Fisher John P. e.a. (ed.) Tissue Engineering
Подождите немного. Документ загружается.

mikos: “9026_c027” — 2007/4/9 — 15:53 — page 14 — #14
27-14 Tissue Engineering
(4) architectural differences and relative position between implant and host tissue. Understanding how
normal functioning of the cardiac cell network changes with the presence of different types of cellular,
structural, and functional heterogeneities is a necessary step in the design of safer and more efficient cell
and tissue transplantation therapies.
For example, it is already known from computational and experimental studies that contact between
two cells with different resting potentials (e.g., injured and healthy cell [130]) or action potential durations
(e.g., purkinje and ventricular cell [131], epicardial and M cell [132]), may trigger afterdepolarizations or
create conduction block depending on the degree of their electrical coupling. It is also known that partial
decoupling between the cells may actually increase the safety of propagation [133,134] as is the case in
transverse vs. longitudinal propagation in healthy cardiac muscle [47]. On the other hand, excessive gap
junction decoupling [134], presence of fibrotic regions [135], geometrical expansions [136], and repetitive
tissue branching [137] (e.g., sparse cardiac network in ischemic or infarcted area [138]) can yield extreme
slowing of impulse propagation and occurence of conduction block and introduce the susceptibility of
cardiac tissue to formation of micro- or macroreentrant circuits. In the ideal world, the safest and most
efficient therapy would be to engineer a cardiac patch that exactly mimics the geometry, architecture, and
function of the “missing region” in the heart, and to perfectly couple it to the host tissue, as “a piece of
the jigsaw puzzle.” In the “semi-real” world, even if one is to produce a patch with perfect anisotropic
architecture, its optimal orientation relative to host tissue when implanted may change depending on
the electrical differences between the donor and host cells, or capability of patch to couple with the host
tissue. In the real world, things are very complex due to interplay of many factors. For example, the use of
skeletal myoblasts or stem cell-derived cardiomyocytes may demand different patch design and different
implantation strategy as determined by the functional differences between these cell types (e.g., shorter vs.
longer action potential, different resting potentials, none vs. significant expression of gap junctions, etc.).
The simulation may be further complicated by the presence of a fibrous capsule at the implantation site.
Due to the complexity of the problem, carefully designed studies on possible implantation scenarios will
be crucial as a prescreening tool before the actual implantation. The author’s view is that there are at least
two simplified settings that could be used to systematically and reproducibly study the factors affecting the
likelihood of arrhythmia arising from cell and tissue cardiomyoplasty. One is the use of micropatterned
cocultures [139,140] of host cardiomyocytes and different types of donor cells or mixtures of donor
cells, with the possibility for well-controlled studies based on (1) simplified cellular composition and
tissue architecture compared to the 3D heart, (2) precise control of the cell microenvironment, cellular
geometry and distribution, and geometry of cellular interactions between donor, host, and donor and
host cells, and (3) the possibility to optically assess and exactly correlate electrical/mechanical activity
and underlying tissue architecture at microscopic and macroscopic spatial scales. Optical mapping of
transmembrane potentials and intracellular calcium [141] are well-suited not only for these studies, but
also for electrophysiological evaluation of engineered cardiac patch pre and postimplantation ex vivo.
The other setting is the use of computer models that incorporate cell-specific membrane properties, cell
geometry, distribution of intercellular connections, and discrete tissue microarchitecture. With increase
in computing efficiency, these detailed models could be used as counterparts to different in vitro or in vivo
implantation scenarios to help interpretation and design of experiments, and eventually yield safe and
efficient therapies.
27.4.6 Spontaneous Activity
Another electrophysiological parameter for consideration is a somewhat misinterpreted presence of
spontaneous contractile activity in cardiac cell cultures. It is important to understand that although
spontaneous contractions in cardiac cultures represent convenient way to visually identify cardiac cells,
they are by no means a physiologically normal state for adult or neonatal ventricular muscle (which is most
often the source tissue for cell dissociation). While early embryonic ventricular cells still spontaneously
depolarize and contract [142], their resting potential hyperpolarizes with maturation such that neonatal
ventricular cells already exhibit steady resting potentials (less than −70 mV), fast action potential upstroke

mikos: “9026_c027” — 2007/4/9 — 15:53 — page 15 — #15
Cardiac Tissue Engineering 27-15
(more than 100 V/sec), and no spontaneous activity [76,142,143]. Rather, spontaneous activity of cardiac
cells observed in vitro is an artifact of the cell culture possibly caused by (1) membrane depolarization
due to cell injury during or after dissociation, (2) dedifferentiation of cultured cells to more embryonic
state due to presence of high serum and inadequate media formulation, (3) large presence of nodal or
other pacemaking cells due to unselective cell dissociation, and/or (4) decreased intercellular coupling
compared to native tissue due to 2D or sparse 3D arrangement of ventricular cells. The first three causes
can be alleviated with time in culture, proper cultivation conditions, and careful cell dissociation. How-
ever, the sparse cardiac network, if present, will always result in less electrotonic load “seen” by a cell and
facilitate propagation from single or small group of pacemaking cells into the quiescent tissue, favoring
spontaneous activity [144,145]. Our observations that spontaneous contractions in cardiac constructs
can be more readily observed when cells are less coupled (e.g., at lower seeding density, in the beginning
of cultivation, or on the perturbing polymer fibers at the edges of the tissue construct) are in agreement
with this reasoning. After 5 to 7 days in culture, tissue constructs in our studies usually become quiescent,
presumably due to increased packing density and connectivity of cardiac cells. The low percentage of
nonmyocytes in tissue constructs as assessed by immunostaining, and increase in conduction velocity
between culture days 4 and 7, exclude fibroblast overgrowth as a possible cause of cardiac cells quiescence.
