Jan Lindhe. Clinical Periodontology
Подождите немного. Документ загружается.

ORTHODONTICS AND PERIODONTICS • 755
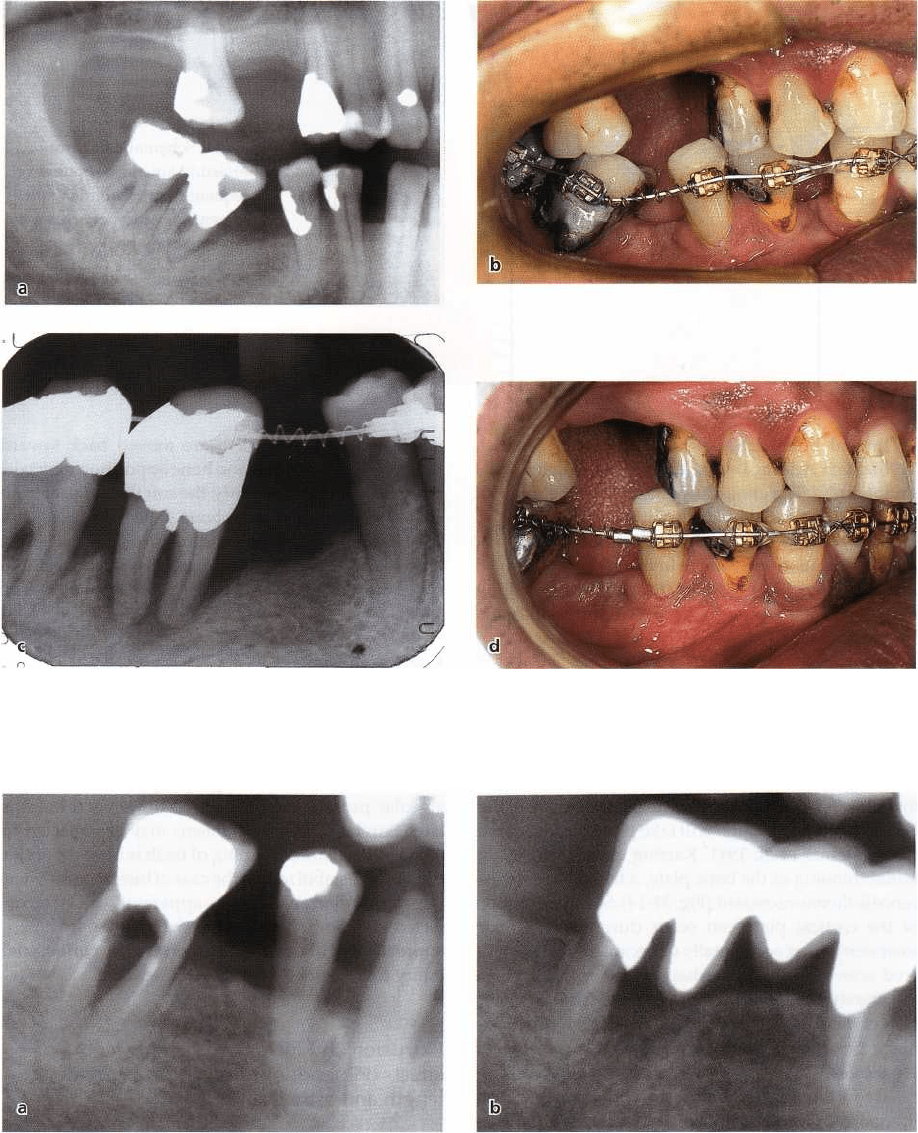
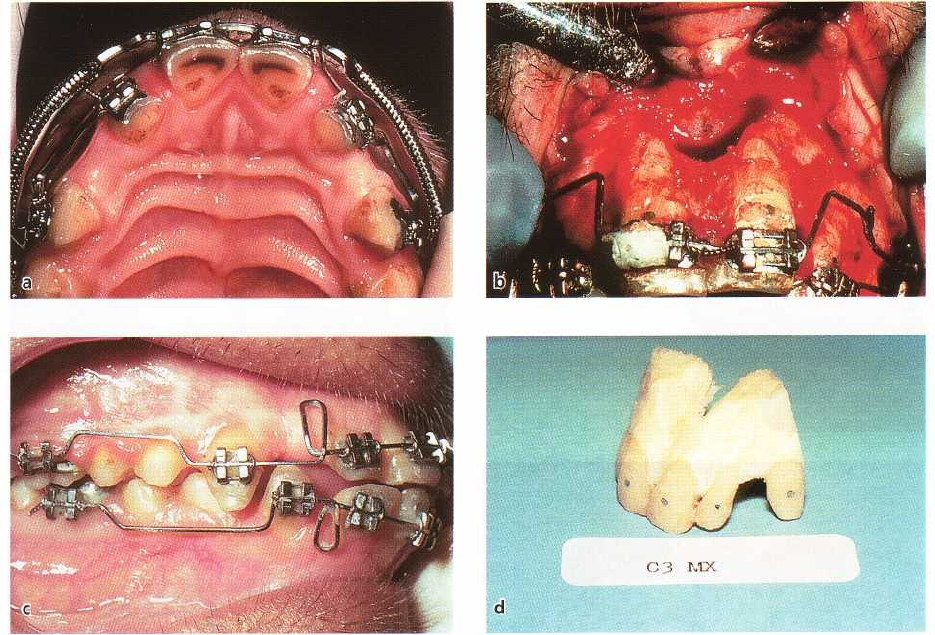
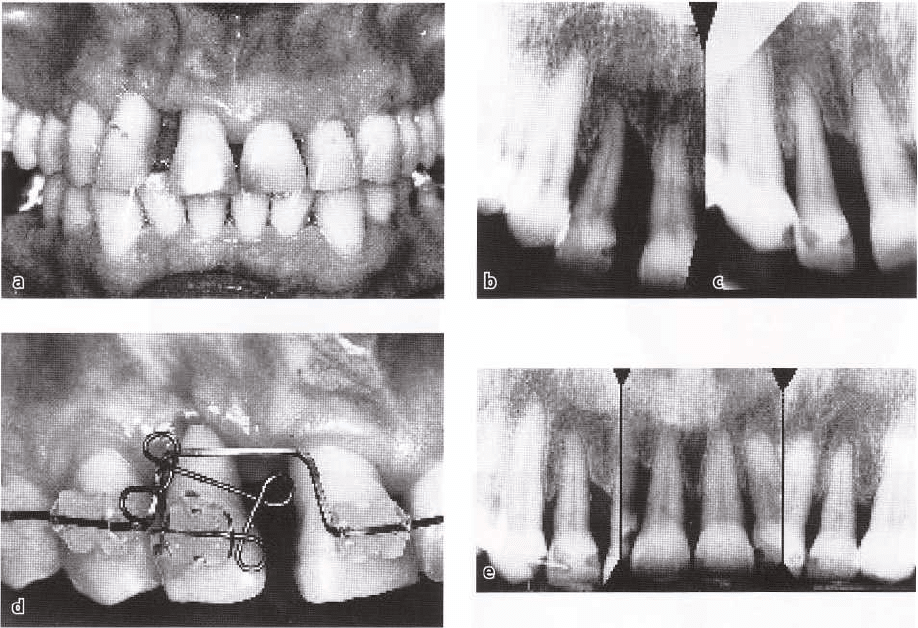
Fig. 31-9. "Hopeless" mandibular right first molar (a) can be used as part of anchorage to move the premolars
mesially and upright the second molar (b-d). The first molar may be kept, or extracted, after the orthodontic treat
ment period.
