Jan Lindhe. Clinical Periodontology
Подождите немного. Документ загружается.

ENDODONTICS AND PERIODONTICS • 333
for direct visual examination (Fig. 14-19e,f; Walton et
al. 1984).
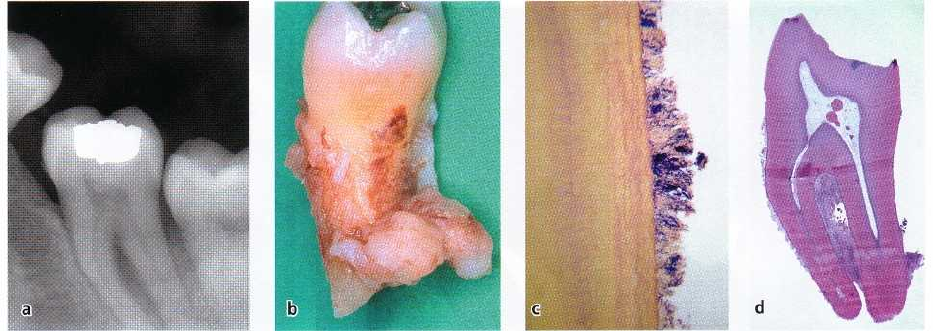
Data on prevalence of vertical root fractures are
scarce in the literature. While the prevalence appears
to be low, vertical root fractures probably occur more
often than clinicians are able to diagnose (Tamse et al.
1999b). There seems to be an overrepresentation of
endodontically treated teeth compared to teeth with
vital pulps (Fig. 14-21), with molars and premolars
more often affected than incisors and canines (Meister
et al. 1980, Testori et al. 1993). In longitudinal clinical
follow-up studies of patients treated with fixed pros-
theses, vertical root fractures were frequent in root-
filled teeth with posts and, in particular, among those
teeth serving as terminal abutments in cantilever
bridges (Randow et al. 1986).
It is of clinical interest to note that root fracture of
endodontically treated teeth may occur and/or be
diagnosed several years after the completion of endo-
dontic therapy and final restoration of the tooth (Fig.
14-19). In a study comprising 32 vertical root fractures,
the average time between the completion of endodon-
tic treatment and diagnosis of fracture was 3.25 years,
with a range varying between 3 days and 14 years (
Meister et al. 1980). In another study comprising 36
teeth, symptoms of root fracture developed on aver-
age more than 10 years after completion of treatment
(Testori et al. 1993).
Although the subject of considerable study, the eti-
ology of vertical root fractures is not well established.
In some situations the cause is undoubtedly iatrogenic
from pin and post placements, root canal filling pro-
cedures, and seating of intracoronal restorations. Re-
sults of experimental studies suggest that loss of tooth
structure from caries, trauma and restorative proce-
dure weakens teeth and makes them susceptible to
fracture from mastication forces (Reeh et al. 1989,
Sedgley & Messer 1992). The reason vertical root frac
tures appear to be associated with endodontically
treated teeth may be that the access opening prepara-
tion as well as overzealous root canal preparation
results in substantial loss of fracture resistance. It has
also been speculated that, along with loss of vital pulp
tissue, mechanoreceptive functions are lost concomi-
tantly, allowing larger loads to be placed during mas-
tication than the patient would normally tolerate (
Lowenstein & Rathkamp 1955, Randow & Glantz
1986). Suggestions that endodontically treated teeth
with time become brittle due to changes in the
biomechanical properties of dentin and, thus, less
resistant to mastication forces have not been substan-
tiated in careful analyses (Sedgley & Messer 1992).
Also, clinically intact teeth with no or minimal
restorations may be subjected to vertical root fracture (
Fig. 14-21). Traumatic occlusal forces may induce
fracture, and mandibular molars appear to be espe-
cially at risk (Yang et al. 1995, Chan et al. 1999). Sub-
sequent to these fractures typical pulpitis symptoms
may be initiated followed by breakdown of the pulp
and abscess formation, if the fracture involves the
pulp tissue directly.
Vertical root fractures that involve the gingival sul-
cus/pocket area usually have a hopeless prognosis
due to continuous bacterial invasion of the fracture
space from the oral environment. While there are re-
ports on successful management of fractured teeth by
reattaching the fragments with a bonding resin after
extraction and re-implantation, fractured teeth are
normally candidates for extraction. In multirooted
teeth a treatment alternative is hemisection and ex-
traction of the fractured root.
Conclusion
Symptoms and signs associated with vertical root
fractures show a varying character and may be diffi-
cult to distinguish from those associated with peri-
odontal and endodontic lesions. A variety of diagnos-
tic procedures should be considered. Except for the
leads obtained from anamnestic findings and pocket
probing depths in buccal or lingual positions or both,
clinical examination should include measures to make
fracture lines visible: application of dye solutions, the
use of fiberoptic light, inspection in the surgical mi-
croscope or endoscope and by a surgical flap. Pain on
selective loading of cusps may be an indication of root
fracture. A vertical root fracture should be anticipated
in root-filled teeth, which, after a long history of being
asymptomatic and without signs of endodontic infec-
tion, suddenly present with tenderness, pain symp-
toms and radiographic bone destruction (Fig. 14-20).
Roots with vertical root fracture usually have a hope-
less prognosis and should be extracted.
INFLUENCE OF EXTERNAL ROOT
RESORPTIONS
External resorption of roots normally progresses with-
out clinical symptoms and without causing periodon-
tal defects that can be mistaken for endodontic or
periodontal disease. However, in their advanced
stages they may interfere with the gingival sulcus and
cause the development of a periodontal abscess (Fig.
14-22). Since such lesions may be associated with both
increased pocket probing depths and drainage of pus
upon probing, this section of the chapter addresses
various forms of external root resorptions, their
mechanisms, clinical features and management.
