Jan Lindhe. Clinical Periodontology
Подождите немного. Документ загружается.

SUPPORTIVE PERIODONTAL THERAPY (SPT) • 7
8
5
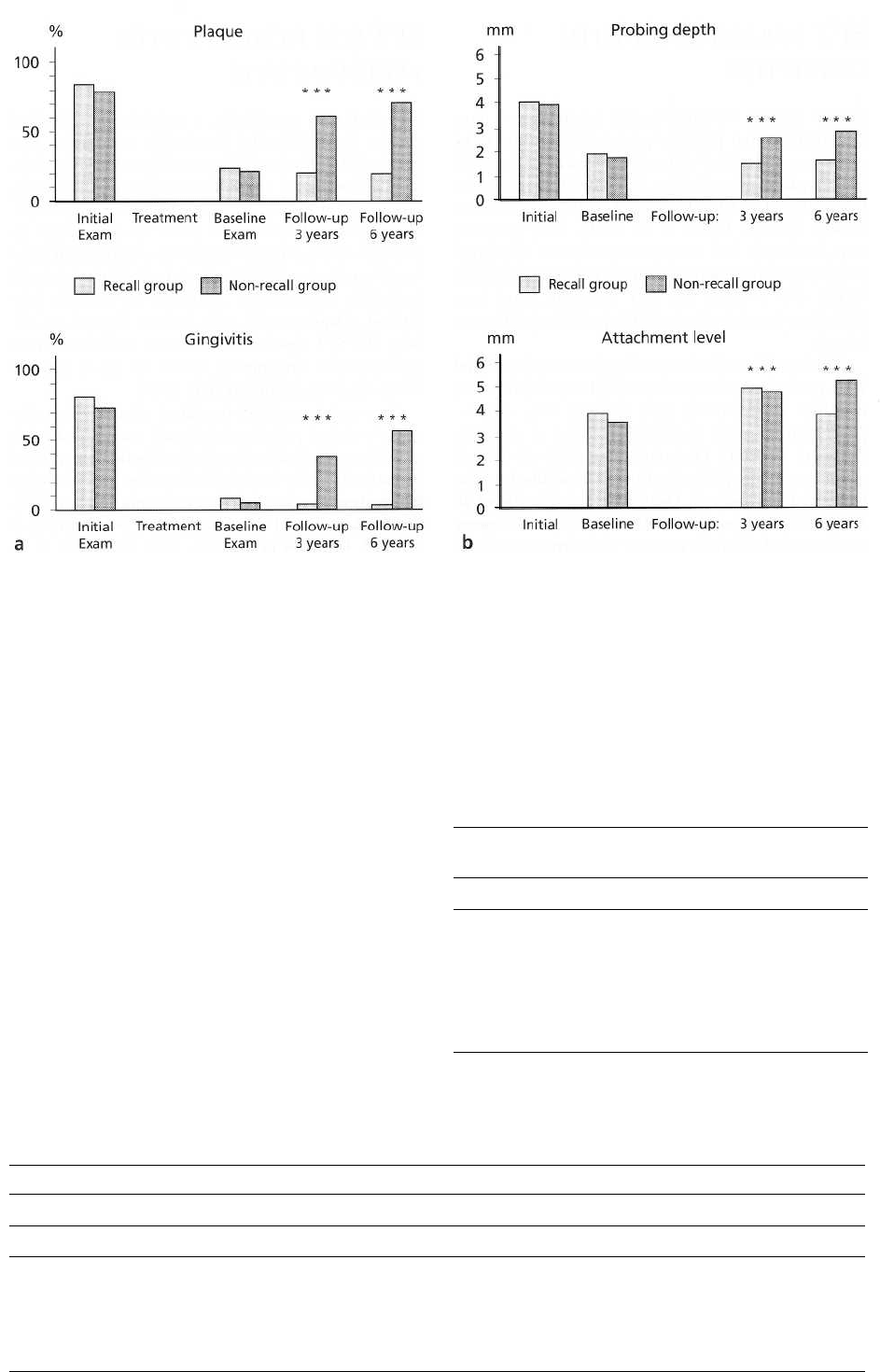
Fig. 32-2. Histograms showing (a) average percentages of tooth surfaces harboring visible plaque (above) and in-
flamed gingival units (bleeding on probing) (below), and (b) average probing depth (above) and probing attach-
ment levels (below), at initial, baseline and follow-up examinations. (Data from Axelsson & Lindhe 1981b.)
recall group (Table 32-1). In the latter patients, 55% of
the sites showed a 2-5 mm further loss of attachment
at the 6-year examination, and 20% of the pockets were
4 mm deep or more (Tables 32-1 & 32-2).
Summary
Patients susceptible to periodontal disease are at high
risk for reinfection and progression of periodontal
lesions without meticulously organized and per-
formed
SPT. Since all patients who were treated for
periodontal
diseases belong to this risk category by
virtue of their
past history, an adequate maintenance
care program is
of utmost importance for a beneficial
long-term
treatment outcome. SPT has to be aimed at the regular
removal of the subingival microbiota and
must be
supplemented by the patient's efforts for
optimal
supragingival plaque control.
Table 32-1. Percentage of sites showing various
changes in probing attachment level between base-line
examination, 2 months after completion of ac
tive
periodontal therapy and follow-up examination
6 years
later. (Adapted from Axelsson & Lindhe
1981h)
Change in attachment level
Percentage of surfaces
showing change
Recall
Non-recall
Attachment level improved
17
1
No change
Attachment level worse by
72 10
1 mm
10 34
2to5mm
1
55
Table 32-2. Percentage of various probing depths in recall and non-recall patients at the initial examination, 2
months after active periodontal treatment and at 3 and 6-year follow-up visits. (Adapted from Axelsson &
Lindhe 1981b)
Examinations
Percentage of pockets of various depths
3 mm
4-6mm
7 mm
Recall
Non-recall
Recall
Non-recall
Recall
Non-recall
Initial
35 50
58 38
8
12
Baseline
99
99
1 0 0
3 years
99
91
9 0 0
6 years
99 80 19
0
1
786 • CHAPTER 32
SPT
FOR PATIENTS WITH
GINGIVITIS
Several studies – predominantly in children – have
documented that periodic professional prophylactic
visits in conjunction with reinforcement of personal
oral hygiene are effective in controlling gingivitis
(
Badersten et al. 1975, Poulsen et al. 1976, Axelsson &
Lindhe 1981a,b, Bellini et al. 1981). This, however,
does not imply that maintenance visits in childhood
preclude the development of more severe disease later
in life. It is obvious that SPT, therefore, must be a
lifelong commitment of both the patient and the pro-
fession.
