Markovchick Vincent J., Pons Peter T., Bakes Katherine M.(ed.) Emergency medicine secrets. 5th ed
Подождите немного. Документ загружается.

208
CARDIAC DYSRHYTHMIAS, PACEMAKERS,
AND IMPLANTABLE DEFIBRILLATORS
CHAPTER 30
Christopher B. Colwell, MD, and Ashley C. Mull, MS, MD
1. What is a sinus beat?
At the end of each heartbeat, all myocardial cells are depolarized and experience a
refractory period. At this point, certain cardiac cells (sinoatrial and atrioventricular [AV]
nodes and some ventricular cells) float back up toward threshold potential. It is like a
race, and typically the sinoatrial node cells win this race, achieve threshold, fire, and
assume the pacemaker sinus beat function of the heart.
2. What is the AV node?
The AV node is not simply a passive connection between the atria and ventricles. It is
smart. Normally, all atrial impulses are conducted to the ventricles. When the ventricular
rate becomes sufficiently rapid that cardiac output is compromised, conduction velocity
begins to slow in the AV node. This progressive slowing filters the rapid atrial impulses so
that serial atrial impulses are not conducted at all. This progressive AV nodal conduction
block is a protective mechanism to prevent a dysfunctional rapid ventricular rate.
3. Is it necessary to identify a dysrhythmia before treating it?
If the patient is hemodynamically unstable, no. In the unstable patient, a general rule of
thumb: if the heart rate is fast, shock (perform electric cardioversion); and if the heart
rate is slow, pace.
4. What is hemodynamic compromise?
In an adult, hemodynamic compromise is hypotension (a systolic blood pressure ,90 mm
Hg) in combination with alteration in mental status, chest pain, or shortness of breath.
5. How do I know whether a patient’s dysrhythmia is causing hemodynamic
compromise?
Typically, if a patient’s ventricular rate is between 60 and 100 beats per minute, any
hemodynamic instability is caused by something else. It is unusual, although not
impossible, for a tachydysrhythmia with a rate less than 150 beats per minute to be the
primary cause of hemodynamic instability. It is extremely rare for a patient with a heart
rate less than 150 beats per minute to require electrical cardioversion.
6. How do I treat bradyarrhythmias?
Do not treat bradycardia if the patient is hemodynamically stable and asymptomatic.
Always treat the patient, not a number. If the patient has a heart rate less than 60 beats
per minute and is hemodynamically unstable:
n
Give 0.5 mg (0.01 mg/kg in a child) intravenous (IV) atropine (may be repeated).
n
Initiate pacemaker therapy, starting with external pacing. Placement of a transvenous
pacemaker (especially without fluoroscopy) always takes much longer than you think
it will.
7. How do I treat tachyarrhythmias?
Any unstable patient with a tachyarrhythmia that either is or may be the cause of the
hemodynamic instability requires electric cardioversion. Supraventricular tachycardia

Chapter 30 CARDIAC DYSRHYTHMIAS, PACEMAKERS, AND IMPLANTABLE DEFIBRILLATORS 209
(SVT) and atrial flutter often respond to low voltages (50 J), whereas most other
tachyarrhythmias typically require at least 100 J to convert to a sinus rhythm. If the patient is
hemodynamically stable, the next step is to identify whether the tachyarrhythmia is narrow-
complex or wide-complex.
8. What is a narrow-complex tachycardia?
The AV node conducts impulses directly to the Purkinje system, which courses over the
endocardial surface of the ventricles. An electrical impulse travels along the Purkinje fibers
quickly: 2 to 3 m/sec. If an impulse enters the ventricles from the AV node, it can rapidly
activate the entire ventricular muscle mass—in 0.12 sec, 120 msec, or three little boxes on
electrocardiogram (ECG) paper. We see this as a narrow-complex QRS on the ECG: a QRS
complex with a width of less than 120 msec. A narrow-complex tachycardia must originate
above the AV node. Sinus tachycardia, SVT, atrial fibrillation (AF) with rapid ventricular
response, and atrial flutter are examples of narrow-complex tachycardias.
9. How do I make the diagnosis of AF when the ventricular rate is fast?
AF is by definition an irregular rhythm, but very rapid AF may appear regular and be impossible
to differentiate from SVT on a cardiac rhythm strip. The diagnosis of AF is made by palpating a
peripheral pulse and simultaneously auscultating the heart or visualizing the cardiac rhythm. AF
is the only arrhythmia that results in a pulse deficit (fewer beats palpable than observed or
auscultated) and that has an irregular pulse with varying intensity of the pulse.
10. How do I treat narrow-complex tachycardia in a hemodynamically stable
patient?
