Caballero B. (ed.) Encyclopaedia of Food Science, Food Technology and Nutrition. Ten-Volume Set
Подождите немного. Документ загружается.


abnormal nodules. Alcoholic cirrhosis is mostly
micronodular in type, with a size of nodules from
1 to 5 mm. Macronodules with a size ranging from
5 to 50 mm may occur, especially in the late phases of
the disease. The loss of normal liver architecture, with
separation of the portal tracts and the central zones of
the liver by septa of fibrotic tissue, results in alter-
ations of the vascular supply and a disturbance of the
intrahepatic blood circulation.
0016 Morbidity and mortality resulting from alcoholic
cirrhosis are related principally to the loss of liver cell
function, to derangements in the vascular system of
the liver, or to both. The onset of cirrhosis is often
insidious and associated with nonspecific symptoms
such as fatigue, anorexia, weight loss, nausea, and
abdominal discomfort. As the disease progresses,
signs of hepatocellular failure became prominent.
The most severe complications are iron overload,
hepatic encephalopathy, and portal hypertension
with ascites and bleeding from esophageal varices.
0017 In association with cirrhosis of the liver, hepatocel-
lular carcinoma may develop. The pathogenesis of the
carcinomatous transformation is still unclear, espe-
cially because these tumor forms may also occur in
noncirrhotic livers.
0018 Ethanol leads to a number of metabolic and struc-
tural alterations in the liver that predispose this organ
to derangements in its functional integrity. These are
as follows: an increase in the ratio of NADH (the
reduced form of nicotinamide adenine dinucleotide,
or NAD) to NAD; interactions of ethanol with lipid
and protein metabolism; stimulation of fibrosis with
deposition of collagen; inhibition of liver cell regener-
ation; humoral and cellular immunological alter-
ations; and excessive production of free radicals and
cytokines. Alcohol induces cell death and inflamma-
tion, which can result in scarring that distorts the
liver’s internal structure and impairs its function.
Acetaldehyde, the first oxidation product of ethanol
metabolism, may exert some toxic effects of its own
in liver tissue; it activates stellate cells directly and
promotes liver scarring in the absence of inflamma-
tion.
0019 All stages of liver injury can be produced in the
baboon fed high-protein and vitamin-supplemented
diets. This evidence suggests that toxic effects of
alcohol, and not malnutrition, are the principal
causes for the development of cirrhosis in chronic
alcoholics. But alcohol abuse establishes only the
conditions for the generation of cirrhotic lesions,
which require the addition of some independent
factors emerging over time.
0020 Abstinence from alcohol is the essential factor for
prevention and treatment of alcoholic cirrhosis. If
irreversible liver damage is already established, some
complications of cirrhosis can be alleviated by nutri-
tional treatment. Portal-systemic encephalopathy, for
example, often responds to an application of amino
acid mixtures, enriched with branched-chain amino
acids, whereas ascites responds favorably to sodium
restriction.
Wernicke’s Encephalopathy and
Korsakoff’s Syndrome
0021Wernicke’s encephalopathy and Korsakoff’s psych-
osis are diseases of the central nervous system (CNS)
secondary to alcoholism. They represent a continuum
of the same neuropathological process and develop in
about 2–3% of alcoholics. Wernicke’s disease is often
followed by Korsakoff’s syndrome. Severe alcoholics
may have both diseases, but some of them show
Korsakoff’s psychosis without preceding Wernicke’s
encephalopathy. Wernicke’s disease is an acute or
chronic encephalopathy with a triad of clinical abnor-
malities: ophthalmoplegia, ataxia, and mental con-
fusion. Korsakoff’s syndrome is a psychosis with
marked abnormalities in cognitive function: the car-
dinal symptoms are anterograde amnesia, disorien-
tation, learning deficits, and confabulations. The
relationship between the two diseases is not entirely
clear. The neuropathological changes seen in autopsy
materials of Wernicke–Korsakoff patients consist of
circumscribed, symmetrical lesions in the diencepha-
lon and brainstem. Most affected are the mammillary
bodies and the dorsomedial nuclei of the thalamus. In
acute cases the lesions are widespread and severe. In
chronic cases the lesions are more restricted and show
great variations in extent and severity within the
affected area. There are corresponding variations of
the clinical symptoms.
0022Extreme deficiency of thiamin, induced by malnu-
trition and interaction of ethanol with thiamin ab-
sorption and metabolism, is regarded as the primary
cause of this syndrome. Patients with Wernicke’s dis-
ease often have a high energy intake, consisting
mainly of ethanol and/or carbohydrates, without suf-
ficient protein and vitamins. Beyond that a direct
toxic effect of alcohol on the brain has also been
implicated. The Wernicke–Korsakoff’s disease is not
confined to alcoholism, but is also present in other
conditions associated with thiamin malnutrition, e.g.,
hyperemesis gravidarum, Hodgkin’s lymphoma, car-
cinoma of the stomach, and anorexia nervosa. Thia-
min application can reverse Wernicke’s syndrome in
many but not all patients, at least when administered
early in the course of the disease. In contrast, Korsak-
off’s patients often show poor response to thiamin
therapy. Additional factors, of as yet unknown origin,
seem to be necessary for the full development of
1326 CIRRHOSIS AND DISORDERS OF HIGH ALCOHOL CONSUMPTION

Korsakoff’s psychosis. There is evidence to suggest
that a genetic predisposition is involved in the eti-
ology of the Wernicke–Korsakoff syndrome.
0023 In some patients a variant form of transketolase
with a low affinity for its coenzyme thiamin pyro-
phosphate has been diagnosed. This isoenzyme re-
quires much larger amounts of thiamin to function
than the normal enzyme. Some authors suggest that a
variant transketolase and thiamin deficiency together
contribute to the pathogenesis of the brain damage of
the Wernicke–Korsakoff syndrome. In other studies
this hypothesis has not been confirmed. (See Anorexia
Nervosa.)