Adults whose effective oral hygiene was combined
with periodic professional prophylaxes clearly were
healthier periodontally than patients who did not
participate in such programs (Lovdal et al. 1961,
Suomi et al. 1971). One particular study of historic
significance was performed on 1428 adults from an
industrial company in Oslo, Norway (Lovdal et al.
1961). Over a 5-year observation period, the subjects
were recalled 2-4 times per year for instruction in oral
hygiene and supragingival and subgingival scaling.
Gingival conditions improved by approximately 60%
and tooth loss was reduced by about 50% of what
would be expected without these efforts.
In another study (Suomi et al. 1971) loss of peri-
odontal tissue support in young individuals with gin-
givitis or only loss of small amounts of attachment
was followed over 3 years. An experimental group
receiving scaling and instruction in oral hygiene every
3 months yielded significantly less plaque and gingi-
val inflammation than the control group in which no
special efforts had been made. The mean loss of prob
-
ing attachment was only 0.08 mm per surface in the
experimental as opposed to 0.3 mm in the control
group.
When adult patients with gingivitis were treated
with scaling and root planing, but did not improve
their oral hygiene procedures, the gingival condition
did not improve compared with individuals receiving
prophylaxes at 6-month intervals (Listgarten &
Schifter 1982).
Summary
The available information indicates that the preven-
tion of gingival inflammation and early loss of attach
-
ment in patients with gingivitis depends primarily on
the level of personal plaque control, but also on further
measures to reduce the accumulation of supragingival
and subgingival plaque.
SPT
FOR PATIENTS WITH
PERIODONTITIS
As mentioned previously, a series of longitudinal
studies on periodontal therapeutic modalities was
performed in the past 25 years, first at the University
of Michigan, later at the University of Gothenburg,
Sweden, and also at the Universities of Minnesota,
Nebraska and Loma Linda. These studies always in-
corporated the patients into a well-organized mainte-
nance care system with recall visits at regular intervals
(generally 3-4 months). Although the patients per-
formed plaque control with various degrees of effi-
cacy, the SPT resulted in excellent maintenance of
postoperative attachment levels in most patients
(
Knowles 1973, Ramfjord et al. 1982).
On average, excellent treatment results with main
-
tained reduced probing depths and maintained gains
of probing attachment were documented for most of
the patients in the longitudinal studies irrespective of
the treatment modality chosen (Ramfjord et al. 1975,
Lindhe & Nyman 1975, Rosling et al. 1976, Nyman et
al. 1977, Knowles et al. 1979, 1980, Badersten et al.
1981, 1987, Hill et al. 1981, Lindhe et al. 1982a,
Pihlstrom et al. 1983b, Westfelt et al. 1983a,b, 1985,
Isidor & Karring 1986).
In a study on 75 patients with extremely advanced
periodontitis, who had been successfully treated for
the disease, a result of cause-related therapy and
modified Widman flap procedures (Lindhe & Nyman
1984), recurrent infection occurred in only very few
sites during a 14-year period of effective SPT. How-
ever, it has to be realized that recurrent periodontitis
was noticed at completely unpredictable time inter-
vals, but was concentrated in about 25% of the patient
population (15 out of 61). This suggests that, in a
periodontitis-susceptible risk population, the major-
ity of patients can be "cured" provided an optimally
organized SPT is performed, while a relatively small
proportion of patients (20-25%) will suffer from occa-
sional episodes of recurrent periodontal reinfection. It
is obviously a challenge for the diagnostician to iden-
tify such patients with very high disease susceptibility
and to monitor the dentitions for recurrent periodon-
titis on a long-term basis.
As opposed to the study by Lindhe & Nyman (1984)
which involved exclusively patients with advanced
periodontitis, another study on 52 patients with gen-
eralized mild to moderate adult periodontitis ad-
dressed the efficacy of SPT 8 years following comple-
tion of cause-related periodontal therapy (Bragger et
al. 1992). Full mouth intraoral radiographs were used
to assess changes in the radiographic alveolar bone
height as a percentage of the total tooth length. As a
result of cause-related therapy, a gain in probing at-
tachment followed by a loss of 0.5-0.8 mm over the
following 8 years was observed. The radiographic loss
of alveolar bone height in the same time period was
less than 2% and thus clinically insignificant.
h1
this
SUPPORTIVE PERIODONTAL THERAPY (SPT) • 787
patient group initially presenting with mild to mod-
erate periodontitis, the frequency of SPT rendered per
year did not affect the rate of progression of periodon-
tal desease. However, patients seeking SPT less than
once per year over 8 years lost further periodontal
attachment during the period of observation. From
these studies it is evident that patients having experi-
enced periodontitis need some kind of SPT. Obviously,
the frequency of SPT visits has to be adapted to the
risk of susceptibility for the disease. Patients with
advanced periodontitis may need SPT at a regular and
rather short time interval (3-4 months), while for mild
to moderate forms of periodontitis, one annual visit
may be enough to prevent further loss of attachment.
Sumniary
SPT is an absolute prerequisite to guarantee beneficial
treatment outcomes with maintained levels of clinical
attachment over long periods of time. While the main-
tenance of treatment results for the majority of pa-
tients has been documented up to 14 years, it has to be
realized that a small proportion of patients will expe-
rience recurrent infections with progression of peri-
odontal lesions in a few sites in a completely unpre-
dictable mode. The continuous risk assessment at sub
ject, tooth and tooth site levels, therefore, represents a
challenge for the SPT concept.