Although reported spontaneous beating rates in cardiac constructs are usually lower than regular heart
rate, presence of paracrine chronotropic factors (e.g., epinephrine, adrenaline) after implantation in
the heart may result in faster activity and possible arrhythmogenic hazard. For electrical safety reasons,
a nonstimulated ventricular cardiac patch should be electrically quiescent, but readily excitable and fast
conducting, similar to native ventricular muscle. Moreover, a quiescent avascular patch may have lower
metabolic demand and increased chance for survival after implantation compared to a spontaneously
contractile patch. However, persistent contractions and presence of mechanical load are essential for
maintenance of ventricular mass in vivo [146], and for cell hypertrophy [147], spreading to confluence
[148], and establishment of cell contacts in vitro [149,150]. (Our experience is that if cardiac cell culture
is noncontracting for more than 3 days, cells start to atrophy and loose cell contacts.) Therefore, spontan-
eously quiescent engineered cardiac constructs still need to be maintained mechanically active in culture
either by use of electrical, mechanical, or chemical (e.g., small concentrations of epinephrine) stimulation
[150], or by coculture with spatially distinct population of pacemaking cells, which can be easily dissected
before the implantation in the ventricle.
In any case, thorough evaluation of electrical properties and susceptibility to conduction block and
arrhythmic behavior should be routinely done in cultured cardiac constructs and used as one of the
tissue design criteria. From our experience, it is important to assess the properties of engineered tissue in
challenging regimes such as fast or premature stimulation, similar to standard clinical pacing protocols for
testing the susceptibility to arrhythmias [151]. Forexample, a tissue construct can support macroscopically
continuous and relatively fast electrical propagation at low pacing rates, but yield conduction blocks and
high incidence of reentrant arrhythmias [122] when paced rapidly (Figure 27.4) due to large spatial
dispersion of refractoriness, or abundance of microscopic anatomic heterogeneities.
27.5 Future Work
The crucial technical aspect of this and all other cell-based therapies will be a choice of appropriate cell
source, which is to be primarily determined by developmental biologists, geneticists, and immunologists.
Engineering of a functional cardiac tissue patch using embryonic or adult stem cells and subsequent
implantation studies are still to be done. Simultaneous efforts on design of appropriate scaffolds and
control over the cellular connectivity and tissue architecture in three dimensions will be essential to the
development of functional cardiac patch for use in laboratory and clinics. Systematic in vitro and in vivo
studies on the role of heterogeneities on structure and function of cardiac tissue will help in designing more
efficient and safer therapies. Possible engineering of the patent capillary- and microcapillary-like networks
inside the tissue constructs may enable culture of thick tissue slices, and facilitate immediate perfusion
mikos: “9026_c027” — 2007/4/9 — 15:53 — page 16 — #16
27-16 Tissue Engineering
0 ms 40 140
240 340 420
(a)
(b)
200 ms
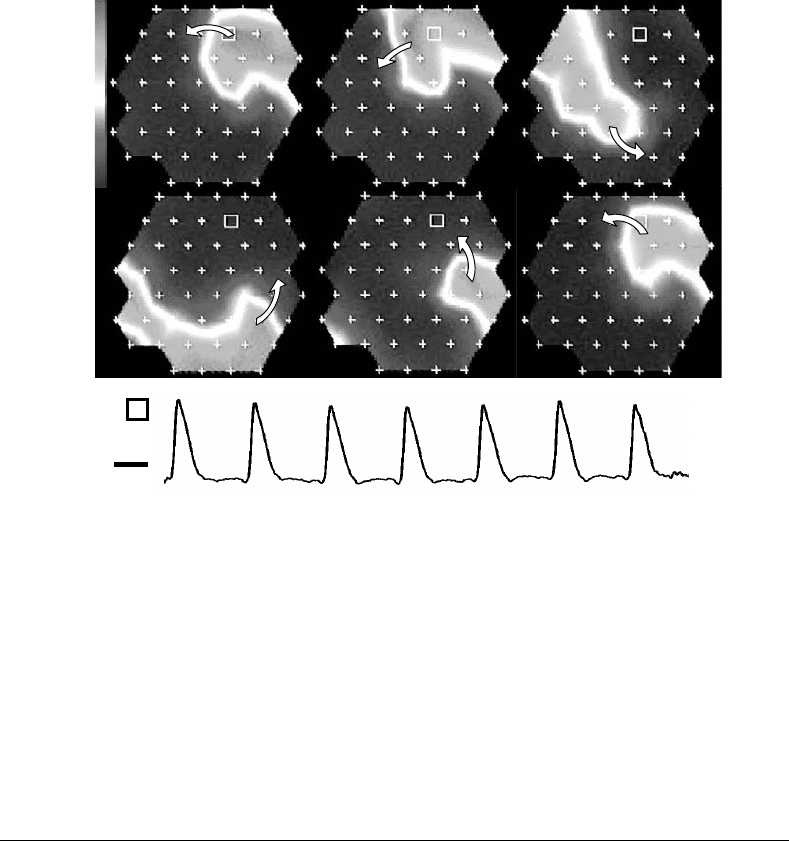
FIGURE 27.4 Functional reentry in a cardiac tissue construct induced by rapid point pacing, and assessed by optical
mapping of transmembrane potential. (a) Single rotation of a counterclockwise reentrant wave shown through a series
of voltage snapshots in time. Frames progress left to right, top to bottom. Time in milliseconds is marked at the top
left corner of each frame. Arrows denote the direction of wave front. + denotes 2-mm spaced recording sites. Gray
scale bar next to the first frame corresponds to a normalized transmembrane voltage with bottom and top denoting
rest and peak of an action potential, respectively. (b) Recording of transmembrane voltage from the site marked by a
white square in the frames of panel A. Reentrant activity appears stationary and periodic.
during implantation by attachment to one of the host arteries. The success will only be accomplished by a
profound understanding of a number of complex topics, and achieved through a joint effort among basic
scientists, engineers, and clinicians.
27.6 Conclusions
Cardiac tissue engineering is a new and exciting field with many obstacles to be surmounted before start of
clinical trials. With technical aspects resolved, the main advantage of implanted cardiac tissue patch over
the injected cells will be a structural and functional repair of large tissue defects. Given that implantation
of cardiac patch will repair a centimeter-size tissue region, inference about the quality of tissue construct
sprior to implantation should be based not only upon different assessments at cellular or subcellular
level, but also upon detailed evaluation of both electrical and mechanical function at centimeter-size scale
(i.e., measurements of impulse propagation and contractile force in constructs relative to those in native
cardiac muscle). Similarly, only systematic micro- and macroscopic assessments of heart structure and
electromechanical function postimplantation will provide necessary selectivity towards the design of safe
and efficient clinical therapies.