A narrow-complex tachycardia must originate above the AV node. To control the ventricular
rate, you need to block the AV node pharmacologically. If the patient has a rapid narrow-
complex tachycardia that cannot be definitively identified, the best initial agent is adenosine,
6 mg IV rapid bolus followed by 12 mg, if needed (which also may be repeated). For SVT,
adenosine has a response rate of 85% to 90%, few serious side effects, and a very short
half-life. Alternatively, verapamil, 5 to 10 mg, or diltiazem, 20 mg, intravenously over to 1–2
minutes, terminates or controls the ventricular response rate in 80% to 90% of cases. If the
patient clearly has AF, rate control, rather than conversion to a sinus rhythm, is the primary
goal. b-blockers (metoprolol, 5–10 mg over 2 minutes) and calcium channel blockers
(diltiazem, 20 mg over 2 minutes) are effective AV nodal blocking agents and can achieve
adequate rate control in most patients with AF. Patients may experience chest tightness,
nausea, and shortness of breath with adenosine and should be warned about these
temporary unpleasant effects. Rarely, calcium channel blockers can cause hypotension, and
there are case reports of life-threatening events after administration of adenosine, so it is
important to have good IV access and an advanced cardiac life support (ACLS) cart nearby
when giving any of these agents. Adenosine exhibits little effect on infranodal conduction,
which has led some authors to recommend its use as a diagnostic agent in wide-complex
tachycardias.
11. Is there a time when I shouldn’t use adenosine or a calcium channel blocker
for a narrow-complex tachycardia?
The one situation where it would be potentially dangerous to use these agents is AF in the
setting of Wolff-Parkinson-White syndrome (WPW). In this disorder, there is an accessory
pathway between the atria and the ventricles that bypasses the AV node. If an AV nodal
blocking agent is given, conduction through the accessory pathway could speed up, making
the tachycardia worse and potentially precipitating hemodynamic collapse. AF in WPW can
present as narrow- or wide-complex tachycardia. It is difficult to tell on the ECG if someone
has WPW if the rhythm is very fast, but if the patient has a known history of WPW, do not
give adenosine or a calcium channel blocker. Procainamide or electricity should be used
instead.

Chapter 30 CARDIAC DYSRHYTHMIAS, PACEMAKERS, AND IMPLANTABLE DEFIBRILLATORS210
12. Define premature ventricular contraction.
A premature ventricular contraction occurs when a ventricular site wins the race among
myocardial cells and ventricular depolarization originates from an ectopic ventricular site.
13. What is a wide-complex tachycardia?
When an impulse originates from damaged or ischemic ventricular muscle instead of the
sinoatrial or atrioventricular node, it does not use the Purkinje superhighway of conduction
and therefore takes longer to activate the ventricular mass: .0.12 second, 120 msec, or three
little boxes on the ECG paper. We see this as a wide complex QRS complex.
14. What is the most common cause of wide-complex tachycardia?
Ventricular tachycardia (VT). Of awake patients presenting to the ED with a wide complex
tachycardia, 70% to 90% have VT, and only 10% to 30% have supraventricular tachycardias
with aberrancy (see question 16). VT is even more likely if the patient has a history of a prior
myocardial infarction or congestive heart failure. Other causes of wide-complex tachycardia
include ventricular fibrillation (VF), a wide-complex, irregular, nonperfusing rhythm that
requires electrical defibrillation; and torsades de pointes, a wide-complex rhythm associated
with prolonged QT interval.
15. Is VT always hemodynamically unstable?
No. Hemodynamic status should not be used to determine the nature of a wide QRS
tachycardia: Do not assume a wide-complex tachycardia is not VT if the patient is
hemodynamically stable.
16. What is a supraventricular rhythm with aberrancy?
Usually a supraventricular rhythm traverses the AV node and courses through the large
endoventricular conduction fibers, activating the ventricles rapidly and resulting in a
narrow QRS complex (,0.12 sec). A wide-complex tachycardia typically represents a
tachycardia of ventricular origin. Although less frequent, a supraventricular origin impulse
that travels through the ventricle in an aberrant fashion also can be wide and is called
supraventricular rhythm with aberrancy. One example, as discussed in Question 11, is AF
in the setting of WPW; this is a supraventricular arrhythmia that can present as a narrow-
or wide-complex tachycardia depending on the direction of conduction through the
accessory pathway.
17. Differentiate VT from SVT with aberrancy based on findings on the 12-lead
ECG.
In general, assume VT and treat accordingly whenever there is any question. These findings
on the 12-lead all strongly suggest VT:
n
AV dissociation
n
Fusion or capture beats
n
Left or right axis deviation
n
QRS width of greater than 140 msec
n
Concordance of QRS complexes
n
Monophasic or biphasic QRS in lead V1
n
RS or QS in lead V6
n
History of coronary artery disease or congestive heart failure
n
Evidence of AV dissociation on physical examination (Cannon A waves)
Heart rate is not an accurate way to differentiate VT from SVT with aberrancy. Again, if there is
any doubt, assume VT. Treating SVT with aberrancy as if it were VT is less problematic than
treating VT as if it were SVT with aberrancy.
