Jan Lindhe. Clinical Periodontology
Подождите немного. Документ загружается.

IMPLANTS IN THE LOAD CARRYING PART OF THE DENTITION • 947
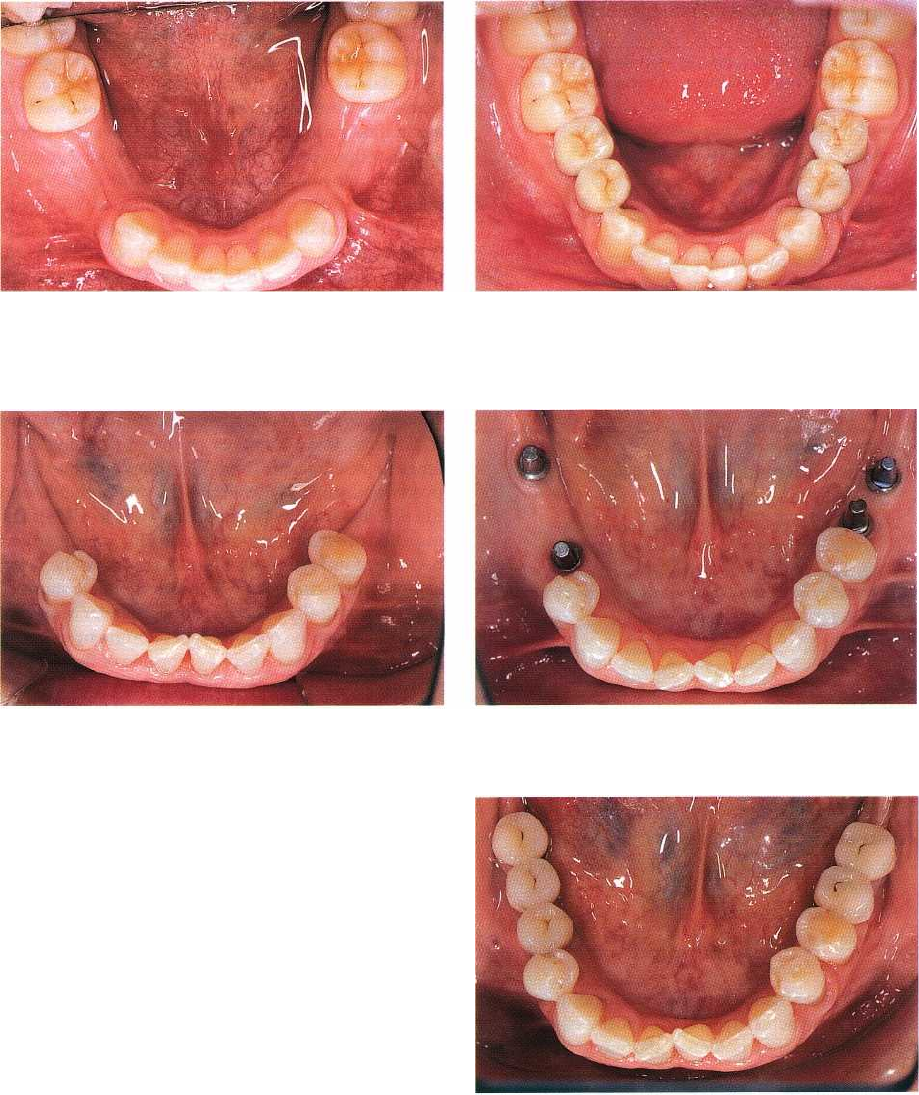
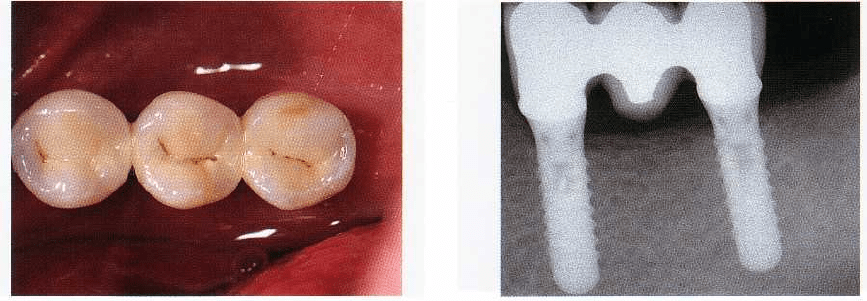
Fig. 41-4. Occlusal view of the mandible of a 22-year
-
old male patient. All premolars are congenitally miss
-
ing, the remainder of the dentition is intact.
Fig. 41-5. Final view after insertion of four implants, re
-
stored with cemented metal-ceramic suprastructures.
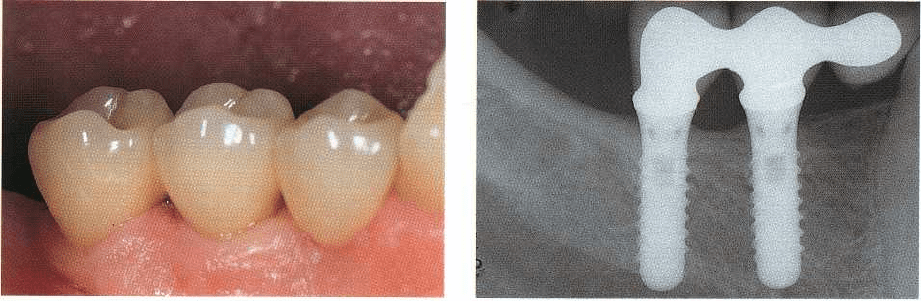
Fig. 41-6. Bilaterally distally shortened dental arch in
the mandible of a 66-year-old female patient.
cal advantage, as it contributes to the reduction of the
lever effect and resulting bending moments acting on
the junction between implant and suprastructure.