Alcoholic Polyneuropathy, and Beriberi in
Alcoholics
0024 Symmetric and predominantly distal polyneuropathy
is probably the most common sequela of chronic
alcohol abuse. It occurs in about 20% of all alcohol-
ics. First symptoms include paresthesia, dysesthesia
and pain sensations affecting primarily the lower ex-
tremities, accompanied by reduced or absent reflex
activity. These symptoms are usually followed in the
more advanced stages of the disease by marked motor
impairments, such as weakness and atrophy of the
anterior tibial muscles. Electrophysiological slow-
down of the sensory and motor conduction velocities
of the peripheral nerves, as well as myopathic changes,
are usually observed. The predominant pathological
abnormalities are distal pronounced axonal degen-
erations, mainly of the large fibers with a gradient
of changes toward the extremities (‘dying-back de-
generation’). Segmental demyelination appears as a
secondary phenomenon. Alcoholic polyneuropathy
is clinically indistinguishable from beriberi (‘dry
beriberi’) neuropathy. As in the Wernicke–Korsakoff
syndrome, thiamin deficiency is regarded as the pri-
mary cause. Besides that, a long-lasting low protein-
energy supply seems to be one of the main pathogenic
factors for the development of the typical lesions of
peripheric nerves. In addition, insufficient intake
or absorption of pyridoxine, folates, B
12
and other
B vitamins contributes to the development of the
disease, and direct toxic effects of ethanol and its
metabolites are involved in the destruction of nerve
ultrastructure and function. Recovery from alcoholic
peripheral neuropathy is slow and often incom-
plete. The most important therapeutic factors are
abstinence from alcohol and improvement of the
overall nutritional status. Additional supplementa-
tion with high doses of B-complex vitamins is ne-
cessary. With this therapeutic schedule a slow
diminution of symptoms may be expected in many
but not all cases.
Pancreatitis
0025The association between alcohol consumption and
pancreatitis is well recognized. In general, about
60–90% of all cases of chronic pancreatitis are alco-
hol-related. As with alcoholic cirrhosis, there has
been an increasing prevalence of alcoholic pancrea-
titis in industrialized countries in the last 30 years.
This disease often develops without obvious clinical
symptoms. However, in autopsies of patients with a
history of alcoholism, marked pancreatic lesions are
frequently observed. Patients with severe or compli-
cated forms of this disease may rapidly develop
marked generalized malnutrition. (See Gallbladder.)
0026A favored hypothesis regarding the mechanism of
action of chronic alcohol consumption on the pan-
creas is the observation that ethanol increases the
protein content of pancreatic juice, with a concomi-
tant decrease in water and electrolytes. This induces
a precipitation of protein plugs within the pancre-
atic ducts, followed by retraction and calcification,
resulting in pancreatic stones, atrophy of the duct
epithelium, and proliferation of the connective tissue.
The consequences are stenosis or dilatations of the
ducts, cysts and pseudocysts, and progressive dis-
appearance of the pancreatic exocrine tissue which
is replaced by fibrosis. Pathologically, the gland is
edematous and hemorrhagic. Besides chronic over-
consumption of alcohol, both a high-fat, high-protein
diet and, paradoxically, malnutrition have been im-
plicated in the pathogenesis of the disorder.
0027Alcoholic pancreatitis tends to be recurrent and
progressive and to result in pancreatic exocrine insuf-
ficiency. Some 1–2% of alcoholics suffer from an
acute form. This complication can be quite severe,
with violent epigastric pain, nausea, and vomiting.
Cases of sudden death from acute attacks have been
reported.
0028Even heavy drinking does not modify the risk for
pancreatic cancer. Several epidemiologic studies do
not support an association between alcohol consump-
tion and incidence of pancreatic cancer.
Effect of Chronic Alcohol Consumption on
the Brain
0029Ethanol – in common with other centrally acting
agents – rapidly diffuses across the blood–brain bar-
rier and equilibrates in brain tissue. Its concentration
depends upon the plasma concentration, vasculariza-
tion, local blood flow, and water content of the con-
cerned brain area. Chronic ethanol consumption is
associated with a variety of deficits in brain function
over a wide range of doses and is often followed by
clinically obvious brain damage.
CIRRHOSIS AND DISORDERS OF HIGH ALCOHOL CONSUMPTION 1327

Alcoholic Dementia
0030 Alcoholics often suffer from disorders in cognitive
processes, varying from a relatively slight memory
reduction to deep dementia. The deficits in cognitive
function are similar to those seen in patients with
Alzheimer’s disease or multiinfarct dementia. His-
topathologically, the brain structures that are pos-
sibly involved do not show any lesion or atrophy,
but there is considerable evidence that alcoholic de-
mentia may potentially result from progressive loss of
some neurons, synapses, and/or their associated re-
ceptors. Prolonged abstinence has a considerable re-
ducing effect on dementia symptoms, but in most
subjects the reversibility is only partial. Alcoholic
dementia seems to be a severe form of Korsakoff’s
syndrome.
Alcohol Tolerance and Dependence
0031 Functional tolerance and physical dependence are
inexorably linked phenomena reflecting adaptive
changes in the brain which compensate for the inhib-
ition of functions by ethanol. Functional tolerance
means a decrease in the sensitivity of the CNS pro-
duced by chronic alcohol intake. Physical dependence
means hyperexcitability of the CNS following alcohol
withdrawal after adaptation. The molecular mechan-
isms underlying both phenomena are as yet unknown.
Possibly the effects are primarily related to changes in
the microorganization and physical state of brain
membranes.
Brain Shrinkage
0032 Cerebral shrinkage seems to be one of the most fre-
quent brain lesions induced by chronic alcohol con-
sumption. It can be demonstrated by computerized
tomography (CT) scanning in patients with alcohol-
ism and even in ‘social drinkers.’ Cerebral shrinkage
relates to a loss of white matter rather than of gray
matter. In alcoholics the shrinking results in a lower
brain weight compared to age- and sex-matched con-
trols. After cessation of alcohol drinking cerebral
shrinkage is often partially reversed.
Cerebellar Atrophy
0033 Many alcoholics show cerebellar atrophy with pro-
gressive ataxia of stance and gait and, occasionally,
an impairment of speech and ocular motility. This
cerebellar degeneration is characterized by great
uniformity of the clinical and pathological manifest-
ations. In the majority of cases the disorder develops
over several weeks or months, followed by years of
stability. The pathological changes consist of degener-
ation of neuronal elements of the cerebellar cortex,
particularly of the Purkinje cells. The dendritic
networks of these cells show alterations in length
parameters under the influence of ethanol in rats.
Topographically, the lesions of the cerebellum are
restricted to the anterior and superior vermis and to
the hemispheres.
