to see whether the hospital is dispensing the
drug and whether the patient’s insurer will pay for it,
the order must be transmitted to the hospital pharmacy,
where the pharmacist double-checks the dose to make
sure it is appropriate for the patient’s age, weight, and
condition. After the pharmacist dispenses the drug, it
must be conveyed to the right location in the hospital,
where a nurse will pick it up, administer it to the pa-
tient, and document the time of administration (perhaps
using a barcode scanner to make sure the right patient is
being given the right medication).
The trade-off for the easy flow of information across
the enterprise is in specificity and implementation time.
The best area-specific systems do one thing only, and
do it better than the current generation of enterprise sys-
tems. Smaller, more discrete systems are also easier and
faster to install. As the technology matures, however,
we will see a convergence as enterprise systems acquire
the greater depth of area-specific capabilities.
Part H 77.3
1396 Part H Automation in Medical and Healthcare Systems
77.4 Conclusion
The practice of healthcare is incredibly complex gen-
erates massive amounts of mission critical data that
must be assimilated and acted upon quickly. In many
cases, the margins for error are slim and the costs
of error immense. Information technology has the po-
tential to transform the way we practice medicine by
turning data into knowledge and knowledge into ac-
tion. This will enable providers to deliver better quality
care at lower cost, to maintain consistency of care for
a given disease while appropriately tailoring care to
each individual patient’s unique condition and genetic
makeup, and to localize the application of care guide-
lines based on knowledge about specific populations of
patients.
Some of the tools to accomplish these goals exist
today, but they need to be modified or adapted to suit
the uniquedemands of healthcare.We have systems that
can alert clinicians to potential errors, for example, but
these systems must be fine-tuned to prevent alert fa-
tigue. Other challenges, such as interoperability, which
enables data sharing among systems from different ven-
dors, remain largely unanswered at the moment.
References
77.1 L.T. Kohn, J.M. Corrigan, M.S. Donaldson (Eds.):
To Err Is Human: Building a Safer Health System
(National Academy Press, Washington 1999)
77.2 J.E. Wennberg: Unwarranted variations in health-
care delivery: implications for academic medical
centers, Br. Med. J. 325, 961–964 (2002)
77.3 E.A. McGlynn, S.M. Asch, J. Adams, J. Keesey,
J. Hicks, A. DeCristofaro, E.A. Kerr: The quality of
health care delivered to adults in the United States,
New Engl. J. Med. 348(26), 2635–2645 (2003)
77.4 R. Mangione-Smith, A.H. DeCristofaro, C.M. Setodji,
J. Keesey, D.J. Klein, J.L. Adams, M.A. Schuster,
E.A. McGlynn: The quality of ambulatory care de-
livered to children in the United States, New Engl.
J. Med. 15, 1515–1523 (2007)
77.5 C. Clancy, K. Cronin: Evidence-based decision mak-
ing: global evidence, local decisions, Health Aff.
24(1), 151–162 (2005)
77.6 R. Hillestad, J. Bigelow, A. Bower, F. Girosi, R. Meili,
R. Scoville, R. Taylor: Can electronic medical record
systems transform health care? Potential health
benefits, savings, and costs, Health Aff. 24(5), 1103–
1117 (2005)
77.7 Clinical Content: http://www.clinicalcontent.com/
about (last accessed May 20, 2009)
77.8 M.A. Shipp, K.N. Ross, P. Tamayo, A.P. Weng,
J.L. Kutok, R.C. Aguiar, M. Gaasenbeek, M. An-
gelo, M. Reich, G.S. Pinkus, T.S. Ray, M.A. Koval,
K.W. Last, A. Norton, T.A. Lister, J. Mesirov,
D.S. Neuberg, E.S. Lander, J.C. Aster, T.R. Golub:
Diffuse large B-cell lymphoma outcome predic-
tion by gene expression profiling and supervised
machine learning, Nat. Med. 8(7), 68 (2002)
77.9 S. Adak, K. Illouz, W. Gorman, R. Tandon, E.A. Zim-
merman, R. Guariglia, M.M. Moore, J.A. Kaye:
Predicting the rate of cognitive decline in aging
and early Alzheimer disease, Neurology 63(1), 108–
14 (2004)
77.10 H.B.Nguyen,J.Banta,T.Cho,C.VanGinkel,
K. Burroughs, W.A. Wittlake, S.W. Corbett: Mor-
tality predictions using current physiologic scoring
systems in patients meeting criteria for early
goal-directed therapy and the severe sepsis re-
suscitation bundle, Shock 30(1), 23–28 (2008)
77.11 C.M. Birkmeyer, D.E. Wennberg: Patient Safety
Standards (Leapfrog Group, 2003)
Part H 77

1397
Medical Auto
78. Medical Automation and Robotics
Alon Wolf, Moshe Shoham
Robotic systems that are integrated in medical
applications are designed to help and assist rather
than injure a human being, whether it is the
patient or the operator. This chapter presents
the classification of medical robots as passive,
semiactive, active, remote manipulators, and
navigators. The kinematic structure of medical
robots is discussed next, as are the fundamental
requirements from medical robots. Finally, the
main advantages and emerging trends in medical
robotics are given.
78.1 Classification of Medical Robotics Systems1398
78.1.1 Passive Medical Robotic Systems ....1398
78.1.2 Semiactive Medical
Robotic Systems ...........................1399
78.1.3 Active Medical Robotic Systems ......1399
78.1.4 Remote Manipulators ...................1400
78.1.5 Navigators...................................1401
78.2 Kinematic Structure
of Medical Robots.................................1403
78.3 Fundamental Requirements
from a Medical Robot............................1404
78.4 Main Advantages
of Medical Robotic Systems....................1404
78.5 Emerging Trends
in Medical Robotics Systems ..................1405
References ..................................................1406
1. A robot may not injure a human being or, through
inaction, allow a human being to come to harm.
2. A robot must obey orders given to it by human
beings except where such orders would conflict with
the First Law.
3. A robot must protect its own existence as long as
such protection does not conflict with the First or
Second Law.
