Markovchick Vincent J., Pons Peter T., Bakes Katherine M.(ed.) Emergency medicine secrets. 5th ed
Подождите немного. Документ загружается.


Chapter 33 ESOPHAGUS AND STOMACH DISORDERS238
17. Discuss the emergency management of upper GI bleeding.
Management begins with a rapid assessment and management of the patient’s airway,
breathing, and cardiovascular status. Patients should be undressed, placed on cardiac and
SaO
2
monitors, and if SaO
2
,93% (at sea level), given supplemental oxygen. The history of GI
bleeding (i.e., vomiting blood or passing black or bloody stool) is sufficient to lead to the
placement of a large-bore, peripheral intravenous catheter with infusion of normal saline. A
focused physical examination should be done, checking for signs of shock (e.g., altered
mental status, tachycardia, hypotension, cool extremities, and delayed capillary fill). Patients
who have abnormal vital signs or signs of shock should have two or more intravenous lines
placed and be given rapid infusion of crystalloid. The evaluation should include testing of stool
for blood. During the initial examination and resuscitation, a history should be obtained. Blood
should be drawn for type and cross-matching, hematocrit, platelet count, prothrombin time,
electrolytes, BUN, and creatinine. Elderly patients, patients with a history of cardiovascular
disease or chest pain, and patients who are severely anemic should have an ECG to evaluate
for signs of cardiac ischemia (i.e., ST depression). An upright chest radiograph should be
obtained to rule out subdiaphragmatic air or pulmonary aspiration. A nasogastric or orogastric
tube should be placed to determine the presence of blood in the stomach and then removed.
18. What happens to patients with GI hemorrhage?
GI bleeding usually stops spontaneously, and no further ED management is necessary other
than admission and perhaps transfusion if there is significant anemia (i.e., hematocrit ,25%).
In 20% or less of patients, continued GI hemorrhage requires further management and
treatment.
19. How do I facilitate the placement of an NG tube?
Applying an anesthetic spray to the nose and posterior pharynx or having the patient breathe
nebulized 4% lidocaine decreases the discomfort of placing an NG tube.
20. How should a patient with continued GI hemorrhage be managed?
Blood replacement should begin in patients who continue to show signs of shock or
cardiovascular instability. Surgery and gastroenterology consultation should be initiated
quickly. Patients who do not respond promptly (i.e., remain hypotensive) to a 30 mL/kg
infusion of crystalloid should be given O-negative blood if type-specific blood is not yet
available. Cross-matched blood usually takes approximately 45 to 60 minutes to become
available. Upper GI bleeding can often be stopped endoscopically, but emergency operative
repair may be required in patients with persistent GI bleeding.
21. Is placement of a nasogastric or orogastric tube contraindicated in someone
with esophageal varices?
There is no evidence that a properly placed NG or orogastric tube results in a significantly
increased risk of tearing varices or increased size of a Mallory-Weiss tear. NG or orogastric
tubes can perforate the esophagus or posterior pharynx if they are placed too aggressively.
Diagnostic NG or orogastric tubes are unnecessary if the patient vomits gastric contents in the
ED because this may be inspected for the presence of blood.
22. When should gastric lavage be used in patients with upper GI bleeding?
Gastric lavage is necessary only in patients who have no aspirate after the NG tube is placed.
Regular tap water is used for lavage; the fluid need not be saline or sterile.
23. Should all patients with upper GI bleeding undergo endoscopy?
Endoscopy is the most accurate diagnostic tool available for the evaluation of patients with
upper GI bleeding. Endoscopy will identify a lesion in 78% to 95% of patients if it is done
within 12 to 24 hours of hemorrhage. Accurate identification of the bleeding site allows risk
stratification with respect to predicting rebleeding and mortality. Risk stratification facilitates a
proper disposition decision.
Chapter 33 ESOPHAGUS AND STOMACH DISORDERS 239
24. What are the low-risk criteria that allow a patient who is complaining of GI
bleeding to be sent home?
n
No comorbid diseases
n
Normal vital signs
n
Normal or trace positive stool guaiac
n
Negative gastric aspirate, if done
n
Normal or near-normal hemoglobin and hematocrit
n
Proper understanding of signs and symptoms of significant bleeding
n
Good home support
n
Follow-up arranged within 24 hours
n
Immediate access to emergent care, if needed
KEY POINTS: ESOPHAGUS AND STOMACH DISORDERS
1. Epigastric pain may be due to myocardial ischemia, so an ECG should be obtained in adult
patients with epigastric discomfort, visceral-type pain, or cardiac risk factors.
