Jan Lindhe. Clinical Periodontology
Подождите немного. Документ загружается.


594 - CHAPTER 27
Fig. 27-28. A 9-year-old boy showing recession at tooth 41. The tooth is rotated and buccally positioned (a). The
minimal amount of gingiva found apical to the recession shows pronounced signs of inflammation. The plaque con
-
trol in the region was improved but surgical intervention was postponed. (b) The same tooth area at the age of 14
years. Note the spontaneous soft tissue repair that has taken place at tooth 41 as a consequence of the improved
plaque control and the growth in the alveolar process.
Fig. 27-29. Spontaneous repair of soft tissue recessions following orthodontic tooth movement. A 22-year-old
woman showing recessions and thin marginal tissues at prominently positioned teeth, particularly 23, 33, 41 and 43
(a). Following proper alignment of the teeth (b), the recessions have spontaneously been resolved and an increased
gingival height can be noted.
periodontal tissue support at the proximal surfaces of
the tooth.
Recession defects in the child need particular atten-
tion. In the growing child, recession defects may be
eliminated spontaneously, provided an adequate
plaque control is established and maintained (Fig.
27-
28). Andelin-Sobocki et al. (1991) reported from a
3-
year prospective study that 25 out of 35 recessions
with an initial depth of 0.5-3.0 mm spontaneously
healed following improvement of the oral hygiene
standard. Furthermore, all but three of remaining re-
cessions showed a decrease and no site demonstrated
an increase in depth. Hence, reparative surgical treat-
ment of soft tissue recessions in the developing denti-
tion may not be necessary and should preferably be
postponed until the growth has been completed.
Furthermore, in an orthodontic case showing a re-
cession defect and a thin (delicate) gingiva due to
prominent position of the tooth (Fig. 27-29a), surgical
treatment for root coverage should be postponed until
the orthodontic therapy is completed. The recession, as
well as the dehiscence, will decrease as a conse
quence of the lingual movement of the tooth into a
more proper position within the alveolar bone (Fig.
27-
29b) and, if still indicated, the root coverage proce
dure
will show higher predictability if performed after
than
before the tooth movement.
Root coverage procedures
Surgical procedures used in the treatment of recession
defects may basically be classified as (1) pedicle soft
tissue graft procedures and (2) free soft tissue graft
procedures.
The pedicle graft procedures are, depending on the
direction of transfer, grouped as (1) rotational flap
procedures (e.g. laterally sliding flap, double papilla
flap, oblique rotated flap) or (2) advanced flap proce-
dures (e.g. coronally repositioned flap, semilunar
coronally repositioned flap). The latter procedures do
not include rotation or lateral movement of the pedicle
graft. Within the group of pedicle graft procedures,
guided tissue regeneration procedures may also be
596 • CHAPTER 27
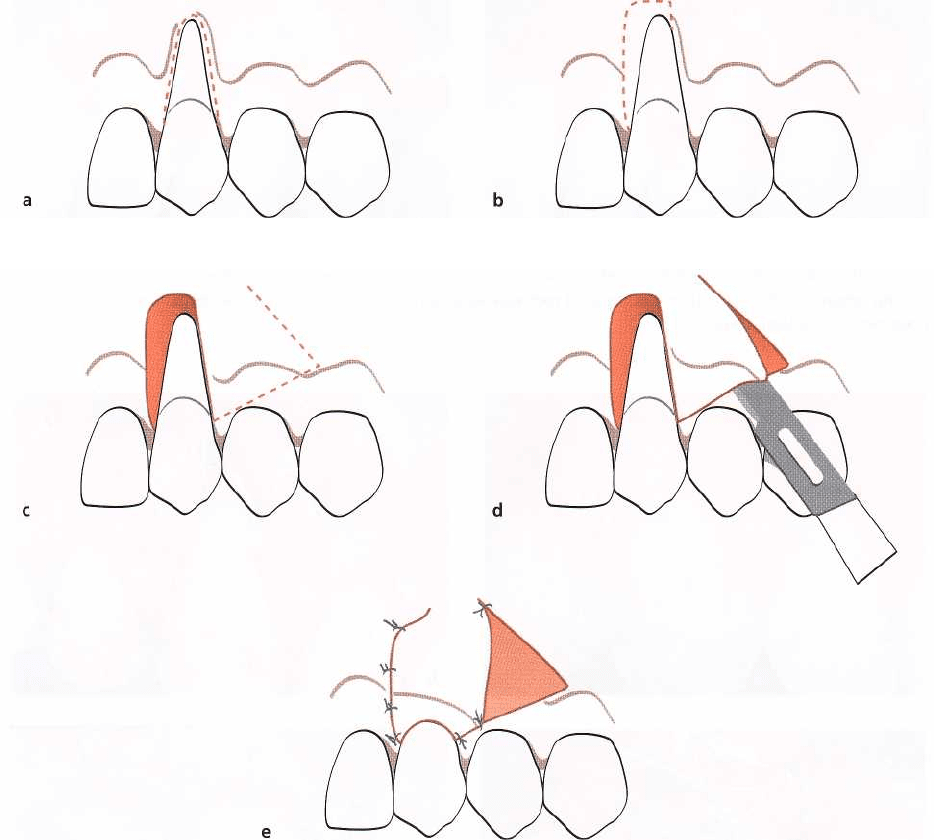
Fig. 27-32a-e.
