Jan Lindhe. Clinical Periodontology
Подождите немного. Документ загружается.

584 • CHAPTER
27
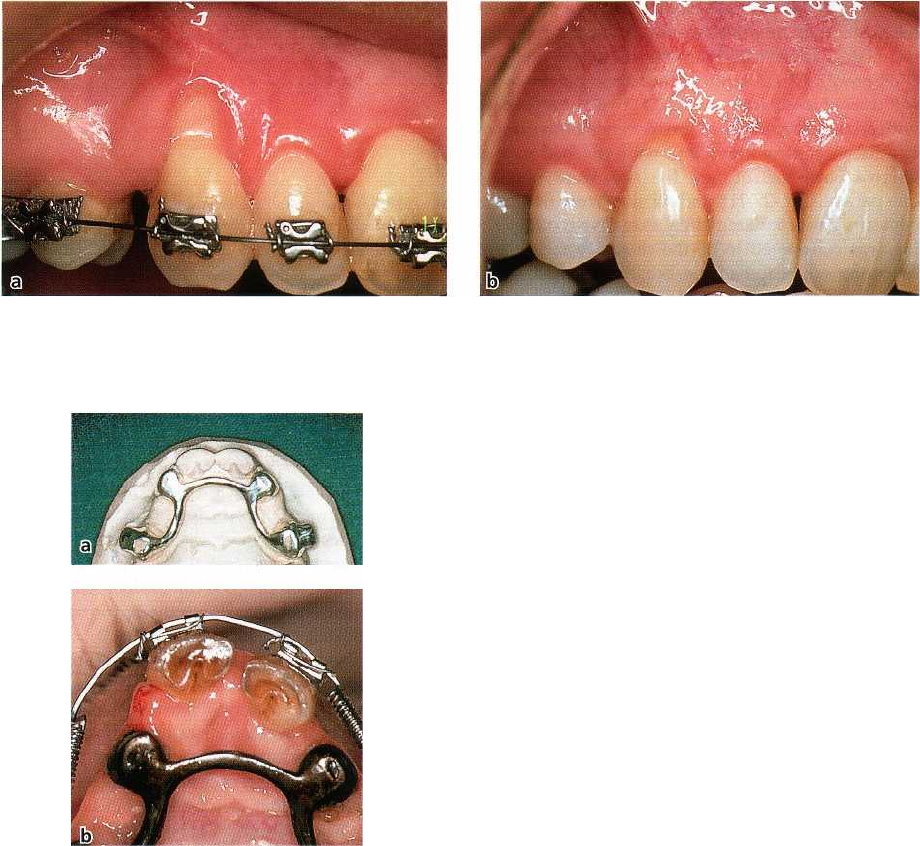
Fig. 27-14. A prominently positioned 13 showing soft tissue recession (a). The same tooth following the completion
of the orthodontic tooth movement (b). Note the reduction of the recession that has taken place as a consequence of
the changed position of the tooth.
Fig. 27-15. Occlusal view of the maxilla in a monkey
showing the position of the central incisors before (a)
and after (b) bodily movement in labial direction. The
canines and lateral incisors were joined in an individ
-
ual fabricated silver splint and used as anchorage teeth.
studies have shown that labial bone will reform in the
area of a dehiscence when the tooth is retracted to-
wards a proper positioning of the root within the
alveolar process (Engelking & Zachrisson 1982, Kar-
ring et al. 1982) (Fig. 27-13). It is therefore likely that
the reduction in recession seen at a previously promi
-
nently positioned tooth which has been moved into a
more proper position within the alveolar process, is
also accompanied by bone formation (Fig. 27-14).
Alterations occurring in gingival dimensions and
marginal tissue position in conjunction with ortho-
dontic therapy are related to the direction of tooth
movement. Facial movement results in reduced facial
gingival dimensions, while an increase is observed
following lingual movement (Coatoam et al. 1981,
Andlin-Sobocki & Brodin 1993). Batenhorst et al.
(
1974) and Steiner et al. (1981) used the monkey as an
experimental animal and studied soft tissue altera-
tions following either tipping and extrusion move-
ments or bodily movements of incisors. It was re-
ported that such tooth movements resulted in reces-
sion of the labial gingival margin and loss of attach-
ment. However, similarly designed studies carried out
in dogs (Karring et al. 1982, Nyman et al. 1982) and
humans (Rateitschak et al. 1968) failed to demonstrate
that labial tooth movement is accompanied by mar-
ginal tissue recession and attachment loss. This dis-
crepancy in the response of the marginal soft tissue to
orthodontic therapy in the studies referred to is diffi-
cult to understand but may be related to differences
with respect to (1) the amount of labial tooth displace
-
ment, (2) the magnitude of force applied, (3) the pres-
ence/absence of plaque and gingival inflammation in
the regions subjected to tooth movement and/or (4)
differences in gingival dimensions. Steiner et al. (1981)
speculated on mechanisms by which gingival tissue
could be lost as a result of labial tooth movement and
suggested that tension in the marginal tissue created
by the forces applied to the teeth could be an impor-
tant factor. If this hypothesis is valid, obviously the
volume (thickness) of the gingival tissue at the pres-
sure side rather than its apicocoronal height would
determine whether or not marginal tissue recession
develops during orthodontic therapy.
Support for this hypothesis is obtained from an
experimental study in monkeys (Wennstr6m et al.
1987) in which teeth were orthodontically moved into
areas with varying thickness and quality of the mar-
MUCOGINGIVAL THERAPY — PERIODONTAL PLASTIC SURGERY • 585
Fig. 27-16. The buccal aspect of the central incisors in the same monkey as in Fig. 27-15, before (a) and after (b) the
labial tooth movement. No obvious change in the location of the gingival margin has occurred despite the pro-
nounced labial displacement of the incisors.
ginal soft tissue. Following extensive bodily move
ment
of incisors in labial direction through the alveolar bone
(Fig. 27-15), most teeth showed a small apical
displacement of the soft tissue margin but no loss of
connective tissue attachment (Fig. 27-16). In other
words, the apical displacement of the gingival margin
was the result of a reduced height of the free gingiva
(
Fig. 27-17), which in turn may be related to tension —
"
stretching" — in the soft tissues during the facial tooth
movement and reduced buccolingual tissue thickness.
