Bongard Frederic , Darryl Sue. Diagnosis and Treatment Critical Care
Подождите немного. Документ загружается.

TRANSFUSION THERAPY
87
serve to promote rational use of blood products for the ben-
efit of patients as well as protecting the limited supply of
blood from waste. These trials have clearly influenced trans-
fusion practices in well-defined clinical situations. There are
many situations, however, where no empirical data exist, and
the clinician must determine the benefits of transfusion on
an individualized basis. Massive repeated transfusion in
patients with uncorrectable vascular defects or who are ter-
minally ill—and platelet and plasma transfusions for
patients without demonstrated response to such
transfusions—may deplete the blood supply without sub-
stantially improving the outcome for those patients.
The medical team caring for a patient with massive
uncontrollable bleeding or a terminal illness should make
every effort to discuss the limits of care with the patient and
family members, to establish long-term treatment goals and
expectations, and to decide when continued blood transfu-
sion is no longer of benefit to the patient. In addition, family
members should be strongly encouraged to donate blood to
help replace some of the units used. Ineffective therapy
should not be given prophylactically (eg, daily platelet trans-
fusions in patients with consumptive thrombocytopenia
without bleeding or plasma therapy in patients with multiple
severe coagulation deficiencies not corrected with large doses
of plasma).
REFERENCES
Boshkov LK: Transfusion-related acute lung injury and the ICU. Crit
Care Clin 2005;21:479–95. [PMID: 15992669]
Circular of Information for the Use of Human Blood and Blood
Components; from www.fda/gov/cber/dglns/crclr.pdf.
Corwin HL et al: Efficacy and safety of epoetin alfa in critically ill
patients. N Engl J Med 2007;357:965–976. [PMID: 17804841]
Davenport RD: Pathophysiology of hemolytic transfusion reactions.
Semin Hematol 2005;42:165–8. [PMID: 16041666]
Drews RE: Critical issues in hematology: Anemia, thrombocytope-
nia, coagulopathy, and blood product transfusions in critically ill
patients. Clin Chest Med 2003;24:607–22. [PMID: 14710693]
Gajic O et al: Pulmonary edema after transfusion: How to differ-
entiate transfusion-associated circulatory overload from
transfusion-related acute lung injury. Crit Care Med 2006;34:
S109–13. [PMID: 16617253]
Goodnough LT, Shander A, Brecher ME: Transfusion medicine:
Looking to the future. Lancet 2003;361(9352):161–9. [PMID:
12531595]
Goodnough LT: Risks of blood transfusion. Crit Care Med
2003;31(suppl 12):S678–86. [PMID: 14724466]
Hebert PC, Tinmouth A, Corwin HL: Controversies in RBC transfu-
sion in the critically ill. Chest 2007;131:1583–90. [PMID:
17494811]
Hebert PC et al: A multicenter, randomized, controlled clinical trial
of transfusion requirements in critical care. N Engl J Med
1999;340:409–17. [PMID: 9971864]
Hebert PC: Clinical consequences of anemia and red cell transfusion
in the critically ill. Crit Care Clin 2004;20:225–35. [PMID:
15135462]
Hellstern P: Solvent/detergent-treated plasma: Composition, effi-
cacy, and safety. Curr Opin Hematol 2004;11:346–50. [PMID:
15666659]
Hill SR et al: Transfusion thresholds and other strategies for guiding
allogeneic red blood cell transfusion. Cochrane Database Syst Rev
2002;2:CD002042. [PMID: 12076437]
Lauzier F: Fresh frozen plasma transfusion in the critically ill. Crit
Care Med 2007;35:1655–9. [PMID: 17522577]
McIntyre L et al: Is a restrictive transfusion strategy safe for resusci-
tated and critically ill trauma patients? J Trauma 2004;57:563–8.
[PMID: 15454803]
Napolitano LM, Corwin HL: Efficacy of red blood cell transfusion in
the critically ill. Crit Care Clin 2004;20:255–68. [PMID:
15135464]
Ohene-Frempong K: Indications for red cell transfusion in sickle cell
disease. Semin Hematol 2001;38(1 suppl 1):5–13. [PMID:
11206961]
Rao SV et al: Relationship of blood transfusion and clinical out-
comes in patients with acute coronary syndromes. JAMA
2004;292:1555–62. [PMID: 15467057]
Schiffer CA et al: Platelet transfusion for patients with cancer:
Clinical practice guidelines of the Society of Clinical Oncology. J
Clin Oncol 2001;19:1519–38. [PMID: 11230498]
Shander A: Anemia in the critically ill. Crit Care Clin 2004;20:
159–78. [PMID: 15135458]
Silliman CC, Ambruso DR, Boshkov LK: Transfusion-related acute
lung injury. Blood 2005;105:2266–73. [PMID: 15572582]
Klein HG, Spahn DR, Carson JL: Red blood cell transfusion in clini-
cal practice. Lancet 2007;370(9585):415–26. [PMID: 17679019]
Stanworth S et al: Prophylactic platelet transfusion for haemorrhage
after chemotherapy and stem cell transplantation. Cochrane
Database Syst Rev 2004;18:CD004269. [PMID: 15495093]
Stubbs JR: Alternatives to blood product transfusion in the critically
ill: Erythropoietin. Crit Care Med 2006;34:S160–9. [PMID:
16617261]

88
Critically ill patients are almost always given many different
drugs. For example, patients may require broad-spectrum
antibiotics, vasopressor agents, and antiarrhythmics. At the
same time, clinicians often must give sedatives and muscle
relaxants to patients in order to tolerate mechanical ventila-
tion, and there is strong evidence that ICU outcome is
improved by empirical prophylaxis for GI bleeding with pro-
ton pump inhibitors or other antacids and prophylaxis for
deep venous thrombosis with heparin.
One estimate is that ICU patients receive twice as many
different drugs as other hospitalized patients. It is no wonder,
therefore, that medication errors, a major focus of hospital
safety improvement, are increased in ICU patients. In fact, an
error in preparation, dosage, or rate of infusion has been
found in as many as 10% of intravenous medications.
Furthermore, complex changes in pharmacokinetics and
pharmacodynamics are seen frequently in these patients,
necessitating consideration of dosage, interaction, and organ
function.
Pharmacokinetics is the movement of a drug through the
body over time and is defined by the following: absorption,
distribution, metabolism, and elimination—basically, how
the patient affects a drug. Pharmacodynamics is the relation-
ship between drug concentration and drug effect—or how a
drug affects the patient. Both pharmacokinetic and pharma-
codynamic changes compared with baseline occur in critical
illness and the management of patients in the ICU.
PHARMACOKINETIC PARAMETERS
The most important pharmacokinetic parameters are clear-
ance and volume of distribution. The disposition of a drug,
once it has entered the body, depends on both clearance (CL)
and the volume of distribution (V
d
). Clearance is propor-
tional to the rate at which a drug is eliminated from the body.
Volume of distribution is a theoretical volume that relates
the concentration in the plasma to the total amount of drug
in the body. The elimination half-life (t
1/2
) depends on the
preceding independent variables and is described by the fol-
lowing mathematical relationship:
t
1/2
= (0.693 × V
d
/CL)
Hence either decreased clearance or an expanded volume
of distribution will result in an increased pharmacologic
half-life. A practical understanding of this mathematical
relationship is essential for developing optimal dosing regi-
mens in the critically ill patient.