Rotational flap procedure.
Schematic drawings illustrating the surgical technique in utilizing rotational
pedicle grafts to cover localized recession defects (see text for explanation).
depth between teeth that had been instrumented (root
planed) or polished only (Oles et al. 1985, Pini Prato
et al. 1999). Extensive root planing may therefore only
be performed in situations where a reduced root
prominence would be considered beneficial for graft
survival or tissue regeneration, or if a shallow root
caries lesion is diagnosed. The presence of a filling in
the root does not preclude the possibility for root
coverage (Fig. 27-30), but the filling should be re-
moved before the root is covered with soft tissue.
Miller (1985b) advocated the use of root surface
demineralization agents to be an important treatment
component in the free soft tissue graft procedure. In
addition to the removal of the smear layer, the use of
acid demineralization of the root surface is intended
to facilitate the formation of a new fibrous attachment
through exposure of collagen fibrils of the dentine
matrix and allow subsequent interdigitation of these
fibrils with those in the covering connective tissue.
However, controlled clinical trials comparing the ef-
fect of free gingival graft procedures with and without
root conditioning (Ibbott et al. 1985, Bertrand & Dun
-
lap 1988, Laney et al. 1992, Bouchard et al. 1997, Caf
fesse et al. 2000) have failed to demonstrate a benefi-
cial clinical effect from the use of acid root biomodifi-
cation. Also, controlled studies comparing the effect
of laterally positioned flap with and without root
conditioning showed no statistically significant posi-
tive effect of the use of acid root conditioning (Oles et
al. 1985, Caffesse et al. 1987). Gottlow et al. (1986)
evaluated the healing following treatment of localized
gingival recessions with coronally positioned flaps
and
citric acid root biomodification in a controlled
study in
dogs. The histological analysis after 3 months
of
healing disclosed no differences in the amount of
root
coverage or new connective tissue attachment
MUCOGINGIVAL THERAPY - PERIODONTAL PLASTIC SURGERY •
597
between citric acid treated sites and saline treated
control sites. Although root resorption was a common
finding among the citric acid treated teeth in this dog
model, such a finding has not been commonly re-
ported in humans. Hence, the literature clearly indi-
cates that the inclusion of root conditioning does not
improve the healing outcome of root coverage proce-
dures.
Pedicle soft tissue graft procedures
Rotational flap procedures
The use of a laterally repositioned flap to cover areas
with localized recession was introduced by Grupe &
Warren (1956). This technique, which was called
the
laterally sliding flap
operation, involved the reflection
of a full thickness flap in a donor area adjacent to the
defect and the subsequent lateral displacement of this
flap to cover the exposed root surface (Fig. 27-19). In
order to reduce the risk for recession on the donor
tooth, Grupe (1966) suggested that the marginal soft
tissue should not be included in the flap. Staffileno
(
1964) and Pfeifer & Heller (1971) advocated the use
of a split thickness flap to minimize the potential risk
for development of dehiscence at the donor tooth.
Other modifications of the procedure presented are
the
double papilla flap
(Fig. 27-31) (Cohen & Ross 1968),
the
oblique rotational flap
(Pennel et al. 1965),
the rotation flap
(Patur 1977), and
the transpositioned flap
(Bahat et al.
1990).
Technique
• The rotational flap procedure (Fig. 27-32) is initiated
with the preparation of the recipient site. A reverse
bevel incision is made all along the soft tissue mar-
gin of the defect (Fig. 27-32a). After removal of the
dissected pocket epithelium, the exposed root sur-
face is thoroughly curetted.
• At a distance of approximately 3 mm from the
wound edge which delineates the defect at the side
opposite the donor area, a superficial incision is
made extending from the gingival margin to a level
approximately 3 mm apical to the defect (Fig. 27-
32b). Another superficial incision is placed horizon
-
tally from this incision to the opposite wound edge.