0034Although cerebellar atrophy is most frequently en-
countered in chronic alcoholic patients, it has also
been reported in old people and in malnourished
individuals, who allegedly did not drink. It has been
postulated that alcohol and the aging process super-
imposed upon malnutrition may be responsible for
the damage caused to the cerebellum.
Fetal Alcohol Syndrome
0035Prenatal exposure to alcohol produces various mor-
phological, physiological, and behavioral abnormal-
ities in the newborn, termed fetal alcohol syndrome
(FAS). It has been observed in 1 in every 1000 chil-
dren born to alcoholic mothers, and is the most
common known cause of mental retardation. The
Fetal Alcohol Study Group of the Research Society
on Alcoholism has defined three criteria for the diag-
nosis of FAS:
.
0036growth retardation
.
0037abnormalities of the CNS
.
0038abnormal facial features
0039The mechanisms by which alcohol produces these
effects are not yet fully elucidated. Possibly ethanol
affects NMDA and g-aminobutyric acid receptors in
the developing brain, leading to neuron death. The
minimum level of alcohol consumed during preg-
nancy that causes FAS has not been established.
Animal models have demonstrated conclusively that
ethanol can cross the placenta and is teratogenic in
several species. The effect is dose-dependent and the
type of malformation observed depends upon the
stage of development when the exposure occurred.
Besides the toxic effects of ethanol, another potential
cause of FAS is maternal and/or fetal malnutrition
induced by impaired placental transfer of essential
nutrients.
0040Among the neuroanatomical alterations observed
in humans and animal models with FAS are decreased
brain weight, delays in dendritic development, de-
creased numbers of pyramidal neurons in the hippo-
campus, and sprouting in the dentate gyrus. The
clinical symptoms of the CNS dysfunction are
mental retardation, hyperactivity, and learning dis-
abilities. Despite nutritional rehabilitation, the phys-
ical and mental development of the children remains
impaired. To date, a safe intake of alcohol for preg-
nant women has not been established. (See Preg-
nancy: Safe Diet.)
1328 CIRRHOSIS AND DISORDERS OF HIGH ALCOHOL CONSUMPTION
See also: Alcohol: Metabolism, Beneficial Effects, and
Toxicology; Alcohol Consumption; Anorexia Nervosa;
Calcium: Physiology; Cholecalciferol: Physiology;
Cobalamins: Physiology; Folic Acid: Physiology;
Gallbladder; Liver: Nutritional Management of Liver and
Biliary Disorders; Magnesium; Pregnancy: Safe Diet;
Retinol: Physiology; Thiamin: Physiology; Vitamin B
6
:
Properties and Determination; Zinc: Physiology
Further Reading
Bitsch I (1983) Perspektiven der Alkoholforschung. Erna¨h-
rungs-Umschau 30: 132–135.
Bitsch R (1987) Alkohol und Vitaminstoffwechsel. Erna¨h-
rungs-Umschau 34: 161–166.
Eriksson K, Sinclair JD and Kiianmaa K (eds) (1980)
Animal Models in Alcohol Research. London.
Hall PM (ed) (1995) Alcoholic Liver Disease: Pathology
and Pathogenesis, 2nd edn. London.
Kalant H, Khanna JM and Israel Y (1991) Advances in
Biomedical Alcohol Research. Oxford.
Lindros KO, Ylikahri R and Kiianmaa K (1987) Advances
in Biomedical Alcohol Research. Oxford.
National Institute on Alcohol Abuse and Alcoholism (1999)
Rockville, Alcohol Alert No 42, 46.
Shils ME, Olson JA and Shike M (eds) (1999) Modern
Nutrition in Health and Disease, 9th edn. Baltimore:
Lippincott, Williams & Wilkins.
Torvik A (1987) Brain lesions in alcoholics: neuropatholo-
gical observations. Acta Medica Scandinavica Supple-
mentum 717: 47–54.
Victor M, Adams RD and Collins GH (1989) The Wer-
nicke–Korsakoff Syndrome, 2nd edn. Philadelphia.
Ziegler EM and Filer LJ (eds) (1996) Present Knowledge in
Nutrition, 7th edn. Washington, DC: ILSI.
Citric Acid Cycle See Tricarboxylic Acid Cycle; Oxidative Phosphorylation
CITRUS FRUITS
Contents
Types on the Market
Composition and Characterization
Oranges
Processed and Derived Products of Oranges
Lemons
Grapefruits
Limes
Mandarins
Types on the Market
J Forsyth, Formerly of New South Wales Agriculture,
Orange, NSW, Australia
J Damiani, Australian Citrus Growers Inc., Mildura,
Victoria, Australia
Copyright 2003, Elsevier Science Ltd. All Rights Reserved.
Background
0001 Citrus is the main fruit tree crop grown throughout
the world. It is made up of many species that vary in
importance due to different uses, markets, growing
conditions, and climatic zones. The large production
has significance in local and world trade for both
fresh and processed products. Brief details on the
classification of the species, growing regions and con-
ditions, production statistics, with the utilization of
the main and also lesser known types are discussed.
Classification
0002The taxonomic classification of the Citrus species is
complex and diverse, and not universally agreed
upon, but those used by Swingle and Reece will be
followed in this article. Citrus, as a social and cultural
CITRUS FRUITS/Types on the Market 1329
fruit crop, also has countless local names and iden-
tities throughout the world, often for an identical
cultivar.
0003 Citrus trees belong to the plant family Rutaceae,
subfamily Aurantioideae, which comprises 33 well-
known and described genera and 203 species. In add-
ition, many natural and man-made hybrids also exist
that have resulted in new edible cultivars. Many
genera contain unusual or remote relatives of citrus
with nonedible fruit, but of ornamental value like
Merrillia and Murraya, or have genetic importance
in breeding programs like Poncirus and Severinia.
0004 True citrus fruit trees, which have a berry fruit
called a hesperidium, belong to six genera: Citrus,
Fortunella, Poncirus, Microcitrus, Eremocitrus,and
Clymenia. Only the Citrus and Fortunella genera
have fresh fruit cultivars of commercial importance.
Both these genera are evergreen and unifoliate, and
the genus Citrus provides nearly all of the commercial
cultivars grown throughout the world.
Main Types on the Market
0005 Citrus fruits are principally marketed according to
how they are consumed:
1.
0006 As fresh or dessert fruits – sweet oranges, manda-
rins (eaten out of hand), grapefruit, or pummelo
(spooned). Juice, slices, segments, rind, and leaves
are also used to garnish food.