PHARMACOKINETIC CONSIDERATIONS
Absorption
Drug absorption is influenced by a variety of factors, includ-
ing the site of absorption, the amount metabolized before
reaching the systemic circulation (“first-pass” effect for orally
administered drugs), and drug interactions. In critical illness,
the site of absorption is of utmost importance. The extent of
oral absorption—bioavailability—may be diminished as a
result of low cardiac output or shunting of blood from the
mesentery to the peripheral circulation. In patients who are in
the ICU for a longer duration, intestinal atrophy and motility
dysfunction may play a role. While highly encouraged in suitable
patients, enteral nutritional support may cause inadvertent mal-
absorption of some orally administered medications. Therefore,
therapeutic “failures” may be due to inadequate bioavailability
rather than absence of effect at the intended receptor site.Acutely
ill patients may have decreased perfusion of sites of parenteral
administration of drugs. These patients may have poor or unreli-
able absorption of subcutaneously or intramuscularly adminis-
tered medications. In general, the intravenous route is preferred
for critical medications, and oral, subcutaneous, or intramuscu-
lar administration should be avoided.
4
Pharmacotherapy
∗
Darryl Y. Sue, MD
∗
Jennifer H. Cupo Abbott, PharmD, and Maria I. Rudis, PharmD,
were the authors of this chapter in the second edition.
Copyright © 2008 by The McGraw-Hill Companies, Inc. Click here for terms of use.
PHARMACOTHERAPY
89
Distribution
The distribution of drugs in the body depends on factors such
as blood flow, body composition, and plasma protein binding
(Table 4–1). For a single-compartment model, initial plasma
concentration (before elimination) equals the dose of drug
given divided by the apparent volume of distribution. In nor-
mal subjects, the volume of distribution of a drug is generally
well described and usually is related to some measure of
patient size (eg, total body water for a water-soluble drug and
extravascular volume for a large molecule). However, volume
of distribution is strongly influenced by drug lipid solubility,
protein binding, and intra- versus extracellular partitioning.
In critical illness, fluid overload can increase a patient’s
volume of distribution significantly, and insufficiently
effective drug concentrations may result. For drugs with
extensive tissue distribution (eg, digoxin), the volume of
distribution is approximately 500 L, or several times actual
body weight. Thus it is unlikely that changes in fluid status
can affect the distribution of digoxin significantly. For
drugs apparently distributed largely into extracellular
water, however, drug concentrations can be affected. It is
not uncommon for a critically ill patient to gain several
kilograms of extracellular water (ECW). Because this space
is roughly 20% of body weight, or about 12 L in a 60 kg
adult, gaining even 2 L of ECW would reduce expected con-
centration of such a drug by 15–20%. A drug such as gen-
tamicin exhibits concentration-dependent killing of
bacteria. A peak level of 25 μg/kg (dose = 5–7 mg/kg, nor-
mal V
d
= 0.25 L/kg) is expected. However, V
d
in critically ill
patients may be as high as 0.6 L/kg, resulting in a much
lower than expected serum level.
Body composition and the lipophilicity of a given drug
are also important factors to consider. In general, lipophilic
agents such as diazepam readily distribute into fat. For these
agents, dosing should be based on total body weight. Since
most agents used in the ICU setting are not lipophilic, such
as pressors and most antimicrobials, it may be more accu-
rate to use ideal body weight in dosing calculations.
However, an increasingly important question is how to
adjust medication dosages for obese patients because the
volume of distribution likely will change. Considerations
include unexpected changes in the proportion of adipose
tissue compared with total body weight, thereby changing
estimates of total body and extracellular water, and some-
times the difficulty in obtaining accurate scaled weights.
Analgesics, including opiates, and sedatives should be
titrated to desired clinical effect in the absence of studies of
weight-adjusted dosing. Antibiotic dosing should be guided
by therapeutic drug monitoring when possible, adjusting for
both desired antimicrobial effect and toxicity. Low-
molecular-weight heparin is a special situation because the
effect when dosed as milligrams per kilogram is no longer
predictable in the obese patient; in this case, measurement
of factor Xa activity may be useful.
Protein binding is another important determinant of dis-
tribution. Only the unbound fraction of a drug can diffuse or
be transported into tissues. Thus the influence of protein
binding is a limiting factor in drug distribution for highly
bound drugs (see Table 4–1). Serum pH, often abnormal in
critically ill patients, also may affect the degree of protein
binding of drugs. Phenytoin is a highly protein-bound drug
(~90%). The remaining 10% circulates as unbound or “free”
drug and is the fraction responsible for the pharmacologic
