Caballero B. (ed.) Encyclopaedia of Food Science, Food Technology and Nutrition. Ten-Volume Set
Подождите немного. Документ загружается.

certain tropical oils such as coconut and palm kernel
oils. Arachidic acid occurs, albeit in small amounts, in
a wide range of tropical vegetable fats. Animal fats, in
addition to palmitic and stearic acids, contain small
amounts of odd-numbered and branched-chain satur-
ated acids. The lower fatty acids from butyric (4:0)
to capric (10:0) are significant in ruminant milk fats.
(See Palm Oil.)
0007 The next four items in Table 1 are monounsatu-
rated fatty acids. Oleic acid is universally important
in food lipids, in some cases being as much as 80% of
the component fatty acids (e.g., olive oil). Palmitoleic
acid is also ubiquitous, though in much smaller
amounts. Erucic and petroselinic acids, though im-
portant in a few seed oils, are of restricted occurrence,
the former in the Cruciferae and the latter in the
Umbelliferae. Except for erucic acid, these and all
the acids referred to later in this section are liquid at
ambient temperatures.
0008 Linoleic acid is of almost universal importance in
vegetable oils, but it does not occur to a significant
extent in animal products. This diunsaturated fatty
acid, the only really important one, is the ‘essential
fatty acid’ on which most nutritional studies have
been based and is the key member of the widely
advertised ‘polyunsaturates.’
0009 The triunsaturated fatty acids, a- and g-linolenic
acids, are found, though very rarely together, in
many seed oils, the former being the commoner. a-
Linolenic acid is the major fatty acid of leaf and root
lipids and many seed oils, especially those of northern
latitudes. g-Linolenic acid, though less widespread, is
found in the oil seeds of many plant species, in some
algae and fungi and certain animal products.
0010 Of the last three fatty acids named in Table 1,
arachidonic acid is of exclusively animal origin
(e.g., eggs and certain meat offals) whilst the last
two occur in substantial proportions in fatty fish
(herring, mackerel) and fish liver oils (cod, halibut).
(See Fish Oils: Dietary Importance; Offal: Types of
Offal.)
0011Apart from those listed, and certain isomers and
homologs of them, many other fatty acids, though
less common, are well known. These may contain con-
jugated unsaturated systems (e.g., punicic acid), trans
double bonds (e.g., columbinic acid), triple bonds
(e.g., crepenynic acid), homocyclic (e.g., sterculic
acid) or heterocyclic (e.g., vernolic acid) rings or sub-
stituent functional groups (e.g., ricinoleic acid). Some
of these are occasionally consumed in food lipids.
Glycerides
0012Food scientists and technologists are much more con-
cerned with glycerides than with fatty acids as such.
Many, but not all, of the properties of fatty acids are
mirrored in those of the nonpolar triglycerides. How-
ever, the mono- and diglycerides, in which, respect-
ively, only one or two of the hydroxyls of glycerol are
esterified, have both lipophilic and hydrophilic prop-
erties. The resulting surface activity enables them to
serve as emulsifiers and foam stabilizers in processed
foods. (See Emulsifiers: Organic Emulsifiers; Uses in
Processed Foods.)
Mono- and Diglycerides
0013Monoglycerides containing a fatty acid (RCO
2
H)
exist in the form of 1-monoglycerides (1) or the iso-
meric 2-monoglycerides (2). Both forms revert, on
storage, to an equilibrium mixture in which the
1-monoglyceride dominates (90%). Monoglycerides,
accompanied by diglycerides, are produced by the
base-catalyzed interesterification (randomization) of
a triglyceride (5) with glycerol. The resulting mixed
product is often used without purification, but if
high-quality monoglycerides are desired, these can
be obtained by molecular distillation of the mixed
product. Monoglycerides have important applica-
tions in the food-processing industry for the sta-
bilization of both water-in-oil (e.g., margarine) and
oil-in-water (e.g., artificial cream) emulsions. (See
Margarine: Methods of Manufacture.)
(1)
RCO
2
HO
HO
(2)
HO
RCO
2
HO
(3)
RCO
2
HO
RCO
2
(4)
RCO
2
RCO
2
HO
(5)
RCO
2
RCO
2
RCO
2
0014Diglycerides also exist in two forms ((3) and (4)),
the 1,3-diglyceride (3) being dominant in the
tbl0001 Table 1 The more important natural food fatty acids
Trivialname Empirical formula Shorthand structure
Lauric acid C
11
H
23
CO
2
H 12:0
Myristic acid C
13
H
27
CO
2
H 14:0
Palmitic acid C
15
H
31
CO
2
H 16:0
Stearic acid C
17
H
35
CO
2
H 18:0
Arachidic acid C
19
H
39
CO
2
H 20:0
Palmitoleic acid C
15
H
29
CO
2
H 16:1 n-7
Oleic acid C
17
H
33
CO
2
H 18:1 n-9
Petroselinic acid C
17
H
33
CO
2
H 18:1 n-12
Erucic acid C
21
H
41
CO
2
H 22:1 n-9
Linoleic acid C
17
H
31
CO
2
H 18:2 n-6
a-Linolenic acid C
17
H
29
CO
2
H 18:3 n-3
g-Linolenic acid C
17
H
29
CO
2
H 18:3 n-6
Arachidonic acid C
19
H
31
CO
2
H 20:4 n-6
Eicosapentaenoic acid
a
C
19
H
29
CO
2
H 20:5 n-3
Docosahexaenoic acid
a
C
21
H
29
CO
2
H 22:6 n-3
a
In these cases, systematic names are given in the absence of trivial
names.
2298 FATTY ACIDS/Properties

equilibrium mixture. They are much less polar than
monoglycerides and have few food applications.
Triglycerides
0015 These are the dominant components (more than
90%) of all edible oils and fats. Since they contain
about four to 10 significant amounts of different fatty
acids, they comprise a very large number of individual
triglycerides. The fatty acids are, however, not ran-
domly distributed but tend to follow certain rules.
0016 In oils and fats of vegetable origin, the preferred
sites for saturated acids are the 1- and 3-positions,
whilst unsaturated acids occupy the 2-position for
preference. In animal fats (e.g., lard), the reverse is
the case, except for the fats of ruminants (e.g., beef
and mutton tallow, milk fat), in which the distribu-
tion is approximately random.
0017 The positions of substituent saturated and unsatur-
ated fatty acids in the triglyceride molecule are im-
portant in determining the hardness, elasticity, and
melting characteristics (Table 2) of fats containing
them. These physical parameters control the texture
and mouth-feel of foods in which they are major
components. Such compositional features are parti-
cularly important in the case of monounsaturated
disaturated triglycerides, which can be represented
as the isomers SUS and SSU.