The epithelium together with the outer portion of
the connective tissue within the area delineated by
these incisions and the wound edges is removed by
sharp dissection (Fig. 27-32c). In this way a 3-mm-
wide recipient bed is created at the one side of the
defect, as well as apically to the defect.
• A tissue flap to cover the recession is then dissected
in the adjacent donor area. The preparation of this
flap is initiated by a vertical superficial incision
placed parallel to the wound edge of the recession
and at a distance which exceeds the width of the
recipient bed and the exposed root surface of ap-
proximately 3 mm (Fig. 27-32c). This incision is
extended beyond the apical level of the recipient
bed and is terminated within the lining mucosa
with an oblique releasing incision directed towards
the recession site. An incision connecting the verti-
cal incision and the incision previously made
around the recession is placed approximately 3 mm
apical to the gingival margin of the donor site.
A split thickness flap is then prepared by sharp
dissection within the area delineated by these inci-
sions so that a layer of connective tissue is left
covering the bone in the donor area when the flap
is laterally displaced over the denuded root surface
(
Fig. 27-32d). It is important that the oblique releas
-
ing incision is made so far apically that the tissue
flap can be placed on the recipient bed without
being subjected to tearing forces when adjacent soft
tissues are moved. The prepared tissue flap is ro-
tated about 90° when sutured at the recipient bed
(
Fig. 27-32e).
The suturing of the flap should secure a close
adaptation of the pedicle graft to the underlying
recipient bed. Pressure is applied against the flap for
2-3 min in order to further secure a good adaptation.
To protect the surgical area during the initial phase
of healing, a periodontal dressing is applied. Alight
curing dressing material, e.g. Barricai
d
T
`" (Dentsply
International Inc., Milford, DE, US), is preferably
used since this can be applied without dislocating
the flap and has a favorable esthetic appearance.
Following removal of the dressing and the sutures,
usually after 10-14 days, the patient is instructed to
avoid mechanical toothcleaning for a further 2
weeks, but to use twice daily rinsing with a chlor-
hexidine solution as a means of plaque control.
Advanced flaps
Since the lining mucosa is elastic, a mucosal flap raised
beyond the mucogingival junction can be stretched in
coronal direction to cover exposed root surfaces (
Harvey 1965, Sumner 1969, Brustein 1979, Allen &
Miller 1989, Wennstr6m & Zucchelli 1996, Pino Prato
et al. 1999). The coronally advanced flap can be used
for root coverage of a single tooth as well as multiple
teeth, provided suitable donor tissue is available. In
situations with only shallow recession defects and
minimal probing pocket depth labially, the
"semilunar
598 • CHAPTER 27
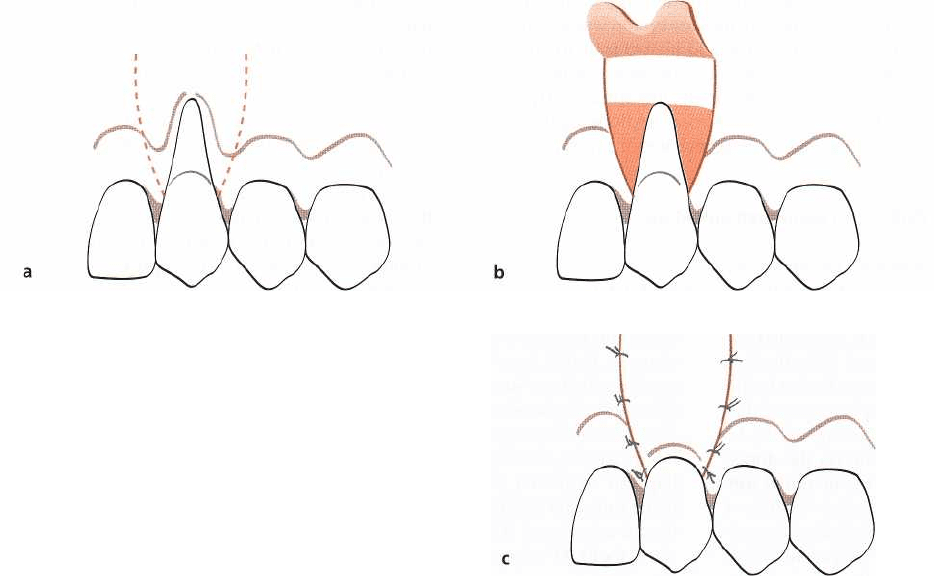
Fig. 27-33a-c.
Coronally advanced flap procedure.
Schematic drawings illustrating the surgical technique in utilizing
coronally advanced pedicle grafts to cover localized recession defects (see text for explanation).
coronally repositioned flap"
may offer an alternative
approach (Harlan 1907, Tarnow 1986).