effect. If a patient with normal albumin has a phenytoin level
of 12 mg/L, the free fraction would be approximately 1.2 mg/L.
However, with decreased serum albumin, as is found in
patients with CNS trauma or those with end-stage liver dis-
ease, less serum protein is available to bind phenytoin. The
laboratory reports total phenytoin concentrations, which
includes bound and unbound drug. In a patient with hypoal-
buminemia, the total phenytoin level will be unchanged, but
the percentage of “free” drug (ie, pharmacologically avail-
able) will increase. For example, a patient with a serum albu-
min of 2 g/dL and a measured phenytoin plasma concentration
(C
meas
) of 12 mg/L has more free drug, resulting in an adjusted
phenytoin plasma concentration (C
adj
) of 24 mg/L.
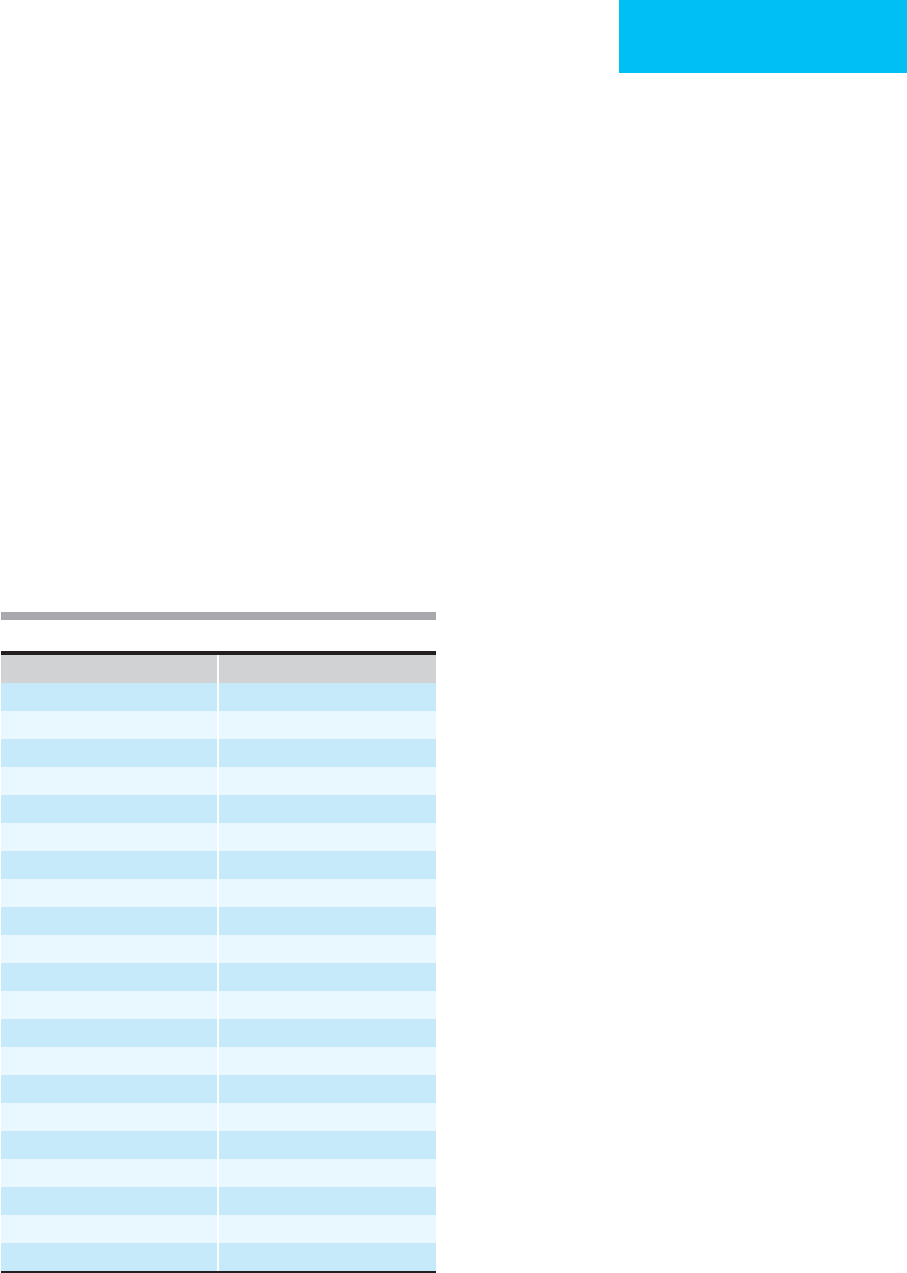
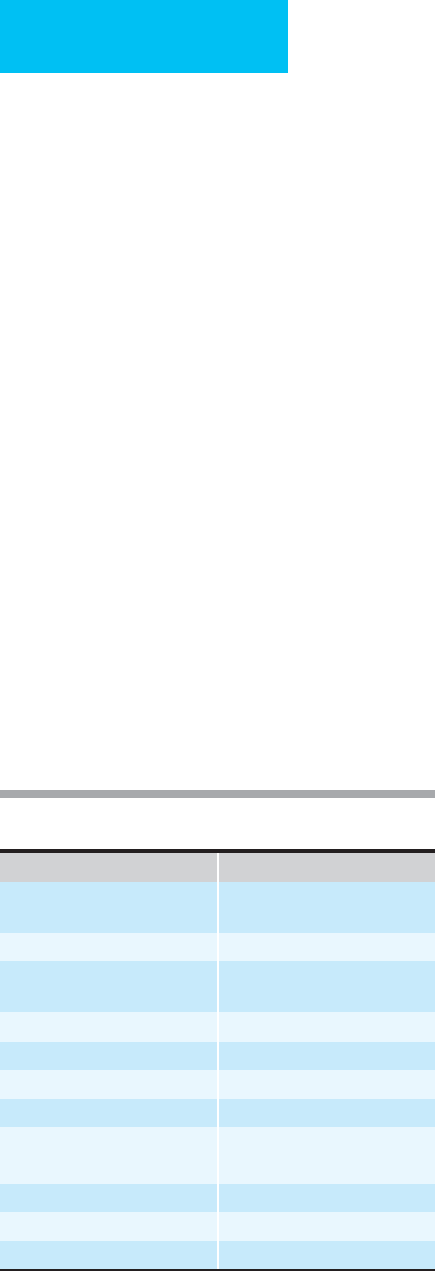
Drug Protein-Bound
Amphotericin B 90–95%
Ceftriaxone 93–96%
Chlordiazepoxide 94–97%
Clindamycin 93%
Diazepam 84–98%
Erythromycin 96%
Ethacrynic acid 95%
Furosemide 91–99%
Haloperidol 90–92%
Heparin >90%
Hydralazine 90%
Lorazepam 90%
Midazolam 94–97%
Nafcillin 70–90%
Nifedipine 89–92%
Oxacillin 89–94%
Phenytoin 90%
Prochlorperazine 90%
Rifampin 84–91%
Vecuronium 60–90%
Verapamil 90%
Table 4–1. Protein binding.
CHAPTER 4
90
The uremia accompanying renal failure also displaces
phenytoin from its binding sites because endogenous com-
petitors for binding accumulate. It is important to recognize
that malnourished patients and those with renal failure
will have a lower than normal “therapeutic range” for
phenytoin. For this reason, it is clinically more relevant to
monitor free phenytoin concentrations or to use these values
in calculation of dosage adjustments.
Drug Clearance (Elimination)
With limited exceptions, most pharmacologic agents are
eliminated either renally or hepatically, but drug clearance is
considered the effect of all pathways of elimination taken
together. Since multiorgan dysfunction is commonly
encountered in critically ill patients, drug accumulation and
toxicity are of concern. Specific dosage adjustment is often
required in the setting of renal or hepatic impairment. Some
of the most frequently used agents with predominantly renal
elimination are listed in Table 4–2. Most antimicrobials,
including aminoglycosides, vancomycin, beta-lactams, and
fluoroquinolones, are eliminated primarily via the kidneys.
Although some dosage adjustment is needed when these
antimicrobials are used in critically ill patients with renal
failure, studies have found both under- and overdosing of
antimicrobial agents because of renal function considera-
tions. Importantly, the initial concentration of an antimicro-
bial drug is related to its dose and volume of distribution, not
its elimination. Therefore, the “first dose” of an antimicrobial
need not be adjusted for renal failure, only subsequent doses.
Failure to recognize this concept leads to a delay in achieving
desired therapeutic levels.
Other drugs with primarily renal elimination used in the
critical care setting are the low-molecular-weight heparins.
Currently, dosage of enoxaparin is reduced 25–50% for
patients with a creatinine clearance of less than 30 mL/min,
but not for mild or moderate renal insufficiency. Some prac-
titioners advocate monitoring factor Xa activity for these
patients. Some drugs have mixed routes of elimination and
require adjustment for both renal and hepatic function for
proper dosing.
Renal Dysfunction
Medications used in the ICU are often eliminated by the kid-
neys, and dosages are adjusted in the face of renal insuffi-
ciency. Common causes of renal insufficiency in the ICU
include chronic kidney disease, acute renal failure from
shock or hypoperfusion, exposure to nephrotoxic drugs, and
obstructive uropathy.
Several studies have demonstrated that dosing of renally
excreted drugs (cleared by glomerular filtration) is
improved when creatinine clearance rather than serum cre-
atinine concentration alone is used to estimate renal func-
tion. This is especially true in the elderly and those who are
underweight, in whom a “normal” serum creatinine concen-
tration (0.8–1 mg/dL) may be associated with significantly
reduced renal function. Less commonly, patients with rhab-
domyolysis produce more than the expected amount of cre-
atinine; in these patients, elevated serum creatinine may not
indicate decreased glomerular filtration rate (GFR). Rarely,
some medications interfere with creatinine secretion, fur-
ther dissociating the relationship between serum creatinine
and GFR.
When the serum creatinine level is known, an estimate of
creatinine clearance can be obtained to assist with dosage
adjustment using the Cockroft-Gault equation:
(For females, multiply the numerator by a factor of 0.85.)
Although this equation and several others are used fre-
quently in ICU patients and generally are better estimates
than serum creatinine alone, some studies demonstrate that
they are far from perfect. In fact, even short-term collections
() )140
72
−×
×
age weight (in kg
serumcreatinine
C
C
Alb
mg/L
(0.2)(
ad j
meas
=
+
=
(.)( ) .
02 01
12
22.0 g/dL)
mg/L
+
=
01
24
.