This is clinically relevant, as one should be aware of
the existence of an increasing body of evidence report-
ing technical complications, such as loosening/frac-
ture of screws or fracture of components/veneers,
related to implant-supported prosthetic suprastruc-
tures (Lundgren & Laurell 1994, Wie 1995, Hebel &
Gajjar 1997, Rangert et al. 1997, Bosse & Taylor 1998,
Glantz & Nilner 1998, Taylor 1998, Bragger 1999, Goo
-
dacre et al. 1999, Isidor 1999, Keith 1999, Schwarz 2000,
Johnson & Persson 2001). Besides mechanical type of
complications, a number of other conditions that are
rather biological in nature, like for example peri-im-
plantitis, are reported in the recent literature (Elle-
gaard et al. 1997a,b, Ellen 1998, Lang et al. 2000, Brag
-
ger et al. 2001, Quirynen et al. 2001, 2002). As these are
addressed in detail in another chapter, we will only
focus on aspects related to fixed posterior implant
restoration design and maintenance.
It is the aim of this chapter to present clinically
oriented guidelines and procedures for implant ther-
apy of various types of edentulism located in the load
carrying part of the dentition, addressing primarily the
partially dentate patient and mainly focusing on fixed
implant-supported prostheses.
Fig. 41-7. Four implants have been inserted to lengthen
the arch bilaterally to the region of the first molars.
Fig. 41-8. Five premolar-sized metal-ceramic elements
were used to restore the four implants.
Indications for implant restorations in the
load carrying part of the dentition
When it comes to partial edentulism in the posterior
segments of the jaws, implants are increasingly used
to either preserve sound mineralized tooth structure
or
to avoid removable partial dentures (RPDs) and
high-
risk conventional fixed partial dentures (FPDs).
This
includes situations with missing teeth in other-
wise
intact dentitions (Figs. 41-4, 41-5), the distally
shortened dental arch (Figs. 41-6 to 41-8), extended

948 • CHAPTER 41
Table 41-1. Indications for posterior implants
•
Replacement of missing teeth in intact dentitions (e.g.
congenitally missing premolars), i.e. preservation of tooth
structure
•
Avoidance of removable partial dentures (RPDs)
•
Increase of the number of abutments:
•
reduction of the prosthetic risk
•
application of the principle of segmenting
•
ease of eventual reinterventions
•
Maintenance of pre-existing crowns and FPDs
•
Following prosthetic complications and failures
Table 41.2. Impact of dental implants related to the
treatment of posterior partial edentulism
•
Favorable overall long-term results
•
Preservation of mineralized tooth structure
•
"Mechanical" advantages:
•
commercially pure (c.p.) titanium (biocompatibility,
mechanical properties, no risk for caries)
•
reproducible, prefabricated ("machined") primary,
secondary and tertiary components and auxiliary parts
•
Simplified clinical and laboratory protocols
Table 41.3. "High risk" conventional fixed partial
dentures (FPDs)
•
Long-span fixed partial bridges
•
Cantilever units (mainly distal extensions)
•
Missing "strategic" tooth abutments
•
Structurally/periodontally/endodontically compromised tooth
abutments
•
Reduced inter-arch distance
•
Presence of occlusal parafunctions/bruxism
edentulous segments, missing "strategic" tooth abut-
ments and structurally, endodontically or periodon-
tally compromised potential abutment teeth (Table
41-1).
The rapid advance in terms of the broad utilization
of dental implants is not exclusively based on the
associated favorable long-term reports for this treat-
ment modality. Other parameters such as purely "me-
chanical" advantages and the availability of prefabri-
cated components and auxiliary parts, which in turn
contribute notably to the simplification of the treat-
ment, had a significant impact on current concepts
and strategies as well (Table 41-2). Furthermore, clini-
cal decision making based on prosthetically oriented
risk assessment (Table 41-3), frequently leads to the
need for an increased number of abutments. The ob-
jective is to reduce the overall risk associated with a
given prosthetic solution on the one hand, and to
implement the principle of segmenting on the other.
A representative clinical example is given in Figs. 41-9
and 41-10. Instead of a conventional five-unit FPD,
replacing the missing maxillary left first and second
premolars as well as the absent first molar, three im-
plants have been inserted. This approach allowed the
avoidance of a long span bridge, a full coverage prepa
ration of the second molar and an associated surgical
crown lengthening procedure. The additional cost re-
lated to the three implants was justified by an overall
reduced prosthodontic risk. The question about ade-
quate number, size and distribution of implants will
be addressed later in this chapter. Prosthetically ori-
ented risk assessment comprises the comprehensive
evaluation of potential natural abutment teeth, in-
cluding their structural, restorative, periodontal and
endodontic status. As often several well-documented
treatment modalities are possible to replace missing
posterior teeth, this objective evaluation is of primary
importance and represents an ever increasing chal-
lenge to the clinician. This is illustrated by a maxillary
posterior segment where both the first premolar and
the first molar were missing (Figs 41-11 to 41-14). The
insertion of a five-unit tooth-borne FPD was discarded
because of its too invasive nature related to the intact
canine, and owing to a slightly questionable status of
the endodontically treated second premolar in view of
its eventual use as so-called "peer-abutment". Finally,
an implant has been placed at the site of the missing
first premolar and subsequently restored with a sin-
gle-unit restoration. As the proximity of the maxillary
sinus at the location of the missing first molar would
have required a grafting procedure to make an im-
plant installation possible, a three-unit tooth sup-
ported FPD was — after having duly discussed the
respective advantages and shortcomings with the pa-
tient — ultimately chosen. Having attributed to the
moderately compromised second premolar a "strate-
gic value" by using it as abutment of a short span
bridge, there was still a difficulty in consistently es-
tablishing clinical treatment plans that were fully
based on scientific evidence.
