Nof S.Y. Springer Handbook of Automation
Подождите немного. Документ загружается.

Automation in Hospitals and Healthcare 77.2 The Role of Medical Informatics 1385
ical ontologies are needed to explicitly articulate the
relationships.
The second example is rule writing for decision
support or reporting. While electronic medical records
systems have allowed institutions to write rules for de-
cision support utilization of rules has been low. In part,
this is due to the difficulty of writing rules without an
ontology. Consider writing a rule that would generate
a list of all patients with lung disease who are also on
blood pressure medication. With ontology this is a sim-
ple task; without one, it requires compiling exhaustive
lists of all possible lung diseases and all possible blood
pressure medications, and then mapping this back to
specific field names in the medical record. These lists
would have to be maintained as new drugs come on the
market or new conditions identified.
77.2.4 Knowledge Generation
Knowledge generation uses information technology to
augment pulling information from the clinicians’ under-
standing of the medical literature. The daily activities of
patient care generate new information about individual
patients and entire populations, but the sheer quantity of
data is overwhelming. Once data has been digitized, IT
systems can synthesize even massive amounts of infor-
mation into usable insight through two key routes: data
analysis and visualization.
Other industries rely on data analysis and data min-
ing as a significant source of insight. In healthcare,
where an operating margin of 2–4% is considered ex-
ceptional, many institutions have implemented some
level of financial data analysis. With respect to clinical
data, however, the lack of digitized information has hin-
dered the use of data analysis to generate insight about
clinical practices outside the academic research setting.
Data analysis can enable clinicians to make in-
quiries about the efficacy of daily practice in the same
waythat knowledge canbe derivedfrom controlled clin-
ical trials. A review of data at the population level can
reveal patterns that are not observed in isolation. In this
way the process of managing patients leads to greater
insight about the best way to manage those patients
going forward.
For example, it is widely recognized that induc-
ing labor before the 39th week of pregnancy can have
deleterious effects that compromise the health of the
newborn, yet early inductions still occur with relatively
high frequency. In a one-on-one interaction between pa-
tient and physician, it is easy to find reasons to induce
this patient’s labor early: late stages of pregnancy are
increasingly uncomfortable for the woman, the doctor
will be out of town, or other calendar issues come into
play. With each individualdecision, neitherprovider nor
patient is looking at the bigger picture.
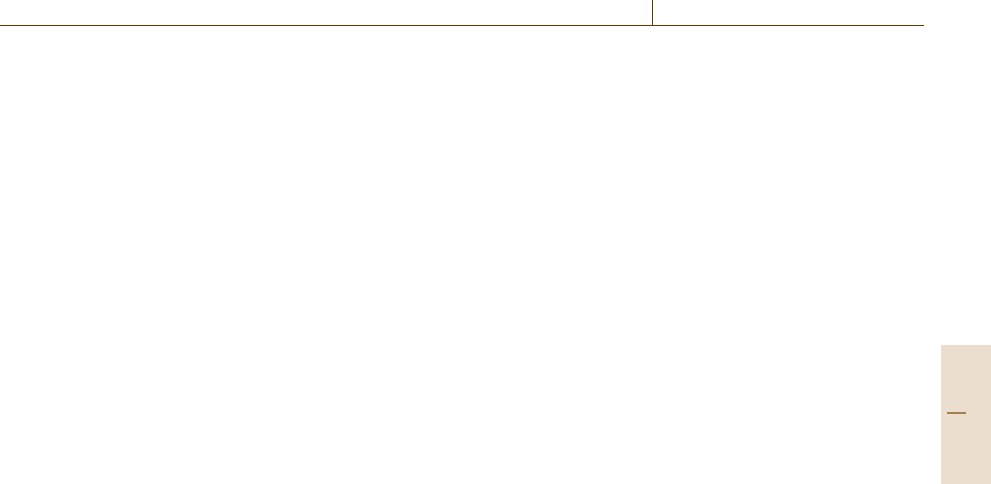
At Intermountain Healthcare, an integrated delivery
network headquartered in Salt Lake City, data analysis
of almost 40000 delivers deliveries in 2000–2001 re-
vealed an increased rate of neonatal intensive care unit
(NICU) admission for babies induced before week 39
(Fig.77.5). The research revealed a one to two weeks
delay could have avoided as many as 220 NICU ad-
missions. Once this data was available, the institution
developed and implemented an evidence-based triage
protocol that set a higher threshold for elective induc-
tions. The rate of early elective inductions dropped
to 5%, significantly reducing unnecessary NICU ad-
missions. Thus, the generation of knowledge through
population data analysis also led to insight that moti-
vated providers to change their practice.
Looking for trends also enables institutions to
improve management of patient care. Ideally, these
insights will extend beyond clinical knowledge to en-
compass the process of care. Electronic medical records
enable institutions to capture information about cost,
clinical data resource utilization, and process times. Us-
ing this information, they can begin to understand the
consequences of practice patterns and resource alloca-
tions, and assess the value of the care they deliver. As
institutions often focus on cutting costs without know-
ing the impact on quality, the analysis can demonstrate
ways to provide the right kind of care while actually
driving down per capita cost. Many examples exist
where institutions deliver the highest quality of care
with the lowest per capita rates, as consists of com-
plicated processes, resource allocations and practice
patterns with multi-fauceted practice patterns attribute.
This analysis will become essential as more third-party
payers adopt pay-for-performance programs that base
reimbursement on quality rather than quantity of care.
With paper records, physicians write summaries that
effectively filter out much of the granular information
about a patient’s condition. Other information may be
stored in archives, or simply filed in some other part of
the healthcare organization where they cannot be im-
mediately accessed. One of the paradoxes of digitizing
information is that the amount of accessible informa-
tion quickly becomes so overwhelming that clinicians
can no longer sift through all of it to find the relevant
information they need.