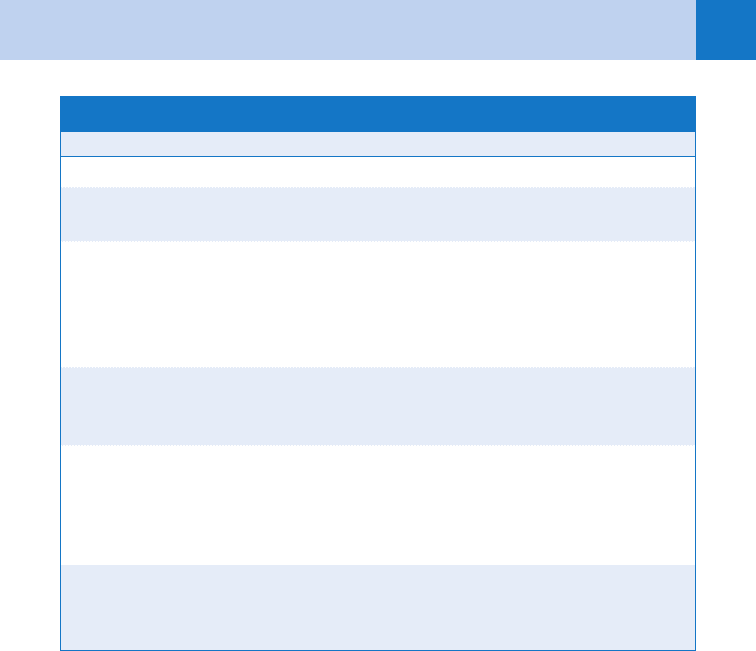
18. How do I treat wide-complex tachycardia?
See Table 30-1.
Chapter 30 CARDIAC DYSRHYTHMIAS, PACEMAKERS, AND IMPLANTABLE DEFIBRILLATORS 211
19. What does amiodarone do?
Amiodarone is a class III antiarrhythmic that, among other effects, prolongs the action
potential duration and refractory period, slows automaticity in pacemaker cells, and slows
conduction in the AV node. It is approved for the treatment of ventricular and supraventricular
arrhythmias, including AF, atrial flutter, and accessory pathway syndromes. Current ACLS
guidelines suggest amiodarone be used as a first-line agent for stable VT, and it is also a good
option to consider in a hemodynamically stable patient with a wide-complex tachycardia of
unknown mechanism. Primary side effects are hypotension and bradycardia. The loading dose
for adults is 150 mg intravenously given over 10 to 15 minutes. Amiodarone exhibits a slow
onset of action and an even slower clearance.
20. What drug is contraindicated in the treatment of any wide-complex
tachycardia?
Verapamil. Because all wide-complex tachycardias must be considered to be of ventricular
origin, verapamil carries a high risk of causing hypotension and may cause degeneration of
the rhythm to VF or asystole.
21. What is synchronized cardioversion?
Synchronization of delivered energy to match the QRS complex. This reduces the chance that
a shock will induce VF, which can occur when electrical energy impinges on the relative
refractory portion of the cardiac electrical activity (down slope of the T wave).
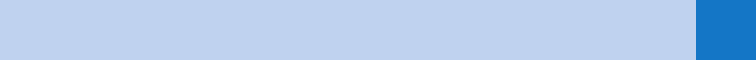
TABLE 30-1. TREATMENT OF WIDE-COMPLEX TACHYCARDIA
Clinical Situation Treatment
Unstable patient Cardioversion
Wide-complex tachycardia known to be
SVT with aberrancy
Adenosine (6 mg intravenous push followed by
12 mg intravenous push if ineffective)
Wide-complex tachycardia of unknown
type with preserved cardiac function (no
clinical signs of congestive heart failure)
Amiodarone (150 mg IV given over 10–15 min-
utes) or procainamide (17 mg/kg IV at a rate of
20 mg/min, to be stopped if the dysrhythmia is
suppressed, hypotension occurs, or the QRS
complex widens by 50% of its original width)
Wide-complex tachycardia of unknown
type in a patient with clinical evidence of
congestive heart failure
Amiodarone
Rhythm known to be ventricular in origin Amiodarone, procainamide, or lidocaine (1.0 to
1.5 mg/kg IV, repeated every 5 minutes to a maxi-
mum of 3 mg/kg; consider magnesium
(2 g IV) if torsades de pointes suspected
IV, intravenously; SVT, supraventricular tachycardia.
Adapted from Shah CP, Thakur RK, Xie B, et al: Clinical approach to wide QRS complex tachycardias. Emerg
Med Clin North Am 16:331–360, 1998.