2. Antacids often provide symptomatic relief of abdominal discomfort related to gastroesopha-
geal disease.
3. H. pylori is a common, treatable cause of peptic ulcer disease.
4. Patients with upper GI bleeding who are hemodynamically unstable should receive rapid
intravenous crystalloid infusion, urgent surgery, and gastroenterology consultation.
BIBLIOGRAPHY
1. Berman DA, Porter RS, Graber M: The GI cocktail is no more effective than plain liquid antacid: a randomized,
double blind clinical trial. J Emerg Med 25(3):239–244, 2003.
2. Byers SE, Chudnofsky CR, Sorondo B, et al: Incidence of occult upper gastrointestinal bleeding in patients
presenting to the ED with hematochezia. Am J Emerg Med 25(3):340–344, 2007.
3. Cappell MS, Friedel D: Initial management of acute upper gastrointestinal bleeding: from initial evaluation up to
gastrointestinal endoscopy. Med Clin North Am 92(3):491–509, xi, 2008.
4. Henneman PL: Gastrointestinal bleeding. In Marx JA, Hockberger RS, Walls RM, editors: Rosen’s emergency
medicine concepts and clinical practice, ed 6, St. Louis, 2006, Mosby, pp 220–227.
5. Lowell MJ: Esophagus, stomach, and duodenum. In Marx JA, Hockberger RS, Walls RM, editors: Rosen’s
emergency medicine concepts and clinical practice, ed 6, St. Louis, 2006, Mosby, pp 1382–1401.
6. Witting MD, Magder L, Heins AE, et al: ED predictors of upper gastrointestinal tract bleeding in patients without
hematemesis. Am J Emerg Med 24(3):280–285, 2006.
240
BOWEL DISORDERS
CHAPTER 34
Vikhyat S. Bebarta, MD
1. When do you consider evaluating a patient for appendicitis?
Consider appendicitis in anyone presenting with abdominal pain. It can occur at any age,
but is most prevalent in the teens and twenties. With the high prevalence of appendicitis
in the population, atypical presentations are common. Appendicitis is one of the most
commonly missed diagnoses in the ED, and it is the most common nonobstetrical
emergency during pregnancy.
2. What is the pathogenesis of acute appendicitis?
The appendiceal lumen becomes obstructed, most commonly by a fecalith, leading to
bacterial overgrowth and dilation of the appendix. Early on, the distended lumen causes
dull, diffuse abdominal pain. As the inflammation progresses, a localized peritonitis
develops, producing the classic right lower quadrant (RLQ) pain with involuntary
guarding and rebound on physical examination.
3. How does appendicitis present clinically?
The classic presentation is nonspecific, umbilical abdominal pain that migrates over
several hours to the RLQ of the abdomen. Associated symptoms include nausea,
anorexia, and fever. However, variation of the appendix location leads to varied clinical
presentations. For example, a retrocecal appendix may cause back or flank pain that can
be mistakenly diagnosed as pyelonephritis or symptomatic nephrolithiasis. An extra long
appendix with an inflamed tip may produce left lower quadrant pain. In pregnancy, the
appendix is displaced into the right upper quadrant and, when inflamed, may be
mistaken for symptomatic gallbladder disease. Other diagnoses of RLQ pain should
also be considered (see Table 34-1).
4. Is the physical examination reliable in appendicitis?
Unfortunately, the classic physical examination findings of appendicitis—RLQ guarding
and rebound, and positive psoas, obturator, or Rovsing’s signs—are neither specific nor
sensitive enough to accurately diagnose appendicitis. Standard laboratory test results
may raise or lower your clinical suspicion, but only an abdominal computed tomography
(CT) scan or direct visualization with surgery can reliably diagnose an inflamed
appendix. Frequently, nonspecific RLQ pain and tenderness are the only clinical findings
of appendicitis. Parenteral analgesia, such as morphine, may improve the physical
examination for appendicitis.
