Caballero B. (ed.) Encyclopaedia of Food Science, Food Technology and Nutrition. Ten-Volume Set
Подождите немного. Документ загружается.


equivocal evidence suggests a potential role for vita-
mins A, C, E, and niacin and the minerals chromium
and vanadium in diabetes. Alternative sweeteners,
e.g., sorbitol and saccharin, are accepted in diabetes
management but their value is unclear. The control of
hyperglycemia by diet and medication is associated
with reduced risk of some of the long-term compli-
cations of diabetes.
Obesity
0025 The determination of obesity in the elderly is prob-
lematic since few body weight standards specific to
this age group are in use. The prevalence of obesity
appears to increase with age. Weight gain normally
occurs during the adolescent growth spurt and again
during middle age. Basal metabolic rate and energy
expended for physical activity decline during adult-
hood so that fewer calories are required to maintain
energy balance; however, many middle-aged and
older adults often do not adjust their caloric intake
to compensate for their reduced energy requirements
and gain weight even though they do not eat more
than before. Body weight generally peaks between 35
and 55 years in men and between 55 and 65 years in
women; body weight decreases thereafter in both
sexes. Obesity aggravates many health conditions
found among the elderly including arthritis, cardio-
vascular diseases and hypertension, and type 2
diabetes.
Osteoporosis
0026 Primary osteoporosis is an age-related disorder char-
acterized by decreased bone mass and increased
susceptibility to fractures in the absence of other
recognizable causes of bone loss. Postmenopausal
osteoporosis (type 1) occurs in women within 15–20
years after menopause and is thought to result from
factors related to or exacerbated by estrogen defi-
ciency. Age-related osteoporosis (type 2) occurs in
men and women over 75 years of age and may be
more directly related to the aging process. Whites are
at higher risk of osteoporosis than blacks. Other risk
factors include dietary factors, cigarette smoking,
physical inactivity, alcohol abuse, being underweight,
and family history of osteoporosis. Osteoporosis is
more than six times as common among women than
men due to their smaller peak bone mass, earlier
onset of bone loss, longer life expectancy, and lower
calcium intake.
0027 Substantial evidence supports a role for calcium as
a protective agent against osteoporosis. High calcium
intake during early years contributes to greater peak
bone mass and during later years prevents negative
calcium balance and reduces the rate of bone loss.
Poor calcium nutriture is common among the elderly
due to inadequate intake, an age-related decline in the
capacity for calcium absorption, and the presence of
diseases associated with reduced calcium absorption
and/or increased calcium excretion. Vitamin D is
essential for the efficient absorption of calcium but
vitamin D status is quite low among the elderly due to
inadequate intake and age-related impairments in the
metabolic conversion of vitamin D to its biologically
active form, including lower precursor concentra-
tions of 7-dehydrocholesterol in the skin. Less
well-established dietary risk factors for osteoporosis
include low intakes of vitamin K or boron and high
consumption levels of caffeine, protein, or alcohol.
The principal measures employed in the prevention
of osteoporosis include estrogen replacement in
postmenopausal women, elemental calcium intakes
of 1000–1500 mg day
1
, vitamin D intakes of
10–20 mg cholecalciferol day
1
, and a program of
modest weight-bearing exercise. These measures may
retard further bone loss in the elderly but will not
restore lost bone or reverse the loss in height or col-
lapsed vertebrae characteristic of osteoporosis.
See also: Anemia (Anaemia): Other Nutritional Causes;
Anorexia Nervosa; Cancer: Epidemiology; Diet in
Cancer Prevention; Coronary Heart Disease: Etiology
and Risk Factor; Prevention; Dehydration; Dietary Fiber:
Effects of Fiber on Absorption; Lipoproteins; Obesity:
Etiology and Diagnosis; Epidemiology; Osteoporosis
Further Reading
Bendich A and Deckelbaum R (1997) Preventive Nutrition,
The Comprehensive Guide for Health Professionals.
Totowa, NJ: Humana Press.
Chernoff R (1999) Geriatric Nutrition. Rockville, MD:
Aspen.
Graham I, Refsum H, Rosenberg IH and Ueland PM (1997)
Homocysteine Metabolism: From Basic Science to
Clinical Medicine. Boston: Kluwer Academic.
Harman D, Holliday R and Meydani M (1998) Towards
Prolongation of the Healthy Life Span. New York, NY:
New York Academy of Sciences.
Holliday R (1995) Understanding Ageing. New York, NY:
Cambridge University Press.
Rosenberg IH (1995) Nutritional Assessment of Elderly
Populations: Measure and Function. New York, NY:
Raven Press.
Rowe JW and Kahn RL (1998) Successful Aging. New
York: Pantheon Books.
Schneider EL and Rowe JW (1996) Handbook of the Biol-
ogy of Aging. Orlando, FL: Academic Press.
Sies H (1997) Antioxidants in Disease Mechanisms and
Therapy. San Diego: CA: Academic Press.
Taylor A (1999) Nutritional and Environmental Influences
on the Eye. Boca Raton, FL: CRC Press.
ELDERLY/Nutritionally Related Problems 2027
Nutritional Management of
Geriatric Patients
M S J Pathy, Cyncoed, Cardiff, UK
A Bayer, Llandough Hospital, Penarth, UK
Copyright 2003, Elsevier Science Ltd. All Rights Reserved.
Background
0001 At all ages, adequate nutrition is critical for maintain-
ing health and quality of life. In general, dietary pro-
tein and energy requirements are substantially less in
the over 85s than those aged 65–74 years, and there is
an increased need for certain vitamins and minerals.
However, individual requirements are influenced
greatly by lifestyle and by disease. Maintenance of
physical fitness and strength in old age largely
depends on continued physical and mental activity,
with enough to eat and a diet that is sufficiently
varied. Elderly people in low socio-economic groups,
those in institutions, and the housebound who are
receiving home care are especially vulnerable to
undernutrition, through underprovision and inad-
equate intake. Drugs and disease may also interact
with the complex metabolic processes necessary for
breaking down and absorption of food. Increasingly,
calorie overconsumption is a problem in Western
society, with 25% of men and 35% of women in the
65–74 age range being reported as overweight and
10% being severely overweight.
0002 In the UK, the Committee on the Medical Aspects
of Food and Nutrition Policy (COMA) laid down
general guidelines for dietary requirements of older
people together with modifications in disease states.