Chapter 30 CARDIAC DYSRHYTHMIAS, PACEMAKERS, AND IMPLANTABLE DEFIBRILLATORS212
22. How do I perform synchronized cardioversion?
n
Apply the defibrillation pads to the patient: one attaches to the anterior chest and the other
is placed on the patient’s back.
n
Turn on the defibrillator.
n
Select a lead on the monitor that clearly reveals an R wave of greater amplitude than the
T wave.
n
Engage the synchronization mode by pressing the sync control button, and look for
markers on the R waves indicating the sync mode is functioning and capturing the QRS
complex and not the T wave.
n
You may need to adjust the R wave again until the sync markers occur with each QRS
complex. Then select the appropriate energy level.
n
Always remember to use adequate sedation in an awake patient. (If you are using defibrillation
paddles, coat both paddles with conductive gel and apply 25 lbs. of downward pressure.)
23. Does it make sense to cardiovert asystole?
Strictly speaking, no. Theoretically, electrical cardioversion synchronously depolarizes all
myocardial cells simultaneously. All cells then should repolarize synchronously and spontaneously
reinitiate sinus rhythm. With asystole, there is nothing to depolarize and nothing to cardiovert.
Although the American Heart Association currently does not recommend the routine shocking of
asystole, there are two scenarios when cardioversion of apparent asystole may be helpful.
n
Conceivably, if the major QRS vector is perpendicular to the axis of the ECG lead, VF may
appear as asystole.
n
It is also possible to have a fine (very low voltage) VF, which is difficult to distinguish from
asystole on the monitor.
If available, a bedside ultrasound of the heart is useful in these circumstances.
24. When is it necessary to anticoagulate a patient with AF prior to
cardioversion?
Anticoagulation in patients who have AF for less than 48 hours is unnecessary because the
risk of thromboembolism is lower. If the duration of AF has been greater than 48 hours and
the patient is stable, cardioversion may be delayed until the patient is fully anticoagulated.
25. Should we be using monophasic or biphasic waveform defibrillation in the ED?
Theoretical advantages to biphasic waveforms include less energy required to achieve effective
defibrillation and less postshock myocardial damage and dysfunction at equivalent energy
levels. A study published in 2003 showed that biphasic waveforms were more likely to achieve
a return to an organized rhythm with one shock than monophasic waveforms but did not see
any statistically significant difference in overall survival. A more recent study saw trends toward
the requirement for fewer shocks, faster return of spontaneous circulation, and improved
survival rates with biphasic waveforms. Despite these promising results, more research is
needed to establish a clear, clinically significant benefit to biphasic waveform defibrillation.
26. What is a pacemaker?
An external source of energy used to stimulate the heart. It consists of a pulse generator
(i.e., power source), an output circuit, a sensing circuit, a timing circuit, and pacing leads. In
the ED, pacing is performed via a temporary external or transvenous pacemaker. Longer-term
therapy requires the placement of a surgically implanted device. It is often possible to palpate
these devices on physical examination; they are also visible as radiopaque foreign bodies on a
chest radiograph.
27. What are the indications for temporary pacemakers?
Temporary emergency pacing is indicated for therapy of significant and hemodynamically
unstable bradyarrhythmias and prevention of bradycardia-dependent malignant arrhythmias.
In symptomatic or unstable patients who don’t respond to atropine or other
Chapter 30 CARDIAC DYSRHYTHMIAS, PACEMAKERS, AND IMPLANTABLE DEFIBRILLATORS 213
pharmacotherapies, emergency pacing should be initiated immediately for any of the following
rhythms:
Sinus node dysfunction
n
Sinus bradycardia
n
Sinus pauses .3 seconds
AV nodal block
n
Second-degree AV block (Mobitz I)
n
Complete heart block
Infranodal block
n
New bifascicular block associated with AMI
n
Alternating bundle-branch block with changing PR interval
n
Complete heart block
Pacemakers also can be used for overdrive pacing in an attempt to terminate VT by placing a
ventricular extrasystole during the vulnerable period of the cardiac cycle. Prophylactic
temporary pacing is indicated for insertion of a pulmonary artery catheter in a patient with an
underlying left bundle-branch block or use of medications that may cause or exacerbate
hemodynamically significant bradycardia.
28. Where are external/transcutaneous pacemakers placed? How are they
operated?
Pacing pads and monitor leads are placed preferably in the midanterior chest and just
below the left scapula. The desired heart rate is chosen, and the current is set to 0 mA.
The external pacemaker is turned on, and the current is increased as tolerated until capture
is achieved.
29. State the limiting factors in the use of external pacemakers.
Skeletal muscle contraction can be uncomfortable and often limits use of external pacemakers.
Placing electrodes over areas of least skeletal muscle may minimize the discomfort. The
physician should use the lowest effective current. Sedation should be strongly considered if
these measures are inadequate.
30. Can an external pacemaker be used if a permanent pacemaker malfunctions?
Yes, but be careful to place the external pacer on a pace only (fixed-rate) mode and not the
sensing mode; otherwise, it may sense spikes from the permanent pacemaker and not fire.
31. What are the advantages of transvenous versus transcutaneous pacemakers?
Transcutaneous leads are the easiest to use for rapid initiation of temporary pacing.
