Caballero B. (ed.) Encyclopaedia of Food Science, Food Technology and Nutrition. Ten-Volume Set
Подождите немного. Документ загружается.


with a riboflavin standard under identical irradiation
conditions for the sample and standard solution.
0009 Although the original lumiflavin method is rarely
used, the principal methodology has been applied to
high-performance liquid chromatography (HPLC)
analyses of riboflavin content in foods with detection
limits of 0.02 ng of riboflavin per injection.
Microbiological Assay
0010 Besides bioassays, as in chicken and curative rat
growth tests, for example, microbial assays are the
first widely used test methods, measuring the bio-
logical activity of preparations containing total vita-
min B
2
. The most frequently used test organism is
Lactobacillus casei ssp. rhamnosus (ATCC No.
7469). The detection limit is indicated to 0.5 ng of
riboflavin absolutely. Occasionally, other test organis-
mus are proposed such as Enterococcus faecalis
(ATCC No. 10100) or Leuconostoc mesenteroides
(ATCC No. 9135) with an enhanced sensitivity of
0.1 ng per milliliter of riboflavin. Microbiological
assays with L. casei have been approved by the Asso-
ciation of Official Analytical Chemists International
Methods for riboflavin determination in vitamin
preparations. The growth response of bacteria is pro-
portional to the riboflavin content of the medium and
can be measured turbidimetrically. Earlier techniques
determined metabolically formed lactic acid by titra-
tion. However, comparisons of turbidimetrically after
16 h of incubation yielded results that agreed with
those obtained by titration of lactic acid after 72 h.
Thus, turbidimetric measurement is currently pre-
ferred in view of its shorter incubation time and easier
handling.
0011 The growth response of Lactobacillus species
differs significantly between free riboflavin and
FMN and FAD. Acidic or enzymatic treatment is
therefore needed for releasing and converting the fla-
vins into riboflavin, as described in Methods of De-
termination, followed by adjustment of the extract to
pH 4.5 before incubation. In case of enzymatic re-
lease using takadiastase or clarase, it should be noted
that some enzyme preparations contain variable
traces of riboflavin.
0012 Starch, glycogen, free fatty acids and other lipids,
and protein degradation products can interfere with
the test by either stimulating or inhibiting bacterial
growth. Lipids can be removed either by filtration or
by ether or petroleum ether extraction before hy-
drolysis. Proteins are precipitated at pH 4.5 and
starch split by the acidic or enzymatic hydrolysis
step. As with the other analytical procedures, the
microbiological test should be carried out in dim
light. Furthermore, it is important that the glass
vessels used do not release any traces of alkali and
should thus be cleaned with acid before used, because
the flavins are alkali-sensitive. Hence, it is advisable
to dissolve riboflavin standards in 0.02 M acetic acid.
An optimal extraction procedure applicable for
microbiological or HPLC determination of thiamin
and riboflavin has been worked out by the European
Measurement and Testing Program. The steps of the
extraction are detailed in autoclaving food samples in
0.1 N HCI at 121
C for 30 min and adjusting there-
after to pH 4.0 with 4 M sodium acetate buffer (pH
6.1), followed by the addition of takadiastase (0.1 g
per gram of sample), incubation at 37–45
C (18 h),
and then filtration or centrifugation after cooling.
HPLC Procedures
0013HPLC methods enable separate quantitation of indi-
vidual flavins or simultaneous analysis of riboflavin,
including FMN and FAD. A broad variety of HPLC
techniques are described, with variations in the
column material, mobile phase, separation mode,
and detection system as well. Of the numerous ana-
lytical and technical variations communicated during
the last 20 years, the separation techniques can be
categorized as follows.
0014In most cases, reversed-phase (RP) C
18
-materials
as stationary phases, and aqueous/organic mobile
phases on the basis of water, methanol, acetonitril
with or without phosphate or acetate buffer have
been used in an isocratic mode. Ion-pair chromatog-
raphy with sodium salts of hexane or heptane sulfonic
acid in the mobile phase (ion-interaction chromatog-
raphy) was rarely used. In some cases, the separation
of riboflavin and flavins was accomplished using the
gradient elution technique. Ion-pair HPLC seems
more favorable only when riboflavin is to be deter-
mined simultaneously with other B-vitamins (e.g., B
1
,
B
6
, niacin, folic acid, B
12
), because this technique
results in better peak shapes.
0015The retention times of vitamin B
2
active com-
pounds are between 5 (FAD) and 20 (riboflavin)
min. Fluorescence monitoring is preferred for detec-
tion, and UV or visible absorbance detection at 270 or
446 nm is restricted to early HPLC analyses or meas-
urements of pharmaceuticals and enriched foods.
The limits of fluorescence detection at 450/520 nm
(ex./em.) for the native flavins were found to
be 0.55 pmol (0.21 ng) of riboflavin, 1.96 pmol
(0.89 ng) of FMN, and 14.19 pmol (11.15 ng) of
FAD. In an earlier HPLC method, the detection limit
could be increased to 0.02 ng of riboflavin/injection
by irradiation of the sample extract and conversion of
the extracted riboflavin to lumiflavin prior to HPLC
separation.
0016In principle, the extraction techniques and sample
clean-up suitable for HPLC analysis resemble those
4986 RIBOFLAVIN/Properties and Determination
tbl0003 Table 3 HPLC analysis of flavins
a
Food sample/matrix
(compounds deter-
mined)
Extraction procedure Column Mobile phase Detection
(nm)
Detectionlimit
Dairy products (total
riboflavin)
Disperse in water, clean
up on C
18
cartridge
Biosil ODS-5S C
18
H
2
O/CH
3
OH/acetic
acid ¼65/35/1
UV 270 10 ng
Fruits, vegetables
(total riboflavin)
0.1 N HCI (30 min) at
100
C, incubation with
mylase (38
C)
Altex Ultrasphere
ODS 5 mm
H
2
O/CH
3
OH ¼60/
40 þ5mM
heptanesulfonic
acid, pH 4.5
Fluorescence
450/530
(ex./em.)
0.2 ng per
injection
Potatoes,
vegetables (total
riboflavin)
0.1 N HCI (30 min) at
121
C, incubation with
takadiastase (45–50
C)
m-Bondapack C
18
CH
3
OH/H
2
O ¼30/70 Fluorescence
450/510
(ex./em.)
0.1 ng per
injection
Dairy products
(FAD, FMN,
riboflavin)
sorboflavin as
internal standard
Homogenize with 6% ,
containing 2 M urea
pass through C
18
solid
phase, elute with 10% /
CH
3
OH ¼4/1
LC-18, 3 mm
(Supelco)
14% acetonitril in
01. M KH
2
PO
4
,pH
2.9
Fluorescence
450/530
(ex./em.)