Mechanisms of hard tissue resorption
The hard tissues of the body consist of two major
components, mineral and matrix. The ratio of these
two components varies between bone, cementum and
dentin, but the same tools — acids and enzymes — are
used by nature to monitor the degradation of these
tissues. Bone is normally remodeled to adapt to func-
334 • CHAPTER 14
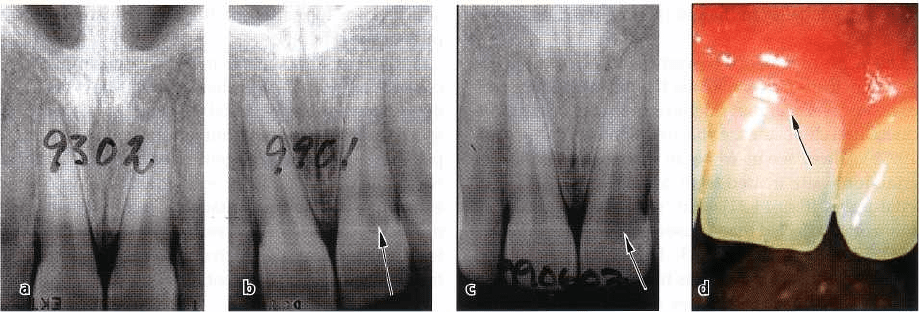
Fig. 14-22. Series of radiographs taken at different time periods showing the appearance of an external root resorp-
tion in a young adult patient (a-c). At the age of 15 years there is no sign of resorption (a). Six years later a small ra
diolucency is seen (arrow) (b). In just 6 months the lesion had expanded considerably (arrow) (c) and
appeared clinically as a pink area (arrow) (d). Courtesy of Dr Anders Molander.
tional changes, but as far as dental hard tissues in
permanent teeth are concerned resorption should be
seen as an expression of a pathological process. Bone
as well as cementum and dentin and also enamel,
when applicable, are resorbed by clast cells (Hammar-
strom & Lindskog 1992). Osteoclasts are large, multi-
nucleated, motile cells emanating from hematopoietic
precursor cells in the bone marrow (Marks 1983, Vaes
1988, Pierce et al. 1991). Mononucleated cells are also
involved when dental hard tissue is resorbed (Weden-
berg & Lindskog 1985, Lindskog et al. 1987, Sasaki et
al. 1990).
Under normal conditions, hard tissues are pro-
tected from resorption by their surface layers of blast
cells. It appears that as long as these layers are intact,
resorption cannot occur. It is known that hormonal
regulation of bone resorption is mediated by
osteoblasts (Chambers 1988). Stimulation by parathy-
roid hormone will make osteoblasts contract to expose
the bone surface for the osteoclasts (Jones & Boyde
1976, Rodan & Martin 1981). However, parathyroid
hormone exerts no influence on cementoblasts (Lind-
skog et al. 1987). This may explain why bone and not
teeth are remodeled to adapt to functional changes.
A denuded hard tissue surface attracts resorbing
cells. It has been suggested that the removal of the
organic matrix of bone will make it possible for phago
cytic cells to recognize the mineral component (Cham-
bers 1981). Thus it appears that the blast cell layer on
hard tissues forms a protective barrier that has to be
broken down to trigger osteoclastic activity. Under
clinical conditions various forms of damage can affect
the blast cell layer, e.g. trauma or excessive scaling and
root planing in periodontal therapy (Andreasen 1981).
Subsequent to the injury, mobile osteoclasts come and
seal themselves to the exposed hard tissue surface and
excrete acids into the extracellular environment under
their ruffled border to demineralize the tissue. This
event further creates the necessary acid environment
essential for the function of lysosomal enzymes with
low pH optima, to degrade the tissue matrix (Vaes
1968).
Conclusion
Two mechanisms are involved in resorption of a hard
tissue:
1. a trigger mechanism
2. a reason for the resorption to continue.
The trigger mechanism in root resorption is a root
surface detached from its protective blast cell layer.
Detachment may follow any damage to the cemen-
toblastic cell layer. For the resorption to continue, a
stimulus is required, e.g. an infection or a continuous
mechanical force such as the one in orthodontic treat-
ment. Consequently, the treatment of root resorption
should be directed towards the cause for the continu-
ance of the resorption, e.g. removal of infected mate-
rial in a root canal, or the halt of an orthodontic tooth
movement.
Clinical manifestations of external root
resorptions
Root resorptions
per se
do not cause painful symp-
toms. Unless a resorptive process is located coronally
and is undermining the enamel, giving it a pinkish
appearance (Fig. 14-22d), the only way to detect and
diagnose a dental resorption is by means of radiogra-
phy (Fig. 14-22a-c). If only one radiograph is taken it
is usually not possible to exactly define a radiolucent
area found inside the confines of a root. It may be a
resorptive process inside the root canal, or a radiolu-
cent resorptive defect located buccally or lingually
and superimposed on the image of the root. It may also
just be an artifact. Therefore, one should always take
more than one radiograph and use different angula-
tions to observe whether the radiolucent area belongs
to the root or not.
ENDODONTICS AND PERIODONTICS • 335
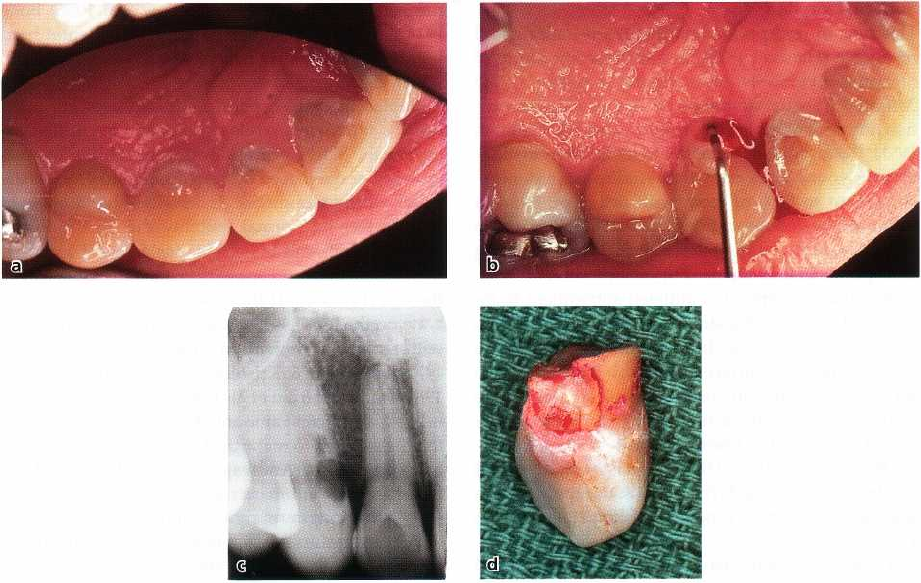
Fig. 14-23. Painful condition associated with a peripheral inflammatory root resorption (PIRR). The 30-year-old
male patient had experienced pain and tenderness of the right maxilla for several weeks (a). Clinically, all teeth
were sensible to pulp testing. Periodontal probing revealed pus drainage from the lingual aspect of tooth #13 (b).