Data analysis can also be used to help providers
synthesize the vast amounts of information that are
Part H 77.2
1386 Part H Automation in Medical and Healthcare Systems
37th week
(4055)
5.3
Admitted to NICU (%)
Gestational age
15
10
5
0
Sep-00
Nov-00
Jan-01
Mar-01
May-01
Jul-01
Sep-01
Nov-01
Jan-02
Mar-02
May-02
Jul-02
Sep-02
Oct-02
Dec-02
Feb-03
Apr-03
Jun-03
Aug-03
Oct-03
Dec-03
Feb-04
Apr-04
Jun-04
Aug-04
Oct-04
Effective inductions < 39 weeks (%)
30
25
20
15
10
5
0
38th week
(10111)
3
39th week
(15341)
2.1
40th week
(8191)
2.6
41th week
(1842)
2.9
42th week
7.3
Fig. 77.5 Results of study by Intermountain Healthcare
that analyzed almost 40 000 deliveries in 2000–2001 to
reveal an increased rate of NICU admission of babies in-
duced before week 39
available about a single patient. For a patient with mul-
tiple chronic diseases, a clinician needs to understand
the interplay of a variety of different test results and
how individual tests vary over time. Visualization tech-
niques can facilitate a clinician’s evaluation of a patient
by supporting the cognitive tasks necessary for making
judgments patient about the patient’s care. An infor-
mation system that automatically collects the relevant
information and presents it in an easy-to-read format
can significantly facilitate a clinician’s evaluation of
a patient. With such an IT system in place, the clini-
cian can work systematically from problem to problem,
rapidly focusing on the next steps and how they in-
teract. The presentation can be further augmented by
embedding relevant contextual information for any task
the clinician is handling. For example, if a provider is
ordering antibiotics thesystem would automaticallydis-
play allergies, drug interactions, previously prescribed
antibiotics, and bacterial sensitivities.
The most effective clinical information systems can
intelligently sift through vast amounts of data, identify
pertinent patient information, and synchronize seam-
lessly to a provider’s. In this setting, visualization
includes the ability to organize data based upon the
patient’s condition and determines what is and is not
relevant.
Knowledge generating systems make it easy for
physicians to focus on the pertinent positive (abnormal)
findings and the pertinent negative findings (normal re-
sults that reduce the likelihood of a specific diagnosis).
In the case of chest pain, pertinent positive findings in-
clude high cholesterol, sudden onset of pain, smoking,
and family history of coronary artery disease – all of
which suggest that the patient is at risk for a heart at-
tack. On the other hand, if the patient is relativelyyoung
with no family history of the disease, has normal lab
tests, electrocardiogram (ECG) and other vital signs,
and had similar normal findings on a recent emergency
department admission for similar pain, the physician
may conclude that coronary artery disease is an unlikely
cause.
A system without knowledge representation can
perform only limited visualization, such as simple
graphing of trends, data grids, and composite displays;
without insight into the meaning and structure of the
data there is little intelligent work that can be performed
by the computer. With knowledge representation, the IT
system can determine how the available data relates to
a patient’s active problems and then organize the entire
record to minimize the time it takes to review, increas-
ing the likelihood that the provider sees and processes
the most relevant information.
Advanced visualization algorithms can be used to
look at data in new ways. Heat maps, cluster analy-
sis, multivariate indexes such as severity scores, and
patient health dashboards all represent potential means
for presenting complicated data using simplified vi-
sual metaphors. Heat maps create color-coded views of
the patient record highlighting the most active or high-
risk areas requiring attention. Cluster analysis is used
to graphically represent the similarity between one pa-
tient and similar patients in a population. It has been
used successfully to predict patients who may be more
likely to respond to certain cancer therapies based on
the expression of different genes associated witha given
type of cancer [77.8]. Other experimental approaches
have been used to predict based on numerous factors,
which patients are more likely to develop Alzheimer
disease [77.9]. Cluster analysis is particularly useful be-
cause it enables clinicians to rapidly see associations
Part H 77.2
Automation in Hospitals and Healthcare 77.2 The Role of Medical Informatics 1387
among different factors even if the underlying scientific
principles are unknown.
Multivariate indexes, such as severity scores, com-
bine different observations about a patient into a single
score. The human mind is limited in the number of
variables it can process simultaneously by collapsing
numerous variables into a single score can make it eas-
ier for clinicians to see trends that may otherwise be
hidden in complex relationships. For example, sever-
ity scores can help clinicians identify at an earlier stage
which patients are at greatest risk for worsening illness
allowing them to intervene earlier and potentially pre-
vent the worst effects of the disease [77.10]. Patient
dashboards can be used to combine patient-specific data
and severity scores to create a prioritized list of patients,
so that the provider can quickly identify which patients
are most in need of attention. One sign of well-designed
visualization systems is that significantly fewer obtru-
sive alerts are required to avert provider mistakes; when
the data is clearly presented, users are more likely to
make the right choices the first time.
Unfortunately there are very few examples of
widely adopted systems with detailed knowledge rep-
resentation, so many of these visualization techniques
remain in their infancy.
77.2.5 Knowledge in Action
The next level of knowledge management is to take the
knowledge that has been accumulated – from medical
research, from a patient’s chart, and from data analy-
sis and visualization – and put it to work at the point
of care. Too much of the knowledge that exists today is
inaccessible to clinicians when and where they need it.
IT will build the bridge that enables us to incorporate
the extensive knowledge base into the daily activities
of patient care, resulting in a consistently high standard
of care both within and across healthcare organizations,
with fewer inappropriate variations yet still tailored
to the needs of the individual patient. When knowl-
edge is embedded into clinical workflow, clinicians are
much more likely to actually use the information than
they are to consult a static display in a book or on
a web site.
In addition to improving care of individual patients,
knowledge in action is also a keystone of continuous
quality improvement (CQI) efforts, such as the appli-
cation of Lean manufacturing principles to healthcare.
IT enables the analysis of institution-wide data to break
down processes into their constituent parts and identify
steps that do not add value to the encounter.
The translation of knowledge into action includes
digitizing informationinto a readily searchableform us-
ing knowledge representation; converting digitized data
into an electronic workflow; and organizing and updat-
ing the knowledge database once it has been created.