Similar to results presented by Foushee et al. (1985)
from a study in humans, no relationship was found
between the initial apicocoronal width (height) of the
gingiva and the degree of apical displacement of the
soft tissue margin during orthodontic therapy. Hence,
the findings do not lend support to the hypothesis that
a
certain zone of gingiva is essential for the prevention
of
recession during orthodontic therapy, but rather
corroborate clinical observations reported by Coa
toam
et al. (1981) suggesting that the integrity of the
periodontium can be maintained during orthodontic
therapy also in areas which have only a minimal zone
of gingiva.
Both Steiner et al. (1981) and Wennstr6m et al.
(
1987) reported that teeth which experienced loss of
connective tissue attachment when orthodontically
moved facially showed obvious clinical signs of in-
flammation throughout the experimental period.
Since
it has been demonstrated that, in the presence of
plaque-induced suprabony lesions, orthodontic forc
es
generating bodily tooth movement are incapable of
causing accelerated destruction of the connective tis-
sue attachment (Ericsson et al. 1978), it can be assumed
that "stretching" of the facial gingiva may favor the
destructive effect of the plaque-associated inflamma-
tory lesion due to the decreased buccolingual dimen-
sion of the border tissue. This assumption is validated
by the observations that, in the presence of plaque-in-
duced gingivitis, a thin marginal soft tissue is more
susceptible to complete breakdown than a thick one
(
Baker & Seymour 1976). Furthermore, since attach-
ment loss was found to be similar for plaque-infected
teeth which had been bodily moved
within the alveolar
bone
irrespective of the type of soft tissue (gingiva or
lining mucosa) (Wennstr6m et al. 1987), the thickness
rather than the quality of the marginal soft tissue on
the pressure side of the tooth seems to be the deter-
mining factor for the development of recession defects
during orthodontic therapy in plaque-infected denti-
tions. Hence, the observations made in the studies
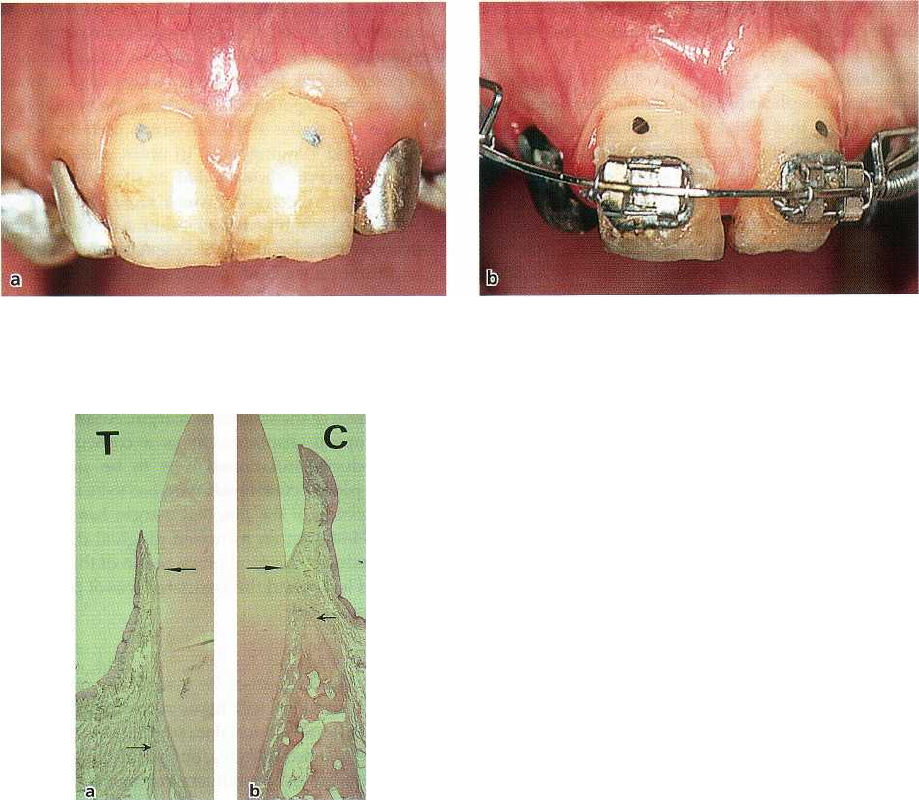
Fig. 27-17. Histologic specimens showing (a) reduced
alveolar bone height at an incisor bodily moved in la-
bial direction and (b) normal alveolar bone height at a
non-moved control tooth. Note the maintained level of
connective tissue attachment and the reduced height of
the free gingiva at the labially displaced incisor (a).
Large arrows indicate the position of the cemento-
enamel junction and small arrows the position of the al-
veolar bone crest.
586 • CHAPTER
27
discussed strongly emphasize the importance of ade-
quate plaque control during orthodontic treatment.
Conclusion
The clinical implication of the results from the studies
discussed is that labial tooth movement should be
preceded by careful examination of the dimensions of
the tissues covering the facial aspect of the teeth to be
moved. As long as the tooth can be moved within the
envelope of the alveolar process, the risk of harmful
side-effects in the marginal tissue is minimal, irrespec
-
tive of the dimensions and quality of the soft tissue. If,
however, the tooth movement is expected to result in
the establishment of an alveolar bone dehiscence, the
volume (thickness) of the covering soft tissue should
be considered as a factor that may influence the devel
-
opment of soft tissue recession during and/ or after the
phase of active orthodontic therapy. A thin gingiva
may serve as a locus
m-inorlts
resistentine
to developing
soft tissue defects in the presence of plaque-induced
inflammation or toothbrushing trauma.
