Caballero B. (ed.) Encyclopaedia of Food Science, Food Technology and Nutrition. Ten-Volume Set
Подождите немного. Документ загружается.

Meeting Nutrient Needs
0007 Enteral formulas, which are nutritionally complete
liquid diets administered through a tube placed in
the gastrointestinal tract, are employed in most in-
stances, as the burn patient cannot usually voluntarily
ingest sufficient food to maintain an adequate energy
intake. Burn patients have been successfully treated
with the end of the tube placed either in the stomach
or in the upper part of the small intestine. It is difficult
to provide adequate energy with a low-fat enteral
diet, because the volumes required are so great. Nu-
trition by a parenteral or intravenous route may be
indicated in special circumstances, for example if the
gastrointestinal tract cannot be used. Occasionally,
parenteral nutrition may be used in combination
with enteral, when use of the latter is not providing
adequate nutrition. Parenteral nutrition, however, is
not the standard more of nutrition for the burn
patient, as it is more costly than, and has not been
shown to be superior to, other routes.
0008 Oral intake is the first choice, but it should be used
only when the patient can consume sufficient food
at meals and in between meal snacks to achieve an
adequate energy intake. Nutrient-dense snacks and
liquid supplements help to achieve an adequate
intake. Occasionally, ad libitum oral intake is com-
bined with enteral formula administered overnight to
provide adequate nutrition.
0009 Since early introduction of nutrition improves pa-
tient response to treatment, nutrient intake is initiated
within the first 24–72 h after injury, as soon as fluid
and hemodynamic status are stabilized. Early feeding
is also important, as it has been shown to help main-
tain the integrity and motility of the gastrointestinal
tract.
Nutritionally Relevant Complications
0010Complications that affect nutrition therapy of the
burn patient can be divided into three classes: (1)
those related to the thermal injury; (2) preexisting
metabolic conditions; and (3) those related to the
method of feeding, e.g., enteral or parenteral nutri-
tion (Table 2). Electric shock can have substantial
neuromuscular effects; the ability to ingest food
orally or gastrointestinal motility may be hampered
(Table 2). Inhalation injury usually means that the
patient will be placed on a ventilator. A very high
carbohydrate intake, such as would occur if a low-
fat diet were used, can exacerbate ventilator depend-
ency, and the overall macronutrient distribution of
energy needs to be evaluated in this context. Oral
and esophageal damage also can occur with pro-
longed exposure to smoke and toxic fumes and
would counterindicate oral ingestion of food. A stress
ulcer in the stomach, known as Curling’s ulcer, which
frequently occurs in the burn patient, is now pre-
vented by prophylatic antiacid therapy. The potential
for a gastric ulcer and the poor gastric emptying that
tbl0001 Table 1 Equations for prediction of energy needs of burn patients (kcal/24 h)
a
For adults:
Curreri (Curreri PW, Richmond P, Marvin J, and Baxter CR (1974) Journal of the American Dietetic Association 65: 415)
(25 kcal preburn weight, kg) þ (40 kcal %BSA)
Long (Long C (1979) Journal of Trauma 19: 904–906)
Male: 66.5 þ (13.7 weight, kg) þ (5 height, cm) (6.8 age, years) activity factor injury factor
Female: 665 þ (9.6 weight, kg) þ (1.8 height, cm) (4.7 age, years) activity factor injury factor
where the activity factor is 1.2 confined to bed and 1.3 out of bed, and the thermal injury factor is 2.1
Toronto (Allard JP, Pichard C, and Hoskino E (1990) Journal of Parenteral and Enteral Nutrition 14: 115–118)
4343 þ (10.5 %BSA) þ (0.23 previous day’s kilocalorie intake) þ (0.84 basal energy expenditure) þ (114 previous day’s
average body temperature) (4.5 days postburn)
where basal energy expenditure is determined using the Long equations without the activity and injury factors
Ireton-Jones (Ireton-Jones C, Turner WW, Liepa GU, and Baxter CR (1992) Journal of Burn Care and Rehabilitation 13: 330–333)
629 (11 age, years) þ (25 weight, kg) (609 obesity)
where the presence of obesity is 1, and the absence is 0.
For children:
Mayes (Mayes T, Gottschlich MM, Khoury J, and Warden GD (1996) Journal of the American Dietetic Association 96: 24–29)
0–3 years: 108 þ (68 weight, kg) þ (3.9 %BSA)
5–10 years: 818 þ (37.4 weight, kg) þ (9.3 %BSA)
a
%BSA is the percentage of body surface area burned. Multiply the result of a formula by 4.18 to convert to kilojoules.
tbl0002Table 2 Pathophysiological complications of the burn patient
Related to thermal injury
Electrical burn
Inhalation damage
Gastrointestinal damage
Infection
Preexisting conditions
Cardiovascular disease
Hypertension
Obesity
Diabetes mellitus
BURNS PATIENTS – NUTRITIONAL MANAGEMENT 715

also may occur in the patient with thermal injury are
reasons why enteral (vs. oral) nutrition is used; the
stomach may be bypassed, and the feeding tube is
placed in the upper part of the small intestine.
0011 The skin is the primary barrier for the body against
the external environment. When it is lost, as in the
severely burned patient, body tissues become exposed
to the environment, which contains a variety of bac-
teria and viruses. Current therapy includes a variety
of techniques and medications to prevent and treat
infection in the burn patient. None the less, a burn
patient frequently has cutaneous infections that may
pass into the blood, causing septicemia. The fever that
accompanies an infection increases energy needs, and
septicemia also produces a hypermetabolic state.
Metabolic rate is estimated to increase about 10%
for each 1
C increase in body temperature. Nutrient
requirements need to be reevaluated in the burn
patient when an infection ensues.
0012 A thermally injured patient may have one or more
preexisting diseases that affect the overall diet pattern
(Table 2). Consideration should be given to lowering
dietary fat if the patient has significant cardiovascular
disease, and sodium if chronic severe hypertension is
present. Obesity complicates the determination of
adequate energy intakes, as well as wound closure
and healing in the burn patient. During the hyper-
metabolic phase, protein becomes a primary substrate
for energy; there is little value in providing a hypo-
caloric diet during this phase, as the obese patient will
metabolize body protein if adequate amounts are not
provided. When normal metabolic pathways resume,
consideration can be given to a modest (10–25%)
reduction in estimated energy needs when the burn
patient is obese. Careful and continual coordination
of insulin availability, blood glucose concentrations,
and food intake is needed in the burn patient who also
has type 1 diabetes mellitus, the form of the disease in
which the body does not produce insulin. Similar
monitoring is also needed for the person with type 2
diabetes, in whom insulin response to food intake is
not normal, but monitoring is less frequent. Extra
care also is needed if the patient with diabetes is
given a very high (more than 55–60% of kilocalories)
carbohydrate diet.