CONTINUOUS MULTILEVEL RISK
ASSESSMENT
As opposed to an initial periodontal diagnosis which
considers the sequelae of the disease process, i.e. docu
ments the net loss of periodontal attachment and the
concomitant formation of periodontal pockets and the
existence of inflammation, clinical diagnosis during
SPT has to be based on the variations of the health
status obtained following successful active periodon-
tal treatment. This, in turn, means that a new baseline
will have to be established once the treatment goals of
active periodontal therapy (i.e. phases 1-3) are reached
and periodontal health is restored (Claffey 1991). This
baseline includes the level of clinical attachment
achieved while the inflammatory parameters are sup-
posed to be under control. Under optimal circum-
stances, supportive periodontal care would maintain
clinical attachment levels obtained after active ther-
apy for the years to come. The relevant question
would, therefore, be which clinical parameters may
serve as early indicators for a new onset or recurrence
of the periodontal disease process, i.e. reinfection and
progression of periodontal breakdown of a previously
treated periodontal site.
From a clinical point of view the stability of peri-
odontal conditions reflects a dynamic equilibrium be-
tween bacterial aggression and effective host re-
sponse. As such, this homeostasis is prone to sudden
changes whenever one of the two factors prevails.
Hence, it is evident that the diagnostic process must
be based on a continuous monitoring of the multilevel
risk profile. The intervals between diagnostic assess-
ments must also be chosen based on the overall risk
profile and the expected benefit. To schedule patients
for supportive periodontal therapy on the basis of an
individual risk evaluation for recurrence of disease
has been demonstrated to be cost-effective (Axelsson
& Lindhe 1981a,b, Axelsson et al. 1991).
By virtue of their previous disease predisposition,
all patients under a periodontal maintenance program
represent a population with a moderate to high risk
for recurrent periodontal infection. As opposed to the
general population without such a history, periodon-
tal patients need to participate in a well-organized
recall system which should provide both continuous
risk assessment and adequate supportive care. With-
out this, the patients are likely to experience progres-
sive loss of periodontal attachment (Axelsson &
Lindhe 1981a, Kerr 1981, Becker et al. 1984, Cortellini
et al. 1994, 1996). On the other hand, it is important to
determine the level of risk for progression in each
individual patient in order to be able to determine the
frequency and extent of professional support neces-
sary to maintain the attachment levels obtained fol-
lowing active therapy. The determination of such risk
level would thus prevent undertreatment, and also
excessive overtreatment, during SPT (Bragger et al.
1992).
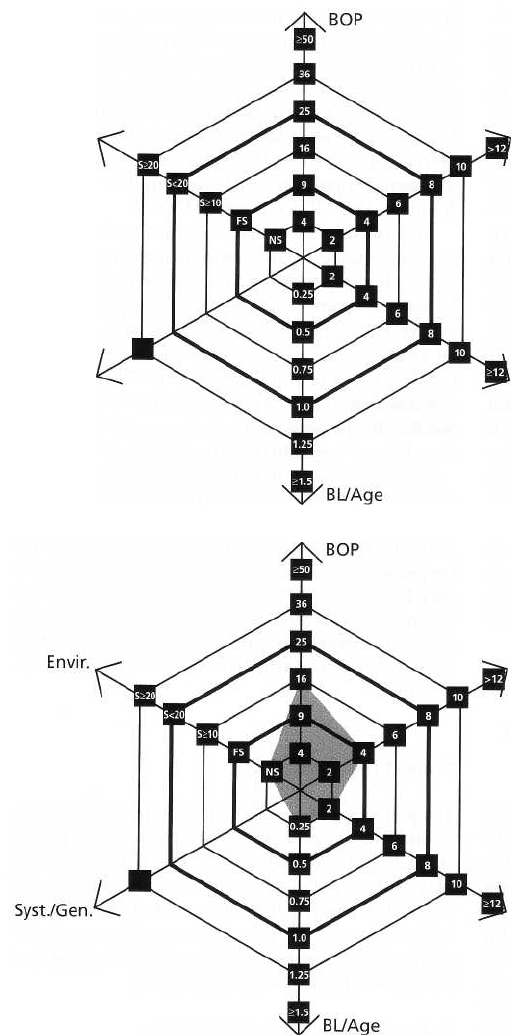
Subject risk assessment
The patient's risk assessment for recurrence of perio-
dontitis maybe evaluated on the basis of a number of
clinical conditions whereby no single parameter dis-
plays a more paramount role. The entire spectrum of
risk factors and risk indicators ought to be evaluated
simultaneously. For this purpose, a functional dia-
gram has been constructed (Fig. 32-3) (Lang & Tonetti
2003) including the following aspects:
1.
Percentage of bleeding on probing
2.
Prevalence of residual pockets greater than 4 mm
3.
Loss of teeth from a total of 28 teeth
4.
Loss of periodontal support in relation to the pa-
tient's age
5.
Systemic and genetic conditions
6.
Environmental factors such as cigarette smoking.
Each parameter has its own scale for minor, moderate
and high risk profiles. A comprehensive evaluation,
the functional diagram will provide an individualized
total risk profile and determine the frequency and
complexity of SPT visits. Modifications maybe made
to
the functional diagram if additional factors become
important from future evidence.
Compliance
with recall
system
Several investigations have indicated that only a mi-
788 • CHAPTER 32
Syst./Gen.
PD>_5mm
Tooth
loss
Envir.
Fig. 32-3a. Functional diagram to
evaluate the patient's risk for recur-
rence of periodontitis. Each vector
represents one risk factor or indicator
with an area of relatively low risk, an
area of moderate risk and an area of
high risk for disease progression. All
factors have to be evaluated together
and hence the area of relatively low
risk is found within the center circle
of the polygon, while the area of
high
risk is found outside the periph
ery
of the second ring in bold. Be
tween
the two rings in bold, there is
the area
of moderate risk.
Fig. 32-3b. Functional diagram of a
low risk maintenance patient. BOP is
15%, four residual pockets ? 5 mm
are diagnosed, two teeth have been
lost, the bone factor in relation to the
age is 0.25, no systemic factor is
known and the patient is a non-
smoker.