2.
0007 As processed products – juice (fresh, chilled,
frozen, canned, blended, or concentrated), syrups
and cordials, segments and rind oil, or essence.
After the juice is extracted, there remain residues
that can be a source material from which over 300
valuable byproducts can be produced. Some spe-
cialized types are also candied, dried, or used for
marmalade manufacture. (See Citrus Fruits: Com-
position and Characterization; Processed and De-
rived Products of Oranges.)
0008 The main types of fresh citrus fruits on the export
or main local markets, and also used for processing,
are normally broadly grouped as oranges, mandarins,
lemons and limes, and grapefruit. There is also a wide
range of other minor or lesser known species and
types that may have regional or local significance.
Some of these are mentioned in a later section. The
following brief comments are made on the main citrus
types, as listed in available statistics and found on
world markets.
Sweet Oranges
0009 The sweet orange types (Citrus sinensis [L.] Osbeck)
are the most widely grown citrus fruits throughout
the world and provide the greatest fruit marketing
production. The many known cultivars can be sub-
divided into three main groups as the acidless or sugar
oranges do not contribute to world trade:
.
0010Common oranges (also known as blond or white
oranges). The Valencia is the main cultivar grown,
with harvesting from spring to autumn, depending
on local climates. The fruit is dual purpose and
suitable for both eating as fresh fruit or processing,
while seedless types are also grown, e.g., Delta and
Midknight. Other common oranges are often seedy
and mainly suitable for processing, e.g., Pera,
Hamlin, and Pineapple.
.
0011Navel oranges are also widely grown as winter
seedless eating fruit (Figure 1). The Washington
navel with numerous clones or selections is the
most important cultivar, while there are many
others navels (over 50 distinct varieties or clones)
available that spread the maturity period from
early (like Fukumoto, Navelina, Leng, and New-
hall) to late (Lane and Navelate), and to what are
now being called ‘summer navels,’ following the
location of many new very late maturing cultivars
in Australia, e.g., Powell, Chislett, and Barnfield. A
new pink/red fleshed navel – Cara Cara – is also
creating marketing interest.
.
0012Blood or pigmented oranges have been popular in
Mediterranean countries for their distinctive flavor
and both rind, flesh, and juice pigments, e.g.,
Tarocco, Sanguinello, and Moro.
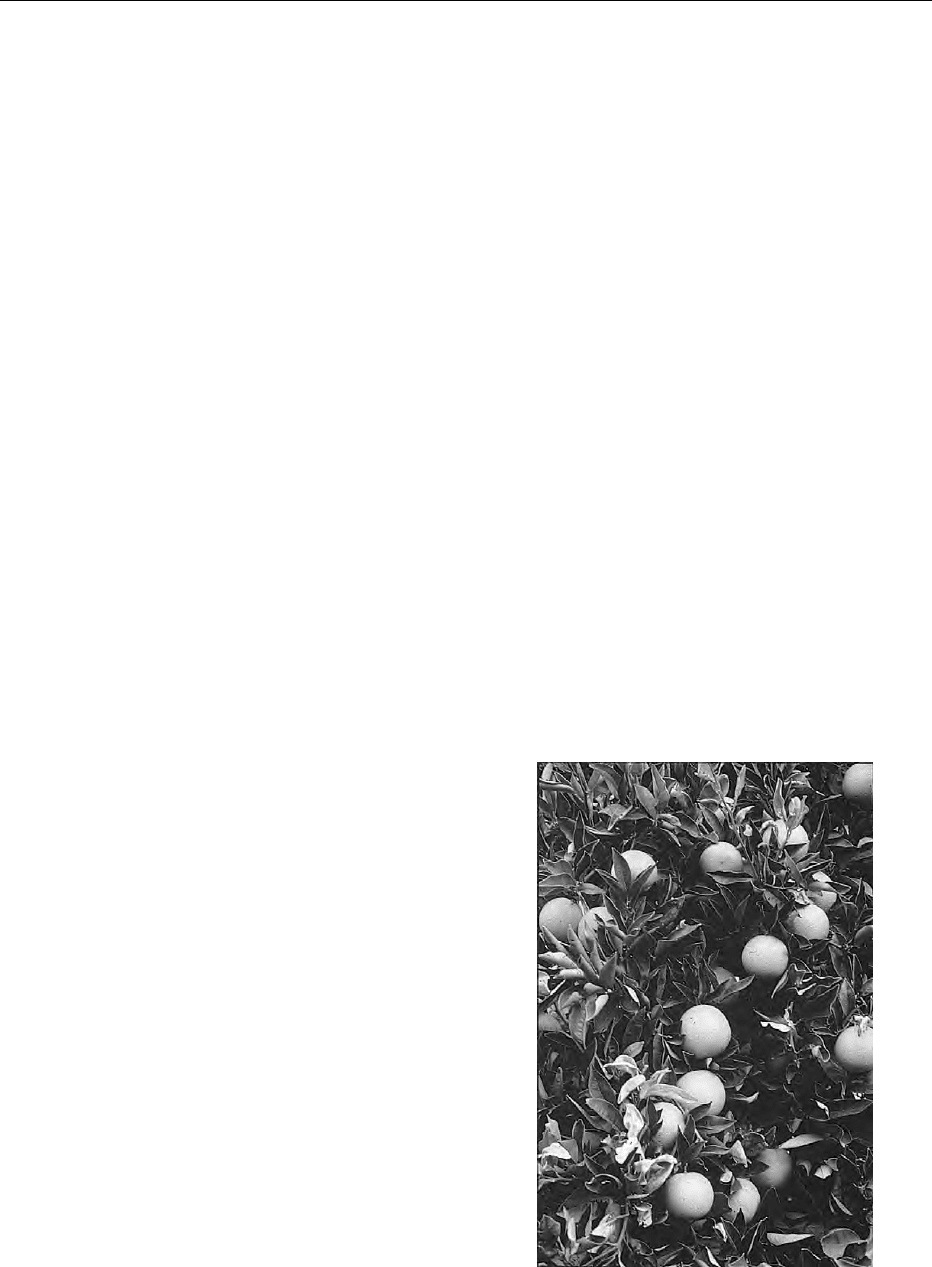
fig0001Figure 1 (see color plate 25) Navels are the most important
sweet, juicy, and seedless orange marketed for fresh fruit
consumption.