FMN 2.5 nM
FAD 3 nM
Riboflavin
2.5 nM
Dairy products, raw
and cooked
meats, cereals
(FAD, FMN,
riboflavin)
7-ethyl-8-methyl-
riboflavin as
internal standard
Homogenize with CH
3
OH/
CH
2
Cl
2
¼9/10 mix with
citrate-phosphate
buffer, pH 5.5
(containing 0.1%
sodium azide),
centrifugation
2PLRP-S, 5 mm
column
temperature 40
C
Acetonitril/0.1%
sodium azide in
0.01 M citrate-
phosphate buffer,
pH 5.5, gradient
elution
Fluorescence
450/522
(ex./em.)
96–113%
recovery
Cereals, various
foods (thiamin
and total
riboflavin)
0.1 N HCI, autoclave
(15 min) at 125
C,
adjust to pH 4.0–4.5
(2 N NaOAc),
incubation with
claradiastase at 50
C
(3 h), 50% TCA and
heating at 90
C
(15 min), adjust to pH
3.5 (2 N NaOAc),
filtration
m Bondapak C
18
CH
3
OH/0.005 M
phosphate buffer
pH 7.0 ¼35/65
Fluorescence
440/520
(ex./em.)
80–96%
recovery
Dairy þ meat
products, fruits,
vegetables, flour,
baked products,
beer, coffee (total
riboflavin)
0.05 M (0.1 N) H
2
SO
4
,
autoclave (20 min) at
121
C, adjust to pH 4.5
(2.5 M acetate buffer),
incubation with
claradiastase at 45
C
(overnight); filtrated
sample passed
through C
18
Sep-Pak,
elution with 40–70%
CH
3
OH
Spherisorb ODS
2.5 mm
H
2
O/CH
3
OH ¼65/35 Fluorescence
445/525
(ex./em.)
20 pg
Blood (FAD, FMN,
riboflavin)
10% TCA at 4
C (30 min),
adding NaOAc-buffer,
centrifugation
Hypersil ODS 5 mm 0.3 M KH
2
PO
4
/
CH
3
OH ¼83.3/
16.7 (pH 2.9)
Fluorescence
470/525
(ex./em.)
FMN 15 nM
FAD 20 nM
Riboflavin
10 nM
Serum, urine
(riboflavin)
isoriboflavin as
internal standard
Homogenize/mix with
TCA (100 gl
1
)
centrifugation, pass
through Sep-Pak C
18
(serum)
ROSIL C
18
HL 5 mm CH
3
OH/H
2
O/
CH
3
COOH ¼36.7/
63.7/0.1
Fluorescence
450/530
(ex./em.)
10 mgl
1
a
Modified according to Ball GFM (1998) Bioavailability and Analysis of Vitamins in Foods, pp. 294–305. New York: Chapman & Hall; Eitenmiller RR and
Landen WO, Jr. (1999) Vitamin Analysis for the Health and Food Sciences, pp. 229–337. Boca Raton, FL: CRC Press; De Leenheer AP, Lambert WE and
Nelis HJ (eds), (2000), Modern Chromatographic Analysis of Vitamins, 3rd edn. New York: Marcel Dekker.
RIBOFLAVIN/Properties and Determination 4987
used for quantification by the other methods dis-
cussed. Most often, vitamin B
2
active substances are
released from the food matrix by autoclaving with
0.1 N mineral acid (HCI or H
2
SO
4
) followed by
enzymatic digestion with papain, takadiastase, or
claradiastase. Solid-phase clean-up prodecures on
C
18
-materials or Florisil are often used for support
prior to injection. The extraction procedure depends
on the type of analysis, whether the total riboflavin
content, i.e. the sum of FAD, FMN, and free ribofla-
vin is to be determined, or whether the separated
quantitation of FAD and FMN in addition to free
riboflavin is required. Treatment with potassium
permanganate can be omitted, because possibly
remaining extraneous fluorescent substances are
chromatographically separated.
0017 Combined acid and enzymatic hydrolysis is advan-
tageous, particularly for foods with a high starch or
protein content, to liberate the bound flavins. Occa-
sionally, autoclaving with dilute mineral acid is in-
complete, particularly for the conversion of FMN to
riboflavin, as indicated by the appearance of an FMN
peak in the following chromatogram. In addition,
FMN may be partially converted during acid hy-
drolysis to biologically active isomeric riboflavin
phosphates, which can be separated from FMN by
HPLC analysis, and are ignored when calculating
total riboflavin. The combination of acidic and en-
zymatic digestion is thus advisable prior to HPLC
analysis for the determination of total riboflavin.
When using this extraction procedure and following
HPLC analysis, the riboflavin content of various
foods such as breakfast cereals, porridges, milk, and
milk products correlates well with the microbio-
logical assay if Lactobacillus casei is used. The simul-
taneous determination of FAD and FMN besides free
riboflavin requires non-degradative techniques, such
as extraction of flavins by methanol/dichloromethane
followed by partitioning with citrate buffer (pH 5.5)
or extraction with 6% formic acid containing 2 M
urea. The HPLC separation and quantitation of the
flavins were carried out using internal standards
(7-ethyl-8-methyl-riboflavin, sorboflavins, isoribo-
flavin, nicotinamide, and others). This analytical
device can be used in the flavin analysis (FAD,
FMN, and riboflavin) of milk and dairy products,
fruits and vegetables, meats, and cereal products. In
many cases, HPLC methods have been developed
for the simultaneous or sequential determination of
riboflavin and thiamin in foods. Both vitamins are
tbl0004 Table 4 Riboflavin content of foods
a
Content
(mgper100 g)
in ingested food
Milk andmilk products Meat and meat prod-
ucts
Cereals Vegetables and
legumes
Fruitsand nuts Fish
> 3.00 Pig’s liver
2.50–3.00 Beef liver, calf liver
2.00–2.50 Beef kidney, calf
kidney
1.50–2.00 Pig’s kidney
1.00–1.50 Pig’s heart
0.70–1.00 Wheatgerms
0.50–0.70 Camembert type,
cheddar type,
Danish blue type,
Parmesan
Wheat bran
0.30–0.50 Cream Brie (50%),
Edam type, fresh
cheese (skim milk),
Eggs, lamb Eel, mackerel
0.20–0.30 Fresh cheese (50%),
Gouda cheese
(45%), yogurt
(low-fat)
Goose, pork (lean)
veal
Green cabbage,
soybean meal
Cashew nuts,
hazel nuts,
sallow thorn
Flounder,
herring,
pilchard,
plaice
0.15–0.20 Cottage cheese,
cows’ milk (fresh)
Beef (lean), chicken,
duck, turkey
Oat flakes,
wholemeal
Broccoli
(boiled),
mangold,
soybean
sprouts,
spinach
(boiled)
Avocado Haddock,
salmon
0.10–0.15 Asparagus
(boiled)
Peanuts
(roasted)
a
According to Souci SW, Fachmann W and Kraut H (2000) Food Composition and Nutrition Tables. Stuttgart: Medpham Scientific.