An institution should also rely on its IT infrastructure to
provide support reviewing outcomes measures and ef-
fectively prioritize implementation of its thousands of
evidence-based guidelines.
Knowledgeinto action can not only help institutions
apply existing evidence to the delivery of patient care,
but it also enable organizations to localize the practice
of evidence based on various populations. The insights
thus gleaned can be fed back into the system to further
refine and improve the care being provided. The Pacific
Northwest, for example, has a higher incidence of mul-
tiple sclerosis than anywhere else in the US – so when
patients present with weakness or back pain, providers
there should consider ordering an magnetic resonance
imaging (MRI) sooner than they might elsewhere. This
localization caneven be applied to an individualpatient:
a person known to have a gene that predisposes him
or her to a particular disease (such as breast or colon
cancer) should be treated more aggressively than the
general population when potential symptoms are seen.
Rather than relying on a clinician to remember and ap-
ply all of these minute variations without assistance,
institutions can applyexpertrules within theirelectronic
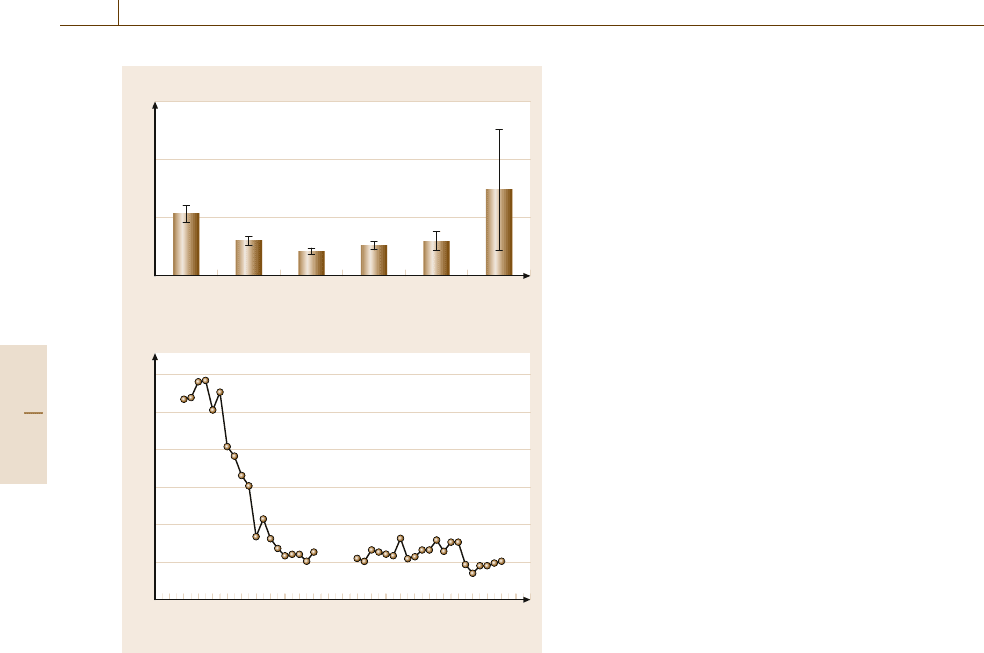
Fig. 77.6 A medical reporting tool. Technology sys-
tems like the Medical Quality Improvement Consortium
(MQIC) can be used to drive continuous quality of care
improvement by capturing current levels of quality. Using
encounter forms and decision support rules, clinicians can
then alter the effect of the care process and monitor the
result of the intervention
Part H 77.2
1388 Part H Automation in Medical and Healthcare Systems
medical record systems that will automatically present
clinicians with evidence that is most relevant to a par-
ticular patient.
One way to bring knowledge into action is through
decision support systems; of these, the most commonly
used are alert engines. These engines display messages
to users in a variety of situations, including:
•
A potentially hazardous situation, such as when
a clinician is about to order a medication to which
the patient is allergic
•
A condition that requires action, such as the receipt
of abnormal lab results
•
Missing data, such as failure to complete a list of
known allergies
•
A gap in care, such as overdue diagnostic tests rec-
ommended for preventive care of a chronically ill
patient.
Alerts are intended to be helpful, highlighting simple
issues that are easy for clinicians to overlook given the
busy nature of healthcare. The challenge is to establish
the right level of alerts. For example, the adverse ef-
fects of a drugallergy or aspecific drug/drug interaction
can have different degrees of severity depending on the
patient’s overall condition. The system would have to
determine when an alert is appropriate for a specific pa-
tient, and many systems err on the side of showing too
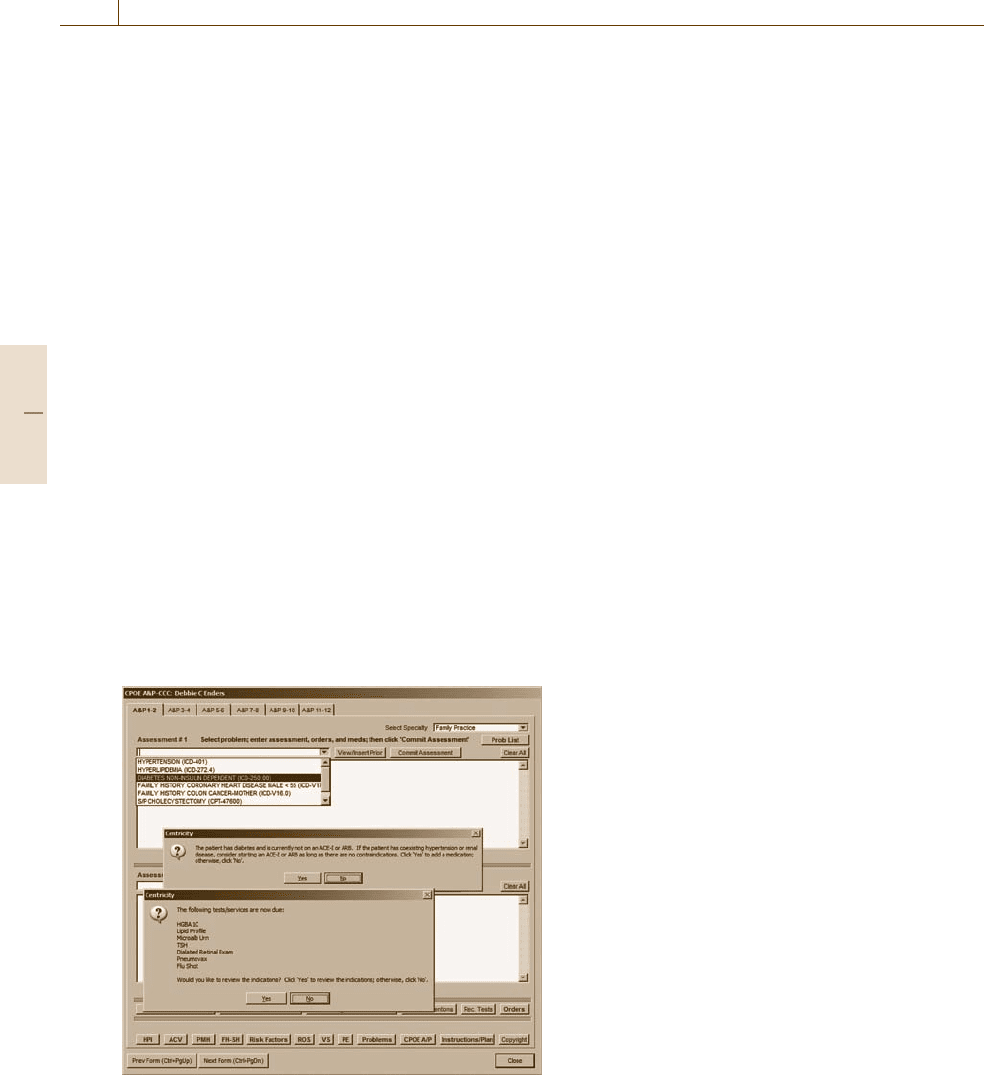
Fig. 77.7 Example of CPOE and clinical decision support.
In this example, a physicianhas beenalerted to elements of
a diabetic patient’s record, including medication manage-
ment, allergy questions, and whether to document insight
gathered from the alert
many alerts. Unfortunately, there is a threshold above
which users experience alert fatigue and begin to ig-
nore alerts – essentially rendering the alerting system
useless. In fact, some institutions turn off alerts in their
electronic medical record systems because they appear
to increase liability (if a clinician ignores an alert) with-
out changing practice.
To overcome these problems, next generation alert-
ing systems will need to have greater granularity in
how they define what triggers an alert, taking into ac-
count both the patient’s condition and the identity of
the provider. A patient with kidney disease will always
have some lab results that are outside the normal range
for the general population, but that reflect the normal
(i.e., stable) state for that individual. Similarly, alerts
