Tadrous P.J. Diagnostic criteria handbook in histopathology: a surgical pathology vade mecum
Подождите немного. Документ загружается.


JWBK208-06 December 8, 2007 16:1 Char Count= 0
Vascular 69
Malignant HT:
r
Hypertrophic arteriolosclerosis: concentric smooth muscle cell onion skin thickening of the intima
r
Fibrinoid necrosis (necrotising arteriolitis) esp. kidney (‘flea bite’ haemorrhages and haematuria) –
assoc
d
with more severe HT
r
Microangiopathy → haemolytic anaemia, retinal haemorrhages, exudates and papilloedema
r
The above changes are also seen in severe forms of TMA (see p. 207).
r
d/dg athero/lipid emboli and the renal vascular changes of Alagille’s syndrome (look for lipid)
r
d/dg: PSS arteritis (vide infra)
Pulmonary HT
See Chapter 8: Respiratory and Mediastinum.
Vasculitides
Diagnostic Table
r
In Table 6.1
√
means typically present and × typically absent – although exceptions occur. GN refers
to the presence of glomerulonephritis (usu. necrotising FSGN or crescentic), not intra-renal arterial
branch involvement. An important d/dg is TMA (see p. 207)
r
d/dg of necrotising vasculitides includes radiation vasculopathy, severe HT changes and TMA (q.v.)
Giant Cell (Temporal) Arteritis
r
Patients are usu. > 50 years old (a strong feature)
r
Changes are focal and GC present in only 55% cases .
.
. take multiple levels of long Bx (e.g. 4 cm)
r
Early: medial necrosis and many PMN, smaller branch involvement.
r
Later: granulomatous lesions in relation to fragments of the IEL (↑refractility but ↓staining)
r
Non-specific transmural mononuclear cell infiltrate and scattered eos. ± PMN ± lumenal thrombus
r
Healed phase: extensive fibrotic replacement of the IEL (e.g.
1
4
circumference)
patchy lymphohistiocytic aggregates in media
patchy fibrosis of media ± neovascularisation
irregular intimal fibrosis.
r
Steroids cause resolution of histology after 14 days continuous use
r