4988 RIBOFLAVIN/Properties and Determination
extracted by a common procedure using acidic and
enzymatic digestion.
0018 For biological samples, such as blood or plasma/
serum, the preferred extraction medium is 5–10%
trichloroacetic acid, which is suitable for denaturat-
ing the relatively weak protein binding, while keeping
the phosphorylated forms intact. In this way, flavins
in whole blood can be analyzed by isocratic RP-
HPLC against an external standard. A list of usual
HPLC procedures is given in Table 3, and an over-
view of the methods of riboflavin determination is
given in Table 2.
Food Content
0019 Vitamin B
2
is widely distributed in animal and vege-
table foods. Protein-rich foods of animal origin are, as
a rule, considerable sources of this vitamin with good
bioavailability. Particularly rich in riboflavin are
offal, such as heart, liver, and kidney. Because of the
relative heat stability, only minor vitamin losses occur
during preparation. Likewise, pasteurization of milk
causes losses of less than 10%. However, exposure to
day light may result in a remarkable decrease in the
riboflavin content in foods, depending on the surface
area exposed. Vitamin losses occur during the milling
of cereals. White flour with a low extraction rate
contains about one-third of the vitamin content of
whole grain flour. Of special importance for the diet-
ary habits in Western countries are milk and dairy
products despite only a medium riboflavin content. If
these are omitted from the diet, it may be difficult to
achieve an adequate vitamin intake (Table 4).
See also: Analysis of Food; Chromatography: High-
performance Liquid Chromatography; Enzymes:
Functions and Characteristics; Milk: Dietary Importance;
Spectroscopy: Fluorescence
Further Reading
Ball GFM (1998) Bioavailability and Analysis of Vitamins
in Foods. New York: Chapman & Hall. pp. 294–305.
De Leenheer AP, Lambert WE and van Bocxlaer JF (eds)
(2000) Modern Chromatographic Analysis of Vitamins,
3rd edn. New York: Marcel Dekker.
Eitenmiller RR and Landen WO Jr. (1999) Vitamin Analysis
for the Health and Food Sciences, pp. 229–337. Boca
Raton, FL: CRC Press.
Friedrich W (1988) Vitamin B
2
: Riboflavin and its bioactive
variants. In: Vitamins. New York: Walter de Gruyter.
Official Methods of Analysis of AOAC International
(1999) 16th edn., vol. II. Gaitherburg, MD: AOAC
International.
Souci SW, Fachmann W and Kraut H (2000) Food Com-
position and Nutrition Tables. Stuttgart: Medpharm
Scientific.
Strohecker R and Henning HM (1965) Vitamin Assay
Tested Methods. Darmstadt: Verlag Chemie.
The Merck Index (1989) 11th edn. Rahway NJ: Merck &
Co.
Physiology
D B McCormick, Emory University School of
Medicine, Atlanta, GA, USA
Copyright 2003, Elsevier Science Ltd. All Rights Reserved.
Introduction
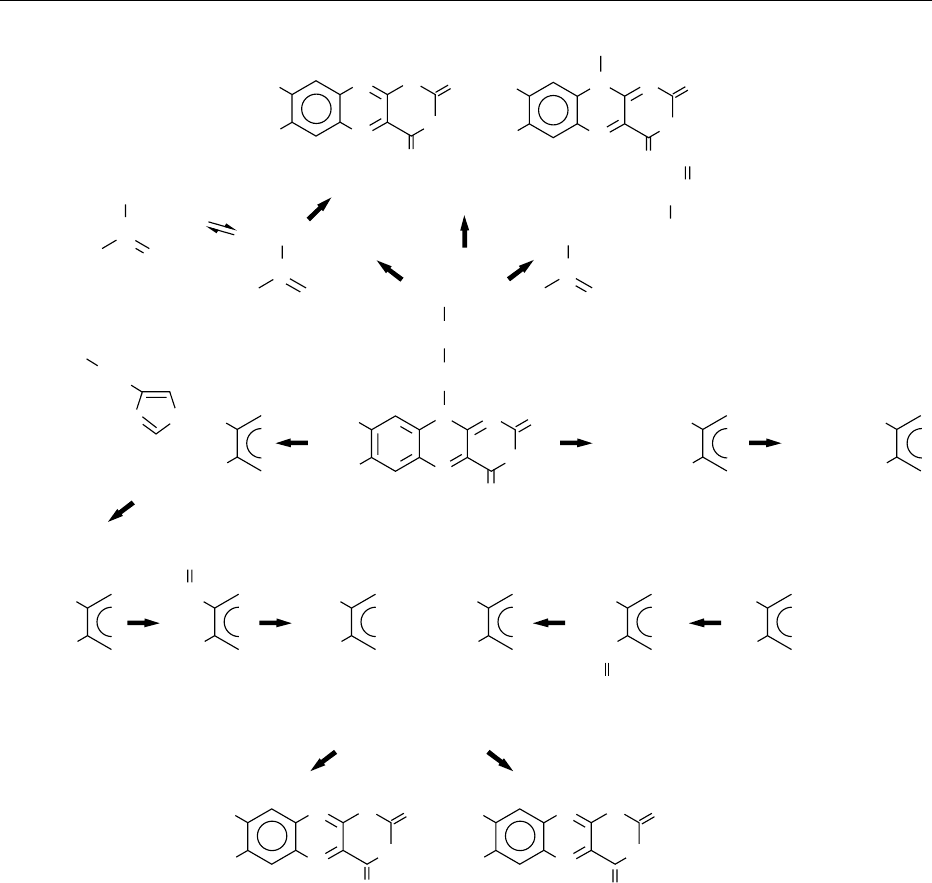
0001Following the earlier identification of riboflavin and
the two most common flavocoenzymes, the more
recent recognition of the greater diversity of natural
flavins has led to a broader appreciation of the mul-
tiple functions and metabolic processing of these im-
portant compounds. Much of the progress in this area
and detail of function of the flavins and flavoproteins
have been given in the periodic symposia held on this
subject. This article reviews the principal features
of the physiological handling of riboflavin and its
natural derivatives in the mammalian body and,
where known, in the human.