PD>_5mm
Tooth
loss
nority of periodontal patients comply with the pre-
scribed supportive periodontal care (Wilson et al.
1984,
Mendoza et al. 1991, Checchi et al. 1994, De
metriou
et al. 1995). Since it has been clearly establ
ished that
treated periodontal patients who comply
with regular
periodontal maintenance appointments
have a better
prognosis than patients who do not
comply (Axelsson
& Lindhe 1981a, Kent 1981, Becker
et al. 1984,
Cortellini et al. 1994, 1996), non-compliant
or poorly
compliant patients should be considered at
higher risk
for periodontal disease progression. A re-port that
investigated the personality differences of patients
participating in a regular recall program as
compared
to patients who did not, revealed that pa
tients who did
not take part in a maintenance program
following periodontal therapy had higher incidences
of
stressful life events and less stable personal relation
-
ships in their lives (Becker et al. 1988).
Oral hygiene
Since bacterial plaque is by far the most important
etiologic agent for the occurrence of periodontal dis-
eases (for review see Kornman & Loe 1993), it is evi-
dent that the full mouth assessment of the bacterial
load must have a pivotal impact in the determination
of the risk for disease recurrence. It has to be realized,
however, that regular interference with the microbial
ecosystem during periodontal maintenance will even-
tually obscure such obvious associations. In patients
treated with various surgical and non-surgical mo-
SUPPORTIVE PERIODONTAL THERAPY (SPT) •
789
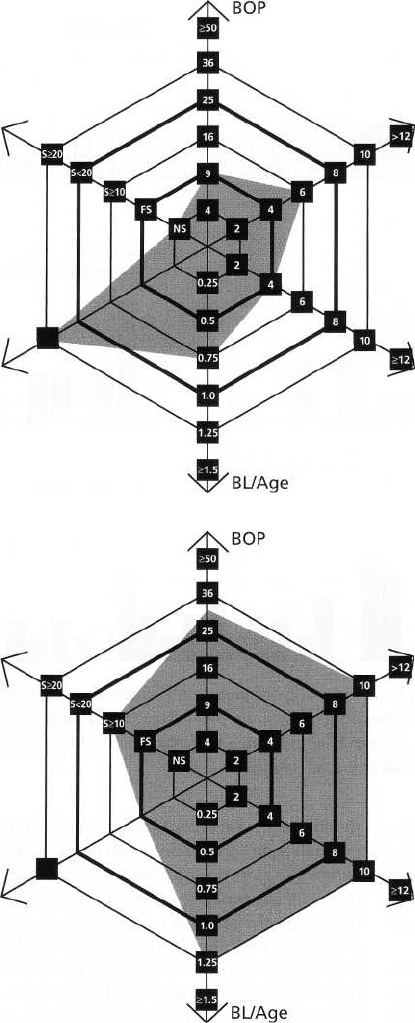
Fig. 32-3c. Functional diagram of a
medium risk maintenance patient.
BOP is 9%, 6 residual pockets ? 5
mm are diagnosed, four teeth have
been lost, the bone factor in relation
to the age is 0.75, the patient is a
Type I diabetic, but a non-smoker.
Syst./Gen.
PD?5mm
Tooth
loss
Envir.
Fig. 32-3d. Functional diagram of a
high risk maintenance patient. BOP
is 32%, ten residual pockets 5 mm
are diagnosed, ten teeth had been
lost, the bone factor in relation to the
age is 1.25, no systemic factor is
known and the patient is a occa-
sional smoker.
Syst./Gen.
PD?5mm
Tooth
loss
Envir.
dalities, it has been clearly established that plaque-in-
fected dentitions will yield recurrence of periodontal
disease in multiple locations, while dentitions under
plaque control and regular supportive care maintain
periodontal stability for many years (Rosling et al.
1976, Axelsson & Lindhe 1981a,b). Studies have thus
far not identified a level of plaque infection compatible
with maintenance of periodontal health. How-
ever, in a
clinical set-up, a plaque control record of 20-40%
might be tolerable by most patients. It is im
portant to
realize that the full mouth plaque score has
to be
related to the host response of the patient, i.e.
compared to inflammatory parameters.
Percentage of sites with bleeding on probing
Bleeding
on gentle probing represents an objective inflammatory
parameter which has been incorpo
rated into index
systems for the evaluation of periodontal conditions (
Loe & Silness 1963, Miihlemann
& Son 1971) and is
also used as a parameter by itself.
In a patient's risk
assessment for recurrence of periodontitis, BOP
reflects, at least in part, the patient's
compliance and
standards of oral hygiene perform
ance. Although
there is no established acceptable level
of prevalence of
bleeding on probing in the dentition
above which a
higher risk for disease recurrence has been established,
a BOP prevalence of 25% has been the cut-off point
between patients with maintained periodontal stability
for 4 years and patients with
recurrent disease in the same time frame in a prospec-
tive study in a private practice (Joss et al. 1994) (Fig.
32-4). Further evidence of BOP percentages between
20% and 30% determining a higher risk for disease
progression originates from studies of Claffey et al.
(
1990) and Badersten et al. (1990).
In assessing the patient's risk for disease progres-
sion, BOP percentages reflect a summary of the pa-
tient's ability to perform proper plaque control, the
patient's host response to the bacterial challenge and
the patient's compliance. The percentage of BOP,
therefore, is used as the first risk factor in the func-
tional diagram of risk assessment (Fig. 32-3). The scale
runs in a quadratic mode with 4, 9, 16, 25, 36 and >
49% being the divisions on the vector.
Individuals with low mean BOP percentages (<
10%
of the surfaces) may be regarded as patients with a low
risk for recurrent disease (Lang et al. 1990), while
patients with mean BOP percentages > 25% should be
considered to be at high risk for reinfection.