Still under the influence of the high level of predict-
ability and longevity reported for implant therapy, the
clinician is currently not only pondering implant-
borne restorations versus conventional FPDs, but in-
creasingly implant versus maintaining a compro-
mised tooth (Figs. 41-15, 41-16). In this particular clini
cal case, the evaluation focused on whether or not it
was objectively opportune to restore the structurally
compromised root of a maxillary second premolar.
This would have required — after elimination of the
decayed dentin — a surgical crown lengthening proce-
dure to create access to the margin, which in turn
would have included the risk for an adverse effect (
furcation proximity of the adjacent first molar) on the
neighboring teeth. Furthermore, a three-unit FPD was
out of the question for obvious reasons. Based on this
rationale and in the context of a more comprehensive
analysis of the situation, it was finally decided to
extract a
per se
treatable root and to replace it by an
IMPLANTS IN THE LOAD CARRYING PART OF THE DENTITION • 949
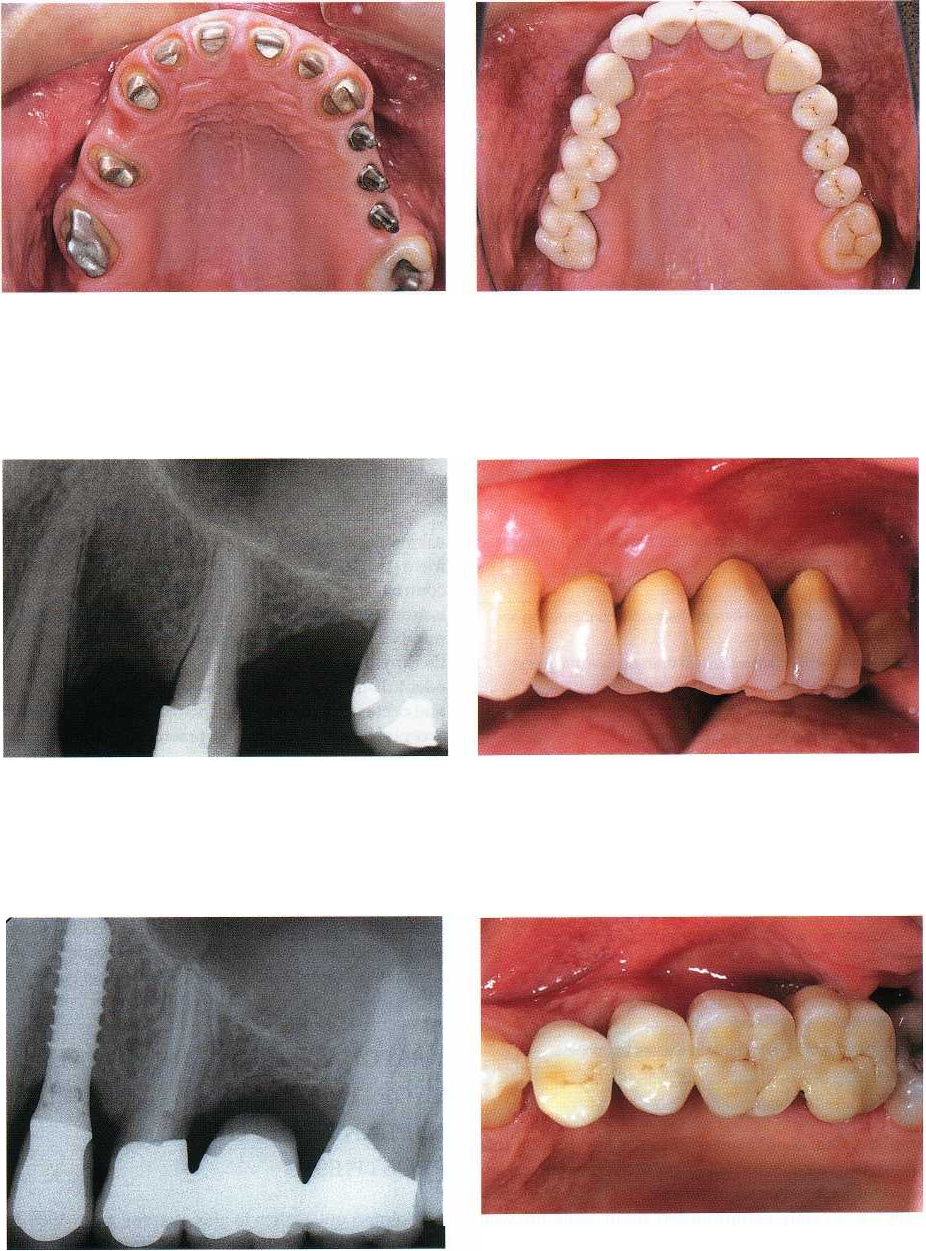
Fig. 41-9. Maxillary occlusal view displaying natural
Fig. 41-10. A similar restorative design has been chosen
and implant abutments prior to the insertion of an ex-for both natural and implant-supported metal-ceramic
tended porcelain-fused-to-metal restoration. In order to
suprastructures.
avoid a high-risk long-span FPD, three implants have been added in the left
posterior segment.
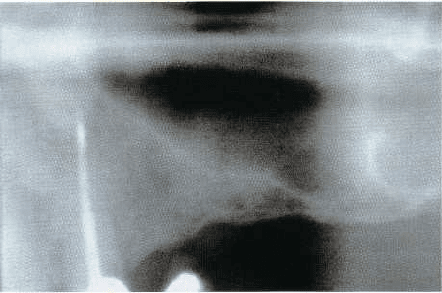
Fig. 41-11. Preoperative radiograph of the left maxilla,
revealing two missing dental elements. One should
note
in particular an intact canine, a structurally re
duced
second premolar and an extended recessus of
the sinus
in the area of the missing first molar.
