Jan Lindhe. Clinical Periodontology
Подождите немного. Документ загружается.

RADIOGRAPHIC EXAMINATION • 847
Fig. 36-16. When a tomographic technique is used with
which thin tomographic layers can be produced, ghost
shadows from surrounding teeth are minimized.
surrounding teeth, particularly if metal crowns or
fillings are present. A technique yielding thin ( 2 mm)
tomographic layers (Fig. 36-16) should be used (Gron
-
dahl et al. 1996).
In many single implant cases, sufficient informa-
tion about the width and height of available bone
volume can be obtained from a clinical examination
supplemented by intraoral radiography. Tomography
is recommended when patient history, the clinical
examination and intraoral radiographs lead to a sus-
picion of a narrow width of the jaw bone. Tomography
is also recommended when a single implant is to be
placed above the mandibular canal.
Conclusion
The distance between opposing root surfaces is pref-
erably measured in intraoral radiographs. Slight vari-
ations in patient positioning can make such a distance
appear too small or too large in panoramic images.
If tomography is considered necessary, thin to-
mographic layers should be used to avoid disturbing
ghost shadows.
Tomography is recommended when a single im-
plant is to be placed above the mandibular canal.
POSTOPERATIVE RADIOGRAPHY
At
abutment connection
For some implant systems such as the Branemark
System
®
it is necessary to control the fit between the
abutment and the implant pillar once the abutment
has been seated. Even a small intermediary gap means
that forces from the suprastructure will not be opti-
mally transferred to the implant pillar. Later, this can
cause a fracture of the abutment screw or of the im-
plant pillar itself. To be able to radiographically dis-
close a small misfit, intraoral radiographs should be
used because of their high geometric resolution. The
irradiation geometry has to be such that the X-ray
beam is directed at a right angle to the longitudinal
axis of the implant. Even small deviations from a
direction of the incident radiation parallel to the upper
surface of the implant and the opposing surface of the
abutment can make a clinically significant gap invis-
ible. Because of less geometric resolution and difficul
-
ties in individual adjustment of the radiation beam
direction, panoramic images cannot be recommended
for abutment controls.
Following crown-bridge installation
Immediately following the connection of the crowns
or
the bridgework, radiographs should be taken both to
provide necessary information at this point in time
and
to serve as reference images for subsequent follow-
up radiographs. The information to be obtained
at this
time again concerns the fit between implant and
abutment, but also that between abutment and the
suprastructure. In addition, the level of the marginal
bone must be determined and the conditions of the
bone that surrounds the implant evaluated.
High demands on image quality
To be meaningful, images obtained in conjunction
with crown or bridge installation as well as at sub-
sequent follow-ups must be of the best possible qual-
ity as regards density and contrast as well as radiation
geometry. Most problems concerning density and con
-
trast depend on suboptimal film developing. Conse-
quently, a strict program for quality maintenance of
the dark-room procedure must be followed. Through-
out the follow-up period the exposure factors (tube
current, tube voltage and focus-to-film distance) must
be kept constant. As regards radiation geometry it is
of the utmost importance that images are taken with
the film placed parallel to the implant and that the
radiation beam is directed perpendicular to the longi-
tudinal axis of the implant (Fig. 36-17). Only then can
a correct estimate of the marginal bone level relative
to some reference point on the implant be obtained.
Furthermore, the bone-implant interface zone cannot
be evaluated in its entirety if the bone, reaching into
the inner parts of the threads, is not visualized. Be-
cause of the high demands made in terms of irradia-
tion geometry and resolution, intraoral radiographs
are to be preferred for all follow-up examinations. In
some cases it is not possible to display the implant in
its entire length when a strict paralleling technique is
used. In the absence of clinical signs and symptoms
this is acceptable, because the significant changes that

848 • CHAPTER 36
Fig. 36-17. For postoperative control radiographs the in
cident X-ray beam should be perpendicular to the lon
-
gitudinal axis of the implant and the film.
may occur are most often found around the marginal
part of the implant. In the presence of clinical signs
and symptoms, such as pain, suppuration and im-
plant mobility, radiographs obtained with the paral-
leling technique can be supplemented with radio-
graphs obtained with a radiation beam angulation
which visualizes the "apical" part of the implant.
Analysis of postoperative radiographs
In the postoperative radiographs the marginal bone
level is compared with that in radiographs obtained
immediately following crown and bridge installation
(
Bragger 1994). Therefore, the demands on radio-
graphs similar in irradiation geometry, density and
contrast are high (Fig. 36-18). When threaded implants
are used, optimal projections in the vertical plan are
at hand when the threads on both sides of the implant
are clearly seen. Due to the spiral right-turned path of
the threads it is possible to determine how to adjust
the angulation of the X-ray beam if the threads are not
clearly seen on either side. Diffuse threads on the right
side of the implant indicate a direction of the X-ray
beam too much from above while diffuse threads on
the left side indicate a beam direction too much from
below. Corrections of the irradiation geometry are
necessary to make it possible to correctly ascertain any
changes in the marginal bone level over time. Even
relatively moderate variations in irradiation geometry
between radiographs to be compared can lead to dif-
ferences in the bone level estimates. Because the mar
ginal bone often can be relatively thin in the buccolin
-
gual direction, or less well mineralized in the early
stages of the postoperative phase, a high density of the
radiographs can make it less visible. This can also lead
to erroneous conclusions about bone level changes.
An important aim of the postoperative controls is
to determine lack of osseointegration. Because it
would be both too costly and inconvenient to detach
the bridgework at all postoperative clinical controls,
radiography is the most feasible tool to use. Radiog-
raphically, lack of osseointegration and thus lack of
clinical stability of the implant is indicated by a radi-
olucent line along the implant surface (Fig. 36-19).