0013 Many of the problems associated with tube feed-
ings can be avoided by the experienced clinician. If
the infusion rate is too fast and administration of the
feeding too frequent, there can be potential problems,
particularly for burn patients, for the simple reason
that they have to be given more in order to meet their
nutrient needs. Gastrointestinal stress that usually
occurs in the burn patient is manifest as a poor empty-
ing of the stomach; thus, ‘residuals,’ or the amount of
feeding remaining 2 h after its administration, need to
be determined frequently if the feeding tube is placed
in the stomach. It is also important to keep the head
of the patient elevated (at least a 30
angle) to prevent
aspiration, which is the movement of gastric contents
toward the mouth and subsequent entrance into the
trachea and ultimately the lungs.
0014Since the feeding tube may be in place for a long
period of time, smaller-diameter tubes are used,
because they are less irritating. These smaller-bore
tubes, however, cause mechanical problems, because
they become more easily clogged. Clogged tubes are
prevented by a rigorous maintenance protocol and by
not administering ground, solid medications through
the tube.
0015Gastrointestinal complications of tube feedings
include nausea and vomiting, diarrhea, constipation,
and abdominal cramping or pain, all of which also
can be caused by the injury and by medications unre-
lated to nutrient intake. Many of the gastrointestinal
problems can be prevented by maintaining constant
administration of the feeding with a pump. Nausea,
vomiting, and abdominal cramping may be a result of
retention of food in the stomach; if this does not
resolve spontaneously within a couple of days, the
tube can be repositioned so that food is delivered to
the gastrointestinal tract beyond the stomach. Diar-
rhea can be caused by gastrointestinal dysfunction,
too rapid a rate of administration, and bacterial
infection in the gut.
Metabolic Modulators
0016Several new therapies have been proposed to counter-
act the catabolism and hypermetabolism that accom-
pany a burn injury. However, many of the studies to
evaluate these new therapies have been very limited in
scope or conducted using animal models or critically
ill patients who were not burned. This is an active
area of research, but data available at this time do not
support the use of most of these therapies. Growth
hormone administration does not appear to benefit
the burn patient. Very high doses of insulin appear to
reduce protein losses, but such doses have not been
well accepted by burn centers, as they require
frequent blood glucose monitoring. Arginine and
glutamine are viewed as conditionally essential
amino acids, that is they are indispensible in situ-
ations of severe metabolic stress when body synthesis
may be inadequate. No convincing evidence exists
that they are of benefit specifically in the burn patient,
although they are included in some protocols, on the
basis that they may help and are unlikely to hamper
recovery.
0017The use of a particular group of enteral feedings,
called immune-enhancing therapies, for the burn
716 BURNS PATIENTS – NUTRITIONAL MANAGEMENT

patient is clearly controversial, with the results of
studies indicating a beneficial effect, no effect, or
possibly a detrimental effect on the burn patient.
These formulas contain various amounts of dietary
nucleotides, arginine, glutamine, carnitine, taurine,
and/or o-3 fatty acids. These formulas are three two
four times more costly than standard enteral formu-
las, and few of these ingredients have been evaluated
for their independent effects.
0018 Metabolic complications of enteral feedings include
hyperglycemia, hypertonic dehydration, hypernatre-
mia, hyperkalemia, hypokalemia, and hypophospha-
temia. Hyperglycemia can be caused by sepsis or
severe infection and the hypermetabolism that
accompanies a thermal injury. Hyperkalemia may
signal compromised cardiac output or renal function.
Generally, these metabolic complications are very
rarely caused by the enteral feeding in the burn
patient, because intake is so closely monitored.
See also: Children: Nutritional Requirements; Coronary
Heart Disease: Intervention Studies; Dietary
Requirements of Adults; Electrolytes: Analysis; Acid–
Base Balance; Energy: Measurement of Food Energy;
Intake and Energy Requirements; Measurement of
Energy Expenditure; Enteral Nutrition; Hypertension:
Hypertension and Diet; Infection, Fever, and Nutrition;
Parenteral Nutrition; Protein: Digestion and Absorption
of Protein and Nitrogen Balance
Further Reading
Berger MM and Shenkin A (1998) Trace elements in trauma
and burns. Current Opinion in Clinical Nutrition and
Metabolic Care 1: 513–517.
Deitch EA (1995) Nutritional support of the burn patient.
Critical Care Clinics 11: 735–750.
Garrel DR, Razi M, Larivie
`
re F et al. (1995) Improved
clinical status and length of care with low-fat nutrition
support in burn patients. Journal of Parenteral and
Enteral Nutrition 19: 482–491.
Gottschlich MM and Warden GD (1990) Vitamin supple-
mentation in the patient with burns. Journal of Burn
Care and Rehabilitation 11: 275–278.
Gueugniaud P-Y, Bertin-Maghit M, Petit P and Cardin
H(2000) Current advances in the initial management
of major thermal burns. Intensive Care Medicine 26:
848–856.
Hansbrough JF (1998) Enteral nutritional support in burn
patients. Gastrointestinal Endoscopy Clinics of North
America 8: 645–667.
Heyland DK and Novak F (2001) Immunonutrition in the
critically ill patient: more harm than good? Journal of
Parenteral and Enteral Nutrition 25: S51–S55.
Khorram-Sefat R, Behrendt W, Heiden A and Hettich R
(1999) Long-term measurements of energy expenditure
in severe burn injury. World Journal of Surgery 23:
115–122.
Mayes T (1997) Enteral nutrition for the burn patient.
Nutrition in Clinical Practice 12: S43–S45.
Raff T, Germann G and Hartman B (1997) The value
of early enteral nutrition in the prophylaxis of stress
ulceration in the severely burned patient. Burns 23:
313–318.
Rodriguez DJ (1995) Nutrition in patients with severe
burns: state of the art. Journal of Burn Care and
Rehabilitation 17: 62–70.
Scaife CL, Saffle JR and Morris SE (1999) Intestinal ob-
struction secondary to enteral feedings in burn trauma
patients. Journal of Trauma: Injury, Infection and
Critical Care 47: 859–863.
Schloerb PR (2001) Immune-enhancing diets: products,
components, and their rationales. Journal of Parenteral
and Enteral Nutrition 25: S3–S7.
Vandevoort M (1999) Nutritional protocol after acute
thermal injury. Acta Chirurgiae Belgium 99: 9–16.
BURNS PATIENTS – NUTRITIONAL MANAGEMENT 717

BUTTER
Contents
The Product and its Manufacture
Properties and Analysis
The Product and its
Manufacture
E Richards, Bridgend, UK
A M Fearon, The Queen’s University of Belfast, Belfast,
UK
Copyright 2003, Elsevier Science Ltd. All Rights Reserved.