Fig. 31-10. "Hopeless" mandibular right first molar (a) was used as anchorage during orthodontic treatment to
close spaces anteriorly, before it was hemisectioned and the distal root employed as a bridge abutment (b).
Histologic observations in animal experiments have
confirmed that when light forces were applied to
move
teeth bodily into an area with reduced bone
height, a
thin bone plate was recreated ahead of the
moving
tooth (Fig. 31-13) (Lindskog-Stokland et al.
1993). The
key to moving teeth with bone is direct
resorption in
the direction of tooth movement, and
avoiding
hyalinization. Teeth can be moved with bone
into the
maxillary sinus also (Melsen 1991).
Conclusion
Although the results of clinical experiments and fol-
low-ups are encouraging, provided light forces are
used and excellent oral hygiene is maintained, it is
probably wise not to stretch the indications for tooth
movement into constricted bone areas too far. Marked
gingival invaginations are sometimes seen in such
areas (Fig. 31-12), and computer tomography analysis
and human histological findings indicate that buccal
756 • CHAPTER 31
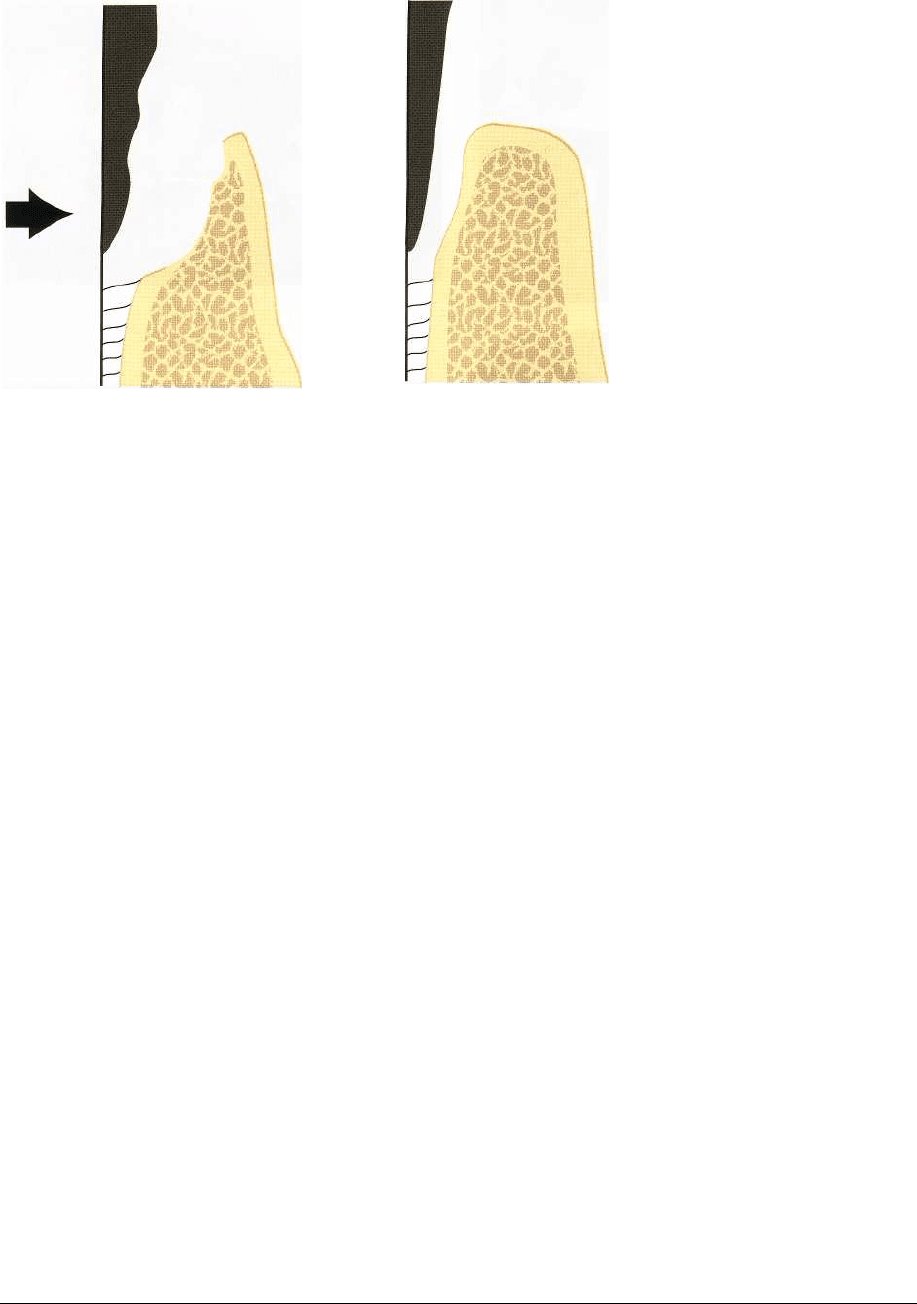
Fig. 31-11. Schematic illustration
of persisting junctional epithelium
subsequent to orthodontic tooth
movement (direction of arrow)
into an infrabony pocket.