An angulated radiograph revealed the presence of a resorptive defect (c). The tooth was deemed beyond
recovery and was extracted. An extensive resorptive defect had undermined the clinical crown (d).
Root resorptions always start at a surface and are
termed external if emanating from the root surface
and internal if initiated in the root canal wall. If the
radiolucent area is situated within the confines of the
root, at least two angulations or tomography are use-
ful to determine whether it is related to the root canal
or the root surface. If the outline of the root canal space
is clearly visible within the radiolucency, as in Figs.
14-22c and 14-23, this is a strong case for an external
origin. Due to its relatively rare occurrence internal
resorptions will not be further discussed in this chap-
ter.
The initial stage of a resorptive process usually
passes undetected as radiographs can only demon-
strate a resorptive cavity after a certain size has been
reached (Fig. 14-23a-c; Andreasen et al. 1987). The
location of the lesion is also important for the detec-
tion. A facial or lingual root resorption cavity is more
difficult to visualize radiographically than a proximal
cavity. Be aware that in the cervical region it may be
difficult to differentiate radiographically between
cavities caused by caries and those caused by resorp-
tion. Resorptive processes and caries develop by dif-
ferent mechanisms, which is useful for distinguishing
these lesions. Bacterial acids, which demineralize
dentin, create carious defects, but the organic part
will remain and render the cavity soft on exploration.
A simultaneous removal of the mineral phase and the
organic matrix of the hard tissue forms the resorptive
defect. This results in a cavity floor, which is hard on
probing.
Different forms of external root resorption
There are different forms of external root resorption.
The underlying mechanism is understood for some of
these, whereas other forms still remain unexplained.
In some instances external root resorptions appear to
be genetically linked, as
they
run in families. There are
also instances when only the enamel of an unerupted
tooth is being resorbed. Furthermore, external resorp-
tions can be caused by precipitation of oxalate crystals
in the hard tissues of patients as a result of increased
concentration of oxalates in the blood due to kidney
failure (Moskow 1989).
Andreasen (1981) has proposed a classification of
those external root resorptions that have a known
mechanism:
• Surface resorption
• Replacement resorption associated with ankylosis
• Inflammatory resorption associated with inflam-
mation in the periradicular tissues adjacent to the
resorption site.
Subforms are:
• Peripheral inflammatory root resorption (PIRR)
• External inflammatory root resorption (EIRR)
336 • CHAPTER 14
Surface resorption
This type of resorption is common, self-limiting and
reversible (Harding 1878). In a microscopic study of
human teeth in individuals varying in age from 16 to
58, only 10% of the teeth showed neither active resorp
tion nor signs of healed resorption (Henry &
Weinman 1951). Resorptions were noted twice as
often in older than in young subjects. Other studies
have demonstrated up to 88% of teeth with active or,
in most instances, healed resorptions (Hotz 1967).
Reports on surface resorptions are sparse as most are
self-limiting and spontaneously repaired upon injury.
A surface resorption is initiated subsequent to in-
jury of the cementoblastic cell layer. Osteoclasts are
attracted by substances from the damaged tissue on
the denuded root surface and resorb the hard tissue
for as long as activating factors are released at the site
of injury, usually for a few days (Hammarstrom &
Lindskog 1992). The resorptive process stops follow-
ing the disappearance of the osteoclasts and the defect
will become populated with hard tissue repairing cells
leading to cementum repair (Lindskog et al. 1983a,b,
1987).
These resorptions may be caused by a localized
injury in conjunction with external trauma (An-
dreasen 1981) and by trauma from occlusion. Resorp-
tion may also result from excessive orthodontic forces.
The mechanism of the latter kind of resorption is
thought to be a function of the hyaline zone that is
formed subsequent to the orthodontic compression of
the periodontal ligament. Along with the resorption
of the hyaline layer, clast cells will resorb the root
surface for as long as the orthodontic force is in place.
Major loss of dental hard tissue giving root fore-
shortening may occur from this kind of iatrogenic
injury.
Conclusion
The large majority of teeth show signs of active or
healed surface resorptions or both. It is conceivable
that minor traumata caused by unintentional biting on
hard objects, bruxism, high fillings, etc., cause lo-
calized damage to the periodontal ligament and trig-
ger the initiation of this type of resorption. The process
is self-limiting and self-healing – no active treatment
is required. During orthodontic treatment caution
should be exercised in monitoring the forces to mini-
mize the risk of foreshortening of roots.
Replacement resorption
This type of resorptive process results in a replace-
ment of the dental hard tissues by bone, hence the
name (Andreasen 1981). When a surface resorption
stops, cells from the periodontal ligament will prolif-
erate and populate the resorbed area (Lindskog et al.
1983a,b, 1987). If the resorption is large it will take
some time for the PDL cells to cover the entire surface.
Cells from the nearby bone tissue may then arrive first
and establish themselves on the resorbed surface (An-
dreasen & Kristersson 1981, Gottlow et al. 1986). Bone
is thus being formed directly upon the dental hard
tissue. This results in a fusion between bone and tooth
which is known as ankylosis.
Replacement resorption and ankylosis are often
used as synonyms. While replacement resorption de-
scribes the active process during which the tooth is
resorbed and replaced by bony tissue, ankylosis is the
Greek word for immobile. It describes the situation of
a tooth lacking normal mobility due to the fusion
between tooth and bone. This fusion can be perma-
nent or transient and appears to depend on the size of
the resorbed area. If the ankylotic area is small, the
bone on the tooth surface can resorb and be replaced
with reparative cementum (Andreasen & Skougaard
1972, Andreasen & Kristersson 1981, Andersson et al.
1985, Hammarstrom et al. 1986). If the ankylotic area
is large, a sufficient amount of bone will be formed on
the root surface to make the fusion between bone and
tooth permanent (Andreasen 1981, Andreasen & Kris-
tersson 1981, Hammarstrom et al. 1986). It has been
shown that long-term rigid splinting following exter-
nal trauma results in a higher incidence of dentoalveo-
lar ankylosis than with a short-term, less rigid fixa-
tion. The latter allows for some movement during the
splinting period and probably prevents ankylosis (
Andreasen 1975).
Clinically, ankylosis is diagnosed by absent tooth
mobility and by a percussion tone that is higher than
in a normal tooth (Andreasen 1975, Andersson et al.
