Leroy C., Rancoita P.-G. Principles Of Radiation Interaction In Matter And Detection
Подождите немного. Документ загружается.

January 9, 2009 10:21 World Scientific Book - 9.75in x 6.5in ws-bo ok975x65˙n˙2nd˙Ed
750 Principles of Radiation Interaction in Matter and Detection
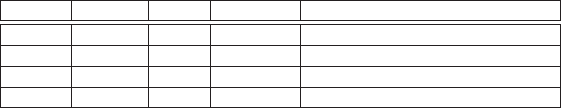
Table 10.3 Values of hS
p
i and hS
n
i for
19
F calculated from various mod-
els. The corresponding ratios R
p
≡ C
p(N)
SD
/C
p
SD
and R
n
≡ C
n(N)
SD
/C
n
SD
are also listed.
S
p
S
n
R
p
R
n
Reference
0.4751 -0.0087 0.903 0.0003 [Divari et al. (2000)]
0.368 -0.001 0.542 1 × 10
−6
[Leroy (2004b)], g
A
/g
V
= 1.25
0.415 -0.047 0.689 0.0088 [Leroy (2004b)], g
A
/g
V
= 1.00
0.441 -0.109 0.778 0.0475 [Pacheco and Strottman (1989)]
and, obviously, hL
p
i = 0.04, hL
n
i = 0. For instance,
73
Ge is an odd-neutron nucleus
with J = 9/2, a G
9/2
state, and with µ
exp
= −0.879. Therefore, Eq. (10.91) gives
the value:
hS
n
i = S
o
= [−0.879 − 0.0 × (9/2)] /(−3.826 − 0.0) = 0.23,
hS
p
i = 0
(10.93)
with hL
n
i = 4.27 and hL
p
i = 0
In the extreme single-particle model(ESPM), it is assumed that the entire spin
of the nucleus comes from the single last unpaired proton or neutron. Thus, one
finds for a nucleus with an unpaired proton
hS
p
i = S
o
= 1/2 {[J(J + 1) + 3/4 − l(l + 1)]/(J + 1)},
hS
n
i = 0
(10.94)
and, vice versa, for a nucleus with an unpaired neutron. It gives hS
p
i = 0.50,
hS
n
i = 0, and hL
p
i = hL
n
i = 0 for
19
F, and hS
n
i = 0.50, hS
p
i = 0, hL
p
i = 0 and
hL
n
i = 4.0 for
73
Ge.
Returning to Eqs. (10.86, 10.87), one considers the effects of meson currents in
the nucleus. It is believed that the dominant one-pion exchange mechanism does
not modify the isoscalar moment
µ
IS
= µ
p
+ µ
n
.
The mean effect of these currents is to introduce additional terms −µ
M
and +µ
M
into Eqs. (10.86, 10.87), respectively. Heavy-vector-meson exchange currents con-
tribute a term µ
x
in Eq. (10.86). Model calculations suggest a form:
µ
x
= −x (S
o
− S
e
), (10.95)
with a factor x to b e determined later. One can rewrite Eqs. (10.86, 10.87) as
µ
p
= g
p
J + (G
p
− g
p
− x) (S
o
− S
e
) − (g
p
− g
n
) J
e
− µ
M
+(G
p
− g
p
+ G
n
− g
n
) S
e
(10.96)
and
µ
n
= g
n
J + (G
n
− g
n
) (S
o
− S
e
) + (g
p
− g
n
) J
e
+µ
M
+ (G
p
− g
p
+ G
n
− g
n
) S
e
.