or lingual bone dehiscences may occur (Diedrich
1996). Such defects are not revealed by conventional
radiography. The clinical significance of the gingival
clefts and bone dehiscences with regard to relapse
tendency and periodontal status is not known. For
orthodontic tooth movement into markedly atrophied
alveolar ridges, the possibility to acquire new bone by,
for example, GBR procedures (see Chapter 38) should
be considered.
Tooth movement through cortical bone
Experimental studies in animals have demonstrated
that when a tooth is moved bodily in a labial direction
towards and through the cortical plate of the alveolar
bone, no bone formation will take place in front of the
tooth (Steiner et al. 1981, Karring et al. 1982). After
initial thinning of the bone plate, a labial bone dehis-
cence is therefore created (Fig. 31-14). Such perforation
of the cortical plate can occur during orthodontic
treatment either accidentally or because it was consid
-
ered unavoidable. It may happen for example (1) in
the mandibular anterior region due to frontal expan-
sion of incisors (Wehrbein et al. 1994), (2) in the max-
illary posterior region during lateral expansion of
cross-bites (Greenbaum & Zachrisson 1982), (3) lin-
gually in the maxilla associated with retraction and
lingual root torque of maxillary incisors in patients
with large overjets (Ten Hoeve & Mulie 1976), and (4)
by pronounced traumatic jiggling of teeth (Nyman et
al. 1982).The soft tissue reactions accompanying such
tooth movements are discussed later in this chapter
and in Chapter 30.
Interestingly, however, there is potential for repair
when malpositioned teeth are moved back toward
their original positions, and bone apposition may take
place (Fig. 31-14). Evidently, the soft tissue facial to an
orthodontically produced bone dehiscence may con-
tain soft tissue components (vital osteogenic cells)
with a capacity for forming bone following reposition-
ing of the tooth into the alveolar process (Nyman et al.
1982).
Conclusion
The clinical implication of these observations is en-
couraging. Bone dehiscences which may occur due to
uncontrolled expansion of teeth through the cortical
plate may be repaired when the teeth are brought
back, or relapse, towards a proper position within the
alveolar process, even if this occurs several months
later. Similar repair mechanisms may be expected to
occur when marked jiggling of teeth is brought under
control and stabilized. In the case of buccal cross-bites,
the initial discrepancy can apparently be overcor-
rected with both slow and rapid expansion treatment
approaches without causing permanent periodontal
injury to the settled occlusion.