Table 1 summarizes the dietary reference values
(DRVs), which replace the earlier recommended diet-
ary allowances (RDA). The reference nutrient intake
(RNI) represents the sum of the estimated average
requirement (EAR) and two standard deviations.
Energy
0003 A reduction in physical activity and lean body mass in
old age lead to a decline in energy requirements by
about one-third. However, there is no reduction in
basal metabolic rate relative to the metabolically
active cell mass. Infection, trauma (accidental or sur-
gical), and the ergonomic impact of disability on daily
living tasks all serve to increase energy demands.
Dyspnea at rest or exertion (commonly seen in pa-
tients with chronic pulmonary obstructive airways
disease) and impaired immunological response to
infection also require increased energy intake as part
of therapeutic management.
0004COMA recommends that 50% of food energy is
derived from carbohydrate – a term that embraces
starch and nonstarch polysaccharides. The main
source of starch is influenced by ethnicity and culture,
with bread, potatoes, breakfast cereals, rice, and
pasta predominant in the UK. Distinction is made
between intrinsic sugars (milk sugar, and sugar in-
corporated in the cellular structure of fruit and vege-
tables) and extrinsic nonmilk sugars (extracted from
the fruit stem and roots of plants and added to food,
confectionery, and soft drinks). A high extrinsic sugar
intake may reduce the dietary quality and in the den-
tate increases the risk of caries.
0005Different carbohydrates have different glycemic
indexes (Table 2). This is the area of the blood sugar
curve produced by a food, compared with the equiva-
lent amount of glucose. Glucose has an arbitrary
glycaemic index of 100. Previously, white bread was
taken as the standard. Excess high glycemic index
carbohydrates are associated with a low high-
density-lipoprotein (HDL) cholesterol concentration,
tbl0001Table 1 Dietary reference values for older men and women
(based on COMA recommendations)
Nutrition Sex/age (years) Estimated
average
requirements
(EAR)
Reference nutrient
intake (RNI)
Energy
a
M 65–74 9.71 MJ
M75þ 8.77 MJ
F 65–74 7.96 MJ
F75þ 7.61 MJ
Protein M 50þ 53.3 g
F50þ 46.5 g
Vitamin A M 700 mg
F 600 mg
Vitamin D M/F 10 mg
Vitamin C M/F 40 mg
Thiamin M 1.0 mg
F 0.8 mg
Riboflavin M 1.3 mg
F 1.1 mg
Niacin M 16 mg
F12mg
Vitamin B
12
M/F No recommendation
Vitamin E M/F No recommendation
Phosphorus M/F 500 mg
Magnesium M 300 mg
F 270 mg
Iron M/F 8.7 mg
Potassium M/F 350 mg
Zinc M/F 9 mg
Copper M/F 1.2 mg
Sodium M/F 6 g
Fluid M/F 1.5 l
a
No RNI for fat/carbohydrates (expressed as EAR due to the close
correlation between energy requirement and expenditure).
M, male; F, female.
2028 ELDERLY/Nutritional Management of Geriatric Patients
rapid absorption, and a high postprandial glucose
and insulin response, ultimately giving rise to
decreased insulin sensitivity. Total cholesterol and
low-density-lipoprotein (LDL) cholesterol are not in-
fluenced. One community study has confirmed that
low-glycemic-index diets are associated with raised
HDL cholesterol levels and the longitudinal Nurse
Health Study reports that diets with a high glycemic
index are associated with an increased risk of coron-
ary heart disease (CHD). Increasing prominence is
being given to the role of high-glycemic diets and
the increasing prevalence of type 2 diabetes mellitus.
0006 Fat is the most concentrated calorie nutrient. In
the USA, it is recommended that 30% or less of
calories should be derived from fat, of which no
more than 10% should be saturated. The UK Health
of the Nation aims to reduce average percentages of
food energy derived from fat by at least 12% by
2003 and that derived from saturated fat by 35%
by 2005. The chief source of saturated fat is meat,
butter, cheese, and cream. Unsaturated fats are de-
rived mainly from plant sources, especially nuts,
olive oil, rapeseed oil, some margarines, and fish.
Evidence supports the role of saturated fats and
trans-fats (hydrogenated polyunsaturates) in athero-
matous vascular disease, although infection may be
the initial trigger. COMA recommended a reduction
of saturated fat and total fat contribution to the diet.
However, there is no correlation between polyunsat-
urated fat intake and LDL levels. Indeed, the unsat-
urated fat in fish and in olive oil – about 70%
monounsaturated – enhances the plasma concentra-
tion of the vascular-protective HDL cholesterol. The
Nurse Health Study showed that women taking at
least one ounce (15 g) of nuts five times or more a
week had a greater reduction in risk of CHD than
those who took them less frequently. Experimental
diets replacing animal fats with nuts lowered LDL
cholesterol and raised HDL cholesterol. Walnuts are
high in linoleic acids, but most nuts are rich in argin-
ine, a precursor of nitric oxide. A major longitudinal
study showed that an increase in polyunsaturated fat
intake accompanied by a reduced consumption of
trans-fats diminishes the risk of type 2 diabetes mel-
litus. Studies based on Mediterranean diets (charac-
terized by abundant fruit and vegetables, especially
garlic and onions, cereals, beans, nuts, seeds, olive
oil, fish and poultry) have reported a reduced risk of
CHD and cancer.
0007Although a reduction in total dietary fat has no
affect in reducing blood pressure, increasing the diet-
ary polyunsaturated : saturated ratio or changing to
diets rich in linoleic acids produces a moderate blood-
pressure reduction. However, one study reported that
attempts to enhance compliance with dietary recom-
mendations in the over-70s was only half as successful
as in the 60–69-year age group.
Protein
0008By age 70, skeletal muscle may have lost an average of
40% of its cell mass. Protein synthesis decreases as
body cell mass falls with age and is associated with a
decline in function. Functional decline is not irrevers-
ible and maintenance of physical activity or physical
training may increase muscle strength and cardiac
output. Protein malnutrition is associated often with
profound muscle loss and weakness, and impaired
immunological competence. However, this stage is
usually compounded by other nutritional deficiencies
and by serious disease.
0009Debate continues about protein requirements in
old age. Studies on free-living and institutionalized
older people suggest that the daily protein require-
ment should be about 1.0 g kg
1
and about 12–14%
total calories. Inflammatory conditions and tissue
necrosis (e.g., pressure sores) increase the protein
turnover and requirement, and pressure-sore healing
rates are influenced greatly by dietary protein intake.