Written almost 65years ago, these three laws of
robotics by the famous science fiction author Issac
Asimov (Runaround, 1942) are still very relevant and
serve, though not literally, as guidelines for the field of
medical automation and robotics. By definition, robotic
systems that are integrated in medical applications are
designed to help and assist rather than injure a human
being, whether it is the patient or the operator. Many
precautions (more than one would find in nonmedical
robotic systems) are being taken to ensure the safety
of patients and operators. As presented in this chap-
ter, these safety measures include, among others, dual
backup systems, as a minimum, and fail-safe systems.
These redundant systems are there to prevent unwanted
motions that may harm the patient or the staff, to assure
accurate performance of the task, and also to protect the
robot itself as stated in the third law of robotics.
As elaborated in this chapter, current medical
robotic systems aredividedinto three categories, mainly
reflecting level of autonomy. The most popular and
widely implemented method is teleoperation, where the
robotic system follows the operator’s (surgeon’s) hand
motions from an offsite control console that can be lo-
cated either in the operating room or even somewhere
overseas using fast communication lines. In this mode
of operation,the robot,just like inAsimov’s second law,
obeys and follows the operator’s commands and mo-
tions. These systems are capable of filtering tremors in
the surgeon’s hand movements (crucial in neurosurgery
and ophthalmic surgery), scaling down the operator’s
motions and forces, and at the same time preventing un-
wanted motions that could harm the patient (the active
constraint concept).
The first swallows of medical robots appeared in
the mid 1980s and early 1990s with the implemen-
Part H 78
1398 Part H Automation in Medical and Healthcare Systems
tation of the Puma 560 for stereotactic neurosurgery.
The application was a computed tomography (CT)-
guided needle steering system for brain biopsy. Then
came ROBODOC from Integrated Surgical Systems
in 1992. ROBODOC milled out precise fittings in the
femur for hip replacement surgery. ROBODOC was
a pioneering surgical active robot that paved the way
for other robotic systems, mainly remotely manipu-
lated, semiactive, and active constraint robots. Current
surgical applications are in the fields of gastroin-
testinal surgery, urology, gynecology, cardiothoracic
surgery, oncology, orthopedic surgery, and neurosur-
gery.
Despite more than two decades of research in the
field of medical robots, it seems that this field has not
yet reached maturity and is still in its infancy. Neverthe-
less this fact does not prevent researchers from thinking
of the next step, i.e., integration of computer-assisted
surgery (CAS) devices into one complete system. This
is called the operating room of the future (ORF). This
initiative is crucial in light of the increasingly growing
number of surgical instruments, monitoring and imag-
ing devices, information systems, and communication
networks used in modern operating rooms and inter-
ventional suites. See also Chap.82 on Computer- and
Robot-Assisted Medical Interventions.
78.1 Classification of Medical Robotics Systems
Medical robots have been classified in the literature
according to the following categories: remote manip-
ulators, and passive, semiactive, and active robots, by
Cinquin [78.1], Stulberg [78.2], Taylor [78.3,4], Troc-
caz [78.5], Bainville [78.6], and Nolte [78.7].
Since this area of research is very dynamic and, in
our opinion,has notyet reached maturity, it is likely that
categories and classifications that are widespread today
will change over time, with the evolution of new con-
cepts. Nevertheless, we present in this chapter a brief
overview of current leading technologies and trends in
the field of medical robotics. For an extensive review
of the literature and classification of existing medical
robotic system we refer readers to [78.8–10].
Finally, we also present the major considerations
to be taken into account in the design of new medical
robotic systems.
78.1.1 Passive Medical Robotic Systems
Passive medical robotic systems support the surgical
procedure, but take no active part during surgery. In
other words, the surgeon is in full control of the sur-
gical procedure at all times, i.e., the actual surgical
procedure is conducted by the surgeon. Early versions
of Arthrobot [78.11] fall into this category of passive
systems. In early stages, the robot was used as an as-
sistant in the operating room to hold the patient’s limb
during joint replacements of knees and hips. Arthrobot
had no sensing capabilities and was able to move only
under explicit human control. Today, one of the main
forms of passive medical robotics is active constraint
robotic systems. Acrobot [78.12] is an example of an
active constraint passive robotic system. Developed by
Davies et al. [78.13–15], its core proprietary technology
centers on thedevelopment of anewtype ofrobotic con-
trol: active constraint robotics for orthopedic surgery.
This concept facilitates synergy between the surgeon
and the robot, provides active assistance to the surgeon,
and prevents surgical errors. The surgeon guides the
surgical tool that is attached to the robot with a han-
dle with a force sensor attached to the robot tip, and
thus uses his/hersuperior humansenses and understand-
ing of the overall situation to perform the surgery. The
robot provides precise geometricaccuracy and increases
the safety by means of a predefined three-dimensional
(3-D) motion constraint that prevents cutting outside
a predefined safe region. This approach, known as
hands-on robotics, keeps the surgeon in the control loop
throughout the surgery. Moreover, the robot is guided
by preoperative image-based planning software. This
image-based software uses a patient’s CT data to facil-
itate precise planning of the surgery, allowing implant
selection and optimal positioning within the joint.
Another passive robot utilizing the active constraint
concept is the MAKO robot, a haptic robotic sys-
Fig. 78.1 Freehand sculptor by BlueBelt
Part H 78.1
Medical Automation and Robotics 78.1 Classification of Medical Robotics Systems 1399
tem that adds the sense of touch to a robotic-assisted
surgical platform. The MAKO Haptic Guidance Sys-
tem is a Food and Drug Administration (FDA)-cleared,
surgeon-interactive robotic system that enables the or-
thopedic surgeon to plan the alignment and placement
of knee resurfacing implants preoperatively and make
intraoperative bone-conserving cuts accurately within
the safe workspace limited by the robot.