Digestion and Bioavailability
0002Riboflavin and lesser amounts of natural derivatives
are released by digestion of complexes, mostly flavo-
proteins, contained within foods. Coenzyme forms
of the vitamin, mainly flavin adenine dinucleotide
(FAD) and flavin mononucleotide (FMN), are re-
leased from noncovalent attachment to proteins as a
consequence of gastric acidification. Nonspecific
hydrolyses of the coenzyme forms by pyrophospha-
tase and phosphatase occur in the upper small intes-
tine. By such actions, FAD is converted to FMN,
which is further converted to riboflavin. Several per
cent of 8a-(amino acid)riboflavins originally in cova-
lent attachment as 8a-FAD linked to certain enzymes,
notably of mitochondrial origin, are also released by
such hydrolases that function together with proteoly-
sis of the attached protein chains, which begins in the
stomach with pepsin and continues in the small intes-
tine with trypsin, chymotrypsin and exopeptidases.
Traces of other ring and side-chain substituted flavins
are similarly released by combinations of the above
actions on non-covalently and covalently bound
flavins. Riboflavin 5
0
-glycosides, for example, are
cleaved by glycosidases present in the succus enteri-
cus. The digestive processes and locale for release of
RIBOFLAVIN/Physiology 4989
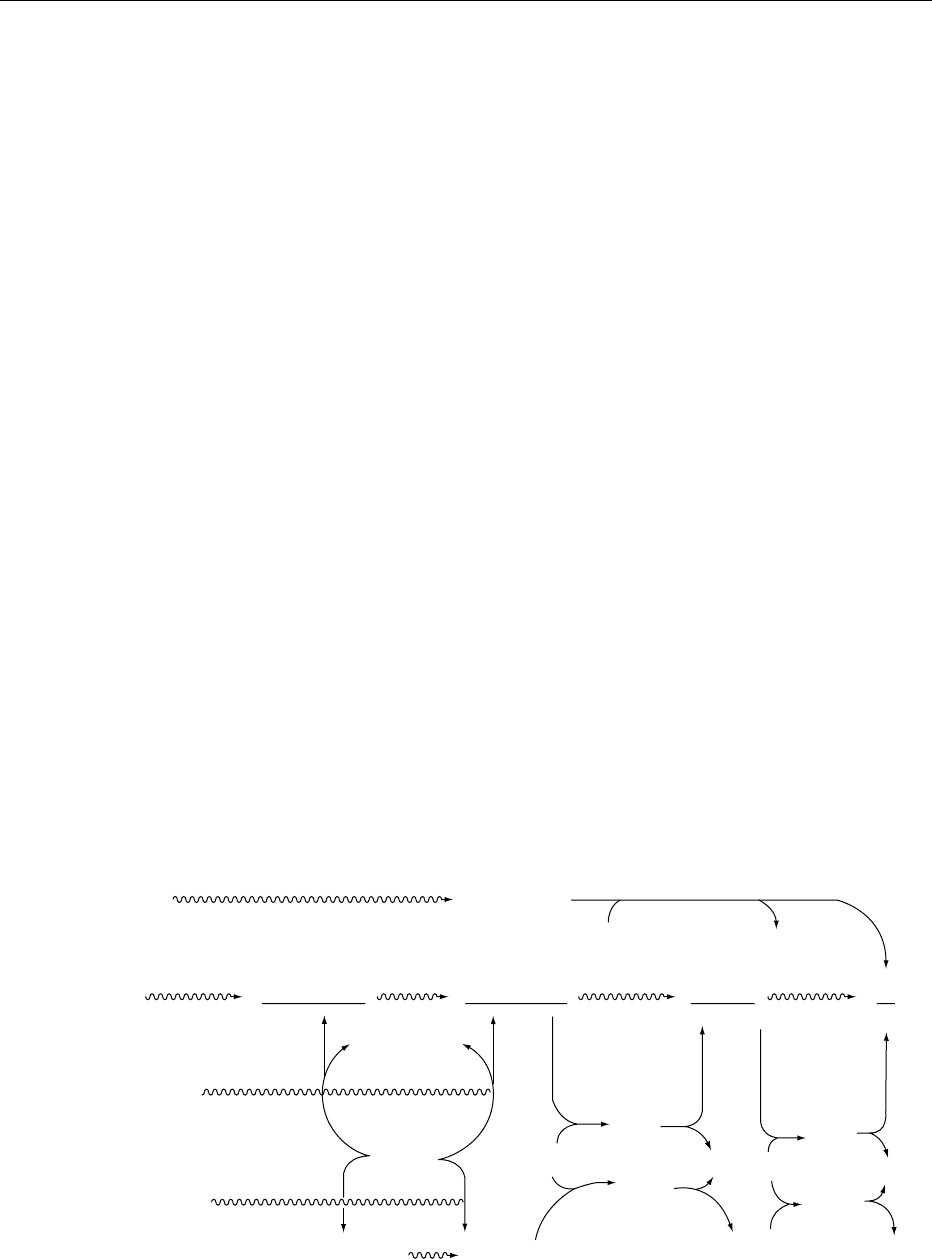
flavins from ingested material is shown in Figure 1.
(See Coenzymes.)
0003 While the efficiency of release of riboflavin from
noncovalently bound forms is essentially complete in
the normal gastrointestinal tract, the vitamin is not
recovered intact from flavin covalently linked to pro-
tein. Since the latter is less than 10% of total flavin
within the diverse foods ingested by people and most
mammals, the average bioavailability of riboflavin is
fairly high. (See Bioavailability of Nutrients.)
Absorption and Transport
0004 Riboflavin and a fraction of flavin metabolites,in-
cluding ring-altered forms, e.g., 8a-(amino acid)ribo-
flavins, and side-chain derivatives, e.g., 7,8-dimethyl-
10-formyl-methylisoalloxazine, are absorbed primar-
ily in the proximal small intestine by a saturable
transport system that is rapid and approximately pro-
portional to dose before levelling off. This saturation
level is achieved with about 25 mg of the vitamin
given in a single bolus to adult humans. Bile salts
appear to facilitate the uptake, and a modest amount
of flavin circulates via the enterohepatic system.
The initial uptake of riboflavin by enterocytes
is Na
þ
-dependent and reflects an adenosine 5
0
-
triphosphatase (ATPase)-involved active cotransport
system. Metabolic trapping by conversion to FMN
and FAD occurs before release of the vitamin to cir-
culation by nonspecific pyrophosphatase and phos-
phatase. (See Bile.)
