Markovchick Vincent J., Pons Peter T., Bakes Katherine M.(ed.) Emergency medicine secrets. 5th ed
Подождите немного. Документ загружается.

Chapter 30 CARDIAC DYSRHYTHMIAS, PACEMAKERS, AND IMPLANTABLE DEFIBRILLATORS218
BIBLIOGRAPHY
1. 2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency
Cardiovascular Care. Part 7.3: Management of symptomatic bradycardia and tachycardia. Circulation 112:
IV-67–IV-77, 2005.
2. Baerman J, Morady F, DiCarlo L Jr, et al: Differentiation of ventricular tachycardia from supraventricular
tachycardia with aberration: value of the clinical history. Ann Emerg Med 16(1):40–43. 1987.
3. Bocka JJ: External transcutaneous pacemakers. Ann Emerg Med 18:1280–1286, 1989.
4. Buxton A, Marchlinski FE, Doherty JU, et al: Hazards of intravenous verapamil for sustained ventricular
tachycardia. Am J Cardiol 59(12):1107–1110, 1987.
5. Cardall TY, Brady WJ, Chan TC, et al: Permanent cardiac pacemakers: issues relevant to the emergency
physician: Part II. J Emerg Med 17:697–709, 1999.
6. Gillis AM: The current status of the implantable cardioverter defibrillator. Annu Rev Med 47:85–93, 1996.
7. Glikson M, Hayes DL: Cardiac pacing: a review. Med Clin North Am 85:369–421, 2001.
8. Harken AH, Honigman B, Van Way C: Cardiac dysrhythmias in the acute setting: recognition and treatment
(or) anyone can treat cardiac dysrhythmias. J Emerg Med 5:129–134, 1987.
9. Holdgate A, Foo A: Adenosine versus intravenous calcium channel antagonist for the treatment of
supraventricular tachycardia in adults. Cochrane Database Syst Rev Oct 18;(4):CD005154, 2006.
10. Hood R, Shorofsky S: Management of arrhythmias in the emergency department. Cardiol Clin 24(1):125–133,
2006.
11. Kudenchuk P, Cobb L, Copass M, et al: Transthoracic Incremental Monophasic vs Biphasic Defibrillation in
Emergency Responders (TIMBER). A randomized comparison of monophasic with biphasic waveform
ascending energy defibrillation for the resuscitation of out-of-hospital cardiac arrest due to ventricular
fibrillation. Circulation 114:2010–2018, 2006.
12. Sarko JA, Tiffany BR: Cardiac pacemakers: evaluation and management of malfunctions. Am J Emerg Med
18:435–440, 2000.
13. Steinman R, Herrera C, Schuger C, et al: Wide QRS tachycardia in the conscious adult. Ventricular tachycardia
is the most frequent cause. JAMA 261(7):1013–1016, 1989.
14. Stewart JA: Questions remain about shocking asystole [correspondence]. Am J Emerg Med 14(3):337–338, 1996.
15. Trohman R, Kim M, Pinski S: Cardiac pacing: the state of the art. Lancet 364(9446):1701–19, 2004.
16. Van Alem A, Chapman F, Lank P, et al: A prospective, randomized and blinded comparison of first shock success
of monophasic and biphasic waveforms in out-of-hospital cardiac arrest. Resuscitation 58(1):17–24, 2003.
17. Weigner MJ, Caulfiel TA, Danias PG, et al: Risk for clinical thromboembolism associated with conversion to
sinus rhythm in patients with AF lasting less than 48 hours. Ann Intern Med 126:615–620, 1997.
50. Name the most frequent type of AICD malfunction.
Inappropriate cardioversion.
51. What will a magnet do when placed over an AICD?
Use of a magnet over the AICD inhibits further shocks, but it does not inhibit bradycardic
pacing should the patient require it. In older devices, application of a magnet produces a beep
for each QRS complex. If the magnet is left on for 30 seconds, the AICD is disabled, and a
continuous tone is produced. To reactivate the device, the magnet is removed and replaced.
After 30 seconds, a beep returns for every QRS complex.
219
HYPERTENSION, HYPERTENSIVE CRISIS,
AORTIC DISSECTION, AND AORTIC ANEURYSMS
CHAPTER 31
Björk Ólafsdóttir , MD, and Bo E. Madsen, MD
1. Describe the blood pressure (BP) classification system used by the latest
Joint National Committee (JNC 7) report.