d/dg normal age change (= elastic splitting, concentric intimal fibrosis, medial hyalinisation ± Ca
2+
)
r
d/dg: Buerger’s, Takayasu’s, Bazin’s/nodular vasculitis, Wegener’s, Churg-Strauss
Takayasu’s Disease (Takayashu’s Disease, Pulseless Disease)
r
< 50 years (strong feature), HT, arm claudication, BP difference >10mmHg between arms, visual Sx
r
Early: granulomatous inflam
n
(± greater adventitial and intimal involvement cf. giant cell arteritis)
r
Mixed chronic inflam
y
infiltrate (esp. adventitial) with elastic destruction
r
± Medial necrosis (proper)
r
Intimal fibrosis ± proliferative endarteritis ± thrombosis
r
d/dg giant cell arteritis, Syphilis, clinically other causes of ‘pulseless disease’ e.g. dissection
Polyarteritis Nodosa (PAN)
r
Asthma and eosinophilia are strongly associated with the Churg-Strauss variant
r
Main visceral arteries (no GN), cutaneous leukocytoclastic vasculitis may accompany PAN
r
Patchy, transmural, fibrinoid necrosis with healing by fibrosis
r
Leukocytes (PMN early, later mixed incl. variable eosinophils) are biased to the adventitia
r
Acute, healing and healed stages usu. co-exist
r
Segmental erosion → aneurysm/rupture/local inflam
n
→ palpable nodule
r
Consequences: ischaemic injury/infarcts/ulcers/thrombosis
r
d/dg 2
◦
arteritis (due to infarction, inflammation or infection)
Microscopic Polyarteritis
r
Segmental fibrinoid necrosis ± leukocytoclasia (incl. venules)
r
Necrotising GN and pulmonary capillaritis, also skin, muscle, GIT and mucosae
r
All lesions tend to be of the same stage
JWBK208-06 December 8, 2007 16:1 Char Count= 0
Vascular 70
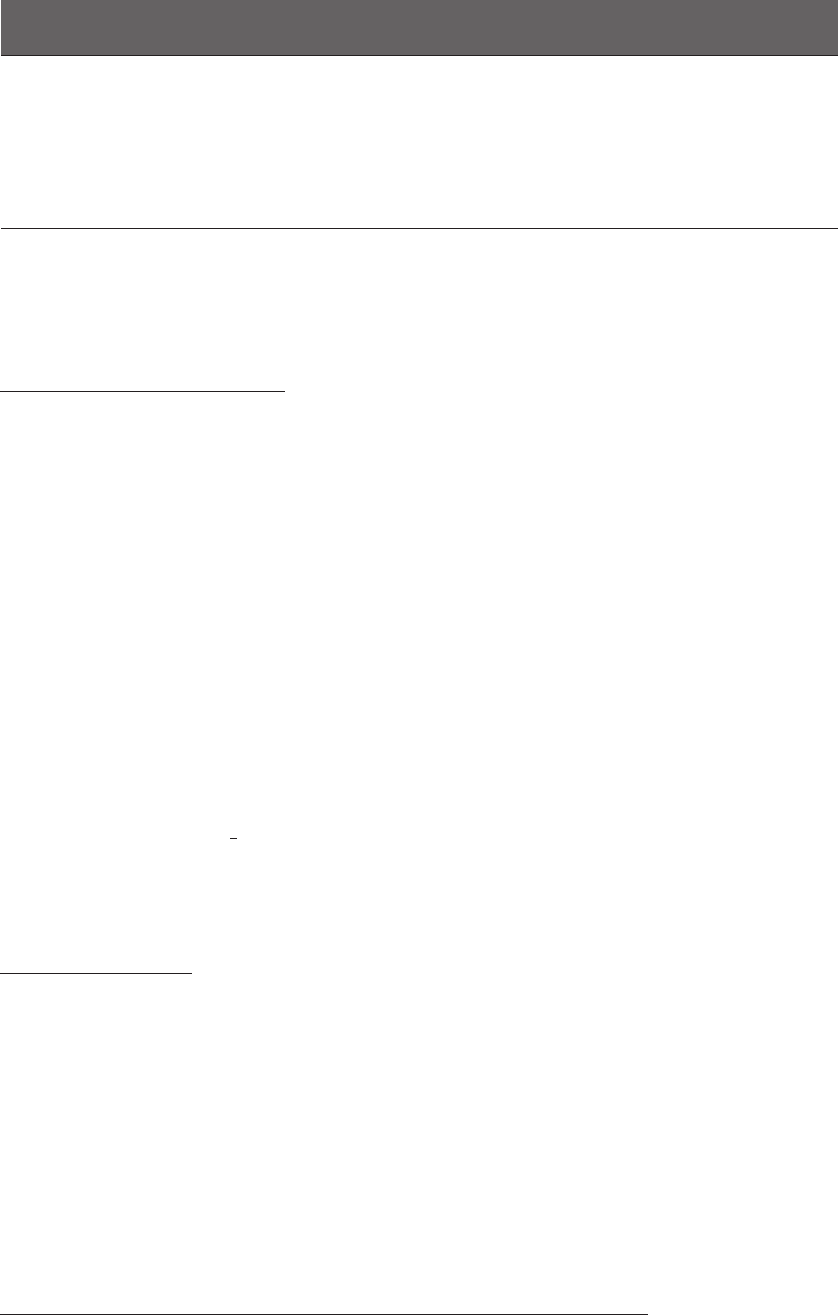
TABLE 6.1 Diagnosing vasculitides
Vessel Type Lung GN Skin Diagnostic Antibodies/Comments
Large Elastic Arteries
Giant cell arteritis ±×±older patients & more restricted to media cf. Takayasu
Takayasu’s disease ±×±exclude Syphilis
Syphilitic aortitis confirm with serology
CTD aortitis ±±±usu. ascending only, sparing of major branches (cf.