(10.97)
January 9, 2009 10:21 World Scientific Book - 9.75in x 6.5in ws-bo ok975x65˙n˙2nd˙Ed
Superheated Droplet (Bubble) Detectors and CDM Search 751
Then, the isoscalar moment is [summing Eqs. (10.96, 10.97)]:
µ
IS
= (g
p
+ g
n
) J + (G
p
− g
p
+ G
n
− g
n
− x) (S
o
− S
e
)
+2 (G
p
− g
p
+ G
n
− g
n
) S
e
(10.98)
or, using g
p
= 1, G
p
= 5.586, g
n
= 0 and G
n
= −3.826,
µ
IS
= J + (0.76 − x) (S
o
− S
e
) + 1.52S
e
(10.99)
or
µ
IS
J
= 1 + (0.76 − x)
µ
S
o
− S
e
J
¶
+ 1.52
S
e
J
. (10.100)
The difference (S
o
−S
e
) and µ
IS
are obtained from a global fit to magnetic moments
in each of the two nuclei and the ft-value for the Gamow-Teller β-decay from one
to the other:
R
2
(S
o
− S
e
)
2
=
µ
6170
ft
− 1
¶
J
J + 1
, (10.101)
where R = g
A
/g
V
is the ratio of the axial-vector to vector weak-interaction coupling
coefficients.
For
19
F, one obtains [Buck and Perez (1983)] from a fit to magnetic moment and
ft-value data: µ
p
/J = 5.2576, µ
n
/J = −3.7708 and, therefore, µ
IS
/J = 1.487. The
quantity R(S
o
− S
e
)/J = 0.9226 is also found. From the original fit, a quenched
value for R was found:
R = 1.00 ± 0.02.
If one uses this value, one obtains
S
o
− S
e
J
= 0.9226. (10.102)
The quantity x in Eq. (10.100) can be found from a table [Raman, Houser,
Walkiewicz and Towner (1978)]. For
19
F, the table gives µ
x
= −0.018. However, to
adapt the present normalization with that of the table, one needs to multiply the
values found in the table by a factor 2. So, one finds µ
x
= −0.036 for
19
F. The value
of x can be extracted using Eqs. (10.95, 10.102) to find:
x =
0.036
0.461
= 0.078. (10.103)
Combining Eqs. (10.100, 10.102, 10.103), one finds:
S
e
= −0.047,
S
o
= 0.415,
(10.104)
which are reported in [Engel and Vogel (1989)]. If one uses the unquenched value
R = 1.249 ± 0.006 ≈ 1.25
obtained in neutron decay experiments, one finds
S
o
− S
e
J
=
0.9226
1.25
= 0.738
and x = 0.036/0.369 = 0.098 and therefore, S
e
= −0.001 and S
o
= 0.368.
January 9, 2009 10:21 World Scientific Book - 9.75in x 6.5in ws-bo ok975x65˙n˙2nd˙Ed
752 Principles of Radiation Interaction in Matter and Detection