Gingival dimensions and restorative therapy
The claim has been made that in segments of the
dentition involved in restorative therapy there is a
particular demand for gingiva (Maynard & Wilson
1979, Nevins 1986). The placement of restoration mar
-
gins subgingivally may not only create a direct opera-
tive trauma to the tissues (Donaldson 1974), but may
also facilitate subgingival plaque accumulation, with
resultant inflammatory alterations in the adjacent
gingiva and recession of the soft tissue margin (Val-
derhaug 1980, Parma-Benfenati et al. 1985). Valder-
haug (1980) evaluated longitudinally over a 10-year
period the soft tissue alterations taking place at facial
sites of 286 teeth with subgingivally or supragingi-
vally placed crown margins in 82 patients. The re-ex-
amination performed 1 year after insertion of the res-
torations revealed that the gingivae at teeth with sub-
gingival restoration margins were more inflamed than
at those with supragingivally placed borders. Of the
150 teeth which at the time of cementation had the
facial crown margin located subgingivally, 40%
showed supragingival exposure of the crown margin
already after 1 year and at the 10-year examination as
many as 71% had become supragingivally positioned
due to recession of the soft tissue margin. Compared
to teeth with supragingivally placed crown margins,
the amount of recession and clinical attachment loss
was greater at sites with subgingivally placed restora-
tion margins.
Stetler & Bissada (1987) evaluated the periodontal
conditions at teeth with subgingivally placed restora-
tion margins on teeth with varying apicocoronal
height of gingiva and found that teeth having a nar-
row (< 2 mm) band of gingiva showed more pro-
nounced clinical signs of inflammation than restored
teeth with a wide gingival zone, but that there was no
difference in loss of probing attachment. However, if
subgingivally placed restorations facilitate plaque ac-
cumulation and the adjacent gingiva is thin, there may
be a potential risk for the development of soft tissue
recession. An experimental study in the beagle dog
(
Ericsson & Lindhe 1984), in which metallic strips
were inserted subgingivally in areas with varying
width of gingiva, showed that in sites with a thin
gingival margin, recession was a more likely conse-
quence of the combined tissue trauma caused by the
insertion of the strip and subsequent plaque accumu
-
lation during a 6-month period than in sites with a
broad gingival zone. The authors suggested that the
placement of restorations in a subgingival position at
sites with a thin gingiva may in the presence of sub-
gingival plaque favor an inflammatory tissue reaction
which results in loss of tissue height, i.e. in apical
displacement of the soft tissue margin. Accordingly, if
such an apical displacement as a consequence of
plaque-induced inflammation is to be prevented,
either the plaque control standard has to be improved
or the
thickness
of the gingival margin has to be in-
creased. However, an increased gingival dimension
will not reduce the apical propagation of the plaque-
associated lesion and the associated loss of periodon
-
tal attachment.
Conclusion
Subgingival placement of the margin of a restoration
is likely to result in soft tissue recession over time.
Experimental and clinical data suggest that the thick
-
ness of the marginal gingiva, but not the apicocoronal
width of the gingiva, is influencing the magnitude of
recession taking place as a result of direct mechanical
trauma during tooth preparation and bacterial plaque
retention.
Indications for gingival augmentation
Scientific data obtained from well-controlled clinical
and experimental studies have unequivocally demon
-
strated that the apicocoronal width of gingiva and the