However, false-negative diagnoses can be made when
the soft tissue layer surrounding the implant is not
wide enough to overcome the resolution of the radio-
graphic system, including that of the observer. On the
other hand, false-positive diagnoses can be made,
above all due to the presence of a so-called Mach band
effect. This causes a thin area adjacent to an area of a
lower radiographic density, in this case the implant,
to look darker than it is in reality. Although radiogra
-
phy is not a perfect tool to reveal lack of osseointegra
-
tion, it has been demonstrated that it performs as well
in this respect as it does for approximal caries diagno
-
sis (Sunden et al. 1995). However, an important pre-
requisite is radiographs of high quality.
At the postoperative follow-ups the state of the
implant components should also be controlled. Al-
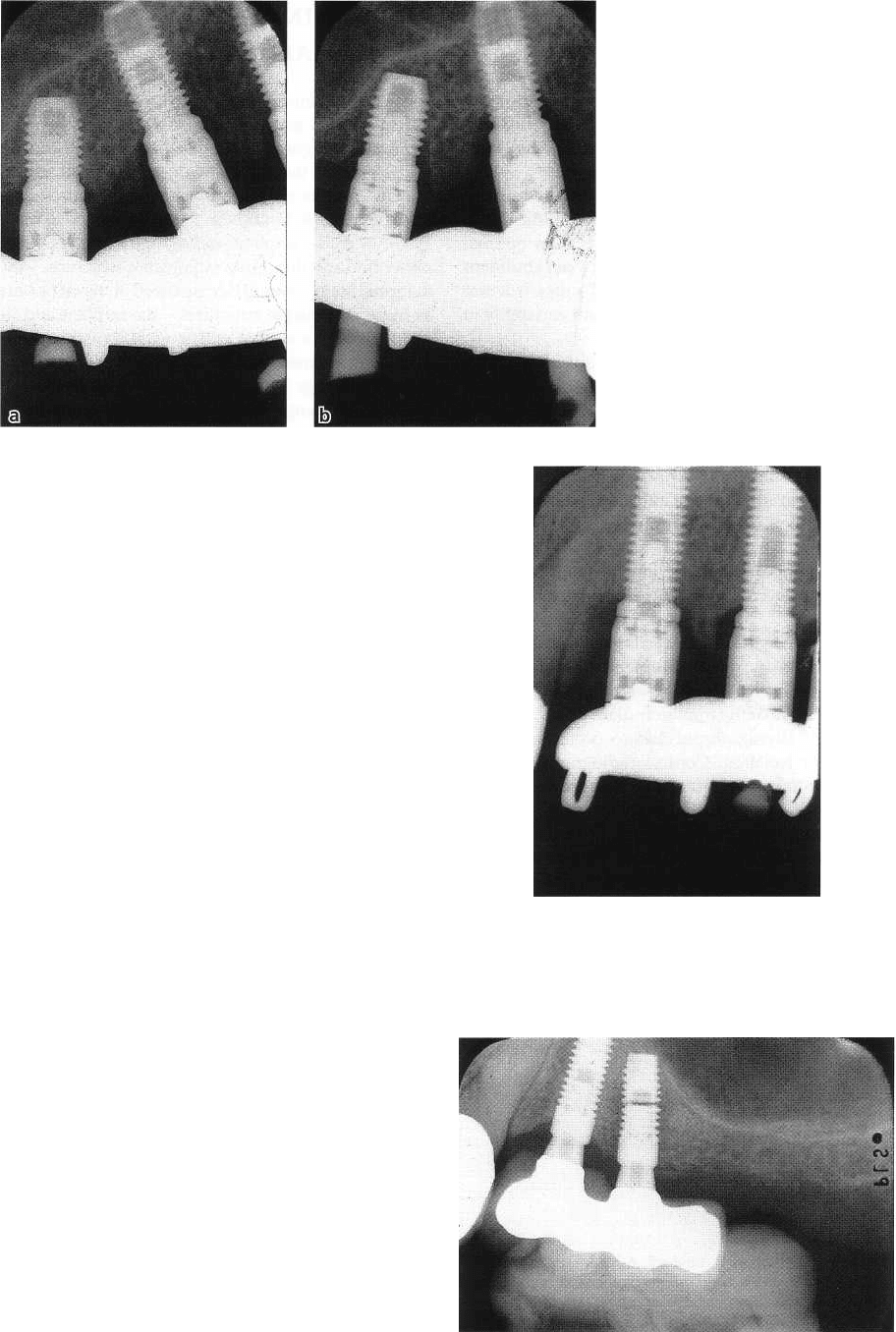
Fig. 36-18. When proper projections are used, the
threads on both sides of the implant are clearly seen.
The marginal bone level can be evaluated relative to a
reference point on the implant.
RADIOGRAPHIC EXAMINATION •
8
49
Fig.
36-19.
Postoperative radio-
graph taken in connection with
bridge installation (a) with no
signs of failure. In a radiograph
taken
2 years later (b) the most
posterior implant is surrounded
by a radiolucent zone indicating
lack of osseointegration.
though infrequently, fractures of the abutment screw
(
Fig. 36-20) or the implant pillar itself (Fig. 36-21)
occur. An indirect sign of a fracture of the abutment
screw is the appearance of a gap between abutment
and the implant pillar. An indirect sign of a fracture of
the implant pillar itself is a pronounced, localized
reduction in the marginal bone level. To be able to
directly detect fractures of the implant components,
the density of the radiographs has to be relatively
high. Hence, there are conflicting demands on the
density of the postoperative radiographs.
