Caballero B. (ed.) Encyclopaedia of Food Science, Food Technology and Nutrition. Ten-Volume Set
Подождите немного. Документ загружается.

The copper intake of nurses was roughly estimated at
between 5.3 and 32 mg copper, and the dose of 5.3 mg
copper day
1
has been adopted by some authorities
as the ‘lowest observed no-effect level’. Other author-
ities have suggested 0.21–0.5 mg kg
1
,orupto30mg
of copper in a 60-kg person, as the maximum toler-
able daily total intake for copper. Proposals for the
maximal allowable amount of copper in drinking
water are in the range of 1–2mg l
1
, but based on
copper poisoning in children, the safe amount for
children may be as low as 0.2 mg l
1
. This wide
range of estimates is attributed to insufficient data,
lack of understanding by toxicologists and regulatory
authorities that copper is an essential nutrient, lack of
awareness that humans are exposed to copper from
both foods and beverages, and concern about copper
toxicosis syndromes such as childhood cirrhosis.
Regulations for copper intakes and copper in drink-
ing water are summarized in Table 7.
0033 Indian childhood cirrhosis was a common killer
until the early 1990s when it became preventable
and treatable. The disease generally occurs between
the ages of 6 months and 5 years, and is characterized
by increased hepatic, urinary, and serum copper
concentrations. Symptoms include nonspecific com-
plaints such as abdominal distension, irregular fever,
excessive crying, and altered appetite. Jaundice is
usually a late feature. If left untreated, the illness
progresses rapidly within a few months and is associ-
ated with liver failure and possibly death. The source
of the dietary copper appears to be milk boiled in
copper or brass (an alloy with about 70% copper
and 30% zinc) vessels that have been used extensively
in India, particularly by traditional Hindu families.
Some investigators also believe that a genetic disorder
enhances susceptibility to this toxicity syndrome
associated with excessive dietary exposure to copper.
Public health campaigns in India designed to discon-
tinue the use of copper-containing vessels markedly
reduced the incidence of this disease.
0034Contamination of drinking from copper plumbing
has emerged as a public health concern. Copper-
associated liver diseases in infants and children, simi-
lar to the condition seen in India, have now appeared
in parts of Europe. The source of copper appears to
be drinking water. Treatment for this liver disease
involved d-pencillamine (a copper chelator) and in
a few cases a liver transplant was conducted. In an
investigation in Wisconsin (USA), one water system
involved had an alkaline pH of 7.2–7.4 that would
not be expected to be corrosive. However, phosphate
was added to sequester iron, and this may have pre-
vented calcium and magensium from depositing on
the inner surface of the copper pipes and providing
a protective coating. Thus, copper was more easily
leached into the water from the pipes. Homes built or
remodeled within the past 10 years had the highest
concentrations of copper in the water. In a second
location, symptoms began after installation of new
copper pipes in a mobile-home park and the water
was naturally corrosive and very low in mineral con-
tent. In both areas, the symptoms were nausea, diar-
rhea, abdominal cramps, and headaches. The copper
concentration of the water associated with toxicity
was up to 3.6 mg l
1
. Flushing the faucet for 1 min
decreased the copper content to below 0.25 mg l
1
.
The authors suggested that owners of homes with
new copper pipes should be informed about the risks
of copper-contaminated drinking water and have their
water tested. They also recommended that copper
intoxication be included in the differential diagnosis
for those presenting with chronic or intermittent
tbl0007 Table 7 Regulations regarding total intakes of copper and copper content of drinking water
Agency Upper limit Rationale
Water content
World Health Organization (WHO) 2.0 mg l
1
Attempt to keep contribution of water to no more than 10% of total
copper intake
European Commission (EC) None Suggested guide of 0.1 mg l
1
at water treatment plant, and 3 mg l
1
after water has stood in pipes for 12 h
US Environmental Protection Agency (EPA) 1.3 mg l
1
Based on a ‘lowest observed adverse-effect level’ of 5.3 mg in
humans (nurses, study), consumption of 2 l water daily, and
addition of safety factors
1.0 mg l
1
Nonenforcible concentration of 1 mg l
1
based on taste
considerations
Total intake
Food and Agricultural Organization/World
Health Organization (FAO)/WHO)
0.5 mg kg
1
Based on no-observed-effect level of 5 mg kg
1
in dogs
US National Academy of Science 10 mg day
1
European Commission 10 mg day
1
Risk of nausea and vomiting increases when this dose is exceeded
Reproduced from Johnson MA (1998) Copper: physiology, dietary sources and requirements. In: Encyclopedia of Human Nutrition. Academic Press, with
permission.
1646 COPPER/Physiology

gastrointestinal upsets, particularly when these symp-
toms can be linked with a change in the water supply.
Infants may be particularly sensitive to high intakes of
copper and some investigators have recommended
that drinking water contain no more than 0.2 mg l
1
.
See also: Copper: Properties and Determination; Dietary
Reference Values
Further Reading
Failla ML, Johnson MA and Prohaska JR (2001) Copper.
In: Bowman BA and Russell RM (eds) Present Know-
ledge in Nutrition, 8th edn., pp. 373–383. Washington,
DC: ILSI Press.
Food and Nutrition Board (2001) Copper. In: Dietary Ref-
erence Intakes for Vitamin A, Vitamin K, Arsenic,
Boron, Chromium, Copper, Iodine, Iron, Manganese,
Molybdenum, Nickel, Silicon, Vanadium, and Zinc,
pp. 224–257. National Academy of Sciences. Washing-
ton DC: National Academy Press.
Hardorn H-B (1999) Copper-associated liver diseases in
children. Introduction. European Journal of Medical
Research 4: 212–213.
Harris ZL and Gitlin JD (1996) Genetic and molecular
basis for copper toxicity. American Journal of Clinical
Nutrition 63: 836S–841S.
Harris ED (1997) Copper. Chapter 8. In: O’Dell BL and
Sunde RA (eds) Handbook of Nutritionally Essential
Mineral Elements. pp. 231–273. New York: Marcel
Dekker.
Johnson MA (1998) Copper: physiology, dietary sources
and requirements. In: Encylopedia of Human Nutrition,
pp. 442–450. London: Academic Press.
Johnson MA, Smith MM and Edmonds J (1998) Copper,
iron, zinc and manganese in dietary supplements, infant
formulas, and ready-to-eat breakfast cereals. American
Journal of Clinical Nutrition 67: 1035S–1042S.
Lo
¨
nnerdal B (1998) Copper nutrition during infancy and
childhood. American Journal of Clinical Nutrition 67
(suppl.): 1046S–1053S.
Olivares M and Uauy R (1996) Limits of metabolic
tolerance to copper and biological basis for present
recommendations and regulations. American Journal of
Clinical Nutrition 63: 846S–852S.
Pandit A and Ghave S (1996) Present interpretation of the
role of copper in Indian childhood cirrhosis. American
Journal of Clinical Nutrition 63: 830S–835S.