Takayasu) e.g. ankylosing spondylitis, RhA, SLE
Medium-sized Muscular
Arteries
Giant cell arteritis ±×±±↑ESR, 50% have polymyalgia rheumatica (PMR)
Takayasu’s disease ±×±vide supra for d/dg with giant cell arteritis
PA N
√
×
√
HBV (40%), p-ANCA/c-ANCA (≤10%)
Buerger’s disease ××±
Wegener’s
√√√
c-ANCA (70%), p-ANCA (20%), neither (10%)
Churg-Strauss
√√√
p-ANCA (75%)
Kawasaki’s disease
Fungal
√
CTD arteritis ±±±Lupus can have dermo-renal involvement with
non-proteinase-3 p-ANCA in 25%. RhA are
seropositive for IgG rheumatoid factor
Arterioles +/ Capillaries
Microscopic polyarteritis
√√√
c-ANCA (45%), p-ANCA (45%), neither (10%)
PA N
√
×
√
vide supra. Larger vessels also involved
Wegener’s
√√√
c-ANCA (70%), p-ANCA (20%), neither (10%)
Churg-Strauss
√√√
Rickettsial
lymphocytic vasculitis ××
√
see Chapter 20: Skin
1
◦
pauci-immune GN ×
√
× p-ANCA (60%), c-ANCA (30%), neither (10%)
Goodpasture’s
√√
× linear IgG + C3 in BMs. p-ANCA (25%).
leukocytoclastic vasculitis ±±
√
HSP (± IgA ANCA), cryoglobulins (± HCV Ags) and
serum-sickness can have dermo-renal involvement ±
elastase p-ANCA. Drug reactions may have
MPO/lactoferrin p-ANCA
Veins/Venules
Buerger’s disease ××±
Wegener’s
√√√
c-ANCA (70%), p-ANCA (20%), neither (10%)
1
◦
cutaneous
granulomatous phlebitis
××
√
very rare
Trousseau’s syndrome ××
√
migratory thrombophlebitis assoc
d
with metastatic
adenocarcinoma. PMNs early, granulomas later
leukocytoclastic ±±
√
Lymphatics
Crohn’s/Sarcoid ±±
√
Granulomatous vasculitis may be 2
◦
to perivascular
lymphatic involvement.
Wegener’s Granulomatosis (WG)
For def
n
and lung and kidney features, see p. 87.
r
Necrotising vasculitis away from necrotic areas (extensive fibrinoid change is unusual)
r
Affects arteries, arterioles and veins
r
Lymphocytes and plasma cells > giant cells and PMN, eos. are usu. sparse (except in the eosinophilic
variant)
r
Granulomatous inflammation may involve whole vessel wall and extend into lumen
r
Arterioles, capillaries and veins may be involved (e.g. in alveolar septa) ± leukocytoclasia
r
d/dg other granulomatous/PAN-like vasculitides (giant cell, Takayasu’s, Churg-Strauss, etc.)
JWBK208-06 December 8, 2007 16:1 Char Count= 0
Vascular 71
Churg-Strauss Vasculitis
r
Eosinophilic PAN
r
Eosinophilic microscopic polyarteritis
r
Eosinophilic WG-like granulomatous vasculitis
r
Eosinophilic phlebitis
r
Eosinophilic leukocytoclastic vasculitis
r
Necrotising FSGN (rarely)
For extravascular details and definition, see p. 87.
Buerger’s Disease (Thromboangiitis Obliterans)
r
Strong (≈ dose-response) association with tobacco smoking
r
Muscular arteries of the forelimbs, skip lesions early on, and involves adjacent veins
r
Acute inflam
n
(early) → chronic inflam
n
→fibrosis affects whole vessel wall incl. adventitia and
surrounding veins and nerves
r
Inflamed, cellular thrombus
r
± Giant cells in/adjacent to thrombus (cf. in the media in other arteritides) These are said to be
r
± Microabscesses in vessel wall
pathognomonic
r
Separation of layers of the vessel wall by inflam
n
/fibrosis
r
Good preservation of the IEL (cf. giant cell/other arteritis or atheroma)
r
d/dg atheroma: preserved IEL, early onset, upper limb involvement, vein involvement, inflam
y
nature,
small vessel involvement.
r
d/dg giant cell arteritis: distribution, giant cell location, preservation of IEL, adventitial involvement,
vein involvement.
Leukocytoclastic Vasculitis (LCV)
For morphology and further information, see p. 301. Example causes are given below.
r
Most drug reaction vasculitides
r
Henoch-Sch¨onlein purpura (HSP)
r
Cryoglobulinaemia (also results in membranoproliferative GN)
r
Serum sickness (see p. 350)
r
Beh¸cet’s disease (see p. 194 and p. 341)
r
Some forms of paraneoplastic vasculitis
r
Neisseria infections (e.g. N. meningitidis)
Urticarial Vasculitis and Lymphocytic Vasculitis
See Chapter 20: Skin.