−20 −15 −10 −5 0 5 10 15 20
−10
−8
−6
−4
−2
0
2
4
6
8
10
a
n
a
p
Tokyo/NaF
SIMPLE
CRESST
NAIAD
DAMA/Xe−2
PICASSO 1pb
Pacheco−Strottman
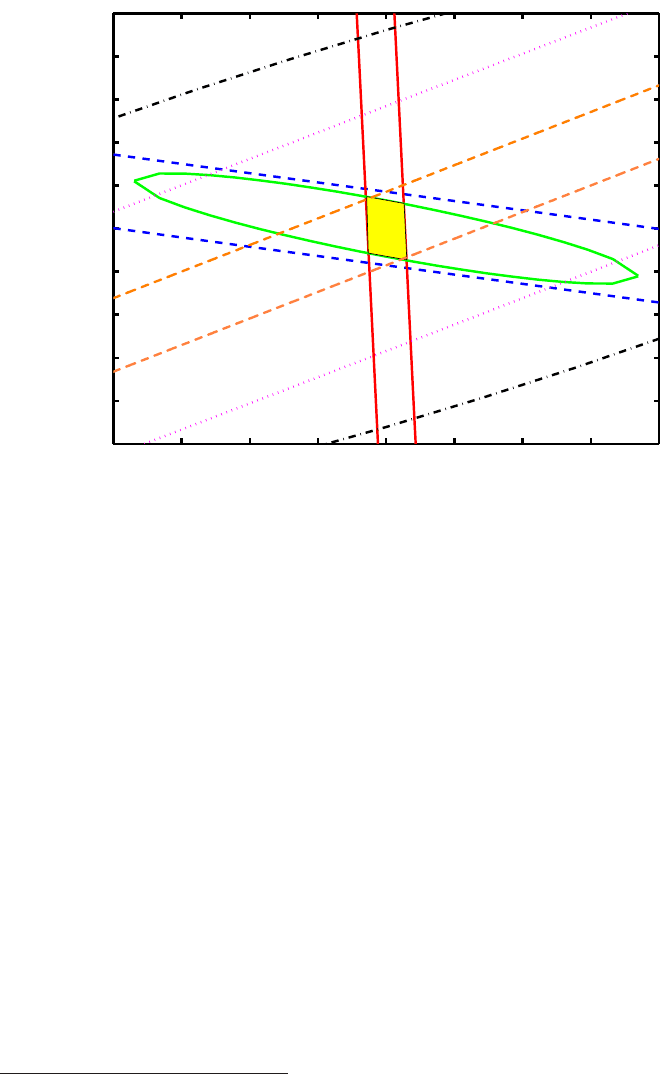
Fig. 10.14 Exclusion plot a
p
versus a
n
for σ
χp
= 1 pb and m
χ
= 50 GeV c
−2
[Genest and
Leroy (2004)], [Leroy (2004b)] using hS
p
i, hS
n
i calculated from model [Pacheco and Strottman
(1989)]. The PICASSO result [Barnab´e-Heider et al. (2005b)] is compared to the results of several
experiments: CRESST [Seide et al. (2002)], DAMA-Xe-2 [Bernabei et al. (1998)], SIMPLE [Girard
R et al. (2005)], Tokyo/NaF [Takeda et al. (2003)]. Other updated and new experimental results
can be found in [Genest (2007)].
10.2.1.4 Shell Models Calculation and Validation of hS
p
i and hS
n
i
The nuclear angular moment and the nuclear magnetic moment can be calculated
from the value of hS
p
i and hS
n
i, as calculated from shell models, and comparison
with the experimental nuclear magnetic moment can be done (Table 10.2) as one
test of the shell model. Using again notations familiar to shell models, the angular
momentum is:
J = hL
p
i + hS
p
i + hL
n
i + hS
n
i (10.105)
and the magnetic moment is given by
µ = g
p
hL
p
i + G
p
hS
p
i + g
n
hL
n
i + G
n
hS
n
i. (10.106)
The calculated magnetic moment of
73
Ge with free particle g-spin factors show
significant improvement in agreement with measured values if quenched g-spin fac-
tors are used (consistent with isovector quenching found in the sd [Brown and
Wildenthal (1987)] and fp [Richter et al. (1991)] shells
‡‡
when fitting to magnetic
moment data). Using quenched isovector component of the spin, one finds effective
‡‡
The reader can find an introduction to nuclear shells in Sect.3.1.5.
January 9, 2009 10:21 World Scientific Book - 9.75in x 6.5in ws-bo ok975x65˙n˙2nd˙Ed
Superheated Droplet (Bubble) Detectors and CDM Search 753
g-spin factors: G
p
= 4.80 and G
n
= −3.04. Then, the calculated magnetic moments
of
73
Ge are µ = −1.084 and -0.879 for [Ressell et al. (1993)]-“small” and [Ressell
et al. (1993)]-“large”, respectively.