Scheinberg IH and Sternlieb I (1996) Wilson disease and
idiopathic copper toxicosis. American Journal of Clin-
ical Nutrition 63: 842S–845S.
Turnlund JR (1999) Copper. Chapter 12. In: Shils ME,
Olson JA, Shike M and Ross AC (eds) Modern Nutrition
in Health and Disease, 9th edn, pp. 241–252. Baltimore,
MD: Williams & Wilkins.
CORONARY HEART DISEASE
Contents
Etiology and Risk Factor
Antioxidant Status
Intervention Studies
Prevention
Etiology and Risk Factor
F G Huffman, S Koutoubi and S Nath, Florida
International University, Miami, FL, USA
Copyright 2003, Elsevier Science Ltd. All Rights Reserved.
Background
0001 Our understanding of the biology and pathophysiol-
ogy of cardiovascular medicine and pathogenesis of
coronary heart disease (CHD), a multifactorial dis-
ease with a complex pathophysiology, continues to
expand as new horizons in epidemiological, experi-
mental, clinical, and genetic research are required.
Even so, CHD remains the leading cause of death,
accounting for more than 7 million of all cases of
mortality, and is responsible for chronic disability
and much of the healthcare costs worldwide. The
World Health Organization predicts that CHD will
prevail as the primary cause of morbidity and mortal-
ity worldwide until the year 2020.
0002No single risk factor consummates the ‘cause
and effect’ relationship. That the presence of any
one isolated risk factor cannot predict which individ-
ual will develop CHD. To date, data from myriad
CORONARY HEART DISEASE/Etiology and Risk Factor 1647

research have documented several hundred risk
factors that are statistically associated with the devel-
opment of CHD. Experts in cardiovascular research
often agree to classify these etiological factors as
major and minor risk factors or modifiable and non-
modifiable risk factors (Table 1). The majority of the
CHD epidemic in developed countries are associated
with the presence of smoking, high blood pressure,
high blood cholesterol, and impaired glucose toler-
ance. Most often, these common risk factors tend to
cluster in individuals who eventually develop CHD
events.
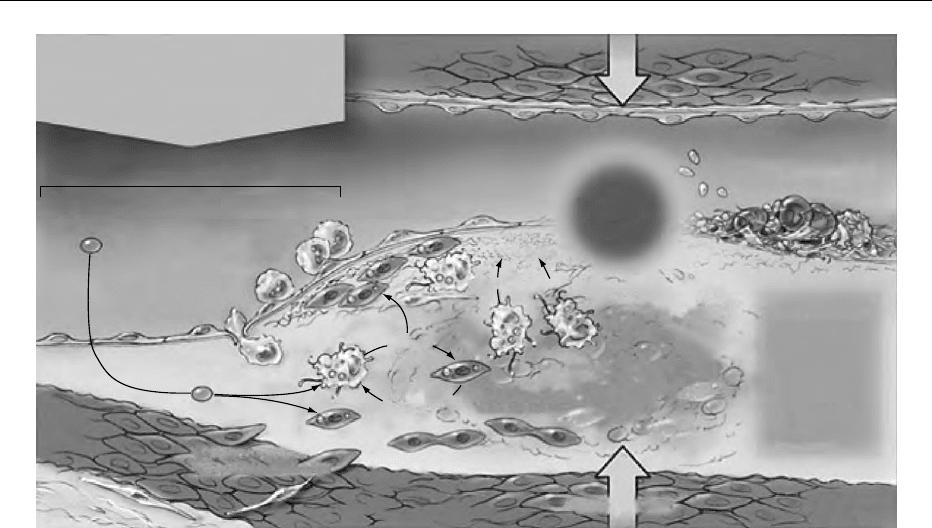
0003 Atherosclerosis, hardening of the arterial wall,
commences in childhood and, after decade-long cellu-
lar, molecular, and biochemical changes, culminates in
a heart attack, a well-known indication of CHD. In
1973, the ‘response-to-injury’ hypothesis of athero-
sclerosis was first outlined, underlining that the ath-
erosclerosis results from an arterial response to
chronic injury. Commonly chronic endothelial cell
injury is initiated by tobacco toxins (smoking), high
blood pressure, diabetes, oxidized low-density-lipo-
protein (LDL) cholesterol, as well as free radicals
resulting from oxidation of homocysteine (Hcy), and
infection (e.g., chlamydia). In response to an injury to
endothelial cells, there is a downregulation of protect-
ive mechanisms and upregulation of several factors
leading to atherosclerosis. For example, at the site of
endothelial injury, there is downregulation of the
potent endogenous vasodilator nitric oxide (NO),
tissue plasminogen activator (tPA), and prostacycline,
leading to a hyperprothrombic environment charac-
terized by upregulation of platelet aggregation and
leukocyte adhesion. At the initial stage, circulating
monocytes are attracted to the vascular intima, the
battleground of the atherosclerotic process. It is
worth mentioning that vascular cell adhesion mol-
ecule, usually expressed on the surface of endothelial
cells due to an inflammatory process, always precedes
the binding of monocytes. Monocytes then squeeze
through the tight junctions of the endothelial cells,
enter the subendothelial layer of the intima and are
transformed to phagocytic state macrophage. Macro-
phages engulf oxidized LDL cholesterol and form the
foam cells, the integral part of the ‘fatty streak.’ At one
stage, smooth muscles cells from the tunica media
migrate to the intima and release an extracellular
matrix. Monocytes, lymphocytes, platelets, endothe-
lial cells, and smooth muscle cells liberate numerous
factors, such as platelet-derived growth factors (a, b),
fibroblast growth factor, insulin-like growth factor-1,
interleukins (IL)-1, -2, -6, and -8, tissue necrosis factor
(TNF), which influence further cellular migration and
proliferation. The size of the fatty streak increases
with the accumulation of different types of cells and
lipids. Eventually, calcium is deposited and forms an
atherosclerotic plaque (Figures 1 and 2).
0004The following subsections detail each risk factor as
it relates to CHD.
Age, Gender, and Menopausal Status
0005The absolute risk of CHD increases with age, as there
is a progressive accumulation of coronary athero-
sclerosis with aging. Coronary heart disease is most
common after the age of 65 years, irrespective of
gender. Men however have a greater risk of CHD
than women; with men developing atherosclerotic
lesions 20 years earlier than women. Behavioral and
physiological differences between men and women
such as prolonged exposure to smoking, dislipidemia
and hormonal differences may partly explain the
gender difference. Among premenopausal women,
CHD is rare (except among smokers and oral contra-
ceptive users). However, the CHD risk is precipitous
among postmenopausal women, approaching that
for men.