Rheumatoid Vasculitis
r
Nerves, skin and main visceral small arteries and capillaries, esp. hands and nail folds
r
Transmural fibrinoid necrotising vasculitis
r
Cutaneous lymphocytic vasculitis These are said to be
r
Cutaneous urticarial vasculitis
pathognomonic
r
d/dg drug reaction
SLE Vasculitis
r
Nerves, skin and main visceral small arteries and capillaries
r
Transmural necrotising vasculitis (PAN-like with ↓overall inflam
n
±↑PMN)
r
Cutaneous urticarial vasculitis
r
LN and spleen arteries may show ‘onion skin’ perivascular fibrosis
r
For GN spectrum, see pp. 204–205; for further detail see pp. 297–298.
r
d/dg lupus ‘anticoagulant’ thrombotic vasculopathy (fibrin thrombi in small vessels → et seq.) [also
called antiphospholipid Ab syndrome: see p. 351 and pp. 61–62]
Progressive Systemic Sclerosis (PSS) Vasculitis
r
Fibrinoid necrotising vasculitis of small arteries
r
↑ Mucopolysaccharide in intima
r
Onion skinning of intima
r
d/dg severe HT changes

JWBK208-06 December 8, 2007 16:1 Char Count= 0
Vascular 72
Kawasaki’s Disease
r
Seen in children with the mucocutaneous LN syndrome (MCLNS)
r
Transmural necrotising vasculitis with PMN predominating early on (PAN-like)
r
Later → mixed mononuclear cell infiltrate (incl. intramural T-cells) and PMN
r
Arterioles and venules may be involved in addition to muscular arteries
r
d/dg: see p. 119, under ‘Kikuchi-Fujimoto disease’
Miscellaneous
Radiation Angiopathy
r
Muscular arteries, arterioles and capillaries. For veno-occlusive disease, see p. 169
r
Early: endothelial atypia (nuclear hyperchromasia, swelling)
fibrinoid necrosis
RBC extravasation
thrombosis
r
Later: proliferative endarteritis and intimal fibroplasia
foam cell accumulation and accelerated atherosclerosis
small vessel telangiectasia
adventitial fibrosis and distortion, fragmentation of the IEL ± inflam
n
(d/dg vasculitis)
hyaline arteriolosclerosis-like changes (q.v. – d/dg HT)
Congophilic (Amyloid) Angiopathy (CAA)
r
Clin.: multifocal superficial cerebral haemorrhage/SAH (± Alzheimer’s)
r
Hyaline eosinophilic material in meningeal +/ cerebral vessels These H&E features may
r
± Evidence of previous haemorrhage
be subtle
r
Immuno for A4 () amyloid is more sensitive cf. Congo red
Aneurysms
Definition
r
An abnormal localised dilatation of a vessel
r
True – surrounded by a complete vessel wall (e.g. atheromatous, congenital, luetic, mycotic)
r
False – extravascular haematoma communicating with the intravascular space (e.g. anastomotic leak,
mycotic aneurysm)
Atherosclerotic:
r
Usu. abdominal and below the renal arteries. Grow by deposition of thrombus (→ laminar structure)
r
Atheromatous erosion (and .
.