Hypertension class is defined as:
n
Normal BP ,120/80 mm Hg
n
Prehypertension systolic blood pressure (SBP) 120–139 mm Hg or diastolic blood
pressure (DBP) 80–89 mm Hg
n
Stage 1 hypertension: SBP 140–159 mm Hg or DBP 90–99 mm Hg
n
Stage 2 SBP .160 mm Hg or DBP .100
2. Describe the importance of anti-hypertensive treatment from a public
health perspective.
Hypertension (HTN) is common. A 55-year-old normotensive patient has a 90% lifetime
risk of developing hypertension. Treating hypertension has a significant impact on
mortality and morbidity and has been associated with a 35% reduction in stroke
incidence, a 20% reduction in myocardial infarction (MI), and a 50% reduction in heart
failure. It is estimated that by achieving a SBP reduction of 12 mm Hg for 10 years in
patients with stage I hypertension and additional cardiovascular risk factors, it will
prevent one death for every 11 patients treated.
3. Should treatment be initiated in asymptomatic patients with elevated BP?
Generally not. It has been found that a significant number of patients even with BP .160
in the ED will not have hypertension on follow-up visits. However, if no follow-up can
be arranged and the physician feels compelled to initiate treatment, it is recommended
to start a thiazide diuretic in the absence of renal or cardiac disease. For patients with
SBP .180 mm Hg or DBP .110 mm Hg, consideration should be given to starting an
antihypertensive agent. Patients with SBP .200 mm Hg or DBP .120 mm Hg should
be started on an antihypertensive agent at discharge.
4. Is ED diagnostic testing necessary in a patient with elevated BP and no
symptoms?
Testing is generally not necessary because these patients should receive urgent
follow-up with a primary care physician who can confirm the diagnosis and perform
diagnostic studies. However, if outpatient treatment is to be started by the emergency
physician, a basic metabolic profile is recommended.
5. What is the difference between primary and secondary HTN?
Essential or primary HTN accounts for more than 90% of patients with true HTN, and
the cause is unknown. Its etiology is likely multifactorial, a combination of both genetics
and environment.
Secondary HTN has an identifiable cause. It can result from:
n
Primary neurologic disorders (increased intracranial pressure [ICP])
n
Renal disorders (glomerulonephritis, polycystic kidney disease, chronic
pyelonephritis)
Chapter 31 HYPERTENSION, HYPERTENSIVE CRISIS, AORTIC DISSECTION, AND AORTIC ANEURYSMS220
n
Vascular disorders (coarctation of the aorta, renal artery stenosis)
n
Endocrine disorders (Cushing’s syndrome [increased cortisol], Conn syndrome [increased
aldosterone], pheochromocytoma [increased catecholamines], thyroid disorders
n
Pregnancy-induced HTN, that is, preeclampsia and eclampsia
n
Sleep apnea
6. List other causes of transient HTN.
Anxiety, pain, illicit drug use (i.e., cocaine, amphetamines, phencyclidine [PCP], or lysergic
acid diethylamide [LSD]), over-the-counter medications containing sympathomimetics, certain
toxidromes, alcoholism, and alcohol withdrawal. In addition, certain foods containing large
amounts of tyramine can cause transient hypertension. The combination of tyramine-
containing foods and monoamine oxidase inhibitors (MAOIs) can cause prolonged severe
HTN. MAOIs, in combination with certain drugs (i.e., meperidine, tricyclic antidepressants
[TCAs], ephedrine, and amphetamines), can also cause severe hypertension.
7. Define hypertensive emergency/crisis and list some examples.
It is defined as severely elevated BP with acute end-organ damage. Examples include
hypertensive encephalopathy; ischemic and hemorrhagic stroke; subarachnoid hemorrhage
(SAH); cerebrovascular accident (CVA); acute myocardial infarction (AMI); congestive heart
failure (CHF); aortic dissection; acute renal failure (ARF); and preeclampsia/eclampsia.
8. How does hypertensive urgency differ from hypertensive emergency?
With hypertensive urgency, a patient has very high BP but no evidence of acute end-organ
damage. There may be a history of chronic HTN and chronic end-organ damage, but if there is
no acute worsening, it is classified as an urgency.