Technique
Coronally advanced flap procedure (Fig. 27-33)
• The coronally advanced flap procedure is initiated
with the placement of two apically divergent verti-
cal releasing incisions, extending from a point coro
-
nal to the cemento-enamel junction at the mesial
and distal line axis of the tooth and apically into the
lining mucosa (Fig. 27-33a).
• A split thickness flap is prepared by sharp dissec-
tion mesial and distal to the recession and con-
nected with an intracrevicular incision. Apical to the
receded soft tissue margin on the facial aspect of the
tooth, a full thickness flap is elevated to maintain
maximal thickness of tissue flap to be used for root
coverage (Fig. 27-33b). Approximately 3 mm apical
to the bone dehiscence, a horizontal incision is made
through the periosteum, followed by a blunt dissec-
tion into the vestibular lining mucosa to release
muscle tension. The blunt dissection is extended
buccally and laterally to such an extent that the
mucosal graft can be easily positioned coronally at
the level of the cemento-enamel junction.
The tissue flap is coronally advanced, adjusted for
optimal fit to the prepared recipient bed, and se-
cured at the level of the cemento-enamel junction by
suturing the flap to the connective tissue bed in the
papilla regions (Fig. 27-33c). Additional lateral su-
tures are placed to carefully close the wound of the
releasing incisions. A light curing dressing may be
applied to protect the area during initial healing.
Fig. 27-34 illustrates the treatment of a recession defect
with the use of the coronally advanced flap procedure.

MUCOGINGIVAL THERAPY — PERIODONTAL PLASTIC SURGERY • 599
Fig. 27-34.
Coronally advanced flap procedure.
A deep and wide recession defect on a canine with a composite resin
restoration in the exposed root portion (a). Before preparation of the pedicle graft, the root is polished with pumice
and a rubber cup. A split flap has been dissected mesial and distal to the root, and a full thickness flap apical to the
recession (b). Approximately 4 mm apical to the bone dehiscence the periosteum has been cut and a blunt dissec-
tion performed to facilitate the coronal positioning of the pedicle graft. The composite resin restoration is removed
(c)
followed by a close suturing of the pedicle graft to cover the exposed root surface (d). Healing outcome 1-year
postoperatively (e).
600 • CHAPTER
27
Fig. 27-35a-c.
Semi-lunar coronally repositioned flap procedure.
Schematic drawings illustrating the surgical technique
in
utilizing coronally displaced pedicle grafts to cover shallow localized recession defects (see text for explanation).
Semi-lunar coronally repositioned flap procedure (Fig
27-35)
A semi-lunar incision is placed apically to the reces-
sion and at a distance from the soft tissue margin,
which should be approximately 3 mm greater than
the depth of the recession. The outline of the incision
should be parallel to the curvature of the gingival
margin (Fig. 27-35a). The incision is extended into
the papilla region on each side of the tooth, but care
should be taken to maintain a broad base of anchor
-
age to secure a collateral blood supply to the pedicle
graft.
A split thickness dissection of the facially located
tissue is then made by an intracrevicular incision
extending apically to the level of the semi-lunar
incision (Fig. 27-35b). The mid-facial soft tissue graft
is coronally repositioned to the level of the cemento-
enamel junction (Fig. 27-35c) and stabilized by light
pressure for 5 min.
No suturing is needed but a light curing dressing is
applied for wound protection.
Coronally advanced flap procedure for multiple recessions
(
Fig.
27-36)
Zucchelli and De Sanctis (2000) described a flap de-
sign for the treatment of multiple recessions, which
allows for optimal adaptation of the flap following its
coronal advancement without placement of vertical
releasing incisions.
• Oblique submarginal incisions are placed in the
interdental areas and connected with intracrevicu
lar
incisions at the recession defects. The incisions are
extended to include one tooth on each side of the
teeth to be treated to facilitate a coronal reposition-
ing of the flap. The oblique incisions over the inter-
dental areas are placed in such a manner that the
"
surgically created papillae" mesial to the midline
of
the surgical field are dislocated apically and dis
tally,
while the papillae of the flap distal to the
mid-line are
shifted in a more apical and mesial
position (27-36a).
• Starting at the oblique interdental incisions, a split-
thickness flap is dissected (Fig. 27-36c). Apical to the
level of the root exposures, a full-thickness flap is
raised to provide maximum soft tissue thickness of
the flap to be coronally positioned over the roots
(Fig.
27-36d).
• At the most apical portion of the flap, the pe
riosteum
is incised and followed by dissection into
the
vestibular lining mucosa to eliminate all muscle
tension. The mobilized flap should be able to pas-
sively reach a level coronal to the CEJ at each single
tooth in the surgical field.