Acknowledgment
The author would like to thank P. Bursac and K. Cahill for reviewing the manuscript. This manuscript
was submitted for press on May 1, 2004. Due to rapid developments in the field, some of the most
mikos: “9026_c027” — 2007/4/9 — 15:53 — page 17 — #17
Cardiac Tissue Engineering 27-17
contemporary work will not be reviewed, and certain statements may be outdated at the time of press.
Author apologizes in advance if this is the case.
References
[1] Anversa P. and Kajstura J. Ventricular myocytes are not terminally differentiated in the adult
mammalian heart. Circ. Res. 1998; 83: 1–14.
[2] Laflamme M.A., Myerson D., Saffitz J.E., and Murry C.E. Evidence for cardiomyocyte repopulation
by extracardiac progenitors in transplanted human hearts. Circ. Res. 2002; 90: 634–640.
[3] Guyatt G.H. and Devereaux P.J. A review of heart failure treatment. Mt. Sinai. J. Med. 2004;71:
47–54.
[4] Miniati D.N. and Robbinson R.C. Heart transplantation: a thirty year perspective. Annu.Rev.Med.
2002; 53: 189–205.
[5] Boehmer J.P. Device therapy for heart failure. Am. J. Cardiol. 2003; 91: 53D–59D.
[6] Moreira L.F. and Stolf N.A. Dynamic cardiomyoplasty as a therapeutic alternative: current status.
Heart Fail. Rev. 2001; 6: 201–212.
[7] Szatkowski A., Ndubuka-Irobunda C., Oesterle S.N., and Burkhoff D. Transmyocardial laser
revascularization: a review of basic and clinical aspects. Am. J. Cardiovasc. Drugs 2002; 2: 255–266.
[8] Sorelle R. Cardiovascular news: totally contained AbioCor artificial heart implanted July 3, 2001.
Circulation 2001; 104: E9005–E9006.
[9] Association A.H. 2000 Heart and Stroke Statistical Update. Dallas, TX: American Heart Association,
1999.
[10] Pasumarthi K.B.S. and Field L.J. Cardiomyocyte cell cycle regulation. Circ. Res. 2002; 90: 1044–
1054.
[11] Orlic D., Kajstura J., Chimenti S., Limana F., Jakoniuk I., Quaini F., Nadal-Ginard B., Bodine D.M.,
Leri A., and Anversa P. Mobilized bone marrow cells repair the infarcted heart, improving function
and survival. Proc. Natl Acad. Sci. USA 2001; 98: 10344–10349.
[12] Dowell J.D., Rubart M., Pasumarthi K.B., Soonpaa M.H., and Field L.J. Myocyte and myogenic
stem cell transplantation in the heart. Cardiovasc. Res. 2003; 58: 336–350.
[13] Chachques J.C., Acar C., Herreros J., Trainini J.C., Prosper F., D’Attellis N., Fabiani J.N., and
Carpentier A.F. Cellular cardiomyoplasty: clinical application. Ann. Thorac. Surg. 2004; 77:
1121–1130.
[14] Zimmermann W.H. and Eschenhagen T. Cardiac tissue engineering for replacement therapy. Heart
Fail. Rev. 2003; 8: 259–269.
[15] Koh G., Soonpaa M., Klug M., and Field L. Long-term survival of AT-1 cardyomyocyte graftsin
syngeneic myocardium. Am. J. Physiol. 1993; 264: H1727–H1733.
[16] Koh G., Klug M., Soonpaa M., and Field L. Differentiation and long term survival of C2C12
myoblasts graft in heart. J. Clin. Invest. 1993; 92: 1548–1554.
[17] Soonpa M.H., Koh G.Y., Klug M.G., and Field L.J. Formation of nascent intercalated disks between
grafted fetal cardiomyocytes and host myocardium. Science 1994; 264: 98–101.
[18] Rubart M., Pasumarthi K.B., Nakajima H., Soonpaa M.H., Nakajima H.O., and Field L.J. Physiolo-
gical coupling of donor and host cardiomyocytes after cellular transplantation. Circ. Res. 2003; 92:
1217–1224.
[19] Reinecke H., Zhang M., Bartosek T., and Murry C.E. Survival, integration, and differentiation of
cardiomyocyte grafts: a study in normal and injured rat hearts. Circulation 1999; 100: 193–202.
[20] Sakai T., Li R.K., Weisel R.D., Mickle D.A., Kim E.J., Tomita S., Jia Z.Q., and Yau T.M. Autologous
heart cell transplantation improves cardiac function after myocardial injury. Ann. Thorac. Surg.
1999; 68: 2074–2080; discussion 2080–2081.
[21] Taylor D., Atkins B., Hungspreugs P., Jones T., Reedy M., Hutcheson K., Glower D., and
Kraus W. Regenerating functional myocardium: improved performance after skeletal myoblast
transplantation. Nat. Med. 1998; 4: 929–933.
mikos: “9026_c027” — 2007/4/9 — 15:53 — page 18 — #18
27-18 Tissue Engineering
[22] Kessler P.D. and Byrne B.J. Myoblast cell grafting into heart muscle: cellular biology and potential
applications. Annu. Rev. Physiol. 1999; 61: 219–242.
[23] Murry C., Wiseman R., Schwartz S., and Hauschka S. Skeletal myoblast transplantation for repair
of myocardial necrosis. J. Clin. Invest. 1996; 98: 2512–2523.
[24] Li G., Ouyang Q., Petrov V.V., and Swinney H.L. Transition from simple rotating chemical spirals
to meandering and traveling spirals. Phys.Rev.Lett.1996; 77: 2105–2108.
[25] Kim E.J., Li R.K., Weisel R.D., Mickle D.A., Jia Z.Q., Tomita S., Sakai T., and Yau T.M. Angiogenesis
by endothelial cell transplantation. J. Thorac. Cardiovasc. Surg. 2001; 122: 963–971.