Protein malnutrition may follow major surgery or
severe acute illness in elderly people and can seriously
impair subsequent rehabilitation if left untreated.
Vitamins and Minerals
0010Vitamin and mineral supplements are necessary to
treat well-defined deficiency disorders, but their role
is less certain in the absence of obvious clinical
tbl0002 Table 2 Glycemic index of selected foods (mean values)
Food Glycemic index
Glucose 100
Instant rice 91
Baked potato 85
Cornflakes 84
White bread 70
Wholemeal bread 69
Sucrose (table sugar) 65
White rice (basmati) 58
Boiled potato 56
Banana 55
Baked beans (canned) 48
Orange 43
Pasta (spaghetti) 41
Apple 36
Milk 27
Kidney beans 27
Fructose 23
Derived from 600 entries in Foster-Powell K and Miller J (1995)
International Table of Glycemic Index. American Journal of Clinical Nutrition
62: 8715–8935.
ELDERLY/Nutritional Management of Geriatric Patients 2029

abnormality. Many older people fail to make the
reference values for vitamin D, but the synthesis of
vitamin D
3
(cholecalciferol) by the action of sunlight
(UVL with a wavelength of 290–310 nnm) on the skin
contributes some two-thirds of the vitamin D stores.
Standard household glass prevents the passage of any
therapeutic wavelength of UVL, and housebound and
institutionalized patients are particularly susceptible
to vitamin D deficiency. Subtle degrees of vitamin D
deficiency lead to secondary hypoparathyroidism, in-
creased bone turnover and osteoporotic fractures.
Common dietary sources of vitamin D include eggs,
cheese, margarine (fortified with vitamins D and A),
and oily fish. Randomized controlled trials of dietary
supplementation with 17.5 mg (700 IU) and 20 mg
(800 IU) of vitamin D and 500 mg of calcium per
day show a reduced incidence of hip and other
nonvertebral fractures, whereas 10 mg (400 IU) of
vitamin D does not reduce the fracture rate. There is
considerable evidence for using vitamin D and cal-
cium supplements in the vulnerable elderly, provided
overdosage is avoided. Exposure to sunlight, even
diffuse sunlight, is also to be encouraged.
0011 Water-soluble vitamin C is readily destroyed during
food preparation and storage, and the COMA recom-
mendation of 40 mg does not take this into account.
The delay between preparation and delivery to the
patient in hospital or nursing home or of meals on
wheels to the person at home is often sufficient
to substantially reduce the vitamin C content. Meals
on wheels are reported to have lost some 90% of the
vitamin C content by the time of delivery. Older
people eat vegetables more regularly than young
adults, but elderly men who live alone have diets
poor in vitamin C-rich foods such as fresh green vege-
tables and fruit. Scurvy is uncommon, but chronic
mild deficiency is not infrequent and may play a role
in atherogenesis and stroke. The inverse correlation
between plasma fibrinogen concentration and serum
ascorbate levels suggests that vitamin C supplemen-
tation may be cardioprotective.
0012 Vitamin A intake is very variable, but needs tend to
decrease with age, as absorption may be increased,
whilst plasma clearance is delayed. However, it is
often difficult to be certain whether homeostasis is
achieved, or whether subclinical vitamin A states are
common and unrecognized. Failure of dark adapta-
tion is a well-recognized vitamin A deficiency phe-
nomenon, but dryness of the eyes and perifollicular
hyperkeratosis are uncommon deficiency manifest-
ations in the Western World. In some third world
countries, vitamin A deficiency is the commonest
cause of blindness. The potential benefit of the anti-
oxidant properties of vitamin A and the closely related
b-carotene have yet to be established.
0013Thiamin (vitamin B
1
) intake is closely related to
energy consumption. Older people generally eat
breakfast (‘something to eat within 2 hours of rising’),
and this commonly includes cereals and fortified
cereals containing adequate thiamin. If disease or
institutionalization impairs energy consumption,
thiamin intake may be deficient. Alcoholism may
give rise to confabulation and short-term memory
impairment (Korsakoff’s psychosis) due to associated
thiamine deficiency or, more rarely, Wernicke’s
encephalopathy – acute confusion, ataxia, and
opthalmoplegia. Acute postoperative delirium is not
improved by large parenteral doses of the vitamin B
group of vitamins. Any associated low plasma thia-
mine concentration may be an epiphenomenon.
0014Pyridoxine (vitamin B
6
) and folate are important
cofactors for the metabolism of homocysteine, and
both vitamins independently lower raised homocys-
teine levels, thought to play a key role in atherogen-
esis. The Nurse Health Study found that a long-term
intake of 3 mg of vitamin B
6
and/or at least 400 mgof
folate per day have a favorable impact on CHD. In
the Framingham Study, 20% of elderly subjects had
folate and vitamin B
6
levels below the recommended
intake.
0015Folic acid in its conjugated form (predominantly
polyglutamate) is present in a wide variety of food,
especially green leafy vegetables, kidney, and liver.
Hydrolysis of the polyglutamate to monoglutamates
is necessary for absorption in the small intestine.
Folate deficiency may be due to several causes, with
inadequate intake the most common, often aggra-
vated by prolonged cooking, which destroys the
vitamin. Disease that impairs absorption (e.g., gluten
enteropathy or ileal resection) or increases metabolic
demand (e.g., vitamin B
12
deficiency, the leukemias,
myelofibrosis, hemolytic anemia, sideroblastic ane-
mia) may result in deficiency. A number of drugs (e.g.,
trimethoprim, methotrexate, triamterene) inhibit con-
version of folate to tetrahydrofolate, which is the main
storage and metabolically active form of the vitamin.
The anticonvulsants, phenytoin, primidone, and
phenobarbitone, and the antibiotic, nitrofurantoin,
may also result in folate deficiency, but the underlying
mechanism has not been firmly established. Defective
DNA synthesis through the purine and pyrimidine
pathways following chronic dietary folic acid defi-
ciency or drug-induced activity gives rise to a megalo-
blastic anemia. Provided that vitamin B
12
deficiency is
not present, treatment with as little as 200 mg daily of
oral folic acid is rapidly effective. In practice, pharma-
cological doses of 1–5 mg daily are used. Folinic acid
(Leukovorin), a form of tetrahydrofolate, is preferable
if the deficiency is due to folate antagonist drugs. The
COMA recommendation of 200 mg per day isadequate
2030 ELDERLY/Nutritional Management of Geriatric Patients

forred cell formationbut may notbeoptimal forhomo-
cysteine metabolism and vascular wall integrity.