Background
0001 Butter has long been recognized as a valuable food.
Its method of manufacture has changed little over the
years except in respect of the equipment used. The
traditional craft methods have given way to large-
scale sophisticated continuous production, but both
can still be found.
0002 In the process of buttermaking, cream is subjected
to severe agitation or ‘churning.’ This causes physical
damage to the milk fat globules and results in phase
inversion from the oil-in-water emulsion of cream to
the water-in-oil emulsion of butter. Butter is com-
posed of a continuous fat phase and a dispersed
phase comprising water and globular fat. (See Col-
loids and Emulsions.)
0003 Butter is permitted to contain certain other ingredi-
ents. These include salt (sodium chloride), coloring
agents such as carotenes and annatto, acidity regula-
tors, and starter cultures for the manufacture of lactic
or ripened butter.
0004 Production of premium quality butter requires
attention to the quality of the raw material, process
hygiene, and efficiency. The equipment used in
creameries today makes a product of more uniform
flavor and texture than the older craft methods and
from a better-quality raw material.
0005 Economic forces are emphasizing the need to maxi-
mize efficiency and flexibility in processing and pro-
duction methods. Butter manufacturers have had to
reexamine their product properties and investigate
technological and other means to enhance these in
the eyes of consumers. (See Butter: Properties and
Analysis.)
Types of Butter
0006 Sweet cream:
.
0007salted with a salt content normally about 2%, but
can vary from 1.5 to 3%;
.
0008unsalted.
0009Lactic:
.
0010slightly salted with a salt content of approximately
1%;
.
0011unsalted.
0012Whey:
Sometimes called ‘farmhouse butter.’ This is found in
localized areas and is manufactured from whey cream
– a by-product of cheesemaking. The salt content is
about 2%. (See Whey and Whey Powders: Production
and Uses.)
Raw Materials
0013The quality and handling of the raw material are
of paramount importance in achieving a premium-
quality end product.
Cream
0014The essential elements are:
.
0015clean milk;
.
0016efficient separation to a specific fat content;
.
0017efficient pasteurization (heat treatment) and
cooling;
.
0018good temperature control during storage;
.
0019care in the physical handling of the cream.
(See Cream: Types of Cream.)
0020Raw milk for butter manufacture must contain less
than 100 000 microorganisms per milliliter. In fact,
milk with a much lower microbiological content (less
than 20 000 organisms per milliliter) is now com-
monly obtained from UK herds. The quality schemes
in operation within the UK insure good milk quality,
and this is reflected in dairy product standards. (See
Milk: Processing of Liquid Milk.)
0021Milk is separated into cream and skimmed milk by
means of a centrifugal separator. At all stages in the
handling of the milk and in the preparation of the
cream, care is taken to avoid damage to the fat glob-
ule membrane (FGM) by excessive pumping or tur-
bulence. The FGM is composed primarily of protein
718 BUTTER/The Product and its Manufacture

and phospholipid and stabilizes the fat phase in milk
while also protecting the fat from oxidation and
enzyme attack. Separators are designed to cause as
little damage as possible, while achieving a high degree
of efficiency.
0022 The optimum fat percentage of the cream, to
obtain the maximum churning efficiency, needs to
be adjusted according to the method and equipment
used to make the butter. Traditional methods advise a
fat content of 30–35%, whereas modern continuous
buttermakers normally operate at 40–44% butterfat
for sweet cream and 38–40% butterfat for an acid or
cultured cream.
0023 Cold separation (<10
C) has the advantage that
milk may be processed on arrival at the factory. Al-
though the separation is less efficient, free fat levels
are low, and the cream has a higher phospholipid
content. This improves its whipping properties.
0024 Heat treatment of the cream can be achieved on a
small scale by heating in a vat to a temperature of not
less than 63
C and holding the cream at that tem-
perature for at least 30 min. This ‘holder method’ is
slow and inefficient, as heating and cooling are
carried out in the same vessel. It is only suitable for
small quantities of cream.
0025 For larger-scale production, cream is treated in a
continuous high-temperature, short-time (HTST)
plate heat exchanger to a minimum of 72
C for at
least 15 s. At higher processing temperatures, there is
a danger of oxidative rancidity promoted by migra-
tion of copper from the serum to the fat globules.
For this reason, it is recommended that cream used
for buttermaking be processed at a maximum of
77
C for 15 s. However, in practice, flash heating to
85
C is often used to produce a desirable slightly
nutty or caramelized flavour. (See Pasteurization:
Principles.)
0026 Feed and weed taints concentrate in the fat phase of
milk, and these may be removed by vacreation, a
form of heat treatment under vacuum. The heated
cream is held in contact with steam under reduced
pressure, then separated to allow volatile taints
to be drawn off. This is a combined heating and
flavor-stripping treatment. Evaporative cooling to ap-
proximately 60
C may also be used to adjust the fat
content of the cream. The final cooling of the cream
takes place in a plate heat exchanger. A milder, flavor-
stripping method using vacuum treatment after an
HTST process may also be used.
0027 The cream used for buttermaking must be cooled
and stored at a low temperature to encourage crystal-
lization of the fat. This period, usually a minimum of
8 h, is often called ‘ageing’ the cream. The latent heat
released will increase the temperature of the cream to
7–8
C from the initial cooled temperature of 5
C.
Aging is essential to achieve a low fat loss into the
buttermilk and produce butter of the desired texture.
(See Butter: Properties and Analysis.)
0028Both the rate of cooling and the temperature of
holding are important in determining the size of the
fat crystals and the proportion of solid-to-liquid fat
achieved within the final butter. Large silo tanks for
storage are preferable to a series of small cream tanks.
There is improved homogeneity, allowing the butter-
making equipment to operate with a more consistent
product for a longer period.
0029Cream temperature treatments (‘Alnarping’) may
be applied to improve butter spreadability and pro-
duce a consistent butter despite seasonal variation
in milk fat composition. However, these have had
limited success. A more effective means has been
through altering the cow’s diet to increase the propor-
tion of unsaturated fatty acids in milk fat. This
reduces butter firmness at low temperatures. Incorp-
orating vegetable oils into cream and applying mar-
garine process technology have been very successful
developments, but the resultant products may not
be identified as ‘butter’.(See Butter: Properties and
Analysis.)
Water
0030Water, wherever used, must be of the highest possible
microbiological quality.
Lactic Cultures
0031A soured or ripened cream is traditionally required
to produce lactic butter. Although it is possible to
allow milk or cream to sour naturally, it is neither
advisable nor practical. A culture of lactic micro-
organisms – Lactococcus lactis subsp. cremoris (for-
merly Streptococcus cremoris), Lactococcus lactis
ssp. lactis (formerly Streptococcus lactis), Lacto-
coccus lactis biovar. diacetylactis (formerly Strepto-
coccus diacetylactis) – may be added to the cream
to produce the desired acidity, flavor, and aroma.