Transvenous leads are more reliable and more comfortable because external pacing requires
30 to 100 times the current needed for internal transvenous pacing.
32. How are transvenous and transthoracic pacemakers placed?
Semifloating or flexible balloon-tipped catheters can be placed with central venous access into
the subclavian or internal jugular veins. In the ED, using ECG guidance, an alligator clip is
connected to a precordial lead such as V
1
with another clip attached to the pacing wire. When
a current of injury (ST elevation) is seen on the monitor, the wire should be withdrawn
slightly, leaving it in pacing position. If available, fluoroscopy is preferred to ensure proper
placement.
33. Can cardiopulmonary resuscitation (CPR) be performed with a pacemaker?
CPR can be performed safely with the external pacing pads in place. Turning the external
pacemaker off during CPR is advisable, in particular when defibrillating or cardioverting a
patient. If using separate defibrillator paddles, they should be placed at least 2 to 3 cm away
from pacing pads to prevent arching of current.
Chapter 30 CARDIAC DYSRHYTHMIAS, PACEMAKERS, AND IMPLANTABLE DEFIBRILLATORS214
34. List the indications for a permanent pacemaker.
Indications for permanent pacing are constantly evolving. Currently, permanent pacing is
indicated for:
n
Sick sinus syndrome
n
Symptomatic sinus bradycardia
n
Tachycardia-bradycardia syndrome
n
AF with a slow ventricular response
n
Complete heart block
n
Chronotropic incompetence (inability to increase the heart rate to match a level of
exercise)
n
Long QT syndrome
More controversial applications include:
n
Cardiomyopathies (hypertrophic or dilated)
n
Congestive heart failure (cardiac resynchronization therapy [CRT])
n
Severe refractory neurocardiogenic syncope
n
Paroxysmal AF (atrial pacing)
35. Describe the complications of permanent pacemaker implantation.
Routine placement of a pacemaker generator into a subcutaneous or submuscular pocket
carries the risk of pocket hematoma, which if large enough to palpate often needs surgical
drainage. Pocket infection can also occur and manifests as local inflammation, fluctuance, and
abscess formation or local cellulitis. Rarely, the pocket itself may erode with extrusion of the
generator secondary to infection, trauma, or local tissue ischemia. Infection usually is caused
by Staphylococcus aureus acutely and Staphylococcus epidermidis in chronic infections.
Treatment is empiric antibiotics and ultimately removal of the device and reimplantation at a
remote site. Wound dehiscence may require admission for debridement and reapproximation of
wound edges.
36. What does a pacer setting of DDD mean?
The letters represent a pacing code. The code consists of five letters that describe the
different types of pacer function; the first three letters are the most relevant to the
emergency physician (see Table 30-2). The first letter indicates the chamber paced; the
second indicates the chamber in which electrical activity is sensed, and the third indicates
the response to a sensed event. A fourth and fifth letter may be added to describe whether
the pacemaker is programmable and whether special functions to protect against
tachycardia are available. A DDD pacer is able to pace and sense atria and ventricles ([D]
ual chambers) and has a (D)ual response to the sensed ventricular and atrial activity (i.e.,
can pace either the atrium or the ventricle). Spontaneous atrial and ventricular activity
inhibits atrial and ventricular pacing; atrial activity without ventricular activity triggers only
ventricular pacing.
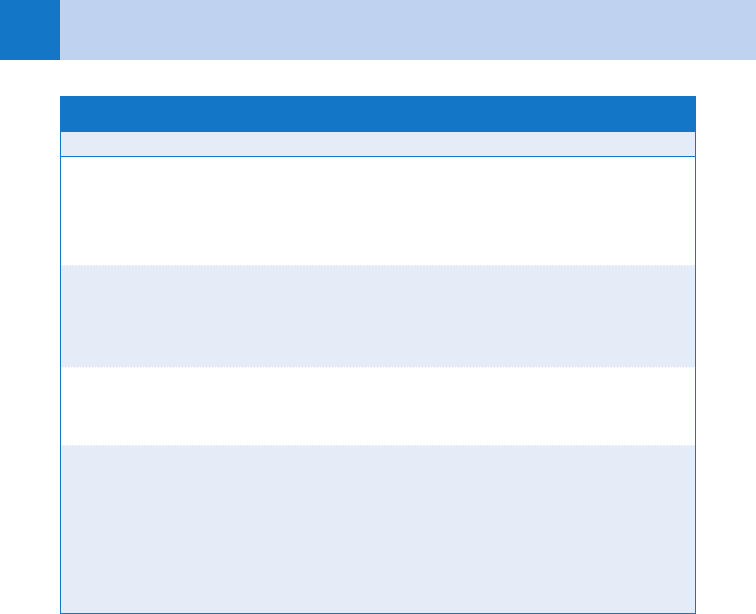
TABLE 30-2. MODIFIED PACING CODE
First Letter: Chamber
Paced to a Sensed Event
Second Letter:
Chamber Sensed
Third Letter: Response
to Sensed Event
A (atrium) A (atrium) I (inhibition)
V (ventricle) V (ventricle) T (triggering)
D (dual chamber) D (dual chamber) D (dual response)
O (none) O (none) O (no response)
Chapter 30 CARDIAC DYSRHYTHMIAS, PACEMAKERS, AND IMPLANTABLE DEFIBRILLATORS 215
37. How can the type of permanent pacemaker be identified in the ED?
Patients should carry a card with them providing information about their particular model.