Family History
0006Based on genetic data, twin studies, and phenotypes
(measurable traits) linked by inheritance, a positive
family history of CHD is one of the most potent
etiological influences on CHD independent of other
major risk factors such as smoking, high blood
tbl0001 Table 1 Etiology of coronary heart disease (CHD)
Nonmodifiable risk factors
Age and gender (men 45 years; women 55 years)
Family history of premature CHD (CHD in male first-degree
relative <55 years; CHD in female first-degree relative <65
years)
Modifiable risk factors
Cigarette smoking
Atherogenic diet
Physical inactivity
High blood pressure (140/90 mmHg)
Obesity
Diabetes mellitus
High blood total cholesterol (200 mg dl
1
)
High blood low-density lipoprotein cholesterol (130 mg dl
1
)
Low blood high-density lipoprotein cholesterol (< 40 mg dl
1
)
High blood triglycerides (150 mg dl
1
)
Thrombogenic factors
Inflammation or infection
Cytomegalovirus
Chlamydia pneumoniae
Helicobacter pylori
Herpes simplex
C-reactive protein
Serum amyloid A protein
Others
High blood homocysteine
Angiotensin II
1648 CORONARY HEART DISEASE/Etiology and Risk Factor
pressure, diabetes, and high LDL cholesterol. For
example, a single gene mutation (genetic variation)
in lipid metabolism is well documented in the devel-
opment of CHD. Plasma lipoprotein(a), Lp(a), is a
new risk factor for CHD. In normal population, the
variability of the apo(a) gene accounts for 90% of the
variability of plasma Lp(a). African Americans have a
higher levels of Lp(a) than white Americans. French
Canadians also have a higher level than expected due
to relative genetic homogeneity, also known as
‘founder effects.’ Familial combined hyperlipidemia,
another well-known lipid disorder, may cause CHD
before the age of 60 years, with a prevalence of about
2%.
0007 The risk of CHD increases in an individual with a
history of CHD in a first-degree relative (parent,
brother, sister, son, or daughter). The family history
is considered positive if clinical CHD or sudden
death can be documented in first-degree male rela-
tives before the age of 55 or in first-degree female
relatives before the age of 65.
Smoking
0008 Cigarette smoking is one of the most important risk
factors for the development and progression of CHD.
It has been estimated that smoking is responsible for
about 30% of CHD-related deaths. Coronary heart
disease events and deaths are attributable to cigarette
smoking in both a dose- and duration-dependent
fashion. Coronary heart disease risk is two to four
times higher in smokers than in non-smokers. Inhaled
cigarette smoke contains thousands of substances,
many of which are toxic to cells. For example, the
extensively studied chemical nicotine appears to
be involved in endothelial cell death, diminished
endothelial cell mitosis rate, and inhibition of NO
synthesis. Detrimental effects of smoking on the car-
diovascular system include an acute increase in vas-
cular resistance and blood pressure, impaired oxygen
transport, constriction of coronary vessel walls, ac-
celeration of LDL cholesterol oxidation, decreased
HDL cholesterol, increased platelet aggregation, and
increased fibrinogen production. Smoking also acts
synergistically with other etiological factors for
CHD, thereby substantially increasing the risk. Pas-
sive smoking or environmental exposure also carries a
substantial risk in the development of CHD. Like
first-hand smoke, environmental smoke contains
many toxins, such as carbon monoxide, benzopyrene,
and hundreds of other chemicals. Many of these
substances are toxic to arterial walls and may cause
endothelial dysfunction and substantially reduce
coronary microcirculation, an early process of
atherosclerosis.
Diabetes mellitus
Tobacco use by-products
Interventional therapies
Infections
Hypercholesterolemia
Homocysteine-derived
free radicals
Other free radicals
Chronic endothelial injury
Increased LDL
permeability
Lumon
Intima
Oxidized
LDL uptake
Media
Adverbha
Smooth muscle cell
and fibroblast migration
Enhanced monocyte
adhesion and
migration
Fibrous cap
formation
Matrix
degradation
Metalloprotease
Atherosclerotic
plaque
Vasoconstriction C.Lynm
Local increase in:
Thromboxane A
2
Serotonin
ADP
Thrombin
PAF
Free radicals
Tissue factor
Endothelin
Extracellular lipid core
and
Cellular debris formation
Platelet aggregation
and
Thrombus development
Form cell
Growth
factors
Chromatactic
factors
Smooth muscle
cell proliferation
Ulceration
or
fissure
Decreased endothelial
production of
NO, tPA, PGI
2
fig0001 Figure 1 (see color plate 39) Mechanisms in the initiation and progression of atherosclerosis. Endothelial injury results from a
variety of factors such as smoking, high blood cholesterol and homocysteine, and ulceration of atherosclerotic plaques, etc. (see text).
At the site of endothelial injury, there is a downregulation of endothelial-derived nitric oxide (NO), tissue plasminogen activator (tPA),
and prostacyclin (PGl
2
) with increased adhesion of platelets and leukocytes, increased permeability to lipoproteins, and vasoconstric-
tion. ADP, adenosine diphosphate; LDL, low-density lipoprotein; PAF, platelet activating factor. From Lefkowitz RJ and Willerson JT
(2001) Prospects for cardiovascular research. Journal of the American Medical Association 285: 581–587 with permission.
CORONARY HEART DISEASE/Etiology and Risk Factor 1649
Psychosocial Risk Factors
0009 There is mounting evidence that exposure to environ-
mental stressors and psychological reactions to stress,
an individual’s personality prototype (type A), lack of
social support, depression, and low socioeconomic
condition are associated with increased CHD risk.
Type A behavior is of special interest since it is associ-
ated with a two- to threefold higher risk for acute
myocardial infarction, as documented by substantial
prospective and case-control studies. A comprehen-
sive explanation of the effects of psychosocial factors
on CHD risk factors (e.g., high blood pressure) has not
yet been established. Psychosocial factors may act in
different ways. For example, they may be related to
risky behaviors or lifestyle factors such as smoking,
poor diet, physical inactivity, or excessive alcohol con-
sumption, which in turn influence the development of
CHD. However, the essential role of the psychosocial
factors in developing CHD event is mediated by a
neuroendocrine mechanism that alters catecholamine
levels. Excessive adrenergic (sympathetic) activity
may cause platelet aggregation, leading to occlusive
arterial thrombus formation. It is also hypothesized
that psychosocial stress may also increase circulating
IL-6, which in turn acts on the hypothalamic–pituit-
ary–adrenal axis, releasing many hormones that even-
tually result in abdominal obesity, insulin resistance,
and various lipid disorders, the risk factors for CHD.