1985). Radiographically, a local disappearance of the
periodontal ligament contour may show an initial
stage of fusion. However, even in non-ankylosed teeth
it is not always possible to observe the entire contour
of the periodontal ligament. Percussion and tooth mo-
bility testing appear therefore more sensitive diagnos-
tic tools than radiography in the early stages of re-
placement resorption (Andersson et al. 1985). When
dentoalveolar ankylosis occurs at a young age, the
tooth will not erupt but will follow the growth pattern
of the bone resulting in so-called infra-occlusion (An-
dreasen & Hjorting-Hansen 1966, Kiirol 1984, Malm-
gren et al. 1984).
The formation of bone on a dentin surface is not
necessarily a pathological process, but one to be re-
garded as a form of repair. The bone has accepted the
dental hard tissue as a part of itself and the tooth
becomes involved in the normal skeletal turnover (
Loe & Waerhaug 1961, Hammarstrom et al 1986). The
turnover phase is fast in the growing child, but slower
in the adult individual. Hence, the rate of bone re-
placement follows this pattern. However, the detailed
mechanism of the resorptive process is not clearly
understood.
Conclusion
Ankylosis is a prerequisite for replacement resorption.
It may be seen as a form for repair of root surface
ENDODONTICS AND PERIODONTICS • 337
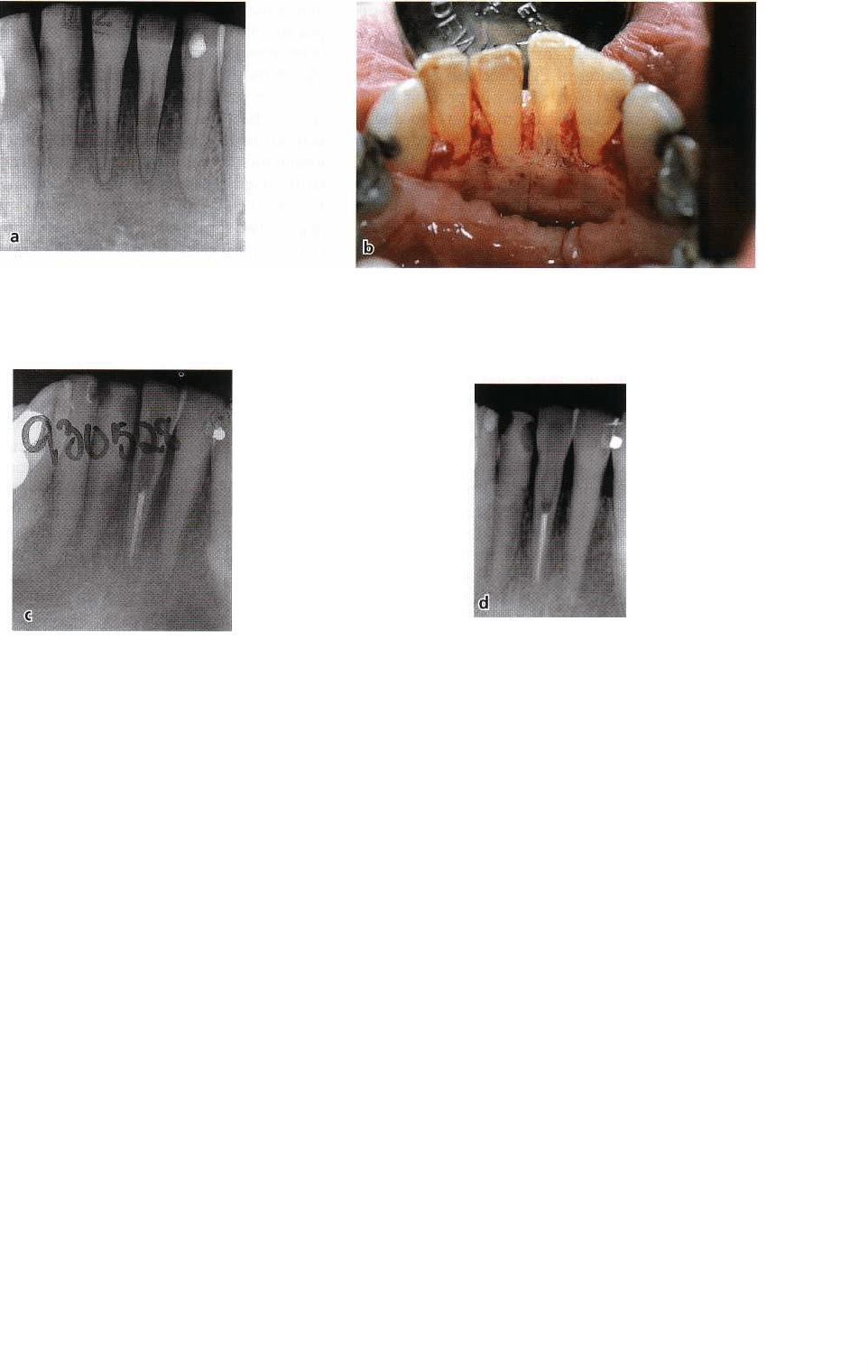
Fig. 14-24. Radiograph from a 78-year-old lady who presented herself to the clinic after an episode of severe pain
and with a lingual periodontal abscess (a). The medical history was unremarkable. Radiograph revealed external
root resorption on the lingual aspect of both the central incisors (a). The patient was initially managed by antibiotic
treatment. Upon flap elevation and accessing the resorbing area and removing the granulation tissue an exposure
to a necrotic pulp of tooth #31 was noted (b). Endodontic treatment was carried out during the surgery
procedure (c). Tooth #41 was left without any further treatment and the case was followed clinically and
radiographically. No recurrence of resorption occurred on either tooth and the patient has remained comfortable.
Radiograph at the last follow-up 8 years after treatment (d). Note that there is no obvious progression of the
resorptive process associated with tooth #41.
resorptions, which from a clinical standpoint is not
desirable. No treatment for this condition is available.
External inflammatory resorption
The term external inflammatory resorption suggests
the presence of an inflammatory lesion in the peri-
odontal tissues adjacent to a resorptive process (An-
dreasen 1985). There are two main forms — peripheral
inflammatory root resorption (PIRR) and external in-
flammatory root resorption (EIRR). Both forms are
triggered by a destruction of the cementoblasts and the
cementoid. In PIRR the factors activating osteoclasts
are thought to be provided by an inflammatory lesion
in the adjacent periodontal tissues (Andreasen 1985,
Gold & Hasselgren 1992). EIRR, on the other
hand, receives its stimulus from an infected necrotic
pulp (Andreasen 1985, Andreasen & Andreasen 1992).
