Fisher John P. e.a. (ed.) Tissue Engineering
Подождите немного. Документ загружается.

mikos: “9026_c023” — 2007/4/9 — 15:52 — page 18 — #18
23-18 Tissue Engineering
has been well documented. When cells remain unattached, tissue formation is absent, while suspension
in hydrogels can promote both bone and cartilage formation [42].
Meshes can be made from degradable or nondegradable synthetic materials. Natural porous meshes,
such as coral hydroxyapatite have also been utilized as scaffolds [43]. Nonwoven meshes of polyglycolic
acid (PGA) and polylactic acid (PLA), used alone or as copolymers, are popular in tissue engineering,
because they have already received approval from the FDA for medical implantation into humans [39].
These materials can be formed into complex shapes by polymerizing or fashioning the material within
anatomic molds. The rate of degradation of the copolymeric scaffolds can also be adjusted by chan-
ging the ratio of the copolymers. While complete hydrolysis of many polymeric meshes will occur,
acidic degradation products may incite an inflammatory response which can adversely affect the form-
ation of bone or cartilage. Nonwoven meshes have already demonstrated their ability to support TMJ
disc fibrochondrocytes [39], osteoblast-like cells [44], and chondrocytes [45] in vitro. These studies
demonstrate the promise of these materials for the reconstruction of an interpositional disc and articular
cartilage.
23.7.4 Signals and Stimulation Issues
Molecular signals and nonbiological stimuli may be used to induce positive and negative gene expression,
and thus biosynthetic responses, in cells. These modulators can take a variety of forms such as growth
factor application, mechanical stimulation, the use of adhesion peptides, and the generation of oxygen
gradients, electrical currents, and sonic stimulation. The effects of these agents can be direct or synergistic
and may produce single or inter-related responses. By varying parameters, such as the bioactivity of
growth factors and proteins, the size and frequency of mechanical and sonic stimulations, the length of
stimulations, and dosage and saturation effects, the regeneration of tissue can be optimized.
Several studies have investigated the effect of growth factors, mechanical stimulation, and oxygen
on tissue engineered constructs. Each stimulant, acting through the modulation of the local envir-
onment, is capable of producing tissue-like ECM proteins. However, the formation of an organized,
three-dimensional tissue array with biochemical and biomechanical properties similar to native tissue
will probably require a combination of signals. One method for creating a multisignal environment
employs bioreactors to supply mechanical stimulation, such as hydrostatic pressure, in combination with
a variety of other signals such as growth factors. Bioreactors capable of perfusion are also able to deliver
molecular signals more efficiently by dispersing the biochemical agent throughout the tissue engineered
construct.
23.7.5 Specific Issues Related to Joint Reconstruction
Since a tissue engineered construct is composed of biological tissue, consideration must be given to the
original disease process or joint loading patterns that initially produced a dysfunctional joint. If parafunc-
tional forces exist, strategies to decrease joint loading must be employed. These include the use of dental
orthotic devices, which reduce forces generated by the muscles of mastication and provide protective
responses through neuromuscular afferent signals from the periodontium surrounding the teeth.
Another challenge is the maintenance of construct viability following implantation. In order to survive,
cells require nutrients diffusing from the surrounding vasculature and a method to remove metabolic
waste. Establishing a vascular supply in a tissue engineered construct is critical, especially for vascu-
lar tissues like bones. Fortunately, fibrocartilage has even lower metabolic requirements, an advantage
where TMJ reconstruction is concerned. A separate concern involves the creation and connection of the
nervous system in a tissue engineered construct to guide the complex movements of the joint and provide
proprioceptive input to the neuromuscular system. Meeting this requirement is important for the return
of normal function to the reconstructed joint. It may be possible to utilize native tissue for these two
functions, if efforts are made at the time of joint or disc removal to preserve the capsule, synovium, and
vascular supply from the bony resection margins. When these structures are compromised, such as the
mikos: “9026_c023” — 2007/4/9 — 15:52 — page 19 — #19
Tissue Engineering of the Temporomandibular Joint 23-19
case with multiply operated patients, the success of any reconstruction diminishes. Avoidance of multiple
surgeries should therefore be part of the overall strategy for using tissue engineering to provide improved
results compared to current modalities.
There are also concerns with the immunogenicity of tissue engineered constructs if nonautologous cells
and a synthetic matrix are used for the construct. This is especially significant if xenogeneic sources are
employed. Possiblesources for TMJ cells include the contralateral joint, provided that it is not also diseased.