Atherogenic Diet
0010Many decades of research have established that diet
plays a key role in atherosclerosis and subsequent
events such as myocardial infarction. The rates
of CHD are strongly associated with atherogenic
diets, which influence other biological factors such
as high blood pressure, LDL cholesterol, HDL chol-
esterol, thrombogenic factors, and obesity. The diet
also affects CHD in other ways: high-calorie, high-
saturated-fat (especially 12–16 carbon atoms) diets,
combined with physical inactivity or a sedentary life-
style, may lead to obesity, diabetes, and high blood
pressure. Experimental models have proved that diet-
ary saturated fat may cause atherosclerotic changes
even in the absence of other classical etiological
Nomenclature and
main histology
Main
growth
mechanism
Growth
mainly
by lipid
accumu-
lation
Accelerated
smooth
muscle
and
collagen
increase
Thrombosis,
hematoma
Earliest
onset
From
first
decade
From
third
decade
From
fourth
decade
Clinical
corre-
lation
Clinically
silent
Clinically
silent
or
overt
Sequences in progression
Type I (initial) lesion
isolated macrophage
foam cells
Type II (fatty streak) lesion
mainly intracellular
lipid accumulation
Type III (intermediate) lesion
Type II changes and small
extracellular lipid pools
Type IV (atheroma) lesion
Type II changes and core
extracellular lipid
Type V (fibroatheroma) lesion
lipid core and fibrotic layer,
or multiple lipid cores and fibrotic
layers, or mainly calcific,
or mainly fibrotic
Type VI (complicated) lesion
surface defect,
hematoma-hemorrhage,
thrombus
I
II
III
IV
V
VI
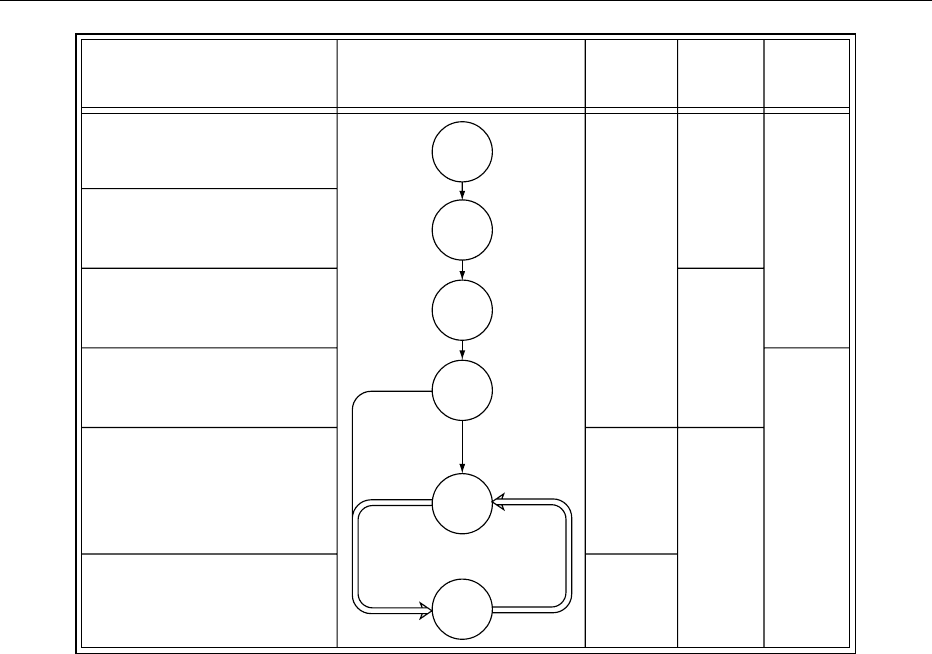
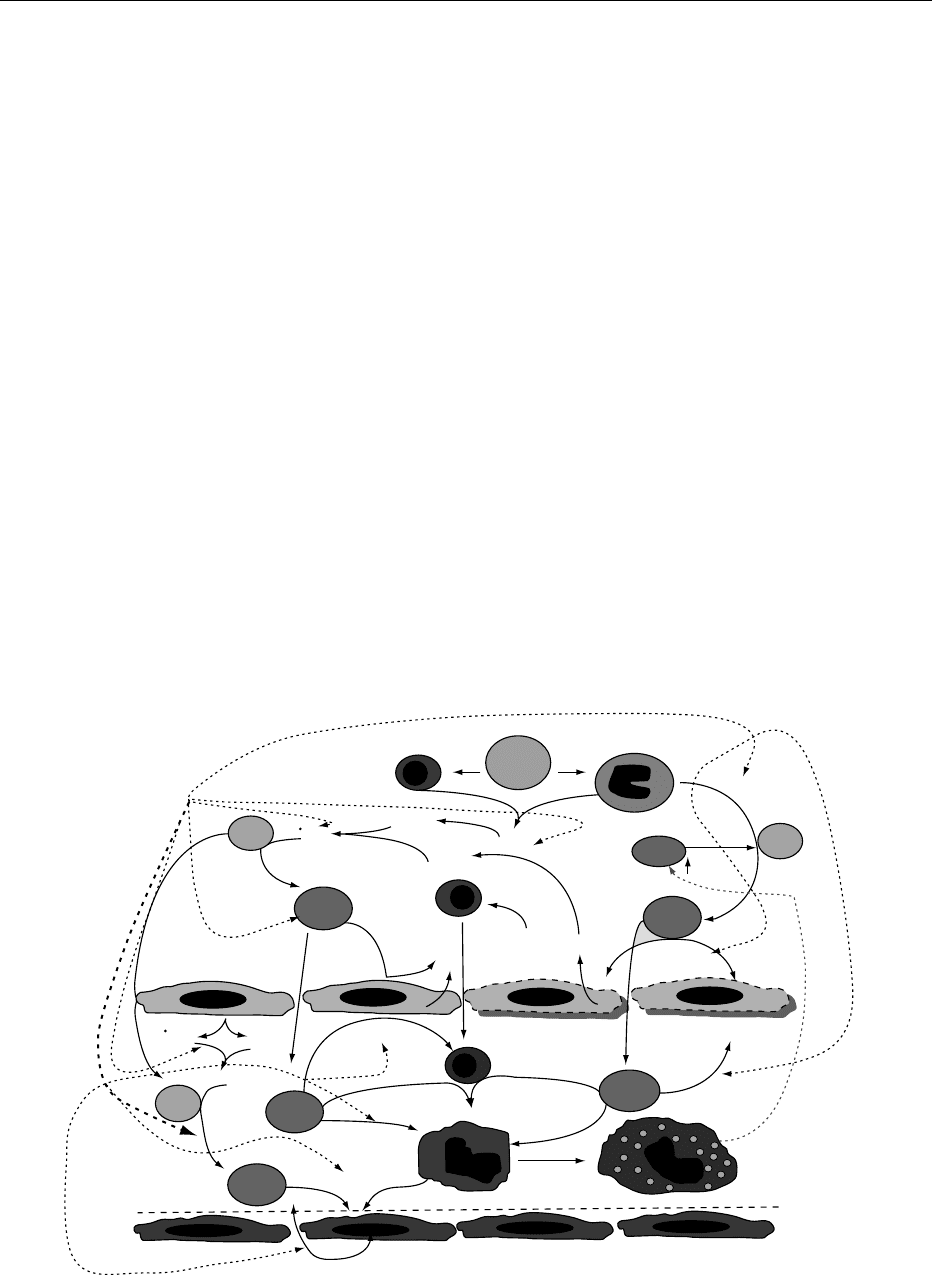
fig0002 Figure 2 Flow diagram of the progression of atherogenesis. Roman numerals indicate histological characteristics of lesions. Loop I
to loop IV illustrates the morphological changes in the lesion due to lipid accumulation. The loop between V and VI illustrates how
lesions increase in thickness when thrombotic deposits form on their surface. From Stary HC et al. (1995) A definition of advanced
types of atherosclerotic lesions and a histological classification of atherosclerosis. Arteriosclerosis, Thrombosis, and Vascular Biology
15: 1512–1531 with permission.