. weakening) of media
r
Complications: rupture
occlusion of vessels/ostia by pressure or thrombus (e.g. renal/vertebral)
compress/erode adjacent structures (e.g. ureter/vertebrae)
embolism
infection (‘mycotic aneurysm’)
retroperitoneal fibrosis ± ureteric involvement
Luetic (syphilitic)
r
Thoracic aorta (usu. the arch)
r
Proliferative endarteritis of vasa vasorum → patchy necrosis (loss) of medial fibroelastic tissue
r
Lymphoplasmacytic periarteritis of vasa vasorum
r
Dense collagenous fibrous patches of intima with grooves (‘tree bark’ macro)
r
Complications: rupture
occlude coronary ostia
compress/erode adjacent structures (→ respiratory difficulties/cough/pain)
annuloaortic ectasia et seq. → cor bovinum
r
d/dg: aortitis of psoriasis, Reiter’s or ankylosing spondylitis
Cirsoid aneurysms (Racemose aneurysms)
r
These are dilated AVMs (congenital +/ traumatic)
r
Occur in the scalp, leptomeninges and elsewhere
Venous aneurysms
r
Rare and usu. 2
◦
to trauma or abnormal infiltrates of the wall (vide infra)
JWBK208-06 December 8, 2007 16:1 Char Count= 0
Vascular 73
Other conditions weakening the vessel wall
r
Congenital (e.g. berry aneurysm)
r
Inflammatory (e.g. PAN)
r
Infective (‘mycotic aneurysm’)
r
Infiltration by diffuse NF tissue in NF-1
r
Trauma (as a result of stretching of the scar) e.g. cardiac, arteriovenous-fistula and caroticocavernous
sinus aneurysms
r
DM (capillary aneurysms e.g. retina)
Arterial Dissection (Dissecting ‘Aneurysm’)
r
Tracking of blood between (usu.) the middle and outer thirds of the media. Commonest in the aorta
r
Potentiating factors: HT and conditions with ↑ MPS deposition e.g. pregnancy/Marfan’s
r
Atheromatous plaques act as barriers to dissection
Aortic dissection:
r
± Intimal tear on ascending aorta (a distal tear → double barrel aorta →↓risk of complications)
r
± ‘Cystic medial necrosis’ (disorganisat
n
of the media, elastic fragmentat
n
and pools of acid MPS
forming pseudocystic [i.e. no lining] spaces – see also p. 78)
r
Complications: rupture into a coelomic cavity → exanguination/cardiac tamponade
occlusion of ostia (e.g. carotid, coronary, renal, mesenteric)
impaired aortic valve function
Fibromuscular Dysplasia (Fibromuscular Arterial Hyperplasia)
r
Muscular arteries; renal > carotid/other sites
r
One or more of the following may be seen:
segmental medial hypertrophy alternates with medial thinning and attenuation of IEL
fibrous replacement of outer half of media
cellular concentric intimal fibroplasia
adventitial fibrous encasement
r
Complications: stenosis, thrombosis, aneurysm (in thinned segments), dissection
r
d/dg NF-1 assoc
d
arterial dysplasia/vasculopathy (vide infra)
NF-1 Associated Vasculopathy (Vascular Neurofibromatosis)
r
Veins and muscular arteries: → renovascular HT, aneurysm, fistulae, haemorrhage (! a per-operative
risk)
r
Veins (± arteries) may have their walls weakened by infiltration with diffuse NF spindle tissue
r
Arteries show concentric cellular myointimal proliferation (MSA +ve cells) with MPS ++
r
Nodules of smooth muscle spindle-cells may be seen in the arterial media and intima (S100 −ve)
r
d/dg fibromuscular dysplasia (vide supra)
Thrombus and Thromboembolus (Features and Dating Criteria)
r
d/dg embolus (e.g. PE)/thrombus vs. PM clot:
embolus is firmer (cf. ‘chicken-fat’ clot) and is not a cast of the vessel
clot does not have a laminar cross-section (lines of Zahn)
thrombus/embolus stands proud of the vessel wall when cut
r
Dating thrombus:
sampling: take a block from the junction of thrombus and vessel wall
two days: endothelial bud proliferation begins
eight days to one year: haemosiderin deposits
age of fibrin (by the MSB method): early = yellow, medium = red, very old = blue
Ehlers Danlos Syndrome
r
Excessive elastic tissue in small arteries
Thrombotic Microangiopathy (TMA) and DIC
See p. 207.
Transplant Rejection Angiopathy
See organ-specific chapters.
Tumours and Malformations
See Chapter 5: Paediatric and Placental, and Chapter 21: Soft Tissues.

JWBK208-06 December 8, 2007 16:1 Char Count= 0
Vascular 74
Bibliography
Bellamy, C.O.C. (2004) Microangiopathies and malignant vascular injury in the kidney. Current Diagnostic Pathology, 10 (1), 36–51.
Cavallo, T. (1998) Pathologic approach to the diagnosis of vasculitis. Current Diagnostic Pathology, 5 (2), 70–81.
Cotran, R.S, Kumar, V. and Collins, T. (eds) (1999) Robbins Pathologic Basis of Disease,6
th
edn, W.B. Saunders Co., Philadelphia.
Knight, B. (1983) The Coroner’s Autopsy,1
st
edn, Churchill Livingstone, Edinburgh.