presence of an attached portion of gingiva are not of
decisive importance for the maintenance of gingival
health and the height of the periodontal tissues. Con
-
sequently, the presence of a narrow zone of gingiva
per
se
cannot justify surgical intervention (Proceedings of
the 1st European Workshop on Periodontology 1994,
Proceedings of the World Workshop on Periodontics
1996). However, gingival augmentation should be
considered in situations where the patient experiences
discomfort during toothbrushing and/or chewing
due to an interfering lining mucosa. Furthermore,
when orthodontic tooth movement is planned and the
final positioning of the tooth can be expected to result
in an alveolar bone dehiscence, an increase of the
thickness
of the covering soft tissue may reduce the risk
for development of soft tissue recession. An increase
of the
thickness
of the gingival margin may in certain
MUCOGINGIVAL THERAPY - PERIODONTAL PLASTIC SURGERY • 5
8
7
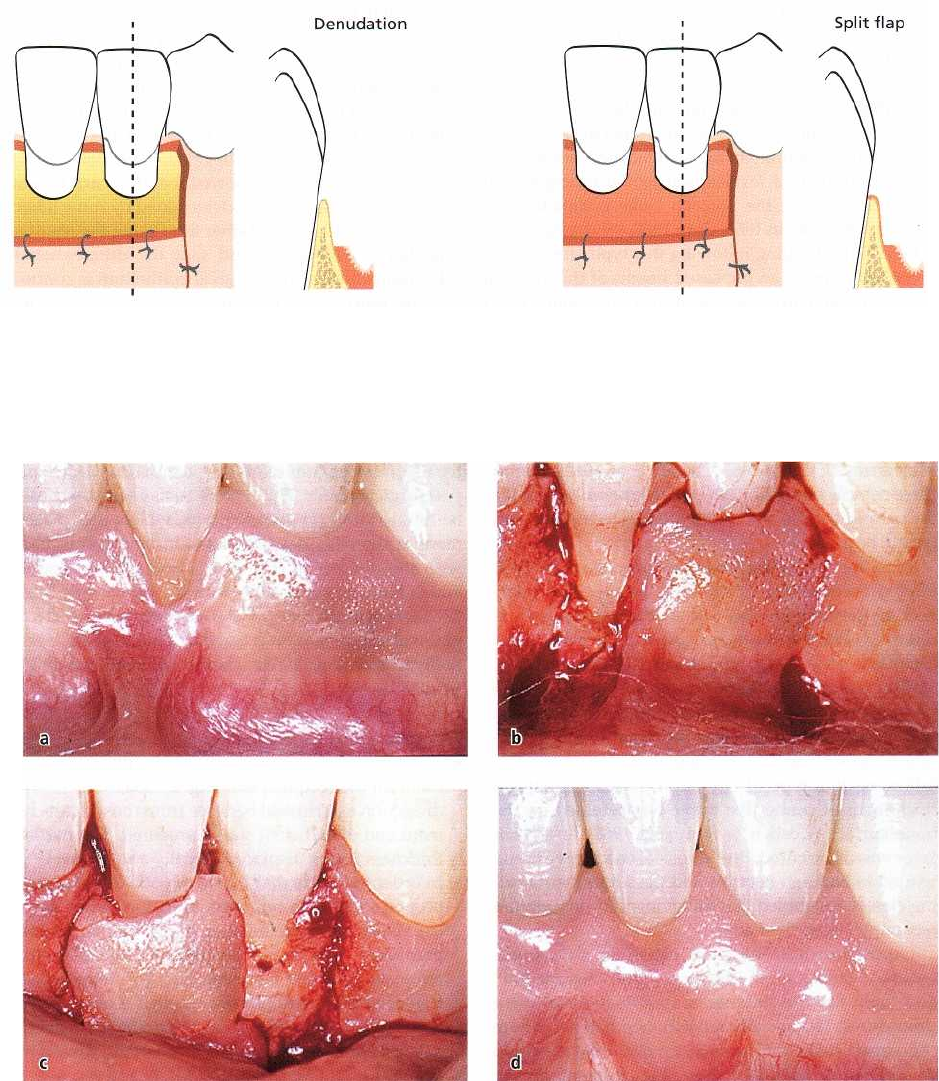
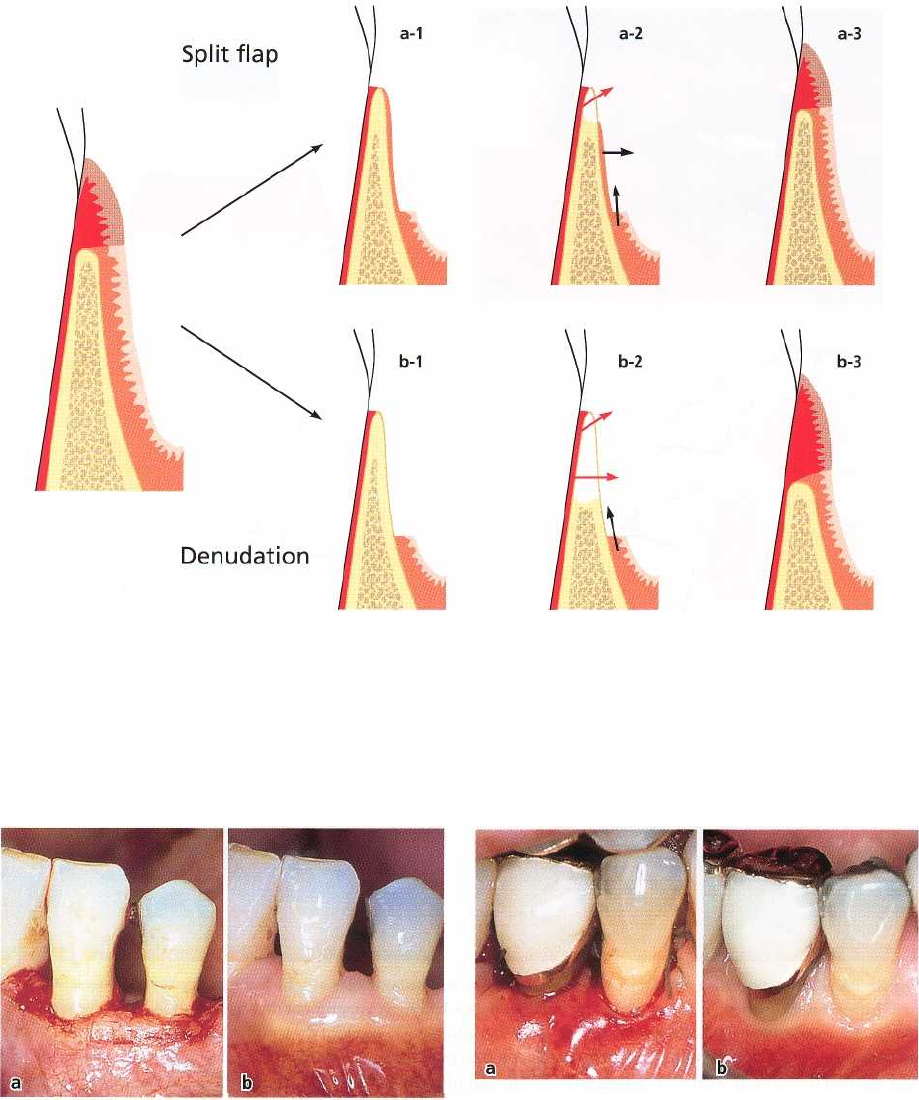
Fig. 27-18. The use of vestibular extension operations for increasing the width of the gingiva involves the produc-
tion of a wound extending from the gingival margin to a level some mm apical to the mucogingival junction. With the
"denudation" technique all soft tissue is removed, leaving the alveolar bone exposed. With the "split flap" pro-
cedure
only the superficial portion of the oral mucosa is removed, leaving the bone covered with connective tissue.
Fig. 27-19.
Pedicle graft procedure for gingival augmentation. A
lower central incisor with facial soft tissue recession as-
sociated with high attachment of a frenulum (a). The frenulum is released and a split flap of keratinized tissue is
dissected from the area of the neighboring tooth (b). The mobilized soft tissue flap is laterally moved and secured
in
position at the recipient site (c). The healing result 1-year post-treatment shows the establishment of a broad
zone
of keratinized tissue without interfering frenulum (d).
situations also be considered when subgingival resto-
rations are placed in areas with a thin marginal tissue.
Gingival augmentation procedures
The gingival augmentation operations comprise a
number of surgical techniques, the majority of which
have been developed mainly on an empirical basis
and
without sufficient knowledge of the biology of the
involved tissues. The earliest of these techniques are
the
"vestibular extension operations", which were de-
signed
mainly with the objective of extending the
depth of the
vestibular sulcus (Bohannan 1962a,b). In
recent years,
however, pedicle or free soft tissue grafts
have become
the most commonly used techniques in
588 •
CHAPTER
27
the management of "insufficient" gingival dimen
sions,
because of higher predictability of the healing
result.
Vestibular/gingival
extension procedures
The "denudation techniques" included the removal of
all soft tissue within an area extending from the gin-
gival margin to a level apical to the mucogingival
junction, leaving the alveolar bone completely ex-
posed (Ochsenbein 1960, Corn 1962, Wilderman 1964)
(Fig. 27-18). Healing following this type of treatment
resulted often in an increased height of the gingival
zone, although in some cases only a very limited effect
was observed. However, the exposure of alveolar bone
produced severe bone resorption with permanent loss
of bone height (Wilderman et al. 1961, Costich & Ram
-
fjord 1968). In addition, the recession of marginal
gingiva in the surgical area often exceeded the gain of
gingiva obtained in the apical portion of the wound
(
Carranza & Carraro 1963, Carraro et al. 1964). Due to
these complications and severe postoperative pain for
the patient, the use of the "denudation technique" can
hardly be justified.