1650 CORONARY HEART DISEASE/Etiology and Risk Factor

factors for CHD. In contrast, substitution of saturated
fat with isocaloric unsaturated fatty acids and com-
plex carbohydrates, especially soluble fiber, lowers
LDL cholesterol. Partial hydrogenation of polyunsat-
urated fatty acids (e.g., margarine) increases LDL
cholesterol. Dietary cholesterol has a small effect on
elevating LDL cholesterol. A diet high in protein can
substantially limit carbohydrate intakes. Proteins
from animal sources are generally higher in fat, satur-
ated fat, and cholesterol and are considered athero-
genic. Excessive salt intake is associated with high
blood pressure in susceptible persons. Dietary supple-
mentation of b-carotene (20 mg per day), a precursor
of vitamin A,mayincreasecardiovascularmortalityby
12–26%, especially among male smokers. Many epi-
demiological studies have shown a J- or U-shaped rela-
tionship between alcohol consumption and all-cause
mortality. Excessive alcohol consumption is associated
with increased CHD, possibly because of an increase in
blood pressure and cardiac arrhythmias. In contrast,
light to moderate alcohol consumption is cardiopro-
tective, since it increases HDL cholesterol and apoli-
poprotein A1, and has favorable effects on markers of
inflammation (e.g., C-reactive protein and IL-6).
Physical Inactivity
0011 Prospective epidemiological studies have shown that
both physical inactivity and a sedentary lifestyle are
independent etiological factors and predictive of in-
creased CHD risk. It is, however, difficult to quantify
the association between the amount of physical activ-
ity and CHD. Results from meta-analyses have con-
cluded that physical activity may lower the rate of
CHD events by 50%. The positive benefits of physical
activity on CHD outcomes may be partially mediated
by lowering high blood pressure, decreasing triglycer-
ides and LDL cholesterol, increasing HDL choles-
terol, and increasing insulin sensitivity by lowering
blood glucose levels.
High Blood Pressure
0012 Although high blood pressure or hypertension is de-
fined as a systolic blood pressure of 140 mmHg or
greater and a diastolic blood pressure of 90 mmHg
or greater, this definition is arbitrary. Several large-
scale epidemiological studies have consistently dem-
onstrated a positive, strong, continuous, graded, and
independent relationship between high blood pressure
and the etiology of CHD. The prevalence of high blood
pressure is approximately 50% in the persons aged 65
years or older in many countries. High blood pressure
promotes the atherogenesis process by several mech-
anisms: increased endothelin production, increased
leukocyte adherence, impaired endothelium-derived
relaxant factor production, increased endothelium-
derived contractile substances, and increased vascular
permeability to lipoproteins. It has been shown that in
essential hypertension, endothelial damage inhibits
NO production, and there is production of endothelin
a potent vasoconstrictor from the activated endothe-
lium. In addition, high blood pressure may also cause
structural remodeling of vascular walls (cell prolifer-
ation) and accumulation of smooth muscle cells in the
tunica intima, which in turn initiates a series of cas-
cades leading to atherogenesis.
Obesity
0013Obesity, particularly central or abdominal obesity, is
considered one of the prime etiological risk factors for
CHD, since the adverse effects of obesity on CHD
risk factors (blood pressure, lipid profiles, and glu-
cose tolerance) are numerous. Central obesity is de-
fined as a waist-to-hip ratio of > 102 cm in men and
> 88 cm in women. Among the several adverse effects
of obesity in mediating CHD, the most profound
effect is high blood pressure. It has been estimated
that more than 75% of high blood pressure is directly
attributed to obesity. It is well documented in medical
literature that blood pressure increases with weight
gain and decreases with weight loss. Another signifi-
cant negative effect of obesity is on lipid metabolism;
obesity increases triglycerides and LDL cholesterol,
and decreases HDL cholesterol. Although it is diffi-
cult to establish the exact contribution of obesity
to glucose intolerance or insulin resistance, the role
of excess body fat, particularly abdominal fat, is posi-
tively correlated with insulin resistance.
Diabetes Mellitus
0014Individuals with either type 1 (insulin-dependent dia-
betes mellitus) and type 2 (noninsulin-dependent
diabetes mellitus) are at higher risk for CHD than
nondiabetic individuals. Atherosclerosis is responsible
for more than 75% of all mortality among diabetics.
Silent myocardial ischemia commonly occurs in pa-
tients with diabetes. Data from longitudinal
epidemiological studies suggest that diabetes or hyper-
glycemia (random plasma glucose concentration
200 mg dl
1
or fasting plasma glucose concentration
125 mg dl
1
) is an independent and well-established
etiological factor for CHD. Diabetes, especially type 2
diabetes, is a strong CHD risk factor in women which
increases CHD-related mortality by 400%.
0015The relationship between diabetes and CHD risk is
complex, poorly understood, and yet to be elucidated.
Diabetes alters endothelial cell function by contrib-
uting several mechanisms such as smooth muscle cell
proliferation and extracellular matrix production, ele-
vation of endothelin and angiotensin II, enhance plate-
let adhesion, and decrease in tPA. All these changes
CORONARY HEART DISEASE/Etiology and Risk Factor 1651

result in the progression of atherosclerosis. In the case
of type 2 diabetes, the hyperinsulinemic state exerts
mitogenic effects on the smooth muscle cells, leading
to an alteration of endothelial structure. In addition,
in the pathogenesis of atherosclerosis process, hyper-
glycemia and other CHD risk factors such as smoking,
high blood pressure, hyperlipidemia, obesity, physical
inactivity, and insulin resistance are interrelated and
intertwined and continue to act independently in pa-
tients with diabetes. The majority of patients with
type 2 diabetes have insulin resistance, which indeed
predisposes then to CHD. There are other factors such
as abdominal obesity, elevated triglycerides and LDL
cholesterol, low HDL cholesterol, high blood pres-
sure, and alterations in coagulation mechanisms that
tend to cluster among type 2 diabetics, collectively
known as metabolic syndrome. Elevated plasminogen
activator inhibitor-1 (PAI-1) concentration, a novel
risk factor of CHD, is another potentially important
thrombogenic factor in this syndrome.
Blood Lipids
0016 The essential roles of blood cholesterol and triglycer-
ides in the etiology of CHD are well established. There
is a continuous and graded risk between total blood
cholesterol and CHD in population-based studies.
However, on an individual basis, total cholesterol
may be used as a risk factor in determining CHD. In
fact, most of the lipid-related risk is explained by the
LDL cholesterol levels, and the positive association
between high LDL cholesterol (160 mg dl
1
) and
the risk of CHD is applicable to individuals with or
without established CHD, in both men and women.