5. What laboratory tests are helpful in evaluating RLQ pain?
Although no laboratory test is diagnostic of appendicitis, tests can aid in the evaluation
of the patient and exclude other diagnoses:
n
White blood cell count: .10,000 per mm
3
in approximately 90% of cases
n
Urinalysis: To exclude urinary tract infection (However, mild pyuria or hematuria may
be present when an inflamed appendix lies near the bladder or ureter.)
n
b-human chorionic gonadotropin: To help exclude ectopic pregnancy
Chapter 34 BOWEL DISORDERS 241
6. What radiologic study is best at imaging the appendix?
Abdominal CT is the imaging modality of choice for appendicitis. The scan is routinely done
with intravenous and oral or rectal contrast enhancement. It has a reported accuracy of 93%
to 98% in ruling in or out the diagnosis of appendicitis and is more sensitive and specific than
any combination of physical examination and laboratory findings. Additionally, the CT scan
may show other diseases responsible for the patient’s symptoms.
Unenhanced CT (CT without contrast) has a sensitivity of 88% to 96% but is dependent on
body habitus. Additional intraperitoneal fat improves sensitivity. However, CT scan has the risk
of radiation and iodinated contrast. Ultrasound may be useful in children, pregnancy, and thin
patients. It has a sensitivity of 88% to 94%, but the sensitivity is variable and is dependent on
the patient’s body habitus and the sonographer’s and radiologist’s experience. Ultrasound is
useful to confirm a suspicion of appendicitis, but it is not useful to exclude it.
7. What is the treatment for appendicitis?
Appendectomy is the definitive treatment. Once appendicitis has been diagnosed, or is highly
suspected, a surgical consult should be obtained. In a suspected case, start fluid
resuscitation, pain control, and broad-spectrum antibiotics while waiting for surgery. A delay
in diagnosis and treatment increases the perforation risk.
8. What is mesenteric ischemia?
Mesenteric ischemia is caused by insufficient blood supply to the intestines leading to tissue
ischemia and infarction. The common causes are arterial emboli (most common) or
thrombus, venous thrombosis, or nonocclusive hypoperfusion states. Patients should be
assessed for risk factors of mesenteric ischemia (see Table 34-2).
Acute ileitis Inflammatory bowel disease
Diverticulitis Acute cholecystitis
Perforated gastric or duodenal ulcer Volvulus
Intussusception Small bowel obstruction
Inflammation of Meckel’s diverticulum Uterine or tubo-ovarian pathology
(e.g., tubo-ovarian abscess, ovarian torsion,
ovarian cysts)
Incarcerated inguinal hernia Ectopic pregnancy
Testicular torsion or epididymitis Mittelschmerz
Mesenteric adenitis Pyelonephritis, symptomatic nephrolithiasis
TABLE 34–1. DIFFERENTIAL DIAGNOSIS FOR RIGHT LOWER QUADRANT ABDOMINAL PAIN
Age greater than 50 years Recent myocardial infarction
Valvular or atherosclerotic heart disease Dysrhythmias (e.g., atrial fibrillation)
Peripheral vascular disease Critical illness with hypotension or sepsis
Congestive heart failure Diuretics or vasoconstrictive drugs
TABLE 34–2. RISK FACTORS FOR MESENTERIC ISCHEMIA

Chapter 34 BOWEL DISORDERS242
9. How do patients with mesenteric ischemia present?
Patients complain of a diffusely painful abdomen. In the early stage, patients complain of
severe pain but have minimal physical findings—the characteristic pain out of proportion
to the examination. As infarction of bowel develops, peritoneal signs occur. Vomiting,
hematochezia, hematemesis, abdominal distention, fever, and shock are late signs that
often indicate infarcted bowel.
10. How do I diagnose mesenteric ischemia?
Diagnosing mesenteric ischemia can be difficult. The combination of clinical suspicion,
radiographic imaging, and laboratory findings can help lead to the correct diagnosis. Direct
surgical visualization of the bowel remains the gold standard. The abdominal CT with
intravenous and oral contrast can show the location of the vascular occlusion and secondary
findings consistent with ischemia, such as air within the bowel wall, intestinal wall thickening,
and local inflammation. Laboratory findings may include leukocytosis; hemoconcentration;
metabolic acidosis; and elevated phosphate, lactate, or lactate dehydrogenase. These lab
findings may indicate ischemic bowel but lack sensitivity and specificity.
11. How is mesenteric ischemia treated?
Initial treatment includes vigorous resuscitation, parenteral antibiotics, correction of
predisposing factors, and early surgical consultation. Definitive management involves selective
vasodilator infusion, anticoagulation in venous occlusion, or embolectomy. Laparotomy is
necessary for resection of necrotic bowel.