Subsequent follow-up examinations
Most clinically significant changes occur during the
first year of function. Control radiographs 6-12
months after crown or bridge installation can there-
fore be recommended. When using systems for which
high success rates have been reported, the application
of rigid protocols for subsequent, frequent radio-
graphic examinations can be questioned, once a clini
-
cian has established that his /her success rate is similar
to that reported from multi-center studies. However,
for a clinician to determine that he/she has reached a
similar, high success rate, control radiography can be
recommended at intervals of 2-3 years. The same is the
case when systems are used for which long-term re-
sults are still lacking. Naturally, any clinical signs and
symptoms which cannot be explained without radi-
ography make this justified at any point in time.
Since pathologic conditions in and around remain
-
ing teeth can have a negative effect on the fate of the
implants, control radiographs covering the teeth
should also be considered. When and how often these
should be obtained depends on the results of the
clinical examination. However, for conditions for
which the clinical examination gives little guidance,
e.g. periapical lesions, annual radiography can be
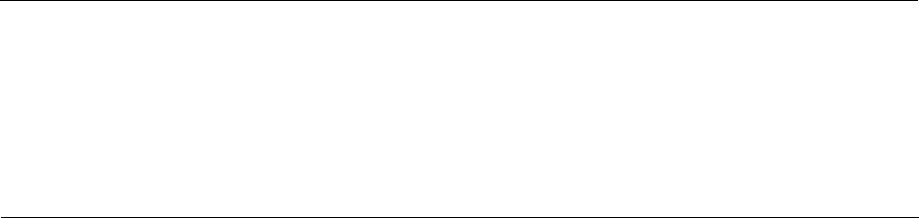
Fig.
36-20.
Fracture of the abutment screw (left im-
plant). Notice dislocation of fragments and small gap
between abutment and implant pillar.
Fig.
36-21. Fracture of the implant pillar. Also notice
lack of osseo-integration.
850 • CHAPTER 36
recommended until it is clear that healing is well
under way.
Conclusion
For abutment controls and all follow-up examina-
tions, intraoral radiography should be used.
Reference images should be taken immediately fol-
lowing crown/bridge installation.
The film should be placed parallel to the implant
and the radiation beam be directed perpendicular to
its longitudinal axis. Small deviations from optimal
projections can make small misfits between abutment
and implant or between implant and suprastructure
invisible. They can also cause significant variability in
bone level estimates.
The visibility of the threads can be used to deter-
mine whether proper projections have been used or
not.
A quality assurance protocol should be used to
maintain optimal image quality over time in terms of
density and contrast.
Variations in film density and contrast can lead to
erroneous conclusions regarding bone level changes
over time.
Provided there is proper image quality, lack of
osseointegration can be determined with a reasonably
high accuracy.
A gap between the implant pillar and the abutment
may be an indirect sign of abutment screw fracture.
A pronounced, localized loss of marginal bone may
indicate fracture of the implant pillar.
Most clinically significant changes occur during the
first year of function. Control radiographs should
therefore be taken
6-12
months after crown/bridge
installation.
Subsequent radiographs in asymptomatic patients
should be obtained with intervals of
2-3
years depend
-
ent on system used and success rates obtained, other
-
wise when clinically needed.
Remaining teeth should be regularly controlled!
DIGITAL INTRAORAL
RADIOGRAPHY
To avoid problems pertaining to the darkroom proce-
dures it seems tempting to use a digital system for
intra oral radiography. These could also contribute to
a
lowering of the radiation doses, since all digital
systems require considerably lower exposures than
film (Wenzel & Grondahl 1995, Borg & Grondahl
1996). Because implant radiography requires that
rather thin and thus quite radiolucent structures — the
marginal bone — should be visualized at the same time
as more radiopaque structures — the implant and its
components — a system with a wide dynamic range
can be recommended. Among the systems so far
tested, the image plate systems seem to have the wid-
est dynamic range. They can thus show structures
with a small mass density with the same exposure
with which they can show structures with a consider
-
ably larger mass density. A wide dynamic range also
means that exposure variations exert a limited influ-
ence on image quality (Borg & Grondahl 1996).
Digital radiographs can be subjected to image proc
-
essing with which the images can be altered to achieve
task specific image characteristics. For example, den-
sity and contrast can be lowered for evaluations of the
marginal bone and increased for evaluations of the
implant components. It is also conceivable that the
influence of the Mach band effect can be reduced
through image processing. The possibilities of
pseudo-coloring, that is, to assign different colors to
different gray-level values, have been suggested to be
of value in evaluating the bone surrounding the im-
plant. So has the possibility to graphically display the
variations in gray-level values over a distance, e.g. one
that covers the implant-bone interface.
Little scientific evidence of the value of these types
of image processing procedures in implant evaluation
has been presented. However, subtraction of serially
taken radiographs in combination with pseudo-color-
ing has been able to demonstrate changes between
radiographs not readily apparent by unaided visual
observations (Bragger & Pasquali 1989, Bragger et al.
1991). It has also been shown that edge enhancement
can be of value to detect a distance between implant
and surrounding bone that may be undetected in
conventional radiographs (Borg et al.
2000).
REFERENCES
Andersson, B., Odman, P., Lindvall, A-M. & Lithner, B. (1995).
Single-tooth restorations on osseointegrated implants. Re-
sults and experiences from a prospective study after 2-3 years.
International Journal of Oral and Maxillofacial Implants
10, 702-
711.
Borg, E. & Grondahl, H-G. (1996). On the dynamic range of
different X-ray photon detectors in intra-oral radiography. A
comparison of image quality in film, charge-coupled device
and storage phosphor systems.
Den tomaxillofacial Radiology
25, 82-88.