[26] Hutcheson K.A., Atkins B.Z., Hueman M.T., Hopkins M.B., Glower D.D., and Taylor D.A.
Comparison of benefits on myocardial performance of cellular cardiomyoplasty with skeletal
myoblasts and fibroblasts. Cell Transplant. 2000; 9: 359–368.
[27] Etzion S., Barbash I.M., Feinberg M.S., Zarin P., Miller L., Guetta E., Holbova R., Kloner R.A.,
Kedes L.H., and Leor J. Cellular cardiomyoplasty of cardiac fibroblasts by adenoviral delivery of
MyoD ex vivo: an unlimited source of cells for myocardial repair. Circulation 2002; 106: I125–I130.
[28] Klug M.G., Soonpaa M.H., Koh G.Y., and Field L.J. Genetically selected cardiomyocytes from
differentiating embronic stem cells form stable intracardiac grafts. J. Clin. Invest. 1996; 98:
216–224.
[29] Orlic D., Kajstura J., Chimenti S., Jakoniuk I., Anderson S.M., Li B., Pickel J., McKay R.,
Nadal-Ginard B., Bodine D.M., Leri A., and Anversa P. Bone marrow cells regenerate infarcted
myocardium. Nature 2001; 410: 701–705.
[30] Vulliet P.R., Greeley M., Halloran S.M., MacDonald K.A., and Kittleson M.D. Intra-coronary
arterial injection of mesenchymal stromal cells and microinfarction in dogs. Lancet 2004; 363:
783–784.
[31] Beltrami A.P., Barlucchi L., Torella D., Baker M., Limana F., Chimenti S., Kasahara H., Rota M.,
Musso E., Urbanek K., Leri A., Kajstura J., Nadal-Ginard B., and Anversa P. Adult cardiac stem
cells are multipotent and support myocardial regeneration. Cell 2003; 114: 763–776.
[32] Sakai T., Li R.K., Weisel R.D., Mickle D.A., Jia Z.Q., Tomita S., Kim E.J., and Yau T.M. Fetal cell
transplantation: a comparison of three cell types. J. Thorac. Cardiovasc. Surg. 1999; 118: 715–724.
[33] Menasche P. Myoblast-based cell transplantation. Heart Fail. Rev. 2003; 8: 221–227.
[34] Menasche P., Hagege A.A., Vilquin J.T., Desnos M., Abergel E., Pouzet B., Bel A., Sarateanu S.,
Scorsin M., Schwartz K., Bruneval P., Benbunan M., Marolleau J.P., and Duboc D. Autologous
skeletal myoblast transplantation for severe postinfarction left ventricular dysfunction. J. Am. Coll.
Cardiol. 2003; 41: 1078–1083.
[35] Menasche P. Cellular transplantation: hurdles remaining before widespread clinical use. Curr.
Opin. Cardiol. 2004; 19: 154–161.
[36] Reinecke H., MacDonald G.H., Hauschka S.D., and Murry C.E. Electromechanical coupling
between skeletal and cardiac muscle. Implications for infarct repair. J. Cell Biol. 2000; 149: 731–740.
[37] Pak H.N., Qayyum M., Kim D.T., Hamabe A., Miyauchi Y., Lill M.C., Frantzen M., Takizawa K.,
Chen L.S., Fishbein M.C., Sharifi B.G., Chen P.S., and Makkar R. Mesenchymal stem cell injection
induces cardiac nerve sprouting and increased tenascin expression in a Swine model of myocardial
infarction. J. Cardiovasc. Electrophysiol. 2003; 14: 841–848.
[38] Hoffman J.I., Kaplan S., and Liberthson R.R. Prevalence of congenital heart disease. Am. Heart J.
2004; 147: 425–439.
[39] O’Dell W.G. and McCulloch A.D. Imaging three-dimensional cardiac function. Annu. Rev. Biomed.
Eng. 2000; 2: 431–456.
[40] Shachar M. and Cohen S. Cardiac tissue engineering, ex-vivo: design principles in biomaterials
and bioreactors. Heart Fail. Rev. 2003; 8: 271–276.
[41] Spach M. Anisotropy of cardiac tissue: a major determinant of conduction. J. Cardiovasc.
Electrophysiol. 1999; 10: 887–890.
[42] Saffitz J., Kanter H., Green K., Tolley T., and Beyer E. Tissue-specific determinants of anisotropic
conduction velocity in canine atrial and ventricular myocardium. Circ. Res. 1994; 74: 1065–1070.
mikos: “9026_c027” — 2007/4/9 — 15:53 — page 19 — #19
Cardiac Tissue Engineering 27-19
[43] Arts T., Costa K.D., Covell J.W., and McCulloch A.D. Relating myocardial laminar architec-
ture to shear strain and muscle fiber orientation. Am. J. Physiol. Heart Circ. Physiol. 2001; 280:
H2222–H2229.
[44] Antzelevitch C., Yan G.-X., Shimizu W., and Burashnikov A. Electrical heterogeneity, the ECG,
and cardiac arrhythmias. In Zipes D.P. and Jalife J., Eds. Cardiac Electrophysiology — From Cell to
Bedside. 3rd ed. Philadelphia, PA: W. B. Saunders Co., 2000, pp. 222–238.
[45] de Bakker J.M. and OptHof T. Is the apico-basal gradient larger than the transmural gradient?
J. Cardiovasc. Pharmacol. 2002; 39: 328–331.
[46] Wolk R., Cobbe S.M., Hicks M.N., and Kane K.A. Functional, structural, and dynamic basis of
electrical heterogeneity in healthy and diseased cardiac muscle: implications for arrhythmogenesis
and anti-arrhythmic drug therapy. Pharmacol. Ther. 1999; 84: 207–231.
[47] Spach M.S., Dolber P.C., Heidlage J.F., Kootsey J.M., and Johnson E.A. Propagating depolar-
ization in anisotropic human and canine cardiac muscle: apparent directional differences in
membrane capacitance. A simplified model for selective directional effects of modifying the
sodium conductance on Vmax, tau foot, and the propagation safety factor. Circ. Res. 1987; 60:
206–219.