1330 CITRUS FRUITS/Types on the Market
Mandarins
0013 Mandarins are also referred to as ‘tangerines’ in some
countries. The mandarin group and related hybrids
is very diverse (with over 100 cultivars), but can
be classified into a number of main groups, some of
which contain a large number of subgroups. This fruit
is more seasonal, with each cultivar maturing and
suitable for harvesting only over a short period of
time, e.g., 6–8 weeks. Some are now available for
the main types that can supply fresh fruit from very
early to very late maturity. Mandarins production is
increasing with a consumer trend towards easier to
peel, segment, and seedless lunch/eaten out of hand
fruit, while limited quantities are processed into juice
or canned segments.
.
0014 Satsuma mandarins (C. unshiu Marcovitch) are
also known as ‘Unshiu mikan’ in Japan and
China. This is an important expanding seedless
group that includes Clausellina, Miho, Miyagawa
and Okitsu.
.
0015 Common mandarins (C. reticulata Blanco) are a
very extensive group of different cultivars widely
grown and available in world markets, e.g., Im-
perial, Nova, Ponkan, Sunburst, and Fortune.
The group also includes the seedless clementines
(like Marisol, Clemenules, and Hernandina), and
two hybrid groups, e.g., tangors, which are hybrids
of the mandarin and orange (like Murcott and
Ellendale), and tangelos, hybrids of the mandarin
and grapefruit or pummelo (Minneola and Sem-
inole).
.
0016 Mediterranean mandarin (C. deliciosa Tenore) is
also known as ‘Willowleaf’ and includes Avana
clones.
Lemons
0017 The lemon (C. limon [L.] Burm. f.) is an important
fresh fruit group in world markets. Even though they
are not eaten fresh, they are widely used for their acid
juice content and slices, and for processing. The main
cultivars are dual purpose and include Eureka,
Lisbon, Meyer (a hybrid), Fino, and Verna. A minor
related group of sweet or acidless cultivars and
hybrids also exists.
Limes
0018 Limes are also a varied group with a distinctive flavor
and aroma, consisting mainly of two broad sub-
groups:
.
0019 Acid limes are small fruited (C. aurantifolia Swing)
with West Indian, Mexican, or Key lime as the
main cultivar, and often also processed into cordial;
the large fruited (C. latifolia Tan) with Persian,
Tahiti, or Bearss the main cultivar, is normally
marketed as a fresh seedless fruit (Figure 2).
.
0020Sweet limes (C. limettioides Tan), also known as
the Palestine or Indian sweet lime, are insipid and
not normally attractive to Western palates.
Grapefruit
0021Grapefruit is one of the newer types (C. paradisi
Macfadyen) of citrus. It contains several distinct
groups according to the rind or flesh-colored pig-
ments:
.
0022Common or white fleshed, with Marsh (seedless)
the main cultivar.
.
0023Pigmented, where the older cultivars were con-
sidered ‘pink’-fleshed (with Thompson and Ruby
the main cultivars), while newer selections, muta-
tions or cultivars bred in the USA are now classified
as ‘red’-fleshed, due to the deeper pigmentation in
both the rind and flesh while also being seedless.
From this group, Star Ruby, Flame, and Rio Red are
becoming important in world markets (Figure 3).
A recent breeding program in California, where an
acidless pummelo was crossed with a white seedy
grapefruit, has resulted in the selection and release
of two new low-acid seedless grapefruit type cultivars
– Melogold and Oroblanco (also called ‘Sweetie’ in
Israel and some other countries).
Growing Regions and Conditions
0024Production regions are located in a wide range of
climatic conditions, including the humid tropics,
arid subtropics and intermediate climates. Commer-
cial production tends to be located in two narrow
belts in the subtropics and between 20 and 40
latitude north and south of the equator.
fig0002Figure 2 (see color plate 26) Limes are normally harvested for
fresh marketing when mature but with green or light green to
silver-colored rinds.
CITRUS FRUITS/Types on the Market 1331
0025 Citrus grows best in cooler, frost-free, Mediterra-
nean-type climates, provided that the soils are suit-
able and rainfall is at least 1200 mm, distributed
evenly throughout the year, or supplemented by irri-
gation. Climate can significantly affect yield, fruit
quality, and tree health. In particular, minimum tem-
peratures and degrees of frost restrict commercial
production within many countries of the world.
0026 Some cultivars have been bred or selected that
extend production into marginally cooler climates,
e.g., satsuma mandarins in Japan and China. Limes
and pummelos grow well in tropical areas, where the
normal rind color of oranges does not develop. High-
quality grapefruit tend to be grown in hot desert
areas.
Production Statistics
0027 Commercial citrus production has been recorded by
the FAO in over 100 different countries and through
out six regions – Africa, North America, South Amer-
ica, Asia, Europe (Mediterranean), and Oceania.
The world’s citrus production has been gradually in-
creasing through a 3-year average of 87 980 10
3
t
in 1995–1998, to a slightly smaller total crop of
82 166 10
3
t in 1998–1999, as shown in Table 1.