0005Circulatory transport of flavin involves loose asso-
ciation with albumin and tight associations with
some globulins. A subfraction of immunoglobulin G
(IgG) has been found to bind avidly a small portion of
the total free flavin in blood, and several immuno-
globulins contribute significantly to plasma transport
of the vitamin. Some riboflavin-binding proteins in
plasma are pregnancy-specific, including the classic
case of the estrogen-induced egg-white protein. These
proteins have at least some portion of the binding
domain in common and are essential for fetal devel-
opment. Placental transfer of riboflavin in the human
and other mammals involves binding proteins that
help vector the vitamin and enhance supply to the
fetus.
0006Uptake processes for flavins by mammalian cells
have some characteristics in common, but there are
both qualitative and quantitative differences among
different cell types. Entry of riboflavin appears to be
carrier-mediated (facilitated) at physiological concen-
trations of the vitamin, since there is relative specifi-
city to a saturable component that is responsible for
initial rapid uptake. A riboflavin-binding protein has
even been isolated from the plasma membrane of rat
liver cells. The nonepithelial hepatocyte does not
depend on Na
þ
for riboflavin import, as do bipolar
epithelial types such as the enterocyte or renal prox-
imal tubular cell. Slower passive diffusion becomes
more evident when the facilitating transporter is
exceeded by pharmacological levels of the vitamin.
In all cases, metabolic trapping of riboflavin by
Stomach:
glycosides
H
2
O
glycose
glycosidases
Flavinyl glycosides
(glucose, etc.)
Free flavins
(Rb, FMN, FAD)
Flavoprotein complexes
(FAD > FMN > Rb)
(poly) peptides
(poly) peptides
trypsin,
chymotrypsin,
peptidases
nucleotide
pyrophosphatase
AMP
alkaline
phosphatase
P
i
H+,
pepsin
H
2
OH
2
O
H
2
O
Flavoprotein compounds
(Proteinyl 8α-FAD)
peptidyl 8α-FAD 8α-FAD
8α-FMN 8α-Rb
Rb, FMN, FAD Rb, FMN, FAD Rb, FMN Rb
Small intestine:
fig0001 Figure 1 Digestion of flavins in monogastric mammals. Rb, riboflavin; P
i
, inorganic phosphate. Reproduced with modifications from
Riboflavin: Physiology, Encyclopaedia of Food Science, Food Technology and Nutrition, Macrae R, Robinson RK and Sadler MJ (eds),
1993, Academic Press.
4990 RIBOFLAVIN/Physiology
phosphorylation dependent upon cytosolic flavoki-
nase follows passage of the vitamin through the
plasma membrane. Release of riboflavin from cells
requires hydrolysis of FMN by nonspecific phosphat-
ases.
Cellular Interconversions
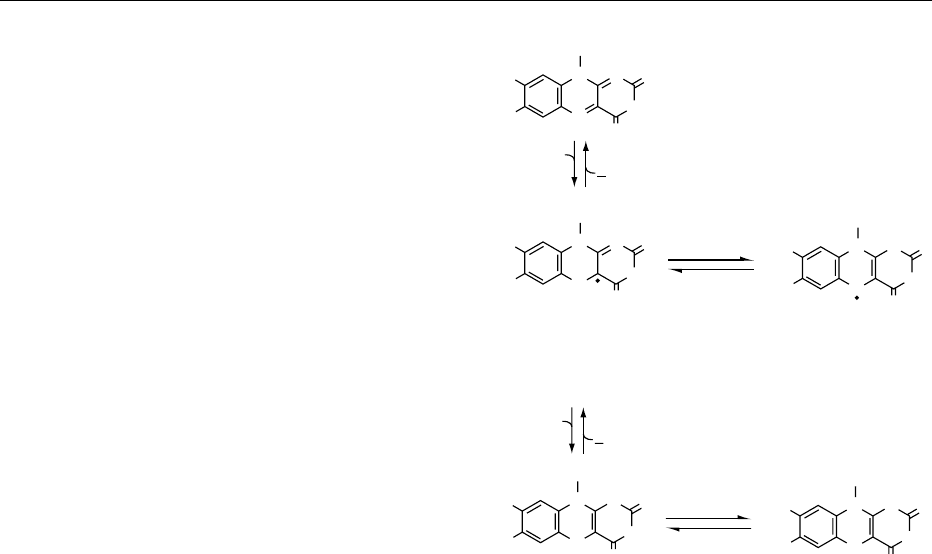
0007 The metabolic interconversions of riboflavin and
flavocoenzymes are summarized in Figure 2.
0008 Conversion of riboflavin to coenzymes occurs
within the cellular cytoplasm of most tissues, but
particularly in the small intestine, liver, heart, kidney,
and brain. The obligatory first step is the adenosine
5
0
-triphosphate (ATP)-dependent phosphorylation of
the vitamin catalyzed by flavokinase, which utilizes
Zn
2þ
. The FMN product can be complexed with
specific apoenzymes to form several functional flavo-
proteins, but the major portion is further converted to
FAD in a second ATP-dependent reaction catalyzed
by FAD synthetase, which utilizes Mg
2þ
. It is clear
that the biosynthesis of flavocoenzymes is regulated
by supply of riboflavin (flavin status), competition for
ATP (energy status), and hormonal balances. Thyrox-
ine and triiodothyronine stimulate FMN and FAD
synthesis in mammalian systems. This seems to in-
volve a hormone-mediated increase in an active form
of flavokinase. As a product of the synthetase, FAD is
also an effective inhibitor at this second step and may
help regulate its own formation. FAD is the predom-
inant flavocoenzyme present in tissues where it is
mainly complexed with numerous flavoprotein
dehydrogenases and oxidases. Several percent of the
FAD also becomes covalently attached to specific
amino acid residues of a few important apoenzymes.
Examples for the human include the 8a-N
3
-histidyl
FAD within the mitochondrial dehydrogenases for
succinate, dimethylglycine and sarcosine, and the
8a-S-cysteinyl FAD within monoamine oxidase,
also of mitochondrial localization. (See Hormones:
Thyroid Hormones.)
0009Turnover of covalently attached flavocoenzymes
requires intracellular proteolysis, and further degrad-
ation of the coenzymes involves nonspecific pyro-
phosphatase and specific 5
0
-nucleotidase cleavage
of FAD to AMP (adenosine monophosphate) and
FMN and action by nonspecific phosphatases on the
latter.