Borg, E., Grondahl, K., Persson, L.G. & Grondahl, H-G. (2000).
Marginal bone level around implants assessed in digital and
film radiographs:
in vivo
study in the dog.
Clinical Implant
Dentistry and Related Research
2,
10-17.
Bragger, U. (1994). Radiographic parameters for the evaluation
of peri-implant tissues.
Periodontology 2000
4, 87-97.
RADIOGRAPHIC EXAMINATION • 851
Bragger, U., Burgin, W., Lang, N.P. & Buser, D. (1991). Digital
subtraction radiography for the assessment of changes in
peri-
implant bone density.
International Journal of Oral and
Maxillofacial Implants
6,
160-166.
Bragger, U.
It
Pasquali, L. (1989). Color conversion of alveolar
bone density changes in digital subtraction images.
Journal of
Clinical
Periodontology
16,
209-214.
Bruggenkate, C.M., Krekeler, G., Kraaijenhagen, H.A., Foizik, C.,
Nat, P. & Oosterbeek, H.S. (1993). Hemorrhage of the floor of
the mouth resulting from lingual perforation during implant
placement: a clinical report.
International Journal
of
Oral and
Maxillofacial Implants 8,
329-334.
Clark, D.E., Danforth, R.A., Barnes, R.W. It Burtch, M.L. (1990).
Radiation absorbed from dental implant radiography: A com-
parison of linear tomography, CT scan and panoramic and
intra-oral techniques.
Journal of Oral Implants
16, 156-164.
Curry, T., Dowdey J. & Murry R. (1990).
Christensen's introduction
to
the physics of radiology.
Philadelphia: Lea and Febiger.
Eckerdal, O. & Kvint, S. (1986). Presurgical planning for osseoin-
tegrated implants in the maxilla. A tomographic evaluation
of
available alveolar bone and morphological relations in the
maxilla.
International Journal of Oral and Maxillofacial Surgery
15,
722-6.
Ekestubbe, A. It Grondahl, H-G. (1993). Reliability of spiral
tomography with the Scanora
®
technique for dental implant
planning.
Clinical Oral Implant Research 4,
195-202.
Ekestubbe, A., Grondahl, K., Ekholm, S., Johansson, P.E. & Gron
-
dahl, H-G. (1996). Low-dose tomographic techniques for den-
tal implant planning.
International Journal of Oral and Maxillo-
facial Implants 5,
650-659.
Ekestubbe, A., Thilander, A., Grondahl, K. & Grondahl, H-G. (
1993). Absorbed doses from computed tomography for den
tal
implant surgery: comparison with conventional tomogra
phy.
Dentomaxillofacical Radiology 22,
13-17.
Esposito, M., Ekestubbe, A. & Grondahl, K. (1993). Radiological
evaluation of marginal bone loss at tooth surfaces facing
single
Branemark implants.
Clinical Oral Implant Research
4,
151-
157.
Fredriksen, N.L., Benson, B.W. & Solokowski, T.W. (1995). Effec-
tive dose and risk assessment from computed tomography of
the maxillofacial complex.
Dentomaxillofacial Radiology 24,
55-
58.
Grondahl, K., Ekestubbe, A. & Grondahl, H-G. (1996).
Radiogra-
phy in oral endosseuos prosthetics.
Goteborg: Nobel Biocare.
Grondahl, K., Ekestubbe, A., Grondahl, H-G. & Johnson, T.
(
1991). Reliability of hypocycloidal tomography for the evalu-
ation
of
the distance
from
the alveolar crest to the mandibular
canal.
Dentomaxillofacial Radiology
19, 200-204.
Ivanoff, C.J, Sermerby L. & Lekholm, U. (1996). Influence of
mono- and bicortical anchorage on the integration of titanium
implants. A study in the rabbit tibia.
International Journal of
Oral and Maxillofacial Surgery 25,
229-235.
Lindh, C., Petersson, A. & Klinge, B. (1992). Visualisation of the
mandibular canal by different radiographic techniques.
Clini-
cal Oral Implant Research 3,
90-97.
Lindh, C., Petersson, A. & Klinge, B. (1995). Measurements of
distances related to the mandibular canal in radiographs.
Clinical Oral Implant Research
6,
96-103.
Lindh, C., Petersson, A., Klinge, B. & Nilsson, M. (1996b). Tra-
becular bone volume and bone mineral density in the mandi-
ble.
Dentomaxillofacial Radiology 26,
101-106.
Lindh, C., Petersson, A. & Roblin, M. (1996a). Assessment of the
trabecular pattern prior to endosseous implant treatment.
Dentomaxillofacial Radiology 82,
335-343.
Sennerby, L., Thomsen, P. & Ericson, L. (1992). Amorphometrical
and biomechanical comparison of titanium implants inserted
in rabbit cortical and cancellous bone.
International Journal of
Oral and Maxillofacial Surgery
7, 62-71.
Sunden, S., Grondahl, K. & Grondahl, H-G. (1995). Accuracy and
precision in the radiographic diagnosis of clinical instability
in
Branemark dental implants.
Clinical Oral Implant Research
6,
220-226.
Tronje, G. (1982). Image distortion in rotational panoramic radi-
ography.
Dentomaxillofacial Radiology
Suppl 3.
van der Stelt, P. (1979).
Periapical hone lesions.
Dissertation. Am-
sterdam: University of Amsterdam.
Wenzel, A. It Grondahl, H-G. (1995). Direct digital radiography
in
the dental office.
International Dental Journal
45, 27-34.