Alternatively, fibroblasts and fibrochondrocytes, the lineages found in TMJ tissue, may be harvested from
another fibrocartilaginous joint such as the sternoclavicular joint. It should be kept in mind that biological
tissue is capable of varying degrees of adaptation according to the local environment. While this tenet has
not been explored in tissue engineering reconstruction of the TMJ, it would not be unreasonable to expect
that an engineered construct composed of cells from other diarthrodial joints or cartilaginous structures
are capable of phenotypical transformation into cells more closely resembling those of the native TMJ. The
successful use of such unrelated tissues as scar bands, fascia, auricular cartilage, costochondral cartilage,
dermis, and fat support this contention.
The time required to create a viable tissue engineered construct for the reconstruction of a disc or total
joint must also be considered. At this stage, an estimation of the period necessary for the population
of an implant with sufficient cells of the desired lineage with properties suitable for handling, surgical
implantation and attachment, is unknown. While TMJ reconstruction is generally an elective procedure,
it would be unreasonable to consider tissue engineering techniques requiring more than several months
as viable alternatives to current modalities.
Another important concern focuses on the ability to stabilize a construct within the joint. Even after the
successful creation of replacement tissue, the implant must be anchored to existing structures. To facilitate
this process, the implant must possess sufficient bulk, surface area, strength, and tenacity to attach it to the
remaining skeleton. Current methods for repositioning a disc include the use of sutures threaded through
holes made in the adjacent bone or attaching it to bone anchors such as the Mitek® device inserted into
the condylar head. Single point attachment of structures which usually require circumferential fixation
for positional anchorage are inherently unstable. Methods for providing multiple attachments of a disc
replacement need to be developed for successful function to be restored. This is especially true when the
zonal differences and functional properties of each zone are considered. Attachment of a condylar or fossa
engineered implant is a little easier, provided that the construct possesses sufficient bulk and strength.
Bone plates and screws are currently available for the fixation of skeletal structures and these could be
used for a tissue engineered construct.
With the reconstruction of a joint, lubrication of the articulating surfaces must be considered. This
function is normally performed by the synovial fluid, but the effects of disease or surgery may compromise
the normal secretion and composition of the fluid available. Synthetic adjuvants, such as hyaluronic acid
substitutes, may be used in conjunction with joint replacement procedures to protect the implant from
unwanted forces, while the synovium heals.
The last issue concerning the successful application of tissue engineering techniques for the reconstruc-
tion of TMJ components concerns the unavoidable consequences of any surgical maneuver, specifically
the development of intra-articular scars. Steroid injections can help reduce this natural consequence of
surgery, but perhaps the most effective results are seen through the fastidious employment of postoperat-
ive physical therapy exercises. These maneuvers promote the formation of long vs. short, scars. They also
encourage the necessary plasmatic diffusion of fluids responsible for joint nutrition and metabolism.
23.7.6 The Future of Tissue Engineering in the TMJ
The challenges associated with tissue engineering are immense, but the benefit of utilizing tailored bio-
logical constructs without the morbidity of an autogenous donor site, are obvious. Tissue engineered
initiatives for the reconstruction of the TMJ and disc avoids the problems associated with the implant-
ation of prosthetic devices or tissues dissimilar from natural joint components. Efforts toward tissue
engineering in the TMJ are relatively new, however, emergent technologies and studies add promise to the
mikos: “9026_c023” — 2007/4/9 — 15:52 — page 20 — #20
23-20 Tissue Engineering
goal of tissue engineering TMJ replacement tissues. Along the way, characteristics about TMJ tissues are
revealed and our comprehension of this complex joint’s function and structure increases. Solutions for sev-
eral challenges facing biomedical engineers will be developed with each progressive study. Currently, TMJ
tissue engineering is in its formative years. Only four original studies on tissue engineering of the TMJ disc
had been published at the date of this article’s submission. However, the future promises new knowledge
and innovative technologies which may yet allow for the creation of viable, implantable tissue engineered
constructs.
References
[1] Dolwick, M.F. (1983) The temporomandibular joint: normal and abnormal anatomy. In Internal
Derangements of the Temporomandibular Joint (Helms, C.A. et al., eds.), pp. 1–14, Radiology
Research and Education Foundation.
[2] Gillbe, G.V. (1975) The function of the disc of the temporomandibular joint. J. Prosthet. Dent. 33,
196–204.