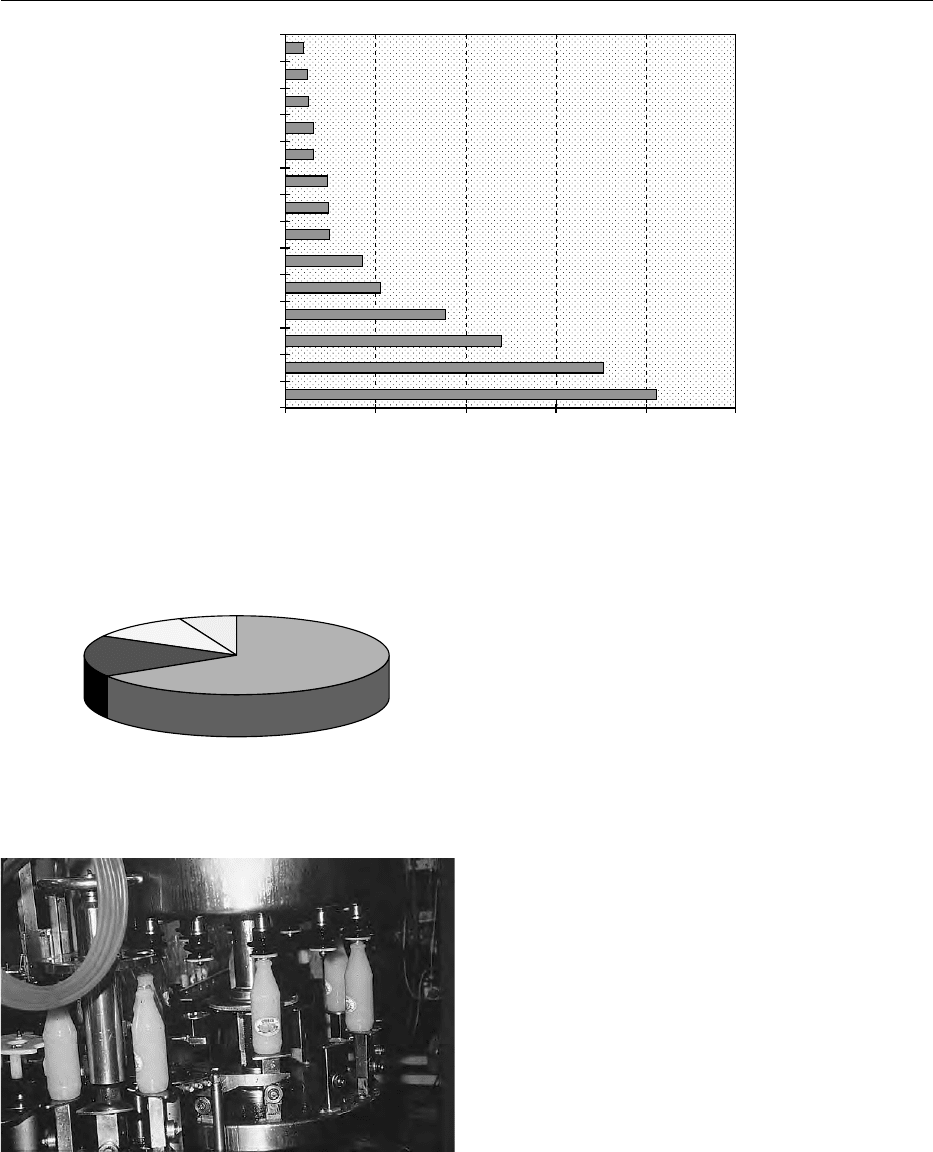
The production for the main types for 1998–1999
is shown in Figure 4. ‘Other’ citrus types totaled
only 5124 10
3
t, with the majority recorded in
Asia. The 4-year 1995–1999 production trends and
percentage of the main citrus types grown are shown
in Figure 5.
0028The largest growing areas are located in the
northern hemisphere, where 68% of world produc-
tion occurs, and include the important Mediterranean
region with 20%, e.g., Spain, Egypt, Italy and the
USA, China, and Mexico, whereas the southern hemi-
sphere (32%) includes the largest producer in the
world – Brazil, together with Argentina and South
Africa. Nonspecified areas of citrus production with
just over 16 000 10
3
t in 1998–1999 would mainly
occur in the subcontinent (especially India) and Asia.
0029Some regions like Japan, China, India, Mexico, and
Asia have important local or domestic markets for
their fresh citrus fruits, whereas others like Spain,
USA, South Africa, Morocco, Turkey, and Argentina
depend on exports as a major outlet for much of their
production. Table 1 indicates total world fresh fruit
exports of 11% in 1998–1999 for the main citrus
types and with FAO recording 92 countries exporting
some citrus.
0030In the two largest producing countries (Brazil and
the USA), there has been an increasing trend for a
large percentage of the production to be processed
into frozen concentrated orange juice for storage
and/or export throughout the world. The processing
of some citrus production in Spain, Argentina,
and Italy is also an important fresh juice market
(Figure 6). Overall, in 1998–1999, 27 664 10
3
t
were processed, or 34% of total citrus production
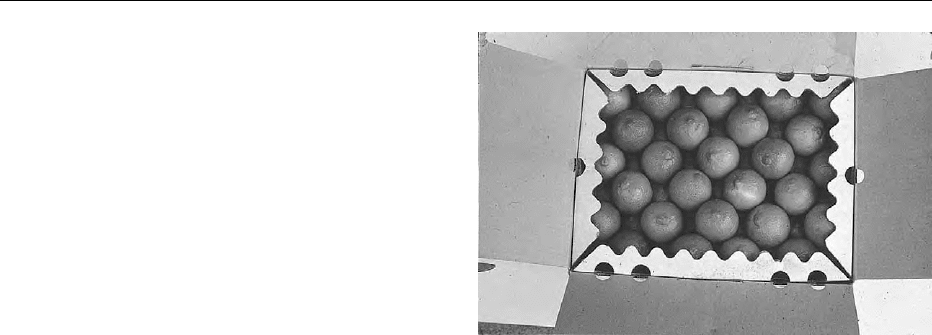
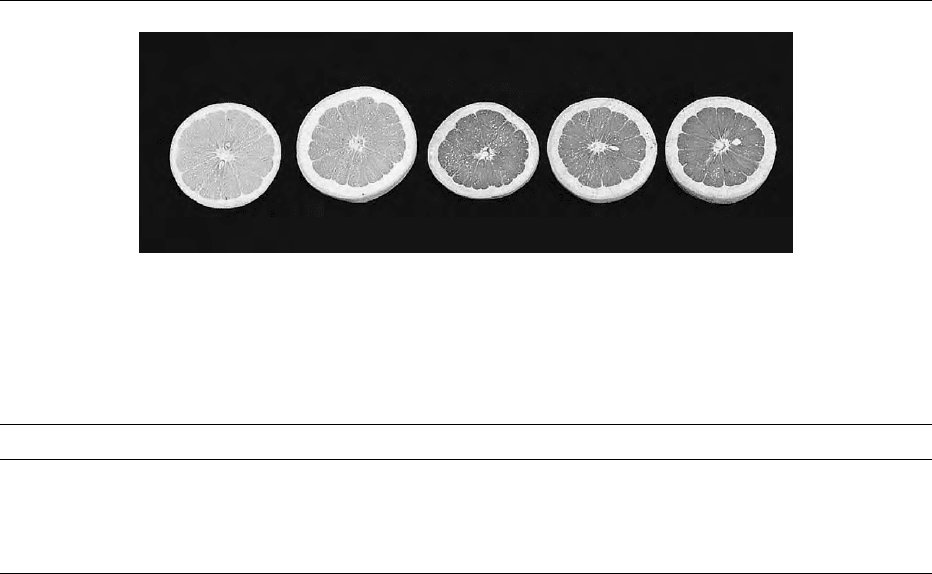
fig0003 Figure 3 (see color plate 28) A range of internal pigments are now available in grapefruit, with consumer interest in the newer red
fleshed cultivars (left to right: Marsh, Thompson, Rio Red, Flame, and Star Ruby).