CHAPTER 37
The Surgical Site
ULF LEKHOLM
Preoperative examination
Primary judgment
Secondary assessment
Treatment planning
Implant placement
Flap design
Bone drilling
Implant
position Implant
direction
Cortical
stabilization
Implant
selection
Healing time
PREOPERATIVE EXAMINATION
The two main prerequisites for proper implant treat-
ment are: well-performed preoperative examination
and thorough pretreatment planning. In part, the out
-
come is also dependent on the medical condition of
the patient as well as the local health and bone mor-
phology of the area considered for implants. Conse-
quently, adequate preoperative assessments, adapted
to individual needs, have to be performed before any
implant treatment is offered. When carried out, the
examinations have to be cost effective and mainly
based on conventional techniques, at least in the rou
-
tine situation. The below protocol, based on experi-
ence of the Branemark implant system, may constitute
one practical way of working in the partially edentu-
lous patient.
h1
essence, the same principles can, of
course, also be valid when working with other oral
implant protocols. The following preoperative exami-
nation levels are thereby recommended:
1.
primary judgment (prosthetic level)
2.
secondary assessment (surgical level)
3.
treatment planning (combined surgical-prosthetic
level)
Primary judgment
When patients are referred – seeking implant treat-
ment – the restorative dentist/prosthodontist must
first of all identify the specific oral problems that the
patient is having. It is also important to discuss his or
her esthetic and functional demands in case of being
treated, i.e. to elucidate what the patient really is
expecting of the treatment. The patient can first then
be presented with alternative prosthetic solutions, im
-
plant therapy being only one option. If implants are
considered, there should be clear motivations given,
as implant treatment ought not to be routinely offered
just because a tooth or some teeth are missing. Indica
tions for oral implants may, for example, be present
in
partially edentulous situations, when removable par
tial dentures are not accepted and fixed prosthetic
reconstructions are wanted, but where remaining
teeth are either too few or are so located that they can
not support conventional fixed bridgework. Implants
may also be indicated in connection with single tooth
losses or small gap situations, especially in younger
individuals, in order to avoid unnecessary mutilation
of intact neighboring teeth. Furthermore, if interden-
tal diastemas are to be preserved, only implants seem
to give an acceptable solution.
However, before suggesting any implant treatment
it is important to roughly judge whether it is realistic
to perform the procedure, from both medical and
anatomic points of view. It is also necessary to check
whether the wishes /prerequisites of the patient match
the potentials of the technique offered. Any sign of
unrealistic expectation, including too cosmetically-
oriented demands, must be identified and discussed,
as otherwise problems may later arise in the patient-
doctor relationship or in the patient's appreciation of
performed treatment. Regarding the medical history,
the same principles as in connection with any type of
oral and maxillofacial surgery can be followed. The
anatomic state within the area considered for implants
can roughly be checked with regard to the available
bone volume via palpation and/or probing through
the mucosa, together with evaluation of obtained
panoramic and periapical radiographs (for X-ray
tech-
THE SURGICAL SITE •
8
53
niques, see Chapter 36). If implant treatment is re-
garded as possible, the X-rays are also used to study
the health condition of remaining teeth and edentu-
lous areas, as the need for pretreatment must be con
-
sidered. No ongoing pathology, such as denture-in-
duced stomatitis, candidosis, hyperplasia or similar
mucosal disorders, root remnants, periodontitis, pe-
riapical lesions, residual jaw infections or cysts, be-
nign or malignant tumors, etc. can be accepted at the
time of implant placement. Consequently, the entire
oral situation, and not only the edentulous area aimed
for implants, must be examined and evaluated, i.e. a
total oral rehabilitation plan should be offered to the
patient. Information on possible results and risks with
the treatment, as well as on expected costs and treat-
ment duration, must also be included, before the pa-
tient is left with the decision of whether or not to
accept the offered tentative treatment plan.
Before continuing with secondary assessments,
there should be signs of ongoing healing regarding all
pathology treated. Depending on the nature and ex-
tent of the pretreatment, the time before advancing to
the next level will vary. Mucosal lesions mostly need
a
few weeks of healing, whereas conditions involving
bone formation may take months to heal, depending
on how much bone restoration is desired. In the case
of tooth extractions, various modalities have been
advocated regarding how soon after the tooth removal
implants can be inserted. Everything from immediate
placement to delayed and/or late insertion of im-
plants has been suggested. The advantages of imme-
diate placement may be that the patient only has to
use provisional removable or fixed constructions for
a
short period, and that the postextraction resorption
of
the alveolar bone may be limited. However, various
levels of implant failures (2-7%) have been found with
the immediate implant insertion technique (Krump &
Barnett 1991, Gelb 1993, Watzek et al. 1995), which is
why delayed (5-6 weeks of healing) or even late im-
plant insertion (9-10 months of healing) seem to be
recommended in the long term. In connection with
endodontic treatment of periapical lesions, at least the
beginning of bone fill within the previous defect
should radiographically be detected before implants
are to be inserted, to prevent residual tooth infections
from migrating to and contaminating the inserted
implants during healing. If periodontal treatment is
needed, positive results from that must be recogniz-
able as well, and the patient should be deemed capable
of continuously maintaining good oral hygiene at
remaining teeth and prosthetic constructions, before
any implant surgery is started. Unfavorable plaque
control and ongoing periodontitis may otherwise ad-
versely affect the implant treatment outcome (Ber-
glund 1993, Hardt et al. 2002).
Summary: primary
judgment
The specific oral problems of the patient must first be
identified by the prosthodontist/restorative dentist,
after which different treatment alternatives can be
presented. If implant therapy is preferred, there
should be clear motivations for this, together with a
rough estimation of how realistic it would be to carry
it out. A total treatment plan must always be offered
to the patient, not just implant therapy of edentulous
areas. Unrealistic expectations of the discussed treat-
ment have to be identified and explored in order to
establish a well-functioning future patient-doctor re-
lationship. Any necessary pretreatment must be initi-
ated and signs of healing seen, before continuing to
the second examination level. Furthermore, costs and
timetables for suggested treatment should be indi-
cated before the patient is left with the decision
whether or not to accept the offered tentative treat-
ment plan.