Peripheral inflammatory root resorption (PIRR)
The outstanding feature of this type of resorption is its
cervical location and invasive nature (Heithersay
1999a). It has therefore been termed invasive cervical
root resorption. However, in the adult, the periodontal
tissue may have receded apical to the cervical area.
Therefore, other names have been used for this lesion
such as subosseous resorption (Antrim et al. 1982) and (
the complete opposite) supraosseous extra-canal in-
vasive resorption (Frank & Bakland 1987). The differ-
ent names reflect the confusion that has surrounded
this type of resorptive lesion. Since the resorptive
process extends into the dentin peripherally towards
338 • CHAPTER 14
the pulp, and the clast activating factors seem to ema-
nate from a periodontal inflammatory lesion, a name
which reflects the etiology of this phenomenon, pe-
ripheral inflammatory root resorption (PIRR), was
proposed (Gold & Hasselgren 1992).
The clinical features of PIRR include granulation
tissue formation that bleeds freely on probing. Occa-
sionally, a periodontal abscess may develop due to
marginal infection, which may mimic a periodontal or
endodontic condition (Fig. 14-23). When the lesion is
located more apically or proximally, probing is usu-
ally difficult. Radiographically the lesion may only be
seen after a certain size has been reached (Fig 14-22).
Sometimes the appearance is mottled due to forma-
tion of hard tissue within the resorptive defect (Se-
ward 1963). The outline of the root canal can often be
seen within the radiolucent area (Fig. 14-22c). The
presence of a profuse bleeding upon probing and
granulation tissue in combination with a hard cavity
bottom confirm the diagnosis. Electric pulp test and
cold tests are usually positive, but will not distinguish
this condition from caries or internal resorption,
which are the two major differential diagnostic op-
tions (Frank & Bakland 1987).
The mechanism for this form of resorption is far
from completely understood. Predisposing factors
seem to be orthodontic treatment, trauma and intra-
coronal bleaching, while periodontal therapy took a
low incidence among 222 examined cases (Heithersay
1999b). The reason for the low incidence following
periodontal treatment could be that even upon exces-
sive scaling and root planing, the damaged area of the
root surface usually becomes covered by junctional
epithelium. Yet, it appears that in the presence of a
periodontal inflammatory lesion the onset of a resorp-
tive process is triggered and that its continuance has
an infectious cause (Brosjo et al. 1990, Gold & Hassel-
gren 1992).
Unmineralized, newly formed tissue in cementum (
Gottlieb 1942), in osteoid (Chambers et al. 1985), and
in predentin (Stenvik & Mjor 1970) has been observed
to be resistant to resorption. This seems to explain the
pattern of progression this form of resorption nor-
mally takes as it avoids invasion of the pulp and
expands laterally instead. Yet, this peripheral exten-
sion can markedly undermine the tooth structure (Fig.
14-23). If there is a non-vital pulp and thus no resorp-
tion inhibition in the form of odontoblast supported
predentin, PIRR will go straight to the pulpal space (
Fig. 14-24). In root-filled teeth, which have been sub-
jected to intracoronal bleaching, tissue toxic bleaching
agents such as hydrogen peroxide have been found to
be capable of penetrating through dentin and cemen-
turn (Fuss et al. 1989). If this occurs under clinical
conditions, damage will be inflicted upon the peri-
odontal ligament cells and cause resorption (Har-
rington & Natkin 1979, Montgomery 1984). Sub-
sequently, bacteria may colonize the chemically emp-
tied dentinal tubules and maintain inflammation and
the resorptive process (Cvek & Lindvall 1985).
The most common form of treatment for PIRR is
surgical exposure of the area, including removal of the
granulation tissue. A base material is subsequently
placed followed by a permanent filling and suturing
of the flap. Other treatment forms include reposition-
ing of the flap apical to the filling or orthodontic
extrusion of the tooth (Gold & Hasselgren 1992). Re-
cently, it has been suggested that guided tissue regen-
eration can be used, after surgical removal of the
granulation tissue, to promote ingrowth of periodon-
tal ligament cells into the resorbed area (Rankow &
Krasner 1996). This kind of resorption may also be
approached from within the tooth structure. Usually
pulpectomy is required. To aid in removal of the resor
bing tissue the use of 90% aqueous solution of
trichloracetic acid has been proposed (Heithersay
1999c).
External inflammatory root resorption (EIRR)
This type of resorption is usually a complication that
follows a dental trauma. It begins as a surface resorp-
tion due to damage of the periodontal ligament and
the root surface in conjunction with the traumatic
injury. The stimulus for EIRR is infectious products
released into the adjacent tissues by way of the denti-
nal tubules exposed by the resorption (Bergenholtz
1974, Andreasen 1985, Andreasen & Andreasen 1992).
The bacterial components will then maintain an in-
flammatory process in the adjacent periodontal tis-
sues that in turn will trigger the continuance of the
resorption. The osteoclastic resorption, basically
aimed at eliminating the irritants, will thus move in
the direction of the infected pulp tissue. As dentin is
being further resorbed, more infectious and inflam-
matory byproducts are released into the surrounding
area, thus perpetuating the inflammatory reaction and
the resorptive process (Andreasen 1985).
The earliest stages are usually hard to detect as the
resorptive cavity needs to reach a certain size to be-
come radiographically visible. The first radiographic
signs of resorption following trauma cannot usually
be seen for several weeks (Andreasen et al. 1987).
Treatment will be directed towards the cause of the
resorption, that is, the root canal infection (Cvek 1993).
In this context the use of calcium hydroxide has been
advocated (Cvek 1993) as it is a useful antibacterial
intracanal medicament (Bystrom et al. 1985). Calcium
hydroxide also aids the cleaning of the canal by its soft
tissue dissolving capability (Hasselgren et al. 1987),
thus eliminating sources for bacterial nutrition. How-
ever, the positive effect of any medicament appears to
be secondary to the elimination of root canal infection.
Hence, clinical follow-ups suggest no difference in
outcome between teeth treated long-term with cal-
cium hydroxide and teeth subjected to instrumenta-
tion and filling with gutta-percha (Cvek 1973).