Fig. 41-13. The postoperative radiograph documents
that
an endodontic revision has been performed on the
second premolar prior to its restoration with an adhe-
sive carbon-fibre-post based build-up and a metal-ce-
ramic crown (bridge retainer).
Fig. 41-12. Vestibular view of the prosthetic rehabilita-
tion of the maxillary left quadrant: an implant-sup-
ported single-tooth restoration on the site of the first
premolar, and a three-unit tooth-borne FPD to replace
the missing first molar.
Fig. 41-14. An identical prosthetic design has been ap
-
plied for both the implant-supported and the tooth-
supported restoration.
950 • CHAPTER 41
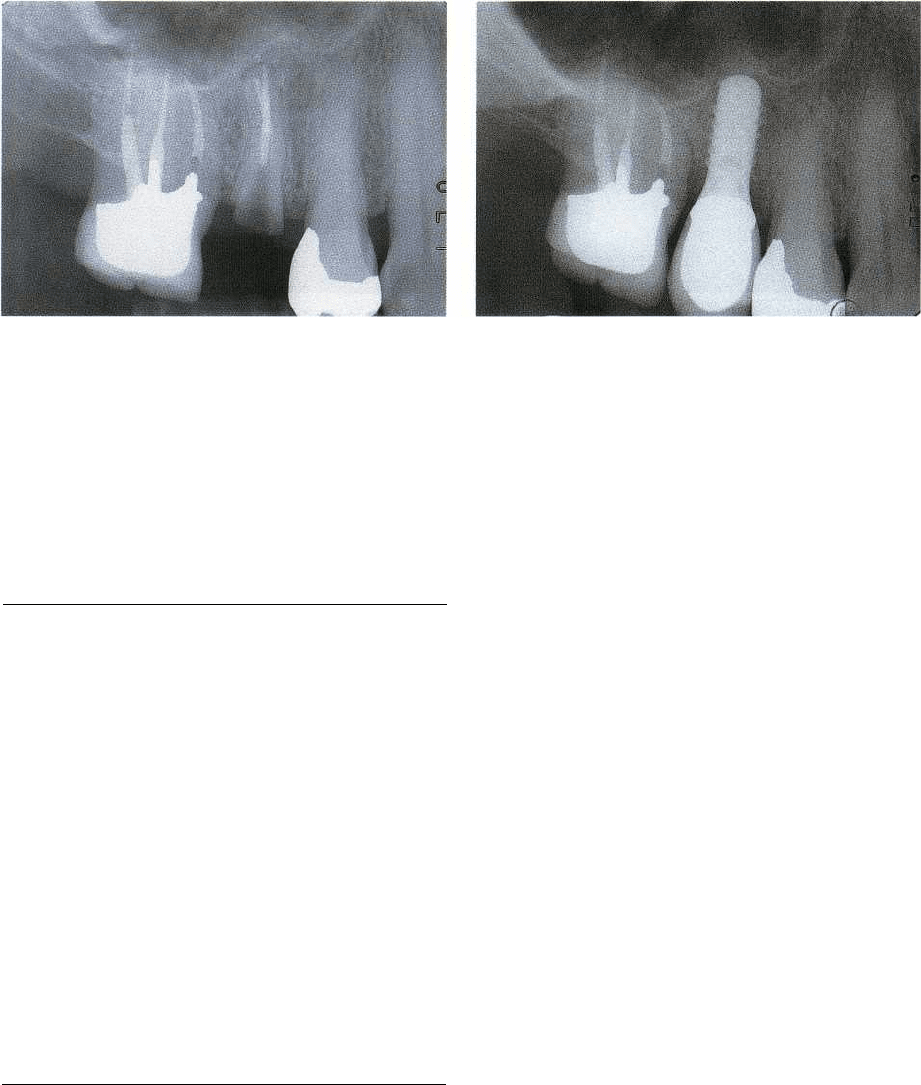
Fig. 41-15. Ad hoc radiograph of the upper right poste
-
rior sextant. One notes the presence of a structurally
compromised second premolar. The treatment of that
particular root would require build-up and crown-
lengthening (margin exposure, creation of an adequate
ferrule) which in turn would negatively affect the adja-
cent teeth.
Fig. 41-16. The postoperative radiograph documents
that the root of the second premolar has been replaced
by a single-tooth implant restoration. In particular, the
pre-existing metal-ceramic crown on the first molar
could be maintained by this approach.
Table 41.4. Controversial issues related to posterior
implant restorations
•
Adequate number, size (length/diameter), configuration and
distribution of implants
•
Cemented versus screw-retained (
transocclusal/transverse
screw-retention)
•
Single units versus splinted adjacent implant restorations
•
Longest possible versus shorter implants
•
Impact of implant axis
•
Optimal implant shoulder sink depth
•
Minimal ratio between implant length and suprastructure
height
•
Combination of natural teeth and implants in the same
restoration
•
Design of the optimal abutment-to-implant connection
•
Implant-specific occlusal concepts, including occluding
restorative materials, non-axial loading, type of guidance
during mandibular excursions
•
Healing times prior to functional loading
(
immediate/early/delayed)
•
Significance of offset/staggered implant positioning
implant. One should never forget, however, that this
trend to consider, under certain circumstances, an
implant as a better solution than treating "acrobati-
cally" a severely compromised tooth, calls for well
defined evidence-based respective criteria and repre-
sents a non-negligible ethical responsibility for the
clinician.