Secondary assessment
Following the primary judgment and suggested pre-
treatment, the patient will advance to secondary as-
sessments, where the medical condition of the patient
as well as the local health and bone morphology of
future implant sites will be analyzed in more detail
from a surgical standpoint.
Medical condition
The patients must meet the physical demands for
surgery in general and have such a psychological
constitution that they can cope with proposed surgical
procedures, i.e. show
general operability.
The same
principles as in connection with any type of oral and
maxillofacial surgery may thereby be followed. So far
no specific condition has been identified which would
exclusively prevent implant surgery, should conven-
tional oral surgery be possible. In connection with this,
patient gender does not seem to have any influence on
the outcome, though theoretically women after meno-
pause are more prone to develop osteoporotic condi-
tions (Lekholm et al. 1994, Friberg et al. 1997, Sennerby
& Rasmusson 2001). Furthermore, age does not seem
to be influential for the establishment of osseointegra
-
tion, as implants become bone anchored both in young
(Thilander et al. 1994) as well as in elderly individuals
(
Kondell et al. 1988, Jemt 1993). Still, it must be remem
-
bered that elderly patients are more susceptible to
infections and/or slow healing, and therefore may
constitute potential risks for problems peroperatively
and postoperatively (Sermerby & Rasmusson 2001). It
must also be observed that implants inserted in grow
-
ing individuals may end up in infra-occlusion (Oil-
man 1994), as they will not follow the growth and
development of the jaws, but rather react like anky-
lotic teeth. Consequently, it is not the chronological
age but rather the dental and skeletal maturation that
must be considered when osseointegrated implants
are to be inserted in adolescents (Thilander et al. 1994).
Individual growth curves should be studied together
with radiographs of the growth zones of the hand
bones, to check that the body growth has ceased or is
854 • CHAPTER 37
close to completion, before any titanium implants are
inserted in adolescents in general. It is only in very
specific situations, and then due to psychosocial rea-
sons mainly, that implants may be inserted in even
younger individuals (Koch et al. 1996).
For implant surgery as well as other types of oral
operations, there are some absolute and relative con-
traindications for treatment that have to be identified.
As examples of absolute contraindications, the follow
-
ing conditions can be mentioned:
1.
Systemic diseases such as developing cancer and
Aids. Even HIV-positive patients ought not to be
considered, as there may be future complications
due to their impaired immunology defense mecha-
nisms, resulting in increased risks for infections
and impaired healing around the implants.
2.
Cardiac diseases, if not otherwise stated by a re-
sponsible medical doctor. Implant surgery should
be carefully considered in patients with heart valve
replacements and should not be performed on pa-
tients having suffered from recent infarcts, i.e.
within the latest 6-month period.
3.
Deficient hemostasis and blood dyscrasias, such
as
hemophilia, thrombocytopenia, acute leukemia
and agranulocytosis, are situations which present
risks for bleeding or may limit the healing capacity
of the tissues. If these conditions are suspected, the
patient should be checked via laboratory tests and
the responsible physician consulted.
4.
Anticoagulant medication or any medication lead-
ing to impaired hemostasia, such as ASA, may
result in extended peroperative and postoperative
bleeding as well as enlarged postoperative hema-
toma formation. If anamnestic information regard-
ing such medication is at hand, tests of coagulation
and/or primary hemostasia should be carried out
and the medication be interrupted, if implants are
to be inserted.
5.
Psychological diseases may carry potential risks as
well, as such patients often have difficulties co-op-
erating and/or lack interest in maintaining suffi-
cient oral hygiene. They may also be using medica-
tion which could interfere with the anesthesia
needed during the surgical procedure.
6.
Uncontrolled acute infections, as in the respiratory
tract, may negatively influence the surgical proce-
dure or may affect the treatment result and are thus
a contraindication for surgical treatment.
There are relative contraindications for implant sur-
gery in connection with some medical and clinical
situations as well as chronic health conditions. How-
ever, as long as conventional precautions for the treat
-
ment of these situations are fully considered during
the surgical interventions, it may still be possible to
perform implant placement.
In the case of diabetes, when there may be an in-
creased risk for infection and reduced healing, it is still
possible to perform implant surgery if the operation
is carried out under antibiotic cover, and provided that
the diabetic condition can be controlled via insulin
medication and/or via the diet (Adell 1992, Sennerby
& Rasmusson 2001). However, if unregulated diabetes
is present, implant surgery ought to be avoided.
Irradiation of the jaw may be another potential risk
factor for implant treatment, specifically if the jaw has
been exposed to irradiation over the level of 50 Gy (
Adamo & Szal 1979, Sennerby & Rasmusson 2001),
due to the risk of developing osteoradionecrosis.
However, it has been suggested that with the use of
hyperbaric oxygen treatment preceding implant ther-
apy, the failure rate can be reduced from around 60%
to about 5% (Granstrom 1992). Furthermore, reports
have indicated (Franzen et al. 1995) a lower risk for
failures if the preoperative irradiation has been less
than 40 Gy and carried out 2 years or more prior to the
implant placement. However, whenever treating irra-
diated patients, a specific follow-up protocol is
strongly recommended postoperatively, in order to
detect possible problems early.
Chemotherapy has been reported (Wolfaardt et al.