0018 Relatively hard vegetable fats (SUS-type triglycer-
ides, 30–40
C), such as cocoa butter melt sharply at,
or slightly below, body temperature and hence are ideal
components in chocolate, cream fillings, and confec-
tionery couvertures. Admixture with fats of the
SSU-type causes a fall in melting point and a marked
increase in melting range. Such mixed triglycerides
may therefore be well adapted to the formulation of
margarines and bakery fats. (See Cocoa: Production,
Products, and Use; Fats: Uses in the Food Industry.)
0019 The melting and crystallization characteristics of
both pure and mixed triglycerides are also very de-
pendent on ‘tempering’ (close control of holding time
and temperature), since they exist in distinct poly-
morphic forms, the most stable being that with the
highest melting point.
0020Natural fats can be physically separated into desir-
able fractions by various industrial processes, viz. by
‘dry,’‘wet,’ or ‘solvent’ fractionation, with appropri-
ate careful temperature control. Fats such as edible
tallow, lard, palm oil, palm kernel oil, and coconut oil
can, in the ‘dry’ process, be separated by pressing or
filtration into a higher-melting crystalline fraction
and a liquid oil. In the ‘wet’ processes, the fat is
mixed with an aqueous solution of a surface-active
agent, which disperses the crystalline fraction into the
aqueous phase. The separation is more efficient than
in the dry processes. The most efficient and selective
fractionation process makes use of a volatile solvent,
usually acetone, to segregate, to a large extent, glycer-
ides according to their degree of unsaturation: SSS,
SUS, SUU, and UUU.
Reactions of Triglycerides
0021In the context of food, very few intentional reactions
are permissible, since both the starting material and
the reaction product must be of acceptable edible
quality. Thus, only two kinds of reactions are of
practical importance – hydrogenation and interester-
ification. To these, however, must be added lipolysis
and autoxidation – undesirable spoilage reactions
affecting oils and fats under unfavorable storage con-
ditions, and thus causing rancidity.
0022Hydrogenation The objects of hydrogenation are
(1) by increasing the degree of saturation of an oil
or fat to raise its melting point and thus extend its
applications, and (2) by reducing its degree of unsat-
uration to reduce its proneness to autoxidation and
thereby to enhance its stability. Hydrogenation is
always partial and sometimes only marginal. In
chemical terms, it involves not only the saturation of
double bonds but also cis–trans isomerization and
migration of some double bonds to neighboring
positions in the fatty chains.
0023Hydrogenation involves the use of hydrogen and a
supported metal catalyst, commonly nickel on Kiesel-
guhr, at temperatures between 100 and 200
C. Con-
ditions are varied according to requirements. Thus,
the use of a fresh catalyst and low temperatures min-
imizes isomerization, whereas an old (‘poisoned’)
catalyst at higher temperatures promotes isomeriza-
tion and minimizes saturation. Trans fatty acids can
be formed in high proportions in hydrogenated fats,
with consequent rises in melting points (note the con-
trast in melting points between corresponding cis and
trans 18:1 n-9 compounds in Table 2).
0024Interesterification The same base-catalyzed reac-
tion, as described earlier for the production of mono-
glycerides, is applicable to the randomization of
tbl0002 Table 2 Melting points (
C) of fatty acids and derived
glycerides
Fattyacid 1-Monoglyceride 1,3-Diglyceride Triglyceride
12:0 44 63 56 46
14:0 54 70 65 57
16:0 63 77 72 65
18:0 70 81 78 73
18:1 n-9 (cis)1635 21 5
18:1 n-9 (trans)4458 55 42
18:2 n-6 612 3 13
FATTY ACIDS/Properties 2299

individual fats or to the randomization of mixtures of
two or more fats or oils. The process has several
advantages. For example, lard, which in its natural
form solidifies very slowly on cooling, producing
large, ‘grainy’ crystals, after interesterification, rap-
idly sets on cooling to a compact mass of very small
crystals. Edible tallow, with an inconveniently high
melting point, after interesterification with a soft oil,
such as soya bean oil, yields a soft fat with a very
usefulmeltingrange.(SeeSoy(Soya)Beans:TheCrop.)
0025 Lipolysis Triglycerides are hydrolyzed, albeit very
slowly, by aqueous media, but much more rapidly
by basic catalysts and, more importantly, by endogen-
ous lipolytic enzymes. Oils and fats (e.g., olive oil,
palm oil, tallow) from fruit coats or animal tissues
are particularly prone to lipolysis if they are allowed
to remain too long in contact with bruised tissue
before processing. As a result of such handling,
major processing losses are suffered as a result of the
need to carry out refining operations to remove harsh
flavor taints.
0026 Autoxidation Access of atmospheric oxygen to
unsaturated fatty acids or glycerides leads to deterior-
ation through oxidation. Saturated and monounsatu-
rated fatty chains oxidize very slowly and do not as a
rule cause problems. Diunsaturated chains, as in 18:2
n-6, oxidize more rapidly and polyunsaturated chains
very rapidly. Oils such as fish oils are so liable to
oxidative degradation that they cannot be used as
such in food formulation but must first be hydrogen-
ated. (See Oxidation of Food Components.)
0027 Autoxidation depends on free-radical chain reac-
tions, which involve the interaction of oxygen with
free radicals generated at methylene groups adjacent
to double bonds, especially at methylene groups be-
tween two double bonds. Hydroperoxides are thus
formed, and these, being unstable, break down to
fission products, including some of low molecular
weight. Equation (1) is a summary of a typical reac-
tion sequence.
(R
1
and R
2
are alkyl and alkylene portions of the fatty
chain; G is the nonvolatile glyceride residue.)
0028The aldehydes and other volatile oxidation prod-
ucts have strong, unattractive odors and flavors, and
make a predominating contribution to ‘rancidity.’
Further, peroxides are toxic food components, so
autoxidation must be minimized by all possible
means. It can be avoided, or at least greatly delayed,
by careful and prompt handling and storage of oils
and fats, by avoidance of prooxidative situations such
as contact with metals, and by the use of various
kinds of antioxidants that inhibit steps in the autoxi-
dation process. (See Antioxidants: Natural Antioxi-
dants; Synthetic Antioxidants.)
See also: Antioxidants: Natural Antioxidants; Synthetic
Antioxidants; Cocoa: Production, Products, and Use;
Emulsifiers: Organic Emulsifiers; Uses in Processed
Foods; Fats: Classification; Uses in the Food Industry;
Fish Oils: Dietary Importance; Margarine: Methods of
Manufacture; Offal: Types of Offal; Oxidation of Food
Components; Palm Oil; Phospholipids: Properties and
Occurrence; Soy (Soya) Beans: The Crop;
Triglycerides: Structures and Properties
Further Reading
Allen JC and Hamilton RJ (1989) Rancidity in Foods.
London: Elsevier Applied Science.
Chapman D (1965) The Structure of Lipids by Spectro-
scopic and X-ray Techniques. London: Methuen.
Forss DA (1972) Odour and flavour compounds from
lipids. In: Holman RT (ed.) Progress in the Chemistry
of Fats and Other Lipids, vol. 13. Oxford: Pergamon
Press.