With the "periosteal retention" procedure or "split
flap" procedure (Fig. 27-18) only the superficial por-
tion of the oral mucosa within the wound area is
removed, leaving the bone covered by periosteum (
Staffileno et al. 1962, Wilderman 1963, Pfeifer 1965,
Staffileno et al. 1966). Although the preservation of the
periosteum implies that less severe bone resorption
will occur than following the "denudation technique",
loss of crestal bone height was observed also
following this type of operation unless a relatively
thick layer of connective tissue was retained on the
bone surface (Costich & Ramfjord 1968). If a thick
layer was not secured, the periosteal connective tissue
tended to undergo necrosis and the subsequent heal-
ing closely resembled that following the "denudation
technique" described above.
Other described gingival extension procedures
maybe regarded as modifications of the "denudation"
and "split flap" techniques or combinations of these
procedures. The apically repositioned flap procedure
(
Friedman 1962), for instance, involved the elevation
of
soft tissue flaps and their displacement during
suturing in an apical position, often leaving 3-5 mm
of alveolar bone denuded in the coronal part of the
surgical area. This resulted in the same risk for exten
-
sive bone resorption as other "denudation tech-
niques". It was proposed by Friedman (1962) that a
postsurgical increase of the width of the gingiva can
be predicted with the "apically repositioned flap", but
several studies indicated that the presurgical width
most often was retained or became only slightly in-
creased (Donnenfeld et al. 1964, Carranza & Carraro
1970).
The described vestibular/ gingival extension proce-
dures were based on the assumption that it is the
frictional forces encountered during mastication
which determine the presence of keratinized tissue
adjacent to the teeth (Orban 1957, Pfeifer 1963). There
-
fore, it was believed that by the displacement of mus-
cle attachments and the extension of vestibular depth,
the regenerating tissue in the surgical area would be
subjected to physical impacts and adapt to the same
functional requirements as those met by "normal"
gingiva (Ivancie 1957, Bradley et al. 1959, Pfeifer 1963).
Later studies, however, showed that the characteristic
features of the gingiva are determined by some inher-
ent factors in the tissue rather than being the result of
functional adaptation, and that the differentiation
(
keratinization) of the gingival epithelium is control-
led
by morphogenetic stimuli from the underlying
connective tissue (see Chapter 1).
Grafting procedures
The gingival and palatal soft tissues will maintain
their original characteristics after transplantation to
areas of the alveolar mucosa (see Chapter 1). Hence,
the use of transplants offers the potential to predict the
postsurgical result. The type of transplants used can
be divided into (1) pedicle grafts, which after place-
ment at the recipient site maintain their connection
with the donor site (Fig 27-19), and (2) free grafts,
which have no connection with the donor area (Fig.
27-20). Free grafts have most commonly been used for
gingival augmentation (Haggerty 1966, Nabers 1966,
Sullivan & Atkins 1968a, Hawley & Staffileno 1970,
Edel 1974).
Technique
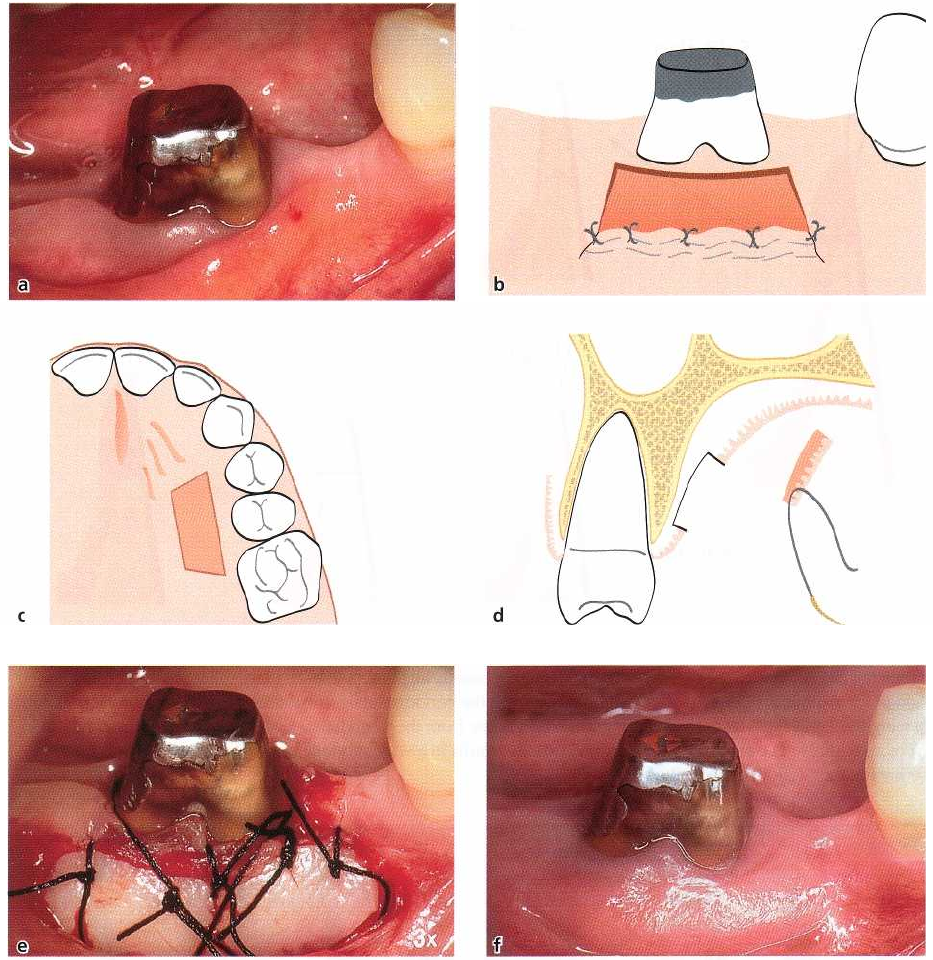
• The surgical procedure is initiated with the prepa-
ration of the recipient site (Fig. 27-20a,b). By sharp
dissection a periosteal bed free from muscle attach-
ment and of sufficient size is prepared. The partial
thickness flap is displaced apically and sutured.