Mooney, E.E. and Shea, C.R. (1997) Cutaneous vasculitis. Current Diagnostic Pathology, 4 (1), 1–9.
Ng, W-K. (2003) Radiation-associated changes in tissues and tumours. Current Diagnostic Pathology, 9 (2), 124–136.
Nopajaroonsri, C. and Lurie, A.A. (1996) Venous aneurysm, arterial dysplasia, and near-fatal hemorrhages in neurofibromatosis type 1. Human
Pathology, 27 (9), 982–985.
Sheaff, M. and Baithun, S.I. (1997) Pathological effects of ionising radiation. Current Diagnostic Pathology, 4 (2), 106–115.
Sternberg, S.S. (ed) (1997) Histology for Pathologists,2
nd
edn, Lippincott Williams & Wilkins, Philadelphia.
Symmers, W. St. C. (ed) (1976) Systemic Pathology, Vol. 1, 2
nd
edn, Churchill Livingstone, London.
Wheater, P.R., Burkitt, H.G. and Daniels, V.G. (1987) Functional Histology: A text and colour atlas,2
nd
edn, Churchill Livingstone, Edinburgh.
PIC
JWBK208-07 December 8, 2007 16:1 Char Count= 0
Heart 75
7. Heart
Normal and Age-Related Changes
Valves
r
Avascular except for microvessels at the root
r
Three-layer sandwich of (from ventricular surface outwards):
◦
1
lamina ventricularis lined by endothelium and containing most elastic fibres
◦
2
lamina spongiosa (MPS-rich, containing muscle in the AV valves near the valve root)
◦
3
lamina fibrosa lined by endothelium, focally thickened at contact points (lines of closure)
Blood Supply
r
LAD supplies: apex, anterior LV, anterior
2
3
of the septum
r
RMC supplies: RV free wall, posterior LV (→ Posterior Descending if right dominant)
r
LCirc supplies: lateral LV (→ Posterior Descending if left dominant)
r
Posterior descending supplies the posterior
1
3
of the septum
Age-Related Changes
r
Brown atrophy (lipofuscin) and basophil degeneration (glucan)
r
Right shift and tortuosity of ascending aorta → HOCMoid sigmoid septum
r
Aortic valve: calcinosis (± stenosis)
r
Mitral valve: bulging, atheromatoid changes, Ca
2+
, Lambl’s excrescences
Ischaemic Heart Disease
Angina
r
May show myocardial scarring / infarction
r
Sig. coronary disease may be absent in LVH or hyperthyroidism
MI (Regional)
r
Usu. transmural and involving: LAD (50%), RMC (30%), LCirc (15%), LMC/combined (5%)
r
Macro: 8–10 hours none, but NBT test may show focal lack of enzyme activity
1–2 days swelling, lack-lustre
2–3 days pale, soft, ± beginning of ‘tigroid’ haemorrhages
3–7 days yellow-grey, haemorrhages, softening (‘myomalacia cordis’)
7–10days sharp definition with vascular granulation tissue
1–2 weeks ‘gelatinous transformation’ at the centre of the infarct
3–12 weeks scar tissue
r
Micro: 2–12 hours blurring of striations, ‘cloudy swelling’ (=eosinophilia and granularity)
1day ↑eosinophilia, myocytes become angulated, wavey and ‘pinched’
2–7 days PTAH shows striations undergoing granular disintegrat
n
with clumping
into ‘contraction bands’ (likened to Chinese writing), ↓nuclear staining,
variable PMN infiltrate, beginning of granulation tissue by 1 week
1st week PMN are prominent
2nd week granulation tissue is prominent
3rd week collagenisation (scarring) begins
6–12 weeks fibrosis, ↓vascularity, myohypertrophy, chamber dilatation
months–years fossilised infarct (an old MI containing a central area that looks like a
recent MI)
r
Complications:
immediate: arrhythmias and SCD
acute rupture of ventricle, septum, pap. muscle
pericarditis
intracardiac thrombus (due to ↑thromboplastin and eddying)
LVF / CCF / cardiogenic shock
Diagnostic Criteria Handbook in Histopathology: A Surgical Pathology Vade Mecum. Paul J. Tadrous
Copyright
C
2007 by John Wiley & Sons, Ltd. ISBN: 978-0-470-51903-5

PIC
JWBK208-07 December 8, 2007 16:1 Char Count= 0
Heart 76
chronic aneurysm (15%) → LVF / emboli
angina (relief or production)
re-infarction (esp. smokers)