In epidemiological studies, LDL cholesterol increases
as total cholesterol increases. Low-density lipopro-
teins increase with age, weight gain, and atherogenic
diets. Genetic factors such as the heterozygous form of
familial hypercholesterolemia further increase LDL
cholesterol in the general population. The oxidized
form of LDL is the main culprit in atherogenesis.
Scavenging macrophages engulf oxidized LDL par-
ticles, resulting in the formation of lipid-laden foam
cells. Subsequently, in combination with smooth
muscle proliferation, the lipid-laden foam cells are
transformed to a fatty streak, as mentioned earlier.
Oxidized LDL cholesterol also inhibits relaxation
factors and promotes contraction factors leading to
modification of vascular tone, which eventually leads
to vasospasm and thrombus formation.
0017 A low level of HDL cholesterol is a strong independ-
ent etiological factor for CHD. Low HDL cholesterol is
defined as a level of < 40 mg dl
1
(Table 2). High-
density lipoprotein cholesterol levels are negatively
influenced by cigarette smoking, overweight/obesity,
physical inactivity, and type 2 diabetes. It has been
hypothesized that cholesterol efflux from athero-
sclerotic lesions is promoted by HDL cholesterol via a
receptor-mediated mechanism.
0018A meta-analysis of prospective studies has indi-
cated that elevated triglycerides, or hypertriglyceride-
mia (200 mg dl
1
), is an independent risk factor for
CHD after controlling for LDL and HDL cholesterol.
Several factors contribute to the development of high
triglyceride levels such as cigarette smoking, obesity
and overweight, physical inactivity, type 2 diabetes,
excess alcohol consumption, and genetic disorders
(e.g., familial hypertriglyceridemia). The proposed
potential mechanisms by which elevated triglycerides
contribute to CHD include increased thrombo-
genicity, increased chylomicron and very low-density
lipoprotein (VLDL) remnant particles, increased LDL
and decreased HDL cholesterol, and altered meta-
bolic processes involved in triglyceride transport.
0019Lp(a) is a cholesterol ester- and apolipoprotein
B-containing particle with the presence of glycoprotein
apo(a) that can promote atherogenesis by enhancing
oxidation of LDL cholesterol, promoting cholesterol
deposition in tunica intima, and interfering with
fibrinolysis. The level of Lp(a) appears to be genetically
determined.
Thrombogenic Risk Factors and Homeostasis
0020Both case-control and prospective studies have shown
that thrombogenic factors (fibrinogen, blood clot-
ting factor VII, tPA and, PAI-1) independently and
tbl0002Table 2 Classification of total, LDL, HDL cholesterol, and
triglycerides (mg dl
1
)
Lipid fraction Classification
Total cholesterol
< 200 Low
200–239 Borderline high
240 High
LDL cholesterol
< 100 Optimal
100–129 Near optimal/above optimal
130–159 Borderline high
160–189 High
190 Very high
HDL cholesterol
< 40 Low
60 High
Tr i g l y c e r i d e s
< 150 Optimal
150–199 Borderline high
200–499 High
500 Very high
HDL, high-density lipoprotein; LDL, low-density lipoprotein.
From (2001) Third Report of the National Cholesterol Education Program
(NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood
Cholesterol in Adults (Adult Treatment Panel III) Executive Summary.NIH
Publication No. 01–3670. Bethesda, MD: National Heart, Lung, and Blood
Institute.
1652 CORONARY HEART DISEASE/Etiology and Risk Factor
consistently increase the risk of CHD. Coronary
thrombosis is generally present in most cases of
acute myocardial infarction. Increased platelet counts
and platelet aggregation are also associated with re-
current CHD. PAI-1 activity or antigen inhibits fibri-
nolysis, and increased concentrations of fibrinogen
promote platelet aggregation, which in turn induces
blood clotting. Several factors elevate fibrinogen,
notably increasing age, smoking, obesity and dia-
betes, use of oral contraceptive pills, and genetic
polymorphism. Blood clotting factor VII plays a piv-
otal role in coagulation initiation and may also be
predictive of myocardial infarction. Plasma concen-
trations of factor VII again are influenced by both
environmental and genetic polymorphism. PAl-
1 regulates the rate of tPA synthesis by the endothelial
cells. Several studies have shown that the levels of
PAl-1 and tPA mass concentrations are predictive of
initial and subsequent myocardial infarction. Ele-
vated plasma fibrinogen, a consistent procoagulant
risk factor for CHD, has several mechanisms;
notably, it increases fibrin formation, platelet aggre-
gation, and plasma viscosity. Other markers such as
the d-dimer, plasmin-a-antiplasmin complex, are in-
dicators of activation of the fibrinolytic system.
Inflammation and Infectious Agents
0021 There is a considerable body of evidence indicating
that inflammation and infection are responsible in the
pathogenesis of CHD as potential etiological factors.
C-reactive protein (CRP) is of special interest. Both
experimental and clinical studies have documented
that elevation of plasma CRP, a marker of low-grade
inflammation, can predict an increased risk of CHD
event in healthy persons independent of other risk
factors. Although the definitive mechanism of actions
of CRP that triggers low-grade inflammatory response
in atherosclerosis is still under further investigation,
possible indirect roles have been as follows: (1) CRP
may act as a procoagulant, (2) it binds avidly with
neutrophils, (3) it facilitates uptake of oxidized LDL
cholesterol by macrophages, (4) it induces comple-
ment activation, (5) it is chemotactic for monocytes,
and (6) it impairs endothelial functions and enhances
tissue injury. Other low-grade markers of inflamma-
tion, notably amyloid A protein, albumin, IL-6, TNF-
a, transforming growth factor b1, and leukocytes may
also be involved in the atherogenesis process. In the
development of coronary event, the proposed mech-
anisms of IL-6 include alterations in insulin sensitivity,
increased hepatic release of fibrinogen, procoagulant
effects on platelets, and increased release of adhesion
molecules. TNF-a inhibits lipoprotein lipase, stimu-
lates lipolysis, and influences endothelial function
leading to a procoagulant state. Recently, chronic
infections by several microorganisms, especially
herpes simplex viruses, cytomegalovirus, Chlamydia
pneumoniae, and Helicobacter pylori, have attracted
interest in the potential roles in the pathogenesis of
atherosclerosis leading to CHD.
Homocysteine
0022There is substantial evidence supporting elevated
plasma levels of Hcy (> 15 mmol l
1
) as an independent
etiological factor for premature atherosclerotic
lesions. Hcy is a metabolite of methionine as a product
of many S-adenosylmethionine-dependent trans-
methylation reactions that require several enzymes
(cystathionine b-synthase, g-cystathionase, betaine-
homocysteine methyltransferase, methionine syn-
thase, 5,10-methyltetrahydeofolate reductase) and
vitamins (folic acid, B
12
,B
6
). Enzymatic defects or
vitamin deficiencies cause Hcy accumulation, which
causes (1) direct toxic effects to the endothelium, (2) in-
creased adhesiveness of platelets, (3) oxidation of LDL
cholesterol, (4) proliferation of smooth muscle, (5)
inhibition of nitric oxide formation, and (6) increased
thromboxane formation. Meta-analyses document
that as much as 10% of the CHD risk may be attribut-
able to elevated Hcy, and each 5 mmol l
1
increment of
Hcy is associated with a 60–80% increase in CHD.