The precision freehand sculptor (PFS) by BlueBelt
is a handheld tool to assist the surgeon in accurately
cutting these shapes (Fig.78.1). Its rotating cutter only
allows the surgeon to remove waste bone; the cutter in
turn retracts when it hits good bone (i.e., bone that is
not supposed to bemachined). Thus the surgeon can use
the PFS freehand while it automatically restricts the cut
to the proper shape [78.16]. This mode of operation is
a modification of the active constraint concept. Instead
of preventing hand motion, the system automatically
and actively prevents cutting.
78.1.2 Semiactive Medical Robotic Systems
The semiactive category is presented in [78.17]. In this
research a robot acts as an assistant during the oper-
ation by holding a tool in a steady position to allow
accurate guidance of surgical tools. Other more up-to-
date examples of semiactive systems are the NeuroMate
(Integrated Surgical Systems, USA) and PathFinder
(Armstrong HealthCare Ltd., UK). They provide guid-
ance ofthe surgical tool but theactual surgical operation
is conducted by the surgeon.
One of the very first applications of robotic sys-
tems in a surgical theater was positioning of a needle
for stereotactic neurosurgery [78.18]. This application
involves placement of a needle in a very accurate man-
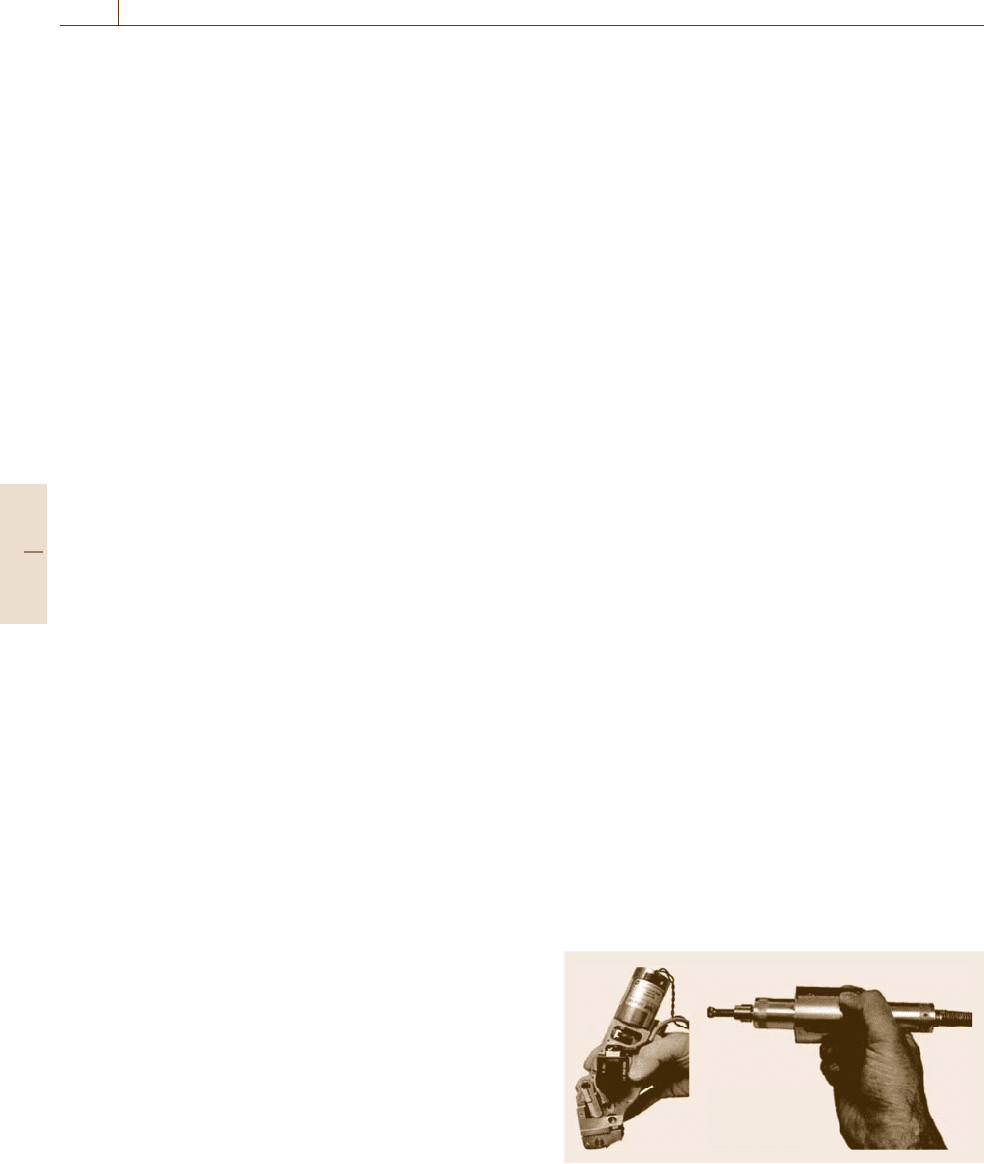
Fig. 78.2 Mazor’s SpineAssist miniature robot for spine
surgery
Fig. 78.3 SpineAssist during surgery
ner in a predefined location in a percutaneous approach
(later used as a semiactive system). Further develop-
ment of this approach is described in [78.19].
A different concept of a semiactive robot had been
developed at the Robotics Laboratory at the Technion–
Israel Institute of Technology and is manufactured and
marketed by Mazor Surgical Technologies [78.20]. Ma-
zor’s SpineAssist (Figs. 78.2 and 78.3)isa2×4inch,
250g, image-based robot designed to guide the surgeon
to precise locations along the patient’s spine according
to a preoperative plan. Its small size and light weight al-
lows mounting the robot directly on the patient’s back,
thus overcoming the patient’s motion relative to the
robot base and as a result improving the accuracy of
the operation. The FDA- and Council Europe (CE)-
approved SpineAssist robot has performed hundreds of
cases and implanted thousands of screws with better
clinical outcome than the freehand approach while at
the same time allowing a minimally invasive approach.
PiGalileo is another bone-mounted guiding system.