Extrusion and intrusion of single teeth -
effects on periodontium, clinical crown
length and esthetics
Extrusion
Orthodontic extrusion of teeth, or so-called "forced
eruption", may be indicated for (1) shallowing out
intraosseous defects and (2) for increasing clinical
crown length of single teeth. The forced eruption tech
-
nique was originally described by Ingber (1974) for
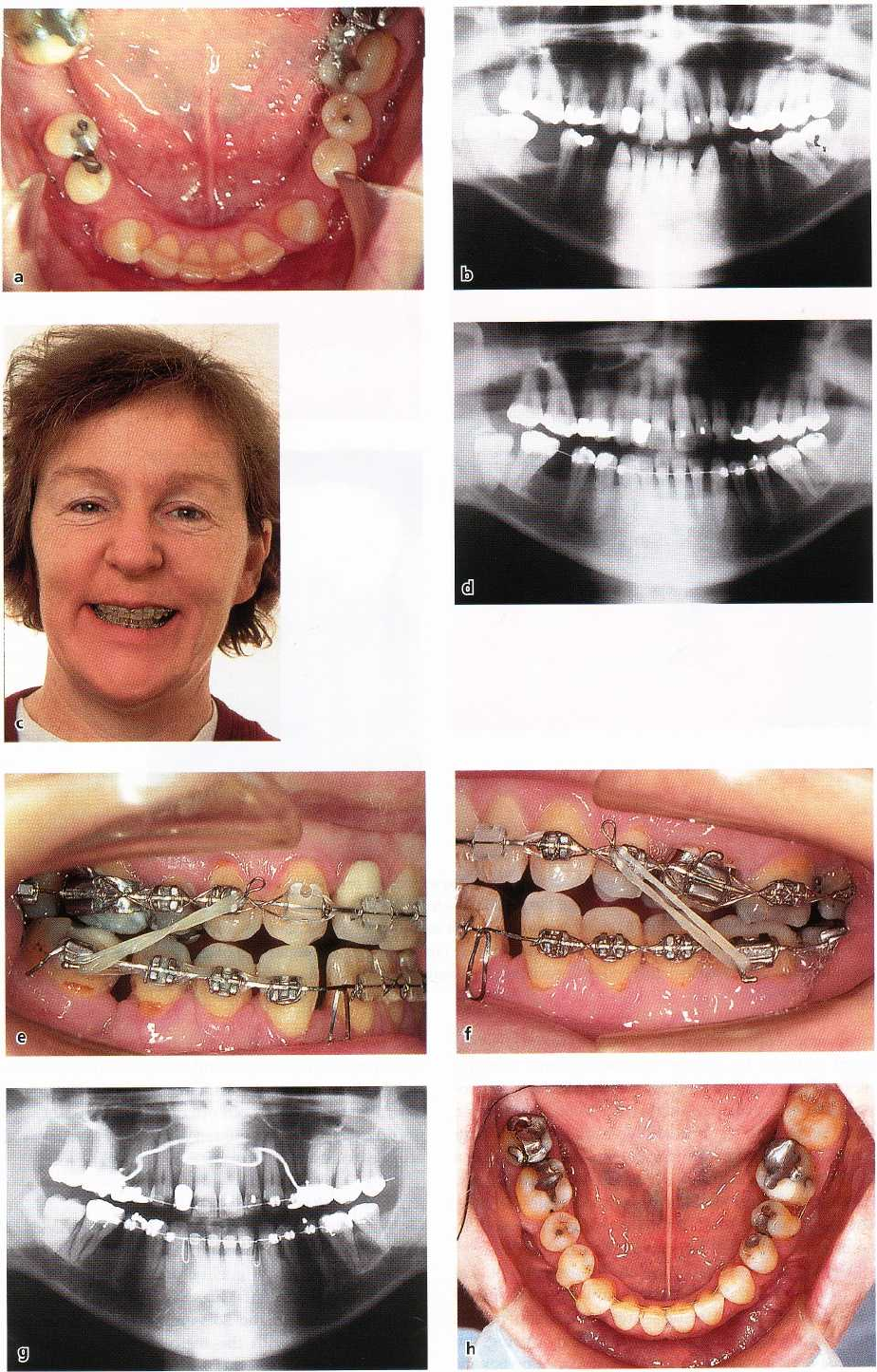
Fig. 31-12. Orthodontic tooth movements into edentulous areas with reduced bone height in compromised mandi
-
ble of adult female patient. During the orthodontic treatment (c-g), the teeth were moved to close three areas of
marked alveolar bone constriction (a,b), most notably in the right first molar area. Note that the impacted third mo
-
lar erupted spontaneously as the second molar was moved mesially (g). (h) shows final result with bonded six-unit
lingual and two-unit labial retainers.
ORTHODONTICS AND PERIODONTICS • 757
758 •
CHAPTER
31
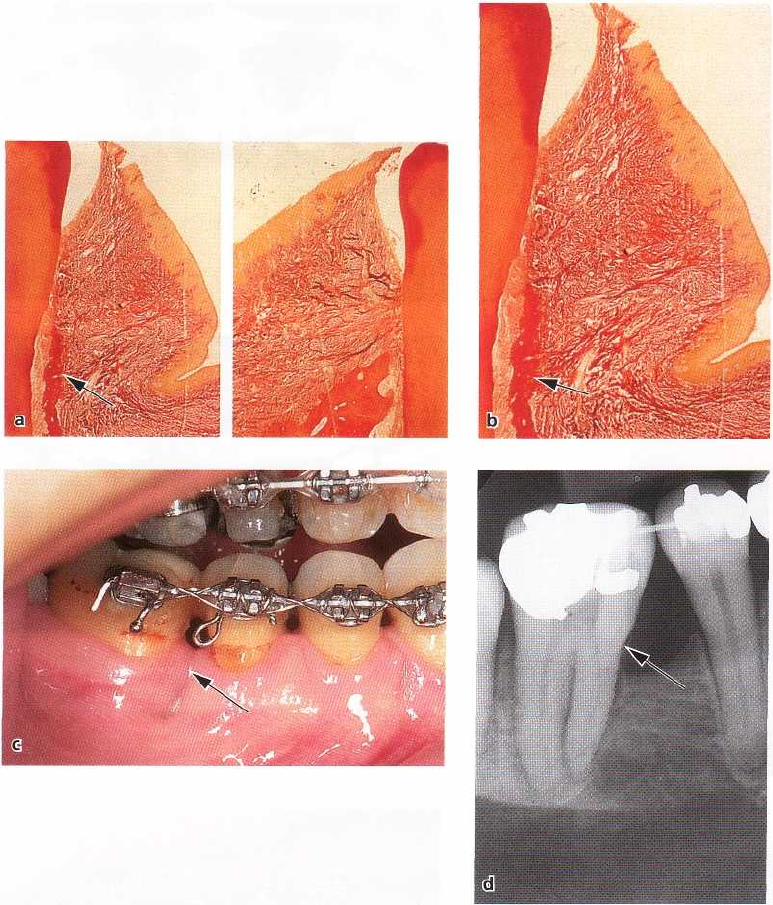
Fig.
31-13.
(a) and (b) show histologic specimens from experimental orthodontic tooth movement into edentulous
areas in dogs. The thin bone spicule along the pressure side of the test tooth (b) indicates tooth movement with,
and not through, bone. (c) and (d) show the same patient as in Fig.
31-12.
Note radiographic visualization of the
thin bone spicule on the mesial side of the second molar (arrow in d). Although the molar is moved to contact the
second premolar, a marked gingival invagination is present in the area (arrow in c). (a) and (b) from Lindskog-Stok
land et al.
(1993).
treatment of one-wall and two-wall bony pockets that
were difficult to handle by conventional therapy
alone. The extrusive tooth movement leads to a coro-
nal positioning of intact connective tissue attachment,
and the bony defect is shallowed out. This was con-
firmed in animal experiments (van Venroy & Yukna
1985)
and clinical trials. Because of the orthodontic
extrusion, the tooth will be in supraocclusion. Hence,
the crown of the tooth will need to be shortened, in
some cases followed by endodontic treatment.
During the elimination of an intraosseous pocket
by means of orthodontic extrusion, the relationship
between the CEJ and the bone crest is maintained. This
means that the bone follows the tooth during the
extrusive movement. This may or may not be benefi-
cial depending on the clinical situation. In other
words, it is sometimes desirable to have the periodon
-
tium follow the tooth and in other situations it is
desirable to move a tooth out of the periodontal sup-
port. This is further discussed under slow versus rapid
eruption of teeth in Chapter 30.