Most pacemaker generators have an X-ray code that can be seen on a standard chest
radiograph. The markings, along with the shape of the generator, may assist with determining
the manufacturer of the generator and pacemaker battery.
38. What is the most common cause of permanent pacemaker malfunction?
Lead dislodgement. Today, most pacemaker failures are the result of problems with the
electrodes or the wires, not the battery or the pulse generator. Because of greater technologic
sophistication, patients with pacemaker problems present to the ED much less commonly now
than in the past.
39. What is the most reliable indicator of pacer malfunction?
Rates that are usually inappropriate for paced hearts. A nonpaced ventricular rate less than 60
beats per minute or a paced rate greater than 100 beats per minute is probably secondary to
pacemaker malfunction.
40. What does a magnet do?
Placing a pacemaker magnet over the pulse generator stops the pacemaker from sensing or
responding to a sensed event. The pacemaker reverts to one of three fixed rate modes:
n
AOO (atrium paced)
n
VOO (ventricle paced)
n
DOO (atrium and ventricle paced)
The purpose is to check the pacing rate, which should be done quickly because the pulse
generator is no longer prevented from firing during the T wave or from inhibiting serious
arrhythmias. Magnets can also be used to turn off some automatic implantable cardioverter
defibrillators (AICDs; see Question 49).
41. How do I assess a patient with potential pacemaker malfunction?
n
Take a focused history on symptoms related to pacemaker malfunction, including
palpitations, weakness, fatigue, shortness of breath, hiccups, syncope, fever, or pain or
erythema at the generator site.
n
The physical examination should focus on vital signs, mental status, cardiovascular system,
and inspection of the generator site.
n
An ECG should be obtained to evaluate pacemaker function, and anteroposterior and lateral
chest radiographs should be obtained to check pacemaker lead placement and lead and
connector integrity.
n
Evaluate the ECG. Are there pacing spikes present?
If pacing spikes are not present, apply a circular magnet over the pacemaker site. If the
application of the magnet does not result in pacing spikes being produced, there is some
mechanical failure present.
If pacing spikes are present, look for capture (a P wave in response to an atrial spike or a
QRS complex in response to a ventricle spike, or both, depending on the type of pacemaker).
If there is failure to capture, it usually indicates mechanical failure such as lead fracture or
dislodgement, but ischemia, metabolic derangements, and certain drugs have also been
implicated. If pacing is occurring at an inappropriately short interval between atrial or
ventricular contractions, it may be because the pacer is oversensing. If a pacer spike is seen
immediately following a native QRS complex, it may be because the pacer is undersensing.
See Table 30-3 for a description of common pacemaker malfunctions.
42. What is pacemaker syndrome?
A clinical spectrum of lightheadedness, fatigue, palpitations, syncope, dyspnea on exertion,
and hypotension that usually is attributed to asynchronous AV contraction and loss of atrial
functional support.
Chapter 30 CARDIAC DYSRHYTHMIAS, PACEMAKERS, AND IMPLANTABLE DEFIBRILLATORS216
43. What is twiddler’s syndrome?
The most common cause of late lead dislodgement. It occurs when the patient twists or
twiddles the pulse generator in its pouch to the point of twisting leads around the generator
box, shortening and dislodging them from their proper position. The pulse generator may
erode through the skin.
44. What is pacemaker-mediated tachycardia?
A normally functioning pacemaker may initiate a tachyarrhythmia. Retrograde conduction of a
ventricular beat may cause the atrium to trigger a second ventricular contraction that falls
during the pacemaker’s refractory period. Because this contraction is not sensed by the
pacemaker, the pulse generator fires, initiating a reentrant tachycardia. Treatment consists of
lengthening the AV time by any of the following methods:
n
Programming an increase in the atrial refractory time
n
Administering adenosine or verapamil
n
Increasing atrial sensory threshold
n
Applying a magnet to stop atrial sensing by the pacemaker
45. What is a runaway pacemaker?
Malfunction of the pacemaker that is manifested by tachycardias secondary to rapid
ventricular pacing. The problem is recognized when rates are greater than the upper rate
limit settings of the pacemaker and may require drastic measures, such as cutting the
pacer leads.