12. What is intussusception?
Intussusception occurs when an intestinal segment invaginates and telescopes into an
adjacent segment. This is a disease predominately seen in children (see Chapter 63), but it
can occur in adults. Typical pathologic lesions include tumors, Meckel’s diverticulum, and
inflammatory lesions. The high frequency of mass lesions in adults mandates surgical
exploration.
13. What is IBD?
Inflammatory bowel disease (IBD) is an idiopathic, chronic inflammatory disease of the
intestine. It encompasses two main groups:
n
Crohn’s disease (CD). CD is also known as regional enteritis or granulomatous ileocolitis.
n
Ulcerative colitis (UC).
CD and UC are rising in incidence. Common clinical features are summarized in
Table 34-3.
14. How do CD and UC present?
Although they are pathologically distinct diseases, CD and UC can present in a similar fashion
and affect all age groups (see Table 34-3). Both diseases may present with diarrhea,
abdominal pain, fever, anorexia, weight loss, and bloody diarrhea; however, UC is more likely
to present with bloody diarrhea. In nonfulminating colitis, the diagnosis can be confirmed by
endoscopy or barium enema.
15. What is the ED management for IBD?
Patients with mild disease and no signs of life-threatening complications can be treated as
outpatients with close follow-up. Treatment usually consists of sulfasalazine, steroids (oral
or rectal), steroid-sparing agents such as 6-mercaptopurine, antidiarrheal agents (e.g.,
loperamide, Lomotil, and cholestyramine), and analgesia. Antidiarrheal agents should be used
with caution because they can predispose to toxic megacolon. Metronidazole may help treat
the chronic perirectal complications of CD. Patients should be admitted if they have severe
disease or any life-threatening complications. Extraintestinal manifestations of IBD can also
occur (see Table 34-4).
Chapter 34 BOWEL DISORDERS 243
Adapted from Podolsky DK: Inflammatory bowel disease. N Engl J Med 347:417–429, 2002.