The primary aroma producers are L. lactis biovar.
diacetylactis and Leuconostoc mesenteroides ssp.
cremoris.(See Lactic Acid Bacteria.)
Salt
0032Salt adds flavor and also acts as a preservative in
sweet cream butter. For short-term storage, bulk
butter is stored at temperatures of 18
C whether
it has added salt or not. Intervention (EC-subsidized)
butter – for long-term storage – is unsalted and is
stored at 25
C.
0033Only pure, finely milled, vacuum-dried salt (of at
least BSI 998 (1969) or equivalent standard) should
be used for butter.
BUTTER/The Product and its Manufacture 719
Manufacturing Processes
Churn Method
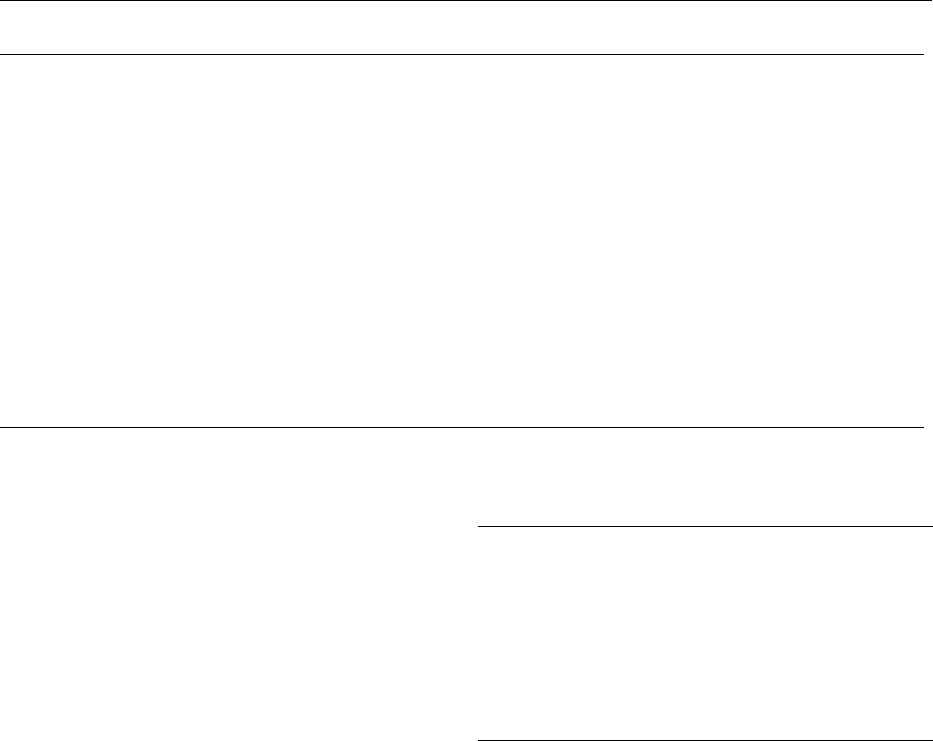
0034 Batch process A batch-type butter churn may vary
in capacity from a few liters up to maximum of about
45 000 l. These churns were originally made of wood
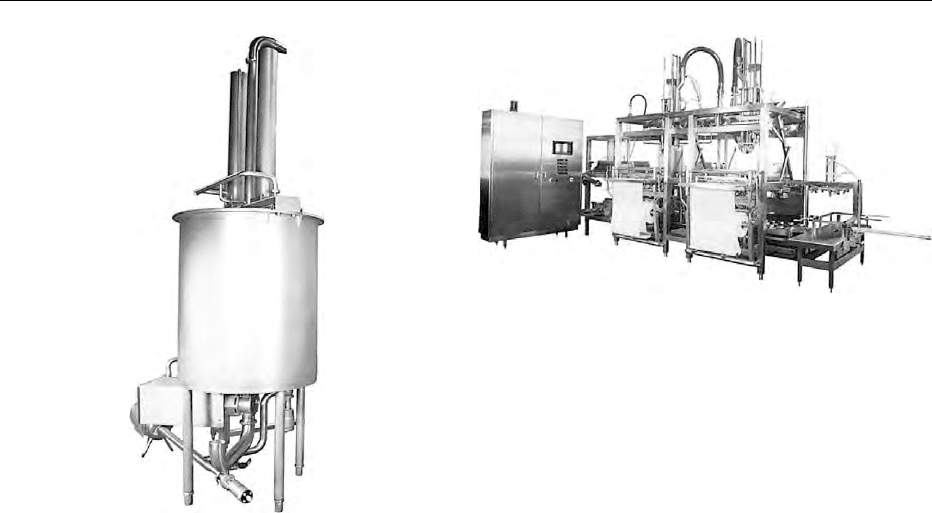
(Figure 1) but latterly of stainless steel (Figure 2).
0035 After cleaning and disinfection, the churn must be
specially prepared to prevent the butter from sticking
to the surface. With wood, this is achieved by scalding
with boiling water and immediately cooling with
chilled water. This treatment leaves a film of water
on the surface of the wood and prevents the butter
from adhering to it. All wooden equipment must be
kept wet until used.
0036 The surface of stainless steel equipment also re-
quires special physical preparation. The detergents
used in the cleaning of such equipment must contain
silicates to maintain the special ‘nonstick’ surface.
(See Cleaning Procedures in the Factory: Types of
Detergent; Types of Disinfectant.)
0037 Batch butter churns may be barrel- or cone-shaped
with fixed or rotating internal ‘workers.’ As the churn
is rotated, the combined actions of rotating and
beating cause the cream emulsion to break, forming
the butter grains (fat phase) and buttermilk (aqueous
phase).
0038During the first few turns, gases, e.g., carbon diox-
ide from heterofermentative fermentation, may be
liberated from the cream. In order to maintain an
even pressure within the churn, it is necessary to
release these gases. This is done by depressing a
small valve in the lid of the churn.
0039Each churn has an indicator glass – a small window
through which it is possible to see what is happening
inside the churn. When hand churning, the cream
feels heavier as it begins to thicken. This takes about
15–20 min from the beginning of churning. The cream
emulsion breaks and small grains of butter form.
These are clearly seen on the indicator glass. The
actual size of the butter grains varies according to
the type and size of the churn. It is essential not to
allow them to grow and form lumps, which will cause
an uneven distribution of buttermilk.
0040For hand churning, the grains should be kept small,
approximately 3 mm in diameter – traditionally
stated as the size of wheat grains.