[3] Detamore, M.S. and Athanasiou, K.A. (2003) Motivation, characterization, and strategy for tissue
engineering the temporomandibular joint disc. Tissue Eng. 9, 1065–1087.
[4] Rees, L.A. (1954) The structure and function of the mandibular joint. Br. Dent. J. 96, 125–133.
[5] Gallo, L.M. et al. (2000) Stress-field translation in the healthy human temporomandibular joint.
J. Dent. Res. 79, 1740–1746.
[6] Zimny, M.L. (1988) Mechanoreceptors in articular tissues. Am. J. Anat. 182, 16–32.
[7] Hills, B.A. and Monds, M.K. (1998) Enzymatic identification of the load-bearing boundary
lubricant in the joint. Br. J. Rheumatol. 37, 137–142.
[8] Minarelli, A.M. et al. (1997) The structure of the human temporomandibular joint disc: a scanning
electron microscopy study. J Orofac. Pain 11, 95–100.
[9] Minarelli, A.M. and Liberti, E.A. (1997) A microscopic survey of the human temporomandibular
joint disc. J. Oral Rehabil. 24, 835–840.
[10] Detamore, M.S. et al. (2004) Quantitive analysis and comparative regional investigation of the
extracellular matrix of the porcine temporomandibular joint disc. Matrix Biol. 24, 45–57.
[11] Berkovitz, B.K. and Pacy, J. (2000) Age changes in the cells of the intra-articular disc of the
temporomandibular joints of rats and marmosets. Arch. Oral Biol. 45, 987–995.
[12] Mills, D.K. et al. (1994) Morphologic, microscopic, and immunohistochemical investigations into
the function of the primate TMJ disc. J. Orofac Pain. 8, 136–154.
[13] Landesberg, R. et al. (1996) Cellular, biochemical and molecular characterization of the bovine
temporomandibular joint disc. Arch. Oral Biol. 41, 761–767.
[14] Detamore, M.S. et al. (2003) Cell type and distribution in the porcine temporomandibular joint
disc. J. Oral Maxillofac. Surg. Accepted.
[15] Milam, S.B. et al. (1991) Characterization of the extracellular matrix of the primate temporo-
mandibular joint. J. Oral Maxillofac. Surg. 49, 381–391.
[16] Kondoh, T. et al. (1998) Prevalence of morphological changes in the surfaces of the temporo-
mandibular joint disc associated with internal derangement. J. Oral Maxillofac Surg. 56, 339–343;
discussion 343–334.
[17] Keith, D.A. (1979) Elastin in the bovine mandibular joint. Arch. Oral Biol. 24, 211–215.
[18] Detamore, M.S. et al. (2003) Structure and function of the temporomandibular joint disc: implic-
ations for tissue engineering. J. Oral Maxillofac. Surg.: Offic. J. Am. Assoc. Oral Maxillofac. Surg. 61,
494–506.
[19] Gross, A. et al. (1999) Elastic fibers in the human temporo-mandibular joint disc. Int. J. Oral
Maxillofac. Surg. 28, 464–468.
[20] Almarza, A.J. et al. (2005) Biochemical content and distribution in the porcine temporomandibular
joint disc. Br. J. Oral Maxillofac. Surg.
mikos: “9026_c023” — 2007/4/9 — 15:52 — page 21 — #21
Tissue Engineering of the Temporomandibular Joint 23-21
[21] Nakano, T. and Scott, P.G. (1989) A quantitative chemical study of glycosaminoglycans in the
articular disc of the bovine temporomandibular joint. Arch. Oral Biol. 34, 749–757.
[22] Nakano, T. and Scott, P.G. (1989) Proteoglycans of the articular disc of the bovine
temporomandibular joint. I. High molecular weight chondroitin sulphate proteoglycan. Matrix
9, 277–283.
[23] Sindelar, B.J.et al. (2000) Effects of intraoral splint wear on proteoglycans in the temporomandibular
joint disc. Arch. Biochem. Biophys. 379, 64–70.
[24] Axelsson, S. et al. (1992) Glycosaminoglycans in normal and osteoarthrotic human temporo-
mandibular joint disks. Acta Odontol. Scand. 50, 113–119.
[25] Scott, P.G. et al. (1989) Proteoglycans of the articular disc of the bovine temporomandibular joint.
II. Low molecular weight dermatan sulphate proteoglycan. Matrix 9, 284–292.
[26] Nakano, T. and Scott, P.G. (1996) Changes in the chemical composition of the bovine
temporomandibular joint disc with age. Arch. Oral Biol. 41, 845–853.