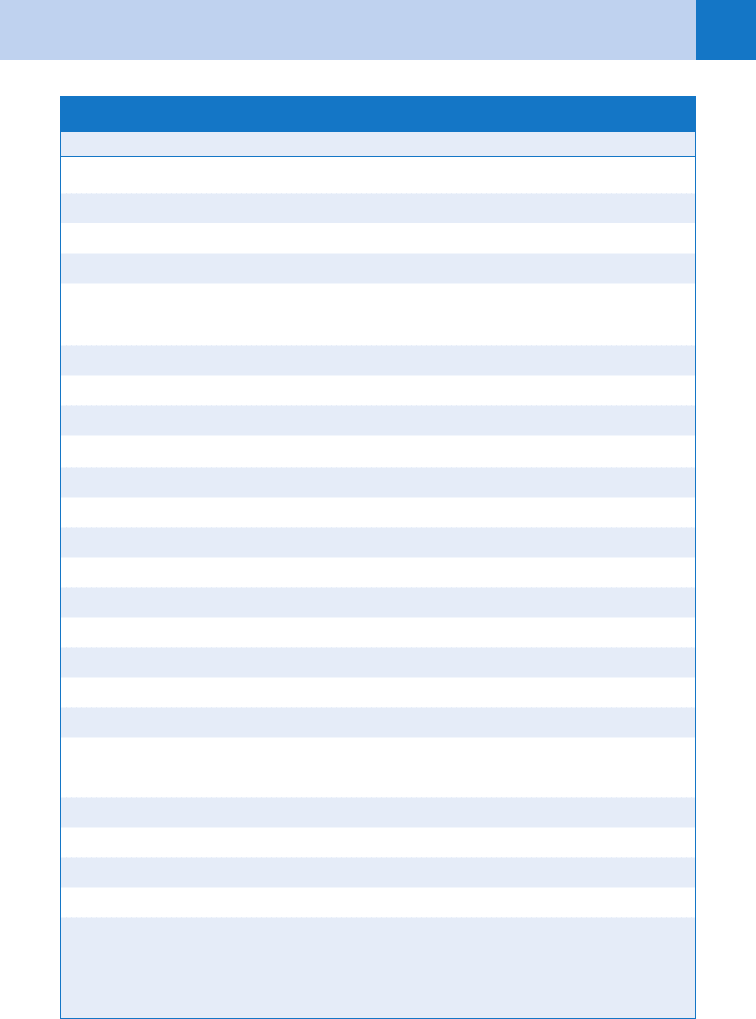
TABLE 34–3. COMMON FEATURES FOR INFLAMMATORY BOWEL DISEASE
Clinical Feature Crohn’s Disease Ulcerative Colitis
Weight loss Common Fairly common
Fever Common Fairly common
Diarrhea Fairly common Very common
Rectal bleeding Fairly common Very common
Perianal disease Common None
Site
Colon
2
⁄3 of patients Exclusively
Ileum
2
⁄3 of patients None
Jejunum, stomach, or esophagus Uncommon None
Intestinal complications
Stricture Common Unknown
Fistulas Fairly common None
Toxic megacolon None Unknown
Perforation Uncommon Unknown
Cancer Fairly common Common
Endoscopic findings
Friability Fairly common Very common
Aphthous and linear ulcers Common None
Cobblestone appearance Common None
Rectal involvement Fairly common Very common
Radiologic findings
Distribution Discontinuous, segmental Continuous
Ulceration Deep Superficial
Fissures Common None
Strictures for fistulas Common Rare
Ileal involvement Narrowed, nodular Dilated
16. Describe what happens during intestinal obstruction.
When the large and small bowels become obstructed, loss of the normal forward flow of
digested food and secretions occurs. Proximal to the obstruction, a buildup of bowel gas,
gastric secretions, and food develops. The bowel then becomes distended, causing pain,
vomiting, and decreased oral intake. The cause of the obstruction can be mechanical or
Chapter 34 BOWEL DISORDERS244
adynamic. Mechanical obstruction from adhesions or tumors frequently requires surgical
intervention, whereas an adynamic ileus usually resolves spontaneously within a few days.
17. What are the common causes of mechanical small bowel obstruction (SBO)?
Overall, adhesions, hernias, and cancer account for more than 90% of mechanical SBO cases.
Postoperative adhesions are the most common cause of an SBO (56%), followed by
incarcerated hernia (25%) and cancer (10%). Other less common causes include IBD,
gallstones, volvulus, intussusception, radiation enteritis, abscesses, congenital lesions, and
bezoars.
18. What are the clinical features of SBO?
Patients present with diffuse abdominal pain, distention, and occasionally, vomiting.
Early on, the pain is mild, crampy, and colicky in nature. An early SBO can be difficult to
diagnose. The patient has pain but continues to have flatus and passage of some stool. As
the obstruction progresses, the intestinal contents build up proximally, leading to nausea
and vomiting. The intestine distal to the obstruction empties of stool and has decreased
peristaltic motion leading to obstipation (inability to pass feces or flatus). Auscultation may
reveal high-pitched, hyperactive tinkling or rushing sounds. Rectal examination may reveal
impacted stool.
19. Describe the radiographic findings in SBO.
The classic finding on abdominal plain films is multiple air-fluid levels and distended loops of
small bowel. When the obstructed intestine contains more fluid than gas, small round pockets
of air may line up to form the string of pearls sign. A paucity of stool and gas is noted distal
to the obstruction. Plain films have a sensitivity of 41% to 86% and a specificity of 25% to
88%; therefore, an early SBO may be missed by using only radiographs. Abdominal CT scan
has a higher sensitivity (100%) and specificity (83%). Additionally, CT scan can show the
location of the obstruction and help identify the cause (e.g., mass or infection such as
appendicitis or diverticulitis).
20. What is the treatment for SBO?
The initial emergency management includes cardiopulmonary support, electrolyte
replacement, decompression with a nasogastric tube, and intravenous fluids. Patients lose a
large amount of fluid into the obstructed bowel and can be significantly intravascularly
depleted. SBOs can often be managed nonoperatively with observation, intravenous fluid
resuscitation, and bowel rest. However, some complete or mechanical obstructions require
surgery. A surgical consultation is indicated while the patient is in the ED.