9. What symptoms might be present in a patient with hypertensive
emergency?
The signs and symptoms of hypertensive crisis are manifestations from the organ systems
involved. Central nervous system involvement may cause headache, lethargy, dizziness,
confusion, focal neurological deficits, paresthesias, or vision changes and, if left untreated,
this can progress to seizures, blindness, and coma. Chest pain, back pain, shortness of
breath, and lower extremity swelling may reveal cardiovascular compromise. Decreased urine
output, nausea, and generalized malaise and weakness may suggest ARF.
10. What signs support the diagnosis of hypertensive crisis?
Confusion, altered level of consciousness, and focal neurologic findings concurrent with
arteriovenous (AV) nicking, copper-wiring, flame-shaped hemorrhages, exudates, and
papilledema on funduscopy examination. Crackles, hepatomegaly, and lower extremity edema
may be present, as well as a gallop, jugular venous distension, and a displaced point of
maximal impulse.
11. What studies should be considered in a patient with a hypertensive
emergency?
n
If neurologic symptoms or examination findings are present, order a computed tomography
(CT) of the head to evaluate for hemorrhagic, ischemic stroke, hypertensive
encephalopathy, or SAH.
n
Obtain an electrocardiogram (ECG) to screen for hypertrophy, ischemia, or infarction and a
chest X-ray (CXR) to look for CHF and aortic dissection.
n
A troponin should be ordered in a patient with chest pain, back pain, shortness of breath,
confusion, or altered level of consciousness.
n
If there is concern for dissection, a stat CT angiogram should be obtained.
n
A chemistry panel will screen for renal failure, and a urine sample can be obtained to check
for protein, blood, and glucose.
Chapter 31 HYPERTENSION, HYPERTENSIVE CRISIS, AORTIC DISSECTION, AND AORTIC ANEURYSMS 221
12. How do I diagnose hypertensive encephalopathy?
The classic triad associated with hypertensive encephalopathy is altered mental status (AMS),
HTN, and papilledema. Symptoms are reversible with appropriate BP reduction but, if left
untreated, coma and death occur within hours.
13. Describe the pathophysiology of hypertensive encephalopathy.
With abrupt, severe elevations in BP, cerebral autoregulation fails. When this occurs, blood
flow to the brain is no longer controlled, causing overperfusion, vasospasm, cerebral
ischemia, and increased vascular permeability. This leads to cerebral edema and elevated ICP.
14. Why is it important to understand cerebral autoregulation?
Cerebral autoregulation works only within a certain range of mean arterial pressure (MAP), above
or below this pressure range cerebral blood flow (CBF) is significantly affected. CBF depends on
cerebral perfusion pressure (CPP) and cerebrovascular resistance (CVR); CBF 5 CPP/CVR. The
CPP is defined as MAP-venous pressure. Under normal conditions venous pressure is governed
by ICP. MAP 5 (2 3 DBP 1 SBP ) ÷ 3. To maintain CBF and CPP at relatively constant levels,
cerebral arteries vasoconstrict when MAP increases and vasodilate when MAP decreases. In
normotensive individuals, cerebral autoregulation maintains constant CBF between a MAP of
60 and 120 mm Hg. In hypertensive patients, the lower limit of autoregulation is higher than in
normotensive patients and, for both hypertensive and normotensive patients, the lower limit of
autoregulation has been found to be approximately 25% below the resting MAP.
15. In a patient with a hypertensive encephalopathy, how much should I decrease
the BP?
When treating hypertensive encephalopathy, it is recommended to carefully decrease the MAP
25% over the first hour.
16. How do I treat a patient with hypertensive encephalopathy?
One of several medications may be chosen. They work by different mechanisms but should
have three important properties in common:
n
An intravenous (IV) drip, enabling easy titration
n
Rapid onset
n
Short duration of action
IV nicardipine, labetalol, or esmolol are the current recommended medications.
17. What is the treatment threshold for hypertension in ischemic stroke?
Currently there is an absence of conclusive data regarding treatment of HTN in the setting of
ischemic stroke. The Stroke Council for the American Heart Association recommends cautiously
lowering the BP in ischemic stroke if the SBP is .220 or DBP is .120 mm Hg. If the patient is
a thrombolysis candidate, it is recommended to lower the BP to ,185/110 mm Hg. The decision
making regarding BP management should be done in close consultation with a neurologist or
neurosurgeon.