1996) to have little effect on the osseointegration of
implants if these have been inserted either before or
after the medication period. However, if the implants
are placed during the medication, or if chemotherapy
is
given in combination with irradiation, higher failure
rates have been indicated (Wolfaardt et al. 1996).
Smoking has been found to negatively affect the
long-term prognosis of osseointegration as well as the
marginal bone remodeling around implants (Bain &
Moy 1993, Lindqvist et al. 1996). Furthermore, it has
been reported that if the patient can stop smoking just
during healing, the implant survival rate may im-
prove (Bain 1996). Other abuse situations such as the
misuse of alcohol and/or drugs must be discussed
too; there are potential risks for complications in such
patients due to their higher propensity for bleeding,
infections and/or impaired healing. Co-operation is
also often lacking in affected persons, and therefore it
is recommended to refer them to a psychiatrist for
analysis to see if their misuse can be related to the
edentulous state, and if implant treatment can help
them to recover.
The cutaneous lesion lichen planus, especially the
erosive type, has in some single cases resulted in total
implant losses; the reason for this is not fully under-
stood at the present time. Changes in the capacity of
the epithelium to adhere to the titanium surface may
be the problem, as the losses seem to occur first after
some time of clinical function. However, there are also
lichen patients, mainly of the reticular type, in whom
implants have been inserted without creating any late
problems, which is why the condition cannot be re-
garded as an absolute contraindication for implant
treatment. Still, potential implant patients having the
disease should be informed that they might experi-
ence late implant failures if treated. It has to be men-
tioned, too, that conditions such as pemphigus, lupus
erythematosus, erythema multiforme, aphthous sto-
THE SURGICAL SITE •
8
55
matitis, herpes zoster and herpes labialis ought to be
handled with caution due to the lack of knowledge
regarding these disorders in combination with oral
implant placement.
Long-standing steroid medication has often been
connected with the gradual development of poor bone
quality, i.e. osteoporosis (Mori et al. 1997), which is
why the medication may also affect the establishment
and/or maintenance of implant osseointegration.
However, patients suffering from severe osteoporosis
have been treated with implants without developing
any negative results in the long term (Friberg et al.
2001, Sennerby & Rasmusson 2001). Therefore, steroid
medication/osteoporosis may not always have a de-
teriorating effect on implant treatment, at least not
when performed in edentulous jaws.
Local health and bone morphology
It is also important to examine the intraoral health
status of the soft and hard tissues as well as of the bone
morphology in future implant areas, i.e. to judge the
local operability.
This is mainly done using both clinical
and radiographic parameters.
The clinical assessments include inspection and
palpation of the edentulous areas considered for im-
plants, in order first of all to decide that no persisting
pathology is present. Via the palpation, a second esti-
mation of the available bone volume is performed,
and any defects should thereby be identified in order
to contemplate the need for augmentation procedures.
If during implant placement, minor fenestrations or
marginal dehiscences would occur, resulting in some
exposed threads, these can in general be left unat-
tended, as in follow-up studies no real adverse mu-
cosal reactions have been observed due to their pres-
ence (Lekholm et al. 1996), at least not as long as good
oral hygiene is provided for in the area. Consequently,
it does not seem necessary to perform bone augmen-
tations just because a few implant threads have be-
come exposed during implant insertion. However, if
the jaws contain defects of such a magnitude that the
implants cannot be placed in favorable positions with
-
out having major parts of their surfaces exposed, some
kind of guided bone regeneration or local bone graft-
ing procedure might be recommended (Buser et al.
1994, Deporter 2001).
Furthermore, the clinical examination must include
a judgment of the interarch and interdental spaces to
see that there is accessibility for the instruments as
well as for the future prosthetic construction. First of
all, the patient must be able to open up sufficiently to
allow access of the hand piece together with the drills.
When occluding, the minimum interarch distance
must be at least 5 mm to harbor the implant-supported
bridgework. The smallest interdental space that can
be accepted, without damaging the periodontal sup-
port of neighboring teeth, is around 7 mm, if implants
of about 4 mm in diameter are to be used. It is also
important to carefully study the jaw relation, as that
will have an influence on the implant direction (fur-
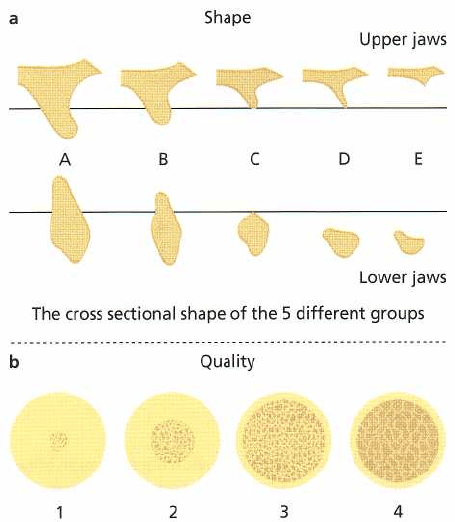
The 4 different groups of bone
quality
Fig. 37-1. Schematic drawings showing: (a) residual
jaw shape classification, and (b) jaw bone quality classi-
fication, according to Lekholm & Zarb (1985).
ther discussed below). The final step of the clinical
assessment is to take impressions for stone cast mod-
els which will later be used during the treatment
planning and for the possible manufacturing of surgi-
cal position and direction stents.