Extrusion with periodontium
Orthodontic extrusion of a single tooth that needs to
be extracted is an excellent method for improvement
of the marginal bone level before the surgical place-
ment of single implants (Figs. 31-15, 31-21). Not only
the bone, but also the soft supporting tissues will
move vertically with the teeth during orthodontic
extrusion. Using tattoo marks in monkeys to indicate
ORTHODONTICS AND PERIODONTICS • 759
Fig. 31-14. Techniques used by Steiner et al. (1981) to bodily advance incisors through the labial bone plate in mon
keys (a,b) and by Engelking & Zachrisson (1982) to retract the incisors to their original position (after the teeth
had remained in extreme labioversion for 8 months) in a study of periodontal regeneration to such tooth movement.
Tis-sue blocks after tooth repositioning (d) show evident bone regeneration.
the mucogingival junction and clinical sulcus bottom,
Kajiyama et al. (1993) made a metric evaluation of the
gingival movement associated with vertical extrusion
of incisors. The results indicated that the free gingiva
moved about 90% and the attached gingiva about 80%
of the extruded distance. The width of the attached
gingiva and the clinical crown length increased sig-
nificantly, whereas the position of the mucogingival
junction was unchanged. Orthodontic extrusion of a "
hopeless" incisor is therefore a useful method also for
esthetic improvement of the marginal gingival level
associated with the placement of implants (Fig. 31-
15).
Extrusion out of periodontium
In teeth with crown-root fracture, or other subgingival
fractures, the goal of treatment may be to extrude the
root out of the periodontium (Fig. 31-16), and then
provide it with an artificial crown. When an increased
distance between the CEJ and the alveolar bone crest
is aimed at, the forced eruption should be combined
with gingival fiberotomy (Pontoriero et al. 1987, Ko-
zlowsky et al. 1988). Berglundh et al. (1991) showed in
animal experiments that when the fiberotomy (i.e.
excision of the coronal portion of the fiber attachment