46. What happens as pacemakers lose battery power?
Pacemakers usually show a decline in the rate of magnet-mediated pacing, usually to a
predetermined manufacturer’s rate. Pacer response varies with manufacturer; some models
may also change pacer mode (e.g., DDD to VVI).
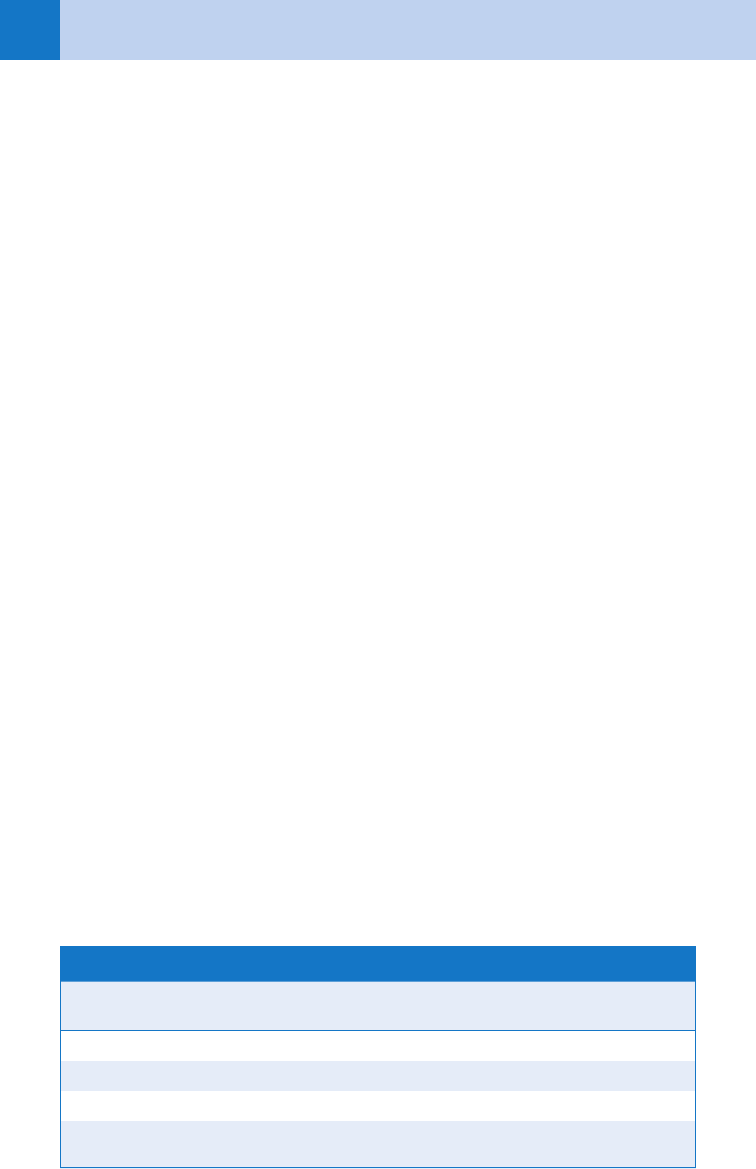
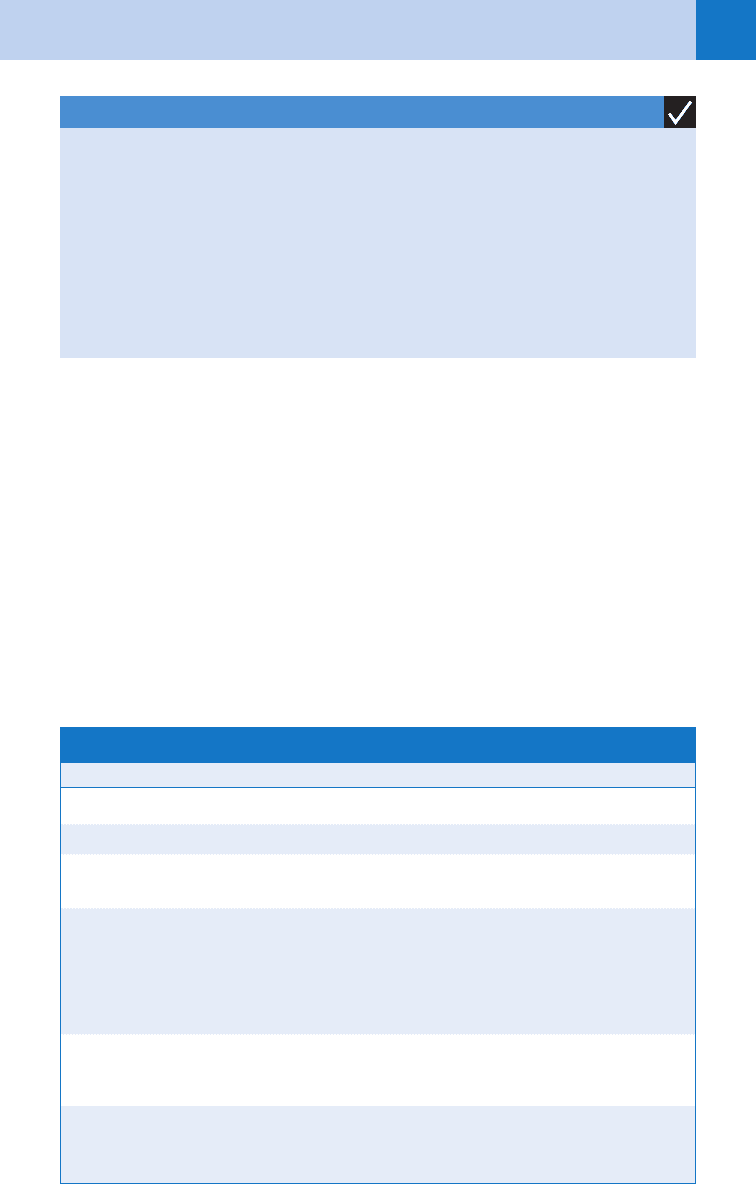
TABLE 30-3. MALFUNCTIONS OF PERMANENT PACEMAKERS
Complication Description
Oversensing Occurs when a pacer incorrectly senses electrical activity and
is inhibited from correctly pacing. This may be due to muscu-
lar activity, electromagnetic interference, or lead insulation
breakage.