• The remaining facial portion of the interdental pa-
pillae is de-epithelialized to create connective tissue
beds to which the flap can be sutured.
• Sutures are placed to accomplish a precise adapta-
tion of the coronally advanced flap against the teeth
and to the interdental connective tissue beds (Fig.
MUCOGINGIVAL THERAPY — PERIODONTAL PLASTIC SURGERY
• 6o1
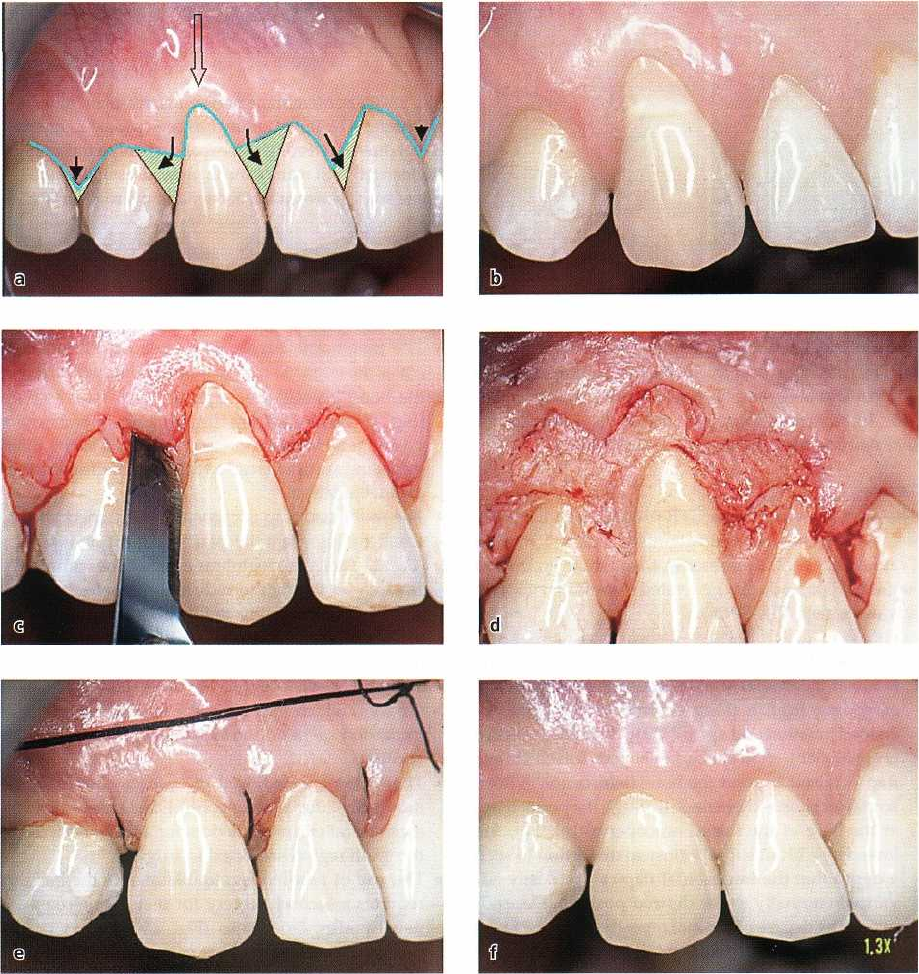
Fig. 27-36.
Coronally advanced flap procedure for multiple recessions. (a-e)
The oblique incisions over the interdental ar
-
eas are placed in such a manner that the "surgically created papillae" mesial to the midline of the surgical field
are
dislocated apically and distally, while the papillae of the flap distal to the mid-line are shifted in a more apical
and
mesial position (see text for explanation). (f) The 1-year post-treatment view.
27-36e). In addition, a horizontal double mattress
suture is placed to reduce lip tension on the mar-
ginal portion of the flap.
Pedicle soft tissue graft procedures combined with
membrane barriers
The use of a membrane barrier, according to the prin-
ciples of guided tissue regeneration (GTR, see Chapter
28), in conjunction with pedicle soft tissue graft pro-
cedures was introduced as a treatment modality for
root coverage (Pini Prato et al. 1992). A membrane
barrier is placed between the graft and the root in
order to favor the regeneration of the periodontium.