Gunstone FD (1967) An Introduction to the Chemistry
and Biochemistry of Fatty Acids and their Glycerides.
London: Chapman & Hall.
Gurr MI and James AT (1975) Lipid Biochemistry: an
Introduction. London: Chapman & Hall.
Hilditch TP and Williams PN (1964) The Chemical Consti-
tution of Natural Fats. London: Chapman & Hall.
Hudson BJF (ed.) (1990) Food Antioxidants. London:
Elsevier Applied Science.
Markley KS (ed.) (1967) Fatty Acids, their Chemistry,
Properties, Production and Uses. New York: Inter-
science.
Mostofsky DI, Yehuda S and Salem N (eds) (2001) Fatty
Acids: Physiological and Behavioral Functions. Totowa,
USA: Humana Press.
Patterson HBW (1983) Hydrogenation of Fats and Oils.
London: Elsevier Applied Science.
Patterson HBW (1989) Handling and Storage of Oilseeds,
Oils, Fats and Meal. London: Elsevier Applied Science.
Swern D (ed.) (1979) Baily’s Industrial Oil and Fat Prod-
ucts, 4th edn. New York: Wiley.
R
1
−CH
=
CH−CH
2
−R
2
−GR
1
−CH
=
CH−CH−R
2
−G
R
1
−CH
=
CH
−
CHO + HO−R
2
−G
OOH
(1)
2300 FATTY ACIDS/Properties
Metabolism
P Mun
˜
iz, Universidad de Burgos, Burgos, Spain
Copyright 2003, Elsevier Science Ltd. All Rights Reserved.
Fatty Acid Availability
0001 Fatty acids are the principal form of stored energy for
most organisms. Almost all tissues can utilize fatty
acids for energy, exceptions being the brain, blood
cells, skin, and renal medulla. The fatty acids present
two advantages compared with other energetic
biomolecules: their high energy density and low
solubility. Thus, oxidation of tryacylglycerols releases
37 kJ g
1
compared with the 16–17 kJ g
1
for sugars,
glycogen, and amino acids, and fatty acids can be
stored without water.
0002 Most of these fatty acids are stored in adipose
tissue, comprising specialized cells, the adipocytes.
Mammals can store 5–25% or more of their body
weight in the form of lipids, and 90% of these lipids
are tryacylglycerols (TGs). The fat storage is not
static, so the tryacylglycerols are in a constant state
of turnover. The liver, the major center of lipid
metabolism, is largely responsible for regulating
lipid levels in the body. Among its important func-
tions are: synthesis of TG from fatty acids, synthesis
of other lipids such as phospholipids and cholesterol,
desaturation of fatty acids, and catabolism of tryacyl-
glycerols for use as energy.
0003 Since most of the tissues contain only small
amounts of storage lipids, energy production depends
on a continuous supply of fatty acids. The fatty acids
are derived primarily from two sources: exogenous
TG obtained from diet and endogenous TG stores
mainly in the adipose tissue.
Diet Fatty Acids
0004 Tryacylglycerols are the predominant type of lipid
ingested by humans, and they are absorbed as fatty
acids from the intestinal mucosa (enterocytes) into
the lymphatic system. The free fatty acids (FFAs)
inside the enterocytes are reesterified into TGs and
packaged with proteins and phospholipids to form
chylomicrons. Chylomicrons enter the lymphatic
system and eventually into the circulatory system at
the thoracic duct.
0005 Most of the chylomicrons are removed from the
blood into cells by the action of lipoprotein lipase, an
enzyme located on endothelial cell lining the capillar-
ies primarily in adipose tissue, skeletal and cardiac
muscle, and the liver. Lipoprotein lipase hydrolyzes
the TGs into fatty acids and glycerol, and is taken up
into these specific tissues. In adipose tissue, the FFAs
are primarily reesterified and stored as TGs, in other
organs as muscle and liver, and small amounts of TG
are stored intracellularly. The primary sites of FFA
oxidation are cardiac and skeletal muscle and liver.
Adipose Tissue Fatty Acids: Lipolysis
0006Fat stored as tryacylglycerols in adipose tissue and
mobilized in the form of plasma free fatty acids is
the main source of energy in the absence of dietary
substrates; up to 150 g of fatty acids can be liberated
daily, corresponding approximately to half of the
daily caloric needs.
0007Hydrolysis of adipose tissue TGs occurs via three
consecutive reactions and is catalyzed by two
enzymes: the triacylglicerol lipase, also called hor-
mone-sensitive lipase (HSL), and the monoglyceride
lipase (MGL). The rate-limiting enzyme in adipose
tissue lipolysis is HSL. HSL hydrolyzes TGs and
diglycerides, whereas the participation of MGL is
required for complete hydrolysis of monoglycerides.
Then, the three FFA molecules leave the adipose cell
and enter the circulation, where they are transported
bound to albumin. The remaining glycerol backbone
also leaves the cell, because adipose tissue does not
contain the enzyme glycerol kinase, and so glycerol is
not reutilized for reesterification in adipocytes.
0008HSL exhibits a preference, although not absolute,
for the (n-3/n-6) fatty acids from TGs, with approxi-
mately three- to fourfold higher hydrolysis rates to
the 1(3)-ester bonds than to the 2-ester bond. Fatty
acids, i.e., oleic and oleoyl coenzyme A (CoA), and
monoacyglycerols have been shown as inhibitors to
HSL. This feedback inhibition was proposed to pre-
vent the accumulation of fatty acids and free choles-
terol in the cells and to ensure that the capacity of
MGL to hydrolyze MGs is not exceeded. Recently,
adipocyte lipid-binding protein (ALBP) was shown to
interact with HSL, raising the possibility that ALBP
sequesters fatty acids resulting from HSL-catalyzed
lipolysis, and thus preventing the feedback inhibition
by lipolytic products.
0009Regulation of adipocyte lipolysis Fatty acid concen-
trations are the result of the balance between the rate
of appearance (lipolysis) and the rate of clearance.
Today, it is generally accepted that lipolysis is con-
trolled mainly by the activity of the sympatic nervous
system and by plasma insulin levels. The main regula-
tor factor of the rate of adipose tissue lipolysis is the
activity of HSL.
0010HSL activity is mainly regulated by the circulating
concentrations of insulin and epinephrine. These
hormones can change during times of stress, such as
FATTY ACIDS/Metabolism 2301

starvation, trauma, or physical exercise, or after feed-
ing, resulting in an alteration in lipolytic rates and
FFA concentrations. Insulin decreases the activity of
hormone-sensitive lipase, which is responsible for the
breakdown of adipose TG and concomitant release of
the free fatty acids into the circulation. Epinephrine,
norepinephrine, and adrenocorticoids, especially ad-
renocorticotropic hormone, increase the rate of fat
mobilization by stimulating HSL activity.