Controversial issues
Despite the ever-growing body of scientific evidence
indicating that implant therapy in the partially eden-
tulous patient is an overall highly predictable treat-
ment modality, several conceptional issues remain
controversial to date (Table 41-4). These controversial
issues include open questions addressing adequate
number, size and distribution of implants for optimal
therapy of a given type and configuration of partial
edentulism, as well as parameters related to occlusion
and occlusal materials, to implant axis, to the minimal
acceptable ratio between suprastructure height and
implant length, and – last but not least – related to
questions focusing more specifically on the mechani-
cal aspects and requirements of posterior implant
prosthodontics. Among these, the kind of connection
between implant and abutment have to be mentioned
in particular. Most of these questions will be discussed
in the remainder of this chapter, at length where pos-
sible and appropriate, or more superficially when solid
information is missing or when the topic is more
adequately covered by other authors in this book.
RESTORATION OF THE DISTALLY
SHORTENED ARCH WITH FIXED
IMPLANT-SUPPORTED
PROSTHESES
As pointed out earlier in this chapter, from 1989 to
2002 the distally shortened arch represented the most
frequent indication for the use of implants at the Uni-
versity of Geneva School of Dental Medicine. In fact,
out of a total of 3638 implants, almost 1500 were
placed in distally shortened arches, with close to 1000
implants inserted in the mandible and about 500 in the
posterior maxilla (Fig. 41-1). Implants were primarily
used when premolars were also missing. Whenever
possible, the adopted treatment strategy consisted of
IMPLANTS IN THE LOAD CARRYING PART OF THE DENTITION • 951
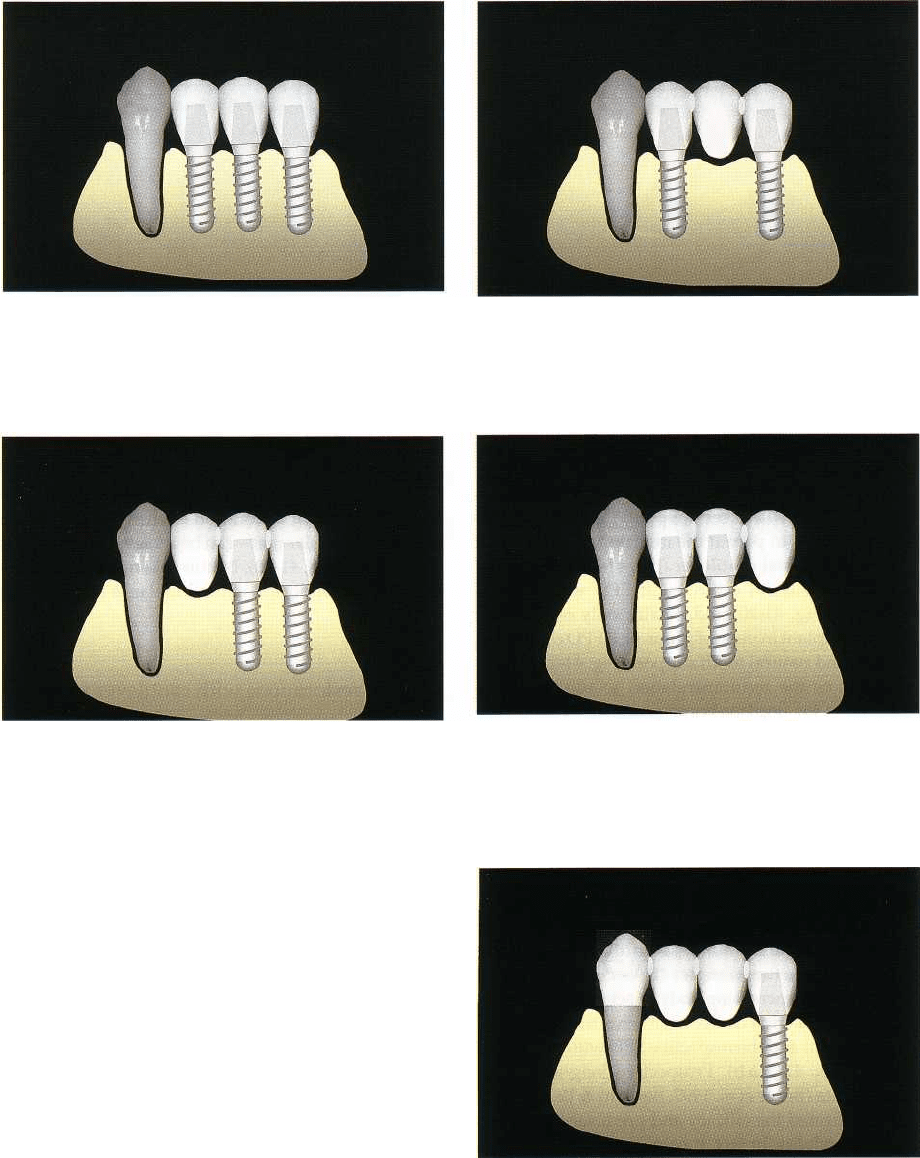
Fig. 41-17. Schematic representation of the distally
shortened dental arch. One therapeutic option consists
of replacing each missing occlusal unit up to the first
molar area with an implant.
Fig. 41-18. An alternative option would be the replace
-
ment of the three missing occlusal units by two im-
plants to support a three-unit suprastructure with a
central pontic.
Fig. 41-19. In a case of an inadequate bone volume in
the area of the missing first premolar, the placement of
two distal implants may be considered, leading to a
three-unit suprastructure with a mesial cantilever.