0016 Dietary deficiency vitamin of B
12
is rare, except
in strict vegans. This is predominantly due to the
efficient recirculation of the vitamin and a reported
half-life of 480–1360 days. The predominant cause
vitamin B
12
deficiency is loss of intrinsic factor pro-
duction by the gastric parietal cells, most often due to
autoimmune disease giving rise to pernicious anemia.
Antibodies against parietal cells and less commonly
against intrinsic factor may be found in the gastric
juice or serum. The inability to separate vitamin B
12
from its dietary binding protein may also cause vita-
min B
12
deficiency; lack of gastric acid and pepsin
contribute, but an unequivocal explanation has yet to
be established. Bacterial overgrowth as in blind loop
syndrome competes for available vitamin B
12
and
reduces the amount available from absorption. Gas-
tric surgery by removing some or all intrinsic factor
producing cells leads eventually to a low serum
vitamin B
12
concentration.
0017 Because the liver stores large amounts of vitamin
B
12
, evidence of deficiency does not occur for about 5
years, even after total gastrectomy. Ileal disease or
surgery often gives rise to vitamin B
12
deficiency.
The gradual but progressive development of anemia
and the well-hemoglobinized red cells often results in
minimal symptoms until an advanced anemic state.
The common symptoms of anemia – fatigue, breath-
lessness, and poor exercise tolerance, occur. Acute
onset of heart failure and angina is not uncommon
because of associated CHD and responds well to
vitamin B
12
treatment. Much has been written on
the relationship of dementia to vitamin B
12
defi-
ciency. Although low serum vitamin B
12
concentra-
tions are not uncommon in demented elderly patients
living in the community, there is little evidence of any
improvement in cognitive function following B
12
dosage. When some improvement does occur, it can
better be ascribed to concurrent treatment of other
comorbid states and correction of impaired total diet-
ary intake and improvement of restricted functional
and social activities. However, some neuropsychiatric
states are improved by vitamin B
12
therapy. Neuro-
logical symptoms are relatively rare. Symmetrical
peripheral neuropathy usually involving the lower
limbs is associated with paraesthetic symptoms and
evidence of ataxia and posterior column involvement
leading to lower-limb weakness and spasticity.
0018 Reduced plasma vitamin B
12
concentration is an
early feature of deficiency, though initially, the blood
picture may be normal. Later, macrocytosis and
megaloblastic bone marrow changes are character-
istic, with low white blood counts and multisegmen-
ted polymorphs. When diagnosis is equivocal, the
Schilling test is justified. In the presence of anemia, it
is useful to measure the reticulocyte response to vita-
min B
12
administration, which reaches its peak on
the 4th or 5th day. Treatment of confirmed deficiency
with 1000 mcg of intramuscular vitamin B
12
daily for
2 weeks rapidly replenishes body stores. Subsequently,
lifetime intramuscular injections every 3 months is
a cost-effective treatment schedule. Absorption of
1–3% of an oral dose of 1 mg of vitamin B
12
daily
generally satisfies the daily requirement of 2–5 mg.
0019The latest recommended vitamin E requirement is
15 mg per day. Vitamin E deficiency may result from
fat malabsorption or defects in the gene for the
a-tocopherol transfer protein and may give rise to
the insidious onset of peripheral neuropathy. A
possible influence of vitamin E (and vitamin C and
b-carotene) on excess free radical formation has led
the media to speculate on an antiageing effect. Al-
though no benefit has been seen in patients with
Parkinson’s disease, a placebo-controlled trial of vita-
min E 2000 IU daily in people with Alzheimer’s
disease has suggested a possible slowing of the rate
of disease progression. The antiadhesive effect of
vitamin E combined with the platelet antiaggregatory
effect of aspirin increases the risk of bleeding, and
caution is appropriate with supplementary vitamin E
in a dose greater than 500 IU per day.
0020Insufficient iron intake is mainly found in house-
bound and institutionalized older people. Meat and
cereals are the major sources of iron in the diet; fruit
and vegetables have much lower proportions. Some
flour and cereals are fortified with additional iron.
Vitamin C enhances, and phytates or tannins in tea
interfere with, iron absorption. Early iron store
reduction is demonstrated by low serum ferritin
concentrations. As iron deficiency progresses, anemia
may develop. Moderate to severe iron-deficiency
anemia is mostly due to chronic gastrointestinal
bleeding due to drugs (e.g., aspirin, anticoagulants,
nonsteroidal antiinflammatory drugs) or disease.
Symptoms of iron deficiency may follow the onset
of anemia and include fatigue, shortness of breath
or exacerbation of concomitant ischemic arterial dis-
ease, e.g., angina, congestive heart failure, and inter-
mittent claudication. Treatment of iron deficiency is
usually with ferrous sulfate, 200 mg two to three
times daily until the hemoglobin and iron stores are
replaced. Concomitant administration of ascorbic
acid as fruit juice or as a 50-mg vitamin C tablet
increases absorption and reduces gastrointestinal
side-effects. In the presence of a malabsorption
state, iron may have to be given parenterally, but the
potential risk of anaphylactic response requires super-
vision. Dietary advice on foods rich in available iron
is an essential part of the long-term strategy, but for
ELDERLY/Nutritional Management of Geriatric Patients 2031

some elderly people, a small dose of oral iron may be
a permanent requirement.
Dietary Fiber
0021 Dietary fiber keeps bowel movements regular and
prevents constipation when taken with a good fluid
intake and adequate exercise. Long-term intake of
dietary fiber decreases the risk of CHD and diverticu-
lar disease and helps management of diabetes mellitus
and hyperlipidemia. Its role in the prevention of col-
orectal cancer is still under debate. Only a minority of
older people consume the recommended daily intake
of 25–35 g of dietary fiber. This may be achieved
by eating more fruit and vegetables (preferably
unpeeled) by substituting whole-grain breads and
cereals for white bread and sugary cereals and adding
wheat bran and beans to soups, stews, and other
dishes. Excess fiber intake should be avoided, as it
may impair the absorption of trace minerals.