[48] Roberge F.A. and Leon L.J. Propagation of activation in cardiac muscle. J. Electrocardiol. 1992; 25
Suppl: 69–79.
[49] Bursac N., Parker K.K., Iravanian S., and Tung L. Cardiomyocyte cultures with controlled macro-
scopic anisotropy. A model for functional electrophysiological studies of cardiac muscle. Circ. Res.
2002; 91: e45–e54.
[50] Spach M.S. and Heidlage J.F. The stochastic nature of cardiac propagation at a microscopic level.
Electrical description of myocardial architecture and its application to conduction. Circ. Res. 1995;
76: 366–380.
[51] Kleber A.G. and Rudy Y. Basic mechanisms of cardiac impulse propagation and associated
arrhythmias. Physiol. Rev. 2004; 84: 431–488.
[52] Antzelevitch C. Basic mechanisms of reentrant arrhythmias. Curr. Opin. Cardiol. 2001; 16: 1–7.
[53] Spach M.S. and Dolber P.C. Relating extracellular potentials and their derivatives to anisotropic
propagation at a microscopic level in human cardiac muscle. Evidence for electrical uncoupling of
side-to-side fiber connections with increasing age. Circ. Res. 1986; 58: 356–371.
[54] Koura T., Hara M., Takeuchi S., Ota K., Okada Y., Miyoshi S., Watanabe A., Shiraiwa K.,
Mitamura H., Kodama I., and Ogawa S. Anisotropic conduction properties in canine atria ana-
lyzed by high-resolution optical mapping: preferential direction of conduction block changes from
longitudinal to transverse with increasing age. Circulation 2002; 105: 2092–2098.
[55] McCulloch A., Bassingthwaighte J., Hunter P., and Noble D. Computational biology of the heart:
from structure to function. Prog. Biophys. Mol. Biol. 1998; 69: 153–155.
[56] de Bakker J.M., van Capelle F.J., Janse M.J., Tasseron S., Vermeulen J.T., de Jonge N., and Lahpor J.R.
Fractionated electrograms in dilated cardiomyopathy: origin and relation to abnormal conduction.
J. Am. Coll. Cardiol. 1996; 27: 1071–1078.
[57] De Bakker J.M.T and Janse M.J. Pathophysiological correlates of ventricular tachycardia in hearts
with a healed infarct. In Zipes D.P. and Jalife J., Eds. Cardiac Electrophysiology — From Cell to
Bedside. 3rd ed. Philadelphia, PA: W.B. Saunders Co., 2000, pp. 415–422.
[58] Spach M.S. and Josephson M.E. Initiating reentry: the role of nonuniform anisotropy in small
circuits. J. Cardiovasc. Electrophysiol. 1994; 5: 182–209.
[59] Wit A.L., Dillon S.M., and Coromilas J. Anisotropic reentry as a cause of ventricular tachyar-
rhythmias in myocardial infarction. In Zipes D.P. and Jalife J., Eds. Cardiac Electrophysiology —
From Cell to Bedside. Philadelphia, PA: W.B. Saunders Co., 1995, pp. 511–526.
[60] Ravens U.Mechano-electric feedback and arrhythmias. Prog. Biophys. Mol. Biol. 2003; 82: 255–266.
[61] Fink C., Ergun S., Kralisch D., Remmers U., Weil J., and Eschenhagen T. Chronic stretch of
engineered heart tissue induces hypertrophy and functional improvement. FASEB J. 2000; 14:
669–679.
mikos: “9026_c027” — 2007/4/9 — 15:53 — page 20 — #20
27-20 Tissue Engineering
[62] Zimmermann W., Fink C., Kralisch D., Remmers U., Weil J., and Eschenhagen T. Three-
dimensional engineered heart tissue from neonatal rat cardiac cells. Biotechnol. Bioeng. 2000;
68: 106–114.
[63] Carrier R., Papadaki M., Rupnick M., Schoen F., Bursac N., Langer R., Freed L., and
Vunjak-Novakovic G. Development of a model system for cardiac tissue engineering: investigation
of key parameters. Biotechnol. Bioeng. 1999; 64: 580–589.
[64] Bursac N., Papadaki M., Cohen R., Schoen F., Eisenberg S., Carrier R., Vunjak-Novakovic G.,
and Freed L. Cardiac muscle tissue engineering: towards an in vitro model for electrophysiological
studies. Am. J. Physiol. (Heart Circ. Physiol. 46) 1999; 277: H433–H444.
[65] Radisic M., Euloth M., Yang L., Langer R., Freed L.E., and Vunjak-Novakovic G. High-density
seeding of myocyte cells for cardiac tissue engineering. Biotechnol. Bioeng. 2003; 82:
403–414.
[66] Dar A., Shachar M., Leor J., and Cohen S. Optimization of cardiac cell seeding and distribution in
3D porous alginate scaffolds. Biotechnol. Bioeng. 2002; 80: 305–312.
[67] Ozawa T., Mickle D.A., Weisel R.D., Koyama N., Ozawa S., and Li R.K. Optimal biomaterial for
creation of autologous cardiac grafts. Circulation 2002; 106: I176–I182.
[68] Pego A.P., Poot A.A., Grijpma D.W., and Feijen J. Biodegradable elastomeric scaffolds for soft
tissue engineering. J. Control. Release 2003; 87: 69–79.
[69] Papadaki M., Bursac N., Langer R., Merok J., Vunjak-Novakovic G., and Freed L. Tissue engin-
eering of functional cardiac muscle: molecular, structural and electrophysiological studies. Am. J.
Physiol. (Heart Circ. Physiol.) 2001; 280: H168–H178.
[70] Zimmermann W.H., Melnychenko I., and Eschenhagen T. Engineered heart tissue for regeneration
of diseased hearts. Biomaterials 2004; 25: 1639–1647.
[71] Akhyari P., Fedak P.W., Weisel R.D., Lee T.Y., Verma S., Mickle D.A., and Li R.K. Mechanical stretch
regimen enhances the formation of bioengineered autologous cardiac muscle grafts. Circulation
2002; 106: I137–I142.