regarding the management of a patient’s diabetes will
be relevant to the patient’s primary care provider, but
not to an orthopedist who is seeing the patient for an
unrelated condition.
An even more effective method of reducing alert fa-
tigue is to initially present information in a way that
reduces the likelihood of triggering an alert in the first
place. In fact, one may argue that alerts – especially
those that interrupt workflow – represent a system de-
fect. A well-designed system should instead ensure that
users do the right things rather than relying on alerts to
correct errors, and it can do this in large part by how
it displays patient data in conjunction with embedded
reference information.
In other words, a system should not need to alert
a clinician that the drug just prescribed is one to which
the patientis allergic. Instead,the listof patient allergies
should be displayed and highlighted before the clinician
even starts the medication order. An intelligent patient
summary screen would display a list of expected diag-
nostic tests based on a patient’s known problems; this
list would include the most recent results of all tests
that have already been performed, indicate which ones
need tobe repeated,and prepare(pending theclinician’s
approval) orders for tests that have not been done. In
a single glance, the clinician can easily determine the
status of the patient and the appropriate next steps that
are required.
Decision support systems are capable of more than
simple alerts. Newer decision support systems translate
existing best practice guidelines into adequately explicit
digital protocols that can be incorporated into a clinical
information system to help track and guide care.
While guidelines are common in medicine, the
terms they use are often too ambiguously defined to
be adequately represented in logic that can be enforced
Part H 77.2

Automation in Hospitals and Healthcare 77.3 Applications 1389
by a computer. A clinician will likely understand what
a guideline means if it suggests changing a medication
if a patient has not responded within a reasonable time.
In contrast, an adequately explicit version of the same
protocol would specify that if a patient’s blood pressure
has not dropped below 120/80 following administra-
tion of a maximum daily dose of 200 mg of Metoprolol
for 1 month, or if the patient’s heart rate has dropped
below 50, then the patient should be given a calcium
channel blocker.
In order to incorporate knowledge in action, there is
a significant amount of work to be done to adequately
define protocols and intelligent alerting systems. Ex-
isting guidelines tend to be written rather generically,
and need to be tailored to the specific needs of clin-
icians at a particular location. To date, much of this
work has been done by a small number of healthcare
organizations, organizations, using commercially avail-
able systems as a starting point. Because of inconsistent
terminologies and the lack of interoperability among
systems, however, another – thus, reducing or elimi-
nating the potential for synergies that could accelerate
advancement of the technology, does not easily reuse
work done at one institution. There have been a number
of attempts to create knowledge representations for pro-
tocols and alerts that could move across systems, but,
to date, none have been successfully and consistently
adopted.
Adequately explicit protocols give rise to a dia-
log over time between the provider and the computer
system that jointly determines the next appropriate in-
terventionfor care. Thefact that aprotocol isadequately
explicit, however, does not replace the need for a de-
termination to be made as to whether the protocol is
appropriate for a specific patient. A patient with kidney
failure will have changes in drug metabolism such that
some protocols should never be administered. Or a pa-
tient who starts on a particular protocol may experience
changes that make the protocol no longer appropriate.