18. What are the recommendations regarding treatment of hypertension in
hemorrhagic stroke?
This is currently unclear. There are several ongoing trials aiming at clarifying this. The
importance is striking a balance between reducing BP to reduce hemorrhagic volume but
avoiding ischemia in the surrounding tissue for hypotension. The decision making regarding
BP management should be done in close consultation with a neurologist or neurosurgeon.
19. How do I treat HTN if associated with SAH?
There are no definitive data on what blood pressure is beneficial to the patient. However, most
try to achieve a SBP ,160. The medications used are labetalol, esmolol, and nicardipine.
Other modalities, such as analgesics for pain, should also be used.
Chapter 31 HYPERTENSION, HYPERTENSIVE CRISIS, AORTIC DISSECTION, AND AORTIC ANEURYSMS222
20. How do I treat a patient with severe HTN and evidence of pulmonary edema?
Start with standard treatment for pulmonary edema: oxygen, diuretics, and afterload reduction
with nitroglycerine, which will treat both the hypertension and pulmonary edema.
21. How do I treat a patient with severe HTN and chest pain due to ischemia?
Angina is often accompanied by severe HTN. Reduction of BP is crucial to decrease the work
of the myocardium and prevent ongoing ischemia. First-line treatment is IV nitroglycerin
combined with a b-blocker and morphine. If this fails to control BP, nicardipine or fenoldopam
can be added. Avoid nitroprusside because it can cause a coronary-steal phenomenon in
patients with coronary artery disease, causing increased mortality in the presence of an AMI.
22. What are the agents of choice in a patient with severe HTN and ARF?
IV fenoldopam is a dopamine-1-receptor agonist, which is short acting and has advantages
over traditional nitroprusside therapy. It increases renal blood flow, creatinine clearance,
sodium excretion, and diuresis, and there is no issue with potential cyanide toxicity. It is as
effective as nitroprusside with no reported adverse effects. It is, however, more costly. Other
reasonable alternatives include nicardipine and labetalol. Angiotensin-converting enzyme
(ACE) inhibitors should be avoided if bilateral renal artery stenosis has not yet been ruled out.
23. What should you always think about in a pregnant or postpartum woman with
HTN?
Preeclampsia! See Chapter 79.
24. What are the two types of antihypertensive medications that, if stopped
abruptly, can cause rebound HTN?
Short-acting sympathetic blockers, such as clonidine, and b-blockers.
25. What antihypertensive medications are contraindicated in a catecholamine-
induced hypertensive emergency?
b-blockers. b-receptor-induced vasodilation results in unopposed alpha-adrenergic
vasoconstriction and elevates BP further. In patients with concomitant cocaine ingestions,
b-blockers enhance coronary artery vasoconstriction, increase BP, fail to decrease heart rate,
decrease the seizure threshold, and increase mortality. Labetalol, an a- and b-blocker,
theoretically avoids the problem of unopposed alpha, but some sources say it may still cause
harm in patients with cocaine ingestion or pheochromocytoma. Antihypertensive agents that
can be used for treatment of a catecholamine-induced hypertensive emergency include
nicardipine, fenoldopam, phentolamine, and nitroprusside. However, most cocaine or
amphetamine-induced HTN responds to appropriate doses of benzodiazepines.
26. What about using oral agents to treat hypertensive emergencies?
They should not be used. The response is unpredictable, cannot be discontinued immediately,
or is rapidly titrated. Oral agents are preferable for use in patients with hypertensive urgencies
if it is needed to start an antihypertensive medication.
KEY POINTS: SPECIAL CONSIDERATIONS WITH HYPERTENSIVE
EMERGENCIES
1. Avoid precipitous or excessive drop in BP with cerebrovascular emergencies.
2. Start esmolol before nitroprusside with aortic dissections, or use labetalol.
3. Do not give pure b-blockers for catecholamine-induced hypertensive emergencies.
Chapter 31 HYPERTENSION, HYPERTENSIVE CRISIS, AORTIC DISSECTION, AND AORTIC ANEURYSMS 223
AORTIC DISSECTION
27. Is ischemia the only cause of chest pain to worry about in a hypertensive
patient?