Prevalence of
residual pockets greater than 4 mm
The enumeration of the residual pockets with probing
depths greater than 4 mm represents — to a certain
extent — the degree of success of periodontal treatment
rendered. Although this figure
per se
does not make
much sense when considered as a sole parameter, the
evaluation in conjunction with other parameters such
as bleeding on probing and/or suppuration will re
flect
existing ecologic niches from and in which rein
fection
might occur. It is, therefore, conceivable that
periodontal stability in a dentition would be reflected
in
a minimal number of residual pockets. Presence of
high frequencies of deep residual pockets and deep-
ening of pockets during supportive periodontal care
has, in fact, been associated with high risk for disease
progression (Badersten et al. 1990, Claffey et al. 1990).
On the other hand, it has to be realized that an in-
creased number of residual pockets does not necessar-
ily imply an increased risk for re-infection or disease
progression, since a number of longitudinal studies
have established the fact that, depending on the indi-
vidual supportive therapy provided, even deeper
pockets may be stable without further disease pro-
gression for years (e.g. Knowles et al. 1979, Lindhe &
Nyman 1984).
Nevertheless, in assessing the patient's risk for dis-
ease progression, the number of residual pockets with
a probing depth of 5 mm is assessed as the second risk
indicator for recurrent disease in the functional
diagram of risk assessment (Fig. 32-3). The scale runs
790 • CHAPTER
32
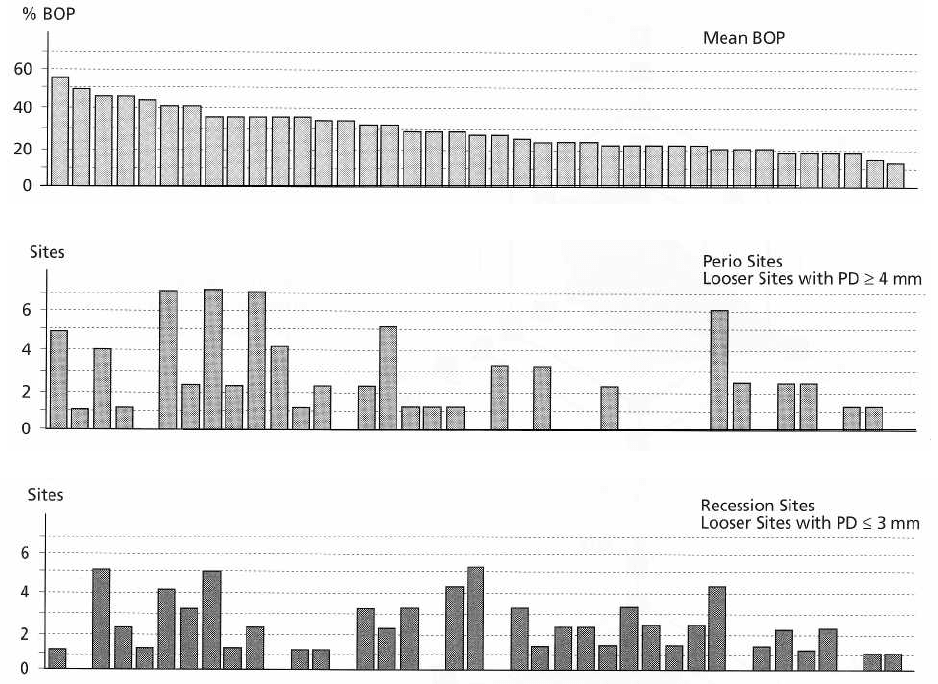
Fig. 32-4. Distribution of "looser" sites (probing depth PD ? 4 mm) due to periodontal disease progression with or
without concomitant recession, dependent on the mean bleeding on probing percentage (BOP) during an observa-
tion period of 4 years. Patients are sorted by decreasing mean BOP percentages. Patients with < 20% BOP have a
significantly lower risk for disease recurrence. (Data from Joss et al. 1994.)
SUPPORTIVE PERIODONTAL THERAPY (SPT) • 791
in a linear mode with 2, 4, 6, 8, 10 and 12% being the
divisions on the vector.
Individuals with up to four residual pockets may
be regarded as patients with a relatively low risk,
while patients with more than eight residual pockets
may be regarded as individuals with high risk for
recurrent disease.
Loss of teeth from a total of
28
teeth
Although the reason for tooth loss may not be known,
the number of remaining teeth in a dentition reflects
the functionality of the dentition. Mandibular stability
and individual optimal function may be assured even
with a shortened dental arch of premolar to premolar
occlusion, i.e. 20 teeth. The shortened dental arch does
not seem to predispose the individual to mandibular
dysfunction (Witter et al. 1990, 1994). However, if
more than eight teeth from a total of 28 teeth are lost,
oral function is usually impaired (Kayser 1981, 1994,
1996). Since tooth loss also represents a true end-point
outcome variable reflecting the patient's history of
oral
diseases and trauma, it is logical to incorporate
this
risk indicator as the third parameter in the func-
tional diagram of risk assessment (Fig. 32-3). The
number of teeth lost from the dentition without the
third molars (28 teeth) is counted, irrespective of their
replacement. The scale runs also in a linear mode with
2, 4, 6, 8,10 and 12% being the divisions on the vector.
Individuals with up to four teeth lost may be re-
garded as patients in low risk, while patients with
more than eight teeth lost may be considered as being
in high risk.
Loss of periodontal support in relation to the
patient's age
The extent and prevalence of periodontal attachment
loss (i.e. previous disease experience and susceptibil-
ity), as evaluated by the height of the alveolar bone on
radiographs, may represent the most obvious indica-
tor of subject risk when related to the patient's age. In
light of the present understanding of periodontal dis-
ease progression, and the evidence that both onset and
rate of progression of periodontitis might vary among
individuals and during different time frames (van der
Velden 1991), it has to be realized that previous attach
ment loss in relation to the patient's age does not rule
out the possibility of rapidly progressing lesions.
Therefore, the actual risk for further disease progres-
sion in a given individual may occasionally be under-
estimated. Hopefully, the rate of progression of dis-
ease has been positively affected by the treatment
rendered and, hence, previous attachment loss in re-
lation to patient's age may be a more accurate indica-
tor during SPT than before active periodontal treat-
ment. Given the hypothesis that a dentition may be
functional for the most likely life expectancy of the
subject in the presence of a reduced height of peri-
odontal support (i.e. 25-50% of the root length), the
risk assessment in treated periodontal patients may
represent a reliable prognostic indicator for the stabil-
ity of the overall treatment goal of keeping a func-
tional dentition for a lifetime (Papapanou et al. 1988).