Clinical Category Disorder
Ocular Uveitis, episcleritis
Dermatologic Erythema nodosum, pyoderma gangrenosum
Musculoskeletal Ankylosing spondylitis, peripheral arthritis, sacroiliitis
Hepatobiliary Cholelithiasis, pericholangitis, hepatitis, fatty liver, primary
sclerosing cholangitis, cholangiocarcinoma, pancreatitis
Hematologic Thromboembolic disease, chronic anemia
Renal Nephrolithiasis, amyloidosis leading to renal failure
TABLE 34–4. COMMON EXTRAINTESTINAL MANIFESTATIONS OF INFLAMMATORY BOWEL DISEASE
Chapter 34 BOWEL DISORDERS 245
21. What are the characteristics of an ileus?
The terms ileus and adynamic ileus are synonymous for a paralyzed intestine. The bowel is
unable to perform peristalsis. This is the most common cause of SBO. Causes of an ileus
include infection (e.g., peritonitis), drugs (e.g., narcotics, anticholinergics), electrolyte
imbalance (e.g., hypokalemia), spinal cord injuries, and recent bowel surgery. Patients present
with abdominal distention, nausea and vomiting, and obstipation. Abdominal examination
reveals hypoactive bowel sounds, mild tenderness, and absence of peritoneal signs.
Radiographs usually show minimally distended bowel throughout the entire gastrointestinal
(GI) tract, with diffuse air-fluid levels in the small bowel.
22. How is an ileus treated?
Management is similar to SBO. Limit oral intake, resuscitate with intravenous fluids, and
correct electrolyte abnormalities, particularly hypokalemia. If abdominal distention is present,
place a nasogastric or orogastric tube to decompress the stomach. Identify and limit the
administration of medications, such as opioids, that slow intestinal motility. If the ileus is
prolonged (.3–5 days), obtain additional imaging to search for an underlying cause.
23. What are the causes of large bowel obstruction (LBO)?
LBO is caused most commonly by colon cancer (60%), volvulus (20%), and diverticular
disease (10%). Primary adenocarcinoma accounts for most cancerous lesions. Other less
likely causes include metastatic carcinoma, gynecologic tumors, IBD, intussusception, and
fecal impaction. In infants, consider congenital disorders, such as Hirschsprung’s disease or
an imperforate anus. Hernias and adhesions are uncommon causes of LBO.
24. What are diverticula and what are common complications?
Diverticula are sac-like outpouchings of the colon that occur through weakened areas of the
muscularis of the colon wall. They commonly occur in persons of industrialized nations and
increase in frequency with age. It is estimated that one third of the U.S. population will
develop diverticula by age 50, and two thirds by 85 years. Complications from diverticula
include bleeding and diverticulitis, a localized infection. Diverticulitis is caused by obstruction
of the opening of diverticula, usually by stool, leading to infection from the proliferation of
colonic bacteria and build-up of bowel secretions within the diverticula.
25. How does diverticulitis clinically present?
The most common symptom of diverticulitis is abdominal pain. The pain usually evolves over
1 to 2 days from dull, diffuse abdominal pain to more intense, localized left lower quadrant
pain. Patients may complain of fever, nausea, vomiting, and decreased appetite. Diverticulitis
occurs most frequently in the descending and sigmoid regions of the colon but can occur
throughout the colon. The abdominal CT scan is the diagnostic procedure of choice and can
show evidence for abscesses, bowel perforation, and severity of disease.
26. How do you manage diverticulitis?
Management consists of intravenous fluids, electrolyte replacement, parenteral analgesics,
bowel rest, and broad-spectrum antibiotics. Patients with mild symptoms who are able to eat
and have close follow-up can be managed as outpatients with oral antibiotics and close
follow-up. Patients who have systemic or severe symptoms, older age, comorbidities,
abscess, or bowel perforations require hospitalization, intravenous antibiotics, and serial
examinations. Surgery may be required for repeat episodes or for bowel perforation. Abscess
requires surgical or interventional radiology catheter drainage.
27. What are common causes of lower GI bleeding?
Patients frequently present to the ED with complaints of rectal bleeding. Lower GI bleeds
occur from many causes, and a thorough history and examination are vital to diagnose the
bleeding source. Investigating anatomically from the rectum proximally, evaluate for
Chapter 34 BOWEL DISORDERS246
hemorrhoids and rectal fissures, then, based on history and examination, consider
diverticulosis, polyps, cancer, arteriovenous (AV) malformation, IBD, ischemic colitis,
infectious diarrhea, and finally an upper GI source.
28. How do you perform anoscopy?
Anoscopy can provide a direct view of the anus and distal rectum. A lubricated anoscope with
the obturator in place is advanced gently through the anal orifice. The obturator is removed to
view the distal rectal mucosa; a light source is shined into the barrel of the anoscope, and the
anoscope is withdrawn slowly while searching for internal hemorrhoids, fissures, abscess,
masses, or bleeding proximal to the rectum.