No. Always think about the possibility of acute thoracic aortic dissection because this can be a
rapidly fatal cause of chest pain, and HTN is the most common risk factor. Other risk factors
include congenital heart disease, Ehlers-Danlos, Marfan syndrome, intra-aortic balloon pump
use, age, male gender, pregnancy, smoking, family history, stimulant use, or major trauma
(due to deceleration injury [not to be discussed here]).
28. What symptoms or signs may be present in a patient with thoracic aortic
dissection?
Classic symptoms include:
n
Sudden onset of severe chest pain and pain in the jaw/neck/interscapular region that is
most severe at onset and is often described as sharp, ripping, or tearing in quality.
n
Additionally the patient can experience propagating pain as the dissection progresses.
n
The patient often has high blood pressure on arrival.
n
Nausea, vomiting, diaphoresis, lightheadedness, and apprehension may be present.
n
Syncope can also be the presenting complaint, in some cases even the only symptom.
Proximal dissections may cause aortic regurgitation and tamponade.
n
Occlusion of aortic branches may cause AMI (coronary artery involvement); stroke (carotid
involvement); or paresthesias and arm pain (subclavian artery involvement), which may be
suggested by unequal bilateral arm pressures and unequal pulses.
n
Spinal artery occlusion will cause neurologic compromise, and hoarseness may result from
recurrent laryngeal nerve compression.
n
Chest pain unrelieved by large doses of narcotic analgesics should raise the concern for
this diagnosis.
n
Peak age: Proximal dissection: 50 to 55 years
n
Distal dissection: 60 to 70 years
29. What diagnostic studies should be done when thoracic aortic dissection is
suspected?
Order a CXR followed by a CT, magnetic resonance imaging (MRI), or transesophageal
echocardiography (TEE). CXRs are abnormal in more than 80% of the cases but the
abnormalities are non-specific. Spiral contrast enhanced CT is the most practical modality in
the ED because it is quick, accurate, and readily available. MRI is sensitive and specific, but
scan times are long and access to the patient during the study is limited. TEE is great for
determining involvement of the aortic valve and coronary arteries and can detect the
presence of pericardial effusion or tamponade, but emergent access to this study is likely
limited. Aortography, once considered the gold standard, is rarely used any longer as the
initial diagnostic study. If the patient is hypotensive, a bedside echocardiogram can rule out
pericardial effusion with tamponade. An ECG should be done to evaluate for AMI or
myocardial ischemia.
30. What findings on a CXR suggest thoracic aortic dissection?
Widened mediastinum, loss of the aortic knob, left pleural effusion, deviation of the trachea or
nasogastric tube to the right, apical pleural capping, and the calcium sign (displacement of the
intimal calcium layer in the aorta). The CXR can be normal in up to 20% of cases.
31. Describe the difference between type A and type B thoracic aortic dissections.
Type A dissections (60%) involve the proximal/ascending aorta and require emergent surgical
repair, whereas type B dissections (40%) affect the descending aorta (distal to the great
vessels) and are managed medically.
Chapter 31 HYPERTENSION, HYPERTENSIVE CRISIS, AORTIC DISSECTION, AND AORTIC ANEURYSMS224
32. How do I treat a patient with suspected aortic dissection?
Provide opioids in adequate doses for pain control. Start IV antihypertensive medications
immediately if hypertensive and call a cardiothoracic surgeon before the patient heads for the
scanner. ED therapy for both types of dissections aims to lessen the pulsatile load and shear
forces on the aorta. Rapid reduction of SBP to a range of 100 to 110 mm Hg is indicated.
Traditional therapy includes an IV b-blocker such as esmolol in combination with IV
nitroprusside. Esmolol is started before nitroprusside to prevent reflex tachycardia and
increased shear forces. Alternative treatment regimens include IV labetalol used as a single
agent and IV nicardipine or fenoldopam in place of nitroprusside. If the patient is hypotensive,
perform a bedside ultrasound to evaluate for pericardial tamponade. Pericardiocentesis can be
a life-saving, temporizing intervention until the patient reaches the operating room.