10.2.2 The PICASSO Experiment, an Example
As said previously the PICASSO Experiment [Barnab´e-Heider et al. (2005a)] is
measuring the neutralino–
19
F cross section. This cross section is largely dominated
by the spin-dependent contribution. The neutralino induced recoil (R) spectrum of
19
F is given by [Lewin and Smith (1996)]:
dR
E
R
≈ c
1
R
0,P
E
R
[F
SD
(E
R
)]
2
exp
µ
−c
2
E
R
hE
R
i
¶
, (10.107)
where F
SD
(E
R
) is the form factor for spin-dependent intereactions: F
SD
(E
R
) < 1,
it is due to the finite size of the nucleus and dependent mainly on nuclear radius
and recoil energy;
R
0,P
=
403
A
T
m
χ
[σ
SD
/(1 pb)]
£
ρ
χ
/(0.3 GeV cm
−3
)
¤£
hvχi/(230 km s
−1
)
¤
(10.108)
is the total rate of neutrino–nucleus interaction (assuming zero momentum transfer),
R
0,P
is expressed in counts per kg and per day; A
T
is the atomic mass number of
the target atoms (
19
F in the present case), ρ
χ
in GeV c
−2
the mass density of the
neutralino (the local neutralino mass density at the position of the solar system
is assumed to be 0.3 GeV cm
−3
), hvχi is the relative average neutralino velocity
(230 km s
−1
is the velocity dispersion of the dark matter halo);
E
R
= 2
m
A
m
2
χ
(m
A
+ m
χ
)
2
vχ
2
®
(10.109)
is the mean recoil energy with m
A
the nucler mass of the recoil nucleus, F
2
(E
R
) ∼ 1
for
19
F and small momentum transfer; c
1
= c
2
= 1 for v
E
= 0 (v
E
is the velocity of
the earth relative to the dark matter distribution) [Lewin and Smith (1996)]; and
c
1
= 0.75 and c
2
= 0.56 for v
E
= 244 km s
−1
) [Lewin and Smith (1996)]. Combining
the
19
F recoil spectra expected from neutralino interactions [Eq. (10.107)] and the
measured detector threshold for
19
F recoil energy at a given operating temperature
(T ), one can determine the neutralino detection efficiency, ²(m
χ
, T )) as a function
of the neutralino mass and operating temperature. Then, the observable neutralino
count rate, R
obs
, as a function of temperature, neutralino mass and cross section is
given by:
R
obs
(m
χ
, σ
SD
, T ) =
c
1
c
2
R
0,P
(m
χ
, σ
SD
) ²(m
χ
, T ))
= 1.34 R
0,P
(m
χ
, σ
SD
) ²(m
χ
, T )). (10.110)
The cross section, σ
SD
, is given by Eq. (10.62). A combined fit of alpha background
and neutralino response to the PICASSO data brought an upper limit of 1.31 pb on
σ
χp
, 21.5 pb on σ
χn
for a mass m
χ
= 29 GeV c
−2
[Barnab´e-Heider et al. (2005b)].
January 9, 2009 10:21 World Scientific Book - 9.75in x 6.5in ws-bo ok975x65˙n˙2nd˙Ed
754 Principles of Radiation Interaction in Matter and Detection
One can also calculate the a
p
/a
n
limits. If one considers the example of a cross
section σ
χp
= σ
p
SDlim
= 1 pb for m
χ
= 50 GeV c
−2
, one finds:
π
24G
F
2
µ
χp
2
= 2.92 pb
−1
. (10.111)
σ
p
SDlim
being fixed, from the ratio of Eqs. (10.65, 10.66) assuming the same mass
for proton and neutron, one finds
σ
SDlim
p
σ
SDlim
n
=
C
p(N)
SD
/C
p
SD
C
n(N)
SD
/C
p
SD
(10.112)
with
C
p(N)
SD
C
p
SD
=
(8/π)a
p
2
hS
p
i
2
[(J + 1)/J]
(6/π)a
p
2
=
4
3
µ
J + 1
J
¶
hS
p
i
2
= 0.778 (10.113)
and
C
n(N)
SD
C
p
SD
=
(8/π)a
n
2
hS
n
i
2
[(J + 1)/J]
(6/π)a
n
2
=
4
3
µ
J + 1
J
¶
hS
n
i
2
= 0.0475. (10.114)
One has used the values
hS
p
i = 0.441,
hS
n
i = −0.109,
(10.115)
given in [Pacheco and Strottman (1989)] (Table 10.3).