The estimation of the loss of alveolar bone is per-
formed in the posterior region on either periapical
radiographs, in which the worst site affected is esti-
mated gross as a percentage of the root length, or on
bite-wing radiographs in which the worst site affected
is estimated in mm. One mm is equated with 10% bone
loss. The percentage is then divided by the patient's
age. This results in a factor. As an example, a 40-year
-
old patient with 20% of bone loss at the worst posterior
site affected would be scored BL/Age = 0.5. Another
40-year-old patient with 50% bone loss at the worst
posterior site scores BL/Age = 1.25.
In assessing the patient's risk for disease progres-
sion, the extent of alveolar bone loss in relation to the
patient's age is estimated as the fourth risk indicator
for recurrent disease in the functional diagram of risk
assessment (Fig. 32-3). The scale runs in increments of
0.25 of the factor BL/Age, with 0.5 being the division
between low and moderate risk and 1.0 being the
division between moderate and high risk for disease
progression. This, in turn, means that a patient who
has lost a higher percentage of posterior alveolar bone
than his/her own age is at high risk regarding this
vector in a multifactorial assessment of risk.
Systemic conditions
The most substantiated evidence for modification of
disease susceptibility and/or progression of peri-
odontal disease arises from studies on Type I and Type
II (insulin-dependent and non-insulin-dependent)
diabetes mellitus populations (Gusberti et al. 1983,
Emrich et al. 1991, Genco & Loe 1993).
It has to be realized that the impact of diabetes on
periodontal diseases has been documented in patients
with untreated periodontal disease, while, as of today,
no clear evidence is available for treated patients. It is
reasonable, however, to assume that the influence of
the systemic conditions may also affect recurrence of
disease.
In recent years, genetic markers have become avail
-
able to determine various genotypes of patients re-
garding their susceptibility for periodontal diseases.
Research on the interleukin-1 (IL-1) polymorphisms
has indicated that IL-1 genotype positive patients
show more advanced periodontitis lesions than IL-1
genotype negative patients of the same age group
(
Kornman et al. 1997). Also, there is a trend to higher
tooth loss in the IL-1 genotype positive subjects
(
McGuire & Nunn 1999). In a retrospective analysis of
over 300 well-maintained periodontal patients, the
IL-1 genotype positive patients showed significantly
higher BOP percentages and a higher proportion of
patients which yielded higher BOP percentages dur-
ing a 1-year recall period than the IL-1 genotype nega
tive control patients (Lang et al. 2000). Also, the latter
group had twice as many patients with improved BOP
percentages during the same maintenance period, in
-
dicating that IL-1 genotype positive subjects do in-
792 • CHAPTER 32
deed represent a group of hyper-reactive subjects even
if they are regularly maintained by effective SPT (Lang
et al. 2000). In a prospective study over 5 years on
Australian white collar and blue collar workers on a
University campus, the IL-1 genotype positive age
group above 50 years showed significantly deeper
probing depth than their IL-1 genotype negative coun
-
terparts, especially when they were non-smokers.
In assessing the patient's risk for disease progres-
sion, systemic factors are only considered, if known,
as the fifth risk indicator for recurrent disease in the
functional diagram of risk assessment (Fig. 32-3). In
this case, the area of high risk is marked for this vector.
If not known or absent, systemic factors are not taken
into account for the overall evaluation of risk.
Research on the association and/or modifying in-
fluence in susceptibility and progression of periodon-
titis of physical or psychologic stress is sparse (Cohen
-
Cole et al. 1981, Green et al. 1986, Freeman & Goss
1993). The hormonal changes associated with this con
dition, however, are well documented (Selye 1950).
Cigarette smoking
Consumption of
tobacco,
predominantly in the form of
smoking or chewing, affects the susceptibility and the
treatment outcome of patients with adult periodonti-
tis. Classical explanations for these observations have
included the association between smoking habits and
poor oral hygiene as well as unawareness of general
health issues (Pindborg 1949, Rivera-Hidalgo 1986).
More recent evidence, however, has established that
smoking
per se
represents not only a risk marker, but
probably a true risk factor for periodontitis (Ismail et
al. 1983, Bergstrom 1989, Bergstrom et al. 1991, Haber
et al. 1993). In a young population (19-30 years of age),
51-56% of periodontitis was associated with cigarette
smoking (Haber et al. 1993). The association of smok-
ing and period ontitis has been shown to be dose-de-
pendent (Haber et al. 1993). It has also been shown that
smoking will affect the treatment outcome after scal-
ing and root planing (Preber & Bergstrom 1985), modi
-
fied Widman flap surgery (Preber & Bergstrom 1990),
and regenerative periodontal therapy (Tonetti et al.
1995). Furthermore, a high proportion of so-called
refractory patients has been identified as consisting of
smokers (Bergstrom & BlomlOf 1992). The impact of
cigarette smoking on the long-term effects of peri-
odontal therapy in a population undergoing suppor-
tive periodontal care has been reported. Smokers dis-
played less favorable healing responses both at re-
evaluation and during a 6-year period of supportive
periodontal care (Baumert-Ah et al. 1994). In spite of
the paucity of evidence relating cigarette smoking to
impaired outcomes during supportive periodontal
care, it seems reasonable to incorporate heavy smok-
ers (> 20 cigarettes/day) in a higher risk group during
maintenance.
In assessing the patient's risk for disease progres-
sion, environmental factors such as smoking must be
considered as the sixth risk factor for recurrent disease
in the functional diagram of risk assessment (Fig.
32-
3). While non-smokers (NS) and former smokers
(FS)
(more than 5 years since cessation) have a rela
tively
low risk for recurrence of periodontitis, the
heavy
smokers (HS), as defined by smoking more than
one
pack per day, are definitely at high risk. Occasional (
OS; < 10 cigarettes a day) and moderate smok
ers (
MS) may be considered in moderate risk for dis
ease
progression.