Conclusion
Peripheral inflammatory root resorption (PIRR) and
external inflammatory root resorption (EIRR) are two
ENDODONTICS AND PERIODONTICS • 339
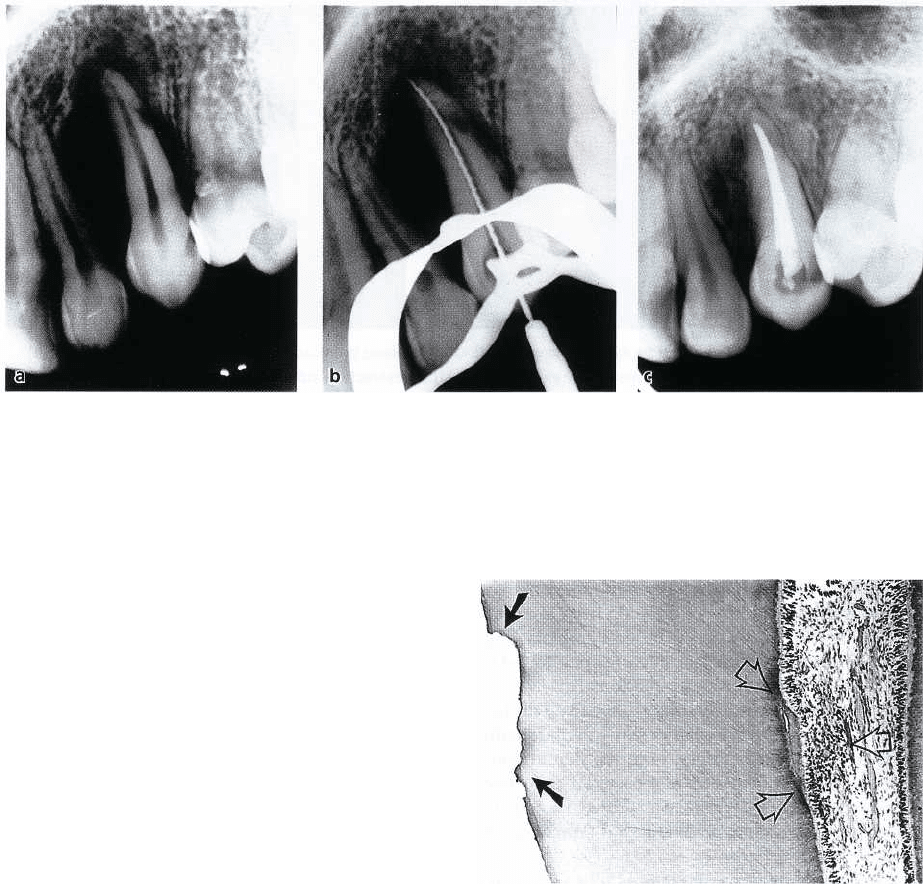
Fig. 14-25. Radiographs from a 27-year-old woman, showing the left maxillary canine which had been autotrans
planted into a surgically prepared socket 2 months earlier. External inflammatory root resorption (EIRR) is
visible on the distal aspect of the root (a). Endodontic treatment was initiated (b) and following the preparation
of the canal, calcium hydroxide was placed as a long-term dressing. Radiograph following root filling (c) shows
that the external resorption cavity is more rounded and a periodontal contour can be seen between the root and
bone which has grown into the prepared socket.
forms of progressing external root resorption associ-
ated with inflammation in the periodontal tissues. The
mechanism of EIRR is thought to be the release of
bacterial elements from an infected pulp devitalized
in conjunction with trauma. By focusing the treatment
on the endodontic infection the resorption can usually
be stopped as this takes away the reason for the con-
tinuance of the resorption (Fig. 14-25). In the sub-
sequent healing phase there is risk of ankylosis. The
greater the resorbed area, the greater is the risk for this
complication (Andreasen & Kristersson 1981, Gottlow
et al. 1986).
INFLUENCE OF PERIODONTAL
DISEASE ON THE CONDITION OF
THE PULP
The formation of bacterial plaque on detached root
surfaces following periodontal disease has the poten-
tial to induce pathologic changes in the pulp along the
very same pathways as an endodontic infection can
affect the periodontium in the opposite direction.
Thus, bacterial products and substances released by
the inflammatory process in the periodontium may
gain access to the pulp via exposed lateral canals and
apical foramina, as well as dentinal tubules.
A clearcut relationship between progressive peri-
odontal disease and pulpal involvement, however,
does not invariably exist. In fact, while inflammatory
alterations as well as localized necrosis of pulp tissue
have been observed adjacent to lateral canals in teeth
exposed by periodontal disease (Seltzer et al. 1963a,
Rubach & Mitchell 1965), a number of clinical studies
Fig. 14-26. Histologic section of a monkey tooth ex-
posed to experimental periodontal tissue breakdown.
Beneath resorptive defects in the external root surface a
slight infiltrate of inflammatory cells and a small rim of
reparative dentin are observed in the pulp. From Ber-
genholtz & Lindhe (1978).
have failed to confirm a direct correlation between
periodontal disease and pulp tissue changes (Mazur &
Massler 1964, Czarnecki & Schilder 1979, Torabine-
jad & Kiger 1985). In a study in monkeys, Bergenholtz
& Lindhe (1978) observed the nature and frequency of
tissue changes in the pulp of teeth following an experi-
mentally induced breakdown of the attachment appa-
ratus. They found that the majority of the root speci-
mens examined (70%) exhibited no pathologic pulp
tissue changes, despite the fact that approximately
30-40% of the periodontal attachment was lost. The
remaining roots (30%) displayed only small inflam-
matory cell infiltrates and/or formations of reparative
dentin in areas of the pulp subjacent to root areas
exposed through the periodontal tissue destruction.
340 • CHAPTER 14
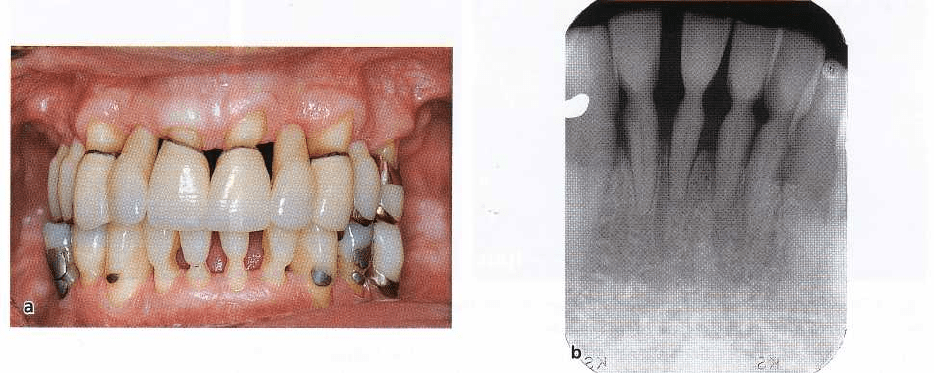
Fig. 14-27. Case of a lower second molar with severe periodontal tissue breakdown and furcation involvement (
a) that was extracted and subjected to histologic examination. Upon extraction substantial amounts of calculus is
seen on the distal root surface (b). While there was bacterial accumulation on the cementum layer (c), the pulp
tissue has remained functional and without inflammatory involvement (d). Courtesy of Dr Domenico Ricucci.