[27] Gage, J.P. et al. (1995) Collagen type in dysfunctional temporomandibular joint disks. J. Prosthet.
Dent. 74, 517–520.
[28] Allen, K.D. and Athanasiou, K.A. (2005) A surface-regional and freeze-thaw characterization of the
porcine temporomandibular joint disc. Ann. Biomed. Eng. 33, 859–897.
[29] Detamore, M.S. et al. (2003) Tensile properties of the porcine temporomandibular joint disc.
J. Biomech. Eng. 125, 558–565.
[30] del Pozo, R. et al. (2002) The regional difference of viscoelastic property of bovine temporo-
mandibular joint disc in compressive stress-relaxation. Med. Eng. Phys. 24, 165–171.
[31] Kim, K.W. et al. (2003) Biomechanical characterization of the superior joint space of the porcine
temporomandibular joint. Ann. Biomed. Eng. 31, 924–930.
[32] Berteretche, M.V. et al. (2001) Histologic changes associated with experimental partial anterior disc
displacement in the rabbit temporomandibular joint. J. Orofac. Pain 15, 306–319.
[33] Hinton, R. et al. (2002) Osteoarthritis: diagnosis and Therapeutic Considerations. Am. Family Phys.
65, 841–847.
[34] Feinberg, S.E. et al. (2001) Image-based biomimetic approach to reconstruction of the temporo-
mandibular joint. Cells Tissues Organs 169, 309–321.
[35] Temenoff, J.S. et al. (2004) Thermally cross-linked oligo(poly(ethylene glycol) fumarate) hydrogels
support osteogenic differentiation of encapsulated marrow stromal cells in vitro. Biomacromolecules
5, 5–10.
[36] Fisher, J.P. et al. (2004) Effect of biomaterial properties on bone healing in a rabbit tooth extraction
socket model. J. Biomed. Mater. Res. 68A, 428–438.
[37] Holland, T.A. et al. (2004) Transforming growth factor-beta1 release from oligo(poly(ethylene
glycol) fumarate) hydrogels in conditions that model the cartilage wound healing environment.
J. Controll. Release: Offic. J. Control. Release Soc. 94, 101–114.
[38] Chai, Y. et al. (2000) Fate of the mammalian cranial neural crest during tooth and mandibular
morphogenesis. Development 127, 1671–1679.
[39] Almarza, A.J. and Athanasiou, K. (2004) Seeding techniques and scaffolding choice for the tissue
engineering of the temporomandibular joint disc. Tissue Eng. 10, 1787–1795.
[40] Poshusta, A.K. and Anseth, K.S. (2001) Photopolymerized biomaterials for application in the
temporomandibular joint. Cells Tissues Organs 169, 272–278.
[41] Behravesh, E. et al. (2003) Three-dimensional culture of differentiating marrow stromal osteo-
blasts in biomimetic poly(propylene fumarate-co-ethylene glycol)-based macroporous hydrogels.
J. Biomed. Mater. Res. 66A, 698–706.
[42] Weng, Y. et al. (2001) Tissue-engineered composites of bone and cartilage for mandible con-
dylar reconstruction. J. Oral Maxillofac. Surg.: Offic. J. Am. Assoc. Oral Maxillofac. Surg. 59,
185–190.
[43] Roux, F.X. et al. (1988) Madreporic coral: a new bone graft substitute for cranial surgery. J.
Neurosurg. 69, 510–513.
mikos: “9026_c023” — 2007/4/9 — 15:52 — page 22 — #22
23-22 Tissue Engineering
[44] Lu, H.H. et al. (2003) Three-dimensional, bioactive, biodegradable, polymer-bioactive glass com-
posite scaffolds with improved mechanical properties support collagen synthesis and mineralization
of human osteoblast-like cells in vitro. J. Biomed. Mater. Res. 64A, 465–474.