tbl0001 Table 1 Fresh citrus crop production and utilization (with respective percentages), and the main producing countries of each for the
major types produced throughout the world in 1998–1999
Citrus type Totalproduction (10
3
t) % Exports (10
3
t) % Processed (10
3
t) % Main producing countries
Oranges 53 644 65 4 327 48 22 784 82 Brazil, USA, Mexico, Spain, China
Mandarins 14 463 18 2 191 24 1 206 5 China, Spain, Japan, Brazil, Korea
Lemons and limes 9 446 11 1 362 15 1 991 7 Argentina, Mexico, Brazil, Spain, Egypt
Grapefruit 4 614 6 1 135 13 1 682 6 USA, Israel, Cuba, China, Argentina
Total world 82 166 9 015 11 27 664 34 Brazil, USA, China, Spain, Mexico
1332 CITRUS FRUITS/Types on the Market
(Table 1), whereas Brazil is reported to have pro-
cessed 73% of their total orange production in
1989–1999, and the USA 88%.
Utilization of Lesser-Known Citrus Types
0031Some minor and lesser-known citrus fruit types
that have fresh or processing uses and have some
market importance in different countries or regions
of the world are listed in alphabetical order. In
many situations, local names exist for some of these
types.
Bergamot (
C. bergamia
Risso)
0032This appears to be a variant of the sour orange and is
mainly grown for its unique aromatic rind oil or
essence in the coastal region of Calabria, a province
of Italy. This essence is widely used in the food trade
and in confectionery, and as an aroma for liqueurs,
teas, sweets, and candied fruit.
Calamondin (
C. madurensis
Loureiro)
0033This resembles the mandarin and is grown extensively
in the Orient, China, Taiwan, Japan, and the Philip-
pines (where it is known as the ‘Calamonding’ or
‘Kalamansi’). The fresh fruit is sour but is widely
used for processing and as an ornamental tree.
Citrons (
C. medica
L.)
0034Like the other members of the acid group of lemons
and limes, these also have two classes, the acid and
the sweet, each with several cultivars. Citron are
principally used for candied peel, but the etrog citron
is also used in Jewish religious ceremonies. The
Fingered Citron or Buddha’s Hand, has an unusual
appearance, with a distinctive and pervasive aroma,
fig0006 Figure 6 Juicing of oranges into various products is an import-
ant market in many countries. Fresh juice and citrus drinks are
normally sold in consumer convenience packs.
Greece
South Africa
Morocco
Japan
Turkey
Italy
Argentina
Egypt
Mexico
Spain
China
USA
Brazil
Rest of World
0 100005000 15 000 20 000 25 000
'000 tonnes
fig0004 Figure 4 World citrus production, 1998–1999 for major producers and the rest of the world (which includes Cuba, Israel, Australia,
Venezuela, South Korea, Lebanon, Uruguay and Cyprus).
Grapefruit
6%
Lemons/limes
11%
Mandarins
17%
Oranges
66%
fig0005 Figure 5 (see color plate 27) Average production percentages
for the main citrus types grown in the world between 1995 and
1996 and between 1998 and 1999.
CITRUS FRUITS/Types on the Market 1333
and is also used in religious ceremonies, perfuming
rooms, and clothing for its medicinal values, and
serves to highlight fruit-bowl arrangements.
Kaffir Lime (
C. hystrix
DC)
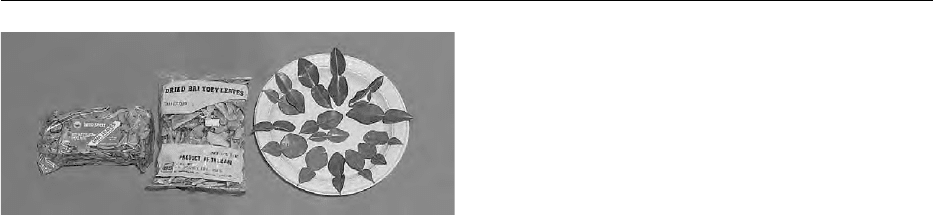
0035 This belongs to the subgenus Papeda and is not a true
‘lime,’ but as the Kaffir lime is widely grown in Thai-
land, Philippines, Malaysia, Indonesia, and generally
throughout Asia. It has unusual looking leaves
(having a large winged petiole, see Figure 7) that are
used (fresh or dried) with the fruit rind (as the fruit is
normally not eaten) as a seasoning, flavoring, and
garnishing in Asian food or recipes.
Kumquats (
Fortunella
spp.)
0036 Also known as ‘cumquats,’ these are the smallest of
the true citrus fruits. They can be eaten as fresh fruit
or marmalade, or can be brandied. Several distinct
cultivars that bear edible fruits are known:
.
0037 Nagami or oval kumquat (F. margarita [Lour.]
Swing)
.
0038 Marumi or round kumquat (F. japonica [Thumb.]
Swing)
.
0039 Meiwa or large round kumquat (F. crassifolia
Swing).
Several minor kumquats are also grown mainly for
ornamental purposes, e.g., Hong Kong (F. hindsii
Swing) and Malayan (F. polyandra Tan).
Pummelo (
C. grandis
[L.] Osbeck)
0040 This is also known as ‘shaddock’ or ‘pomelo’ and
is the largest of the citrus fruits. Because pummelo
hybridizes very readily, this has resulted in acid, acid-
less or sweet, pigmented or nonpigmented flesh, seedy
or seedless cultivars being grown. This citrus type is
common in some Asian countries, e.g., Thailand,
China, and Indonesia, but is not common in Western
countries or in world markets. It is usually eaten as a
spooned desert fruit.
Sour oranges (
C. aurantium
L.)
0041Also known as bitter oranges, sour oranges are nor-
mally used for processing (marmalade or rind oil to
flavor soft drinks and liqueurs). Most cultivars can be
classified into three groups:
.
0042Common, bitter, or sour oranges, of which the
Seville (rough or smoothed skinned) is the most
important.
.
0043The bittersweet orange is a subgroup of the above
common sour orange but has a lower acidity and
better flavor.
.