33. Describe the two different types of aortic aneurysms.
n
A true aneurysm, as seen with most abdominal aortic aneurysms (AAAs), involves dilation
of all three layers of the arterial wall: the intima, media, and adventitia.
n
In a pseudoaneurysm as is seen with acute thoracic aortic dissections, blood
communicates with the arterial lumen but is contained solely within the adventitia or
surrounding soft tissue. This is much less common.
34. Are aortic dissections and aortic aneurysms somehow related?
No. These two disease processes are totally unrelated, have different symptoms, require
different work-ups, and are managed differently. Aortic dissection is caused by a weakness/
tear of the intima leading to the formation of a false lumen within the media. Blood enters here
and dissects proximally, distally or both.
35. What risk factors are associated with aortic aneurysms?
Aneurysms result from a degenerative process that affects the aortic wall. Risk factors include:
tobacco use, hypercholesterolemia, HTN, male gender, family history, and advanced age. Other
rare causes include infection, such as tertiary syphilis (which leads to aneurysmal dilation in the
aortic root/ascending aorta), after blunt chest trauma (usually resulting in pseudoaneurysms),
patients with connective tissue diseases (such as Marfan syndrome and Ehlers-Danlos), and in
arteritis. Although true aneurysms can develop anywhere along the aorta, 75% are AAAs.
ABDOMINAL AORTIC ANEURYSM
36. What are common presenting signs and symptoms of an abdominal aortic
aneurysm (AAA)?
Most patients with AAAs are asymptomatic, and their aneurysm is found incidentally on physical
examination or on diagnostic studies done for other reasons. It is estimated that 2% to 3% of
men older than 50 years of age have an occult AAA. Approximately 75% of aneurysms .5 cm
can be palpated, but only 5% to 10% of patients with an AAA have an abdominal bruit. The
classical triad of ruptured AAA is pain, hypotension, and a pulsatile abdominal mass. Oftentimes
the patients only have one or two of these symptoms and sometimes none. A patient with an
acutely expanding or ruptured aneurysm will likely complain of constant abdominal pain, radiating
to the back, flank, chest, thigh, inguinal area, or scrotum. It is often described as dull, throbbing,
or colicky. Hypotension, syncope, or low hematocrit may signify significant blood loss.
37. What should I do when I suspect a ruptured AAA?
Place two large-bore IVs, type, and cross-match for at least six units of packed red blood cells,
and call a vascular surgeon. The goal should be to get the patient to the operating room (OR) as
soon as possible, and transport should not be delayed for definitive studies or to attempt full
resuscitation in the ED. A bedside ultrasound can be done quickly to screen for an AAA. The
ultrasound can confirm AAA but rarely detects rupture because most AAAs rupture into the
retroperitoneum. CT scans are only appropriate in hemodynamically stable patients, but have a

Chapter 31 HYPERTENSION, HYPERTENSIVE CRISIS, AORTIC DISSECTION, AND AORTIC ANEURYSMS 225
100% sensitivity for detecting AAA and 77% to 100% sensitivity for picking up retroperitoneal
bleeding. The CT can be performed without contrast if there is concern over the patient’s kidney
function. The mortality for elective repair of an unruptured AAA is approximately 5% as opposed
to a greater than 50% mortality associated with acute repair of an already ruptured AAA.
38. Discuss the dilemmas behind aggressive fluid resuscitation in a hypertensive
patient with ruptured AAA.
Unfortunately, no prospective studies exist to guide optimal fluid resuscitation, and the
appropriate amount of volume to give is controversial. Allowing some degree of hypotension
may slow bleeding, allow some clot formation and temporarily tamponade the bleeding; too
much fluid may have the opposite effect and may also cause an increased blood pressure and
a dilutional coagulopathy, further increasing bleeding. On the other hand, these patients likely
have other comorbid conditions that could be potentially fatal in the presence of prolonged
hypotension. The goal should be to maintain adequate perfusion to the vital organs, using
warm saline/blood without intentionally raising the BP above 90 to 100 mm Hg systolic.
39. What common diseases may mimic ruptured AAA?
Everything! Renal colic, syncope attributed to other causes, pancreatitis, perforated peptic
ulcer, AMI, gallbladder pathology, diverticulitis, appendicitis, perforated viscus, bowel
obstruction, musculoskeletal back pain, and intestinal ischemia. Thus, always consider this
diagnosis in the patients older than 50 years of age with any one of the symptoms in the
classic triad: pain, hypotension, and pulsatile mass.