[45] Ma, P.X. and Langer, R. (1999) Morphology and mechanical function of long-term in vitro
engineered cartilage. J. Biomed. Mater. Res. 44, 217–221.
mikos: “9026_c024” — 2007/4/9 — 15:52 — page1—#1
24
Engineering Smooth
Muscle
Yu Ching Yung
University of Michigan
David J. Mooney
University of Michigan
Harvard University
24.1 Introduction.............................................. 24-1
24.2 Cell Source ............................................... 24-2
Differentiated SMCs • Smooth Muscle Progenitor Cells •
Recruitment of SMCs
24.3 Extracellular Signaling................................... 24-4
24.4 Synthetic Extracellular Matrix .......................... 24-4
Self-Assembly • Polymer Scaffolds: Synthetic and Naturally
Derived
24.5 Engineered Smooth Muscle Tissues .................... 24-6
24.6 Conclusion/Future Directions .......................... 24-9
References ....................................................... 24-9
24.1 Introduction
Tissue engineering has emerged over the past two decades to address the growing need for biological
substitutes to restore or replace damaged tissues and organs [1]. Current approaches to organ repair rely
primarily on transplantation of whole or partial organs and tissues from autogeneic, allogeneic, and less
frequently, xenogeneic sources. The imbalance of need versus availability of organs poses as a significant
and inherent limitation to this method [2]. Tissue engineering promises an alternative via rebuilding
tissues or organs from targeted cell populations, often with the participation of matrices that guide tissue
regeneration while providing specific instructions with signaling molecules.
Diseases related to the malfunction of cardiovascular, gastrointestinal and urinary tissues account for
millions of deaths annually [1], and smooth muscle (SM) tissue has a critical role in the structure and
function of a number of these tissues. In blood vessels of the cardiovascular system, the smooth muscle
cell (SMC) component (medial layer) provides mechanical strength and elasticity. SM tissue plays a key
role in the gastrointestinal system through its ability to drive the transport of solids and liquids, and
malfunction of these tissues typically result in malnutrition. The SM in the intestinal tract, in contrast to
SM tissue in blood vessels, is organized in two layers of opposing orientation, and provides for propulsive
movements of food through peristalsis. The SM of the bladder also regulates the reservoir function of this
tissue, as it controls the storage and release of urine. In all of these tissues, the SMCs contain a highly
organized structure of actin and myosin filaments that allow the cells to efficiently modulate and respond
to a mechanically dynamic environment and regulate the operation of the organ. A functional smooth
24-1
mikos: “9026_c024” — 2007/4/9 — 15:52 — page2—#2
24-2 Tissue Engineering
muscle component will be critical to the success of engineered tissues intended to replace any of these
tissues or organs.
24.2 Cell Source
A critical question in the engineering of smooth muscle tissues is the appropriate source of the SMCs that
will comprise the tissue. The majority of research to date has utilized smooth muscle procured from the
tissue of interest. However, the isolation of smooth muscle progenitors may allow for a less invasive and
destructive approach. In addition, it may be possible to directly recruit SMCs to the site at which one
wants a tissue to form.
24.2.1 Differentiated SMCs
The most direct approach to form smooth muscle tissues is to utilize SMCs obtained from the tissue
that one desires to engineer. In this approach, smooth muscle containing tissue is typically explanted
and dissociated into individual cells. The cells are then directly transplanted or expanded in culture, and
subsequently transplanted (Figure 24.1a,b). Direct transplantation may be advantageous as it bypasses
in vitro culturing, which can alter the contractile phenotype of SMCs. In contrast, culture of SMCs prior
to transplantation may lead to phenotypic changes [3,4], but this approach allows one to greatly expand
the cell population. This may allow a relatively small explant to ultimately yield sufficient cells to engineer
a large tissue. The phenotypic changes noted in SMCs, as they revert to a synthetic phenotype [5] may be
reversed or prevented through appropriate culture conditions (i.e., cyclic mechanical loading) [6].