Just like in the case of SpineAssist, the actual surgical
operations done with PiGalileo are still performed by
a surgeon, with the electromechanical positioning de-
vice aiding the surgeon in instrument positioning. This
technology is completely under the surgeon’s control
at all times, providing valuable intraoperative feed-
back to the surgeon to help improve precision, thereby
potentially leading to better implant alignment and po-
sitioning.
78.1.3 Active Medical Robotic Systems
Active robotic systems perform surgical tasks, such as
drilling or milling, autonomously with no direct inter-
vention of the surgeon [78.21–23]. This group includes
Part H 78.1
1400 Part H Automation in Medical and Healthcare Systems
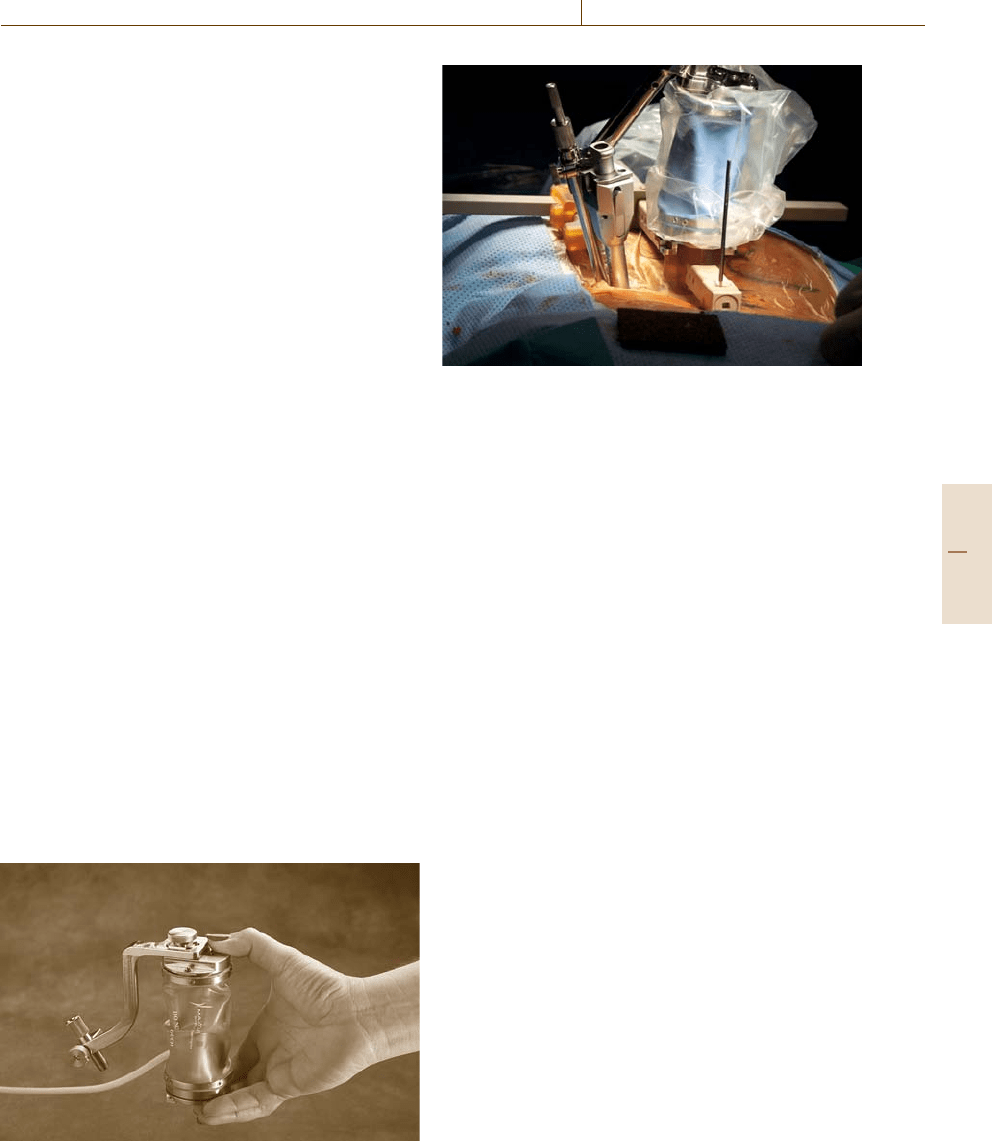
Fig. 78.4 MBARS used for joint arthroplasty
active robots such as RoboDoc,CASPAR, and MBARS.
Perhaps one of the most famous active robots today is
RoboDoc (Integrated Surgical Systems), developed by
Paul et al. [78.24,25]. The system was originally used
for total hip replacement procedures, yet was later mod-
ified foruse in total knee replacement procedures(today
it is less used because of controversy over long-term
clinical effectiveness).
MBARS (Fig.78.4) is an active version of the bone-
mounted robotic system concept. Although this is still
an academic study, the system demonstrates the capa-
bility to actively prepare the bone cavity for an implant
during joint arthroplasty procedures.
The robot is composed of six linear actuators that
are connected in parallel between two rigid platforms:
the lower reference platform and the upper platform,
which is the moving end-effector of the robot. This
structure is known as the classical Stewart–Gough six-
degree-of-freedom robot. The robot is attached to the
femur by three pins: one pin is inserted into the medial
epicondyle, one into the lateral epicondyle, and one into
the metadiaphyseal region of the femur. A rigid con-
nection of the robot to the operated bone is obtained
through these three pins. The robot is equipped with
a milling device, which actively mills the bone accord-
ing to the preoperative plan.
The CyberKnife robotic radiosurgery by Accuracy
System is a radiosurgery system designed to treat tu-
mors anywhere in the body with high accuracy. Using
image-guidance technology and computer-controlled
robotics, the CyberKnife system is designed to track
the tumor continuously, detect its location, and correct
for tumor and patient movement in real time throughout
the treatment. Because of its extreme precision, the Cy-
berKnife system does not require invasive head or body
frames to stabilize patient movement, vastly increasing
the system’s flexibility.