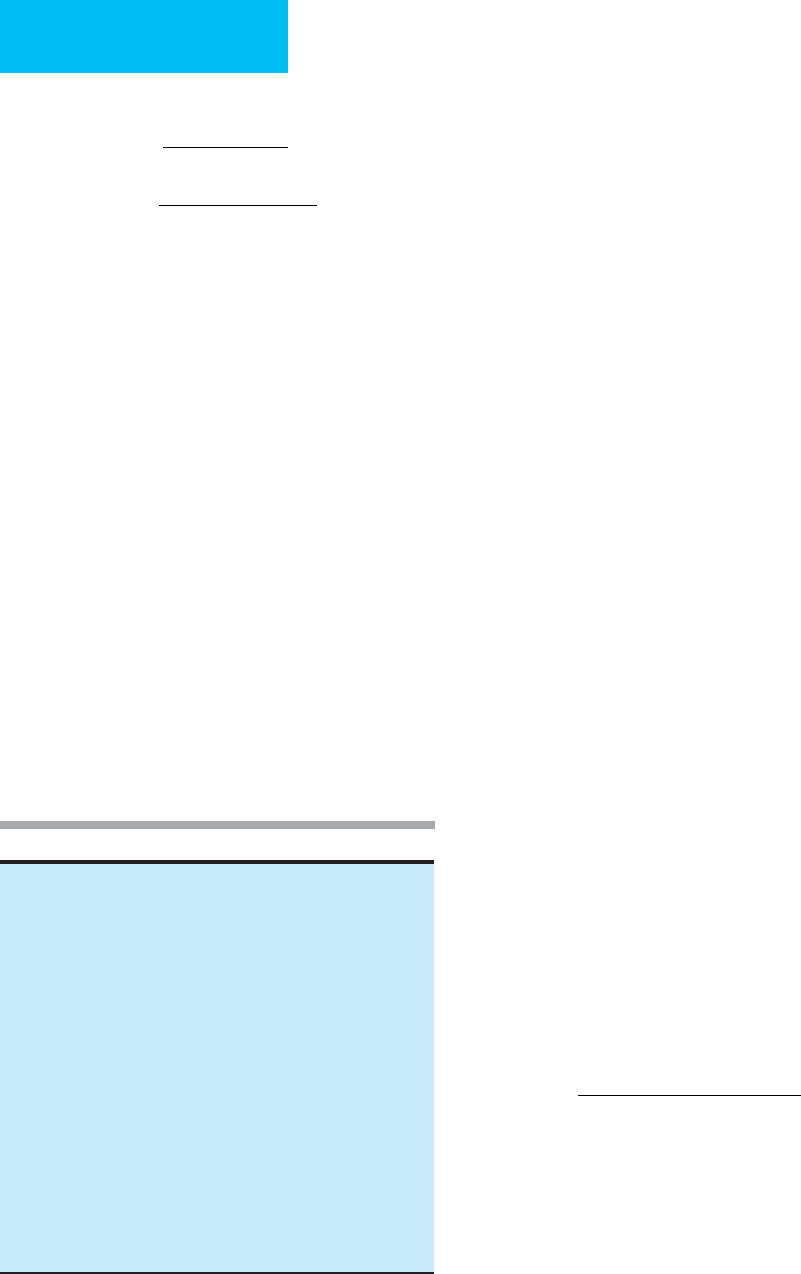
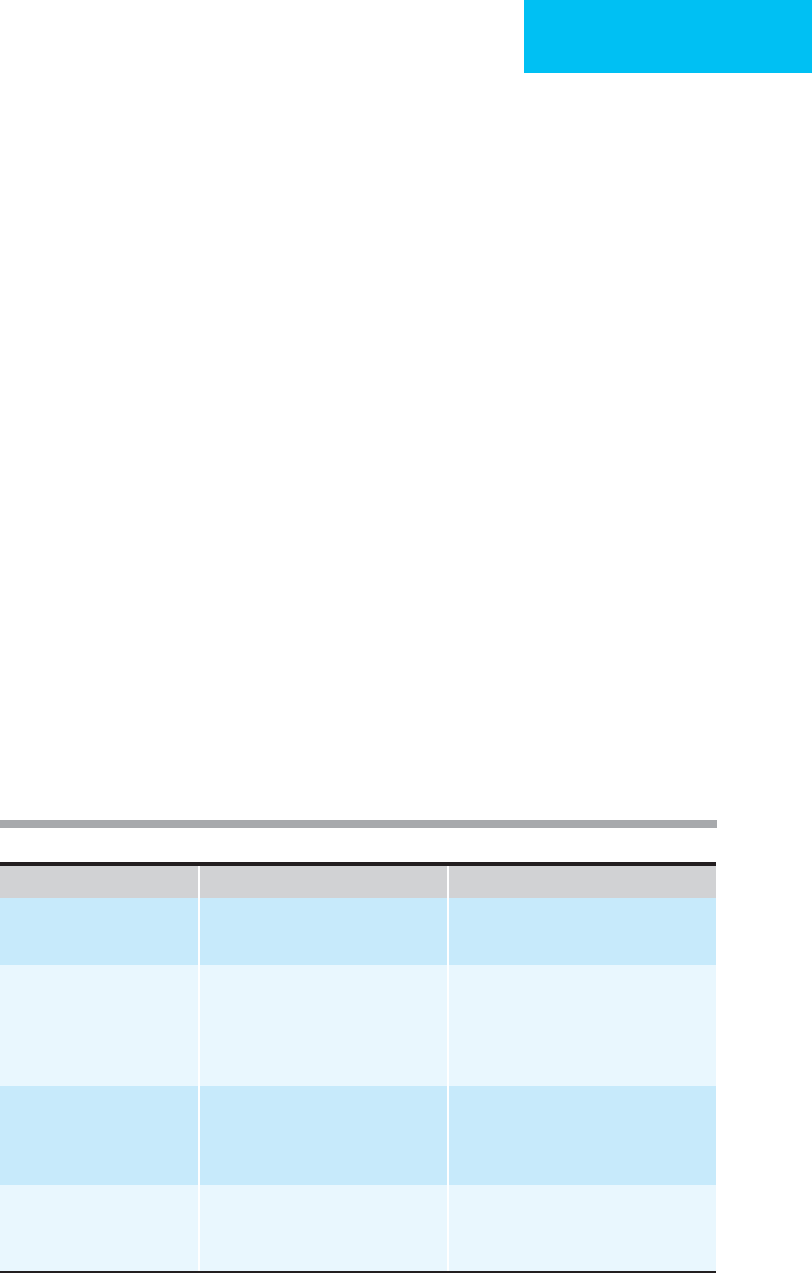
Table 4–2. Drugs with primarily renal elimination.
Antimicrobials
Acyclovir Ciprofloxacin Meropenem
Amikacin Fluconazole Penicillin G
Ampicillin Flucytosine Piperacillin
Cefazolin Ganciclovir Ticarcillin-clavulanate
Cefepime Gatifloxacin Tobramycin
Cefotetan Gentamicin Trimethoprim-sulfamethoxazole
Cefoxitin Imipenem-cilastatin Vancomycin
Ceftazidime Levofloxacin
Ceftizoxime
Antihypertensives
Diazoxide
Methyldopa
Nitroprusside
Antiarrhythmic agents
Bretylium
Digoxin
Procainamide
Miscellaneous drugs
Ranitidine
Pancuronium
of urine for calculation of creatinine clearance are less accu-
rate than 12- or 24-hour collections, probably because of
variability in GFR over time.
For patients requiring hemodialysis, it is essential to
know the extent to which drugs can be removed by dialysis.
Knowledge of pharmaceutical properties such as
hydrophilicity, molecular weight, plasma protein binding,
and volume of distribution (Table 4–3) can help to distin-
guish agents that are dialyzable. Low-molecular-weight,
water-soluble drugs with low protein binding are highly
dialyzable. If they have a small volume of distribution, then
an appreciable amount of the drug can be eliminated by
dialysis. Conversely, drugs with extensive tissue distribution
such as digoxin or the calcium channel blockers and highly
lipophilic drugs are not affected by dialysis. Other impor-
tant considerations for drug clearance include the duration
and type of dialysis. Short dialysis sessions are less likely to
remove significant amounts of drug. New forms of dialysis
are more efficient and remove drugs previously thought
to be minimally dialyzable. Hemodialysis with high-flux
filters removes significant amounts of vancomycin, previ-
ously considered not to require replacement for drug lost to
dialysis. Continuous renal replacement therapy is a much
more efficient process than conventional hemodialysis
and equates to a clearance of approximately 30 mL/min for
creatinine, but not clearly comparable for other drugs. It
is essential to review the medication regimen closely
when patients are dialyzed with high-flux filters or are
switched from hemodialysis to continuous renal replace-
ment because the dosages of some drugs will have to be
increased.