Fig. 41-20. In a case of an inadequate bone volume in
the area of the missing first molar, the placement of
two mesial implants may be considered, leading to a
three-unit suprastructure with a distal cantilever.
restoring the shortened dental arch to the region of the
first molars. Occasionally, implant therapy was re-
stricted to the premolar area, according to the princi-
ples of the well-established premolar occlusion con-
cept, or extended to the second molar area if an an-
tagonistic contact had to be established for an oppos-
ing natural second molar.
Number, size and distribution of implants
Although it is still unclear to date how many implants
of which dimension at which localization are required
to optimally rehabilitate a given edentulous segment in
the load carrying part of the dentition, a number of
different respective recommendations and related
strategies are currently in use, mostly derived from
traditional prosthodontic experience and attitudes,
and
based on so-called clinical experience and com
mon
sense rather than on solid scientific evidence. In
defense of the situation one should be aware, however,
that it is often difficult to design and carry out ran-
domized clinical trials evaluating exclusively and
Fig. 41-21. In a case of inadequate bone volume in the
area of the two missing premolars, the placement of a
distal implant may be considered, leading to a four-
unit suprastructure with a mixed (tooth and implant)
support.
without interference one specific parameter of con-
ceptual relevance.
In a situation where the canine is the most distal
remaining tooth of a dental arch, at least five different
options can be taken into consideration if one plans to
952 •
CHAPTER 41
Fig. 41-22. (a) Occlusal view of a cemented three-unit metal-ceramic FPD, supported by a mesial and a distal im
-
plant. (b) The corresponding 3-year follow-up radiograph confirms stable conditions at the implant to bone inter
-
face of the two 12 mm solid screw implants.
replace the missing teeth up to the first molar area
(
Figs. 41-17 to 41-21). These include the replacement
of
each missing occlusal unit by one implant (Fig.
41-
17), a mesial and a distal implant to support a
three-
unit FPD with a central pontic (Fig. 41-18), two
distal
implants to permit the insertion of a three-unit
FPD
with a mesial cantilever (Fig. 41-19), two mesial
implants to sustain a three-unit FPD with a distal
cantilever (Fig. 41-20) and, finally, only one distally
inserted implant in view of a four-unit FPD combining
implant and natural tooth support (Fig. 41-21).
As far as the recommendation to use premolar-
sized units for implant-borne posterior FPDs is con-
cerned, it has proven its practical validity in more than
ten years of clinical experience (Buser et al. 1997,
Bernard & Belser 2002). In fact, a crown featuring a
mesio-distal diameter of 7-8 mm at its occlusal surface
allows the optimal generation of a harmonious axial
profile, gradually emerging from the standard im-
plant shoulder
(0
4-5 mm on average) to the maxi-
mum circumference. In addition, the width of the
occlusal table is confined, limiting thereby the risk for
unfavorable bending moments to the implant-abut-
ment-suprastructure complex (Belser et al. 2000).
Based on an increasing body of scientific evidence,
most clinicians' first choice represents the mesial and
distal implant and the respective FPD with the central
pontic (Figs. 41-22a,b). Prospective long-term mul-
ticenter data (Buser et al. 1997, Bernard & Belser 2002)
have confirmed the efficacy and predictability of this
specific modality. In fact, it permits the defined treat-
ment objective with a minimal number of implants
and associated costs. Although presently still lacking
formal evidence at the level of prospectively docu-
mented, randomized clinical trials, it appears from
clinical experience that the use of two implants to
support a four-unit FPD with two central pontics (
Figs. 41-23, 41-24) may be adequate in certain clinical
situations. Clinicians tend to use this approach in the
presence of favorable bone conditions, permitting
standard-size or wide-diameter implants with appro-
priate length (i.e. 8 mm or more).
If the alveolar bone crest dimension is also suffi
cient in an oro-facial direction, the utilization of wide-
diameter/wide-platform implants is preferred. Due
to
their increased dimensions a more adapted supras
-
tructure volume and improved axial emergence pro-
file of the implant restoration – when compared to a
so-called premolar unit – can be achieved in the molar
area (Figs. 41-25, 41-28). By this token the intercuspa
-
tion with an opposing natural molar is facilitated as
well.
Implant restorations with cantilever units
There is strong evidence in the relevant dental litera-
ture that cantilever units – in particular distal exten-
sions – of conventional tooth-borne FPDs are associ-
ated with a significantly higher complication rate
when compared to FPDs featuring a mesial and a
distal abutment and a central pontic. Respective fail-
ure rates could be attributed to decisive factors such
as non-vital abutment teeth as well as specific occlusal
conditions such as a reduced interarch distance
and/or occlusal parafunctions (Glantz & Nilner 1998).
These authors concluded in their review of the current
relevant literature that risks were lower for mechani-
cal failures with cantilevered implant-borne recon-
structions than with comparable conventional fixed
situations. The risks, however, do exist. As loss of
retention, which was one of the frequent complica-
tions encountered on conventional cantilevered pros-
theses, can easily be prevented when it comes to im-
plant-supported restorations of this type, the latter
seem to be a viable alternative in cases where the local
alveolar bone crest conditions do not allow the inser-
tion of an implant at the most favorable location. In
such situations the clinician has to ponder whether a
bone augmentation procedure can be objectively jus-
tified or if the risk for complications of a more simple,
straightforward approach can be considered low.
The 6-year clinical and radiographic follow-up of a
three-unit FPD featuring a mesial cantilever is pre-
sented in Figs. 41-29 and 41-30.

IMPLANTS IN THE LOAD CARRYING PART OF THE DENTITION • 953
Fig. 41-23. Occlusal view of a cemented four-unit metal-
ceramic FPD supported by a mesial and a distal im
plant.
Fig. 41-24. The related 2-year follow-up radiograph
documents that at the distal site a 10 mm solid screw
implant with an increased diameter ("wide body im-
plant") has been used.