antimyocardial autoimmunity (→ Dressler’s: fever, tachycardia, pleuroperi-
carditis)
MI (Subendocardial)
r
Severe coronary atheroma (except in aortic valve disease)
r
Usu. whole LV circumference ± regional transmural infarct
Sudden Cardiac Death (SCD)
r
May see an old infarct or angina changes
r
Most do not have a fresh infarct
Inflammatory Heart Disease
Viral Myocarditis
r
Coxsackie B (common in the UK) – diagnose by serology, pericardial fluid, throat swab / faeces
r
Mixed mononuclear cell infiltrate
r
± Necrosis, ± granulomatous myocarditis
Systemic Diseases
r
RhA: nodules
r
SLE: fibrinoid, histiocytes, apoptoses, Libman-Sacks fibrin vegetations (not related to closure lines,
present on the surface of the influx of blood, valve shows fibrinoid necrosis at site of attachment)
r
Vasculitides: Wegener’s, PAN, Kawasaki
r
Sarcoid
r
Whipple’s disease: focal fibroses, valve deformities (d/dg rheumatic fever), DPAS +ve foamy M
r
Chagas’ disease (of Trypanosoma cruzi): acute → fever, LNp, unilateral orbital oedema, rash, etc.;
Chronic → megaoesophagus/colon/heart (cardiomegaly); see Chapter 23: Infection and Immunity
Granulomatous Myocarditis
r
Idiopathic (not to be confused with idiopathic giant cell myocarditis)
r
Sarcoid
r
Infective: usu. TB or viral
r
Rheumatic fever (Aschoff bodies)
r
d/dg M cytomyolysis which accompanies cerebral infarct, head injuries, etc.
Idiopathic Giant Cell Myocarditis
r
Rapid clinical deterioration → death
r
Serpiginous necrosis
r
Giant cells at periphery
Floppy Mitral Valve
◦
1
focal destruction of the lamina fibrosa with replacement by . . .
◦
2
. . . accumulations of MPS
Acute Rheumatic Fever
r
Pancarditis: pericarditis, myocarditis, endocarditis
r
Aschoff bodies:
Aschoff cells: eosinophilic ragged cytoplasm
nucleus has a clear zone around elongated nucleolus to give an ‘owl’s
eye’ or ‘caterpillar’ appearance
early: swelling, fragmentation and eosinophilic change of connective tissue
interstitial basophilic material
later: granulomatous foci and fibrinoid change
located around small vessels
PIC
JWBK208-07 December 8, 2007 16:1 Char Count= 0
Heart 77
r
Myocardial damage: lymphocyte predominant infiltrate
muscle necrosis, vacuolation and multinucleation
± Aschoff bodies (esp. in septum)
r
Vasculitis: affects vessels of any size
may be PAN-like in larger vessels
perivascular fibrin
adventitial scarring
medial oedema
intimal and medial elastification with loss of distinction between intima and media
thromboses and recanalisation
r
Valve disease: seen along lines of closure
intimal ulceration
‘verrucae’ of platelets and fibrin
± Aschoff bodies
Chronic Rheumatic Fever Valve Disease
r
Fibrosclerotic thickening
r
Vascularisation of the valve
r
± Non-specific chronic inflammation
Cardiac Allograft (Transplant) Rejection
r
Predominantly T-cell infiltrate
r
± Granulocytes (usu. eosinophils > PMN)
r
± Myocyte necrosis
r
A mixed infiltrate (lymphocytes, plasma cells, histiocytes ±granulocytes) is said to be evidence against
rejection
r
Changes due to healing of a previous biopsy site:
granulation tissue ± organising fibrin with local distortion of myocytes
± early lipofuscin (‘ceroid’) M
usu. seen on only one of the submitted fragments
r
Ischaemia and reperfusion injury: foci of myocyte necrosis / vacuolisation / dropout ± a mild PMN
infiltrate. No evidence of a rejection infiltrate (mononuclear cells ± eosinophils)
r
Subendocardial thickening / fibrosis
r
Subendocardial dense lymphocyte collections (‘Quilty lesions’) without (Type A) or with (Type B)
infiltration of adjacent myocardium are of uncertain significance (? localised rejection)
r
Mild Acute Rejection = sparse T-cells, no eosinophils or necrosis
r