Although smooth muscle tissues characteristically contain contractile apparatus and form the muscular
components of visceral structures, there are differences between SM in various tissues [7]. These likely
relate to the specific microenvironment and physiology of each tissue type. For this reason, SM biopsies
are typically procured for the specific type of tissue being engineered. The artery is the most commonly
excised tissue for vascular regeneration [8–11] primarily because it is the largest blood vessel, and hence
contains the thickest medial layer. Current methods for bladder replacement require a biopsy to obtain
EC/SMC/progenitors
Cell expansion
scaffold
(a)
(b)
(c)
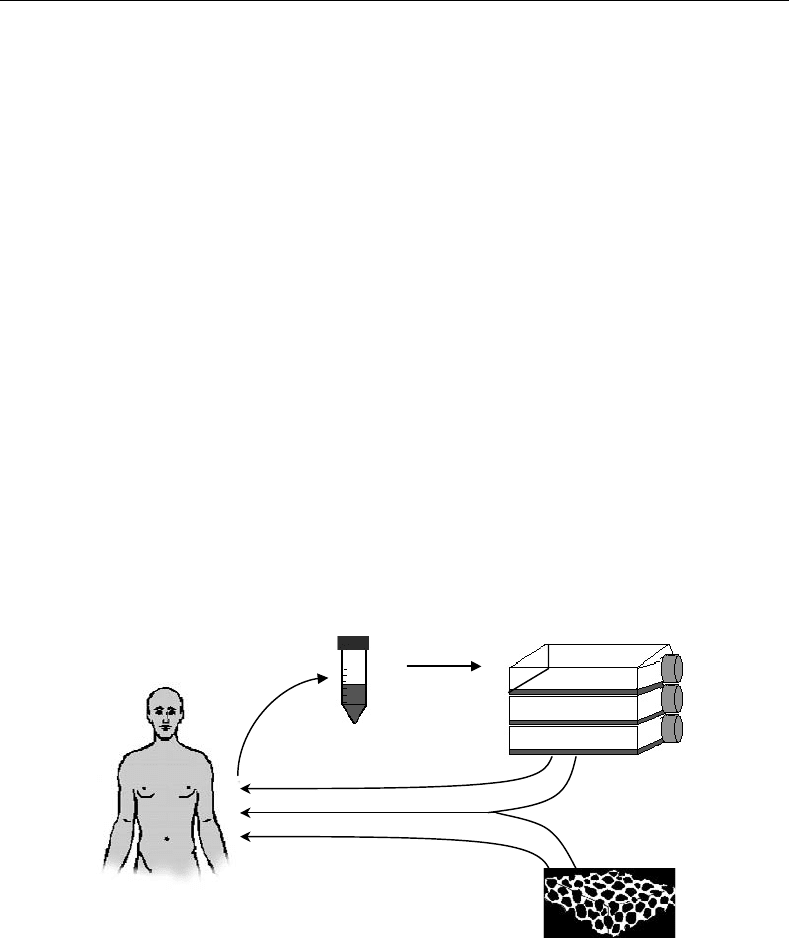
FIGURE 24.1 Scheme of approaches to engineer SM tissue. (a) The direct cell transplantation approach first involves
the procurement of the appropriate cell types for the tissue of interest (e.g., EC, SM, or progenitor cells). The cells are
typically expanded in culture, and induced to differentiateinto SMCs beforeimplantation if necessary. (b)Alternatively,
the expanded cells may be seeded onto a scaffold, and subsequently implanted as a cell–matrix construct. (c) Third,
acellular matrices may be implanted without seeded cells, and in this situation one relies on the recruitment of
neighboring SMCs or progenitors to infiltrate scaffold and form the new SM tissue.
mikos: “9026_c024” — 2007/4/9 — 15:52 — page3—#3
Engineering Smooth Muscle 24-3
a small specimen of the donor or host bladder tissue, which is then used to expand separate cultures
of urothelial and SMCs [12]. Ureter or renal pelvis cells can be similarly harvested. Regeneration of
gastrointestinal organs, specifically the stomach and the intestine, has most commonly utilized organoid
units which contain SM precursors [13,14].
Differentiated SMCs have shown tremendous utility for the successful regeneration of SM tissues.
However the invasive nature of this cell procurement, the inherent limited proliferation capability of
primary cells, and maintenance of smooth muscle phenotype are all limitations to this cell source.
24.2.2 Smooth Muscle Progenitor Cells
Smooth muscle progenitors may potentially be isolated using minimally invasive techniques, and sub-
sequently induced to differentiate down a smooth muscle lineage. Cells isolated from bone marrow are
termed bone marrow stromal cells (BMSCs), or mesenchymal stem cells (MSCs) depending on the mode
of cell purification selection in vitro.
Bone marrow can be obtained easily from the medullary canals of long bones or the cancellous cavities
[15], and the resultant BMSC can be readily expanded in culture. BMSCs have demonstrated the ability to
differentiate into multiple mesenchymal cell lineages, and offer an alternative source of SMCs [7,16–23].
Recent studies have shown that BMSCs are inducible down a smooth muscle pathway, and this process
is regulated by an interplay between stimulatory molecules [24,25], with TGF-β and PDGF as the main
modulators [24]. Mechanical stimulation has also been shown to effect differentiation of bone marrow
stromal cells [26]. However, the mechanism of this effect is still unclear. SM progenitors can also be
derived from embryonic stem cells [27,28], circulating blood [29,30], bone marrow [31,32], and other
tissues [33].