These tissue changes were frequently associated with
root surface resorption (Fig. 14-26), suggesting that
dentinal tubules have to be uncovered before irritation
can be transmitted. This observation further suggests
that the presence of an intact cementum layer is im-
portant for the protection of the pulp from injurious
elements produced by the plaque microbiota (Fig. 14-
27). Consequently, the lack of correlation found in
clinical observations between periodontal disease and
pulp tissue alterations may simply depend on the fact
that few open pathways exist in many periodontally
involved teeth. Furthermore, once the dentin/pulp
complex has been exposed to a bacterial challenge,
repair and healing will often be instituted, leaving the
remaining tissue relatively unaffected (Warfvinge &
Bergenholtz 1986, Bergenholtz 2000).
In the study by Bergenholtz & Lindhe (1978), de-
structive periodontal disease was produced experi-
mentally during a comparatively short period (5-7
months), while in humans a similar degree of destruc-
tion of periodontal tissue normally requires several
years. It has been reported that the pulp of teeth with
long-standing periodontal disease develops fibrosis
and various forms of mineralizations (Fig. 14-1;
Bender & Seltzer 1972, Lantelme et al. 1976). The
number of blood vessels and nerve fibers can also be
reduced. It seems reasonable that tissue changes of
this nature represent the accumulated response of the
pulp to the relatively weak, but repeatedly occurring,
insults of the tissue via exposed dentinal tubules and
lateral canals.
Conclusion
It seems that periodontal disease rarely jeopardizes
the vital functions of the pulp. In teeth with moderate
breakdown of the attachment apparatus, the pulp
usually remains in proper function. Breakdown of the
pulp presumably does not occur until the periodontal
disease process has reached a terminal state, i.e. when
bacterial plaque involves the main apical foramina
(Langeland et al. 1974). Apparently, as long as the
blood supply through the apical foramen remains
intact, the pulp is capable of withstanding injurious
elements released by the lesion in the periodontium.
INFLUENCE OF PERIODONTAL
TREATMENT MEASURES ON THE
PULP
Scaling and root planing
Scaling and root planing are indispensable procedures
in the treatment of periodontal disease. However, not
only will bacterial deposits be removed from the root
surface but so also may cementum and superficial
parts of dentin. Therefore, by this instrumentation,
dentinal tubules will be exposed and normally left
unprotected to the oral environment. Subsequent mi-
crobial colonization of the exposed root dentin may
result in bacterial invasion of the dentinal tubules (
Adriaens et al. 1988). As a consequence, inflamma-
tory lesions may develop in the pulp (Bergenholtz &
Lindhe 1978). Yet, the vitality of the pulp is not nor-
mally put at risk (Bergenholtz & Lindhe 1978, Nilveus
& Selvig 1983, Hattler & Listgarten 1984), even though
root dentin hypersensitivity frequently develops fol-
lowing such measures, presenting an uncomfortable
and difficult problem to manage (see below).
During the maintenance phase of periodontal ther-
apy, scaling and planing of roots are frequently re-
peated procedures. At each recall session, the root
surfaces are debrided and some dentin is removed.
This therapy can result not only in weakening of the
tooth structure but also in extensive reparative dentin
formation in the pulp (Fig. 14-28). Whether such repair
processes impair pulp functions on a long-term basis
is not well studied. In a patient material subjected to
ENDODONTICS AND PERIODONTICS • 341
Fig. 14-28. Clinical photograph of a patient, who has been in the maintenance phase after treatment for periodontal
disease (a). While there are excellent gingival conditions and no pocket probing depths, there is substantial loss of
cervical root dentin. One of the lower incisors later fractured off, but without a pulpal exposure due to accumula
tion reparative dentin in the coronal portion of the pulp chamber (b). Courtesy of Dr Sture Nyman.
maintenance therapy for over 4-13 years, pulp tissue
necrosis was a rare finding (3%), and, when occurring,
it was attributed to caries and progression of peri-
odontal disease rather than to the periodontal treat-
ment
per se
(Bergenholtz & Nyman 1984). On rare
occasions deep periodontal scaling may expose lateral
canals that in turn can induce severe painful symp-
toms of pulpitis.
Conclusion
Results of clinical observations and animal experi-
ments support the view that scaling and root planing
procedures normally do not threaten the vitality of the
pulp. Adjacent to instrumented root surfaces localized
inflammatory alterations may on occasion emerge,
but in most instances these will be followed by repair
processes. (Figs. 14-1, 14-28b).
Root dentin hypersensitivity
Patients subjected to scaling and root planing in peri-
odontal therapy may after the instrumentation proce-
dure experience increased sensitivity of the treated
teeth to evaporative, tactile, thermal and osmotic stim-
uli (Fischer et al. 1991, Kontturi-Narhi 1993, Chaban-
ski et al. 1996). Usually, the symptoms, when occur-
ring, develop and peak during the first week to sub-
side or disappear within the subsequent weeks and
are, although uncomfortable, most often a temporary
and sustainable complication. However, occasionally
the condition may become a chronic pain problem and
may persist for months or years. Patients appear to be
especially at risk after periodontal surgery. In a com-
prehensive questionnaire survey, severe painful
symptoms were reported to prevail in 26% of the
subjects 6 months to 5 years after the completion of
treatment, while 16% treated non-surgically had pain
symptoms (Kontturi-Narhi 1993). In a clinical trial
comprising 35 patients, Tammaro et al (2000) observed
that, while a majority of patients subjected to non-sur-
gical periodontal instrumentation developed sensi-
tive teeth, only a few teeth in a small number of the
patients developed highly sensitive root surfaces.
The main initial symptom is sharp pain of rapid
onset that disappears once the stimulus is removed. In
more severe, long-standing cases, shorter or longer
periods of lingering, dull or aching pain symptoms
may be provoked. Even a minimal contact of a tooth-
brush with the root dentin surface may result in in-
tense pain – a condition not only uncomfortable but
one likely to hinder proper oral hygiene measures.