Gamma Knife PERFEXION is Elekta’s new Lek-
sell system for stereotactic radiosurgery in the brain,
cervical spine, and head and neck regions. The Leksell
Gamma Knife PERFEXION expands treatment reach,
offering a wider range of treatable anatomical struc-
ture. This expanded anatomical treatment area offers
dramatic new opportunities to increase patient volume.
Leksell Gamma Knife PERFEXION makes the entire
procedure more efficient and user-friendly. Collimator
changes can be made by the control program, optimiz-
ing the workflow and significantly reducing treatment
time.
78.1.4 Remote Manipulators
Perhaps the most commonly used medical robots to-
day are remote manipulators. Remote manipulators are
robotic system that can be operated from a remote loca-
tion. In other words, the surgeon does not have to be at
the bedside, nor even in the operating room, and yet can
still perform the surgical procedure using the robotic
system, which serves as his hands and eyes.
Remote manipulators are robotic systems that can
be operated from a remote location. Medical proce-
dures utilizing this mode of operation are often named
telesurgery. The first concept was developed at Stanford
Research Center as a project for the USArmy. The con-
cept of telesurgerywas firstdemonstrated in2001, when
an expert surgeon removed the gallbladder of a 68-year-
old patient. This looks like a very common procedure
that is done on a daily basis in many locations around
the world, with one exception: the patient was oper-
ated on in Strasbourg, France and the surgeon operated
Part H 78.1
Medical Automation and Robotics 78.1 Classification of Medical Robotics Systems 1401
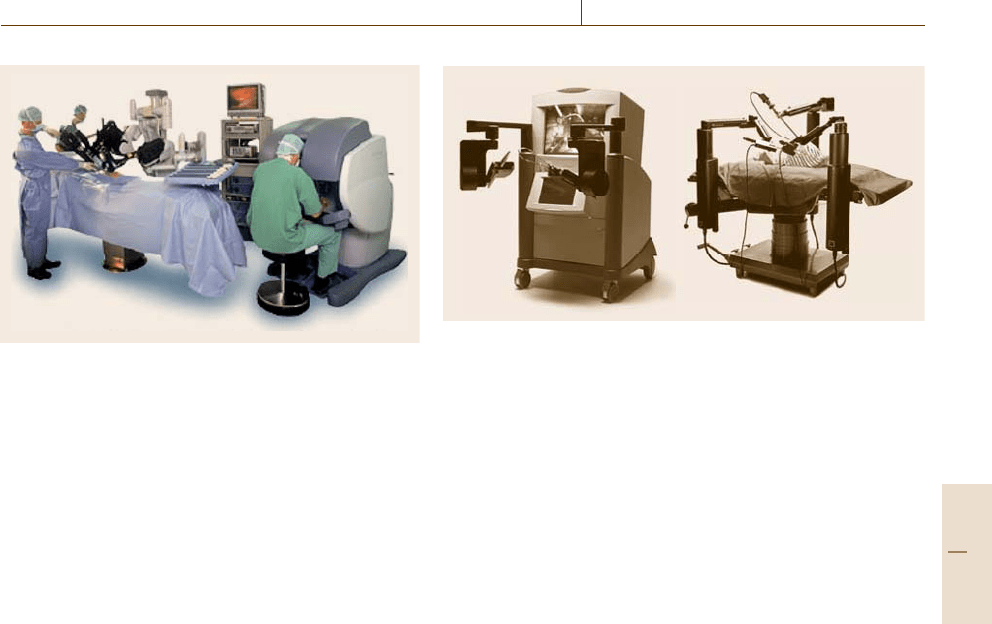
Fig. 78.5 Da Vinci system
from New York. For successful performance of such
a telesurgery, a high-speed computer connected through
a reliable high-speed network is required. This success-
ful demonstration has opened new horizons of surgical
procedures performed worldwide with experts sitting in
communication centers. Telesurgery can bring experts
to places where there are scarce medical facilities and
medical professionals, suchas third-world countriesand
war zones.
Although the first telesurgery was carried out only
in 2001, telesurgical systems were introduced earlier.
Computer Motion (now Intuitive Surgical Inc., USA)
introduced in 1994 the AESOP system. This robotic
system was used to manipulate a camera during laparo-
scopic surgery. Overall, about 70 000 surgeries were
performed worldwide using this system. Once acquired
by Intuitive, the AESOP system was not sold anymore.
Instead, Intuitive Surgical Inc. introduced the Da Vinci
medical robot. During surgery, the surgeon operates the
robot from a remote console using a specially design
control mechanism and a stereo vision system. In April
2005, the Da Vinci system (Fig. 78.5) was approved by
the FDA toperform gynecological procedures, although
it is used for other procedures as well, such as urologic,
general laparoscopic,noncardiovascular, thoracoscopic,
and others.
Although Intuitive Surgical is a world leader in the
development of robotic technology of minimally inva-
sive surgery (MIS) with its Da Vinci robot, it is worth
mentioning another medical robot that competes with
the Da Vinci system for the same market. Computer
Motion (now owned by Intuitive Surgical) introduced
the Zeus system (Fig.78.6). Just like the Da Vinci sys-
tem, Zeus is composed of multiple robotic arms capable
of manipulating MIS tools and visualization equipment
for cardiac surgery.
a) b)
Fig. 78.6a,b Zeus system: (a) console, and (b) robot arms
On 5 April 2001 a 63-year-old male patient un-
derwent multivessel off-pump coronary artery bypass
surgery at the University of Pittsburgh Medical Center
(UPMC) Presbyterian Hospital using the Zeus system.
This was the first time ever that such a procedure was
carried out. MarcoA. Zenati from the UPMC Depart-
ment of Surgery operated the robot while seated at
a console about 10 feet from the patient. The robot was
equipped with an endoscope, whichwas manipulated by
one of the robotic arms using voice commands, while at
the same time the other two arms were controlled by
operating handles that resemble conventional surgical
instruments.
