Cui Dongmei. Atlas of Histology: with functional and clinical correlations. 1st ed
Подождите немного. Документ загружается.

CHAPTER 18
■
Male Reproductive System
365
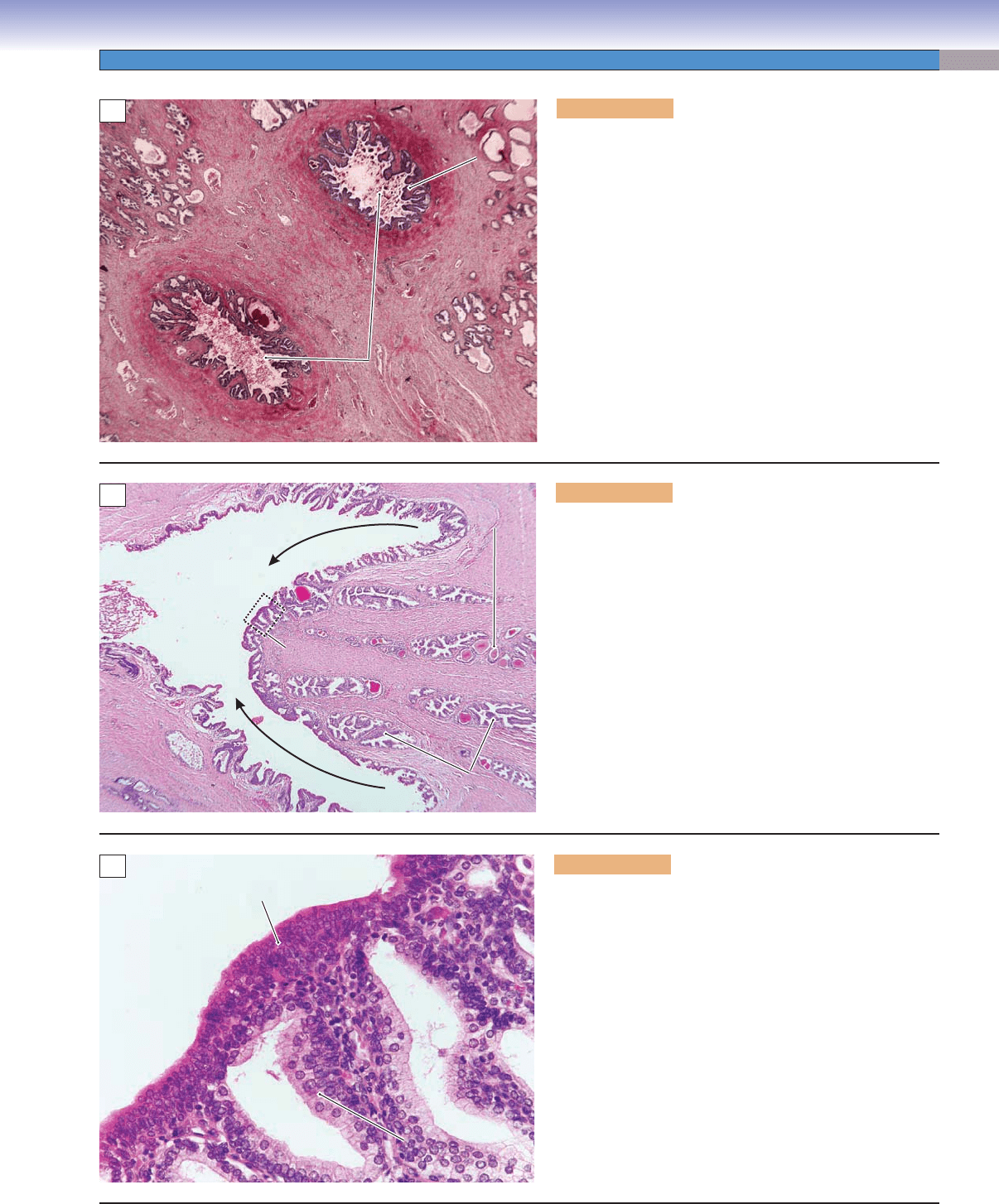
Figure 18-19A. Ejaculatory duct, prostate gland. H&E,
11
The ampulla of the ductus deferens continues after it joins
with the duct of the seminal vesicle to form the ejaculatory
duct. The two ejaculatory ducts pass through the prostate
gland to join with the urethra. Each ejaculatory duct is a
short, straight tube (1–2 cm in length) and has a thin wall
lined by pseudostratifi ed (or simple) columnar epithelium
and supported by connective tissue. Smooth muscle is pres-
ent in the initial segment but disappears in most of the
ejaculatory ducts. Here is an example of the two ejacula-
tory ducts within the prostate gland, surrounded by large
amounts of connective tissue. The mucosa forms many folds
extending into the lumen. The lumen may contain prostatic
concretions (secretory material of the prostatic gland and
often seen in older male patients).