Storage and Catabolism
0010There is little storage of riboflavin as such, since most
exists within flavocoenzymes that are in relatively
tight associations in holoenzymatic systems. During
such severe deficiency of the vitamin as leads to death
of experimental animals, there is a reduction in the
level of extractable flavin that can approach about
half of that found in an optimally supplemented con-
trol. Hence, there is moderately effective retention of
riboflavin by its metabolic commitment to bound
forms; however, even a modest deficit of the vitamin
is reflected in the decrease in function of certain
flavoproteins well before full-blown symptoms of
deficiency.
0011Though certain bacteria, especially of the Pseudo-
monas genus, can extensively degrade both the ring
system and side-chains of flavins, mammals are more
limited in their abilities to catabolize the vitamin. The
considerable diversity of flavin metabolites in and
from mammals reflects the composite of reactions of
photochemical processes on the skin, microfloral ac-
tivities in the gastrointestinal tract, as well as somatic
actions both directly on flavin and on derivatives
presented to cells by circulatory recovery from dermal
tissue and by enterohepatic retrieval from the gut.
The diverse flavin-related products identified from
humans and other mammals are summarized in
Figure 3.
0012Cleavage of the d-ribityl side-chain at position 10
is mainly, if not entirely, attributable to light and
intestinal microflora. Both can lead to partial frag-
mentation to form the 10-formylmethylflavin. This
can be oxidized by alimentary bacteria of the rumin-
ant and human to form the 10-carboxymethylflavin,
and a further fraction of the formylmethyl compound
is interconverted with the 10-hydroxymethylflavin as
a result of pyridine-nucleotide-dependent dehydro-
genase in tissue. Lumichrome-level compounds not
only can result from complete removal of the side-
chain by microflora, which can be decreased by anti-
biotic administration, but can accompany lumiflavin
as a photoproduct from action of light on flavin
within the dermal tissue. Catabolites of riboflavin
that primarily derive from oxidations within tissues
ATP
P
i
H
2
O
RIBOFLAVIN
FMN
F'MN
AMP
H
2
O
FAD
F'AD
ATP
PP
i
ADP
flavokinase
(Zn
2+
)
(Mg
2+
)
phosphatase
Pyrophosphatase
synthetase
fig0002 Figure 2 Metabolic interconversions of riboflavin and
flavocoenzymes. Reproduced from Riboflavin: Physiology, En-
cyclopaedia of Food Science, Food Technology and Nutrition,
Macrae R, Robinson RK and Sadler MJ (eds), 1993, Academic
Press.
RIBOFLAVIN/Physiology 4991
are the 7- and 8-hydroxymethylriboflavins (7a-and
8a-hydroxyriboflavins). These, and products from
further oxidation of the hydroxymethyl functions to
formyl and carboxyl groups, reflect microsomal
mixed-function oxidase activity. Other flavin catabo-
lites include those from 8a -(amino acid)riboflavins
released from covalently bonded FAD. An 8a-
sulfonylriboflavin may derive from the 8a-cysteinyl-
FAD of monoamine oxidase. A peptide ester and
a glucoside, both linked to the 5
0
-hydroxymethyl
terminus of the vitamin, have also been found.
Excretion and Secretion
0013Since no isoalloxazine (flavin) can be biosynthesized
within the cells of mammals that lack riboflavin
synthetase, excretion and secretion reflect dietary
intake and catabolic and photodegradative events.
Essentially all known catabolites of riboflavin have
been detected in urine; many of the lumichrome-level
compounds are also in feces. For normal adults
eating varied diets, riboflavin comprises 60–90%
of urinary flavin, 7-hydroxymethylriboflavin 3–7%,
H
3
C
H
3
C
H
3
C
H
3
C
NN
O
H
O
N
NH
N
O
O
O-C-CH
2
-R
CH
2
-CH
2
OH
Lumichrome + Lumiflavin
CH
2
- CHO
5⬘
CH
2
OH
1⬘
CH
2
CH
2
-S-CH
2
R-SO
2
-CH
2
H
3
CH
3
C
αα
N
10
CH
2
-(CHOH)
3
-CH
2
N
10
N
10-Hydroxyethyl-
flavin
10-Formylmethyl-
flavin
8α-N
3
-Histidyl-
FAD
8α-S-Cysteinyl
FAD
8α-Sulfonyl-
riboflavin
(HOCH)
3
5⬘-Riboflavinyl-peptide/ester
10
O
NH
10
N
CH
3
N
10
CH
2
N N - CH
2
H
3
CH
3
C
H
3
CN
N
Riboflavin
Catabolites
O
HC
H
3
C
NH
N
O
O
10
1
4
2
3
5
8
7
8
7
8
7
8
7
8
7
8
7
8
7
8
7
8
7
8
7
9
6
8
7
8
7
HOCH
2
H
3
C
HO
2
C
HO
2
C HOCH
2
H
3
C
H
3
CH
3
CH
3
C
HC
O
8-Hydroxymethyl-
riboflavin
8-Formyl 8-Carboxy 7-Carboxy 7-Formyl 7-Hydroxymethyl-
riboflavin
HO
2
C
HO
2
C
NN
H
O
N
N
N
N
O
O
NH
H
NH
O
H
3
C
H
3
C
8-Carboxylumichrome 7-Carboxylumichrome
fig0003 Figure 3 Photochemical, microfloral, and cellular catabolism of riboflavin within mammals. Reproduced from Riboflavin: Physi-
ology, Encyclopaedia of Food Science, Food Technology and Nutrition, Macrae R, Robinson RK and Sadler MJ (eds), 1993, Academic
Press.
4992 RIBOFLAVIN/Physiology
8a-sulfonylriboflavin 2–15%, 8-hydroxymethylribo-
flavin 1–8%, 10-hydroxyethylflavin 1–7%, riboflavi-
nyl peptide ester up to 5%, with traces of lumiflavin
and, sometimes, the 10-formylmethyl- and carboxy-
methylflavins.
0014 The presence in milk of ‘lactoflavin,’ an early name
for riboflavin, led to the recognition of this food as a
good source of the vitamin. For milk from both cows
and humans, the flavin in highest concentration other
than the free vitamin is FAD, which can comprise
over a third of total flavin. Much of this is hydrolyzed
to FMN by pasteurization. Fairly significant quan-
tities of the 10-(2
0
-hydroxyethyl)flavin are notable,
since this catabolite has antivitamin activities, as
reflected in competitive inhibition of both cellular
uptake and subsequent flavokinase-catalyzed phos-
phorylation of riboflavin. Hence, this catabolite,
which may reach 10–12% of flavin in cow’s milk,
modestly subtracts from the biological activity of
this food. Several percent of both 7- and 8-hydroxy-
methylriboflavins are also present, with more of the
former. Smaller amounts of other catabolites, includ-
ing the 10-formylmethylflavin and lumichrome,
comprise most of the rest. (See Milk: Dietary
Importance.)