78.1.5 Navigators
Surgical navigators are the central element in many
medical robotic system [78.26]. They come into play
during the registration procedure. Registration is a cru-
cial and necessary procedure, during which each part
of the medical system is synchronized. Most medi-
cal robotic systems include preoperative (sometimes
intraoperative) planning of the medical procedure. Dur-
ing this step, a virtual surgery can be performed
and simulated on a computer screen (just like with
any computer-aided design system). The data pro-
videdtothesurgeonispatientspecificandisusually
based on a preoperative CT or magnetic resonance
imaging (MRI) scan. The end result of this proce-
dure is the transformation that maps the anatomical
position in the operating room to its preoperative
CT/MRI-based model. One example of a method for
achieving this transformation is minimization of the
pointwise distance between a cluster of anatomical
points collected intraoperatively and points on the
preoperative surface model. The coordinates of anatom-
ical points are acquired by touching points on the
Part H 78.1
1402 Part H Automation in Medical and Healthcare Systems
patient’s anatomy (anatomical landmarks) using an
optically tracked probe [78.27]. It is sometimes eas-
ier to think of these systems as global positioning
systems (GPSs) for the operating room. The basic
concept of a surgical navigation system is to ascer-
tain the position, i. e., the location and orientation, of
the relevant components of the system and the pa-
tient’s anatomy in a global coordinate system such
that their relative position can be determined. Dur-
ing surgery, the position coordinates provide precise
guidance to the surgeon to perform a preplanned pro-
cedure.
In 1974, Schlondorff et al. [78.28] developed one
of the first systems for navigational calculations involv-
ing bone. The system used a radiographic centimeter
scale held between the patient’s teeth during a lateral
roentgenogram. The measurements enabled the calcula-
tion of the distances between several anatomical points.
Later, Watanabe et al. [78.29] from Siemens Corpo-
ration published their work on the first model of the
Neuronavigator, a mechanical device based on a multi-
joint 3-D digitizer. The device is used to track the tip of
the sensor arm by indicating its location on preoperative
CT or MRI images.
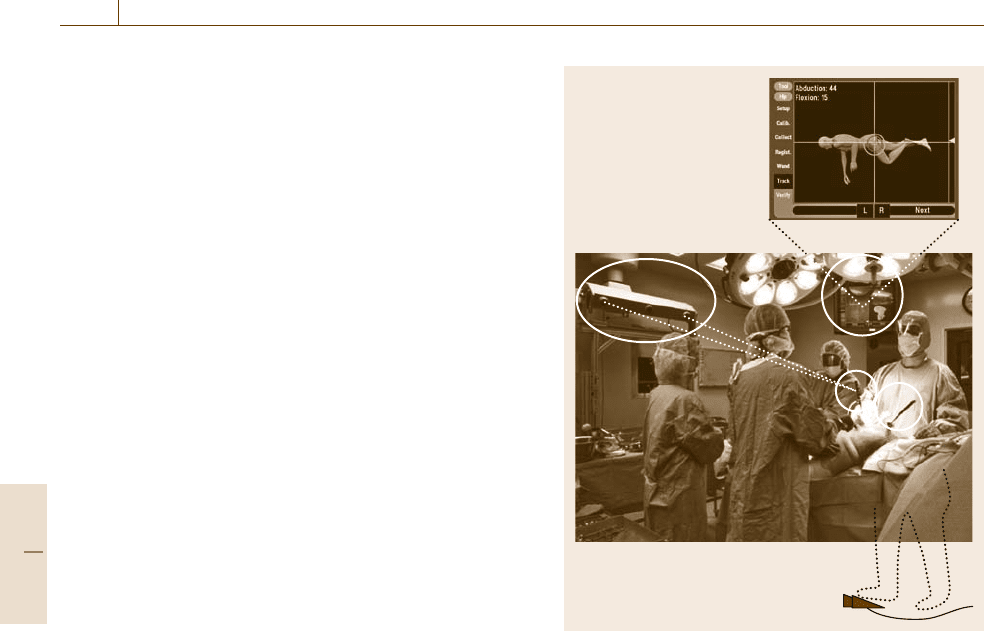
One of the first systems to use an optical-based
navigation technique was HipNav (Fig. 78.7), devel-
oped at Carnegie Mellon University in Pittsburgh, PA
(USA) by DiGioia and Jaramaz [78.30]. The sys-
tem was the first computer-assisted navigation system
for cup placement in total hip replacement (THR)
surgery. Beside its significant clinical contribution, this
has set the standard for preoperative planning and
range-of-motion (ROM) simulations for THR.HipNav
incorporated informationprovided toit by the OptoTrak
system by Northern Digital Inc., Waterloo, Ontario.
The OptoTrak system is composed of three charge-
coupled device (CCD) cameras contained in a rigid
enclosure and a set of active trackers, where the body
of each tracker incorporates a set of light-emitting
diodes (LEDs) mounted at precise relative positions,
and the position of each tracker can be resolved in
the OptoTrak coordinate system. For the HipNav sys-
tem, the trackers were fixed to tools, implants, and
the patient’s bones, enabling active tracking of their
positions during operative procedures. Since HipNav,
there have been other systems that employ this type
of technology, including the VectorVision, SurgiGATE,
Navitrack, StealthStation, Stryker, and Surgetic sys-
tems.