0011 HSL is hormonally regulated via phosphorylation/
dephosphorylation. The hormone stimulated by
HSL acts through a membrane-bound receptor and
activates the membrane-bound enzyme adenylate
cyclase, resulting in an increase in cyclic adenosine
monophosphate (cAMP) levels in the adipocyte.
cAMP directly activates a protein kinase A (PKA),
which phosphorylates and activates HSL. Lipolytic
agents generally increase the levels of cAMP far
above the concentrations required for maximal
activation of protein kinase A.
0012 Epinephrine is the primary stimulator of lipolysis
working through a b-adrenergic receptor in the
plasma membrane of the adipose cell resulting in
phosphorylation and activation of HSL. The physio-
logical state can affect the sensitivity to epinephrine.
For example, in short-term (3-day) fasting, the
lipolytic responsiveness to epinephrine infusion is
enhanced, whereas in obesity, the responsiveness to
epinephrine is blunted. Catecholamines are able to
stimulate lipolysis via three subtypes of b-adrenergic
receptors, which are positively coupled to adenyl
cyclase by Gs proteins and to inhibit lipolysis via
a2-adrenergic receptors, negatively coupled to the
enzyme by Gi proteins. In humans, the interplay
between a2 and b-adrenergic receptors plays an
important role in modulating cAMP levels in
adipocytes.
0013 However, the inhibition of HSL catalyzes its
dephosphorylation, and so insulin induces a decrease
in cAMP levels and a concomitant decrease in
PKA activity, and inhibits HSL, thus catalyzing its
dephosphorylation. Glucose is the predominant
signal for insulin release, so an effect of glucose intake
on lipolysis would be expected. Thus, in humans, an
increase in glucose concentration in the plasma stimu-
lates insulin release with concomitant increase in glu-
cose uptake and fatty acid reesterification, and a
decrease in lipolysis. The inhibitory effect of glucose
on lipolysis is mediated entirely by insulin.
0014 Under most physiological circumstances, the rate
of lipolysis is largely determined by the balance
between the stimulatory effect of epinephrine and
the inhibitory effect of insulin. For example, in
short-term fasting, there is a marked increase in
the rate of lipolysis, which can be attributed to
both a decrease in blood glucose (and thus insulin)
concentration and an increase in epinephrine concen-
tration and sensitivity to epinephrine. The striking
aspect of the regulation of lipolysis is that the factors
that are primary regulators (insulin and epinephrine)
are not released in response to a signal related to any
aspect of fatty acid metabolism. For example, acute
changes in fatty acid concentrations by infusion do
not affect insulin, catecholamines, or the rate of lipo-
lysis. Therefore, insulin and catecholamines, rather
than being primary regulators of lipolysis, may be
considered to be regulators of other physiological
and metabolic processes that also affect lipolysis. In
fact, the rate of resting lipolysis generally provides
fatty acids at a rate that is far in excess of the rate
required for oxidation. Fatty acids that are released
from adipocytes, but not oxidized, are reesterified,
thereby completing a substrate cycle.
Cellular Uptake of Fatty Acid
0015Fatty acids from the diet or produced by lipolysis are
transported, bound to proteins in blood, and their
cellular uptake is similar. The majority of complex
lipid is hydrolyzed by two related lipases, hepatic
lipase and lipoprotein lipase, and this hydrolysis
enables free fatty acids to enter cells.
0016The uptake of fatty acids across the plasma mem-
brane takes place either by diffusive processes, involv-
ing partitioning of the fatty acid molecule into
the lipid bilayer of the plasma membrane, or by the
presence of different lipid-binding proteins in the cell
membranes, called plasma membrane fatty-acid-
binding proteins (FABPpms).
0017At least five plasma membrane-associated fatty
acid binding proteins were proposed to play a role
in free fatty acid (FFA) uptake, a plasma membrane
fatty-acid-binding protein (FABPpm, 40 kDa), fatty
acid translocase (FAT, 88 kDa), fatty acid transport
protein (FATP 63 kDa), caveolin, and 56-kDa kidney
fatty acid binding protein. Once inside the cell, fatty
acids are bound noncovalently to a family of intra-
cellular fatty acid-binding proteins (FABPs) that may
play a role in the transfer of FFAs to intracellular
destinations where they are used. FABPs comprise a
family of 14–15-kDa proteins that bind long-chain
fatty acids.
Catabolism of Fatty Acids
0018Once within the cell and depending on the tissue and
its metabolic demand, fatty acids are either converted
to tryacylglycerols or membrane phospholipids, or
oxidized in the mitochondria for energy production.
Some metabolic routes are common to most of the
2302 FATTY ACIDS/Metabolism
cells, like b-oxidation, whereas others are tissue-
specific for prostanoid synthesis.
001 9 Before being directed into storage or membranes or
oxidation, fatty acids are first activated to acyl-CoAs.
Fatty Acids Activation and Transport into
Mitochondria
0020 A requisite step for fatty acid entering several meta-
bolic pathways is the formation of fatty acyl-CoA-
thioesters, catalyzed by fatty acyl-CoA synthetase,
with some substypes showing fatty acid chain-length
specificity. The fatty acyl-CoA products of these
enzymes are also bound to FABP.
002 1 Short- and medium-chain fatty acids are trans-
ported into the mitochondria matrix as free acids
and form the acyl-CoA derivatives over there. How-
ever, long-chain fatty acids are normally activated in
outer mitochondrial membrane, but this may also
occur at the surface of the endoplasmic reticulum.
002 2 The enzyme acyl-CoA synthetase, also called acyl-
CoA ligase or fatty acid thiokinase, catalyzes the
formation of a thiol ester bound between the fatty
acid and the thiol group of coenzyme A (eqn (1)).
Fatty acid þ ATP þ CoA-SH !Fatty acyl-CoA
þAMP þ 2Pi ð1Þ
0023 The reaction is accompanied by the hydrolysis of
ATP to form AMP and pyrophosphate. The pyro-
phosphate is rapidly hydrolyzed by inorganic
pyrophosphatase to two molecules of phosphate,
and the synthetase reaction is strongly promoted.
0024 The long-chain acyl-CoA derivatives cannot be
transported into the mitochondria matrix directly.
They must be converted to acylcarnitine derivatives
and then transported through the inner membrane of
the mitochondrion. This transport system consists of
the enzyme carnitine palmitoyltransferase I (CPTI)
localized in the mitochondrial outer membrane, of
an integral inner membrane protein the carnitine:a-
cylcarnitine translocase, and of the enzyme carnitine
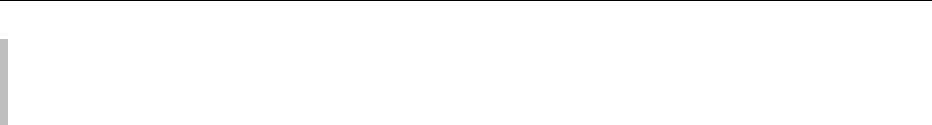
palmitoyltransferase II localized on the matrix side
of the inner membrane as shown in Figure 1. The
enzyme CPTI catalyzes the formation of the O-
acylcarnitine, which is transported across the inner
membrane by a translocase. Inside the mitochondria,
the enzyme carnitine palmitoyltransferase II (CPTII)
transfers the fatty acyl group back to CoA and obtain
fatty acyl-CoA.
b-Oxidation Reactions
0025Once inside the mitochondrial matrix, the fatty acyl-
CoA is catalyzed by the enzymes in the b-oxidative
pathway, resulting in acetyl-CoA production. Energy
produced in the b-oxidation of fatty acids and the
oxidation of acetyl-CoA in the tricarboxylic acid
cycle is used to generate ATP via oxidative phos-
phorylation. The fatty acid oxidation begins with
the oxidation of the carbon that is in ‘b’ position to
the carboxyl carbon, and so this process has come to
be known as b-oxidation.