Hepatic Dysfunction
Liver failure is a common problem in the ICU and may be
due to chronic liver disease (eg, cirrhosis or hemochromato-
sis) or acute liver disease (eg, acute hepatitis, drug-induced
hepatitis, alcohol, or toxins). Some drugs require dosage
adjustment in hepatic insufficiency (Table 4–4). However,
most commonly used tests of “liver function” describe the
degree of liver damage and not the liver’s capacity for drug
elimination. Determining the degree of hepatic dysfunction
is difficult because no quantitative equations exist.
Laboratory tests of hepatic synthetic function (eg, prothrom-
bin time, serum albumin, and conjugated bilirubin) are most
predictive of drug elimination. For drugs metabolized by the
liver, the route of metabolism is important in determining
the effects of liver disease on drug clearance. Some enzyme
systems are remarkably well preserved even in end-stage liver
disease. Drugs such as lorazepam that are metabolized pri-
marily by conjugation with glucuronic acid are minimally
affected in cirrhosis, so little dosage adjustment is required.
For drugs whose clearance depends on oxidative metabolism
(eg, metronidazole, theophylline, opioids, and sedative-
hypnotics), cirrhosis reduces their elimination. Generally
speaking, acute liver disease (eg, hepatitis) does not alter
drug clearance significantly.
Congestive heart failure may cause hepatic congestion
and decreased hepatic blood flow and decrease hepatic elim-
ination of drugs. The hepatic clearance of theophylline, for
example, is markedly reduced in patients with congestive
heart failure (CHF). Patients with chronic liver disease fre-
quently have hypoalbuminemia, thereby reducing the
amount of drug protein binding. For such highly protein-
bound drugs as phenytoin, the proportion of free unbound
drug rises with hypoalbuminemia.
PHARMACOTHERAPY
91
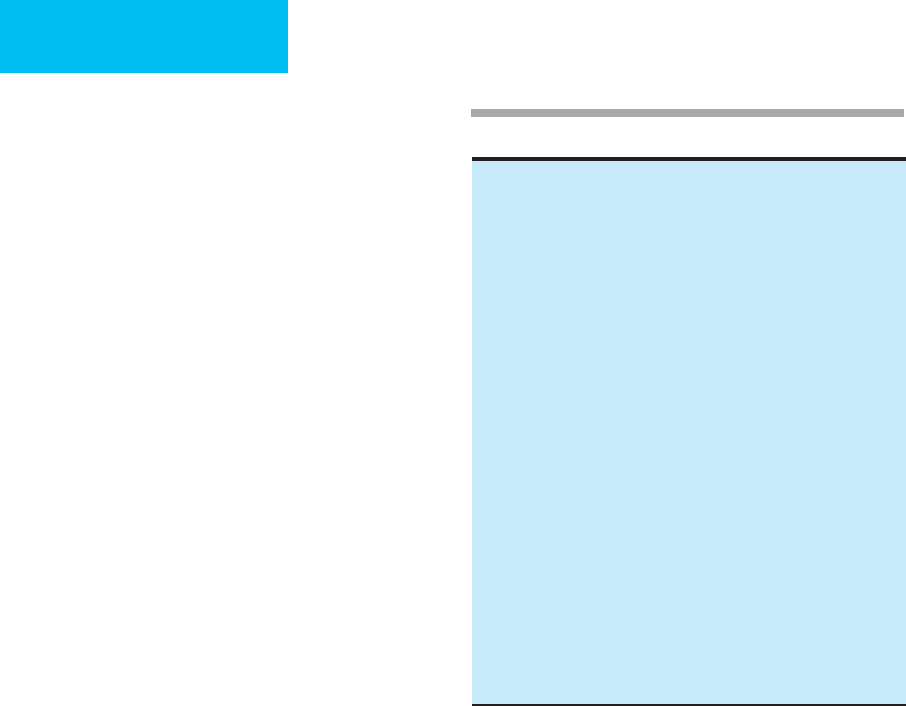
Table 4–3. Drugs significantly removed by hemodialysis.
Antimicrobials
Aminoglycosides Ceftizoxime Meropenem
Ampicillin Chloramphenicol Metronidazole
Cefazolin Ciprofloxacin Penicillin G
Cefepime Gatifloxacin Piperacillin
Cefotaxime Imipenem-cilastatin Quinupristin-
Cefotetan Levofloxacin dalfopristin
Cefoxitin Linezolid Trimethoprim-
Ceftazidime sulfamethoxazole
Antihypertensives
Diazoxide
Methyldopa
Nitroprusside
Antiarrhythmic agents
Bretylium
Digoxin
Procainamide
Miscellaneous drugs
Ranitidine
Pancuronium
Table 4–4. Drugs requiring dosage adjustment in severe
hepatic insufficiency.
Analgesics Antimicrobials
Acetaminophen Cefoperazone
Opioids Ceftriaxone
Salicylates Chloramphenicol
Antiarrhythmics Clindamycin
Lidocaine Erythromycin
Quinidine Isoniazid
Verapamil Metronidazole
Anticonvulsants Nafcillin
Phenobarbital Rifampin
Phenytoin Sedative-hypnotics
Antihypertensives Chlordiazepoxide
Hydralazine Diazepam
Labetalol Midazolam
Nitroprusside Miscellaneous
Haloperidol
Theophylline
CHAPTER 4
92
Therapeutic Drug Monitoring
Agents with a narrow therapeutic index have only a small dif-
ference between serum drug concentrations that produce
therapeutic and toxic effects, and monitoring of serum drug
concentrations is recommended (Table 4–5). Examples of
agents with low therapeutic indices are the aminoglycosides,
digoxin, theophylline, and phenytoin.
In many ICUs, routine blood samples are collected at a set
time. For therapeutic drug monitoring, this may not be
acceptable because the time the sample is drawn must be
related to the time since the last dose of the drug was given.
First, for some drugs, an estimate of peak concentration is
desired. This level should be obtained after distribution of the
dose into the volume of distribution is achieved. For example,
digoxin levels should be drawn about 4–6 hours after admin-
istration in order to distribute into its very large V
d
. If peak
aminoglycoside or vancomycin levels are sought, these are
usually reached at 30 minutes to 1 hour after administration.
Second, sometimes the “trough,” or lowest, value before
administration of the next dose is wanted. Obviously, the
sample is drawn just prior to administration. Finally, for
many drugs, dosing is predicted by formulas or nomograms
that use serum levels at designated times (eg, aminoglycosides
and vancomycin), such as 4–10 hours after dosing. Drug dis-
tribution is also of concern following dialysis. It is important
to allow at least 3 hours to elapse after dialysis to obtain drug
levels to allow for redistribution of drug from other tissues
into the main compartment (eg, intravascular space). This
is illustrated also in the case of hemodialysis for a toxic
ingestion of lithium. A lithium level of 10 meq/L (therapeutic
level is 0.5–2 meq/L) obtained before dialysis may decrease to
1 meq/L immediately after hemodialysis. However, a third
level obtained 3–4 hours after dialysis may rebound to a toxic
level of 5 meq/L, showing evidence of redistribution from the
CNS back into the main compartment. This indicates the
need for longer or more frequent hemodialysis.
Phenytoin serum levels are often used to adjust dosing.
Phenytoin is eliminated by first-order kinetics at low serum
levels, but elimination is saturable at higher levels, even
within the therapeutic range. Therefore, at these levels, small
increases in dosing may result in unexpectedly high levels.
Ethanol is eliminated by alcohol dehydrogenase and obeys
zero-order kinetics; thus a constant fall in serum level with
time is expected, usually 30-40 mg/dL per hour.
Drug Interactions
Given the number of drugs prescribed for critically ill
patients, the potential for drug interactions is high. Drug
interactions may occur as a result of pharmacodynamic, phar-
maceutical, or pharmacokinetic effects. Pharmacodynamic
interactions result from the drugs actions and may enhance or
antagonize a drug’s effects. Pharmaceutical interactions can
result from a number of causes, one of which is the relationship
between two drugs. The most striking interactions are phar-
macokinetic, which occur when one drug affects the absorp-
tion, distribution, or clearance of another.