[72] Zimmermann W., Schneiderbanger K., Schubert P., Didie M., Munzel F., Heubach J., Kostin S.,
Nehuber W., and Eschenhagen T. Tissue engineering of a differentiated cardiac muscle construct.
Circ. Res. 2002; 90: 223–230.
[73] Kofidis T., Akhyari P., Wachsmann B., Mueller-Stahl K., Boublik J., Ruhparwar A., Mertsching H.,
Balsam L., Robbins R., and Haverich A. Clinically established hemostatic scaffold (tissue fleece) as
biomatrix in tissue- and organ-engineering research. Tissue Eng. 2003; 9: 517–523.
[74] Yost M.J., Baicu C.F., Stonerock C.E., Goodwin R.L., Price R.L., Davis J.M., Evans H., Watson P.D.,
Gore C.M., Sweet J., CreechL., Zile M.R., and Terracio L. A novel tubular scaffold for cardiovascular
tissue engineering. Tissue Eng. 2004; 10: 273–284.
[75] Shimizu T., Yamato M., Isoi Y., Akutsu T., Setomaru T., Abe K., Kikuchi A., Umezu M.,
and Okano T. Fabrication of pulsatile cardiac tissue grafts using a novel 3-dimensional cell
sheet manipulation technique and temperature-responsive cell culture surfaces. Circ. Res. 2002;
90: e40.
[76] Bursac N., Papadaki M., White J.A., Eisenberg S.R., Vunjak-Novakovic G., and Freed L.E. Cul-
tivation in rotating bioreactors promotes maintenance of cardiac myocyte electrophysiology and
molecular properties. Tissue Eng. 2003; 9: 1243–1253.
[77] Akins R.E., Schroedl N.A., Gonda S.R., and Hartzell C.R. Neonatal rat heart cells cultured in
simulated microgravity. InVitroCellDev.Biol. 1997; 337–343.
[78] Akins R.E., Boyce R.A., Madonna M.L., Schroedl N.A., Gonda S.R., McLaughlin T.A., and
Hartzell C.R. Cardiac organogenesis in vitro: reestablishment of three-dimensional tissue
architecture by dissociated neonatal rat ventricular cells. Tissue Eng. 1999; 5: 103–118.
[79] Eschenhagen T., Fink C., Remmers U., Scholz H., Wattchow J., Weil J., Zimmerman W.,
Dohmen H., Schafer H., Bishopric N., Wakatsuki T., and Elson E. Three-dimensional recon-
stitution of embryonic cardimyocytes in a collagen matrix: a new heart muscle model system.
FASEB J. 1997; 11: 683–694.
mikos: “9026_c027” — 2007/4/9 — 15:53 — page 21 — #21
Cardiac Tissue Engineering 27-21
[80] Vandenburgh H., Del Tatto M, Shansky J., Lemaire J., Chang A., Payumo F., Lee P., Goodyear A.,
and Raven L. Tissue-engineered skeletal muscle organoids for reversible gene therapy. Hum. Gene
Ther. 1996; 7: 2195–2200.
[81] Holubarsch C., Ruf T., Goldstein D.J., Ashton R.C., Nickl W., Pieske B., Pioch K., Ludemann J.,
Wiesner S., Hasenfuss G., Posival H., Just H., and Burkhoff D. Existence of the Frank–Starling
mechanism in the failing human heart. Investigations on the organ, tissue, and sarcomere levels.
Circulation 1996; 94: 683–689.
[82] Rau T., Nose M., Remmers U., Weil J., Weissmuller A., Davia K., Harding S., Peppel K., Koch W.J.,
and Eschenhagen T. Overexpression of wild-type Galpha(i)-2 suppresses beta-adrenergic signaling
in cardiac myocytes. FASEB J. 2003; 17: 523–525.
[83] El-Armouche A., Rau T., Zolk O., Ditz D., Pamminger T., Zimmermann W.H., Jackel E., Hard-
ing S.E., Boknik P., Neumann J., and Eschenhagen T. Evidence for protein phosphatase inhibitor-1
playing an amplifier role in beta-adrenergic signaling in cardiac myocytes. FASEB J. 2003; 17:
437–439.
[84] Zolk O., Munzel F., and Eschenhagen T. Effects of chronic endothelin-1 stimulation on cardiac
myocyte contractile function. Am. J. Physiol. Heart Circ. Physiol. 2004; 286: H1248–H1257.
[85] Zimmermann W.H., Didie M., Wasmeier G.H., Nixdorff U., Hess A., Melnychenko I., Boy O.,
Neuhuber W.L., Weyand M., and Eschenhagen T. Cardiac grafting of engineered heart tissue in
syngenic rats. Circulation 2002; 106: I151–I157.
[86] Li R.K., Yau T.M., Weisel R.D., Mickle D.A., Sakai T., Choi A., and Jia Z.Q. Construction of a
bioengineered cardiac graft. J. Thorac. Cardiovasc. Surg. 2000; 119: 368–375.
[87] Kofidis T., Akhyari P., Wachsmann B., Boublik J., Mueller-Stahl K., Leyh R., Fischer S., and
Haverich A. A novel bioartificial myocardial tissue and its prospective use in cardiac surgery. Eur.
J. Cardiothorac. Surg. 2002; 22: 238–243.
[88] Kofidis T., Lenz A., Boublik J., Akhyari P., Wachsmann B., Mueller-Stahl K., Hofmann M., and
Haverich A. Pulsatile perfusion and cardiomyocyte viability in a solid three-dimensional matrix.
Biomaterials 2003; 24: 5009–5014.
[89] van Luyn M.J., Tio R.A., Gallego y van Seijen X.J., Plantinga J.A., de Leij L.F., DeJong-
ste M.J., and van Wachem P.B. Cardiac tissue engineering: characteristics of in unison contracting
two- and three-dimensional neonatal rat ventricle cell (co)-cultures. Biomaterials 2002; 23:
4793–4801.
[90] Evans H.J., Sweet J.K., Price R.L., Yost M., and Goodwin R.L. Novel 3D culture system
for study of cardiac myocyte development. Am J. Physiol. Heart Circ. Physiol. 2003; 285:
H570–H578.