• In order to ensure that a graft of sufficient size and
proper contour is removed from the donor area,
usually the palatal mucosa in the region of the
premolars, it is recommended to produce a foil
template over the recipient site. The template is
transferred to the donor site where it is outlined by
a
shallow incision (Fig. 27-20c). A graft with a thick
-
ness of approximately 1.5-2 mm is then dissected
from the donor area (Fig. 27-20d). It is advocated to
place the sutures in the graft before it is cut com-
pletely free from the donor area, since this may
facilitate its transfer to the recipient site.
• The graft is immediately transferred to the prepared
recipient bed and sutured (Fig. 27-20e). In order to
immobilize the graft at the recipient site the sutures
must be placed in the periosteum or the adjacent
attached gingiva. After suturing, pressure is exerted
against the graft for 5 min in order to eliminate
blood and exudate between the graft and the recipi-
ent bed. The graft as well as the palatal wound is
protected with a periodontal dressing. To retain the
dressing in the palatal site, a stent usually has to be
used.
MUCOGINGIVAL THERAPY — PERIODONTAL PLASTIC SURGERY • 5
8
9
Fig. 27-20.
Grafting procedure for gingival augmentation. A
mandibular molar at which the patient experiences discom
-
fort during toothbrushing due to interfering lining mucosa and high attachment of a frenulum (a). The decision
was made to apically displace the attachment of the frenulum and augment the gingival zone through the place-
ment of a free graft.
A
partial thickness flap is dissected to prepare a recipient bed. The flap is apically displaced
and sutured (b).
A
graft with a thickness of 1.5-2 mm and of sufficient size and contour (a foil template of the recipi
-
ent site may be used) is dissected from the palatal mucosa in the region of the premolars (c-d). The graft is immedi
-
ately transferred to the prepared recipient bed and anchored by sutures to secure a close adaptation of the graft to
the recipient bed (e).
A
periodontal dressing is applied to protect the graft. Following healing, a broad zone of kerat
-
inized tissue has been established (f).
• The sutures and periodontal dressing are removed
after 1-2 weeks.
For a description of the pedicle graft procedure, see
"
Root coverage procedures" later in the chapter.
Healing following gingival augmentation
procedures
Vestibular/gingival extension procedures
Since the specificity of the gingiva is determined by
some inherent factor in the tissues, the postoperative
results of vestibular extension procedures depend on
the degree to which the various tissues contribute to
the
formation of granulation tissue in the wound area
590 • CHAPTER 27
Fig. 27-22. Clinical photographs of the buccal aspect of
a canine and a premolar following the removal of the
entire zone of gingiva by a gingivectomy procedure (a).
The healing result 9 months after surgery (b) shows the
regain of keratinized tissue.
(Karring et al. 1975). Following the "denudation" or
"
split flap technique", the wound area is filled with
granulation tissue derived from the periodontal liga-
ment, the tissue of the bone marrow spaces, the re-
tained periosteal connective tissue, and the surround-
ing gingiva and lining mucosa (Fig. 27-21). The degree
of bone resorption induced by the surgical trauma
Fig. 27-23. Clinical photographs of a tooth region sub-
jected to excision of the entire zone of gingiva by a flap
procedure. The alveolar mucosa has been coronally dis
-
placed to achieve complete coverage of the surgically
exposed alveolar bone (a). Healing has resulted in the
reformation of a narrow zone of gingiva on the buccal
aspect of the teeth, 9 months post-surgery (b).
influences the relative amount of granulation tissue
which grows into the wound from these various tissue
sources. The resorption of crestal bone exposes vary
ing
amounts of the periodontal ligament tissue in the
marginal area allowing granulation tissue from the
periodontal ligament to fill out the coronal portion of
the
wound. The greater the bone loss, the greater the
Fig. 27-21. Schematic drawing illustrating different stages of healing following the "split flap" (a) and "denuda
tion" (
b) techniques. Cells from the oral mucosa, bone and periodontal ligament (arrows) participate in granulation tissue
formation. Due to the difference in the degree of bone resorption (a-2, b-2), a larger area of the coronal por
tion of
the wound is filled with granulation tissue from the periodontal ligament following "denudation" than fol
lowing the
"split flap" technique. Since granulation tissue from the periodontal ligament possesses the ability to in
duce a
keratinized epithelium,
"
denudation" usually results in a wider zone of keratinized tissue than is the case
following
the "split flap" technique (a-3, b-3).
MUCOGINGIVAL THERAPY — PERIODONTAL PLASTIC SURGERY • 591
portion of the wound which becomes filled with
granulation tissue from the periodontal ligament. This
particular tissue possesses the capability to induce
keratinization of the covering epithelium. This means
that the widening of the keratinized tissue following "
denudation" and "split flap" operations is achieved
at
the expense of a reduced bone height. The "denu-
dation technique" results usually in more bone loss
than the "split flap technique". Therefore, a greater
amount of granulation tissue with the capability of
inducing a keratinized epithelium develops in the
marginal area following the "denudation technique"
than following the "split flap technique". This is in
accordance with the clinical observation that the
"
denudation technique" usually is superior to the
"
split flap technique" in increasing the width of kerat-
inized tissue (Bohannan 1962a,b).
In a clinical study by Wennstr6m (1983) periodontal
pockets were eliminated by the use of a "gingivec-
tomy" or a "flap" procedure, both of which involved
the
complete removal of the keratinized tissue. In the
"
gingivectomy" procedure the wounded area was left
to
heal by second intention, while in the "flap" proce-
dure the alveolar mucosa was repositioned to achieve
complete coverage of the surgically exposed alveolar
bone (Figs. 27-22a & 27-23a). Irrespective of the surgi
-
cal technique used, healing resulted in the reformation
of keratinized tissue, the width of which, however,
was greater following the "gingivectomy" procedure
than following the "flap" procedure (Figs. 27-22b &
27-23b). The gingiva was formed because granulation
tissue from the periodontal ligament with the capacity
of inducing a keratinized epithelium had proliferated
coronally along the root surface. This granulation tis-
sue formation was obviously favored by a more pro-
nounced bone resorption during the healing follow-
ing the "gingivectomy" procedure.