In other words, a protocol is a method to ensure con-
sistency of care but it does not eliminate the need for
careful observation and judgment.
77.3 Applications
Existing health IT systems can be organized by func-
tions they perform and the locationswhere they perform
them. The basic functions fall into five healthcare-
separate categories: patient access, healthcare billing,
healthcare administration,clinical care, and patient con-
nectivity; a subset of these functions is then tailored
to the specific needs of a given care location. Finally
interoperability represents the functionality required to
share information across the boundaries of healthcare.
(There are a number of other core IT functions, such
as ERP or customer relationship management (CRM)
modules, which are applicable to any business and have
been adapted to healthcare, which will not be reviewed
here). Although this discussion begins with a separate
review of each function, the true power of health IT is
recognized only in enterprise systems that tie all these
functions together.
77.3.1 Patient Access
Patient access systems manage how a patient interacts
with the healthcare system; they can be further bro-
ken down into scheduling and location management.
Healthcare scheduling is complex and is key to the ef-
ficient operation of a healthcare system. The simplest
scheduling systems focus on finding a time slot for
a patient to be seen by a specific doctor in a specific
clinic. They may also take into account the level of re-
sources or services available at different times of day to
help balance the caseload. At the other end of the spec-
trum are enterprise scheduling systems, which are used
to help orchestrate the delivery of care across multiple
locations. For patients with complex conditions, these
systems ensure that appointments are scheduled in the
appropriate sequence and that a patient is not scheduled
to be in two different locations at the same time.
Location management functions, commonly re-
ferred to as patient administration message (ADT)or
admission/transfer/discharge, include tracking the loca-
tions of the patient in the hospital and storing basic
demographic information about the patient. For inpa-
tient care, the digital management of patient location is
crucial to the appropriate provision of services (know-
ing which patient in which room is to be taken for a CT
scan, for example) as well as for accurate billing.
77.3.2 Healthcare Billing
Healthcare billing systems focus on generating charges
based upon services delivered and supplies consumed,
Part H 77.3
1390 Part H Automation in Medical and Healthcare Systems
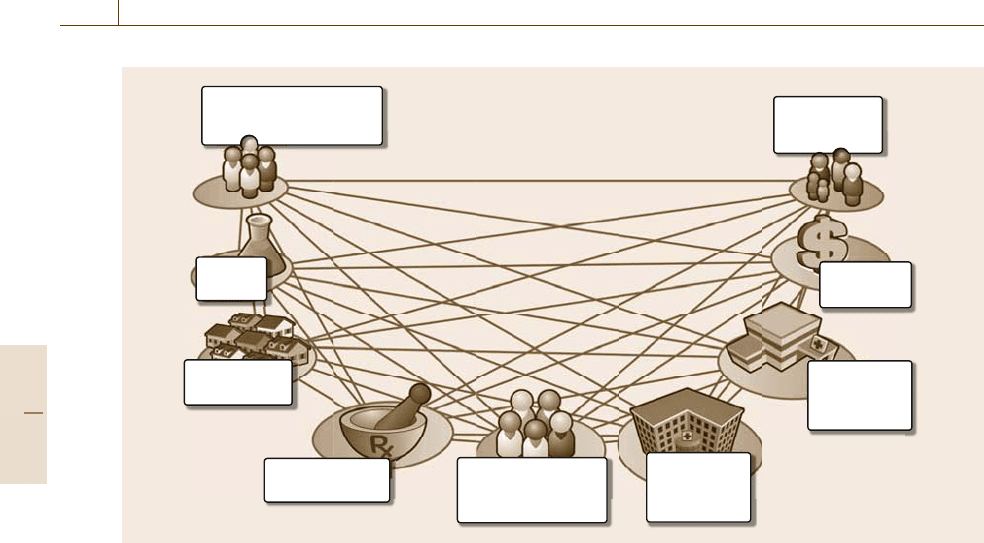
Fig. 77.8 By establishing a single electronic connection
to over 1000 payers, this healthcare application simplifies
and automates eligibility checking and claims process-
ing to help drive more efficient workflows and accelerate
reimbursement
and then presenting invoices to those responsible for
payment (whether patient, insurance company, or some
other third party). Both the capture of charges and the
billing process itself are fairly complicated in medicine.
Charges comprise both professional service fees
(incurred when a clinician performs a service for the pa-
tient) and institutional/facility fees (based on the cost of
resources consumed and the procedures performed by
the institution’s staff).
Professional service fees are codified by type and
complexity of the service provided, from a simple clinic
Fig. 77.9 Sophisticated billing solutions will include task
management, claims processing, and tools to automate in-
teractions across the healthcare systems
visit to open-heart surgery. Most IT systems capture
these charges by having doctors select specific billing
codes from a defined list.Significant training is required
for physicians to bill appropriately and legally. More
advanced IT systems provide some decision support
that reviews the doctor’s clinical documentation to help
determine the appropriate level of billing for a given
service.
For inpatient care, however, hospitals are not neces-
sarily reimbursed based upon the actual care delivered.
Instead there are DRGs (diagnostic related groups) that
typically specify reimbursement levels for specific dis-
eases or procedures; it is left up to the hospital to
manage cost so as to maintain profitability. As a re-
sult, billing systems need both cost accounting and bill
management to adequately address the address the rev-
enue cycle. Cost accounting allows institutions to track
the cost of performing basic operations and specific
care actions. Cost accounting is crucial for an institu-
tion to understand its cost structure and optimize its
productivity. Billing and revenue tracking are further
complicated because reimbursement often comes from
multiple sources: government (Medicare/Medicaid) and
insurance companies, as well as patients.
Patient billing systems focus on submitting charges
to third-party payers in such a way as to minimize rejec-
tions and shorten time to reimbursement. Increasingly,
both insurance companies and government payers typi-
cally require additionalclinical documentationto justify
the charges – increasing the demand for integration be-
tween financial and clinical systems.