Calculating the patient's individual periodontal risk
assessment (PRA)
Based on the six parameters specified above, a multi-
functional diagram is constructed for the PRA. In this
diagram, the vectors have been constructed on the
basis of the scientific evidence available. It is obvious
that ongoing validation may result in slight modifica-
tions.
A low PR patient has all parameters within the low
risk categories or at the most one parameter in the
moderate risk category (Fig. 32-3b).
A moderate PR patient has at least two parameters in
the moderate category, but at most one parameter
in the high risk category (Fig. 32-3c).
A high PR patient has at least two parameters in the
high risk category (Fig. 32-3d).
Summary/
The subject risk assessment may estimate the risk for
susceptibility for progression of periodontal disease. It
consists of an assessment of the level of infection
(full
mouth bleeding scores), the prevalence of resid
ual
periodontal pockets, tooth loss, an estimation of
the
loss of periodontal support in relation to the pa
tient's
age, an evaluation of the systemic conditions of
the
patient, and finally, an evaluation of environ-
mental
and behavioral factors such as smoking and stress.
All these factors should be contemplated and
evaluated together. A functional diagram (Fig. 32-3)
may help the clinician in determining the risk for
disease progression on the subject level. This may be
useful in customizing the frequency and content of
SPT visits.
Tooth risk assessment
Tooth position
within the dental arch
Early clinical surveys have associated the prevalence
and severity of periodontal diseases with malocclu-
sion and irregularities of tooth position (Ditto & Hall
1954, Bilimoria 1963). However, many subsequent
studies using clinical evaluation methods could not
confirm these conclusions (Beagrie & James 1962, Gei
ger 1962, Gould & Picton 1966). Although a relation-
ship between crowding and increased plaque reten-
tion and gingival inflammation has been established
(
Ingervall et al. 1977, Buckley 1980, Griffith & Addy
1981, Horup et al. 1987), no significant correlation
SUPPORTIVE PERIODONTAL THERAPY (SPT) •
793
between anterior overjet and overbite (Geiger et al.
1973), crowding and spacing (Geiger et al. 1974) or
axial inclinations and tooth drifts (Geiger & Wasser-
man 1980) and periodontal destruction, i.e. attach-
ment loss subsequent to gingival inflammation, could
be established. It is evident from the literature men-
tioned that crowding of teeth might eventually affect
the amount of plaque mass formed in dentitions with
irregular oral hygiene practices, thus contributing to
the development of chronic gingivitis, but, as of today,
it remains to be demonstrated whether tooth malpo-
sition within the dental arch will lead to an increased
risk for periodontal attachment loss.
Furcation
involvement
It is evident that multirooted teeth with periodontal
lesions extending into the furcation area have been the
subject of intensive therapeutic studies for many years
(Kalkwarf & Reinhardt 1988). Retrospective analyses
of large patient populations in private periodontal
practices of periodontal specialists (Hirschfeld & Was
-
serman 1978, McFall 1982) have clearly established
that multirooted teeth appear to be at high risk for
tooth loss during the maintenance phase. The most
impressive long-term documentation maintained 600
patients for an average duration of 22 years, and 10%
of these patients were even maintained for more than
30 years (Hirschfeld & Wasserman 1978). While 83%
of the patients could be considered "well maintained"
and had lost only 0-3 teeth during the observation
period, a patient group of 4% (25) was identified with
an extreme risk for disease progression and had lost
between 10 and 23 teeth during a regularly scheduled
maintenance program. Irrespective of the patient
group of low, moderate, and high risk for disease
progression during maintenance, the majority of the
teeth lost were furcation-involved molars (Hirschfeld
& Wasserman 1978). Similar results were obtained in
a study on 100 treated periodontal patients main-
tained for 15 years or longer (McFall 1982).
Prospective studies on periodontal therapy in mul-
tirooted teeth have also revealed significant differ-
ences between non-molar sites and molar flat surfaces
on the one hand and molar furcation sites on the other,
when looking at the treatment outcomes evaluated as
bleeding frequency, probing depth reductions and lev
-
els of attachment (Nordland et al. 1987). Again, teeth
with furcation involvement and original probing
depths > 6 mm had reduced treatment outcomes.
The assumption that the prognosis for single rooted
teeth and non-furcation-involved multirooted teeth is
better than the prognosis for furcation-involved mul-
tirooted teeth has also been confirmed by Ramfjord et
al. (1987) in a prospective study over 5 years. It has to
be realized, however, that these results are not in-
tended to imply that furcation-involved teeth should
be extracted, since all the prospective studies have
documented a rather good overall prognosis for such
teeth if regular supportive care is provided by a well-
organized maintenance program.
Iatrogenic factors
Overhanging restorations and ill-fitting crown mar-
gins certainly represent an area for plaque retention,
and there is an abundance of association studies docu
menting increased prevalence of periodontal lesions
in
the presence of iatrogenic factors (for review see
Leon
1977). Depending on the supragingival or sub-
gingival location of such factors, their influence on the
risk for disease progression has to be considered. It has
been established that slightly subgingivally located
overhanging restorations will, indeed, change the
ecologic niche, providing more favorable conditions
for the establishment of a Gram-negative anaerobic
microbiota (Lang et al. 1983). There is no doubt that
shifts in the subgingival microflora towards a more
periodontopathic microbiota, if unaffected by treat-
ment, represent an increased risk for periodontal
breakdown.
Residual periodontal support
Although many clinicians believe that teeth with re-
duced periodontal support are unable to function
alone and should be extracted or splinted, there is
clear evidence from longitudinal studies that teeth
with severely reduced, but healthy, periodontal sup-
port can function either individually or as abutments
for many years without any further loss of attachment
(Nyman & Lindhe 1979, Nyman & Ericsson 1982,
Bragger et al. 1990). Hence, successfully periodontally
treated teeth can be maintained over decades and
function as abutments in fixed bridgework or as indi-
vidual chewing units irrespective of the amount of
residual periodontal support, provided that physi-
ologic masticatory forces do not subject such teeth to
a
progressive trauma which may lead to spontaneous
extraction. Obviously, by virtue of the already reduced
support, should disease progression occur in severely
compromised teeth, this may lead to spontaneous
tooth exfoliation.