0026The mitochondrial b-oxidation of saturated fatty
acid acids proceeds by repeated cycles of four
reactions (flavin adenine dinucleotide (FAD)-linked
dehydrogenation, hydration, nicotinamide adenine
dinucleotide (NAD)
þ
-linked dehydrogenation, hy-
dration, NAD
þ
-linked dehydrogenation, and thio-
lysis) with chain shortening being achieved by the
successive cleavage of a C
2
unit as acetyl-CoA at
each cycle until the substrate has been completely
converted in acetyl-CoA. This is catalyzed by the
sequential action of four enzymes families (acyl-CoA
dehydrogenase, enoyl-CoA hydratase, l-hydroxy-
acyl-CoA dehydrogenase, and l-ketoacyl-CoA thio-
lase) each with a different substrate specificity for
short-, medium-, and long-chain acyl-CoAs.
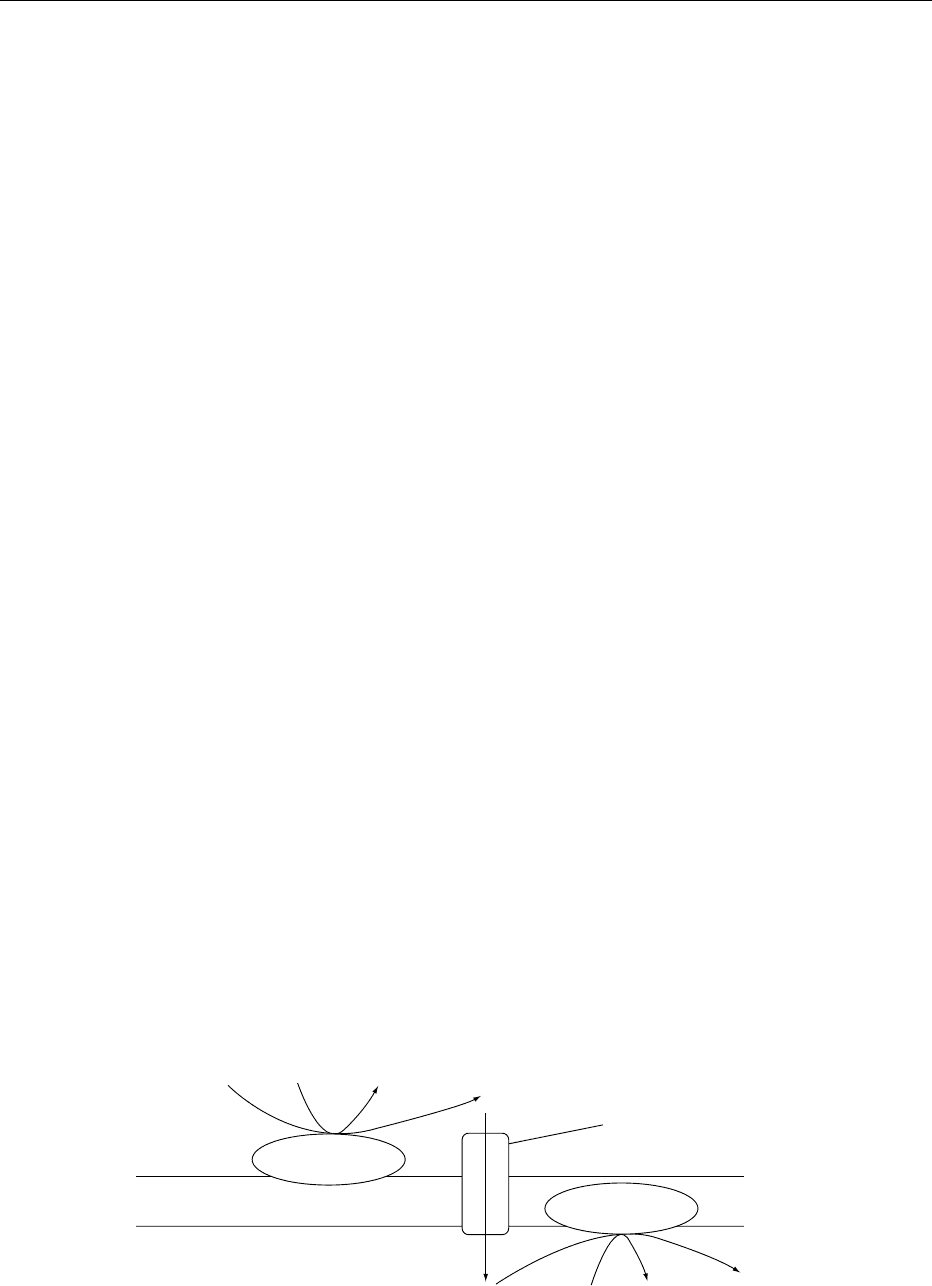
0027As shown in Figure 2, the first reaction is catalyzed
by acyl-CoA dehydrogenase, a flavoprotein that is
present as a family of three enzymes that differ in
their specificity for the length of acyl-CoAs. Their
mechanism involves the oxidation of Ca–Cb bound
L-carnitine Fatty acyl-CoA CoA-SH O-acylcarnitine
Intermembrane
space
Carnitine:acylcarnitine
translocase
O-acylcarnitine CoA-SH Fatty acyl-CoA L-carnitine
Mitochondrial matrix
CPT-I
CPTII
fig0001 Figure 1 Transport into mitochondria of fatty acid.
FATTY ACIDS/Metabolism 2303
to form a trans double bond. During the oxidation of
the fatty acid, the FAD is reduced to FADH
2
, and the
electrons are transfered to an electron transfer flavo-
protein (ETF). Reduced ETF is reoxidized by a
specific oxidoreductase that donates electrons to the
electron transport chain at the level of coenzyme Q.
The next past is a hydrogenation reaction, catalyzed
by the ligase enoyl-CoA hydratase that saturates the
new double bond by the addition of a hydroxyl group
in the beta position. At least three enoyl-CoA hydra-
tase activities are known. These enzymes present
stereospecific and specifically converted trans-enoyl-
CoA derivates to l-b-hydroxyacyl-CoA. The fourth
reaction cleaves the b-keto ester, yielding one mol-
ecule of acetyl-CoA and a fatty acyl-CoA shortened
in two carbons.