Homocystinuria is a rare autosomal recessive genetic
disorder that is associated with a 10-fold increase of
blood Hcy levels.
Emerging Risk Factors
0023Accumulating evidence suggests that the renin–angio-
tensin II system plays an integral role in the multiple
processes critically implicated in the pathogenesis of
atherosclerosis. The inflammatory response of angio-
Psychosocial
stress
Catech-
olamines
Smoking (Central)
obesity
Pollution
migration
infection
HPA
axis
+ve
−ve
Genotype
programming
CRP
Insulin
resistance
Hyper
tension
Dys-
lipidemia
Endothelial
dysfunction
Coagulation
CHD
Interleukin-6
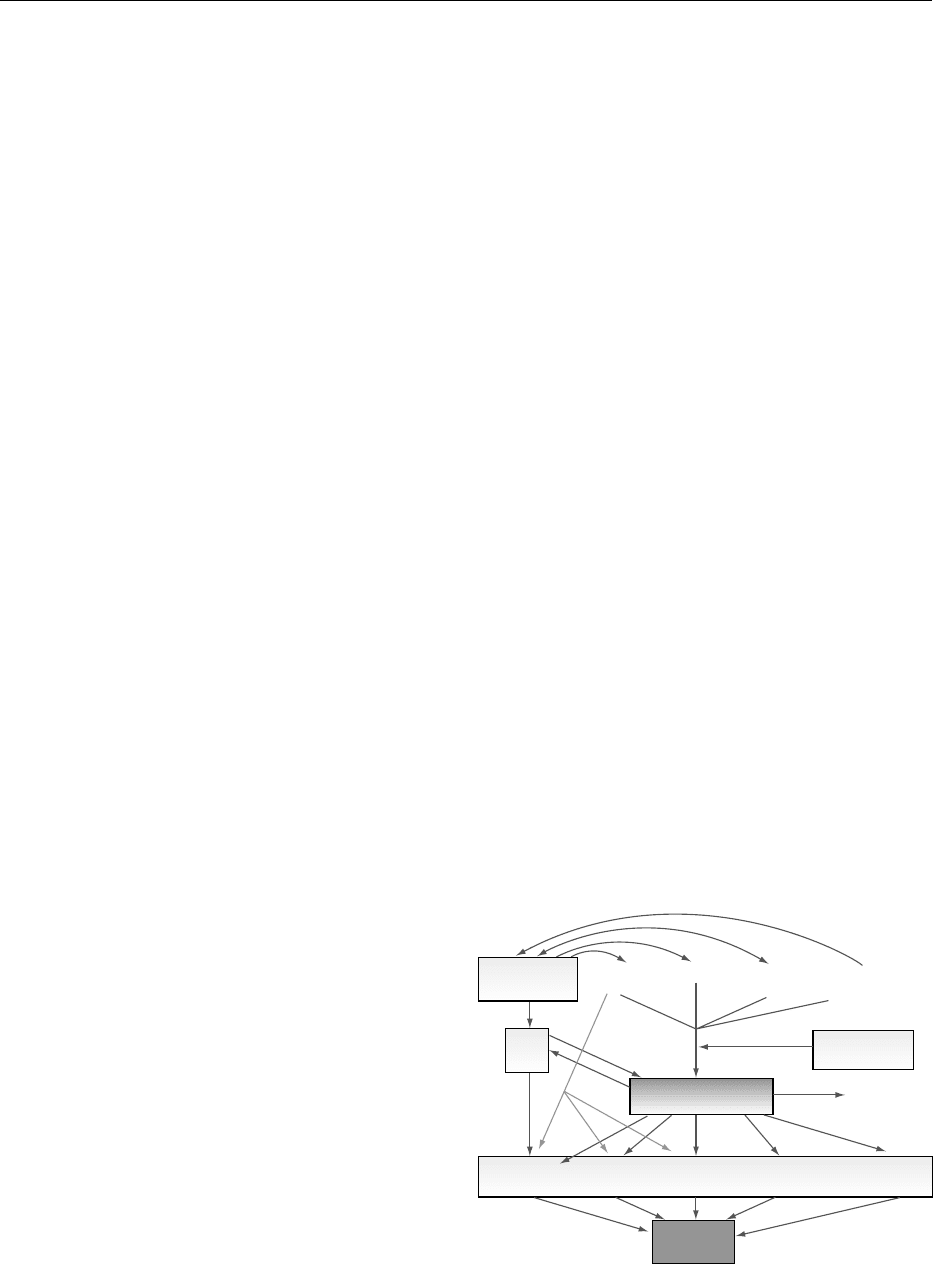
fig0003Figure 3 Possible mechanisms of action of IL-6 in the patho-
genesis of CHD. From Atherosclerosis 148(2): 209–214 with
permission.
CORONARY HEART DISEASE/Etiology and Risk Factor 1653

tensin II on endothelium is mediated by the release of
platelet-derived growth factor, insulin-like growth
factor, IL-1, IL-6, and IL-8. Angiotensin II may also
alter the structural integrity of endothelium, antagon-
ize NO synthesis, increase the growth and migration of
smooth muscle cells and fibroblasts, and promote LDL
cholesterol oxidation and deposition in the intimal
layer. IL-6 may also initiate the atherosclerotic process
by changing metabolic, endothelial, and coagulant
mechanisms. The possible mechanisms of action of
IL-6 in CHD pathogenesis are illustrated in Figure 3.
0024 The multifactorial etiology of CHD and the contri-
bution of these factors, individually or in combin-
ation, to the risk of developing a CHD event in
future is of prime importance in terms of both pri-
mary and secondary prevention.
See also: Atherosclerosis; Cholesterol: Role of
Cholesterol in Heart Disease; Coronary Heart Disease:
Antioxidant Status; Intervention Studies; Prevention;
Diabetes Mellitus: Secondary Complications; Exercise:
Metabolic Requirements; Hypertension: Physiology;
Hypertension and Diet; Obesity: Etiology and Diagnosis;
Smoking, Diet, and Health; Vitamin B
6
: Properties and
Determination
Further Reading
Boyle E Jr., Lille S, Allaire et al. (1997) Atherosclerosis.
Annals of Thoracic Surgery 64: S47–S56.
Folsom A (1999) ‘New’ risk factors for atherosclerotic dis-
eases. Experimental Gerontology 34: 483–490.
Fuster V, Gotto A, Libby P et al. (1996) Pathogenesis of
coronary disease: the biological role of risk factors. Jour-
nal of the American College of Cardiology 27: 964–976.
Hajjar D and Nicholson A (1995) Atherosclerosis. An
understanding of the cellular and molecular basis of the
disease promises new approaches for its treatment in the
near future. American Scientist 83: 460–467.