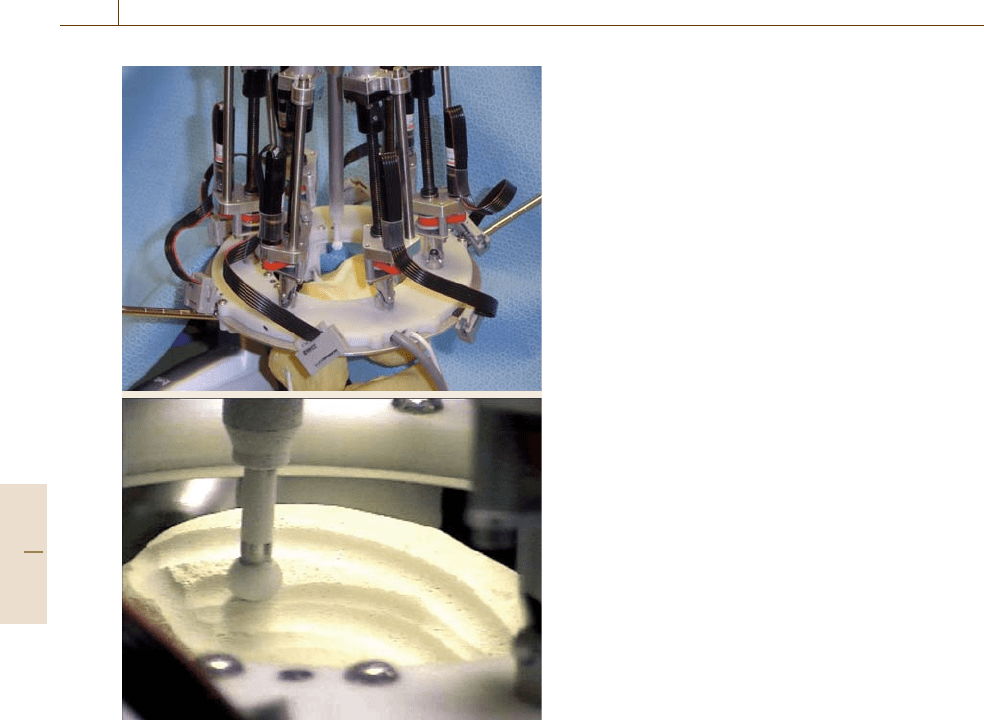
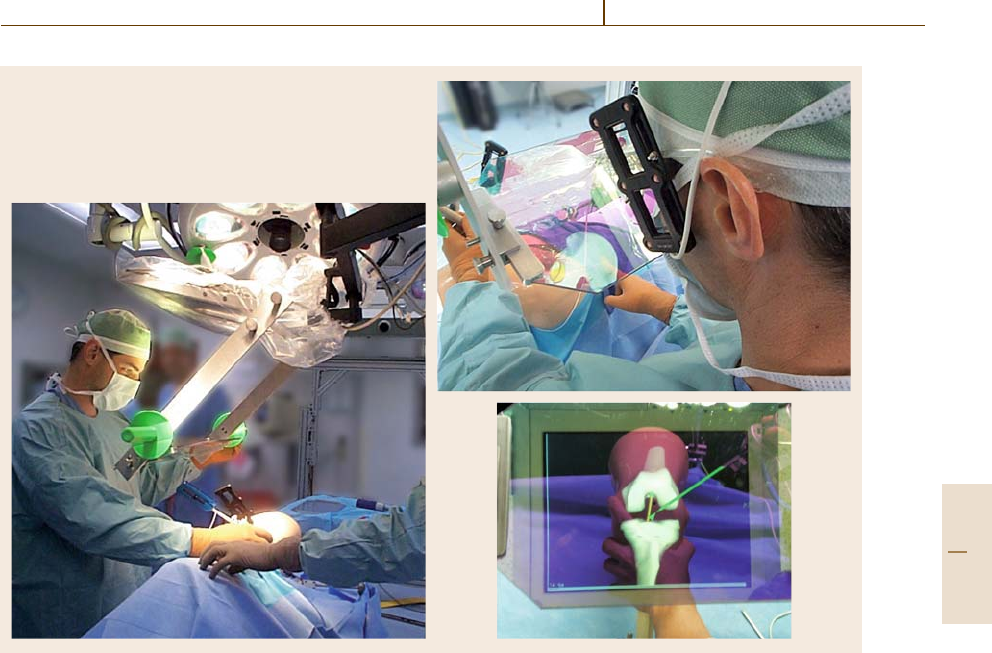
A new version of medical navigators is the image
overlay concept (Fig.78.8). Image overlay is a com-
HipNav system in DiGioia’s
operating room
Fig. 78.7 HipNav system
puter display technique that superimposes computer
images over the viewer’s direct view of the real
world [78.31]. In other words, it is a form of augmented
reality in that it merges computer-generated informa-
tion with real-world images by the projection of virtual
objects in real scene. To do this the system needs to
project the virtual image onto some sort of screen. The
most common measure used is a semitransparent dis-
play device (like a heads-up display in fighter planes),
which allows both viewing the real objects while at the
same time overlaying the virtual image on them. For
example, a 3-D image of a bone, reconstructed from CT
data, can be displayed to a surgeon inside the patient’s
anatomy at the exact location of the real bone, regard-
less of the position of either the surgeon or the patient
(Fig.78.8), creating an elusion of an image which ap-
pears to the viewer to be inside the real objects. To do
this in a convincing yet accurate way, the positions of
the viewer’s head, objects in the environment, and com-
ponents of the display system are all tracked in space.
These positions are used to transform the images so
that they appear to be an integral part of the real-world
environment.
Part H 78.1
Medical Automation and Robotics 78.2 Kinematic Structure of Medical Robots 1403
Fig. 78.8 Image overlay
This technology has many clinical applications; one
of the most common is needle steering, i.e., manipulat-
ing a real/virtual needle into remote unexposed organs
for biopsy, drug delivery, and interventions.
78.2 Kinematic Structure of Medical Robots
In most up-to-date medical robotic systems, a serial
robot is used as a surgical assistant. These robots
suffer from numerous drawbacks related to the se-
rial manipulator, such as low rigidity and accuracy.
The fact that theses robots are integrated in medical
procedures, where accuracy and safety is a matter of
life and death, has led researchers to look for bet-
ter manipulators suited for a specific surgical task or
field of tasks. A family of robots found suitable for
medical application is parallel robotic mechanisms.
Grace and Brandt [78.32, 33] stressed the advantages
of parallel manipulators compared with serial manip-
ulators in surgical operations, mainly due to their low
weight, compact structure, better accuracy, stiffness,
restricted workspace, and low price. However, paral-
lel manipulators have some drawbacks. One of the
main disadvantages of parallel robots is their lim-
ited workspace. Nevertheless, limited workspace can
be considered as an advantage in medical applications
where therequired workspaceis itselfvery limited. This
attribute limits the potential placement positions of the
robot in the operating room (OR), since the parallel
robot has to be positioned very close to the operating
area in order to be able to perform a surgical task within
its limited workspace. In most cases, this requirement is
not feasible due to physical conditions in the OR.One
of the tested solutions has been designed with the en-
tire robotics system attached to the OR ceiling so that
the robot works upside down, as proposed for example
in Fig. 78.5. Inthis way,the robotdoes notinterfere with
the surgical procedure, and is activated and maneuvered
to the operating area when required.