0028 The repetitions of this cycle with the shortened
fatty acyl-CoA achieve the complete b-oxidation of
fatty acid. At the final step of this cycle, a fatty acid
with an even number of carbons yields two molecules
of acetyl-CoA.
0029 Fatty acids with an odd number of carbon atoms
are rare in mammals but are common in plants and
marine organisms. Humans and animals, whose diets
include these food sources, metabolize odd-carbon
fatty acids via the b-oxidation pathway. The final
product of b-oxidation in this case is the 3-carbon
propionyl-CoA instead of acetyl-CoA. Three special-
ized enzymes then carry out the reaction that converts
propionyl-CoA to succinyl-CoA, a TCA cycle inter-
mediate that may be oxidized to CO
2
.
0030The oxidation of polyunsaturated fatty acids in-
volves the action of two additional mitochondrial
enzymes NADPH (nicotinamide adenine dinucleotide
phosphate)-linked enoyl-CoA isomerase and D
2
D
4
–
enoyl-CoA reductase. They are needed to handle the
cis-double bonds of naturally occurring fatty acids.
Other Aspects of Fatty Acid Oxidation
0031Peroxisomes also have a system for the limited
b-oxidation of long-chain fatty acids to short-chain
acyl-CoA esters and acetyl-CoA. This short-chain
product must be transferred to the mitochondria for
further breakdown. Peroxisomal b-oxidation is
similar to mitochondrial b-oxidation, except that
the initial double-bond formation is catalyzed by an
FAD-dependent acyl-CoA oxidase.
0032In microsomes, unsaturated fatty acids are oxidized
to form eicosanoids and epoxy and hydroxy-fatty
acids. Some of these oxidative steps yield regulatory
molecules involved in cell signaling. For example,
arachidonic acid released from the sn-2 position
of the membrane phospholipids by the action of
phospholipase A
2
provides a substrate for cyclooxy-
genaxes, lipoxygenase, or monooxygenase.Cycloox-
ygenase and lipoxygenase products of arachidonic
acid (20:4, n-6) produce eicosanoids as prosta-
glandins, thromboxanes, and leukotrienes. These
eicosanoids play a critical role coordinating physio-
logical interactions among cells and have an influence
in a wide variety of functions, including those of the
central nervous system and the contraction of smooth
muscles. They also inhibit the mobilization of fatty
acids from adipose tissue, have an antiinflamatory
effect and modify the blood pressure, aggregation of
blood platelets, and cardiac function.
0033Branched-chain fatty acids are oxidized by
a-oxidation pathway. The CoA ester of this metabolic
pathway can undergo b-oxidation in the normal way.
Regulation of Fatty Acid Oxidation
0034Acetyl-CoA formed by mitochondrial oxidation can
be oxidized by the citrate cycle. The complete oxida-
tion of fatty acids in peripheral tissues is therefore
a major source of metabolic energy and heat in
humans. In liver, most of the acetyl-CoA formed by
b-oxidation is converted to ketone bodies (acetoace-
tate and 3-hydroxybutyrate), which are exported as
metabolic fuels for extrahepatic tissues. Peroxisomal
b-oxidation in the liver is less pronounced than in
mitochondria, but it has a key role in metabolizing
some very-long-chain fatty acids, although it is
Fatty acyl-CoA
FAD
FADH
2
Acyl-CoA
dehydrogenase
trans ∆
2
−Enoil-CoA
Enoyl-CoA
hydratase
H
2
O
L-β-hydroxyacyl-CoA
L-hydroxyacyl-CoA
dehydrogenase
NAD
+
NADH + H
+
β-Cetoacyl-CoA
Thiolase
CoA-SH
Acetyl-CoA
Fatty acyl-CoA
(Shortened by two carbons)
fig0002 Figure 2 b-Oxidation of saturated fatty acids.
2304 FATTY ACIDS/Metabolism

not directly linked to ATP synthesis. The rate of b-
oxidation is adjusted to physiological needs. This
sequence of events has two potential sites of regula-
tion, (a) transport of fatty acids into the cell, and (b)
enzymatic regulation.
0035 Fatty acid transport Long-chain fatty acids can be
transferred passively across mammalian cell mem-
branes. A simple diffusion process becomes signifi-
cant at higher molar ratios of fatty acid to albumin as
the concentration of free fatty acid in solution is
increased. However, under physiological conditions
of low fatty acid to albumin ratios in the circulation,
the major fraction of uptake appears to be mediated
by a protein component. Therefore, the plasma-
membrane-associated and cytoplasmic fatty-acid-
binding proteins are involved in cellular fatty acid
uptake, transport, and metabolism in tissues. These
binding proteins may also act modulate the metabol-
ism of long-chain fatty acids implicated in the regula-
tion of cell growth and other cellular functions.
0036 An acute increase in fatty acid concentration causes
a corresponding increase in fatty acid uptake without
necessarily increasing fatty acid oxidation. Thus,
fatty acid oxidation is more likely to be regulated by
factors inside the cell than by limitations in transport.
0037 The FABP exists within both the cytosol and
nucleus, which suggests that fatty acids or fatty
acid-CoA may be in the nucleus and act as ligands
that regulate the activity of specific transcription
factors.
0038 Enzymatic regulation When plasma FFAs enter the
cells, the first important step in their oxidation is the
formation of fatty-acyl-CoA. The enzymatic regula-
tion of CPT-I will then determine whether the fatty-
acyl-CoAs will be transferred into the mitochondria
for subsequent oxidation.
0039 The reaction catalyzed by CPT-I has been con-
sidered to be rate-limiting. CPT-I is subject to regula-
tion at the transcriptional level and to acute control
by malonyl-CoA. Thus, the N-terminal domain of
CPT-I is essential for malonyl-CoA inhibition.
0040 Malonyl-CoA, which is synthesized by acteyl-CoA
carboxylase, is an essential metabolic intermediate in
the regulation of fatty acid oxidation. A decrease in
malonyl-CoA level results in an increase in CPT-I
mediated fatty acid uptake into the mitochondria.
As fluctuations in tissue malonyl-CoA content are
parallel with changes in acetyl-CoA carboxylase
activity, which in turn is under the control of 5
0
-
AMP-activated protein kinase, the CPT-I/malonyl-
CoA system is part of a fuel-sensing gauge, turning
fatty acid oxidation on and off, depending on the
tissue’s energy demand.
0041No allosteric regulation or control of their activ-
ities by covalent modification of the other enzymes of
the b-oxidation pathway appears to have been de-
scribed, and it is now recognized that flux control of
flux through a pathway is shared between all the
enzymes involved, although their individual flux-
control coefficients may be very different.
Fatty Acid Biosynthesis. Lipogenesis
0042Long-chain fatty acids are essential constituents of
membrane lipids and are important substrates for
energy metabolism of the cell. When total energy
intake is in excess of the energy used, fatty acids and
triacylglycerol are synthesized.