One can determine the neutralino mass independent ratio:
σ
SDlim
p
σ
SDlim
n
=
1/0.778
1/4.75 × 10
−2
= 0.061. (10.116)
Therefore, fixing σ
χp
= σ
p
SDlim
= 1 pb and choosing m
χ
= 50 GeV c
−2
, one obtains
from Eq. (10.116), the value σ
χn
= σ
n
SDlim
= 16.37 pb. Then, the value σ
χp
=
σ
p(N)
SDlim
= 1 pb corresponds to σ
SDlim
χF
= 158.78 pb.
Equation (10.80) for m
χ
= 50 GeV c
−2
reads
2.92
pb
≥
µ
a
p
√
1.0 pb
±
a
n
√
16.37 pb
¶
2
, (10.117)
giving the two exclusion boundary limits [Genest and Leroy (2004)], [Leroy (2004b)]:
a
p
= 1.708 + 0.247a
n
(10.118)
and
a
p
= −1.708 + 0.247a
n
. (10.119)
The lines corresponding to Eqs. (10.118,10.119) represents the PICASSO expe-
riment exclusion limits (Fig. 10.14) for a neutralino of 50 GeV c
−2
mass and
σ
χp
= 1 pb.
January 9, 2009 10:21 World Scientific Book - 9.75in x 6.5in ws-bo ok975x65˙n˙2nd˙Ed
Chapter 11
Medical Physics Applications
The knowledge about the physics governing the interactions of particles with mat-
ter and particle detection finds applications in the field of nuclear medicine imaging
technique. This technique uses the injection into the patient of radionuclides directly
emitting photons, or of radiopharmaceuticals, labeled with a positron emitting iso-
tope. Photons directly produced by radionuclides or produced by the annihilation
of positrons emitted by the radiopharmaceutical with bo dy electrons are detected
by radiation detectors. This allows one to reconstruct three dimensional images
representing the distribution of radioactivity inside the patient’s body and to mea-
sure metabolic, biochemical and functional activities in tissue. Magnetic Resonance
Imaging (MRI) is another imaging technique, which does not require the use of
any radioactive material and uses instead the non-zero nuclear spin, an intrinsic
property found in nuclei (see page 226). MRI uses magnetic fields
∗
varying from 0.2
to 2 T and radio-frequency (RF) waves to observe the magnetization change of the
non-zero spin nuclei. The hydrogen isotope
1
H, which has a nuclear spin of
1
2
, is a
major component of the human body and is used as the main source of information.
Two techniques exploit the interaction of the produced photons with the ac-
tive material of radiation detectors (imager or scanner): Single Photon Emission
Computed Tomography (SPECT) and Positron Emission Tomography (PET). We
have seen, in Sect. 2.3, that photons interact with matter in several ways. These
are Compton scattering, photoelectric effect, and pair production. The two other
possible interactions are discarded for medical applications: Rayleigh or coherent
scattering (see Sect. 2.3.2.2) and photonuclear absorption (see Sect. 2.3.4). Rayleigh
scattering is a process predominant in the forward direction, i.e., in which photons
scatter from atomic electrons without exciting or ionizing the atom and, therefore,
no energy is absorbed in that process. Also, the incoming photon beam (usually
from a source) is hardly altered by this process. The Rayleigh cross section, σ
coh
(see Sect. 2.3.2.2), may be large for low photon energies (around 1 keV or less) and
rapidly decreases with the photon energy. However, for practical energies faced in
medical applications, σ
coh
is much smaller than the Compton (incoherent) cross
∗
1 T = 10
4
G. The Earth magnetic field is ≈ 0.5 G.
755

January 9, 2009 10:21 World Scientific Book - 9.75in x 6.5in ws-bo ok975x65˙n˙2nd˙Ed
756 Principles of Radiation Interaction in Matter and Detection
section. In particular, at energies where coherent and Compton cross sections com-
pete (the coherent cross section could even dominates the Compton cross section),
they are both largely dominated by the photoelectric cross section.
The photonuclear absorption is a nuclear interaction, in which the photon is
absorbed by the nucleus. It becomes relevant for photons with energy b eyond a few
MeV’s, although smaller than the pair production cross section, but these energies
are not encountered in medical applications. The energies encountered in medical
physics range from a few keV up to a few MeV.