0041Chilled water at approximately 5
C is added to
harden and control the size of these grains, as well
as removing the traces of buttermilk. Washing re-
duces the yield, and is not necessary if the cream is
of good quality and all the necessary hygienic precau-
tions have been observed in the preparation of the
butter churn.
0042Salt may be added dry or in the form of brine as a
final wash. The addition of brine (10% solution) to
butter grains has been used to reduce the need for
chilled water. This can be important during warm
weather when there is a lack of chilled water. It will
fig0001 Figure 1 Wooden butter churn (nineteenth century). From
National Museums and Galleries of Northern Ireland, Ulster
Folk & Transport Museum, with permission.
fig0002Figure 2 (see color plate 12) Stainless steel batch butter churn
(twentieth century). From APV Unit Systems, Denmark, with per-
mission.
720 BUTTER/The Product and its Manufacture
also prevent streakiness due to uneven mixing of the
salt. For dry salting, the calculated quantity is
sprinkled on to the butter grains to give approxi-
mately 2% in the final product.
0043 The butter grains are ‘worked’ to expel excess
moisture, create an even, fine distribution of water
droplets and produce a close textured, evenly colored
product. This may be carried out using the workers
inside the churn or externally on a small scale, by using
Scotch hands. These are made of grooved wood (or
plastic) and are also used to shape and print attractive
designs on the finished packs (Figure 3).
0044 During the period of working, drainage, and add-
ition of dry salt, samples are tested to determine the
salt and moisture contents. The operator determines
the ‘end point’ of working when the moisture content
is between 15.5 and 16% and by visual assessment of
the butter. At this stage, the butter is removed from
the churn in readiness for packing.
0045 The moisture content of butter must not exceed
the legal maximum of 16%. Manufacturers attempt
to be as near to that limit as possible to ensure the
maximum yield.
0046 Cultured butters Traditionally, cream is inoculated
with specific cultures of bacteria. The reduction in pH
and development of flavors produce a lactic-flavored
end product. This is regarded by some as a more
desirable product, i.e., a fuller-flavored butter. (See
Starter Cultures.)
0047 This method of making butter requires starter cul-
ture facilities with the necessary laboratory controls,
and additional equipment such as cream-ripening
tanks as well as cooling and aging facilities. There
must also be a well-controlled program of tempera-
ture controls and pH monitoring.
0048The cream is inoculated with approximately 1% of
culture and incubated at 20–27
C to achieve a final
pH of 5.3–4.7, depending on the preferred lactic
flavor. The cream is then cooled to stop the fermenta-
tion and to attain the desired fat crystallization.
0049The method of manufacture on a batch basis is no
different from that employed for sweet cream. The
disadvantage of this traditional system is that the
buttermilk has a lactic content that causes problems
in its disposal. The behavior of the starter culture is
not always consistent, and this can result in end-
product variations.
0050Because of the problems and expense of culturing
cream and the disposal of ‘lactic’ buttermilk, several
methods have been developed to make lactic or
cultured butter from sweet cream.
0051The NIZO method developed in the mid-1970s
consisted of churning sweet cream and adding a
special mix containing cultured whey concentrate
and bacterial culture while working the butter grains.
This gave the major advantage of being able to manu-
facture from sweet cream, thus producing sweet
cream buttermilk, which has a far greater commercial
value than cultured cream buttermilk.
0052The indirect biological culturing system, as de-
scribed, for example, by Pasilac – Danish Turnkey
Dairies Ltd, involves the addition of two types of
prepared starter culture to the churn at the working
stage. The combination of aroma-producing bacteria
and the acidity of the culture mix result in the final
pH and flavor of the butter conforming to that of
traditional cultured butter.
0053The addition of a starter distillate provides an al-
ternative method of flavoring butter without the need
for culturing equipment, while acidity is increased by
addition of lactic acid.
Continuous Buttermaking
0054Continuous buttermaking equipment began to be
widely used in the 1960s. The success of this equip-
ment was such that, within a decade, most of the
batch churns used in commercial butter manufacture
had been superseded.
0055Continuous buttermaking equipment gives an ad-
vantage over the batch process in terms of hygiene,
uniform product quality, and process efficiency.
0056Cream processing is an integral part of the
whole buttermaking system. The preparation of
the cream is similar to that for traditional manufac-
ture. From the storage tanks, it is pumped into the
first stage of the buttermaker at a constant speed and
temperature.
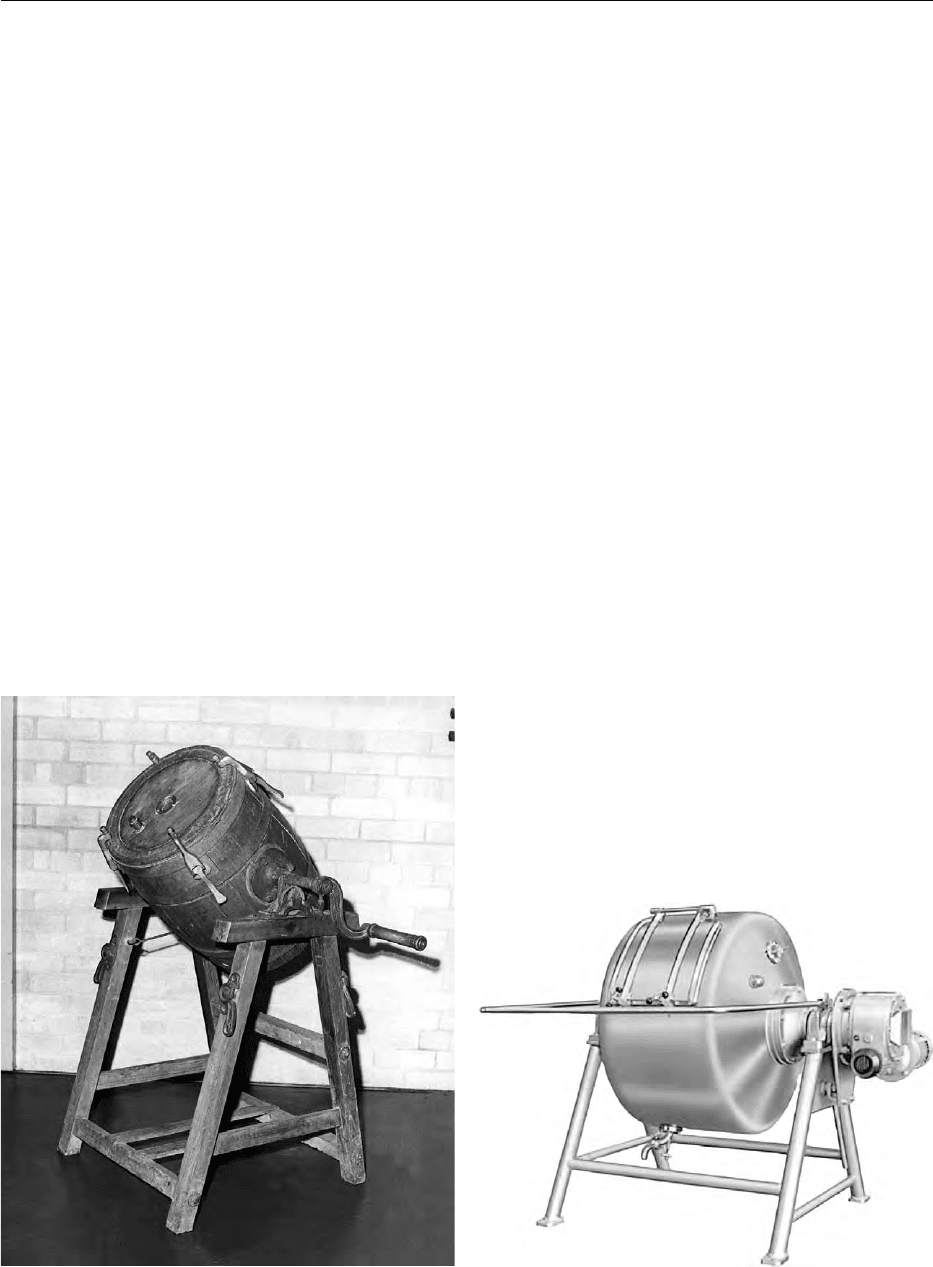
fig0003 Figure 3 Using Scotch hands to work butter. From National
Museums and Galleries of Northern Ireland, Ulster Folk & Trans-
port Museum (L882/10), with permission.