Biochemical Functions
0015 In bound coenzymic forms, riboflavin participates in
oxidation–reduction reactions in numerous meta-
bolic pathways and in energy production via the re-
spiratory chain. A variety of chemical reactions are
catalyzed by flavoproteins. The redox functions of a
flavocoenzyme (Figure 4) include one-electron trans-
fers, during which the neutral, oxidized quinone level
of flavin is half reduced to the radical semiquinone,
which can exist within natural pH ranges as neutral
or anionic species. A further electron transfer can lead
to a fully reduced hydroquinone. In addition, a single-
step, two-electron transfer from substrate to flavin
can occur with hydride ion transfer, e.g., from re-
duced pyridine nucleotide, or by base abstraction of
a substrate proton together with carbanion addition.
0016 There are flavoprotein-catalyzed dehydrogenations
that are both pyridine-nucleotide dependent and
independent, reactions with sulfur-containing com-
pounds, hydroxylations, oxidative decarboxylations,
dioxygenations, and reduction of oxygen to hydrogen
peroxide. The intrinsic abilities of flavins – to be
varyingly potentiated as redox carriers upon differen-
tial binding to proteins, to participate in both one-
and two-electron transfers, and to react in reduced
(1,5-dihydro) form with oxygen – permit wide scope
in their operation.
Requirements and Intakes
0017The requirement levels for riboflavin, in contrast to
those for thiamin, are not raised when energy utiliza-
tion is increased. Because of the interdependence of
protein, energy intake, and metabolic body size, how-
ever, allowances calculated on these three bases do
not differ significantly. Clinical signs of deficiency in
adults can be prevented with intakes of riboflavin
above 0.4 mg per 1000 kcal, but over 0.5 mg per
1000 kcal may be required to maintain tissue reserves
in adults and children as reflected in urinary excre-
tion, erythrocyte riboflavin, and erythrocyte glu-
tathione reductase. From these considerations, the
riboflavin allowances are now computed as 0.6 mg
per 1000 kcal for people of all ages. This leads to US
Recommended Dietary Allowances (RDAs) ranging
from 0.4 mg per day for early infants to 1.7 mg per
day for young adult males. However, for elderly
people and others whose daily calorie intake may be
less than 2000 kcal, a minimum of 1.2 mg per day is
recommended in the USA. Since pregnancy imposes
extra demands, reflected by decreased excretion
R
e
−
N
N
NO
Flavoquinone: yellow, fluorescent,
neutral, oxidized level
Flavosemiquinone:
blue, neutral radical
Flavohydroquinone:
neutral reduced level
Flavohydroquinone:
anionic reduced level
Flavosemiquinone:
red, anionic radical
NH
O
O
2
H
3
C
H
3
C
R
N
N
H
NO
NH
O
H
3
C
H
3
C
1
4
R
N
N
N
−
O
NH
O
H
3
C
H
3
C
e
−
O
2
R
N
N
H
N
H
H
N
O
NH
O
H
3
C
H
3
C
1
4
R
NN
−
O
NH
O
H
3
C
H
3
C
pK
a
~ 8.4
pK
a
~ 6.2
fig0004Figure 4 Oxidation–reduction states of flavocoenzymes func-
tioning physiologically. Reproduced from Riboflavin: Physiology,
Encyclopaedia of Food Science, Food Technology and Nutrition,
Macrae R, Robinson RK and Sadler MJ (eds), 1993, Academic
Press.
RIBOFLAVIN/Physiology 4993

and an elevated FAD stimulation of erythrocyte
glutathione activity, an additional 0.3 mg per day is
recommended. The lactating woman secretes ap-
proximately 35 mg per 100 ml of milk for an output
of about 0.26 mg per day (750 ml) during the first 6
months and 0.21 mg per day (600 ml) during the
second 6 months. Since the utilization of the
additional riboflavin for milk production is assumed
to be 70%, an additional intake of 0.5 mg is
recommended for the first 6 months and 0.4 mg for
the second. (See Lactation: Physiology.)
0018 Small amounts of riboflavin, largely as digestible
coenzymes, are present in most plant and animal
tissue. Good sources are eggs, lean meats, milk, broc-
coli, and enriched breads and cereals. Such losses as
occur during cooking are largely attributable to
leaching of the heat-stable but light-sensitive flavins
into water.
0019 When supplementation or therapy with riboflavin
is warranted, oral administration of five to 10 times
the RDA is usually satisfactory.
Deficiency Causes and Symptoms
0020 Pure, uncomplicated riboflavin deficiency is probably
never encountered in patients, but is accompanied by
multiple nutrient deficiencies. Ariboflavinosis can
result from such primary and secondary factors as
commonly affect supply or utilization of other nutri-
ents as well. Inadequate dietary intake most com-
monly related to limited availability of food, but
sometimes exacerbated by poor storage or process-
ing, remains the major cause. In addition, anorexic
persons rarely ingest adequate amounts of riboflavin
and other nutrients.
0021 Decreased assimilation results from abnormal di-
gestion, absorption, or both. Lactose intolerance as a
result of lactase insufficiency, mostly encountered
among Blacks and Asians, argues against such people
consuming nonlactase-treated milk, which is a good
source of the vitamin. Malabsorption can occur as a
result of tropical spure, celiac disease, malignancy
and resection of the small bowel, and gastrointestinal
and biliary obstruction. Poor absorption also results
from disorders that increase motility and decrease
gastrointestinal passage time, such as diarrhea, infec-
tious enteritis, and irritable bowel syndrome. (See
Food Intolerance: Lactose Intolerance.)
0022 Rather rarely encountered, but usually significantly
improved by therapeutic treatment with riboflavin,
are certain inborn errors where the genetic defect is
in formation of a normal flavoprotein. Cases in this
category include fatty acid desaturases in which spe-
cific defects have been found for the mitochondrial
FAD-dependent dehydrogenases for short-chain,
long-chain, and multi-chain acyl-CoAs (acyl coen-
zyme As). The young patients have a lipid storage
myopathy, often accompanied by carnitine insuffi-
ciency, and exhibit glutaric aciduria. A low, FMN-
dependent pyridoxine 5
0
-phosphate oxidase activity
due to an erythrocyte deficiency of FMN, confirmed
by response to oral riboflavin, was reported in the
majority of subjects with d-glucose 6-phosphate
dehydrogenase deficiency. Such cases seem to have
an accelerated conversion of FMN to FAD so that
glutathione reductase is saturated. This contrasts
with heterozygous b-thalassemia, in which there is
an inherited slow erythrocyte conversion of riboflavin
to FMN, a decrease in subsequent FAD, and a high
stimulation of the erythrocyte glutathione reductase
by extraneous FAD.