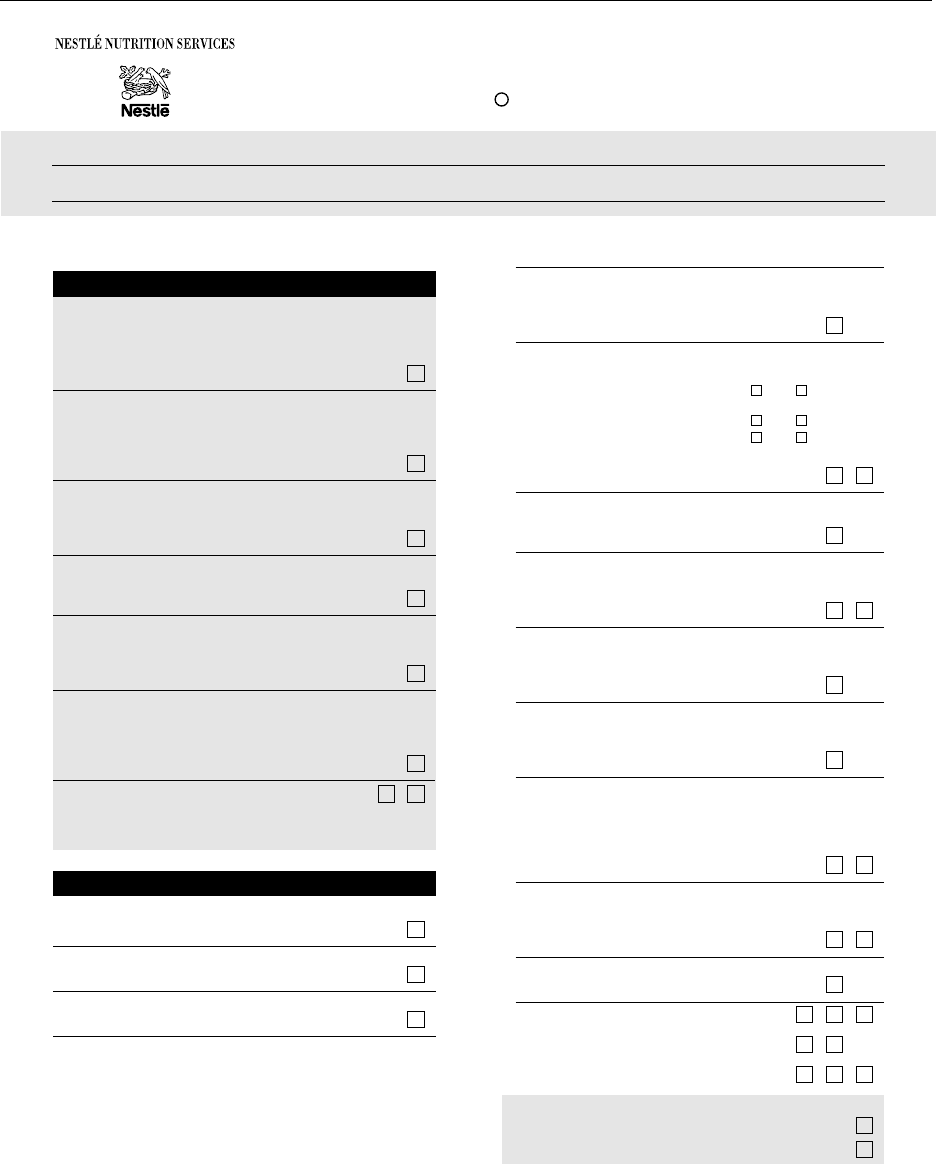
Clinical Evaluation
0022 Once clinical symptoms and signs appear, nutritional
impairment is firmly established. The Mini Nutri-
tional Assessment (MNA; Figure 1) can be under-
taken in 15 min and has been used successfully in
free-living older people, in residents of nursing
homes, and in hospital inpatients. A Danish 5-year
longitudinal study showed an increased mortality in
subjects with an MNA score of less than 23.5. Sub-
jects in a New Mexico Study with a high MNA score
of 27 or greater were classified as having very good
health.
0023 Weight is the traditional simple measure of nutri-
tional state and often goes unrecorded in medical and
nursing-home case notes. The body mass index (BMI)
(weight in kilograms/height, in meters, squared) is not
always feasible in disabled and bed-bound persons,
but the height can be calculated using the sitting knee
height (knee to floor or heel) or the demispan (sternal
notch to finger web in the outstretched arm). People
aged over 65 years are recommended to have a BMI
between 24 and 29. A BMI under 20 indicates under-
nutrition. Mortality rates increase in the very elderly
with low BMIs (under 20).
0024 Body fat distribution changes with age, and in both
sexes there is an increase in abdominal fat distribu-
tion and an increase of omental fat. In women, a
waist/hip ratio over 0.9 is associated with a threefold
risk of CHD when compared with a ratio of less than
0.7. Waist circumference is an independent risk
factor, and women with a waist circumference of
greater than 97 cm (38 inches) have a threefold risk
of CHD. Men with a waist circumference of greater
than 100 cm (40 inches) have a 2.5- to 4.5-fold
increase in one or more cardiovascular risks. Gall
bladder disease, cancer, and osteoarthritis are more
common in the overweight, and obesity, particularly
abdominal obesity, is a significant independent risk
factor for insulin resistance and type 2 diabetes.
0025In older underweight persons, the cornerstone of
management is to identify and treat aggressively the
cause of weight loss. Poor appetite may improve with
treatment of depression or review of drugs, such
as digoxin, dopaminergic agents, and anticholines-
terases. Treatment of poor oral hygiene, swallowing
disorders, or malabsorption syndromes will increase
food intake and absorption. Good management of
systemic diseases such as cancer, chronic organ fail-
ure, infection, and inflammatory disorders, and rele-
vant metabolic diseases such as hyperthyroidism, all
require attention to the nutritional state. Attention to
social and economic factors and to countering phys-
ical disabilities may also be necessary. Highly restrict-
ive ‘medically indicated’ diets, for example, for
lowering cholesterol or managing diabetes, may also
lead to unintentional weight loss and nutritional
deficiencies, and a more relaxed, well-balanced, and
varied diet is likely to be preferable.