BUTTER/The Product and its Manufacture 721
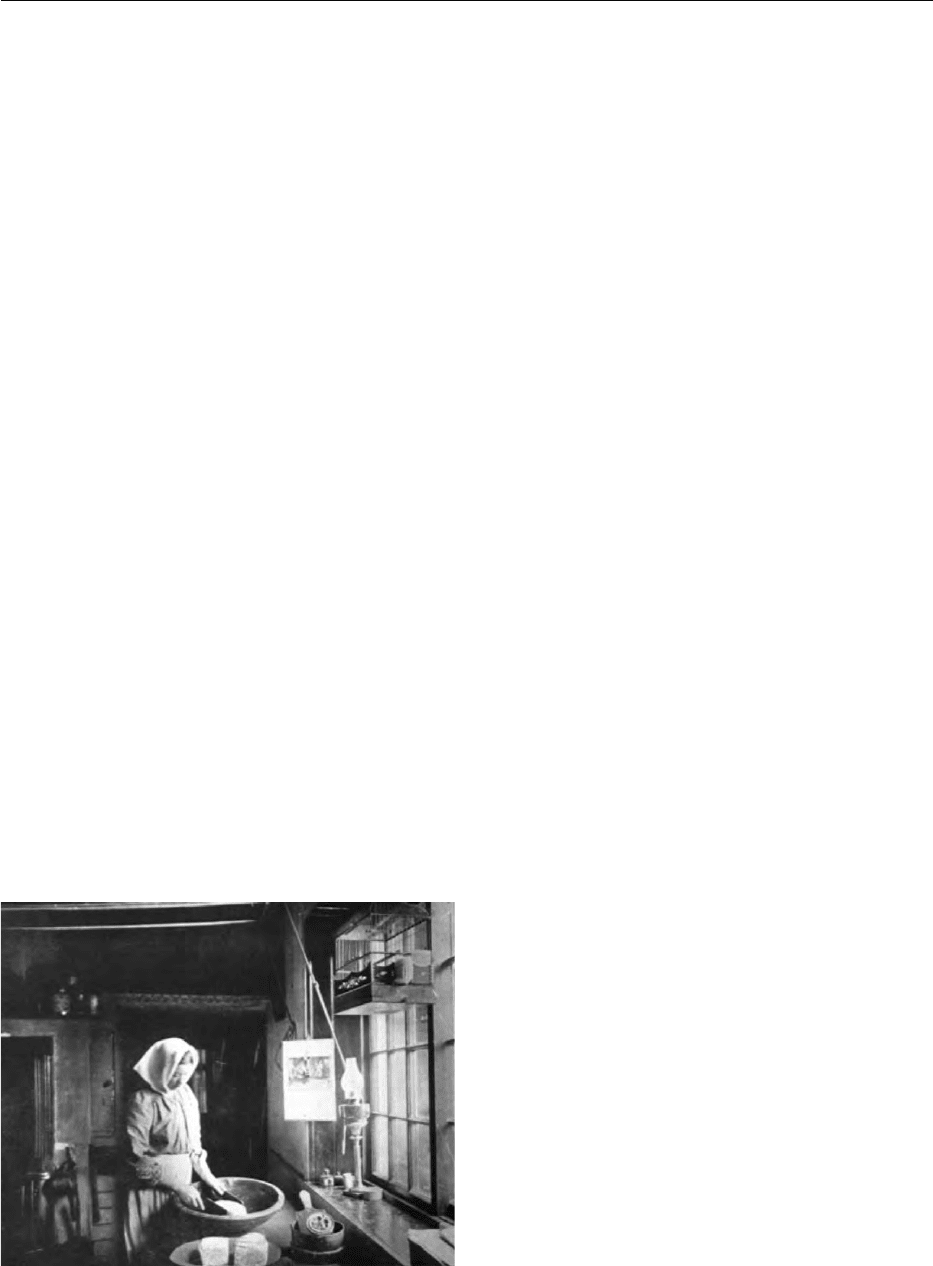
0057 The capacity of continuous buttermakers varies
from small units of 12 kg h
1
to more than
10 000 kg h
1
(Figure 4).