According to the concept of the GTR, a critical factor
for the outcome of the treatment procedure is that a
space for tissue formation is established between the
facial root surface and the membrane and maintained
during the healing. In order to create such a space, Pini
Prato et al. (1992) suggested that extensive root plan-
ing should be carried out to produce a concave root
morphology. In addition, bending of the membrane by
the placement of a Teflon suture (Fig. 27-37) in mesio-
distal direction through the membrane could facilitate
the maintenance of an adequate space. Specially de-
signed membranes for the treatment of recession type
defects are also available, such as non-absorbable tita-
602 • CHAPTER 27
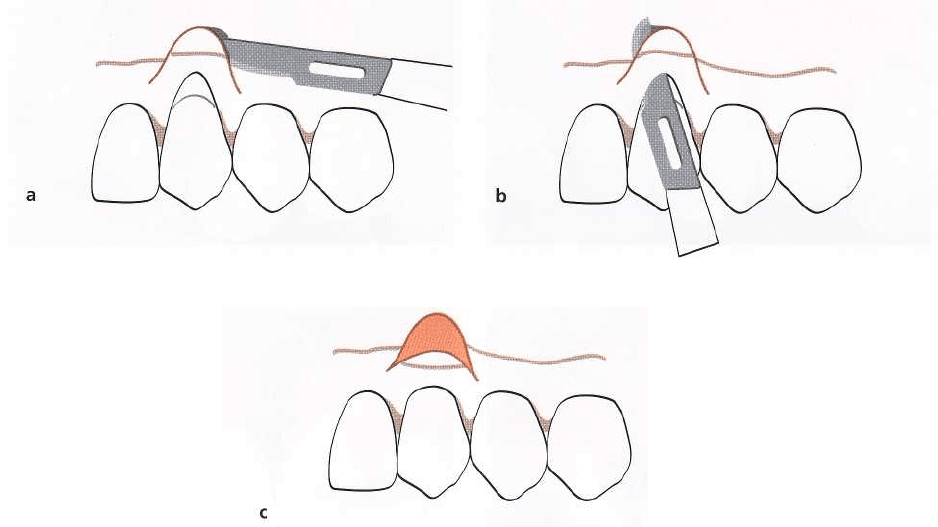
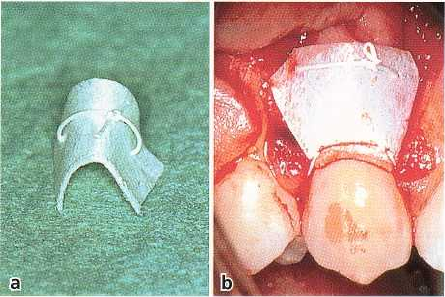
Fig. 27-37a,b. Membrane barrier for treatment of reces
-
sion defects. A Teflon suture has been placed in mesio
distal direction through an expanded polytetrafluore
-
thylene (ePTFE) membrane in order to establish ade-
quate space between the barrier and the root
surface.
nium-reinforced expanded polytetrafluorethylene
(
ePTFE) membranes (Fig. 27-38). In addition, a variety
of bioabsorbable membranes are commercially avail-
able, but many of these may not be rigid enough for
maintaining required space during healing.
Technique
The principles of using a GTR procedure in the treat-
ment of recessions were originally outlined by Pini
Prato et al. (1992). Commonly, the pedicle graft used
in the GTR procedure is generated through a coronally
advanced flap (Fig. 27-38).
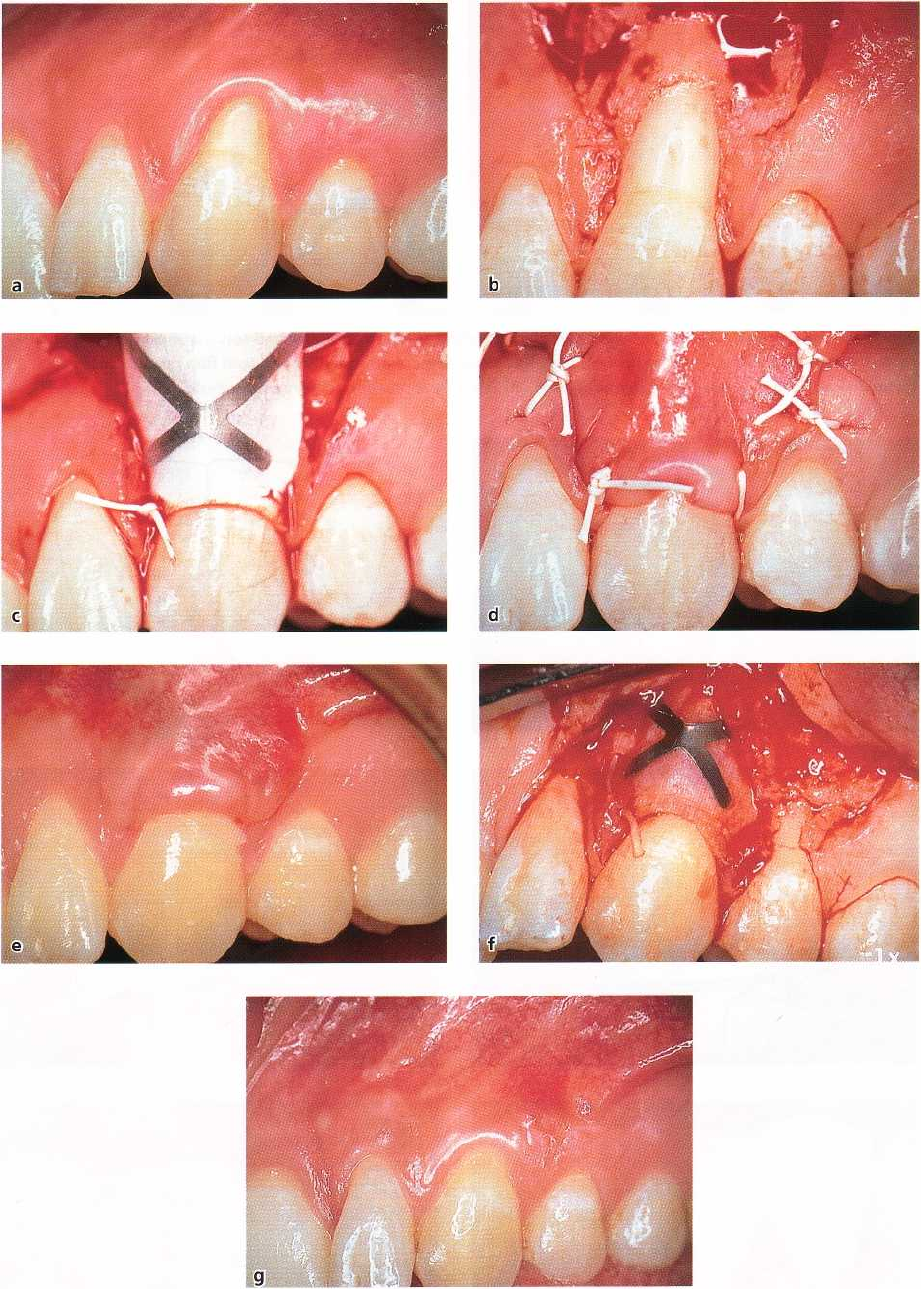
•
Apically divergent vertical releasing incisions are
made at the mesial and distal line axis of the tooth,
extending from a point coronal to the cemento-
enamel junction and apically into the lining mucosa
(Fig. 27-38b). A trapezium-shaped full-thickness
flap is raised beyond the bone dehiscence. A hori-
zontal incision is then made through the periosteum
at the base of the raised mucoperiosteal flap, fol-
lowed by a blunt supraperiosteal dissection to such