Pharmacodynamic Interactions
Pharmacodynamic drug interactions can result in synergis-
tic, additive, or antagonistic pharmacologic effects. A benefi-
cial additive effect would be observed in a patient with
poorly controlled hypertension who receives a second anti-
hypertensive agent from a different class and then achieves
optimal blood pressure control. Synergistic combinations are
noted when the resulting pharmacologic effect with combi-
nation therapy is greater than the expected sum of drug
effects. This phenomenon occurs infrequently and is best
described for antimicrobial combinations. A beta-lactam
antimicrobial (eg, piperacillin or ceftazidime) in combina-
tion with an aminoglycoside may be more effective than a
beta-lactam alone and results in a lower incidence of
acquired bacterial resistance in the treatment of infections
with aerobic gram-negative organisms. On the other hand,
antagonism may be encountered when beta-blockers reverse
the pharmacologic benefit of beta-agonists in patients with
chronic obstructive pulmonary disease (COPD). While some
beta-blockers such as atenolol are more cardioselective at
lower doses, they still have the potential to antagonize bron-
chodilators such as albuterol and salmeterol. The concomitant
use of antimicrobials from the same class also carries the
potential for antagonism. For example, some beta-lactams
induce production of beta-lactamase. The combination of a
strongly inducing beta-lactam with a labile compound
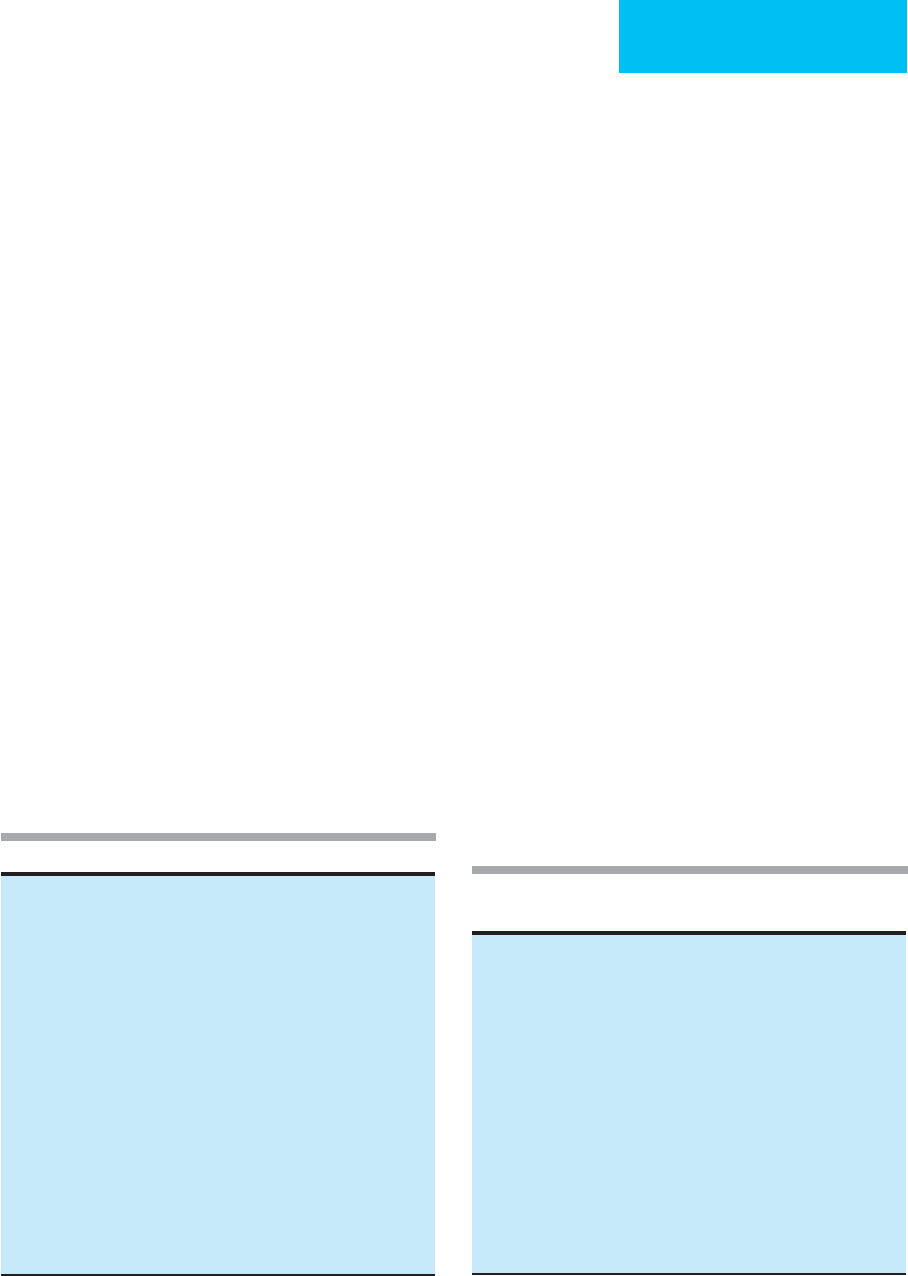
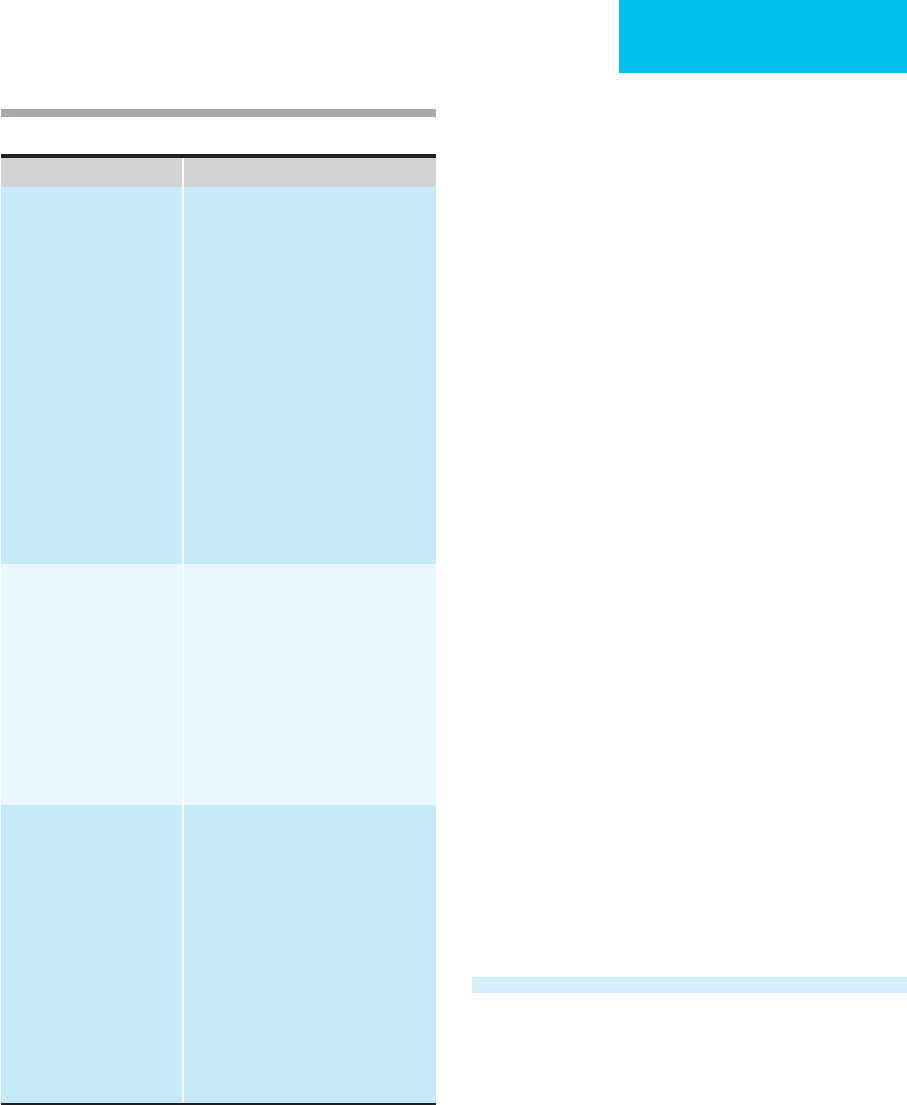
Drug Therapeutic Range
Amikacin Peak: 25–35 mg/L
Trough: <10 mg/L
Amiodarone 0.8–2.8 mg/L
Gentamicin, tobramycin Peak: 8–12 mg/L
Trough: <1 mg/L
Digoxin 1–2 μg/L
Lidocaine 1–5 mg/L
Phenobarbital 10–30 mg/L
Phenytoin 10–20 mg/L
Procainamide 4–8 mg/L
N
-Acetylprocainamide <30 mg/L
Salicylates 100–300 mg/L
Theophylline (in COPD) 8–10 mg/L
Vancomycin Trough: 5–15 mg/L
Table 4–5. Therapeutic ranges for drugs commonly used
in critical care.