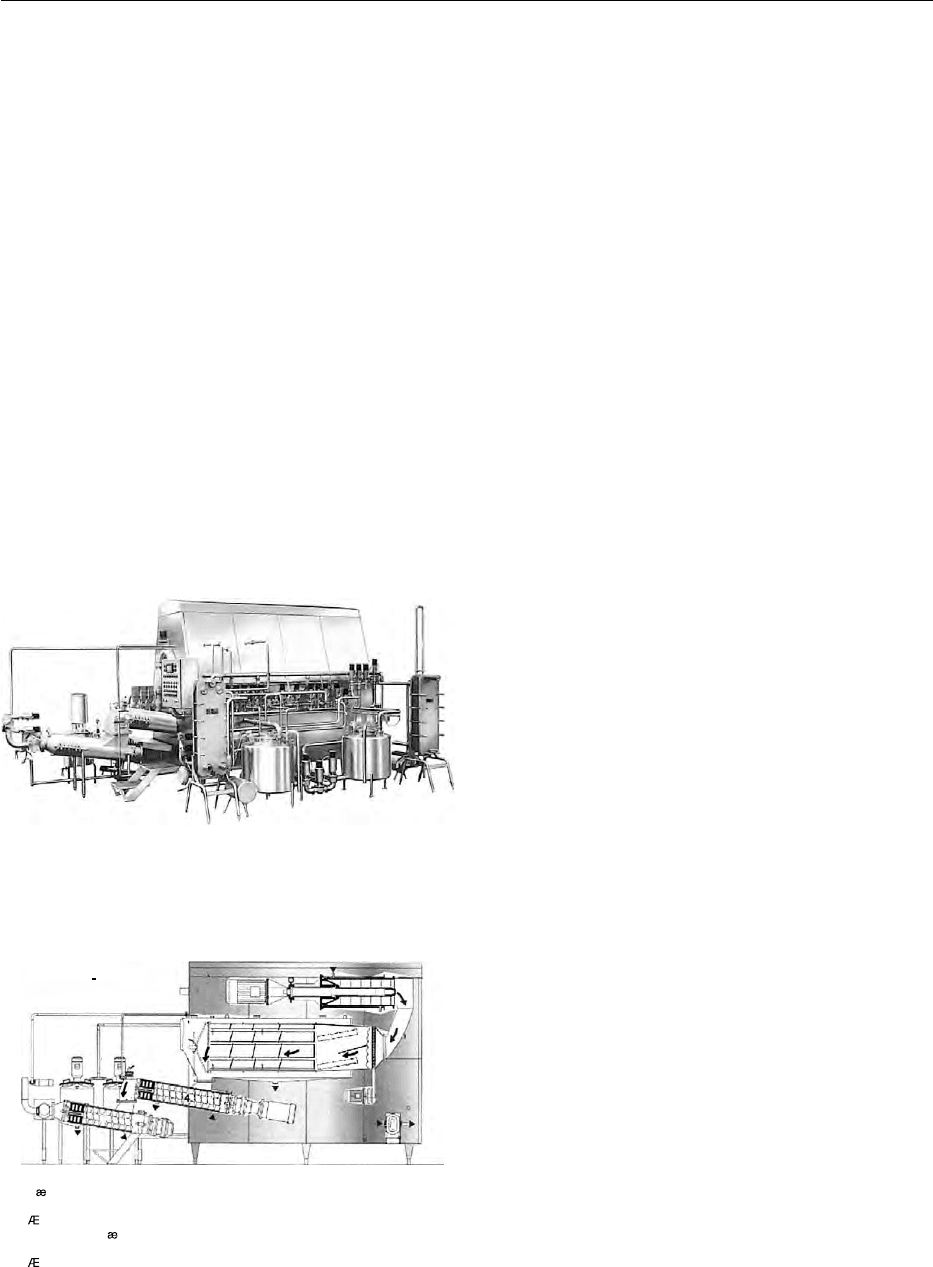
0058 Although design features vary, the basic principles
remain the same. A continuous buttermaker consists
of: (1) the churning section; (2) the separating section
and (3) the working section(s) (Figure 5).
0059 Churning section A multibladed beater operating at
high speeds (approximately 1000 rpm) within a cylin-
drical chamber introduces air into the cream and
damages the fat globules. The distance between the
cylinder wall and the beater blades is only 2–3mm.In
just a few seconds, the cream emulsion is broken, and
the initial agglomeration of fat globules takes place. A
mixture of small butter grains and buttermilk is then
transported from this beating chamber into the next
unit, the separating chamber.
0060 Separating chamber This consists of a rotating
drum where the final churning takes place and in
which there is a perforated filter – a separation
drum – to separate the buttermilk from the butter
granules. The drum rotates slowly so that as the
buttermilk is drained away, the butter grains are
gradually clumped together.
0061Cooling may be achieved by circulating chilled
water in the walls of either churning chamber. In
some machines, the first buttermilk is cooled and
recirculated. It is in this particular section that the
grains of butter are allowed to grow to the required
size.
0062The speed of the beaters, the temperature of
churning, and the butterfat content of the cream will
all vary slightly. An experienced butter manufacturer
will adjust these parameters according to the season,
equipment, texture, and consistency of the resultant
butter. A firmer milk fat and, therefore, firmer butter
are obtained in winter than in summer. In addition,
the temperature of the cream has to be maintained at
a lower temperature, e.g., 5–7
C, in summer, whereas
it could be at 10
C in winter.
0063There is an observation window for the operators –
similar to the sight glass of traditional equipment.
The control panels may also have display screens,
allowing operators to observe the processes inside
the machine.
0064Working sections Augers transport the butter along
the working sections and through aperture plates.
The process kneads or works the butter, expelling
more buttermilk and influencing the final body and
texture of the finished product. The moisture droplets
must be fine and evenly dispersed.
0065During this process of working, salt (if required) is
added in the form of a 50% saturated slurry. Water
may be added to adjust the final moisture content,
and in the case of lactic butters, the mix of flavor
distillates or concentrated bacterial cultures is added
at this stage. The second part of the working section
operates at a much higher speed to ensure that the
culture or salt is correctly distributed.
0066The working sections are cooled with chilled water.
The link between the first and second working
sections operates under vacuum. This provides con-
trolled deaeration of the butter, thus giving the end
product a very close texture and improving the shelf-
life. The body and texture of butter worked under
vacuum are quite different from the open structure of
traditionally worked butter.
0067To allow for the stoppages that must occur during
normal production, a ‘balance tank’ is maintained
between the buttermaker and packing equipment to
buffer flow variation (Figure 6). This butter ‘trolley,’
as it is known, is constructed of stainless steel and
performs the essential task of maintaining the flow of
Standardudforelse:
Standard design:
Standardausfuhrung:
3
2
1
5
6
4
7
8
1. Flodepumpe 1. Cream pump
2. Chuming section
3. Separating section
4. Working section I
5. Regulating gate
6. Vacuum chamber
7. Working section II
8. Butter pump
1. Rahmpumpe
2. Butterungsabteilung
3. Trennabteilung
4. Knetabteilung I
5. Reglerplatte
6. Vakuumkammer
7. Knetabteilung II
8. Butterpumpe
3. Separeringsafdeling
6. Vakuumkammer
8. Smorpumpe
2. K meafdeling
5. Reguleringsspj ld
4. teafdeing l
7. teafdeing lI
fig0005 Figure 5 Schematic outline of a continuous buttermaking
machine. From APV Unit Systems, Denmark, with permission.
fig0004 Figure 4 Continuous buttermaking machine. From APV Unit
Systems, Denmark, with permission.
722 BUTTER/The Product and its Manufacture
butter both from the buttermaker and to the packing
equipment.
Packing
0068 Wholesale The butter is packed in bulk or retail
packs directly from the churn or from the trolley of
a continuous buttermaker. Bulk butter is normally
packed in 25-kg quantities in cardboard cartons.