It can be concluded that the success or failure in
extending the width of keratinized tissue by the
"
denudation" or "split flap" techniques rests with the
origin of granulation tissue, which is related to the
extent of bone loss induced by the surgical trauma.
This in turn means that the result with respect to
increasing the gingival width by methods involving
periosteal exposure or denudation of the alveolar
bone is unpredictable. The use of such methods is
therefore not justified in periodontal therapy. The pro
-
cedures discussed merely represent examples of how
lack of knowledge about basic biologic principles may
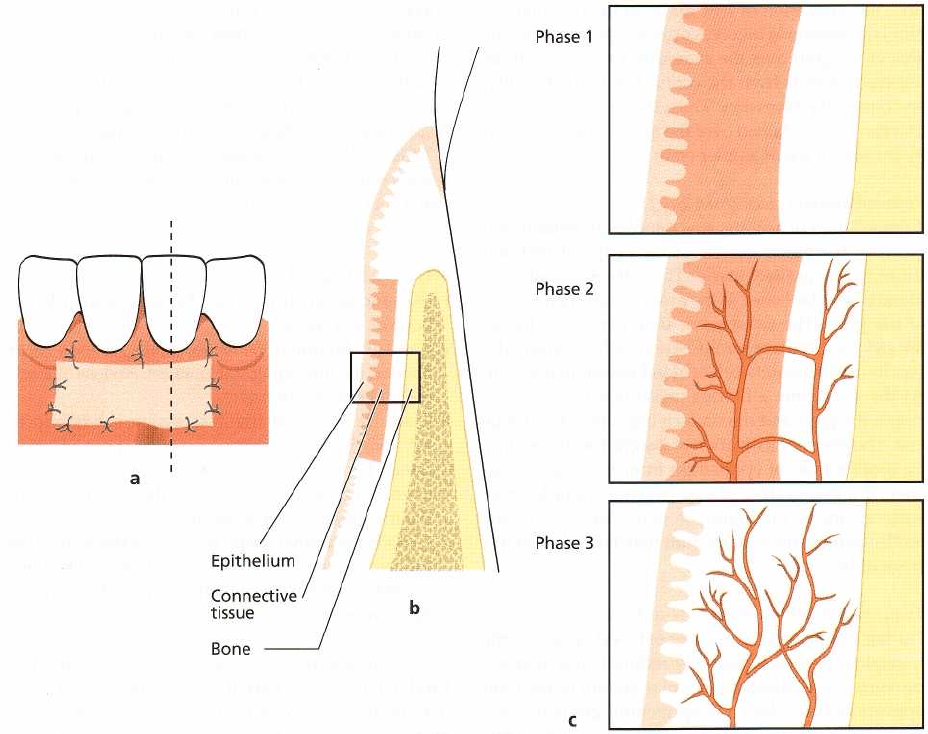
Fig. 27-24. Schematic drawings illustrating healing of a free gingival graft placed entirely on a connective tissue re-
cipient bed (a). A cross-section through the area is shown in (b). The framed areas (c) illustrate the three phases into
which the healing process can be divided.
592 • CHAPTER 27
lead to the development of inappropriate therapeutic
methods.
Grafting procedures
Healing of free soft tissue grafts placed entirely on a
connective tissue recipient bed has been studied in
monkeys by Oliver et al. (1968) and Nobuto et al.
(
1988). According to these authors, healing can be
divided into the following three phases (Fig. 27-24).
The initial phase (from 0 to 3 dams)
In these first days of healing a thin layer of exudate is
present between the graft and the recipient bed. Dur-
ing this period the grafted tissue survives with an
avascular "plasmatic circulation" from the recipient
bed. Therefore, it is essential for the survival of the
graft that a close contact is established to the underly
-
ing recipient bed at the time of operation. A thick layer
of exudate or a blood clot may hamper the "plasmatic
circulation" and result in the rejection of the graft. The
epithelium of the free graft degenerates early in the
initial healing phase, and subsequently it becomes
desquamated. In placing a graft over a recession, part
of the recipient bed will be the avascular root surface.
Since the graft is dependent on the nature of its bed
for diffusion of plasma and subsequent revasculariza-
tion, the utilization of free grafts in the treatment of
gingival recessions involves a great risk of failure. The
area of the graft over the avascular root surface must
receive nutrients from the connective tissue bed that
surrounds the recession. Thus, the amount of tissue
that can be maintained over the root surface is limited
by the size of the avascular area.
Revascularization phase (from 2 to 11 days)
After 4-5 days of healing, anastomoses are established
between the blood vessels of the recipient bed and
those in the grafted tissue. Thus, the circulation of
blood is re-established in the preexisting blood vessels
of the graft. The subsequent time period is charac-
terized by capillary proliferation, which gradually
results in a dense network of blood vessels in the graft.
At the same time a fibrous union is established be-
tween the graft and the underlying connective tissue
bed. The re-epithelialization of the graft occurs mainly
by proliferation of epithelium from the adjacent tis-
sues. If a free graft is placed over the denuded root
surface, apical migration of epithelium along the
tooth-facing surface of the graft may take place at this
stage of healing.
Tissue maturation phase (from 11 to 42 days)
During this period the number of blood vessels in the
transplant becomes gradually reduced, and after ap-
proximately 14 days the vascular system of the graft
appears normal. Also, the epithelium gradually ma-
tures with the formation of a keratin layer during this
stage of healing.
The establishment and maintenance of a "plasmatic
circulation" between the recipient bed and the graft
during the initial phase of healing is critical for the
result of this kind of therapy. Therefore, in order to
ensure ideal conditions for healing, blood between the
graft and the recipient site must be removed by exert-
ing pressure against the graft following suturing.
ROOT COVERAGE
The main indications for root coverage procedures are
esthetic /cosmetic demands (Fig. 27-25) and root hy-
persensitivity and management of shallow root caries
lesions and cervical abrasions. Changing the topogra-
phy of the marginal soft tissue in order to facilitate
plaque control is also a common indication for root
coverage procedures (Fig. 27-26).