The pain condition is termed dentin hypersensitiv-
ity (Holland et al. 1997). But the ailment has also been
given many other names such as sensitive dentin,
cervical dentinal sensitivity and root sensitivity,
which reflect the confusion that still exists regarding
its etiologic background (Orchardson et al. 1994). The
fact that root surfaces become sensitive to a variety of
externally derived stimuli after periodontal instru-
mentation is not surprising as dentinal tubules be-
come uncovered to the oral environment and subject
to hydrodynamic forces. Hence, a variety of pain-
evoking stimuli including evaporative, tactile, ther-
mal and osmotic stimuli may elicit sudden fluid shifts
in the exposed tubules thereby inducing a painful
sensation according to the hydrodynamic theory of
dentin sensitivity (Brannstrom 1966, Pashley 1996).
This mechanism alone can certainly explain the sensi-
tivity patients experience immediately after the in-
strumentation procedure and during a short period
afterwards, while it does not make clear why the
symptoms increase over time and why the pain con-
dition may prevail in certain patients and in certain
teeth.
The increase in pain intensity may have one or both
of the following two explanations. Firstly, the smear
layer formed on the root surface by the scaling proce-
342 • CHAPTER 14
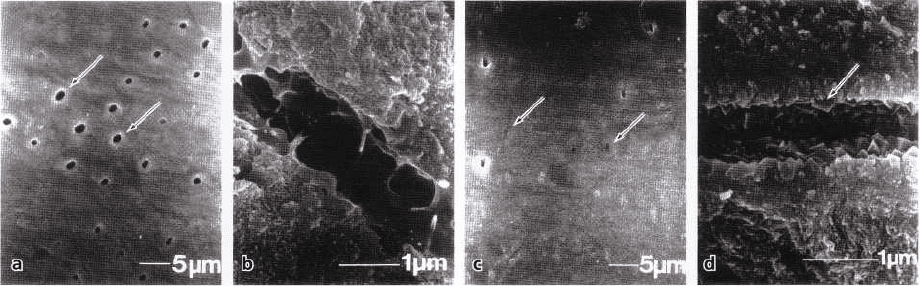
Fig. 14-29. Scanning electron microscopic images of specimens of hypersensitive (a, b) and non-sensitive root
dentin areas of human teeth (c, d). In (a) there are numerous wide tubular apertures. These tubules show no
evidence of hard tissue depositions after being fractured open (b). Most tubules are occluded (c) and below the
surface rhombohedral crystals of from 0.1-0.3 µm are present (d). The images are kindly provided by Dr
Masahiro Yoshiyama and published with permission of the
Journal of Dental Research.
dure will be dissolved within a few days (Kerns et al.
1991). This in turn will increase the hydraulic conduc-
tance of the involved dentinal tubules (Pashley 1996)
and thus decrease the peripheral resistance to fluid
flow across dentin. Thereby pain sensations are more
readily evoked. Secondly, open dentinal tubules serve
as pathways for diffusive transport of bacterial ele-
ments in the oral cavity to the pulp, which is likely to
cause a localized inflammatory pulpal response (Ber-
genholtz & Lindhe 1975, 1978). Indeed, experiments
in dogs have shown that pulpal inflammation greatly
enhances the sensitivity of responding nerve fibers (
Narhi et al. 1994). A large number of intradental A-
delta fibers, normally inactive, are now able to re-
spond upon stimulation (Nth-hi et al. 1996). It has
furthermore been shown that the receptive field of
individual fibers gets wider (Narhi et al. 1996). In
addition, shallow oral exposures of root dentin in the
rat are accompanied by sprouting of new terminal
branches from pulpal axons in areas subjacent to the
root surface injury (Taylor et al. 1988). Sprouting of
nerves is a temporary event and will subside if inflam-
mation disappears – a feature consistent with their
involvement in root dentin hypersensitivity (Byers &
Narhi 1999). In other words, an essential component
of the increasing root sensitivity that patients experi-
ence after an instrumentation procedure in periodon-
tal therapy is likely to be related to a peripheral sensi-
tization of pulpal nociceptors due to release of inflam-
matory mediators.
The fact that root dentin hypersensitivity often dis-
appears a few weeks after the scaling procedure is best
explained by the development of a natural occlusion
of the exposed dentinal tubules by mineral deposits (
Fig. 14-29; Yoshiyama et al. 1989, 1990). The hydrody-
namic mechanism for dentinal pain will thereby be
inactivated. Furthermore, the potential for an inward
diffusion of bacterial elements to the pulp will be
substantially reduced. The observations of few if any
open tubules in non-sensitive radicular dentin (Hiatt
& Johansen 1972, Absi et al. 1987, Yoshiyama et al.
1989, Cuenin et al. 1991, Oyama & Matsumoto 1991,
Kontturi-Narhi 1993), while hypersensitive root areas
show large numbers of tubular apertures on their
surfaces (Absi et al. 1987, Yoshiyama et al. 1989,
Cuenin et al. 1991, Oyama & Matsumoto 1991,
Kontturi-Narhi 1993), support this view.
The fact that only certain individuals become seri-
ously affected may be related to local factors in the oral
cavity, as well as to the level of the subjects' pain
perception. Certain dietary factors, in particular fruit
juices, yoghurt and wines, have been implicated in the
pathogenesis of dentin hypersensitivity (Addy et al.
1987). By their acidity and ability to etch dentin, natu
ral occlusions of dentinal tubules by mineralizations
may thus be dissolved or prevented from forming. It
needs also to be recognized that pain is not only an
expression of injury and noxious stimuli, but also a
psychobiological phenomenon having both a physi-
ological and psychological basis for its perception and
reaction to it. Indeed, a variety of emotional elements
may influence the subjective interpretation of pain (Eli
1992), and anxiety, fear and depression are factors that
are known to affect pain perception and the subject's
ability to identify coping methods (McGrath 1994).
A further factor that is potentially involved in the
symptomatology associated with root dentin hy-
persensitivity is the enhancement of the responsive-
ness of the central nervous system. Indeed it has been
shown that neuroplastic changes in the central no-
ciceptive pathways, including expanded receptive
fields and heightened excitability, may occur follow-
ing peripheral injury and inflammation (see review by
Sessle 2000). Such changes may be maintained even if
peripheral sensitization phenomena are bypassed and
seem to become more prominent in long-lasting pain
conditions (Sessle 2000).
In cases of severe root dentin hypersensitivity, ac-
tive treatment is urgent. However, the methods pres-
ently available provide an unpredictable remedy and
only temporary relief is at best attained (Orchardson
et al. 1994, Ikola 2001). Since tubular patency seems to