0043The synthesis of fatty acids de novo is achieved
by the sequential condensation of two-carbon units
derived initially from acetyl-CoA.
0044Palmitate, the most abundant acid, is synthesized
de novo from acetyl-CoA, by acetyl-coA carboxylase
(ACC) and fatty acid synthase (FAS) in the cytoplasm.
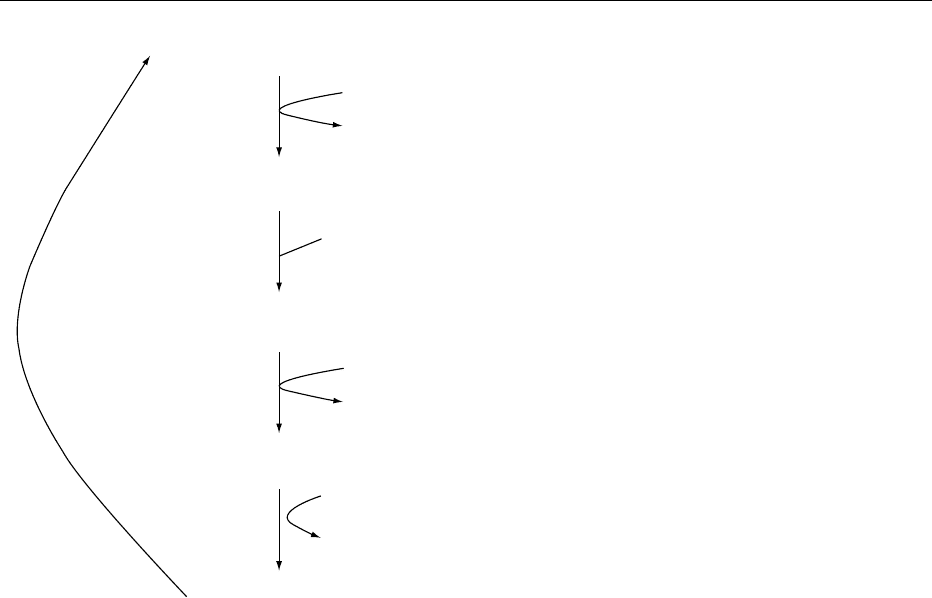
0045ACC catalyzes the carboxylation of acetyl-CoA to
malonyl-CoA in an ATP-dependent manner. The re-
action catalyzed by this enzyme is shown in Figure 3.
0046Two forms of ACC have been identified. The
enzyme that is involved in the synthesis of long-
chain fatty acids has a molecular weight of 265 kDa,
and the other isoform, with a molecular weight of
275–280 kDa, may be involved in the regulation of
mitochondrial oxidation of fatty acids.
0047FAS plays the central role in de-novo lipogenesis in
mammals, catalyzing all reaction steps in the conver-
sion of acetyl-CoA and malonyl-CoA to palmitate by
enzymatic reactions catalyzed by FAS (Figure 4).
0048The reaction of FAS involves increasing the length
of the acetyl group by C
2
units derived from malonyl-
CoA in a stepwise and sequential manner. For in-
stance, in the synthesis of palmitate, there are over
40 steps with at least 30 acyl intermediates. A protein
known as acyl carrier protein (ACP) with its 4
0
-
phosphopantetheine prosthetic group was identified
as the coenzyme that binds all acyl intermediates as
thioester derivatives.
0049Seven enzymes and reactions are involved in the
synthesis of palmitate, as shown in Figure 5. These
reactions are essentially the same in all organisms.
Acetyl and malonyl are introduced as acyl carrier pro-
tein conjugates (reactions 1 and 2). Decarboxylation
HCO
3
+ ATP + E
.
Biotin E
.
Biotin
.
CO
2
+ ADP + P
i
(A)
E
.
Biotin
.
CO
2
+ Acetyl-CoA Malonyl-CoA + E
.
Biotin(B)
−
−
−
fig0003Figure 3 Reactions catalyzed by acetyl-coenzyme A carboxy-
lase.
FATTY ACIDS/Metabolism 2305
drives the b-ketoacyl-ACP synthase and results in the
addition of two carbon units to the growing chain
(reaction 3). The b-ketoacyl derivative is reduced in
three consecutive steps (reactions 4–6) to the satur-
ated acyl derivative, which then acts as a primer
for further elongation and reduction cycles to yield
ultimately a palmitoyl derivative. The latter is either
hydrolyzed to free palmitate (reaction 7), as in animal
cells and bacteria, or transferred to CoA-SH to form
palmitoyl-CoA, as in yeast, or utilized directly in the
triacylglycerol and phospholipid synthesis.
0050 In animal cells, the component enzymes of fatty
acid synthesis are covalently linked on a single poly-
peptide chain. From the N-terminus of FAS to its
C-terminus, amino acids encoding b-ketoacyl syntha-
tase, acetyl-CoA transacylase, malonyl-CoA trans-
acylase, dehydratase, enoyl reductase, b-ketoacyl
reductase, acyl carrier protein, and thioesterase activ-
ities are organized into discrete domains in the order
indicated. This is in contrast to bacterial and plant
FAS, which are multienzyme complexes consisting
of discrete monofunctional enzymes and fungal FAS,
which has functional components that are distributed
between two nonidentical polypeptides.
0051 The most important feature of animal FAS is its
multifunctional character. The animal FAS represents
one of the more complex multifunctional polypeptide
structures discovered to date because a single poly-
peptide structure contains all the catalytic compon-
ents required to direct the 37 reactions that lead to the
formation of palmitic acid from acetyl and malonyl-
CoA. The functional enzyme is a homodimer of the
250-kDa subunits and contains, in separate domains,
the seven different catalytic activities and the site
for the prosthetic group, 4
0
-phosphopantetheine, of
the acyl carrier protein (ACP). The multifunctional
nature of the subunits and their head-to-tail organiza-
tion produce a highly efficient enzyme complex
capable of carrying out multiple reactions leading to
the synthesis of a palmitate molecule from one acteyl
and seven malonyl moieties. This multifunctional
organization of FAS in vertebrates was probably
selected in the course of evolution, because it is
more efficient and because the partial activities are
more easily regulated in a coordinated fashion. The
substrates for each reaction can be channeled to the
active center of the subsequent enzymatic step within
the same polypeptide, thus providing a high efficiency
in long-chain fatty acid synthesis. Moreover, regulat-
ing production of the single polypeptide has an effect
at all the catalytic steps in a concerted manner.
Additional Elongation
0052Palmitate is the primary product of the fatty acid
synthase, but the cells may synthesize many other
fatty acids. Shorter chains can be made easily if the
chain is released before it reaches 16 carbons in
length. Longer chains are made through special
elongation reactions, which occur both in the mito-
chondria and at the surface of the endoplasmic reticu-
lum. The mitochondrial reactions involve addition
and subsequent reduction of acetyl units. The endo-
plasmic reticulum reactions involve the addition of
two-carbon units at the carboxyl end of the chain
by means of oxidative decarboxylations involving
malonyl-CoA.