Based on the radiographic assessments performed
(
for techniques, see Chapter 36) it is possible to also
study the bone volume and the bone quality present
for implants, i.e. to elucidate the
radiographic operabil-
ity. A
grading into five groups depending on the re-
sorption rate (Fig. 37-1a) has been presented for the
residual jaw shape, together with a corresponding
grading into four groups (Fig. 37-1b) regarding the
jaw bone quality (Lekholm & Zarb 1985). Even if not
specifically adapted to the partially edentulous situ-
ation, these classifications may still be roughly ap-
plied also there. The base for the radiographic exami-
nations is mainly the panoramics and the intraoral
apical images from which, besides the shape and qual-
ity parameters, important anatomic landmarks sur-
rounding the edentulous area designated for implants
can be identified. Such structures are, for example, the
floor of sinusal and nasal cavities, incisive nerve, infe-
rior alveolar nerve, roots and apices of neighboring
teeth, and top of the alveolar crest. From the two-di-
mensional pictures it is also possible to get informa-
tion about the height available for implants, but three-
dimensional X-rays, tomographs mainly, are neces-
sary to study the bone volume. Consequently, no final
judgment of the operability can in critical situations
be based on just intraoral radiographs and orthopan-
tomograms, especially not if it is of crucial
importance
856 • CHAPTER 37
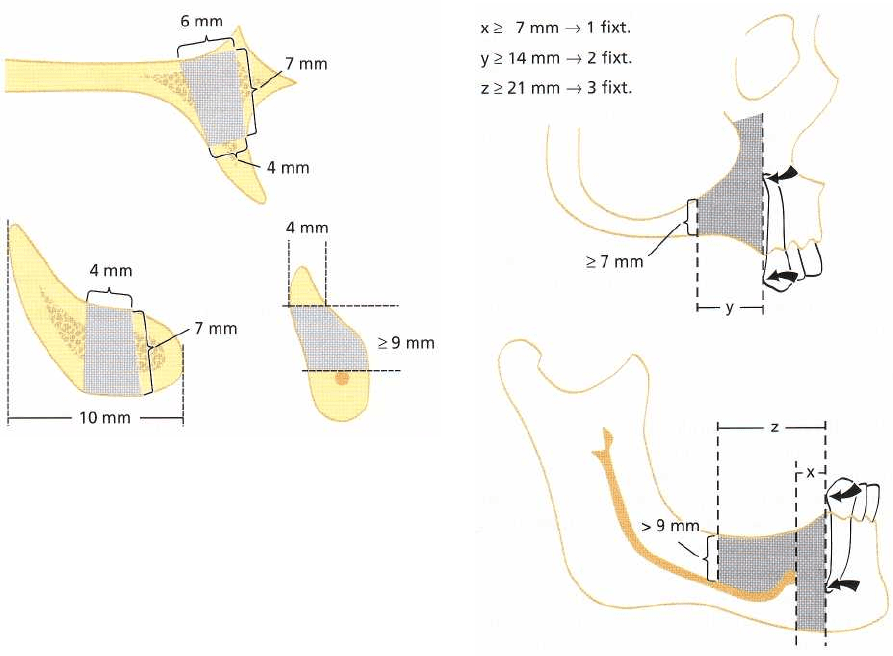
Fig. 37-2. Schematic drawings showing minimum bone
volume needed for standard implants of the Brane-
mark System.
to decide the bone volume present for implants. The
location of the inferior alveolar nerve must, for exam-
ple, be studied via tomography in order to avoid
inserting the implants in such a way that the sensation
of the lower lip and neighboring soft tissues is im-
paired. Tomography may also be used when the clini-
cal palpation has indicated that small bone volumes
are present in other areas, e.g. in the lateral or posterior
regions of the maxilla.
The minimum bone volume needed for a standard
Branemark implant (7 mm long and 3.75 mm in di-
ameter) is where the bone height is 7-9 mm and the
buccal-lingual width amounts to at least 4 mm (Fig.
37-2). When working above the inferior alveolar
nerve, a minimum height of 9-10 mm is needed for a
7 mm long implant. If less height is present, no stan-
dard implant can be placed without damaging the
nerve, as the drills extend about 2 mm deeper than the
length of the implant. Heights of 7-9 mm may only be
accepted if working in between the mental foraminae
or when working in the maxillae, where it is possible
to perforate the second cortex without damaging any
important structures.
From the obtained radiographs, it is possible to
discuss tentative locations of the implants as well as
the number and type of implants needed. This can be
done first after having identified where the minimum
bone volume is located in a distal direction (Fig. 37-3),
keeping in mind that each implant needs a gap dis-
tance of about 7 mm. However, no definite decision
regarding the number and type of implants that may
be used should be made preoperatively, but instead
should be made during stage one surgery and after
the implant sites have been finalized (see below).
Following the second assessments, the patient is
again informed about the clinical procedures, possible
risks, costs involved, treatment timing, etc., in order
Fig. 37-3. Schematic drawings indicating location of
minimum bone volume areas in distal directions, and
giving distances needed for various numbers of im-
plants. Arrows indicate prominence and apex of the
nearest tooth.
to make the final decision whether or not to go on with
the implant therapy suggested.
Summary: second assessment
The second level of clinical and radiographic exami-
nations is performed in order to evaluate the operabil-
ity of the patient from medical and anatomic stand-
points. No specific medical condition has so far been
detected that specifically excludes implant surgery.
Consequently, the same absolute and relative contra-
indications for treatment are present when inserting
implants as when performing other types of oral and
maxillofacial surgery. It is recommended when treat-
ing patients at risk that trained specialists work in
collaboration with the physicians responsible for the
treatment of such conditions when performing the
handling. The local health of edentulous areas consid-
ered for implants must be studied too, and no pathol-
ogy in the soft and hard tissues of the jaws can be
accepted at the time of implant placement. Radio-
graphic evaluations are necessary in order to identify
important landmarks, constituting the limits for the
operation, as well as the jaw shape and bone quality
in
areas considered for implants. Tomography is spe-
cifically needed when working in relation to the infe-
rior alveolar nerve, and when the clinical examination