0026Intentional weight loss in obese older people may be
associated with functional and health benefits, though
some studies indicate that being overweight later in
life does not pose a significant health risk. Weight
reduction is a partnership between patient and med-
ical advisors. Without this approach, it is difficult to
maintain motivation and trust on the part of the pa-
tient. Randomized controlled studies firmly establish
that low-fat diets produce weight loss. A slowly pro-
gressive increase in exercise levels has only a small
impact on weight but has a more substantial benefit
on function and improves insulin sensitivity.
Nutritional Management in Specific
Medical Conditions
0027Pain and discomfort from inflammation of the gums,
mouth, or tongue and missing or illfitting dentures
will hinder adequate chewing and decrease food
intake. Preventive dental care (from an early age) is
the best management, and maintaining active dental
health policies is especially important for those in
institutions. When maintaining adequate nutrition
becomes a problem, high-protein–energy liquids and
soft nonacidic foods may be best tolerated, and a mild
topical local anesthetic mouthwash before meals may
help to relieve pain. Inadequate saliva production
arising from infection, anticholinergic drugs, radi-
ation therapy, or Sjogren’s syndrome will interfere
with taste and swallowing and may be partially
2032 ELDERLY/Nutritional Management of Geriatric Patients
relieved by spraying the mouth with artificial saliva
solution. Normal age-related changes in taste result in
older people being more sensitive to bitter and sour
flavors and less sensitive to sweet and salt. A declining
sense of smell means that food aromas that stimulate
the appetite must be several times stronger than usual.
0028Problems with swallowing (dysphagia) may be due
to inflammatory, traumatic (e.g., postintubation),
Complete the screen by filling in the boxes with the appropriate numbers.
Add the numbers for the screen. If score is 11 or less, continue with the assessment to gain a Malnutrition Indicator Score.
A Has food intake declined over the past 3 months due to loss of appetite,
digestive problems, chewing or swallowing difficulties?
0 = severe loss of appetite
1 = moderate loss of appetite
2 = no loss of appetite
B Weight loss during the last 3 months
0 = weight loss greater than 3 kg (6.6 lbs)
1 = does not know
2 = weight loss between 1 and 3 kg (2.2 and 6.6 lbs)
3 = no weight loss
C Mobility
0 = bed or chair bound
1 = able to get out of bed/chair but does not go out
2 = goes out
D Has suffered psychological stress or acute disease
in the past 3 months
0 = yes 2 = no
E Neuropsychological problems
0 = severe dementia or depression
1 = mild dementia
2 = no psychological problems
F Body Mass Index (BMI) (weight in kg) / (height in m)
2
0 = BMI less than 19
1 = BMI 19 to less than 21
2 = BMI 21 to less than 23
3 = BMI 23 or greater
J How many full meals does the patient eat daily?
0 = 1 meal
1 = 2 meals
2 = 3 meals
K Selected consumption markers for protein intake
At least one serving of dairy products
(milk, cheese, yogurt) per day?
yes no
Two or more servings of legumes
or eggs per week?
yes no
•
•
•
Meat, fish or poultry every day
yes no
0.0 = if 0 or 1 yes
0.5 = if 2 yes
1.0 = if 3 yes .
L Consumes two or more servings
of fruits or vegetables per day?
0 = no 1 = yes
M How much fluid (water, juice, coffee, tea, milk…) is consumed per day?
0.0 = less than 3 cups
0.5 = 3 to 5 cups
1.0 = more than 5 cups .
N Mode of feeding
0 = unable to eat without assistance
1 = self-fed with some difficulty
2 = self-fed without any problem
O Self view of nutritional status
0 = views self as being malnourished
1 = is uncertain of nutritional state
2 = views self as having no nutritional problem
P In comparison with other people of the same age,
how does the patient consider his/her health status?
0.0 = not as good
0.5 = does not know
1.0 = as good
2.0 = better .
Q Mid-arm circumference (MAC) in cm
0.0 = MAC less than 21
0.5 = MAC 21 to 22
1.0 = MAC 22 or greater .
R Calf circumference (CC) in cm
0 = CC less than 31 1 = CC 31 or greater
Assessment (max. 16 points)
.
Screening score
Total Assessment
(max. 30 points)
.
Screening
Screening score (subtotal max. 14 points)
12 points or greater Normal – not at risk – no need to complete assessment
11 points or below Possible malnutrition – continue assessment
Malnutrition Indicator Score
17 to 23.5 points at risk of malnutrition
Less than 17 points malnourished
Assessment
G Lives independently (not in a nursing home or hospital)
0 = no 1 = yes
0 = yes 1 = no
Takes more than 3 prescription drugs per dayH
0 = yes 1 = no
Pressure sores or skin ulcersI
Ref.:
© Nestlé, 1994, Revision 1998. N67200 12/99 10M
Mini Nutritional Assessment
MNA
R
Last name:
First name: Sex: Date:
Age: Weight, kg: Height, cm: I.D. Number:
Guigoz Y, Vellas B and Garry PJ. 1994. Mini Nutritional Assessment: A practical assessment tool
for grading the nutritional state of elderly patients. Facts and Research in Gerontology. Supplement
#2:15-59.
Rubenstein LZ, Harker J, Guigoz Y and Vellas B. Comprehensive Geriatric Assessment (CGA) and
the MNA: An Overview of CGA, Nutritional Assessment, and Development of a Shortened Version
of the MNA. In: “Mini Nutritional Assessment (MNA):Research and Practice in the Elderly”. Vellas
B, Garry PJ and Guigoz Y, editors. Nestlé Nutrition Workshop Series. Clinical & Performance
Programme, vol.1. Karger, Bâle, in press.
fig0001 Figure 1 Mini Nutritional Assessment (MNA).
ELDERLY/Nutritional Management of Geriatric Patients 2033

and neoplastic causes in the mouth or esophagus,
mechanical or neuromuscular causes, or a pharyngeal
diverticulum. Management is primarily directed to
resolution of the causative factors, but there will be
an intervening period of a need for nutritional main-
tenance, or, where the underlying cause cannot be
treated, long-term nutritional support may be re-
quired. Stroke, motor neurone disease, and, less com-
monly, Parkinson’s disease may be associated with
severe swallowing problems. Following an acute
stroke, swallowing difficulties are generally transient
and resolve within a week. However, in 15% of pa-
tients, swallowing impairment with risk of aspiration
excludes oral nutrition. Dehydration leads to rapid
deterioration, and intravenous fluids are required
in the first few days. Three options are available
for nutritional maintenance until safe swallowing
returns. Parenteral nutrition is only practical for a
few days and has a very limited role in poststroke
management. Fine-bore nasogastric tube feeding is
commonly the interim measure for nutritional provi-
sion. In the first week or so, emphasis is on energy and
protein intake, but a balanced nutrient provision with
attention to micronutrients and mineral content
becomes essential for longer-term management. Per-
cutaneous endoscopic gastrostomy is well tolerated
and is the method of choice for long-term manage-
ment. The benefits of early PEG feeding have yet to be
established, but ongoing randomized trials should
provide evidence-based guidance.