around the tooth) was performed frequently (every 2
weeks), the tooth was virtually moved out of the bony
periodontium, without affecting the bone heights or
level of the marginal gingiva of the neighboring teeth.
This procedure is illustrated in Fig. 31-16.
Intrusion
Similar to the indications for extrusion, the orthodon-
tic intrusion of teeth has been recommended (1) for
teeth with horizontal bone loss or infrabony pockets,
and (2) for increasing the clinical crown length of
single teeth. However, the benefits of intrusion for
improvement of the periodontal condition around
teeth are controversial.
As mentioned, the intrusion of plaque-infected
teeth may lead to the formation of angular bony de-
fects and increased loss of attachment. When oral
hygiene is inadequate, tipping and intrusion of the
teeth may shift supragingivally located plaque into a
subgingival position, resulting in periodontal de-
struction (Ericsson et al. 1977, 1978). This explains
why professional subgingival scaling is particularly
important during the phase of active intrusion of elon-
gated, tipped and migrated maxillary incisors com-
monly occurring in association with advanced peri-
odontal disease. Even in a healthy periodontal envi-
ronment the question remains as to whether the ortho-
dontic tooth movement intrudes a long epithelial at-
tachment beneath the margin of the alveolar bone or
whether the alveolar crest is continously resorbed in
front of the intruding tooth.
760 • CHAPTER 31
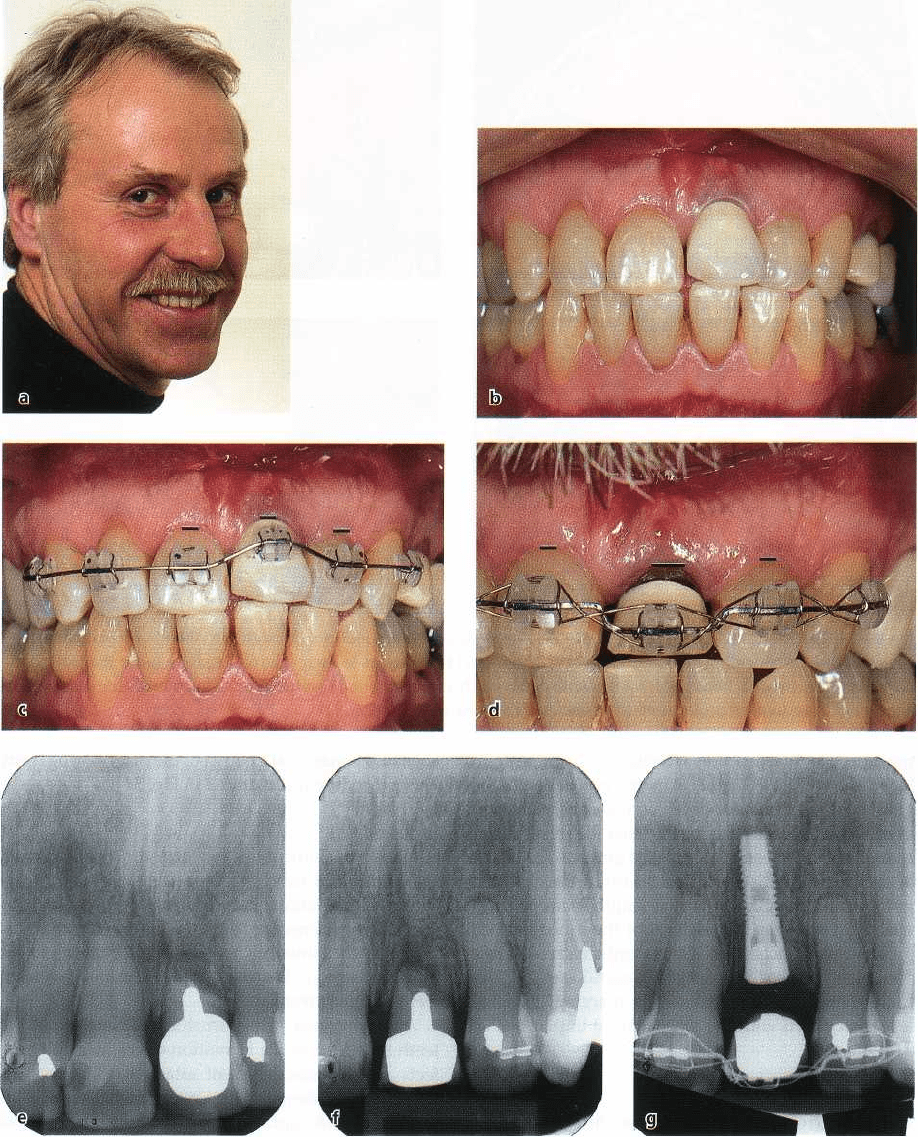
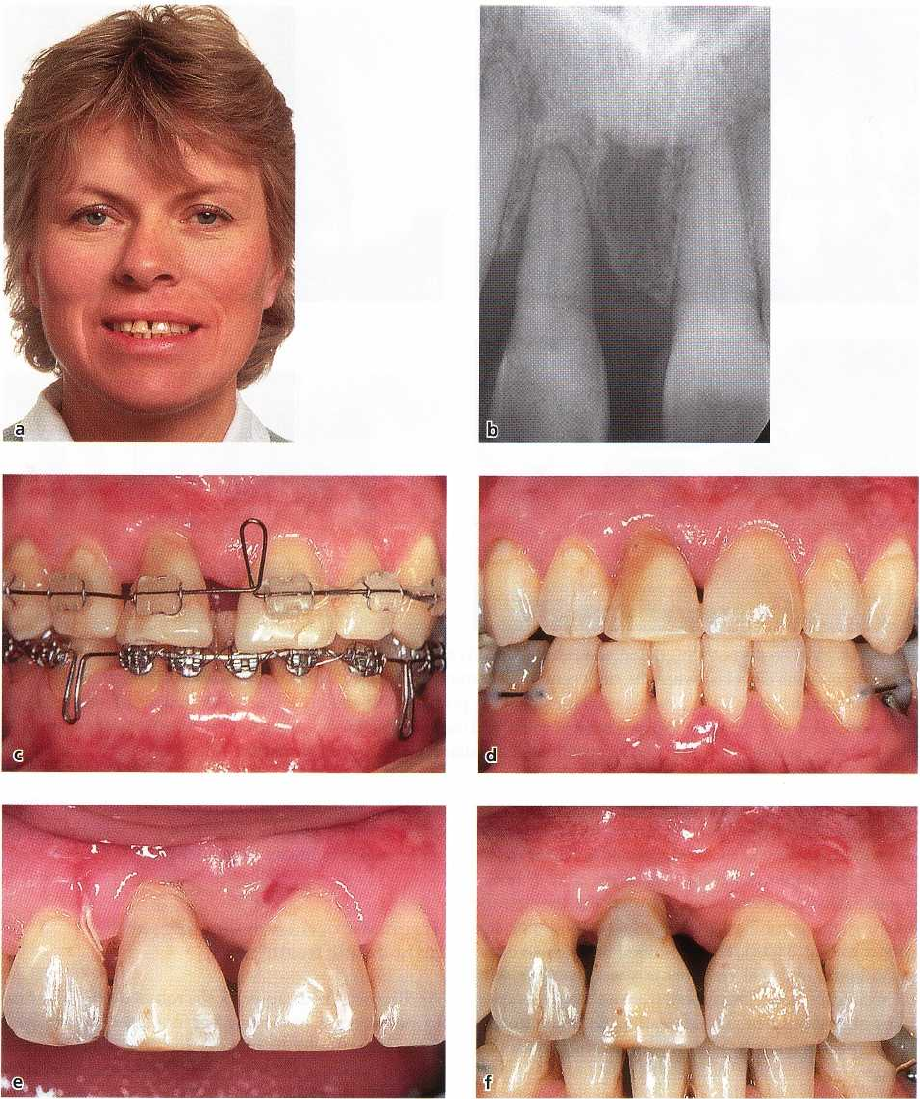
Fig. 31-15. Extrusion with periodontium. Selective extrusion of maxillary left central incisor to improve periodontal
soft and hard tissues before placement of single implant. As shown in (b) to (d), it is necessary to extensively grind
the extruding incisor crown to avoid jiggling with the mandibular teeth. Note evident differences in marginal gingi
-
val levels (lines) on the left central incisor during its extrusion (b-d). (e) to (g) show radiographic appearance at
start, after 4 months and after 10 months, respectively.