Patients are responsible for all charges not reim-
bursed by either insurance or government payers. Often
there are multiple third-party payers involved, increas-
ing the complexity of billing and making the whole
process overwhelming for a patient who is also dealing
with a significant illness and looming large medical ex-
penses. A billing system that can streamline the process
and simplify the experience will have a positive impact
on patient satisfaction with the provider.
77.3.3 Healthcare Administration
Healthcare administration systems focus on the busi-
ness intelligence to understand the operations of the
healthcare system. These include financial dashboards
and reports, which show the financial operations of the
hospital, patient census and bed management, and re-
source management such as nurse staffing and order
communications (the systems that communicate order
requests within a hospital). These systems pull informa-
Part H 77.3
Automation in Hospitals and Healthcare 77.3 Applications 1391
tion from multiple sources to generate comprehensive
views of the healthcare system.
Redundant or inefficient processes can take their
toll on an organization’s bottom line. Healthcare ad-
ministration systems can help identify these processes,
enabling organizations to streamline their operations,
improving both profitability and patient and provider
satisfaction. Increasingly, healthcare administration
systems have become more dependent on clinical care.
As a result, these systems are becoming more closely
tied and potentially integrated with clinical systems.
One significant challenge for these systems is to get
clarity into details of the healthcare process especially
at the point of care. Often the point of care is the least
digitized and yet has the most significant impact on op-
erations. As the point of care becomes more digitized,
it will be easier to understand the healthcare delivery
system in detail. This will create new opportunities to
understand how cost, decision-making, and workflow
affectthe bottom line ofoperations. With greaterinsight
new rules can be built into the point of care through
standard operating procedures, workflow management,
and decision support.
77.3.4 Clinical Care
The earliest clinical systems to be adopted were ded-
icated to reviewing patients’ test results. Before the
advent of these systems, clinicians had to consult mul-
tiple sources to get the results of laboratory tests,
electrocardiograms, x-rays, and pathology reports for
a single patient. Typically the results were available to
only a few people at a time – so that different members
of the care team could not access them simultaneously
– and often the location where the results were stored
was not where the clinician was. Results-viewing appli-
cations can aggregate data from multiple sources and
allow clinicians to access the information from any-
where and at any time, so that the entire care team can
have simultaneous access to a comprehensive view of
the patient’s status.
Another area where there has been significant adop-
tion of IT is diagnostic test systems, which accelerate
the process of performing the tests and manage distribu-
tion of the results. Most hospitals now have laboratory
information systems to manage workflow, task manage-
ment, and aggregation of data for all the tests performed
in the laboratory. Likewise, picture archiving and com-
munications systems (PACS), which are used to capture
digital radiology and cardiology images from imag-
ing hardware such as digital x-rays, CT scanners, and
MRI scanners, are present at most hospitals and in-
creasingly at outpatient imaging centers. Radiologists
use PACS to view and interpret images and provide
diagnostic reports. PACS systems have eliminated the
need for large (and expensive) film storage rooms; they
have also given rise to teleradiology, where radiologists
can view and interpret images remotely. This creates
new possibilities for business models in which aca-
demic institutions can provide advanced services for
rural hospitals that may not be able to attract and sustain
specialized radiologists.
While these types of systems have been widely
adopted, they are often disconnected from the core
workflow of patient management and therefore pro-
vide little opportunity for the application of knowledge
in action. The greatest impact on improving the qual-
ity of patient care comes from clinical documentation
and computerized provider order entry (CPOE); unfor-
tunately, adoption rates for both of these functions are
less than 20% (Fig.77.10).
Orders comprise all the directions that physicians
prescribe for the management of a patient based on all
the knowledge available about that patient at a certain
point in time. Thus the amount of knowledge available
to the clinician at the time of order entry will have a sig-
nificant impact on the quality of care. CPOE not only
ensures that an order is legible and consistently commu-
nicated; it also presents the opportunity to opportunity
to use decision support to validate the appropriateness
of the order prior to it being carried out. Additionally,
CPOE allows the creation of sets of orders which can
be managed as a group to ensure a given disease is man-
aged consistently. A hospital can create a standard order
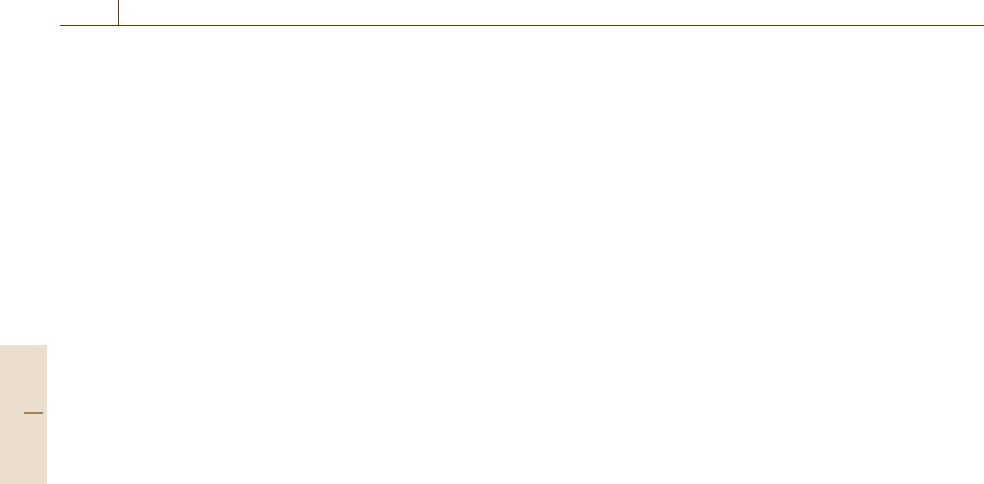
Physiologic
monitoring
Diagnostic
results
Documented
observations
Provider worklists
Physical exam Patient historyHospital course
DiagnosticsTreatments Care team actions
CPOE:
Transforming information into action
Patient response
Fig. 77.10 Example of the cycle of care with the use of clinical
documentation and CPOE
Part H 77.3
1392 Part H Automation in Medical and Healthcare Systems
set for heart attack patients and then rather than having
to remember each specific order, the physician can then
focus on changingor adding orders needed to tailor care
to the individual patient.