[91] Matthews J.A., Wnek G.E., Simpson D.G., and Bowlin G.L. Electrospinning of collagen nanofibers.
Biomacromolecules 2002; 3: 232–238.
[92] Shimizu T., Yamato M., Akihiko K., and Okano T. Two-dimensional manipulation of cardiac
myocyte sheets utilizing temperature-responsive culture dishes augments pulsatile amplitude.
Tissue Eng. 2001; 7: 141–151.
[93] Shimizu T., Yamato M., Akutsu T., Shibata T., Isoi Y., Kikuchi A., Umezu M., and Okano T.
Electrically communicating three-dimensional cardiac tissue mimic fabricated by layered cultured
cardiomyocyte sheets. J. Biomed. Mater. Res. 2002; 60: 110–117.
[94] Carrier R.L., Rupnick M., Langer R., Schoen F.J., Freed L.E., and Vunjak-Novakovic G. Perfusion
improves tissue architecture of engineered cardiac muscle. Tissue Eng. 2002; 8: 175–188.
[95] Carrier R.L., Rupnick M., Langer R., Schoen F.J., Freed L.E., and Vunjak-Novakovic G. Effects of
oxygen on engineered cardiac muscle. Biotechnol. Bioeng. 2002; 78: 617–625.
[96] Radisic M., Yang L., Boublik J., Cohen R.J., Langer R., Freed L.E., and Vunjak-Novakovic G.
Medium perfusion enables engineering of compact and contractile cardiac tissue. Am. J. Physiol.
Heart Circ. Physiol. 2004; 286: H507–H516.
[97] Li R.K., Jia Z.Q., Weisel R.D., Mickle D.A., Choi A., and Yau T.M. Survival and function of
bioengineered cardiac grafts. Circulation 1999; 100: II63–II69.
mikos: “9026_c027” — 2007/4/9 — 15:53 — page 22 — #22
27-22 Tissue Engineering
[98] Ozawa T., Mickle D.A., Weisel R.D., Koyama N., Wong H., Ozawa S., and Li R.K. Histologic changes
of nonbiodegradable and biodegradable biomaterials used to repair right ventricular heart defects
in rats. J. Thorac. Cardiovasc. Surg. 2002; 124: 1157–1164.
[99] Matsubayashi K., Fedak P.W., Mickle D.A., Weisel R.D., Ozawa T., and Li R.K. Improved left
ventricular aneurysm repair with bioengineered vascular smooth muscle grafts. Circulation 2003;
108 Suppl 1: II219–II225.
[100] Leor J., Aboulafia-Etzion S., Dar A., Shapiro L., Barbash I., Battler A., Granot Y., and Cohen S.
Bioengineered cardiac grafts: a new approach to repair the infarcted myocardium? Circulation
2000; 102: III56–III61.
[101] Kehat I., Kenyagin-Karsenti D., Snir M., Segev H., Amit M., Gepstein A., Livne E., Binah O.,
Itskovitz-Eldor J., and Gepstein L. Human embryonic stem cells can differentiate into myocytes
with structural and functional properties of cardiomyocytes. J. Clin. Invest. 2001; 108: 407–414.
[102] Xu C., Police S., Rao N., and Carpenter M.K. Characterization and enrichment of cardiomyocytes
derived from human embryonic stem cells. Circ. Res. 2002; 91: 501–508.
[103] Lanza R., Moore M.A., Wakayama T., Perry A.C., Shieh J.H., Hendrikx J., Leri A., Chimenti S.,
Monsen A., Nurzynska D., West M.D., Kajstura J., and Anversa P. Regeneration of the infarcted
heart with stem cells derived by nuclear transplantation. Circ. Res. 2004; 94: 820–827.
[104] Grusby M.J., Auchincloss H., Jr., Lee R., Johnson R.S., Spencer J.P., Zijlstra M., Jaenisch R.,
Papaioannou V.E., and Glimcher L.H. Mice lacking major histocompatibility complex class I and
class II molecules. Proc. Natl Acad. Sci. USA 1993; 90: 3913–3917.
[105] Leobon B., Garcin I., Menasche P., Vilquin J.T., Audinat E., and Charpak S. Myoblasts transplanted
into rat infarcted myocardium are functionally isolated from their host. Proc. Natl Acad. Sci. USA
2003; 100: 7808–7811.
[106] Reinecke H., Poppa V., and Murry C.E. Skeletal muscle stem cells do not transdifferentiate into
cardiomyocytes after cardiac grafting. J. Mol. Cell Cardiol. 2002; 34: 241–249.
[107] Suzuki K., Brand N.J., Allen S., Khan M.A., Farrell A.O., Murtuza B., Oakley R.E., and Yacoub M.H.
Overexpression of connexin 43 in skeletal myoblasts: relevance to cell transplantation to the heart.
J. Thorac. Cardiovasc. Surg. 2001; 122: 759–766.
[108] Thompson R.B., Emani S.M., Davis B.H., van den Bos E.J., Morimoto Y., Craig D., Glower D., and
Taylor D.A. Comparison of intracardiac cell transplantation: autologous skeletal myoblasts versus
bone marrow cells. Circulation 2003; 108 Suppl 1: II264–II271.
[109] Murry C.E., Soonpaa M.H., Reinecke H., Nakajima H., Nakajima H.O., Rubart M.,
Pasumarthi K.B., Virag J.I., Bartelmez S.H., Poppa V., Bradford G., Dowell J.D., Williams D.A., and
Field L.J. Haematopoietic stem cells do not transdifferentiate into cardiac myocytes in myocardial
infarcts. Nature 2004; 428: 664–668.
[110] Balsam L.B., Wagers A.J., Christensen J.L., Kofidis T., Weissman I.L., and Robbins R.C. Haema-
topoietic stem cells adopt mature haematopoietic fates in ischaemic myocardium. Nature 2004;
428: 668–673.
[111] Leor J., Battler A., Kloner R.A., and Etzion S. Reprogramming cells for transplantation. Heart Fail.