The photoelectric effect is dominant for high-Z materials, while Compton scat-
tering dominates for low-Z materials at the photon energies used in medical physics
(see Fig. 2.75 and consider water as the material closest to tissue). The pair pro-
duction process does not contribute, since the photon energy of the sources used
in SPECT and the photon energy in PET (0.511 MeV) are lower than the thresh-
old energy (2 mc
2
= 1.022 MeV, where m is the electron rest-mass) for creating an
electron–positron pair.
The detection probability of a photon emitted by a source and experiencing
Compton scattering in the body depends on the amount of energy lost as a result of
that scattering. The initial energy (E
0
) of a photon and its energy after Compton
scattering (E
A
) are related through
E
A
= E
0
Á·
1 +
E
0
(1 − cosθ)
mc
2
¸
, (11.1)
where θ is the angle between the initial and final direction (after Compton scatte-
ring) of the photon. Basically, the probability of Compton interaction has a weak
dependence on the atomic number and decreases with the photon energy. The pho-
ton does not disappear in the Compton interaction and is available for further
interaction (with a decreased energy) in another detector, giving directional infor-
mation. This will be exploited in Compton camera, as we will see below.
The photoelectric effect (Sect. 2.3.1) is an interaction of a photon with a tight-
bound atomic electron: K-electron, L-electron, M-electron, . . .. The photon of
energy, hν, is completely absorbed and a photoelectron is ejected with a kinetic
energy K
e
given by
K
e
= hν − B
e
, (11.2)
where B
e
is the binding energy of the electron. The photoelectric effect is inversely
related to the power of ≈ 3.5 of the photon energy and directly related to ≈ the
fifth power of the atomic number. The photoelectric effect cross section also depends
on the electron shell. The photoelectric cross section as a function of the photon
energy presents several discontinuities at low energy. These discontinuities are called
absorption edges and correspond to energies below which it is impossible to eject
certain electrons from the atom. Below the K-edge, the photon cannot eject a K-
electron but still can eject a L-electron or a M-electron (Sect. 2.3.1). For instance, the
vacancy left in the K-shell after interaction is immediately filled by the transition
January 9, 2009 10:21 World Scientific Book - 9.75in x 6.5in ws-bo ok975x65˙n˙2nd˙Ed
Medical Physics Applications 757
of one electron of an outer shell accompanied by the emission of X-rays or an
Auger electron. Therefore, contrary to the Compton scattering, the photon is totally
absorbed in the radiation detector and there is no directional information provided
by the gamma or X-rays in the photoelectric process.
11.1 Single Photon Emission Computed Tomography (SPECT)
Single Photon Emission Computed Tomography (SPECT) has become a routine
technique in medical applications [Brooks and DiChiro (1976)]. This gamma-ray
imaging technique proceeds through the injection into the patient of a radioac-
tive substance, which emits photons of well-defined energy. The distribution of ra-
dionuclides, position and concentration inside patient’s body is externally monitored
through the emitted radiation deposited in a photon detector array rotating around
the body. This rotation allows the acquisition of data from multiple angles. This
procedure allows the study of organs behaviors, bringing the possibility to reveal
signs of malfunctioning as early as possible.
Organ imaging requires a radiation of sufficient energy to penetrate the body tis-
sues. However, the radiation energy must remain low enough to allow its absorption
in the detecting device. Therefore, photons with an energy ranging between 50 keV
and several hundreds of keV can be used for imaging. Photons in this energy range
are produced by specific radionuclides. A widely-used radionuclide is
99m
Tc, an iso-
mer of technetium with a half-life of 6.02 hours, which decays emitting 140.5 keV
(89%) photons (see Fig. 11.1).
Other sources like
201
Tl,
178
Ta and
133
Xe, emitting lower energy photons, are
also used. For instance,
201
Tl emits 135 keV (2%) and 167 keV (8%) photons and
(69–83) keV mercury K X-rays (90%).