24.2.3 Recruitment of SMCs
The recruitment of SMCs or progenitors from a surrounding tissue to an engineered tissue provides an
alternative to SM transplantation (Figure 24.1c). Signaling molecules such as PDGF and TGF-β have
chemotactic effects on SMCs [34], and growth factors (Figure 24.2) released by endothelial cells (ECs)
can also induce the migration of MSCs and their subsequent differentiation into SM like cells [35,36].
Similarly, myoblast recruitment can be modulated by a gradient of a chemotactic agent [37]. This recruit-
ment approach greatly simplifies the process of SM tissue engineering, as it eliminates the isolation and
expansion of cells in vitro. In addition, this approach could have utility in applications such as blood
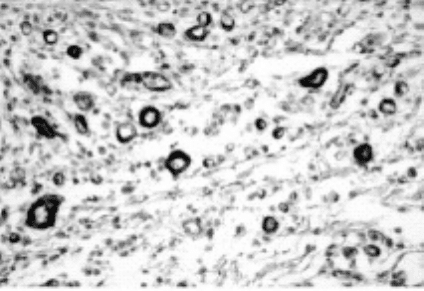
FIGURE 24.2 Sustained and localized delivery of PDGF can lead to the recruitment of SMCs to nascent blood vessels.
Photomicrograph of tissue section stained using standard immunohistochemical techniques to detect (brown stain)
cells containing α-SMA (SMCs) associating with blood vessels. (Photomicrograph was taken from Richardson, T.P.
et al., Nat. Biotechnol., 2001, 19: 1029–1034 used with permission from the Nature Publishing Group.)

mikos: “9026_c024” — 2007/4/9 — 15:52 — page4—#4
24-4 Tissue Engineering
vessel repair where direct placement of smooth cells in the lumen could cause a thrombogenic effect. The
use of signaling molecules to recruit circulating progenitor cells may provide a useful alternative in this
situation.
24.3 Extracellular Signaling
The extracellular environment plays a pivotal role in SM tissue engineering by providing instructions to the
SMCs. Both signaling molecules and mechanical stimuli similar to that found in the native extracellular
environment of SM tissues may be used to induce specific SM responses.
Mitogenic factors that have shown to possess a significant effect on SMCs in culture include platelet
derived growth factor (PDGF), TGF-β, angiopoietin, and to a lesser extent, heparin-binding epidermal
growth factor (HB-EGF) and fibroblast growth factor-2 (FGF-2) [38,39]. PDGF has been shown to have
potent effects on proliferation, migration, and matrix production by SMCs [27,28,34,35,37,40–42] and
potentially has a significant role in cell transplantation where SMC proliferation is necessary. An increase
in the synthesis of SM extracellular proteins is stimulated by TGF-β and these matrix components provide
mechanical integrity to engineered SM tissues [34,36,43–48]. Particularly in strategies where SM recruit-
ment is important, angiopoietin and HB–EGF have both shown to mediate EC and SMC interactions
[39,49–51]. However, SM tissue engineering strategies that utilize growth factors must consider the mode
of delivery. Polymeric encapsulation of growth factors is a common approach to deliver the molecules to
the developing SM tissues in a controlled and sustained manner [52].
Mechanical signals modulate the phenotype of SMCs [40,53,54] and enhance the development and
function of engineered tissues [55–57]. Cyclic mechanical strain of engineered SM tissues [53,56] result
in an increase of matrix production and increased mechanical strength. These mechanical signals are
transmitted intracellularly though various signaling pathways that initiate at the transmembrane receptors
known as integrins [58], which link the extracellular matrix to the cytoskeleton [59,60]. Integrins activate
mitogen activated protein kinase (MAPK) cascades via signaling through extracellular signal-regulated
kinase (ERK) [60–63], either through focal adhesion kinases (FAKs) or through coactivation of growth
factor receptors (GFRs). Cyclic mechanical strain increases levels of focal contact components [64], which
may increase integrin clustering [61], and provide a potential mechanism for the role of mechanical
signals in activation of FAKs. It is currently unclear whether these pathways act synergistically with
growth factor stimulation, but optimal development and function of engineered SM tissues will likely
require appropriate chemical and mechanical signals.
24.4 Synthetic Extracellular Matrix
Tissue engineering utilizes synthetic extracellular matrices (ECMs) to provide an infrastructure for the
formation of tissues by providing a predefined space to localize tissue growth and the mechanical support
necessary to facilitate this growth. Synthetic ECMs may also provide specific signals to the SMCs. Two
general designs of synthetic ECMs for SM tissue regeneration are being pursued, one involving a biological
approach where the matrix is assembled by the resident cells and the other utilizing predefined polymeric
structures.