Order quality and order consistency were key
drivers for a recommendation by The Leapfrog Group
(a consortium of large employers concerned with
improving the safety, quality, and affordability of
healthcare) to recommend that CPOE should be widely
adopted [77.11]. The centrality of order entry to work-
flow has made it difficult, however, to design CPOE
systems that were not perceived to slow down the or-
dering process. In fact, while CPOE may create extra
steps for the physician at the time of ordering, this is
much less than the time required to correct illegible
handwritten orders or address complications that arise
from preventable adverse drug reactions. The problem
is that the physician does not directly experience the
time-saving impact of the workload.
It is only in the past few years, as organizations
have recognized the role of change management in the
success of CPOE, that adoption of these systems has
started to accelerate. One of the key success factors
has been to implement enough facets of the IT sys-
tem to demonstrate value beyond CPOE. Physicians are
more likely to adopt CPOE if at the same time they can
benefit from information access, data visualization and
decision support. Conversely, if CPOE is the only func-
tion implemented, so that workflows are split between
digital and analog systems, creating unnecessary inter-
ruptions in workflow, clinicians will be less likely to
embrace the technology.
Another key portion of a clinician’s workflow is
the documentation process. Healthcare documentation
serves four key purposes:
1. It creates a legal medical record describing both the
reasoning and activities involved a specific patient’s
care.
2. It provides a basis for outcomes analysis, population
management, and reporting.
3. It communicates one care team member’s actions
and reasoning to other members of the care team,
enabling better collaboration and coordination of
care.
4. It assists clinicians to organize their thoughts and
plan their actions.
Thus, good documentation systems are more than
just sophisticated word processors. Rather, these sys-
tems are important for legal accountability, retrospec-
tive data analysis, and data mining, as well as for
orchestrating and coordinating the ongoing work of the
entire care team.
Interdisciplinary documentation, integration of de-
cision support, and integration of key workflow tasks
all contribute to extending the value of these systems.
It is rare that one provider is responsible for all of
the information necessary to manage a single patient.
Interdisciplinary documentation allows providers from
different specialties and disciplines to contribute to the
medical record in an orchestrated fashion, collaborating
on shared documents and leveraging documents created
by others. Each provider can see the work performed
by others and integrate other providers’ observations
into their own work. The hospital physician who sees
a patient once per day relies on the information from
hundreds of encounters by nurses, dieticians, physical
therapists, and social workers to write one note that sets
the direction for the next day of patient care. Similarly,
a case manager will integrate the work of the entire care
team and synchronize the nursing, physician, patient,
and discharge goals all based on the shared documen-
tation of the team.
The more powerful documentation systems com-
bine task and worklist management features to tie the
work of documentation into the details of patient care.
Because documentation is such a consistent part of
healthcare delivery, incorporation of worklists into the
documentation process tends to increase the consistency
of care delivery.
Providers often use documentation as an important
part of their cognitive process, using it to help orga-
nize the information available and form their plan of
action. The basic structure of a progress note taught
to all physicians is called SOAP, which stands for
subjective, objective, assessment, and plan. Thus, the
inherent structure of the note is designed to aggregate
current knowledge about a patient, assess the patient
and then determine the plan of care. Most documen-
tation notes follow a similar structure. Preserving this
cognitive value of documentations is one of the hard-
est problems to solve in digitizing the documentation
process.
Because, as with CPOE, so much reasoning oc-
curs during the process of writing notes, documentation
is another key target for decision support systems.
Decision support can both initiate the documentation
process and occur within the documentation process
itself. Decision support initiated documentation fo-
cuses on dynamically manage managing the task or
action that should occur next. Documentation also be-
Part H 77.3
Automation in Hospitals and Healthcare 77.3 Applications 1393
comes the final step and forcing function to make
sure that a process actually occurs. During docu-
mentation, decision support is used to automatically
aggregate information that should be included in the
note and prompt for actions that should be considered
within the care plan. Documentation links task manage-
ment, results review, care planning, decision support,
and order entry all into a single workflow. The best
documentation systems are built to leverage and dy-
namically interact with all of these functions within the
EMR.
One of the next important trends in clinical applica-
tions is near device decision support. Medical devices
are sprinkled across the healthcare system. There are
advanced physiologic monitors and ventilators in the
intensive care unit, anesthesia machines in the operat-
ing room, ECG machines in the emergency department,
blood pressure cuffs and intravenous infusion pumps al-
most everywhere, and new devices entering the home –
just to name a few. These devices each have their own
innovations and manufacturers seek to find unique and
innovative ways to differentiate their products. As a re-
sult these manufacturers have targeted ways to make
these devices ubiquitous indispensable parts of the care
process. Extending the hardware platform at the core
of these devices with new software applications that
aid in the care process has become increasingly com-
mon. Many of these applications can be considered
near device decision support, as the decision supporting
characteristics are managed by the device rather than
with a clinical information system. For example many
new infusion pumps include the ability to check dose
ranges and verify the barcode of medications before
they are administered. In fact, some of these pumps will
connect to pharmacy information systems to allow the
pharmacist to directly program the pumps wirelessly.
Even more advanced applications are starting to ap-
pear such as ventilators that have embedded weaning
protocols that help guide the process of discontinuing
the use of mechanical ventilation in critically ill pa-
tients. (Ventilatorsare machinesthat breathe for patients
when they are too sick to breath for themselves. One of
the challenges of using a ventilator is helping a patient
gain the strength to breathe independently of the ma-
chine as they begin to improve. This process is called
weaning.) There are numerous applications where soft-
ware combined with medical devices will help manage
complicated and specific care processes. In this space
the line between devices and software will begin to
blur.