Photons, produced after injection of
99m
Tc in the patient’s body, will eventually
reach a detector where their energy deposition is measured. The organ structure and
its evolution are then visualized from the resulting photon absorption patterns. The
images are the projection of a three-dimensional distribution onto a two-dimensional
plane. This can be achieved by rotating the detector around the patient. Series of
two-dimensional projections are taken from different directions.
To create the two-dimensional projections, Anger cameras are often used. First,
the photon emitted from within the patient crosses a collimator. Then, it reaches a
scintillator. The point of scintillation corresponds exactly to the plane coordinates
of the point of emission. Once the initial photon has reached the scintillator, it
excites all the photomultipliers. Analyzing the intensity of the signal coming from
every photomultiplier allows the determination of the plane coordinates. Finally,
the intensity of every photomultiplier’s signal is added. If it equals the energy of
the photon emitted, the information will be kept and helps the formation of the
image. If the energy is inferior, it means that the photon was scattered. Therefore,
the wrong coordinates were found and the information is rejected.
January 9, 2009 10:21 World Scientific Book - 9.75in x 6.5in ws-bo ok975x65˙n˙2nd˙Ed
758 Principles of Radiation Interaction in Matter and Detection
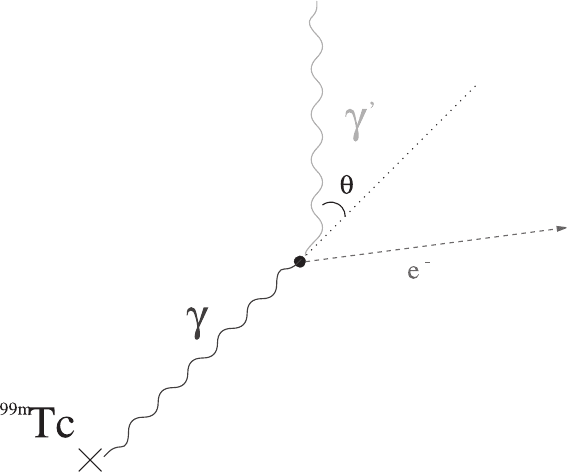
Fig. 11.1 Photons of 140.5 keV energy emitted by a
99m
Tc source of standard use in SPECT,
decaying to its isomer
99m
Tc, followed by a Compton scattering on a nucleus pro ducing a recoiling
electron. θ is the Compton scattering angle.
These cameras need to be operated with a collimator in front of the detecting
material. The collimator is usually made of a thick high-Z metal plate, drilled with
a huge number of small holes. The collimator holes allow only incident radiation
perp endicular to the detector surface and eliminate the obliquely-incident photons
i.e., the secondary photons produced by the interaction of the primary photons (from
the source) with biological matter (tissue, bones, etc. . .). These obliquely-incident
photons, by activating several detector readout cells, may prevent the image forma-
tion or, at best, degrade the image focusing. Their removal is necessary to obtain a
source image of high quality. Compton scattered photons (see Fig. 11.1) have a lower
energy than primary photons and can be rejected by energy discrimination. For a
given energy window, only Compton photons scattered at sufficiently small angle
can be detected [Eq. (11.1)]. If one assumes that the detector has perfect energy
resolution and that a rectangular energy window is applied, centered at E
0
with
a width ∆E (in keV), the maximum allowable scattering angle at the first order,
θ
max
, is given by:
θ
max
= cos
−1
n
1 − mc
2
∆E [E
0
(2E
0
− ∆E)]
−1
o
. (11.3)
As can be seen from Eq. (11.3), the probability to detect a 140.5 keV photon from
a
99m
Tc source in a 15% wide rectangular energy window is zero if the scattering