Mobility
In light of the discussion of abutment teeth with se-
verely reduced but healthy periodontal support, tooth
mobility may be an indicator for progressive trau-
matic lesions, provided that the mobility is increasing
continuously (Nyman & Lang 1994). When assessing
tooth mobility, it has to be realized that two factors
may contribute to hypermobility: (1) a widening of the
periodontal ligament as a result of unidirectional or
multidirectional forces to the crown, high and fre-
quent enough to induce resorption of the alveolar
bone walls; and (2) the height of the periodontal sup-
porting tissues. If this is reduced due to prior peri-
odontal disease, but the width of the periodontal liga-
ment is unchanged, the amplitude of root mobility
within the remaining periodontium is the same as in
a tooth with normal height, but the leverage on the
tooth following application of forces to the crown is
changed. Therefore, it has to be realized that all teeth
that have lost periodontal support have increased
794 •
CHAPTER
32
tooth mobility as defined by crown displacement upon
application of a given force. Nevertheless, this
hypermobility should be regarded as physiologic
(
Nyman & Lindhe 1976).
Since tooth mobility is probably more frequently
affected by reduced periodontal height rather than
unidirectional or multidirectional application of
forces
onto the tooth, its significance for the evaluation
of the
periodontal conditions has to be questioned. Several
studies have indicated that tooth mobility
varies
greatly before, during and after periodontal
therapy (
Persson 1980, 1981a,b). From these studies it
can be
concluded that periodontally involved teeth
show a
decrease in mobility following non-surgical
and/or
surgical periodontal procedures. However,
following
surgical procedures, tooth mobility may
temporarily
increase during the healing phase and
may resume
decreased values later on. Provisional
splinting as an
adjunct to non-surgical or surgical
therapy does not
seem to affect the final result of tooth
mobility.
Summary
The tooth risk assessment encompasses an estimation
of the residual periodontal support, an evaluation of
tooth positioning, furcation involvements, presence of
iatrogenic factors and a determination of tooth mobil-
ity to evaluate functional stability. A risk assessment
on the tooth level may be useful in evaluating the
prognosis and function of an individual tooth and
may indicate the need for specific therapeutic meas-
ures during SPT visits.
Site risk assessment
Bleeding on probing
Absence of bleeding on probing is a reliable parameter
to indicate periodontal stability if the test procedure
for assessing bleeding on probing has been stand-
ardized (Lang et al. 1990). Presence of bleeding upon
standardized probing will indicate presence of gingi-
val inflammation. Whether or not repeated bleeding
on probing over time will predict the progression of a
lesion is, however, questionable (Lang et al. 1986,1990,
Vanooteghem et al. 1987). Nevertheless, a 30% prob-
ability for attachment loss to occur in the future may
be predicted for sites repeatedly positive for bleeding
on probing (Fig. 32-5) (Badersten et al. 1985, 1990,
Lang et al. 1986, Vanooteghem et al. 1987,1990, Claffey
et al. 1990).
Obviously, bleeding on probing is rather sensitive
to different forces applied to the tissues. An almost
linear relationship (R = 0.87) existed between the prob
-
ing force applied and the percentage of bleeding sites
in a study on healthy young adults (Fig. 32-6) (Lang
et
al. 1991). If the probing force exceeded 0.25 N (25 g),
the tissues were traumatized and bleeding was pro-
voked as a result of trauma, rather than as a result of
tissue alterations due to inflammation. To assess the
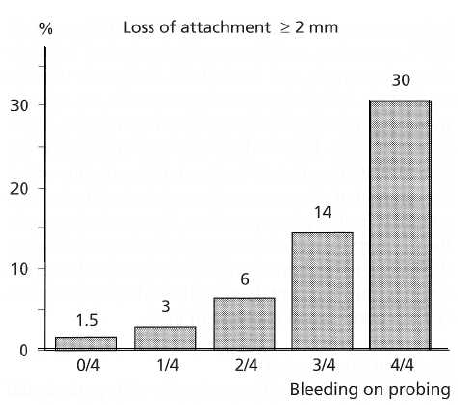
Fig. 32-5. Positive predictive values for loss of probing
attachment of ? 2 mm in 2 years in sites which bled on
probing 0, 1, 2, 3 or 4 times out of four SPT visits in a to-
tal of 48 patients following active periodontal therapy.
(
Data from Lang et al. 1986.)
"true" percentage of bleeding sites due to inflamma-
tion, a probing force of 0.25 N or less should be ap-
plied, which clinically means a light probing force.
This has also been confirmed for patients who have
experienced loss of attachment, i.e. with successfully
treated advanced periodontitis (Fig. 32-7) (Karayian-
nis et al. 1991, Lang et al. 1991).
Since absence of bleeding on probing at 0.25 N
indicated periodontal stability with a negative predic-
tive value of 98-99% (Lang et al. 1990), this clinical
parameter is the most reliable for monitoring patients
over time in daily practice. Non-bleeding sites maybe
considered periodontally stable. On the other hand,
bleeding sites seem to have an increased risk for
progression of periodontitis, especially when the
same site is bleeding at repeated evaluations over
time
(Lang et al. 1986, Claffey et al. 1990).
It is, therefore, advisable to register the sites which
bleed on probing (BOP) in a dichotomous way using
a
constant force of 0.25 N. This allows the calculation of
the mean BOP for the patient, and yields also the
topographic location of the bleeding site. Repeated
scores during maintenance will yield the surfaces at
higher risk for loss of attachment.
Probing
depth and
loss of attachment
Clinical probing is the most commonly used parame-
ter both to document loss of attachment and to establ-
ish a diagnosis of periodontitis. There are, however,
some sources of error inherent in this method which
contribute to the variability in the measurements.
Among these are (1) the dimension of the periodontal
probe; (2) the placement of the probe and obtaining a
reference point; (3) the crudeness of the measurement
scale; (4) the probing force; and (5) the gingival tissue
conditions.