24.4.1 Self-Assembly
SMCs maintained for extended times in culture will synthesize, secrete, and assemble an ECM with
sufficient mechanical integrity to allow a sheet of confluent SMCs to be manipulated and formed into
a three-dimensional tissue [65]. This technique is attractive for tissue engineering because it eliminates the
need for exogenous biomaterials, and thereby eradicates any potential inflammatory issues related to the
material [66,67]. Self-assembly approaches have focused on engineering vascular grafts by individually
culturing cellular sheets to model the defined layers of the blood vessel. A sheet of SMCs is used to
mikos: “9026_c024” — 2007/4/9 — 15:52 — page5—#5
Engineering Smooth Muscle 24-5
form the medial layer, which is subsequently wrapped with a sheet composed of fibroblasts to form the
adventitial layer, and finally seeded with endothelial cells to create the lumen. Initial studies on tissues
formed utilizing this approach reported poor mechanical strength [68,69], which is indicative of a deficient
medial and, or adventitial layers. A revised approach increased the mechanical strength of tissues formed
with this approach [65]. However, a limitation to this approach is the extensive time required to form the
cellular sheets.
24.4.2 Polymer Scaffolds: Synthetic and Naturally Derived
Most approaches to engineer SM tissues have utilized three-dimensional, biodegradable polymeric scaf-
folds. Polymeric scaffolds formed from exogenous biomaterials provide mechanical stability and can
deliver signaling molecules or adhesion peptides to induce appropriate tissue development. These poly-
meric biomaterials are fabricated from either synthetic or naturally derived materials. Synthetic polymers
typically used for engineering SM tissues include several forms of polyesters, elastomeric polymers, and
hydrogels. The most common used naturally derived polymer used to engineer SMC is type I collagen.
24.4.2.1 Synthetic Polymers
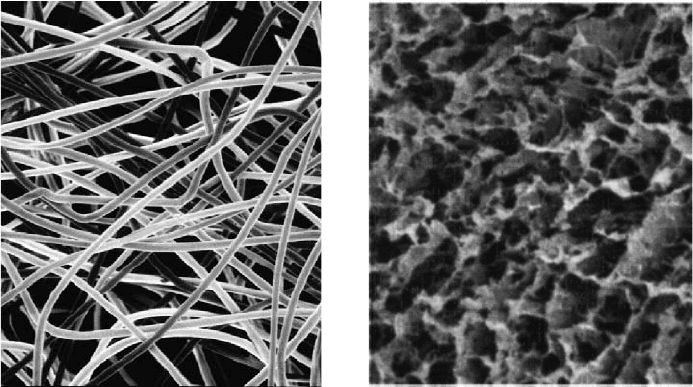
The most prevalent synthetic polymers used to engineer smooth muscle tissues are the polyesters
poly(glycolic acid) (PGA) (Figure 24.3a), poly(l-lactic acid) (PLLA), and poly (lactic-co-glycolic acid)
(PLGA). Advantageous features of these polymers include their reproducible and readily altered mech-
anical properties and degradation rates [70,71]. These polymer scaffolds provide temporary mechanical
support [72] sufficient to resist cellular contractile forces in vitro [73–76], and scaffolds exhibiting par-
tial elastic properties under cyclic strain enabled induction of a more contractile, differentiated smooth
muscle phenotype from attached SMCs [56]. In addition to structural stability, appropriate signals may
be required to guide the development of smooth muscle tissues. Synthetic polymers can be modified
to incorporate signals to alter cellular function, including cell adhesion molecules [77–79] and growth
factors [80,81].
Hydrogel forming polymers have also been investigated for engineering SM tissues. Polyethylene glycol
(PEG) hydrogels intrinsically resist protein adsorption and cell adhesion [82] and this characteristic
(a)
(b)
FIGURE 24.3 Scanning electron photomicrographs of typical polymeric scaffolds utilized for engineering SM tissue.
(a) PGA fiber based scaffold, and (b) type I collagen scaffold. (Photomicrograph was taken from Kim, B.S. and
D.J. Mooney, J. Biomech. Eng., 2000, 122: 210–215; Kim, B.S. and D.J. Mooney, J. Biomed. Mater. Res., 1998, 41:
322–332, and used with permission from John Wiley & Sons and ASME, respectively.)