0029 In motor neurone disease, the early stages of
dysphagia are managed by thickening all fluids and
liquidizing and adapting solid food to a thick custard
consistency. Unfortunately, food consumption can
easily take on an ‘eat to live’ meaning with the loss
of social and pleasurable aspects of eating.
0030 Alzheimer’s disease is the commonest cause of de-
mentia in later life. Weight loss is usual, sometimes
even early in the disease, and vitamin deficiencies and
disturbed eating behavior are common. Where the
cognitively impaired individual lives alone and has
difficulty in buying or preparing an adequate diet or
forgets meals, the cause of the weight loss is readily
apparent. In later stages, restlessness and agitation
may result in excessive energy expenditure, or aver-
sion to food may develop. Often, however, there is no
obvious cause of weight loss. Carers may be able to
provide accurate dietary information to enable moni-
toring of the patient’s nutritional status using the
MNA. There is current interest in the possible role of
inadequate intake of folate and raised homocysteine
in the etiology of cognitive impairment. However, it is
also likely that vitamin deficiencies may develop as a
result dementia. Antioxidant vitamins may have neu-
roprotective effects and, in the experimental animal,
can improve cognitive function. High-saturated-fat
diets are reported to be associated with an increased
likelihood of cognitive impairment, whereas polyun-
saturated fats have a negative influence. Tube feeding
of people with advanced dementia has no measurable
influence on survival and raises important practical
and ethical concerns.
0031Decline in glucose tolerance and type 2 diabetes
mellitus is increasingly common in old age. A raised
2-h postprandial glucose test is associated with in-
creased mortality. Dietary management has changed
considerably over recent years. From the early 1990s,
reducing dietary fat intake, particularly saturated fat,
has been recommended. Currently, a reduction in
saturated and trans-fats is advised, but no restriction
on monosaturated and polyunsaturated fats. Increas-
ing emphasis is also placed on replacing high-with
low-glycemic-index foods. A change in lifestyle is
important in both prevention and treatment, and it
is inappropriate to consider diabetes in isolation from
other risk factors. Hypertension affects at least 50%
of older diabetics, and reduced sodium intake
enhances the overall management of high blood
pressure.
Undernutrition in Institutionalized
Patients
0032Many hospital patients and residents of long-term
care facilities cannot feed themselves, and many are
malnourished. Since the serving and checking of
meals have become a ‘nonnursing duty’ in the UK,
awareness of the patient’s nutrient intake may be
limited. Meals are often kept for some time in heated
wagons before serving, and some nutrients are largely
destroyed. Older people are more likely to eat food
provided when it is served warm, with portion size
individualized, and the eating environment is con-
sidered. In one study, in which plated meals were
weighed before and after serving, elderly patients
were shown often to have inadequate time or ability
to cut and eat their meals. When all food was cut up
into bite-sized pieces, food consumption improved
significantly. Food must also be placed within reach
of disabled patients. An uncluttered, well-lit dining
room with minimal distractions, providing consist-
ent seating at mealtimes and attractive table settings
will enhance eating. Attention to poor hearing en-
hances enjoyment of mealtime conversation. People
with physical disabilities may benefit from feeding
aids such as nonskid place mats, weighted cutlery
with thick handles, plates with wide, curved lips
that help keep food on the plate, and cups with
easy-grip handles and special lids for sipping. Cyclical
menus should be available, recognizing individual
2034 ELDERLY/Nutritional Management of Geriatric Patients

preferences and offering properly prepared and appe-
tizing meals. Dividing up the daily food ration into
lighter, more frequent snacks may be more acceptable
than the traditional three meals a day. Special events
such as picnics and family dinner parties and special
menus for festive occasions such as birthdays will
encourage an interest in eating. Patients requiring a
softer or liquid diet would benefit by having their
food presented creatively.
0033 Water is an important nutrient that is often over-
looked. Thirst lessens with age, so older people need
to adopt the habit of drinking fluids regularly, or
dehydration can occur easily. This is a particular
problem in the physically or mentally frail and the
institutionalized, who are especially susceptible to the
dehydrating effects of fever, vomiting, and diarrhea.
Undernutrition in People at Home
0034 The elderly person living alone is at especial risk of
malnutrition. Grief from the loss of a spouse or family
and friends, loneliness and depression, greater use
or abuse of alcohol, which may substitute for an
adequate food intake, lack of sufficient money for
food, and disability affecting shopping or preparation
of food may all contribute. Poor vision is also an
independent determinant of poor eating, leaving
people less confident in their ability to cook and less
able to get out for groceries. Support from relatives,
neighbors, and homecare assistants providing and
preparing food deserves recognition. Eating should
be a social event, and older people should be encour-
aged to eat with family and friends whenever
possible.
0035 Relevant community services for older people in-
clude meals on wheels, which provide hot meals up to
7 days per week to homebound people in their own
homes. However, arrangements are often inflexible,
and there is limited ability to conform to special diet-
ary needs. Frozen meals delivered weekly and which
can then be easily reheated in a microwave oven may
be a more appropriate and palatable alternative. Day
centers and luncheon clubs have a useful role in sup-
plementing the diet and reinforce the social aspects of
feeding. An emergency store of essential food items in
case of unexpected illness or bad weather is a useful
precautionary measure.
See also: Aging – Nutritional Aspects; Ascorbic Acid:
Properties and Determination; Carotenoids: Occurrence,
Properties, and Determination; Cholecalciferol:
Properties and Determination; Cobalamins: Properties
and Determination; Dietary Reference Values; Dietary
Requirements of Adults; Elderly: Nutritional Status;
Nutritionally Related Problems; Energy: Intake and
Energy Requirements; Folic Acid: Properties and
Determination; Iron: Properties and Determination;
Malnutrition: The Problem of Malnutrition; Minerals –
Dietary Importance; Protein: Requirements
Further Reading
Cummings JH and Bingham SA (1998) Diet and the
prevention of cancer. British Medical Journal 317:
1636–1640.