Introduction of a Single
Cis
Double Bond
0053Prokaryotes and eukaryotes are able to introduce an
unsaturation (one or more double bond) in a fatty
Enzyme Reaction
Acetyl-CoA + ACP-SH Acetyl-ACP + CoA-SH
Malonyl-CoA + ACP-SH Malonyl-ACP + CoA-SH
Acetyl-ACP + synthase-SH acetyl-synthase + ACP-SH
Acetyl-synthase + Malonyl-ACP Acetoacetyl-ACP + CO
2
+ synthase-SH
Acetoacetyl-ACP + NADPH + H
+
D-Hydroxybutyryl-ACP + NADP
+
D-Hydroxybutyryl-ACP Crotonyl-ACP + H
2
O
Crotonyl-ACP + NADPH + H
+
Butyryl-ACP + NADP
+
Palmitoyl-ACP + H
2
O Palmitate + ACP-SH
(1) Acetyl transacylase
(2) Malonyl transacylase
(3) β-Ketoacyl synthase
(condensing enzyme)
(4) β-Ketoacyl reductase
(5) β-Hydroxyacyl dehydratase
(6) Enoyl reductase
(7) Thioesterase
fig0005 Figure 5 Reactions and component enzymes of fatty acid synthase.
Acetyl-CoA + 7 Malonyl CoA + 14 NADPH + 14 H
+
+ 7 ATP + H
2
O Palmitic ac. + 8 CoA + 14 NADP
+
+ 7 ADP + 7 P
i
fig0004 Figure 4 Reaction catalyzed by fatty acid synthase.
2306 FATTY ACIDS/Metabolism

acid. Double bonds in fatty acids are predominantly
of the cis (or Z) configuration. Many prokaryotes
introduce double bonds into fatty acids anaerobically,
whereas eukaryotes have adopted an O
2
-dependent
pathway. So, the advent of an aerobic environment
several billion years ago allowed eukaryotes, cyano-
bacteria, and some bacilli to desaturate the methyl-
ene groups of long-chain fatty acids using enzymes
called fatty acid desaturases. The transition from
anaerobic to aerobic respiration yielded more than
an order of magnitude of energy efficiency, leaving
a surplus available for processes such as oxidative
desaturation. In addition, the ability to regulate
membrane fluidity controlling the number of double
bonds in fatty acids within the membrane in response
to changing temperatures probably conferred a
selective advantage to organisms capable of aerobic
desaturation.
0054 The anaerobic biosynthesis of unsaturated fatty
acids involves dehydration of a hydroxy substrate
followed by trans–cis isomerization of the double
bond. The aerobic reaction can occur anywhere in the
fatty acid chain without the need to activate the desired
bond toward dehydrogenation. Fatty acid desatura-
tion involves an enzymatic reaction in which a double
bond is introduced into an acyl chain, and a molecule
of oxygen is completely reduced to water. Two classes
of fatty acid desaturase enzymes capable of convert-
ing saturated to monounsaturated fatty acids are
known, one soluble and the other membrane-bound.
Desaturase enzymes need the presence of NADH and
oxygen, and two other proteins, cytochrome b
5
and
cytochrome b
5
reductase, are involved.
0055 Mammals require polyunsaturated fatty acids but
must acquire them in their diet. As such, they are
referred to as essential fatty acids (linoleic and lino-
lenic acid). However, mammals can add additional
double bonds to unsaturated fatty acids from their
diets. Three major groups of dietary fatty acids are
oleic acid, linoleic acid, and linolenic acid. These fatty
acids serve as precursors for the biosynthesis of a
long-chain polyunsaturated fatty acid with carbon
lengths of C20/C22. These biosynthetic pathways
consist of a series of desaturation and chain elonga-
tion steps. Desaturation occurs only toward the carb-
oxylic end of fatty acids in mammalian tissues, and
there is no direct crossover among unsaturated fatty
acids from one group to another.
Regulatory Control of Fatty Acid Biosynthesis
0056 Variations in the composition and quantity of the diet
and rates of de novo fatty acid and triacylglycerol
synthesis are tightly regulated by nutritional and
hormonal status to meet the body’s requirement for
lipid and energy storage.
0057The activity of the lipogenic pathway is dependent
on nutritional conditions, both in the liver and in the
adipose tissue. Consumption of a diet rich in carbo-
hydrates stimulates the lipogenic pathway, whereas
starvation or consumption of a diet rich in lipids and
poor in carbohydrates decreases its function. Flux
through the lipogenic pathway depends on the avail-
ability both of lipogenic substrates and of cofactors
such as NADPH produced by the pentose phosphate
pathway. Regulation of the activity of the lipogenic
enzymes involves both short-term and long-term
mechanisms.
0058ACC is the rate-limiting enzyme in the biosynthesis
of fatty acids. The ACC activity and the rate of fatty
acid synthesis fluctuate rapidly in response to various
factors such as hormonal, dietary, developmental,
and genetic factors. In the regulation of ACC, short-
term changes in the enzymatic activity of ACC are
through allosteric regulation, phosphorylation/
dephosphorylation events and polymerization/de-
polymerization mechanisms linked to the presence
of specific metabolites as Ca. However, long-term
regulation mechanisms, particularly those acting at
the gene level of ACC, are controlled at a transcrip-
tion level and involve changes in the concentrations of
regulated enzymes, for example, those observed in
animals being fasted and then fed.
0059The expression of the FAS gene is also highly
dependent on the nutritional conditions in liver and
adipose tissue. Expression of the gene is barely detect-
able in starved animals and is stimulated by refeeding
with a high-carbohydrate, fat-free diet.
0060Thus, the amount of carbohydrate in the diet
appears to be instrumental in turning on transcription
of genes coding for lipogenic enzymes in liver and
adipose tissue. Rates of expression of the genes for
FAS and ACC are stimulated by glucose in adipose
tissue in vivo and in vitro. Expression of FAS and
ACC is stimulated in the liver and of ACC in a pan-
creatic b-cell line. In each case, regulation involves
stimulation of transcription, and to stimulate gene
transcription, glucose must be metabolized. To date,
the role of insulin, either direct or indirect, is still
disputed. Indeed, insulin is reported to restore lipo-
genic enzyme gene expression in diabetic rats, and
glucagon (via cAMP) inhibits expression of the genes
for lipogenic enzymes. In adipose tissue, insulin in-
creases indirectly the expression of FAS and ACC by
stimulating glucose transport.
0061Although normal tissues have low levels of fatty
acid synthesis, a number of recent studies have
demonstrated high levels of FAS expression in a
wide variety of human cancers, including carcinoma
of the colon, prostate, ovary, endometrium, and
breast. The widespread expression of FAS in human
FATTY ACIDS/Metabolism 2307