0023Defective utilization can result from disturbances
in hormonal production, certainly relating to thyroid
hormone, but less likely as a result of taking oral
contraceptives. Phenothiazine derivatives appear to
impair use of riboflavin.
0024Increased destruction of riboflavin occurs during
treatment of neonatal jaundice with phototherapy.
In this case, the side-chain of the vitamin is photo-
chemically destroyed, as it is involved in the photo-
sensitized oxidation of bilirubin to more polar,
excretable compounds.
0025The finding that phenobarbital induces microso-
mal oxidation of the 7-methyl function of the vitamin
lends credence to the belief that long-time use of
barbiturates may jeopardize flavin status.
0026Enhanced excretion of riboflavin occurs in cata-
bolic patients undergoing nitrogen loss. The relation-
ship of the vitamin to protein status has long been
recognized. Also, certain antibiotics and pheno-
thiazine drugs increase excretion of riboflavin. (See
Drug–Nutrient Interactions.)
0027Increased requirements can, of course, be the con-
sequence of one or more of the above-mentioned
factors. For example, protein–calorie malnutrition
commonly accompanies a diminution in both absorp-
tion and utilization of riboflavin. Systemic infections,
even without gastrointestinal involvement, some-
times lead to increased requirements that can result
from decreased intake, defective absorption, poor
utilization, and increased excretion. (See Protein: De-
ficiency.)
0028Clinical deficiency of riboflavin has been reduced
by feeding a riboflavin-deficient diet and/or by the
administration of an antagonist such as galactoflavin.
The deficiency syndrome is characterized by sore
throat, hyperemia and edema of the pharyngeal and
oral mucous membranes, cheilosis, angular stoma-
titis, glossitis (magenta tongue), seborrheic dermatitis,
and normochromic, normocytic anemia associated
4994 RIBOFLAVIN/Physiology

with pure red cell cytoplasia of the bone marrow. As
noted above, some of these symptoms, e.g., glossitis
and dermatitis, when encountered in the field, may
have resulted from other complicating deficiencies.
Severe riboflavin deficiency can also affect the
conversion of vitamin B
6
to its coenzyme and even
curtail conversion of tryptophan to niacin. (See
Niacin: Physiology; Vitamin B
6
: Properties and
Determination.)
Toxicity
0029 Toxicity from ingestion of excess riboflavin by
experimental animals or humans is doubtful. The
capacity of the human gastrointestinal tract to absorb
orally administered riboflavin may be less than 30 mg
in a single dose. The limited solubility and absorptiv-
ity of this vitamin as encountered in multivitamin
preparations and natural foodstuffs, and its ready
excretion as typical of water-soluble vitamins, nor-
mally precludes a health risk. There is one report of
EEG (electroencephalogram) abnormalities in two
patients during long-term treatment with riboflavin
and niacin.
See also: Bile; Bioavailability of Nutrients; Coenzymes;
Drug–Nutrient Interactions; Food Intolerance: Lactose
Intolerance; Hormones: Thyroid Hormones; Lactation:
Human Milk: Composition and Nutritional Value;
Physiology; Milk: Dietary Importance; Niacin: Properties
and Determination; Protein: Deficiency; Vitamins:
Overview; Determination; Vitamin B
6
: Properties and
Determination
Further Reading
Edmondson DE and McCormick DB (eds) (1987) Flavins
and Flavoproteins. Berlin: Walter de Gruyter.
McCormick DB (1999) Riboflavin. In: Shils ME Olson JA,
Shike M and Ross AC (eds) Modern Nutrition in Health
and Disease, pp. 391–399. Baltimore, MD: Williams
and Wilkins.
McCormick DB (1989) Two interconnected B vitamins:
riboflavin and pyridoxine. Physiological Reviews 69:
1170–1198.
McCormick DB (1990) Riboflavin. In: Brown ML (ed.),
Present Knowledge in Nutrition, pp. 146–154. Washing-
ton, DC: International Life Sciences Institute–Nutrition
Foundation.
McCormick DB (1997) Coenzymes, Biochemistry. In: Dul-
becco R (ed.) Encyclopedia of Human Biology, vol. 2,
pp. 847–864. San Diego: Academic Press.
Merrill AH, Jr, Lambeth JD, Edmondson DE and
McCormick DB (1981) Formation and mode of action
of flavoproteins. Annual Review of Nutrition 1: 281–
317.
Mu
¨
ller F (ed.) (1991) Chemistry and Biochemistry of
Flavoenzymes, vols. I–III. Boca Raton, FL: CRC Press.
RICE
B O Juliano, Philippine Rice Research Institute Los
Ban
˜
os, Laguna, Philippines
Copyright 2003, Elsevier Science Ltd. All Rights Reserved.
Global Distribution, Varieties, and
Commercial Importance
0001 Rice is the most important crop in the world in terms
of total developing world production (480 10
6
tonnes of rough rice) and the number of consumers
(2.5 billion) dependent on it as their staple food. It is
widely grown in over 100 countries in every continent
(except Antartica), from 53
Nto40
S, and from sea
level to an altitude of 3 km. The total production in
1998 was 568 10
6
tonnes of rough rice. Asia ac-
counts for 134 of the 149 10
6
ha world area that is
used for rice cultivation. The mean rough rice yield
was 3.74 tonnes ha
1
in 1998. About 90% of the
world’s rice is grown and consumed in Asia. The
major rice producers in 1998 were China, India,
Indonesia, Bangladesh, Vietnam, and Thailand. In
terms of water regime, 54% of the total rice area
was irrigated in 1991, 25% rainfed lowland, 13%
upland, and 9% as flood-prone wetland, correspond-
ing to total rough rice production of 76% from
irrigated, 16% from rainfed lowland, 4% from
upland, and 4% from flood-prone wetland. Since
the rice-growing area is shrinking, rice produc-
tion must keep up with the 1.7% per year increase
in population in tropical Asia through increased
yield.
0002There are estimated to be about 100 000 rice
varieties; only a small proportion is actually widely
cultivated. They vary in grain weight, size and shape,
degree of dormancy, longevity and seedling vigor, and
some have red to purple–black pigments. About 75%
of Asia’s rice area is planted with varieties of im-
proved semidwarf plant type with erect leaves.
The newer, improved varieties have a similar yield
RICE 4995