a depth that the trapezoidal flap can be easily ad-
vanced coronally to the desired position. Depend-
ing on the degree of coronal repositioning, the facial
portion of the interdental papillae may need to be
de-epithelialized to prepare proper recipient beds
for the pedicle graft.
•
The root is extensively planed or ground to obtain
a
concave profile of the root surface, thereby provid
-
ing space for tissue formation. If a titanium-rein-
forced membrane is used, the root profile may not
need to be changed to establish the required space
between the root and the membrane.
•
The membrane barrier to be used is trimmed to
cover the exposed root and approximately 3 mm of
the bone laterally and apically of the dehiscence
(
Fig. 27-38c). Following trimming, the membrane is
positioned over the root and anchored to the tooth
by a sling suture placed at the level of the cemento
-
enamel junction.
•
The mobilized flap is coronally positioned and se-
cured by interdentally placed interrupted sutures
(
Fig. 27-38d). The membrane should be completely
covered by the flap to reduce the risk for bacterial
contamination during the healing. Additional su-
tures are placed to close the lateral wound of the
releasing incisions.
•
To avoid the risk of collapse of the membrane over
the root, which may limit the space for blood clot
formation, a periodontal dressing should not be
applied.
•
The patient is advised to use a chlorhexidine
mouthrinse for plaque control and not to use any
mechanical cleaning devices for at least 6 weeks in
the tooth region subjected to surgery.
•
The use of non-biodegradable membrane barriers
requires a second surgery for membrane removal,
usually after 5-6 weeks (Fig. 27-38e-f). A partial
thickness trapezoidal flap is raised to expose the
membrane. Following its removal, the flap is repo-
sitioned at the level of the cemento-enamel junction
to completely cover the newly formed tissue. Me-
chanical plaque control is reinstituted 4 weeks after
membrane removal.
MUCOGINGIVAL THERAPY — PERIODONTAL PLASTIC SURGERY • 603
Fig. 27-38a-g.