Rev. 2003; 8: 285–292.
[112] Lijnen P., Petrov V. and Fagard R. In vitro assay of collagen gel contraction by cardiac fibroblasts
in serum-free conditions. Meth. Find. Exp. Clin. Pharmacol. 2001; 23: 377–382.
[113] Taggart P., Sutton P.M., Opthof T., Coronel R., Trimlett R., Pugsley W., and Kallis P. Inhomo-
geneous transmural conduction during early ischaemia in patients with coronary artery disease.
J. Mol. Cell Cardiol. 2000; 32: 621–630.
[114] Hunter P.J., McCulloch A.D., and ter Keurs H.E. Modelling the mechanical properties of cardiac
muscle. Prog. Biophys. Mol. Biol. 1998; 69: 289–331.
[115] Terracio L., Miller B., and Borg T.K. Effects of cyclic mechanical stimulation of the cellular
components of the heart: in vitro. InVitroCellDev.Biol. 1988; 24: 53–58.
[116] Simpson D., Majeski M., Borg T., and Terracio L. Regulation of cardiac myocyte protein turnover
and myofibrillar structure in vitro by specific directions of stretch. Circ. Res. 1999; 85: e59–e69.
mikos: “9026_c027” — 2007/4/9 — 15:53 — page 23 — #23
Cardiac Tissue Engineering 27-23
[117] Costa K.D., Lee E.J., and Holmes J.W. Creating alignment and anisotropy in engineered heart
tissue: role of boundary conditions in a model three-dimensional culture system. Tissue Eng. 2003;
9: 567–577.
[118] Simpson D., Terracio L., Terracio M., Price R., Turner D., and Borg T. Modulation of cardiac
myocyte phenotype in vitro by the composition and orientation of the extracellular matrix. J. Cell
Physiol. 1994; 161: 89–105.
[119] Bien H., Yin L., and Entcheva E. Cardiac cell networks on elastic microgrooved scaffolds. IEEE
Eng. Med. Biol. Mag. 2003; 22: 108–112.
[120] McDevitt T., Angello J., Whitney M., Reinecke H., Hauschka S., Murry C., and Stayton P. In vitro
generation of differentiated cardiac myofibers on micropatterned laminin surfaces. J. Biomed.
Mater. Res. 2002; 60: 472–479.
[121] Bursac N., Loo Y., Irby M.E., Leong K., and Tung L. Polymer scaffolds for anisotropic growth
of engineered cardiac tissue. In Vossoughi J., Ed. Southern Biomedical Engineering Conference.
Washington, DC: 2002, pp. 141–142.
[122] Bursac N., Loo Y., Irby M.E., Leong K., and Tung L. Electrophysiological studies in anisotropic 3D
cardiac cultures. In Pace, Ed. NASPE. Washington, DC: Futura, 2003, p. 1045.
[123] Pego A.P., Siebum B., Van Luyn M.J., Gallego y Van Seijen X.J., Poot A.A., Grijpma D.W.,
and Feijen J. Preparation of degradable porous structures based on 1,3-trimethylene car-
bonate and D,L-lactide (co)polymers for heart tissue engineering. Tissue Eng. 2003; 9:
981–994.
[124] Li W.J., Laurencin C.T., Caterson E.J., Tuan R.S., and Ko F.K. Electrospun nanofibrous structure:
a novel scaffold for tissue engineering. J. Biomed. Mater. Res. 2002; 60: 613–621.
[125] Stoker M.E., Gerdes A.M., and May J.F. Regional differences in capillary density and myocyte size
in the normal human heart. Anat. Rec. 1982; 202: 187–191.
[126] Xie Z., Gao M., Batra S., and Koyama T. The capillarity of left ventricular tissue of rats subjected
to coronary artery occlusion. Cardiovasc. Res. 1997; 33: 671–676.
[127] Spach M., Dolber P., and Heidlage J. Properties of discontinuous anisotropic propagation at a
microscopic level. Ann.NYAcad. Sci. 1990; 591: 62–74.
[128] Peters N.S., Coromilas J., Severs N.J., and Wit A.L. Disturbed connexin43 gap junction distribution
correlates with the location of reentrant circuits in the epicardial border zone of healing canine
infarcts that cause ventricular tachycardia. Circulation 1997; 95: 988–996.
[129] Kaihara S., Borenstein J., Koka R., Lalan S., Ochoa E.R., Ravens M., Pien H., Cunningham B.,
and Vacanti J.P. Silicon micromachining to tissue engineer branched vascular channels for liver
fabrication. Tissue Eng. 2000; 6: 105–117.
[130] Arutunyan A., Swift L.M., and Sarvazyan N. Initiation and propagation of ectopic waves: insights
from an in vitro model of ischemia-reperfusion injury. Am. J. Physiol. Heart Circ. Physiol. 2002;
283: H741–H749.
[131] Huelsing D.J., Spitzer K.W., Cordeiro J.M., and Pollard A.E. Conduction between isolated rabbit
Purkinje and ventricular myocytes coupled by a variable resistance. Am. J. Physiol. 1998; 274:
H1163–H1173.
[132] Antzelevitch C., Shimizu W., Yan G.X., Sicouri S., Weissenburger J., Nesterenko V.V.,
Burashnikov A., Di Diego J., Saffitz J., and Thomas G.P. The M cell: its contribution to the
ECG and to normal and abnormal electrical function of the heart. J. Cardiovasc. Electrophysiol.
1999; 10: 1124–1152.
[133] Rohr S., Kucera J., Fast V., and Kleber A. Paradoxical improvement of impulse conduction in
cardiac tissue by partial cellular uncoupling. Science 1997; 275: 841–844.
[134] Shaw R. and Rudy Y. Ionic mechanisms of propagation in cardiac tissue. roles of the sodium
and L-type calcium currents during reduced excitability and decreased gap junctional coupling.
Circ. Res. 1997; 81: 727–741.
[135] Gaudesius G., Miragoli M., Thomas S.P., and Rohr S. Coupling of cardiac electrical activity over
extended distances by fibroblasts of cardiac origin. Circ. Res. 2003; 93: 421–428.