40. When do you need to worry about an AAA?
The risk of rupture is minimal for an AAA measuring ,4 cm, but the risk increases
dramatically at diameters larger than .6 cm. The annual rupture risk for AAA 6 to 7 cm is
10% to 20%, from 7 to 8 cm 20% to 40% and, if .80 cm, the annual rupture risk is
increased to 30% to 50%. Rapid expansion is the greatest predictor of impending rupture, and
routine screening with known AAAs is important because it significantly affects mortality. All
patients with an AAA 5 cm or greater in diameter should have vascular surgery follow-up.
41. When should a symptomatic unruptured AAA be repaired?
This represents a dilemma. It has been found that the mortality associated with emergency
repair of symptomatic AAA is associated with about a 25% mortality as opposed to a 5%
mortality associated with semielective repair. The question is the risk of rupture in the interim.
42. List some atypical symptoms that may be related to the presence of an AAA.
n
Gastrointestinal bleeding in a patient with previous aortic repair may signify fistula
formation between the wall of the aorta and the small or large bowel.
n
A large aneurysm may cause mass effect on surrounding structures resulting in a bowel or
ureteral obstruction.
n
Radicular pain may occur if the bleeding is retroperitoneal. Leg ischemia may occur due to
peripheral embolization of mural plaques.
43. How are AAAs surgically repaired?
Traditional repair involves laparotomy and cross-clamping the aorta. A newer, less invasive
approach involves placement of a self-expanding stent graft via the femoral artery under
fluoroscopic guidance. This approach allows repair of AAA in a group of patients that would
not be candidates for AAA repair.
44. What are the complications of endovascular aortic repair (EVAR)?
Endovascular stent graft repair is an alternative to surgical repair. The short-term outcomes
seem equal or favorable to open repair. However, the longer-term mortality of patients who
have undergone EVAR seem to be equal to the open approach. Additionally, there is a higher
Chapter 31 HYPERTENSION, HYPERTENSIVE CRISIS, AORTIC DISSECTION, AND AORTIC ANEURYSMS226
reintervention rate and AAA rupture rate in the EVAR group. Many of the complications of
EVAR are similar to the complications of open surgical repair. Certain complications have
decreased in occurrence with the development of the technique and advance in materials
used. Complications include:
n
Graft infection, that can lead to aorto-enteric fistula (AEF) formation, commonly presenting