January 9, 2009 10:21 World Scientific Book - 9.75in x 6.5in ws-bo ok975x65˙n˙2nd˙Ed
Medical Physics Applications 759
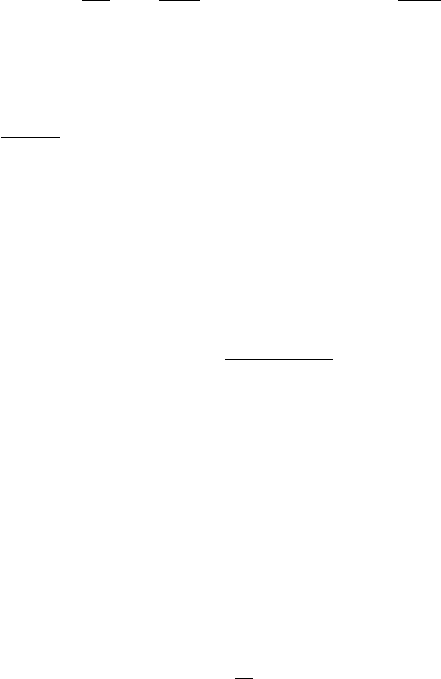
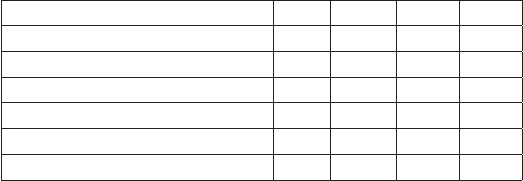
Table 11.1 Characteristics of semiconductor materials for use in medi-
cal imaging.
Characteristics Si GaAs CdTe HgI
2
Atomic number (Z) 14 31,33 48,52 80,53
Density (g/cm
3
) 2.33 5.32 5.80 6.30
Band gap (eV) 1.12 1.42 1.50 2.10
Energy per e-h pairs (eV) 3.62 4.20 4.43 4.15
Electron mobility (cm
2
V
−1
s
−1
) 1350 8500 1000 100
Hole mobility (cm
2
V
−1
s
−1
) 450 400 70 4
angle θ > 45.2
◦
. If the energy window is increased to 20%, the corresponding angle
becomes 53.5
◦
. For a single scattered photon to be detected at a position x of the
collimator, the photon must have been emitted and come out of the b ody along a
path confined to a cone with aperture θ ≤ θ
max
.
The necessity to use a collimator has the adverse consequence to decrease the
detection efficiency and this is a limitation to SPECT. The collimator reduces the
numb er of normal impinging photons to about 10
−4
of their original number, after
passing the collimator. As a consequence, a higher dose has to be given to the
patient in order to provide sufficient statistics for elaborating an accurate image.
Semiconductors have been also considered as detecting medium of gamma scan-
ner. The properties of several semiconductors for this purpose are listed in Ta-
ble 11.1. A priori, the low atomic number (Z = 14) of silicon is seen as a handicap
for this type of application, although silicon detectors naturally offer excellent spa-
tial and energy resolutions. However, it is possible to use silicon as active medium
devices of gamma camera by combining silicon with high-Z material (W or Pb,
for instance) to form a sampling calorimeter of high effective atomic number which
will serve as SPECT detector. The Silicon Collimated Photon Imaging Calorimeter,
(SiCPICal) [D’Angelo, Leroy, Pensotti and Rancoita (1995)], consists of a superpo-
sition of 200 active silicon layers interspersed with 120 µm tungsten layers. A silicon
active layer is made of 145 strips, each strip being 400 µm thick. Each silicon layer
is organized in high spatial resolution readout cells (550 ×550 µm
2
). A detector like
SiCPICal has a high-Z detection volume with high photon conversion, exploiting at
the same time the excellent spatial and energy resolution provided by silicon. The
single readout pixel can b e operated at about 10 MHz, thus no electronic dead time
affects the overall detector performances. This detector can be operated in two dif-
ferent modes. It can select events in which the incoming photons have interacted
either by both Compton and photoelectric effects or by photoelectric effect only. The
operation mode depends on the current discriminator threshold setting.
The formation of a focused image is made possible by the presence of a collimator
with a variable structure, located in front of the detector. This allows one to keep
the minimal image size, of about 0.3 mm
2
for a point source, independently of the
distance between the collimator and the point source.