PHARMACOTHERAPY
93
(eg, piperacillin) for the treatment of infections owing to
Enterobacter species has been shown to produce antagonism
in vitro and in animal models of infection. Hence double
beta-lactam combinations that include a strong inducer
should be avoided.
Pharmaceutical Interactions
Pharmaceutical interactions may be caused by drug incompat-
ibilities or drug adsorption to catheters and to intravenous
administration materials. For example, intravenous adminis-
tration of nitroglycerin requires special equipment to decrease
the likelihood of adsorption. The complexity of drug regimens
in the critically ill patient coupled with limited intravenous
access makes intravenous drug compatibility a significant
issue. Although a great deal is known about the compatibility
of drug combinations, there are still many potential combina-
tions for which no such information is available.
Pharmacokinetic Interactions
Although pharmacokinetic interactions occur as a result of
alterations in drug absorption, distribution, metabolism, or
elimination, the effects on drug metabolism are the most
clinically significant. A commonly seen absorption interac-
tion occurs when fluoroquinolones are administered con-
comitantly with antacids, causing decreased quinolone
bioavailability. Similarly, enteral feeding should be withheld
2 hours before and after the administration of oral phenytoin
formulations because of the decreased and delayed absorp-
tion of phenytoin that occurs.
Drug interactions owing to altered distribution also may
occur. When two drugs compete for binding sites on plasma
proteins or tissues, the unbound or free serum concentration
of one or both drugs may increase. Although this theoreti-
cally may increase a drug’s effect, the enhanced pharmaco-
logic effect is usually transient because more unbound drug
is now available for elimination by the liver and kidney. Thus
the clinical significance of protein-binding displacement
interactions is minimal unless there is concomitant hepatic
or renal disease. However, warfarin and phenytoin may be
transiently displaced by a number of drugs.
Pharmacokinetic drug interactions are frequently due to
altered metabolism involving the cytochrome P450 (CYP)
enzyme system, which is largely responsible for oxidative
metabolism of drugs by the liver. These enzymes are a super-
family of microsomal drug-metabolizing enzymes that
degrade endogenous substances, chemicals, toxins, and med-
ications. The primary ones responsible for drug metabolism
are CYP3A4, CYP2D6, CYP1A2, and CYP2C. Examples of
commonly used drugs that are inducers and inhibitors of
CYP are shown in Table 4–6. The most potent drugs likely to
be encountered are phenobarbital, phenytoin, and rifampin,
with subsequently more rapid metabolism and lower serum
levels for cimetidine, phenytoin, theophylline, warfarin, cor-
ticosteroids, and quinidine. Cigarette smoking and chronic
ethanol use also increase CYP activity. This explains why
alcoholics may require surprisingly high doses of sedatives
(eg, diazepam and midazolam) or analgesics. CYP induction
does not occur immediately, but usually takes at least several
days. Therefore, effects of CYP may be immediate (eg, in a
Drug Affected CYP Inducer/Inhibitor Effect
Benzodiazepines (alprazolam) Inhibitor
Azole antifungal (fluconazole, itracona
zole, ketoconazole)
Increased benzodiazepine concentration
Cyclosporine Inducer
Rifampin, rifabutin, phenobarbital,
phenytoin
Inhibitor
Erythromycin, azole antifungal
Decreased cyclosporine levels
Increased cyclosporine levels
Theophylline Inhibitor
Fluoroquinolone
Inducer
Cigarette smoking
Increased theophylline levels
Decreased theophylline levels
Warfarin Inducer
Phenobarbital
Inhibitor
Cimetidine
Decreased warfarin levels
Increased warfarin levels
Table 4–6. Examples of cytochrome P450 (CYP) induction or inhibition by drugs.
CHAPTER 4
94
chronic smoker) or delayed (eg, after starting a potential
CYP inducer in the hospital). Drugs that inhibit CYP systems
may behave differently than those that are inducers because
the former can act immediately on CYP. The most common
CYP inhibitors in the ICU are allopurinol, amiodarone,
cimetidine, erythromycin, and fluconazole.
The importance of CYP induction and inhibition depend
on the therapeutic indices of the drugs whose metabolism
are affected. The narrower the therapeutic window (level
providing therapeutic effect compared with the level result-
ing in toxic effect), the greater is the likelihood that a CYP
inhibitor will lead to toxicity or an inducer will cause sub-
therapeutic levels.
Adverse Effects & Drug Toxicities
Drugs may adversely affect all organ systems, but the kidney,
liver, heart, CNS, and vascular system are most frequently
affected. In critically ill patients with multiple medical prob-
lems, it can be quite difficult to isolate drug toxicity as the
sole cause of organ failure. Some drug toxicities are dose-
dependent, so attention to dosing and elimination is impor-
tant, as well as to drug interactions that may increase drug
levels (eg, inhibition of cytochrome P450 enzymes). Other
adverse effects are allergic and depend on the host response
and prior exposure. For some adverse effects, the patient may
be more susceptible for genetic or other reasons (long QT
syndrome).
Nephrotoxicity
The most common causes of drug-induced nephrotoxicity
are listed in Table 4–7. Nephrotoxicity in critically ill patients
may be due to drug-induced causes or to hypoperfusion.
Because the mortality rate for ICU patients with acute renal
failure approaches 80%, efforts should be directed at remov-
ing all potential causes of nephrotoxicity. Adequate fluid
resuscitation and maintenance of renal perfusion are of
paramount importance for preventing prerenal acute renal
failure. Appropriate intravascular volume status and pre-
treatment with N-acetylcysteine or sodium bicarbonate
decrease the risk of nephrotoxicity from radiocontrast
agents.
Despite adequate preventive measures, up to 20% of all
cases of acute renal failure may be associated with drug toxi-
city. Drug-induced toxicity may take the form of acute tubu-
lar necrosis, interstitial nephritis, or glomerulonephritis. Of
those drugs associated with acute tubular necrosis, the most
notable are the aminoglycosides and amphotericin B. With
once-daily dosing of aminoglycosides (5–7 mg/kg per day)
and proper therapeutic drug monitoring, the incidence of
acute tubular necrosis is reduced significantly. Novel ampho-
tericin B formulations as well as the increased use of other
antifungals (eg, azoles and echinocandins) reduce the risk of
nephrotoxicity. Interstitial nephritis and glomerulonephritis
are due to hypersensitivity reactions or immune-complex
formation. The most common drugs leading to interstitial
nephritis are antibiotics, even though the most likely culprit,
methicillin, is no longer used.