77.3.5 Patient Connectivity
In a given year most people may see their doctor at most
1h and even patientswith allbut the most severedisease
spend most of their time living their lives independent
of the healthcare system. As a result most of the deci-
sions that affect the health of a person are made during
the activities of daily life. Choices about diet, exercise,
medication compliance, sleep habits, and stress levels
all contribute significantly to the real health outcomes
that face society. If we are to truly improve the health
of a population then we must enable the healthcare sys-
tem to reach beyond the boundaries of its wall directly
into the lives of patients. Essentially, the patient be-
comes the central memberof the care team and effective
collaboration becomes key.
With the advent of increased penetration of the In-
ternet into the average family household and increased
trends toward patient financial responsibility for health-
care due to employers passing the increase costs of
healthcare on to their employees, the patient’s role in
the IT system has begun to expand.
The most common and demanded IT functions are
around managing the patient’s access and finances with
an institution. Many systems are beginning to allow
patients to request appointments online and allow pa-
tients to review their complicated billing histories and
make payments. Thesefeatures keep healthcare systems
on par with other industries and increase the customer
satisfaction of interacting with the healthcare system.
Additionally, since these portals receive a fair amount
of traffic healthcare, institutions use these portals to pro-
vide marketing and relevant institutional information to
patients and prospective patients. This is particularly
important inurban areaswhere healthcaresystems com-
pete for market share.
Although these finance and access features drive
a great deal of consumer satisfaction they have limited
impact on the health of a patient. Recently, EMR ven-
dors and dedicated patient portal vendors have begun
providing clinically oriented applications. The simplest
forms of this application allow patients access to por-
tions of their medical record – such as labs and results –
and allow secure communication with between the pa-
tient and the physician. These e-Visits have recently
begun to be reimbursed by payers as they are becom-
ing more effective and reducing unnecessary and more
expensive office visits.
More advanced versions of these applications in-
clude true disease management applications, which
Part H 77.3
1394 Part H Automation in Medical and Healthcare Systems
Primary care physicians
• Practice management
• EMR
Lab
• Results
Pharmacy/PBMs
• Rx history
Payers
• Claim data
Public health
• Registries
Speciality practice
• Practice management
• EMR
Patient
• Personal
health records
Hospital 2
• EMR/PMs
• Lab
• PACS archive
Hospital 1
• EMR/PMs
• Lab
• PACS archive
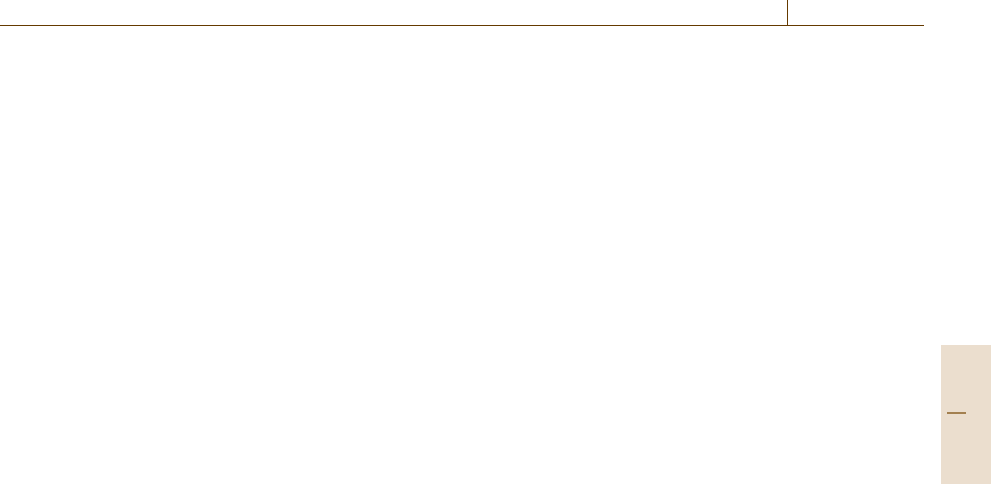
Fig. 77.11 Automation has a crucial role in how frequently a patient will interact with the healthcare system based on
complexity of the experience and how a patient will retrieve healthcare information beyond the episodes of care
allow physicians and/or care managers to interact with
populations of patients to manage specific diseases
such as diabetes, asthma, and congestive heart failure.
These application extend the clinical feature to include
registries of patients with key clinical information to
highlight which patients need help from the healthcare
system and provide tools to enable collaboration with
the patient on a shared plan of care for their diseases.
While these clinical applications tend to be pro-
vided by providers thereis another class ofwellness and
disease management applications that are provided by
insurers and employers. These applications share some
of the same features described above but also include
applications to inspire health behaviors in populations
in consumers. These programs have been shown to re-
duce the costs of healthcare for employers and reduce
the cost of managing populations for insurers.
Finally people are beginning to take more control
of their own healthcare records and there has been
an emergence of digital personal healthcare records
(PHRs). These personal healthcare records allow peo-
ple to record their key clinical information such as labs,
diet, exercise, medication lists, etc. Some PHRs can
connect to EMRs and directly share information be-
tween patients and providers. Some PHRs also include
wellness and disease management features to link the
patients personal data with activities that drive health
and wellness.Although PHRs offer opportunities to em-
power patients, increase sharing and collaboration, and
drive better healthbehaviors,their adoptionremains low
while commercial interest remains high.
77.3.6 Interoperability
Despite the successful digitization and automation of
the workflows within many global locations, most in-
formation is stored in silos and is unable to provide
maximum impact on patient care. Unfortunately, it’s
often at the same boundaries that prevents digital infor-
mation flow from improving quality and safety reside.
For example, when a patient is discharged from the hos-
pital it is most common that medication changes and
follow up plans are confused. It is also at discharge
when a new set of healthcare providers will manage the
patient and often these healthcare providers do not have
a mechanism for accessing the digital patient record
if it is present. Interoperability strategies seek to im-
prove this flow of information. Within the US there
are strategies to create regional health information or-
ganizations (RHIOs) that can manage the exchange of
critical information across these institutional bound-
aries. At a national level there are plans to develop
Part H 77.3