These can be lined with parchment paper, but colored
polythene, enabling the inner wrapper to be readily
seen, is the preferred lining material.
0069 The simplest form of bulk butter packer is the
‘Vane’-type packer – this is simply a hopper into
which the butter is fed, either manually or pumped
from the buttermaker trolley. The butter is extruded
by a screw-conveyor through a suitably sized nozzle
into the lined carton. When the carton is full, the flow
of butter is stopped, and the butter is ‘cut’ with a
heated wire. The full carton is then removed and
checked for weight, which is adjusted manually. The
liner is closed, ensuring there is no exposed product,
and the carton is sealed, coded, and palletized. The
normal quantity is 50 cases of 25-kg butter per pallet.
0070 For large-scale production, automatic packers are
normally an integral part of continuous buttermaking
installations (Figure 7). The cardboard cartons are
loaded flat, and the inner wrap is polythene from a
reel. The machine forms the carton, lines it, and
presents it for filling. Once full, the weight is checked,
and if necessary, additions are made via an ‘injection
unit,’ which adds the required quantity of butter
below the original surface.
0071On achieving the correct weight (25 kg), the liner is
folded over the top surface, and the carton is closed,
sealed, and coded. This minimal exposure to possible
contamination has contributed greatly to the exten-
sion of the keeping quality of butter. Automatic pal-
letization is also a feature of some installations.
0072Retail Butter is required to be sold in metric quan-
tities. Most retail packs are in 250- or 500-g weights.
The shape of the packs vary from a brick of differing
dimensions to rolls, and packs may be foil- or parch-
ment-wrapped. Attractively designed plastic tubs
holding 250 or 500 g are also available.
0073For retail packing, the butter is formed in an ap-
propriately shaped chamber on a rotating drum. This
formed portion (roll or brick) is pushed out of the
chamber into the waiting coded wrapper (parchment
or foil), which is then folded. The portions are check-
weighed before passing onwards to an automatic case
packer and palletizer. The butter at this stage is still
very soft in consistency, and any mishandling is likely
to deform the portion.
0074Catering butter portions are packed in foil or plas-
tic tubs with foil lids. The machines developed to
pack this size of butter portion must operate at max-
imum efficiency. The quality of the butter, in terms of
body and texture, is of secondary importance. The
butter is extruded into the partly folded foil held
within a shaped chamber, and the folding is then
completed. Alternatively, the butter is discharged
into a plastic tub before sealing.
0075Larger catering packs, e.g., 2-kg plastic tubs, are
filled by extrusion before the lid is applied.
0076Reworked butter For marketing or distribution
reasons, it may be necessary to rework bulk butter.
fig0006 Figure 6 Butter buffer tank. From APV Unit Systems, Denmark,
with permission.
fig0007Figure 7 Butter packing line. From APV Unit Systems,
Denmark, with permission.
BUTTER/The Product and its Manufacture 723

This butter, in 25-kg blocks that have been stored at
either 18 or 25
C, can be either attemperated,
i.e., brought to a temperature suitable for packing,
before working, or handled frozen.
0077 Attemperation traditionally involves placing bulk
butter in a store at 5–8
C for a period to attain that
temperature. The use of microwave tunnel heaters
has reduced the space and time necessary, and is a
more efficient way of attemperation. Blocks of butter
may be brought up to blending temperature within
hours, then blended and standardized on a batch or
continuous basis to the required salt and moisture
contents for packing.
0078 An alternative process employs a butter reworking
system that first chops the frozen butter blocks into
strips. The spaghetti-like strips of butter leave the
chopping unit at a temperature of 0–2
C. They
are then transferred into the blender where they are
worked several times and vacuum-treated before
repackaging in retail units (Figure 8).
Product Evaluation
007 9 Notwithstanding the aesthetic requirements of pack-
aging and any legal requirements, the most important
quality parameters of butter are its taste and keeping
quality.
0080 The modern continuous machines and their associ-
ated equipment are normally cleaned in place (CIP).
Close collaboration between the design engineers, op-
erators, and quality controllers is necessary to ensure
effective cleaning. (See Plant Design: Basic Principles;
Designing for Hygienic Operation; Process Control
and Automation.)
0081 Attention to detail, monitoring the critical aspects
of the process, whether it be batch or continuous, is
essential. It is, however, normal to sample the finished
product to confirm that the desired microbiological,
chemical, and organoleptic qualities have been
achieved.
Microbiological
0082Microbiological guidelines for the acceptance of bulk
butter into intervention storage are described by the
Intervention Board for Agricultural Produce. For
butter to be acceptable, it must have:
0083Total viable count: < 1000 organisms per gram
(maximum 5000);
0084Coliforms: absent in 1g;
0085Yeasts and molds: less than 10 g
1
.
Chemical
0086Butter composition and protection of use of the des-
ignated term ‘butter’ are described by the EC Council
Regulations No. 1898/87 and No. 2991/94, respect-
ively. Butter must contain not less than 80% milk fat
but not exceeding 90%; a maximum water content of
16% and a maximum dry nonfat milk material (milk
solids not fat) of 2% are permitted. Substances neces-
sary for the manufacture of butter may be added, but
such substances may not be used to replace in whole
or part any milk constituent. Regulations for butter
composition in other major butter-producing coun-
tries, New Zealand (Regulation 111. Butter, Food
Regulations 1984) and USA (US Code of Federal
Regulations Title 7, Volume 3, 7CFR58.345 and
Title 21, Section 321a), are similar to the EC regula-
tions. However, the New Zealand regulations also
permit the fat phase used to prepare butter to
be standardized for consistency by the removal or
addition of physically fractionated fractions, pro-
vided that the fatty acid profile of the butter falls
within the typical range. Such a product must then
be identified as ‘standardized butter’. The Australian
New Zealand Food Standards Code may be found at
www.anzfa.gov.au/foodstandardscode/.
0087Constant monitoring of the moisture and salt levels
– where appropriate – is carried out during process-
ing. On-line devices are available that link the
machine controls to the moisture and salt determin-
ations. These are necessary to match the manufactur-
ing speeds now possible where traditional chemical
analysis is too slow. However, these automated
techniques still require calibration against standard
laboratory methods.
Organoleptic Grading
0088The grading of butter involves much more than the
tasting of the product. Grading normally takes place
no less than 48 h after manufacture – a period neces-
sary to allow the butter to ‘cool’ and ‘settle.’ Scoring
standards and identification of defects are described
for butter for intervention storage in the Official
Journal of the European Community (1995) No.
fig0008 Figure 8 (see color plate 13) Butter reworking system. From
APV Unit Systems, Denmark, with permission.
724 BUTTER/The Product and its Manufacture