Histologic (Melsen 1986, Melsen et al. 1988) and the axis of the incisors with light forces was initiated
clinical
(Melsen et al. 1989) studies indicate that new following flap surgery. Histologic analysis showed
attachment is
possible associated with orthodontic new cementum formation and connective tissue at-intrusion of teeth. In
monkey experiments, periodon- tachment on the intruded teeth, by an average of 1.5 tal tissue breakdown was
induced and intrusion along mm, provided a healthy gingival environment was
ORTHODONTICS AND PERIODONTICS • 761
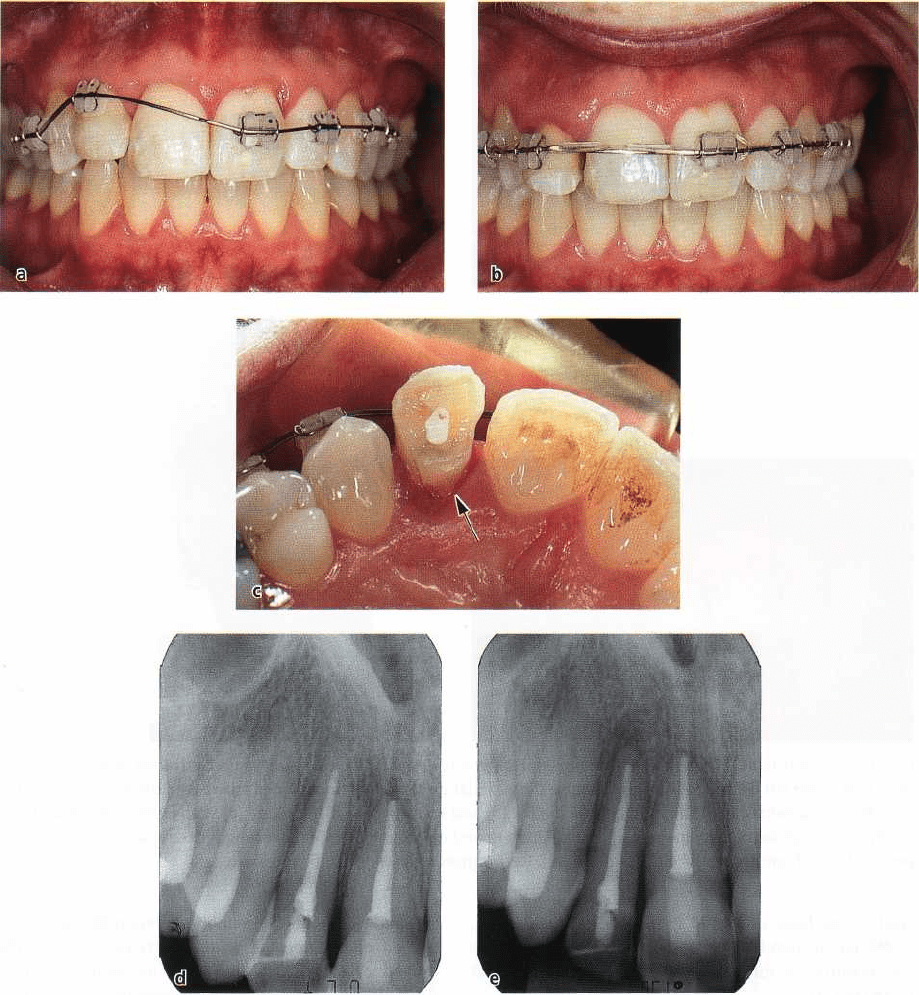
Fig. 31-16. Extrusion out of periodontium. Due to subgingival crown-root fracture on the maxillary right lateral in
cisor (a,d), this tooth was extruded out of the periodontium with a continous force (a-b) and fiberotomy was made
with two-week intervals. The amount of extrusion is evident by comparison of the relationship between lateral and
central incisor root ends in (d) and (e). Having moved the fracture line to a supragingival position (arrow in c), the
tooth can now be safely restored.
maintained throughout the tooth movement. The in-
creased activity of periodontal ligament cells and the
approximation of formative cells to the tooth surface
was suggested to contribute to the new attachment. In
the clinical study, the periodontal condition was
evaluated following the intrusion of extruded and
spaced incisors in patients who had advanced peri-
odontal disease. Judging from clinical probing depths
and radiography, there was despite a large individual
variation a beneficial effect on clinical crown lengths
and marginal bone levels in many cases.
However, the reported clinical and histologic find-
ings associated with a combined orthodontic-peri-
odontal approach must be assessed with great cau-
tion, and these findings have not been confirmed by
others. Furthermore, new techniques like the GTR and
other regenerative procedures (see below) would ap-
pear to be more promising when it comes to creation
of new attachment.
Similar to the case with extrusion, metric and his-
tologic studies have been made after experimental
intrusion of teeth in monkeys. According to Murakaini
et al. (1989), the gingiva moved only about 60%
of the
distance when the teeth were intruded with a
762 • CHAPTER 31
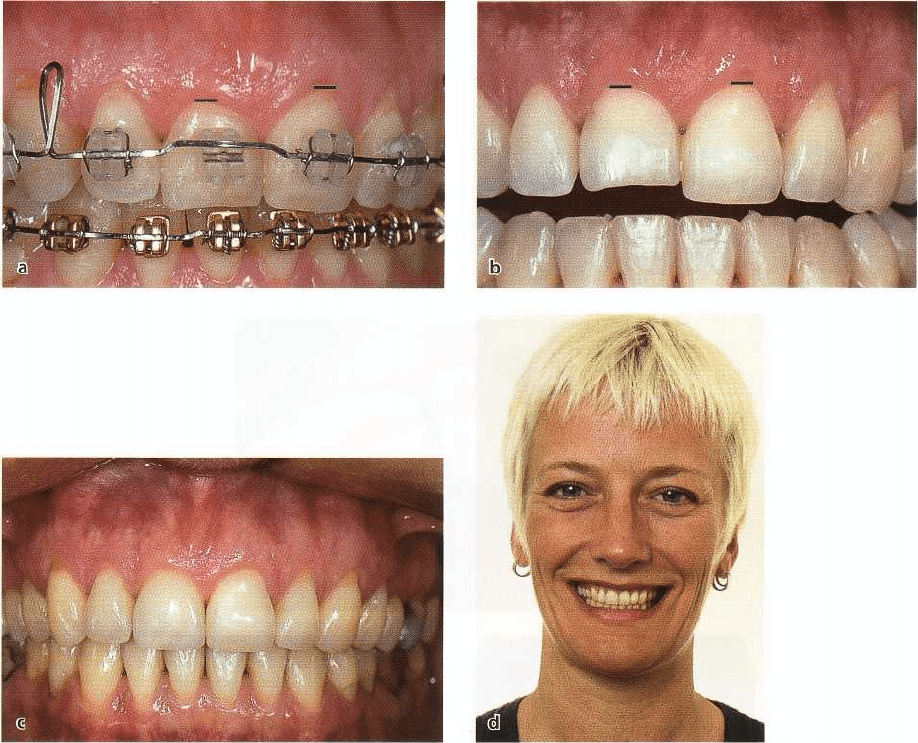
Fig. 31-17. Adult female patient in whom the clinical crown length of the maxillary right central incisor was shorter
than that of the left central incisor (a). Because the sulcular depths were normal, the crown lengths were corrected
by orthodontic intrusion of the right central incisor (b) and restoring the incisal edge (b) with enamel-bonded ul
-
trathin porcelain laminate veneer (c,d). The alignment and correction of the crown length discrepancy has im
-
proved the esthetic appearance of the dentition. Restoration courtesy of Dr S. Toreskog.
continuous force of 80-100 g. However, Kokich et al.