Fig. 41-25. Occlusal view of a bilaterally distally short-
ened mandibular arch. Two implants have been placed
on either side to restore the arch to the area of the first
molars. The two distal implants feature an increased di-
ameter, better suited for the replacement of a missing
molar.
Fig. 41-26. The master model comprises color-coded
aluminum laboratory analogues at the implant sites, fa-
cilitating the technician's work in view of the supra-
structure fabrication. This is in contrast to the site of
the
prepared natural abutment.
Fig. 41-27. Once the metal-ceramic restorations are com-
pleted, no noticeable design difference between im
plant-
supported and tooth-supported suprastructures is
apparent.
Fig. 41-28. The respective clinical view confirms an ac-
ceptable integration of the four implant restorations in
the existing natural dentition.
954 • CHAPTER 41
Fig. 41-29. Six-year clinical follow-up view of a
mandibular three-unit FPD supported by two distal im
-
plants.
Combination of implant and natural tooth
support
There is general agreement that, from a purely scien
-
tific point of view, the combination of implants and
natural teeth to support a common FPD is feasible.
Clinical studies reporting prospectively documented
long-term data did not show adverse effects of splint
-
ing teeth to implants (Olsson et al. 1995, Gunne et al.
1997, 1999, Hosny et al. 2000, Lindh et al. 2001, Naert
et al. 2001a,b, Tangerud et al. 2002). The issue of con
-
necting implants and teeth by means of rigid or non-
rigid connectors, however, remains controversial to
date, but intrusion of natural roots has been reported
in the literature as a potential hazard of non-rigid
connection (Sheets & Earthman 1993). Most of the
recently published respective literature reviews con-
clude with the general clinical recommendation that
one should avoid, whenever possible, the direct com-
bination of implants and teeth as it may frequently
lead to a more complicated type of prosthesis. If there
is
no viable alternative available, a rigid type of con-
nection is preferred to prevent an eventual intrusion
of the involved abutment teeth (Lundgren & Laurell
1994, Gross & Laufer 1997).
Furthermore, it has been demonstrated that despite
the fundamental difference between an osseointe-
grated implant and a tooth surrounded by a periodon
-
tal ligament, the assumption that when these two
structures are combined, the entire occlusal load will
ultimately go to the implant and hence create an un-
favorable "cantilever-type" situation, is not valid from
a scientific point of view (Richter, Isidor, Bragger). In
fact, under normal function, such as during mastica-
tion, the tooth abutment is similarly load-bearing.
This may change, however, during severe occlusal
parafunctions, like nocturnal bruxism.
Fig. 41-30. The 6-year radiograph displays stable bony
conditions around the two implants supporting a ce
-
mented suprastructure with a premolar-sized mesial
cantilever unit.
Sites with extended horizontal bone volume
deficiencies and/or anterior sinus floor
proximity
It is not infrequent that distally shortened dental
arches do not feature an adequate local bone volume
at the prospective implant sites. This may refer to bone
height, bone width, alveolar bone crest axis or to the
vicinity of noble structures such as the mandibular
alveolar nerve canal or the anterior part of the maxil-
lary sinus. Often a combination of several of the men-
tioned limitations is encountered. As implant inser-
tion is clearly a three-dimensional surgical and re-
storative procedure on the one hand, and as "restora-
tion-driven" rather than "bone-driven" implant
placement is widely recommended on the other hand,
a
meticulous presurgical site analysis - based on the
envisioned treatment objective - is of primary impor-
tance. In order to keep the treatment as easy and
finally also as cost-effective as possible, one should
comprehensively evaluate whether a minor deviation
from the ideal implant position could be considered
acceptable, i.e. not leading to a compromise which
might adversely affect predictability, longevity
and/or
subjective comfort. This approach may still
permit in
some cases a professionally defendable re
sult, but
without a complexity of treatment that would
be
difficult to bear by some patients.
Advanced invasive procedures like lateral bone
augmentation, anterior sinus floor elevation, alveolar
ridge splitting or distraction osteogenesis, require a
high level of skills and respective experience and
hence should only be deployed if the relation between
benefit and risk/cost is soundly balanced (Buser et al.
1993, 1995, 1996, 1999, 2002, Chiapasco et al. 1999,
2001a, Simion et al. 2001, von Arx et al. 2001a,b,
Zitzmann et al. 2001).