Pahor M, Elam M, Garriaon R et al. (1999) Emerging
noninvasive biochemical measures to predict cardiovas-
cular risk. Journal of the American Medical Association
285: 581–587.
Pasternak R, Gundy S, Levy D and Thompson P (1996)
Spectrum of risk factors for coronary heart disease. Jour-
nal of the American College of Cardiology 27: 978–990.
Refsum H, Ueland P, Nygard O and Vollset SE (1998)
Homocysteine and cardiovascular disease. Annual
Reviews of Medicine 49: 31–62.
Ross R and Glomset J (1973) Atherosclerosis and arterial
smooth muscle cell. Science 180: 1332–1339.
Schmidt-Ott K, Kagiyama S and Philips M (2000) The
multiple actions of angiontensin II in atherosclerosis.
Regulatory Peptides 93: 65–77.
(1997) The Sixth Report of the Joint National Committee
on Prevention, Detection, Evaluation, and Treatment of
High Blood Pressure. NIH Publication No. 98–4080.
Bethesda, MD: National Heart, Lung, and Blood
Institute.
(2001) Third Report of the National Cholesterol Education
Program (NCEP) Expert Panel on Detection, Evalu-
ation, and Treatment of High Blood Cholesterol in
Adults (Adult Treatment Panel III) Executive Summary.
NIH Publication NO. 01–3670. Bethesda, MD: Na-
tional Heart, Lung, and Blood Institute.
Van Lente F (2000) Markers of inflammation as predictors in
cardiovascular disease. Clinica Chimica Acta 293: 31–52.
Wood D, Backer G, Faergeman O et al. (1998) Prevention
of coronary heart disease in clinical practice: Recom-
mendations of the Second Joint Task Force of European
and other Societies on Coronary Prevention. Athero-
sclerosis 140: 199–270.
Antioxidant Status
D S P Abdalla, Universidade de Sa
˜
o Paulo, Cidade
Universita
´
tia, Sa
˜
o Paulo, Brazil
Copyright 2003, Elsevier Science Ltd. All Rights Reserved.
Introduction
0001Coronary heart disease (CHD) is still the major com-
ponent of total cardiovascular disease (CVD) mortal-
ity. The possibility that antioxidant substances might
safely prevent oxidative stress and antagonize the
atherosclerotic process has raised great interest in
scientific and public communities. Epidemiological
studies have demonstrated that those who consume
higher amounts of fruits and vegetables have lower
rates of CVD events. A possible explanation for this
protective effect is the content of antioxidant micro-
nutrients of fruits and vegetables. This section briefly
summarizes the basic concepts behind the hypothesis
that antioxidants may be helpful to prevent or retard
the progression of CVD.
Oxidative Stress in Atherosclerosis
0002Atherosclerosis is a multifactorial disease of the arter-
ial wall that has been considered to be the primary
cause of most cardiovascular diseases, including
CHD. The so-called oxidative theory of atheroscler-
osis has received great attention in the past 15 years,
and a large body of experimental evidence has been
accumulated. Free radicals may directly damage
arterial endothelium, promote thrombosis, and inter-
fere with normal vasomotor regulation. Oxidation-
related events have been claimed to be involved in
several steps possibly related to atherosclerosis:
(1) the activation of endothelial cells to express adhe-
sion molecules; (2) recruitment of monocytes in
the subendothelial space and their differentiation
into macrophages; (3) formation of foam cells;
1654 CORONARY HEART DISEASE/Antioxidant Status
(4) differentiation, proliferation, and migration of
smooth muscle cells; (5) activation of metalloprotei-
nases; and (6) alterations of vasorelaxation. Oxida-
tive stress, particularly oxidation of low-density
lipoprotein (LDL), has been considered to be a crucial
event in atherogenesis. Free radicals derived from
arterial wall cells can induce oxidative damage
to LDL protein and lipids, which significantly in-
creases its atherogenicity. Oxidatively modified LDL
(oxLDL) can start the chronic inflammatory reactions
of atherosclerosis. OxLDL elicits local vascular cells
to produce monocyte chemotactic protein 1 and gran-
ulocyte and macrophage colony-stimulating factors
promoting monocyte recruitment and differentiation
to macrophages in the subendothelial area of arterial
walls. As oxLDL is more negatively charged, it is
recognized and internalized by the scavenger receptor
pathway on macrophages, which is not regulated by
negative feedback mechanisms, resulting in a massive
uptake of oxLDL leading to foam cell formation.
Furthermore, oxLDL is also cytotoxic to vascular
cells, thus causing the release of lipids and lysosomal
enzymes into the extracellular space of the arterial
wall, perpetuating the inflammatory stimulus and
enhancing the progression of the atherosclerotic
lesion (Figure 1). OxLDL also seems to be involved
in the immune response. Ox-LDL and its immune
complexes have been found in atherosclerotic lesions.
In addition, plasma of rabbits and humans contains
autoantibodies that react with several forms of
oxLDL. Moreover, a positive correlation between
progression of carotid atherosclerosis and the titer
of antibodies against oxLDL has been found.
OxLDL can also impair endothelial function by in-
hibiting the release of endothelium-derived nitric
oxide (
NO). Disturbances of G protein-dependent
stimulation of
NO release, as well as direct inactiva-
tion of
NO, may be involved in this effect, resulting
in enhanced vasospasm and platelet and monocyte
adhesion to endothelium. OxLDL increases endothe-
lial cell tissue factor and decreases protein C
activation and may thus increase procoagulation at
the endothelial surface. The oxidative hypothesis of
atherosclerosis has been validated by a series of in vivo
studies performed in animal models where the initial
development of the atherosclerotic disease was effect-
ively inhibited by supplementation of selected anti-
oxidants.
Diet and Antioxidant Status
0003Diet has a profound effect on antioxidant status. The
overall antioxidant effect of diet is determined
by its components and other factors, such as:
Lumen
EC
Intima
SMC
Media
Migration
Macrophage
CSFs
Proliferation
LDL
LDL
OH
H
2
O
2
Fe
2+
LDLox
LDLox
Monocyte
TG-Lp
LPox
LPox
Foam cell
Decreased
cholesterol
efflux
Ferritin
EC Injury
EC Injury
Chemotactic factors
adhesion molecules
HDLox
LP
Neutrophil
LCAT inhibition
CE Transfer
ONOO
−
LDLox
ONOO
−
NO
Antioxidants
tocopherols
carotenoids
ascorbate
polyphenols
O
−
2
O
−
2
fig0001 Figure 1 (see color plate 40) Possible effects of antioxidants in the atherogenic process. CE, cholesteryl ester; CSFs, colony-
stimulating factors; HDLox, oxidized HDL; LCAT, lecithin: cholesterol acyl transferase; LDLox, oxidized LDL; LPox, oxidized lipopro-
teins; TG-Lp, triacylglicerol-rich lipoproteins; EC, endothelial cells; SMC, smooth muscle cells.
CORONARY HEART DISEASE/Antioxidant Status 1655