Hepatotoxicity
While a number of drugs have been associated with altered
liver function tests, these changes are usually reversible on
discontinuation of the offending agent. Since acute hepatic
injury is classified according to morphology, drug-induced
hepatic injury may cause either direct hepatocellular necro-
sis, cholestasis, or a mixed presentation of both (Table 4–8).
Some drug combinations such as rifampin and isoniazid,
amoxicillin and clavulanic acid, and trimethoprim and sul-
famethoxazole also may increase the possibility of hepato-
toxic reactions. This may occur because one agent alters the
metabolism of the other, leading to the production of toxic
metabolites. Phenytoin induces both hepatic necrosis and
cholestasis in association, producing an immune response
manifested by a rash, eosinophilia, atypical lymphocytosis,
and serum IgG antibodies against phenytoin.
An increasingly important source of drug-induced hepa-
totoxicty is the use of herbal drugs. These may not be disclosed
Acute tubular necrosis
Acyclovir
Aminoglycosides
Amphotercin B
Iodinated contrast dyes
Foscarnet
Pentamidine
Interstitial nephritis
Allopurinol
Cimetidine
Furosemide
Methicillin
Phenytoin
Rifampin
Thiazides
Trimethoprim-sulfamethoxazole
Vancomycin
Glomerulonephritis
ACE inhibitors
Gold salts
Hydralazine
Penicillamine
Rifampin
Renal hemodynamics
ACE inhibitors
Cyclosporine
NSAIDs
Tacrolimus
Table 4–7. Nephrotoxic drugs.
PHARMACOTHERAPY
95
by patients without specific questioning. Toxicity may be
hepatocellular or cholestatic in nature. Some herbs may
inhibit or induce the CYP system (eg, St. John’s wart induces
CYP3A4, reducing concentrations of cyclosporine A), and
several herbal drugs affect metabolism of warfarin.
Cardiac Toxicity
Many drugs used in the ICU have potentially adverse cardiac
effects. These include drugs that cause tachycardia (eg, beta-
adrenergic agonists, dopamine, and theophylline), bradycardia
(eg, beta-adrenergic blockers and certain calcium channel
blockers), myocardial depression, and arrhythmias (eg,
digoxin, theophylline, and, surprisingly, antiarrhythmic drugs).
An important but unusual adverse effect is drug-induced
prolonged QT interval syndrome, sometimes associated with
a chaotic ventricular tachycardia (torsade de points). Both
cardiac and noncardiac drugs have been associated with this
syndrome, including quinindine and procaineamide;
antipsychotic drugs; antibiotics such as macrolides, fluoro-
quinolones, and ketoconazole; histamine-1-antihistamines;
and other drugs. In some cases, patients receiving multiple
drugs develop interactions that increase serum levels of the
contributing agent. It should be noted that some such drugs
have been withdrawn from the market because of the risk of
prolonging the QT interval. Drug-induced prolonged QT
syndrome and torsade de points are more common in
women, those with heart disease and electrolyte disorders,
and those with familial long QT syndrome. In one study, one
or more of these risk factors were present in the majority of
patients who had drug-induced torsade de points.
Electrolyte Abnormalities
Drugs may be associated with a variety of electrolyte and
acid-base abnormalities. Some of the effects are predictable,
such as hypokalemia induced by thiazide diuretics,
furosemide, glucocorticoids, insulin, and beta-adrenergic
agonists and hyperkalemia from spironolactone, tri-
amterene, or angiotensin-converting enzyme (ACE)
inhibitors. On the other hand, less often expected are hyper-
kalemia with heparin, potassium penicillin G, and trimetho-
prim. Hyponatremia may be a feature of thiazide diuretic
administration. Amphotericin B is associated with
hypokalemia, hypomagnesemia, and renal tubular acidosis.
MEDICATION ERRORS & PREVENTION
IN THE ICU
Reduction of medical errors is the focus of many hospital
quality improvement plans, and medication errors usually
make up the vast majority of medical errors. In the ICU,
attention to medication administration is very important,
and systems to reduce errors have been shown to be effective.
Medication errors arise at any point—from ordering to
administration. The most common errors are those of dosing
without due consideration for the patient’s age, size, renal or
hepatic function, or drug interactions. More rare is adminis-
tration of the wrong medication; this can result from tran-
scription errors or failure to match the medication with the
patient. Because critically ill patients often have multiple clini-
cians participating in their care and multiple medications
Table 4–8. Hepatotoxic drugs.
Type of Hepatic Injury Drug
Hepatocellular Acetaminophen
Allopurinol
Amiodarone
Isoniazid
Ketoconazole
Lisinopril
Losartan
Nevirapine
Paroxetine
Pyrazinamide
Rifampin
Risperidone
Ritonavir
Salicylates
Sertraline
HMG-CoA reductase inhibitors (“statins”)
Tetracycline
Trazodone
Valproic acid
Cholestatic Amoxicillin ⁄ clavulanate
Anabolic steroids
Azathioprine
Chlorpromazine
Clopidogrel
Cytarabine
Erythromycin
Estrogens
Oxacillin
Phenothiazines
Sulindac
Tricyclic antidepressants
Mixed Amitryptilline
Azathioprine
Captopril
Carbamazepine
Clindamycin
Cyprohepatadine
Enalapril
Ibuprofen
Nitrofurantoin
Phenobarbital
Phenytoin
Sulfonamides
Trazodone
Trimethoprim-sulfamethoxazole
Verapamil
CHAPTER 4
96
prescribed, it is not surprising that there may be duplication of
medication orders, inadvertent administration of two drugs
for the same purpose, and unrecognized drug interactions.
Systems for minimizing medication errors in the ICU
depend on careful, timely, and regular review of medications
and reconciliation of orders with administered medications.
Standardized intravenous mixtures, protocols for drug
administration (eg, sedation guidelines and IV insulin and
heparin protocols), computerized order entry, and auto-
mated review of potential drug interactions are effective
tools.
REFERENCES
Boucher BA, Wood GC, Swanson JM: Pharmacokinetic changes in
critical illness. Crit Care Clin 2006;22:255–71, vi. [PMID:
16677999]
Chang CY, Schiano TD: Review article: Drug hepatotoxicity. Aliment
Pharmacol Ther 2007;25:1135–51. [PMID: 17451560]
Erstad BL: Dosing of medications in morbidly obese patients in the
intensive care unit setting. Intensive Care Med 2004;30:18–32.
[PMID: 14625670]
Gabardi S, Abramson S: Drug dosing in chronic kidney disease. Med
Clin North Am 2005;89:649–87. [PMID: 15755472]
Kane-Gill S, Weber RJ: Principles and practices of medication safety
in the ICU. Crit Care Clin 2006;22:273–90, vi. [PMID: 16678000]
Lewis JH et al: Drug-induced liver disease. Curr Opin Gastroenterol
2006;22:223–33. [PMID: 16550036]
Mann HJ: Drug-associated disease: Cytochrome P450 interactions.
Crit Care Clin 2006;22:329–45, vii. [PMID: 16678003]
Schetz M et al: Drug-induced acute kidney injury. Curr Opin Crit
Care 2005;11:555–65. [PMID: 16292059]
Stedman C: Herbal hepatotoxicity. Semin Liver Dis 2002;22:
195–206. [PMID: 12016550]
Taber SS, Mueller BA: Drug-associated renal dysfunction. Crit Care
Clin 2006; 22:357–74, viii. [PMID: 16678005]
Trotman RL et al: Antibiotic dosing in critically ill adult patients
receiving continuous renal replacement therapy. Clin Infect Dis
2005;41:1159–66. [PMID: 16163635]
Vandendries ER, Drews RE: Drug-associated disease: Hematologic
dysfunction. Crit Care Clin 2006;22:347–55, viii. [PMID:
16678004]
Zeltser D et al: Torsade de pointes due to noncardiac drugs: Most
patients have easily identifiable risk factors. Medicine
(Baltimore). 2003;82:282–90. [PMID: 12861106]