Coronally advanced flap procedure combined with a non-biodegradable membrane barrier.
A recession defect
at tooth 23 requiring treatment due to the patient
'
s esthetic demands (see text for explanation). (g) The 1-yr postop-
erative healing result.
604 • CHAPTER 27
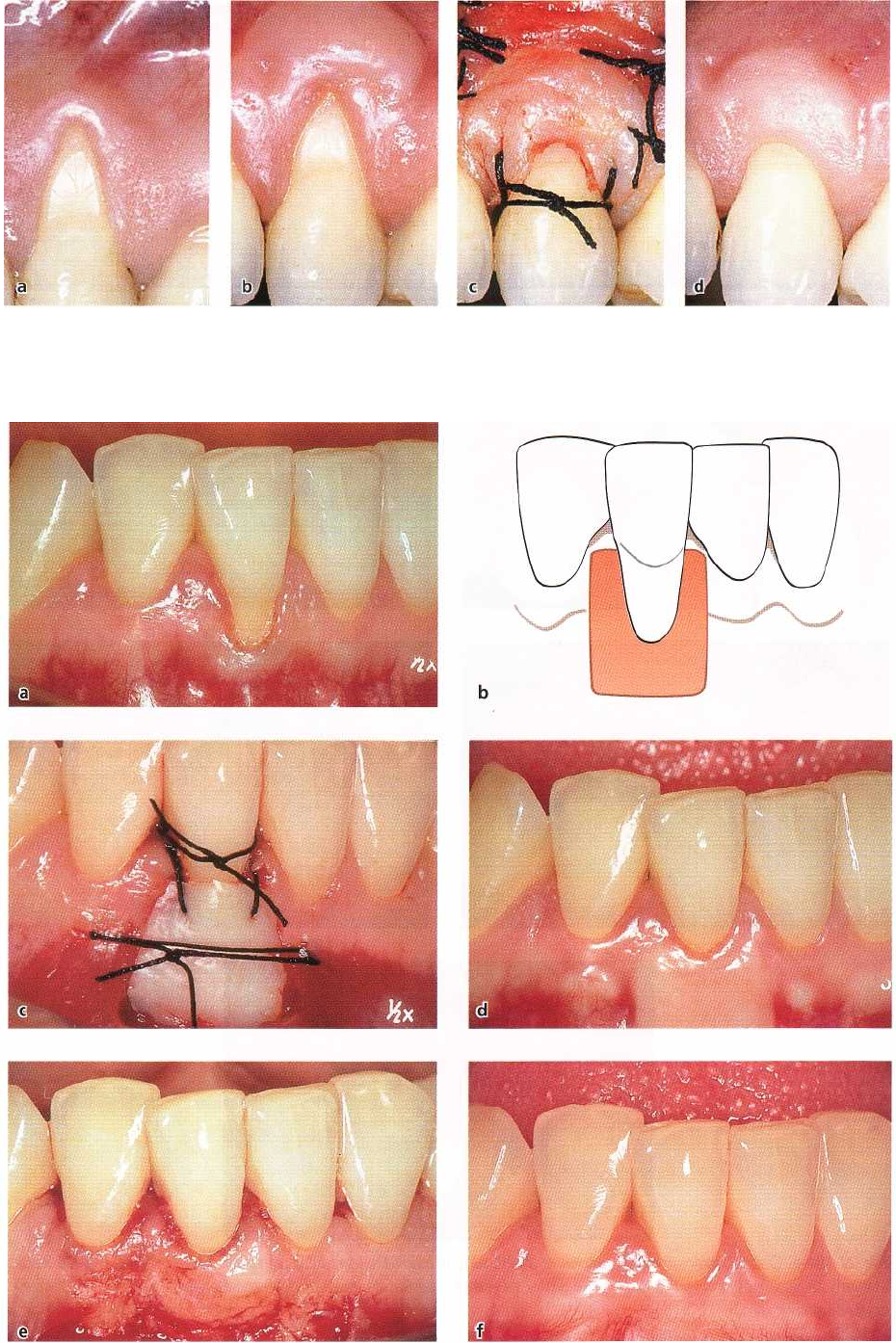
Fig. 27-39.
Two-stage epithelialized free soft tissue graft procedure. (a-c)
An epithelialized soft tissue graft is placed api
cal
to the recession and allowed to heal. At a second stage surgery a coronally advanced flap procedure is per-
formed to
achieve coverage of the denuded root. (d) The 1-year postoperative healing result.
Fig. 27-40a-f.
Epithelial/zed free soft tissue graft procedure.
A recession defect at a mandibular central incisor treated
with the free graft procedure (see text for explanation).