29. What are hemorrhoids?
Hemorrhoids are engorged vascular cushions comprised of internal or external hemorrhoidal
veins and present most often with bleeding, pain, or rectal itching. They are associated with
prolonged increase in resting pressure in the anal canal, most often from constipation but also
seen in pregnancy, excessive straining, and in certain occupations (e.g., truck driver).
30. How do internal and external hemorrhoids differ?
n
Internal hemorrhoids arise above the dentate line, are covered by mucosa, and are not
usually palpable or painful. They are seen during anoscopy and typically present as bright
red blood in the toilet bowl or on toilet paper.
n
External hemorrhoids are covered by skin and are easily visible and palpable at the anal
orifice. A common complication of external hemorrhoids is thrombosis, which is painful
and requires excision of the thrombus.
31. How are hemorrhoids treated?
Treat mildly symptomatic hemorrhoids with irrigation during the shower or bath, stool
softeners, high-fiber diet, bulk laxatives (e.g., psyllium or methylcellulose), increased fluid
consumption, proper anal hygiene, and analgesics if necessary. Nonthrombosed prolapsed
hemorrhoids should be gently reduced. Thrombosed hemorrhoids should be excised. Patients
with intractable symptoms need surgical referral.
32. What is an anal fissure?
An anal fissure is a linear crack or ulcer in the epithelium in the distal anal canal. Anal fissures
are the most common cause of rectal pain. Most are idiopathic, but any anal canal trauma can
cause a fissure. Most benign anal fissures occur in the posterior midline, followed by the
anterior midline. Fissures in other locations are associated with CD, infection, malignancy,
or immunodeficiency.
33. How do I treat an anal fissure?
Most anal fissures can be managed conservatively with sitz baths, stool softeners, high-fiber
diet, bulk laxatives (e.g., psyllium or methylcellulose), additional fluid consumption, proper
anal hygiene, and analgesics. Recent studies have shown good success with the use of topical
0.2% nitroglycerin ointment applied twice daily for 6 weeks or a single botulinum injection.
Fissures that do not improve with conservative therapies should be referred to a surgeon for
consideration of a lateral internal sphincterotomy.
34. Can I drain anorectal abscesses in the ED?
Small isolated perianal abscesses can be drained successfully in the ED. These abscesses can
be painful, requiring both local anesthetic and oral or parenteral sedation. For complicated or
deep rectal abscesses, consult surgery for operative drainage.
Chapter 34 BOWEL DISORDERS 247
BIBLIOGRAPHY
1. Brisinda G, Maria G, Bentivoglio AR, et al: A comparison of injections of botulinum toxin and topical
nitroglycerin ointment for the treatment of chronic anal fissure. N Engl J Med 341:65–69, 1999.
2. Ferzoco LB, Raptopoulos V, Silen W: Current concepts: acute diverticulitis. N Engl J Med 338:1521–1526,
1998.
3. Podolsky DK: Inflammatory bowel disease. N Engl J Med 347:417–429, 2002.
4. Rao PM, Rhea JT, Novelline RA, et al: Effect of computed tomography of the appendix on treatment of patients
and use of hospital resources. N Engl J Med 338:141–146, 1998.
5. Rao PM, Rhea JT, Rattner DW, et al: Introduction of appendiceal CT: impact on negative appendectomy and
appendiceal perforation rates. Ann Surg 229:344–349, 1999.
6. Segatto E, Mortele KJ, Ji H, et al: Acute small bowel ischemia: CT imaging findings. Semin Ultrasound CT MR
24:364–376, 2003.
KEY POINTS: BOWEL DISORDERS
1. Appendicitis is common, and unusual presentations are frequent; therefore, always consider
appendicitis in a patient with abdominal pain.
2. A patient with atrial fibrillation and abdominal pain has mesenteric ischemia until proven
otherwise.
3. Surgical adhesions are the most frequent cause of SBO.
4. Patients with SBO should be aggressively resuscitated with intravenous fluids in the ED due
to the extensive depletion of intravascular fluid.
5. Although diverticulitis is most commonly seen in the older patient population, younger
patients (20–40 years) also develop it.
6. IBD can cause complicated rectal abscesses or fissures that require surgical consultation.