Moderate / Severe Acute Rejection = moderate multifocal infiltrate with eosinophils ± necrosis
r
Chronic rejection:
graft vasculopathy: concentric proliferative endarteritis with atheromatoid features
myocardial cellular rejection
myocyte vacuolisation / coagulative necrosis
parenchymal fibrosis and atrophy
r
Humoural rejection:
= donor Ab-mediated vascular endothelial damage occurring during the acute and chronic
rejection time periods (manifest as graft dysfunction not attributable to cellular rejection or
ischaemia on endomyocardial biopsy)
PMN/M in capillaries, endothelial swelling, congest
n
/haemorrhage, interstitial oedema
immuno: C4d +vity in capillary endothelia (becomes negative as humoural rejection resolves)
r
The presence of contraction band necrosis is said to be evidence against rejection if this is the only
feature but within the context of a picture of acute rejection it is considered to be one form of ‘myocyte
damage’ for grading purposes
r
Opportunistic infection (if present, rejection cannot be reliably assessed):
uncommon but important to exclude due to implications for immunosuppression Rx
CMV: serology is best as inclusions tend to be cytoplasmic only and fragmented
Toxoplasma: ! do not confuse intracellular granular Ca
2+
for Toxoplasma (do von Kossa)
a prominent PMN component should raise suspicion for infection
r
Grading acute cellular rejection (Billingham et al., 1990; Stewart et al., 2005):
PIC
JWBK208-07 December 8, 2007 16:1 Char Count= 0
Heart 78
TABLE 7.1 Grading acute cellular rejection
2004 Revised ISHLT Myocyte Other
Grade Grade Damage
a
Large Lymphocytes Granulocytes Features
mild
⎧
⎨
⎩
1R
1R
1R
1A absent multifocal (perivasc./interstitial) absent
1B absent diffuse but sparse absent
2 1 focus only present absent
mod. 2R 3A multifocal multifocal absent
severe
3R
3R
3B multifocal more diffuse present
4 present diffuse diffuse oedema, vasculitis,
haemorrhage
a
myocytedamageincludesmyocyteswithirregularborderduetoencroachmentbyinflam
y
cells,architecturaldsturbance,
partial replacement of myocytes or myocyte necrosis (incl. contraction band necrosis)
r
For updates and illustrations see: University of Pittsburgh Transplant Internet Service
(www.tpis.upmc.edu) and Slootweg & de Weger (1998).
Non-Inflammatory Heart Disease
Infiltrates / Deposits
r
Amyloid
r
Iron: haemochromatosis
r
Calcium: calcinosis
r
Oxalate: oxalosis
r
Storage diseases (e.g. in rhabdomyomas or in glycogenosis Type 2 = Pompe’s disease)
Hypertrophic Obstructive Cardiomyopathy (HOCM)
r
All ages (even elderly, esp. if assoc
d
with myosin binding protein mutation). Macro may look normal
r
Thickened endocardial patch with sharp lower border on the LV side of the septum is said to be
pathognomonic (if present)
r
‘Disarray’ is the hallmark feature:
present in ≥2 blocks (away from the insertion of the LV into the septum)
fibre bundle disarray: loss of parallel arrangement and presence of fibroid-like whorls
myocyte disarray: bizarre shapes and nuclear pleomorphism
myofibrillar disarray: do a PTAH stain
r
Interstitial fibrosis
r
The RV is involved in ≈
1
3
of cases
Arrythmogenic Right Ventricular Dysplasia (ARVD)
See Chapter 25: Autopsy.
Syndromic Conditions
The Marfan Syndrome / Cystic Medial Necrosis / Floppy Mitral Valve
r
Aorta: disorganisation of the media
disruption of medial elastic fibres
pools of AB +ve MPS
r
Valves: disruption of lamina fibrosa and elastica
pools of acid MPS
thickened and opaque cusp may develop 2
◦
infective endocarditis
Pseudoxanthoma Elasticum
r
Irregularly thickened and fragmented elastic fibres (in arteries and subendocardially)
r
Fibrosis
Sudden Cardiac Death, Congential Heart Disease, Examination of the Heart
See Chapter 25: Autopsy.