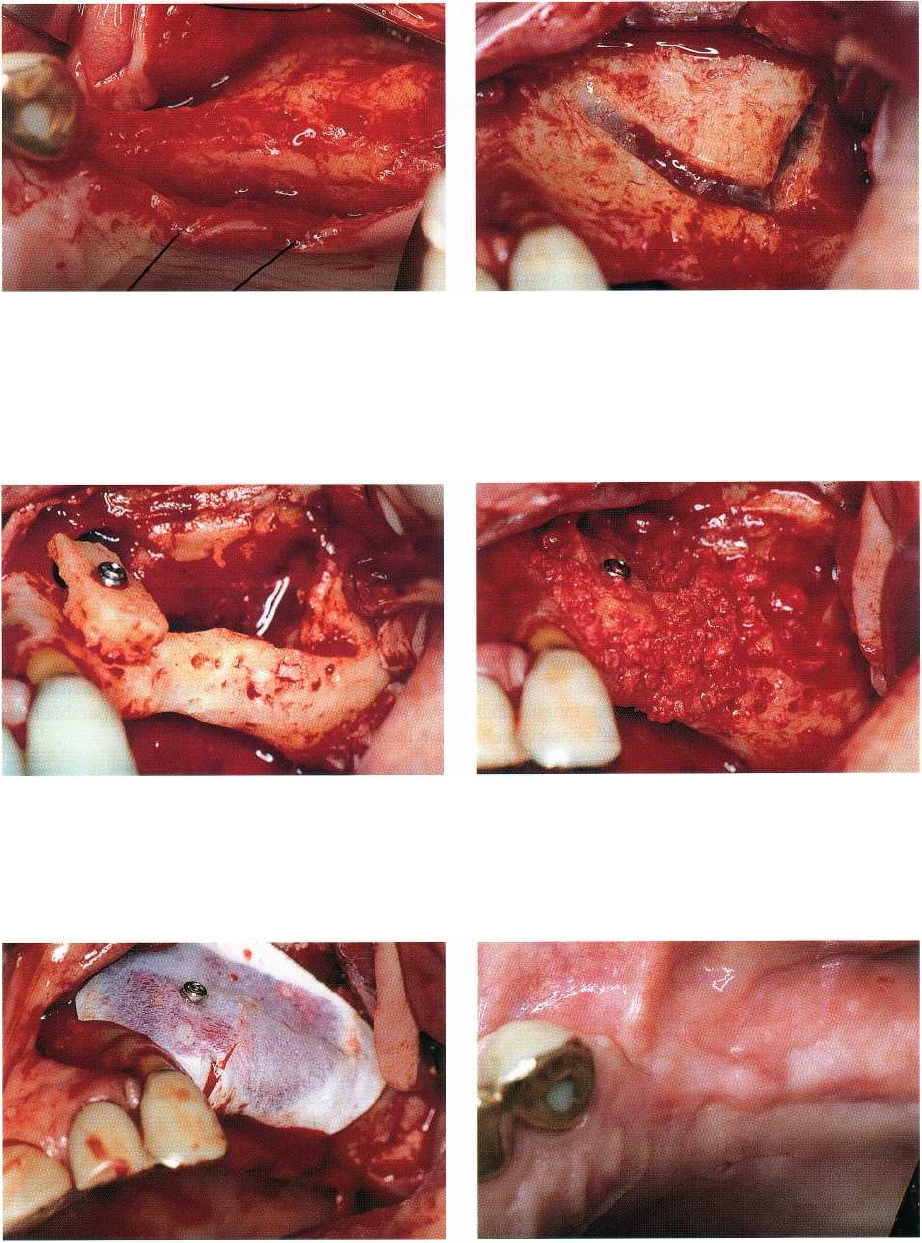
In this specific context, a complex implant treat-
ment of a 67-year-old male patient whose most distal
remaining tooth in the left maxilla was an endodonti-
cally treated canine, is shown in Figs. 41-31 to 41-44.
Preoperative diagnosis revealed the necessity to per-
IMPLANTS IN THE LOAD CARRYING PART OF THE DENTITION • 955
form — according to a staged approach — first a com
-
bined lateral bone augmentation procedure and ante-
rior sinus floor elevation and, after a six months'
healing period, the insertion of implants. For the sinus
floor elevation the so-called "trap-door" technique
was
used and the created space grafted with auto
genous
bone chips and BioOss®. The lateral bone
augmentation comprised the fixation of a large block
graft in the area of the first premolar. After application
of an ePTFE barrier membrane, primary wound clo-
sure was achieved by sectioning of the periosteum of
the respective muco-periosteal flap. This often leads
to a lack of attached keratinized mucosa on the ves-
tibular aspect of the surgical site, which has to be
subsequently corrected, most conveniently at the mo
-
ment of implant placement. When it comes to sites that
have been previously grafted, the majority of sur-
geons advocate inserting one implant per missing
occlusal unit. This attitude appears to be based more
on the reflection that the overall heaviness of the
approach would largely justify this additional secu-
rity and/or on the hypothesis that augmented bone
may not have exactly the same "load-bearing" capac-
ity as the pre-existing bone, than on irrefutable scien
-
tific evidence. Accordingly, three adjacent screw-type
implants — the most distal one an increased-diameter
titanium screw — had been placed and subsequently
restored by a three-unit splinted metal-ceramic FPD
(
Figs. 41-38 to 41-44).
Results from a recently published longitudinal
clinical study (Buser et al. 2002) on 40 consecutively
Fig. 41-31. Initial radiograph of the maxillary left poste
rior segment of a 67-year-old male patient. The
canine
represents the most distal remaining tooth
element.
Note the marked extension of the anterior
recessus of
the sinus.
enrolled patients, who were first treated with a lateral
bone augmentation procedure and subsequently, in a
second stage, received implants inserted in the pre-
viously augmented area. In the totality of treated sites
implants could finally be placed as planned, and at the
5-year clinical and radiographic follow-up examina-
tion a 97% success rate was revealed. It was thus
concluded that lateral bone augmentation is indeed a
predictable procedure and that implants sub-
sequently inserted in augmented sites do have similar
success rates to implants placed in comparable non-
augmented sites.
956 • CHAPTER
41
Fig. 41-32. After elevation of a mucoperiosteal flap, anFig. 41-33. In view of an anterior sinus floor elevation
insufficient horizontal bone volume in the region of the
procedure, the first step for a respective osteotomy is
premolars becomes apparent.
performed. Attention is given not to perforate the
Schneiderian membrane.
Fig. 41-34. After the so-called "hinge-door" procedure
Fig. 41-35. The lateral bone augmentation procedure is
in the region of the maxillary sinus, an autogenous
completed by adding a combination of autogenous
bone block graft, harvested from the patient's retromo-bone chips, bone slurry and BioOss®.
lar area, is positioned and then immobilized by a fixation screw at the location of the missing first
premolar.
Fig. 41-36. Prior to flap repositioning and suturing, a
barrier membrane is applied.
Fig. 41-37. One month after primary wound closure
and uneventful healing, the involved soft tissues have
recovered their normal appearance.