Part H 78.2
1404 Part H Automation in Medical and Healthcare Systems
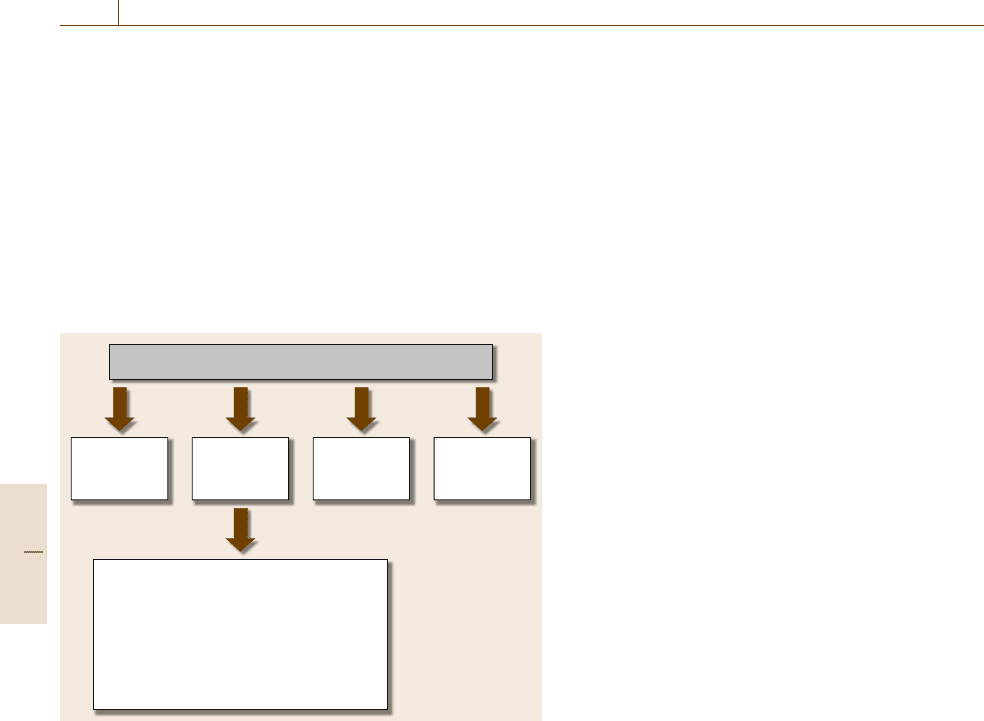
78.3 Fundamental Requirements from a Medical Robot
The fundamental requirements from a medical robot
for surgery tasks were introduced in [78.35], where the
authors stressed the safety requirements (Fig.78.9):
1. Effective control. Both force and speed control of
the end-effector should be allowed or limited by
hardware in all robot configurations.
2. Workspace. The robot workspace has to be limited
to the effective area of the operation, to prevent ac-
Fundamental requirements from a medical robot
Simple
operation
Safety
Easy
sterilization
Compact
size and
low weight
1. Effective control
2. Limited workspace
3. Immunity against magnetic interference
4. Fail-safe mode
5. Safe behavior near singularities
6. Limit force and force feedback
7. Full control option
Fig. 78.9 The fundamental requirements from a medical robot
[78.34]
cidental damage both to the physician and to the
patient.
3. Limited forces or force feedback. The force applied
by the robot during procedures where the robot
takes active tasks and is in contact with live tissue
must be fully controlled. Moreover, in procedures
where different levels of force are applied (such as
bone cutting [78.36]), the physician needs as much
data as possible from the robot concerning the force
applied.
4. Full control option. In procedures where the robot
automatically performs a surgical procedure, the
physician has to be able to take over control of the
robot at any stage during the operation.
5. Fail-safe features. In the event of a malfunction
in the robot, the system has to switch to a fail-
safe mode; for instance, in case of a power failure,
the robot has to remain in its current location until
power is restored.
6. Singularity behavior. The robot path planning must
avoid passing near singular configurations, or ac-
tively prevent the surgeon from driving the robot
through singular configurations, if any, or de-
signed in such a way that all singular poses of
the robot are outside the operating work enve-
lope.
7. Sterilizability. The robot structure must allow steril-
ization, or be protected with a suitable cover.
8. Immunity against magnetic interference of other
surgical tools available in the OR.
78.4 Main Advantages of Medical Robotic Systems
Several researchers have investigated the advantages of
robotic systems in surgery. Kazanzides et al. [78.37]
compared the cross-section of manually broached im-
plant cavities to cavities milled by robots in hip
replacement surgery. The results of this research have
illustrated the robot’s precision compared with the pre-
cision of the human hand. Kavoussi et al. [78.38]
compared the performance of a human to that of a robot
assistant in manipulating the laparoscope. The results
of this research emphasize the superiority of the robot
compared with the human hand in terms of steadiness.
Cameron and Pradeep [78.39] measured the accuracy
of the human hand of four skilled eye surgeons. The re-
sults stressed the tremor and inaccuracy of the human
hand, even for skilled surgeons. An average root-mean-
square (RMS) error of 49μm was obtained when asked
to hold an instrument steady, and 133μm for repeated
actuation. Cameron et al. [78.40] presented a robotic
prototype that incorporates sensing and actuation, re-
porting accuracy of 5μm and better for a robotic system
holding an ophthalmologic microsurgical instrument,
representing a significant improvement with respect to
those presented in the first article [78.39]. These results
indicate that the combination of advanced medicine
with high-technology research capabilities can improve
many surgical procedures that are currently performed
manually and are limited by restricted accessibility and
the lack of preciseness of the human hand. Areas which
Part H 78.4