Undersensing Occurs when a pacer incorrectly misses intrinsic depolarization
and paces despite intrinsic activity. This can be due to poor
lead positioning, lead dislodgement, magnet application, low
battery states, or myocardial infarction.
Operative failures This includes malfunction resulting from mechanical factors
(such as a pneumothorax, pericarditis, infection, hematoma,
lead dislodgement, or venous thrombosis).
Failure to capture Occurs when a pacing spike is not followed by either an atrial
or ventricular complex. This may be due to lead fracture, lead
dislodgement, a break in lead insulation, an elevated pacing
threshold, myocardial infarction at the lead tip, drugs, meta-
bolic abnormalities, cardiac perforation, poor lead connection,
and improper amplitude or pulse width settings.
Chapter 30 CARDIAC DYSRHYTHMIAS, PACEMAKERS, AND IMPLANTABLE DEFIBRILLATORS 217
47. Can a patient with a permanent pacemaker be defibrillated?
Yes, but it is important to place the pads or paddles away from the pulse generator, preferably
in the anteroposterior position. Defibrillation can damage the pulse generator. Temporary and
even permanent loss of ventricular or atrial capture may occur secondary to elevation of the
capture threshold of the pacer leads.
48. What is an AICD?
An automatic implantable cardioverter defibrillator (AICD) is a specialized device designed
to treat a cardiac tachyarrhythmia. If the device senses a ventricular rate that exceeds the
programmed cutoff rate of the implantable cardioverter defibrillator, the device performs
cardioversion/defibrillation. Alternatively, the device may attempt to pace rapidly for a number
of pulses, usually around 10, to attempt pace termination of the VT. Newer AICDs are a
combination of implantable cardioverter defibrillator and pacemaker in one unit.
49. Discuss malfunctions associated with an AICD.
See Table 30-4.
KEY POINTS: CARDIAC DYSRHYTHMIAS
1. An unstable patient with any tachydysrhythmia, regardless of the mechanism, requires
electrical cardioversion.
2. When trying to decide if the rhythm your patient is in is VT or SVT with aberrancy, assume
VT and treat accordingly.
3. The most common reason for early pacemaker malfunction is lead dislodgement.
4. Temporary transcutaneous or transvenous pacing should be used for hemodynamically
unstable bradycardias, as well as for overdrive pacing in an attempt to terminate VT.
5. Calcium channel blockers should not be used to treat wide-complex tachycardias.
TABLE 30-4. MALFUNCTIONS ASSOCIATED WITH AN AICD
Complication Description
Operative failure Similar to operative failures in pacemakers
Sensing failure Oversensing and undersensing occur, for similar reasons as with pacemakers
Inappropriate
cardioversion
May occur if a patient presents in atrial fibrillation or has received multiple
shocks in rapid succession
Ineffective
cardioversion
Can be seen because of T wave oversensing, lead fracture, lead insulation break-
age, electrocautery, MRI, or electromagnetic interference. Can also be caused by
inadequate energy output, a rise in the defibrillation threshold because of anti-
dysrhythmic medications, myocardial infarction at the lead site, lead fracture,
insulation breakage, or dislodgement of the leads of the cardioversion patches
Failure to deliver
cardioversion
Can be caused by failure to sense, lead fracture, electromagnetic interfer-
ence, and inadvertent AICD deactivation
Adapted from Higgins GL III: The automatic implantable cardioverter-defibrillator: Management issues relevant
to the emergency care provider. Am J Emerg Med 8:342–347, 1990.
AICD, automatic implantable cardioverter defibrillator; MRI, magnetic resonance imaging.