(
1984) recommended an interrupted, continuous force
for levelling of gingival margins on supra-erupted
teeth (Fig. 31-17).
The key to understanding why intrusion can be
used to increase clinical crown length is related to the
subsequent restorative treatment. When orthodontic
intrusion is used for levelling of the gingival margins
to desired heights, such teeth must then be provided
with porcelain laminate veneers or crowns (Fig. 31-
17).
Regenerative procedures and orthodontic
tooth movement
The development of barrier membranes to prevent
cells of the epithelium and gingival connective tissue
from colonizing the decontaminated root surface, as
well as the use of Emdogain, would appear to provide
a
distinct improvement in orthodontic therapy in the
periodontally compromised patient. New supracre-
stal and periodontal ligament collagen fibers may be
gained on the tension side, which can transfer the
orthodontic force stimulus to the alveolar bone (Die-
drich 1996). In theory, the regenerative techniques
would be advantageous associated with both extru-
sion and intrusion of teeth with infrabony defects, and
for uprighting of tipped molars with mesial angular
lesions. Moreover, if the epithelium can be prevented
from proliferating apically, a bodily tooth movement
into or through an intraosseous defect could eliminate
the bony pocket more effectively than in the past (Fig.
31-11).
So far, however, relatively little clinical information
is
available about the use of different regenerative
procedures in connection with orthodontic treatment.
Diedrich (1996) reported an experiment in dogs in
which orthodontic intrusion with flap surgery and
GTR were compared with flap surgery only on perio-
dontally affected teeth. In the presence of minimal or
no round cell infiltration, the marking notch was lo-
cated beneath the alveolar margin indicating that new
attachment had formed. The potential of the intru-
ORTHODONTICS AND PERIODONTICS •
7
6
3
Fig. 31-18. Pathologic tooth migration as a result of an advanced periodontal lesion in adult female patient (a).
Se
vere intraosseous defect between the right central and lateral incisors (b). Three months after GTR
treatment
(GoreTex membrane) partial reossification is evident (c), possibly with new attachment. Orthodontic
leveling (d)
with controlled space closure and intrusion of the lateral incisor. Result 6 months after orthodontic
tooth move
ments shows no root resorption and a consolidated alveolar crest (e). From Diedrich (1996).
sive/regenerative mechanism was most impressive
within the interradicular area. Some clinical observa-
tions (Nemcovsky et al. 1996, Stelzel & Flores-de-Ja-
coby 1998, Rabie et al. 2001) confirm that different
regenerative procedures may enrich the therapeutic
spectrum in combined periodontal/orthodontic ap-
proaches (Fig. 31-18). The combined regenerative and
periodontal surgical treatments used together with
orthodontic tooth movements create new perspec-
tives and should be an interesting field for further
experiments on adults with severe loss of periodontal
tissues.
However, other clinical trials have demonstrated
that treatment results with barrier membranes in the
GTR technique may vary between different patients
and that the method is operator and technique-sensi-
tive (Leknes 1995). The patient's oral hygiene during
the healing phase is critical, and inflammation around
the membrane, particularly if it becomes exposed and
contaminated, may lead to discouraging clinical re-
sults with marked gingival retraction (Fig. 31-19).
Since the membrane is covered in the GBR tech-
nique, the risk for inflammation is reduced. The pos-
sibility for orthodontic movement of teeth into alveo-
lar processes with deficient bone volume may thus be
improved (Basdra et al. 1995). Preorthodontic GBR of
markedly constricted alveolar ridges also has the ad-
vantage that tooth movement through cancellous
bone is easier, and the formation of interfering gingi-
val invaginations can be reduced.
Traumatic occlusion (jiggling) and
orthodontic treatment
As discussed in Chapter 15, the role of occlusal trauma
in periodontal treatment has not been determined.
From an orthodontic perspective, it is of interest that
several studies indicate that traumatic occlusion
forces (1) do not produce gingival inflammation or
loss
of attachment in teeth with healthy periodontium,
(2)
do not aggravate and cause spread of gingivitis or
cause loss of attachment in teeth with established
gingivitis, (3) may aggravate an active periodontitis
lesion, i.e. be a co-destructive factor in an ongoing
process of periodontal tissue breakdown (in one way
or another favor the apical proliferation of plaque-in-
duced destruction), and (4) may lead to less gain of
attachment after periodontal treatment – non-surgical
or surgical.
A major problem in this regard is the lack of establ
-
ished and reliable criteria to identify and quantitate
different degrees of traumatic occlusion. Various clini
-
cal and radiographic indications, such as unfavorable
764 • CHAPTER
31
Fig. 31-19. Adult female periodontitis patient with marked vertical bone loss around the maxillary right central inci
sor before (a,b), during (c) and after (d) orthodontic treatment. Attempt to improve the periodontal situation by
means of GTR treatment failed. Due to infection around the GoreTex membrane (e) marked gingival retraction oc
-
curred (f).
crown/root ratio, increased tooth mobility, widened
periodontal ligament space, angular bone loss, altera-
tions in root morphology, etc. are uncertain and insuf-
ficient in diagnosis of occlusal trauma, and there have
been few scientific clinical reports to evaluate these
signs (Jin & Cao 1992).
The extent to which it is necessary to avoid, or
reduce, occlusal trauma during orthodontic treatment
is controversial and unsupported by scientific evi-
dence. Some orthodontists use bite-planes in virtually
every periodontal case with bone deformities, to re-
duce occlusal trauma and for the purpose of shallow-
ing the bony defects, as teeth supra-erupt. However,
independent studies have shown that surgical pocket
elimination including bone sculpturing offers no ad-
vantage compared with more conservative periodon
tal
treatment (Ramfjord 1984), and apparently there is
little
need to shallow or eliminate bony deformities. It