It should be recalled that the two major causative
factors in the development of marginal tissue reces-
sions are plaque-induced periodontal inflammation
and trauma caused by toothbrushing. The control of
these factors will in most cases prevent further pro-
gression of the recession. This means that in tooth
regions with a thin covering soft tissue, with or with-
out an incipient recession, the patient should be en-
couraged to carry out effective but at the same time
non-traumatic plaque control measures. With respect
to toothbrushing, the Bass' method (Chapter 21)
should be avoided and the patient should be in-
structed to use a technique creating as little apically
directed pressure on the soft tissue margin as possible.
A soft toothbrush should, of course, be used.
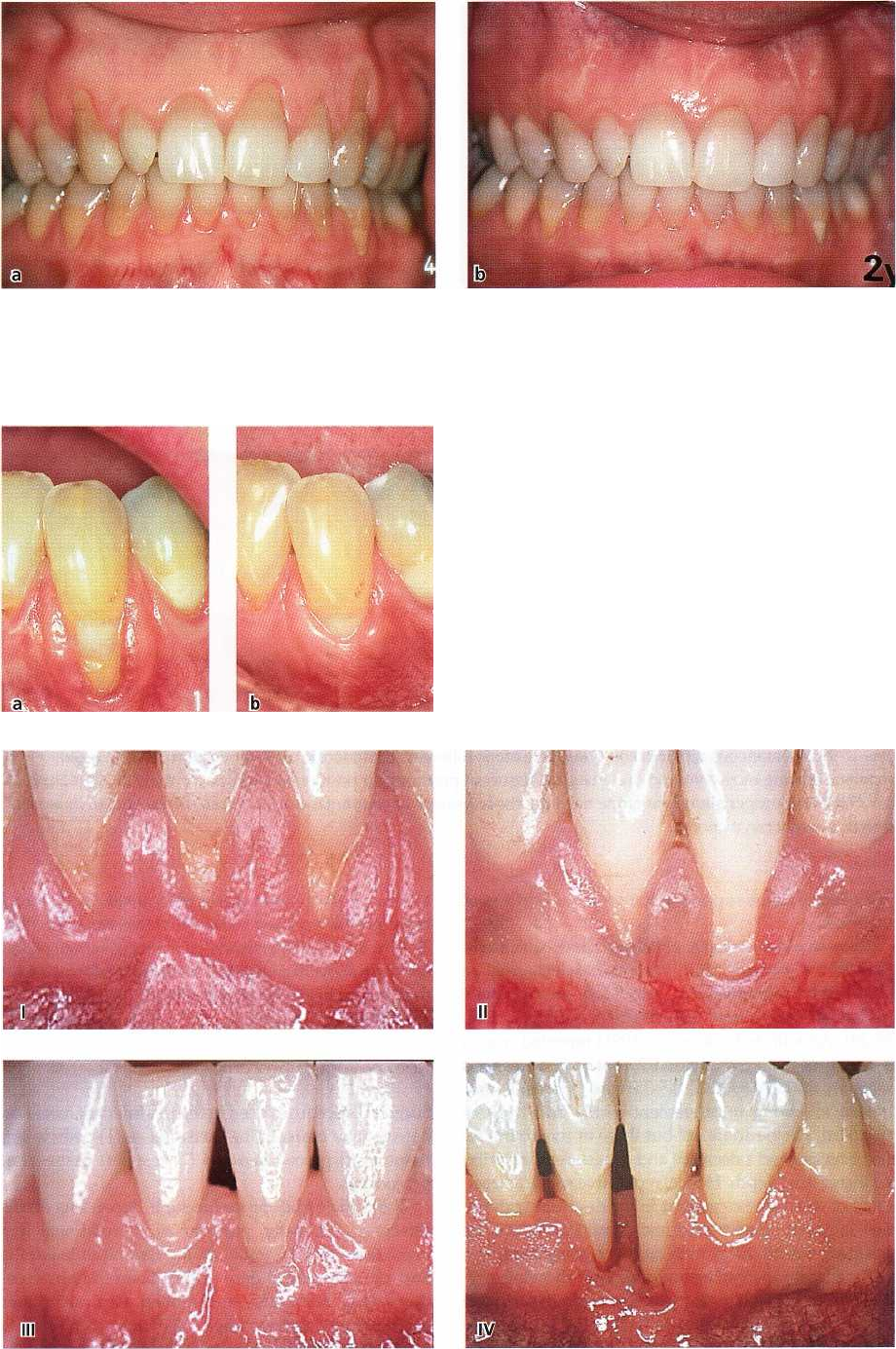
Miller (1985a) described a useful classification of
recession defects, taking into consideration the antici
-
pated root coverage that it is possible to obtain (Fig.
27-27):
• Class I: Marginal tissue recession not extending to
the mucogingival junction. No loss of interdental
bone or soft tissue.
• Class II: Marginal tissue recession extends to or
beyond the mucogingival junction. No loss of inter-
dental bone or soft tissue.
• Class III: Marginal tissue recession extends to or
beyond the mucogingival junction. Loss of inter-
dental bone or soft tissue is apical to the cemento-
enamel junction, but coronal to the apical extent of
the marginal tissue recession.
• Class IV: Marginal tissue recession extends beyond
the mucogingival junction. Loss of interdental bone
extends to a level apical to the extent of the marginal
tissue recession.
While complete root coverage can be achieved in Class
I and II defects, only partial coverage may be expected
in Class III. Class IV recession defects are not amena-
ble to root coverage. Consequently, the critical clinical
variable to assess in order to determine the possible
outcome of a root coverage procedure is the level of
MUCOGINGIVAL THERAPY — PERIODONTAL PLASTIC SURGERY • 593
Fig. 27-25. A 25-year-old woman having esthetic concerns due to multiple soft tissue recessions in the maxilla and a
high lip line (a). The gingiva is healthy and several of the exposed root surfaces show abrasion defects, indicating
toothbrushing trauma as the causative factor for the development of the recessions. The brushing technique was al-
tered and root coverage was surgically achieved. The 2-year post-treatment view (b).
Fig. 27-26. A mandibular canine with a deep recession,
which offers problems with respect to self-performed
plaque control (a). To facilitate plaque control the posi-
tion of the soft tissue margin was altered surgically (b).
Fig. 27-27. The Miller classification of recession defects (see text).