0044Variant bitter oranges or Bouquetiers are an
important perfumery cultivar.
Conclusion
0045Many types of citrus fruits and processed products
are now widely available throughout the world from
local production or importation to supplement local
supplies or in non-producing countries. Citrus is
mainly consumed as fresh fruit, with their distinctive
refreshing appeal and flavor, while also being a
healthy, enjoyable, convenient and nutritious food.
The fruit is also an excellent source of vitamins,
minerals, dietary fiber and still low in kilojoules.
Some fruit are used extensively to garnish food,
while many processed products especially juices, cor-
dials and marmalades are also widely available and
consumed.
See also: Ascorbic Acid: Properties and Determination;
Physiology; Citrus Fruits: Composition and
Characterization; Processed and Derived Products of
Oranges; Jams and Preserves: Methods of Manufacture;
Chemistry of Manufacture
Further Reading
Cottin R (coordinator) (1997) Citrus of the World A Citrus
Directory. San Giuliano, France: SRA INRA-CIRAD.
FAO (1999) Citrus Fruit Fresh and Processed, Annual Stat-
istics, Tables 1–10 and 16–20. Rome: Food and Agricul-
ture Organization.
Reuther W, Webber HJ and Batchelor LD (eds) (1967) The
Citrus Industry, vol. 1. Berkley, CA: University of
California.
Saunt J (1990) Citrus Varieties of the World. Norwich, UK:
Sinclair International.
Sinclair WB (1984) The Biochemistry and Physiology of the
Lemon and other Citrus Fruits, pp. 711–718. Berkley,
CA: University of California.
Swingle WT and Reece PC (1967) The Botany of Citrus and
its Wild Relatives. In: Reuther W, Webber HJ and Batch-
elor LD (eds), vol. 1. The Citrus Industry. Berkley, CA:
University of California.
fig0007 Figure 7 Fresh or dried Kaffir lime leaves are an important
garnish in many Asian recipes. (Market packaged dried leaves
(L) and freshly picked leaves showing their distinctive shape
(R) ).
1334 CITRUS FRUITS/Types on the Market

Young RH (1986) Fresh Citrus Cultivars. In: Wardowski
WF, Nagy S and Grierson W (eds), pp. 110–125. Fresh
Citrus Fruits. Westpoint, CT: AVI Publishing.
USDA (1999) World Fresh Citrus Situation. In: World
Horticultural Trade and US Export Opportunities, Cir-
cular Series FHORTH, pp. 18–32. USA: Foreign Agri-
cultural Service.
Composition and
Characterization
L Izquierdo, Formerly of Consejo Superior de
Investigaciones Cientı
´
ficas, Valencia,
Spain
J M Sendra, Instituto de Agroquı
´
mica y Technologı
´
ade
Alimentos, Valencia, Spain
This article is reproduced from Encyclopaedia of Food Science,
Food Technology and Nutrition, Copyright 1993, Academic Press.
Introduction
0001 Citrus fruits are one of the largest fruit crops in the
world. About 30% of citrus fruits is processed to
obtain various products, mainly juice. Similarly, the
citrus industry is also the second largest fruit-
processing industry, surpassed again by the grape
industry, which mainly produces wine. Neither
orange juice nor wine can be considered essential
foods but they do have an important role in our lives.
0002 Although citrus fruits have been consumed since
ancient times, citrus processing, as it is known
today, was not possible until thermal treatment (to
inactivate enzymes and microorganisms) and concen-
tration processes were commercially available. Since
then, the citrus industry has developed rapidly, be-
coming prominent among food industries.
0003 Although consumption of fresh citrus fruits is
popular in all producing countries, processed prod-
ucts must still be considered almost as luxury prod-
ucts. Breakfast with orange juice is only common in
developed countries. Thus, citrus industries process
value-added products whose quality, nutritional char-
acteristics, and purity are appreciated. Since these
three aspects are closely related to composition, the
analysis of citrus constituents is a frequent subject of
research work, supported by governments and indus-
tries.
0004 This article covers the most important aspects of
citrus fruit composition, its relationship to nutritional
value, and its importance for product authentication.
Several books have been published on these subjects
and the Further reading section lists some of them as
well as published composition tables.
Constituents
0005The genus Citrus has many species and the differences
among them are of great interest to specialists. How-
ever, from a general point of view, the similarities are
greater than the differences, which is not surprising
when considering species of the same genus. The
economic importance also differs among species and
compositional studies of the main species are more
frequent. Thus, data from Citrus sinensis (sweet
orange) are more extensive than from C. reticulata
(tangerine), C. limon (lemon), or C. paradisi (grape-
fruit), and data from these species are more compre-
hensive than from other Citrus species. Within each
species some varieties are better known than others.
Valencia orange is the best-studied sweet orange,
since it is the most important variety for juice extrac-
tion, the main citrus product. Thus, most information
given here will refer to the juice rather than to the
fruit, since juice, accounting for about half of the total
weight of an orange, is the most important part of
the fruit, and is the part of the fruit mainly consumed
by humans.
0006Orange peel constitutes most of the other half of
the fruit, but peel is of much less importance than
juice. Although some byproducts (cattle feed, molas-
ses) are obtained from peel, it is more a question of
removing residues and avoiding pollution than of
economic interest. Only peel oil (obtained before or
during juice obtention) and pectins (obtained only
from suitable species and varieties) are important
peel products for human consumption, perfumery,
and cosmetics.
0007Our knowledge of the chemical composition of
juice and fruits is being continuously improved. The
efficiency of instrumental methods of analysis allows
the rapid identification of more and more minor con-
stituents. But the basic major constituents have been
well known since the application to citrus research of
classical methods of analysis, which are still of inter-
est for some rapid determinations. Both types of
methods will be considered in this article, but it
must be pointed out that analysis is a dynamic
discipline and methods (mainly instrumental) are
continuously being improved. Many of those which
seem almost perfect today will look old-fashioned
tomorrow.
0008Citrus fruit parts are represented schematically in
Figure 1, and the approximate constitution of oranges
is shown in Table 1. Juice vesicles, located in the
endocarp, contain the juice, which constitutes about
50% of the total weight of a typical orange fruit. The
peel is formed by the flavedo (epicarp and outer
mesocarp) and the albedo (inner mesocarp). Flavedo
and albedo account, respectively, for about 10 and
CITRUS FRUITS/Composition and Characterization 1335