Department of Health (1992) The Nutrition of Elderly
People. Great Britain Committee on Medical Aspects
of Food Policy Working Group on the Nutrition of
Elderly People. Report on Health and Social Subjects.
No. 43. London: Stationery Office.
Ebrahim S and Davey-Smith G (1996) Health Promotion
in Old People for the Prevention of Coronary Heart
Disease and Stroke. Health Promotion Effectiveness
Reviews. London: Health Education Authority.
Fiatarone MA, O’Neill EF, Ryan ND et al. (1994) Exercise
training and nutritional supplements for physical frailty
in very elderly people. New England Journal of Medicine
330: 1769–1775.
Finch S, Doyle W, Lowe C et al. (1998) National Diet and
Nutrition Survey: People Aged 65 years and Older.
Volume 1: Report of the Diet and Nutrition Survey.
London: Stationery Office.
Fletcher A and Rake C (1998) Effectiveness of Interven-
tions to Promote Healthy Eating in Elderly People
Living in the Community: A Review. Health Promotion
Effectiveness Reviews No. 8. London: Health Education
Authority.
Gariballa SE and Sinclair AJ (1997) Diagnosing under-
nutrition in elderly people. Reviews in Clinical Geron-
tology 7: 367–371.
Horwitz A, MacFadyen DM, Munro H, Scrimshaw NS,
Steen B and Williams TF (1989) Nutrition in the Elderly.
Oxford: Oxford University Press.
Lilley J and Hunt P (1998) Opportunities for and Barriers
to Managing in Dietary Behaviour in Elderly People.
London: Health Education Authority.
Lipschitz DA (1995) Approaches to the nutritional support
of elderly patients. Clinics in Geriatric Medicine 11:
715–724.
McGee M and Jensen GL (2000) Nutrition in the elderly.
Journal of Clinical Gastroenterology 30: 372–380.
Roe L, Hunt P, Bradshaw H and Rayner M (1997) Review
of the Effectiveness of Health Promotion Interventions
to Promote Healthy Eating. London: Health Education
Authority.
Seiler WO and Stahelin HB (eds) (1999) Malnutrition in the
Elderly. Berlin: Springer-Verlag.
Vellas BJ, Garry PJ and Guigoz Y (eds) (1999) Research and
Practice in the Elderly (Nestle
´
Nutrition Workshop
Series. Clinical and Performance Programme, vol. 1.
Basel: Karger.
Walls AW, Steele JG, Sheiham A, Marcenes W and Moyni-
han PJ (2000) Oral health and nutrition in older people.
Journal of Public Health Dentistry 60: 304–307.
ELDERLY/Nutritional Management of Geriatric Patients 2035
Electrical Supplies See Power Supplies: Use of Electricity in Food Technology
ELECTROLYTES
Contents
Analysis
Water–Electrolyte Balance
Acid–Base Balance
Analysis
G R Ahmad, California State University,
San Bernardino, CA, USA
D R Ahmad, University of California, Riverside, CA,
USA
This article is reproduced from Encyclopaedia of Food Science,
Food Technology and Nutrition, Copyright 1993, Academic Press.
Electrolytes and their Significance
0001 Electrovalent solids exist as crystal lattices composed
of ions bound together by a strong electrostatic force of
attraction between positive and negative charges. The
solutions of such substances in water conduct electri-
city and are therefore called electrolytes. Electrolytes
are classified as anions or cations, depending upon
their direction of movement in an electric field. If an
electrolyte bears a positive charge, it will migrate to the
cathode (negative pole) and is called a cation. Sodium
and potassium are common examples of cations. If the
electrolyte bears a negative charge, it will migrate to
the anode (positive pole) and is called an anion. Chlor-
ide and bicarbonate are examples of anions.
0002 In body fluids, the major electrolytes exist as free
ions, while the trace metals primarily occur in com-
bination with proteins. The electrolytes play very
important roles in the physiology of living organisms.
In the human body, virtually every metabolic process
is dependent on, or is affected by, electrolytes. Elec-
trolytes are involved in the maintenance of the body’s
osmotic pressure, water distribution in the various
body fluid compartments, maintenance of proper
pH, involvement in oxidation – reduction reactions,
acting as cofactors for enzymes, and regulation
of neuromuscular irritability or excitability. Thus,
abnormal levels of electrolytes could be the cause
or consequence of a variety of physiological dis-
orders, which make the determination of eletrolytes
one of the most important functions of clinical la-
boratories. (See Coenzymes; pH – Principles and
Measurement.)
0003The major electrolytes found in the body are
sodium (Na
þ
), potassium (K
þ
), calcium (Ca
2þ
), mag-
nesium (Mg
2þ
), chloride (Cl
), bicarbonate (HCO
3
),
phosphate (HPO
4
2
), and sulfate (SO
4
2
). In clinical
laboratories, the most common electrolytes requested
in a medical diagnosis are commonly referred to as
the ‘electrolyte profile.’ This panel includes four elec-
trolytes: HCO
3
,Cl
,Na
þ
and K
þ
.(See Calcium:
Physiology; Magnesium; Potassium: Physiology;
Sodium: Physiology.)
Specimens Required for Electrolyte
Analysis
0004Electrolytes can be assayed from many body
fluids, including serum, heparinized plasma, whole
blood, vitreous humor, sweat, urine, gastrointestinal
fluid, and aqueous extract from feces. In clinical la-
boratories, serum and urine are the body fluids from
which electrolyte analyses are most frequently per-
formed. These fluids are easily obtained from the pa-
tient, and the reference levels (normal) for these fluids
are available. When the electrolyte level of body fluid
is required, serum is considered the most practical
specimen. When electrolytes are to be determined
from urine, a timed collection is the preferred method.
Timed-collection specimens are needed to allow a
comparison of values with reference ranges or for the
determination of rates of electrolytes lost from the
body. These specimens can be stored at 2–4
C or can
be frozen for delayed analysis. The average serum
levels of common electrolytes are as follows:
.
0005bicarbonate (expressed as total carbon dioxide),
22–31 mmol l
1
;
.
0006chloride, 98–106 mmol l
1
;
2036 ELECTROLYTES/Analysis