with upper gastrointestinal bleed
n
Limb occlusion
n
Device migration
n
Continued sac expansion (endotension)
n
Endoleak is the most frequent complication and occurs in up to one fourth of all patients
who have undergone EVAR. Some types of endoleaks place the patient at a higher risk of
AAA rupture.
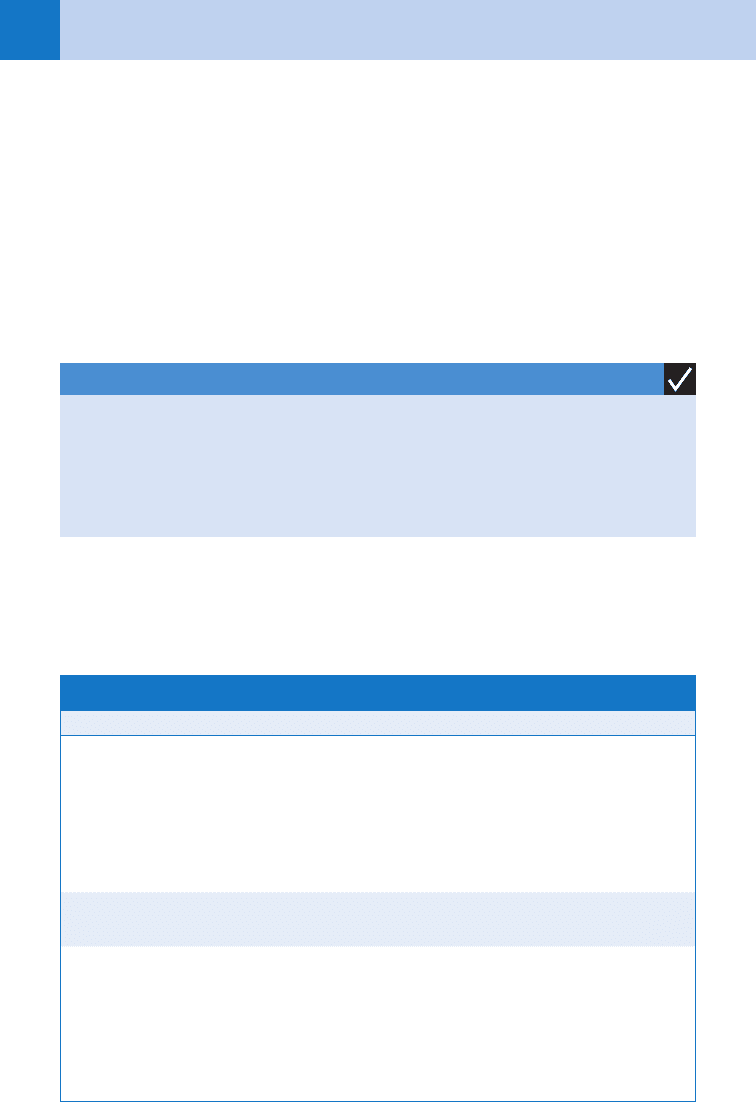
45. Summarize the common parenteral antihypertensive medications and their
indications and contraindications.
See Table 31-1.
KEY POINTS: ABDOMINAL AORTIC ANEURYSMS
1. The triad is abdominal pain, pulsatile mass, and hypotension.
2. Do not wait for a definitive study before calling surgery.
3. Bedside ultrasound is an excellent screening tool for AAA.
4. CT is the gold standard for making the diagnosis of a ruptured AAA.
Drug Dose Onset Duration Indications Contraindications
Nitroprusside 0.3–10
mg/kg/
min IV
1–2
min
1–2 min CHF, aortic
dissection,
catecholamine
excess,
hypertensive
encephalopathy
Pregnancy, AMI,
hepatic or renal
insufficiency,
caution with
increased ICP
Nitroglycerin 10–100
mg/min IV
2–5
min
3–5 min AMI, CHF CVA, ARF
Nicardipine 5–15
mg/hr IV
15
min
6 hours AMI, ARF,
eclampsia,
hypertensive
encephalopathy,
catecholamine
excess
CHF, second- or
third-degree AVB
TABLE 31–1. PARENTERAL ANTIHYPERTENSIVE MEDICATIONS
Continued
Chapter 31 HYPERTENSION, HYPERTENSIVE CRISIS, AORTIC DISSECTION, AND AORTIC ANEURYSMS 227
Drug Dose Onset Duration Indications Contraindications
Fenoldopam 0.1–1.7 mg/
kg/min IV
5–15
min
1–4
hours
AMI, CHF, ARF,
aortic
dissection,
hypertensive
encephalopathy,
catecholamine
excess
Glaucoma (can
cause increased
IOP)
Hydralazine 10–20 mg
IV bolus;
repeat every
4–6 hours
prn (max
40 mg)
10–20
min
3–8
hours
Eclampsia AMI, CVA, aortic
dissection
Esmolol 500 mg/kg
IV bolus
over 1 min,
then 50–300
mg/kg/min
1–2
min
10–20
min
CAD, aortic
dissection
CHF, second- or
third-degree AVB
Labetalol 20 mg IV
bolus, then
40–80 mg
every 10
min up to
300 mg or
2 mg/min IV
2–10
min
2–4
hours
CAD, aortic
dissection,
hypertensive
encephalopathy,
eclampsia
CHF, second- or
third-degree AVB,
asthma
Phentolamine 5 mg IV,
repeat prn
(max 20 mg)
1–2
min
10–30
min
Catecholamine
excess
AMI
AMI, acute myocardial infarction; ARF, acute renal failure; AVB, atrioventricular block; CAD, coronary artery
disease; CHF, congestive heart failure; CVA, cerebrovascular accident; ICP, intracranial pressure; IOP, intraocular
pressure; IV, intravenously; prn, as needed.
TABLE 31–1. PARENTERAL ANTIHYPERTENSIVE MEDICATIONS—cont’d