Fold of the
Fold of the
mucosa
mucosa
Fold of the
mucosa
Connective tissue
Connective tissue
Connective tissue
Prostate
Prostate
gland
gland
Prostate
gland
Prostate
Prostate
gland
gland
Prostate
gland
Ejaculatory ducts
Ejaculatory ducts
Ejaculatory ducts
A
Ejaculatory duct
Prostatic
urethra
Fig. 18-19C
Prostate
Prostate
gland
gland
Prostate
gland
Ejaculatory duct
Prostatic
Prostatic
concretion
concretion
Prostatic
concretion
B
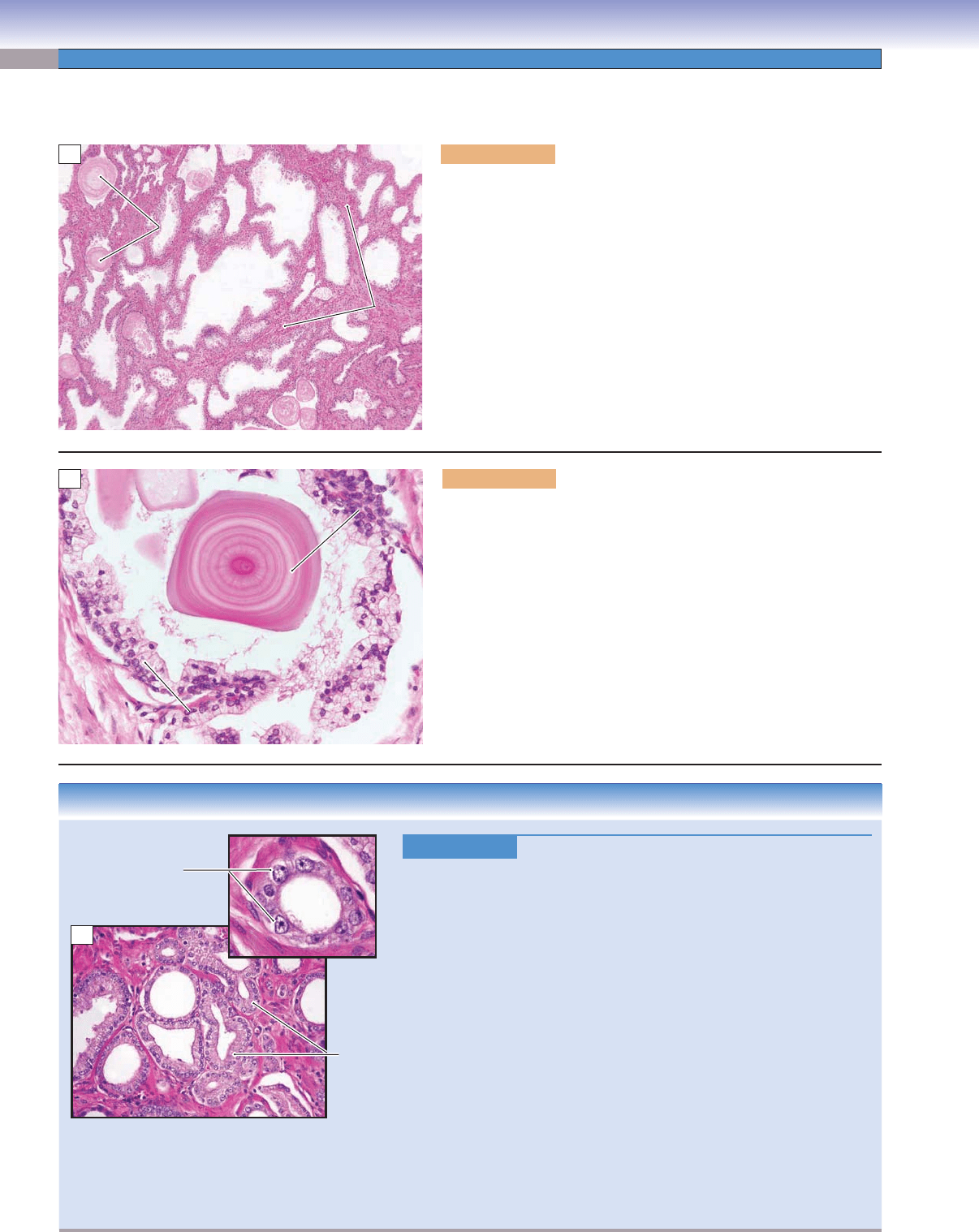
Figure 18-19B. Ejaculatory duct, prostate gland. H&E,
34
The ejaculatory ducts penetrate the prostate gland and open
into the prostatic urethra, at the seminal colliculus (also
called the verumontanum), on the posterior wall of the pro-
static urethra. This portion of the urethra has thick mucosa
and shallow folds as shown here. The function of the ejacu-
latory ducts is to transport spermatozoa and seminal fl uid
into the prostatic urethra. The urethra includes three parts:
the prostatic urethra (proximal part, near the bladder), the
membranous urethra (intermediate part), and the penile
(spongy) urethra (distal part). Prostatic concretions, also
called corpora amylacea, are present in the lumen of the
prostate gland shown here (Fig. 18-20B).
Transitional
epithelium
Prostatic
urethra
Duct of prostate gland
Simple columnar
Simple columnar
epithelium
epithelium
Simple columnar
epithelium
Duct of prostate gland
C
Figure 18-19C. Epithelium of the prostatic urethra. H&E,
272
Where the two ejaculatory ducts merge with the prostatic
urethra, the epithelium changes from simple or pseudostrati-
fi ed columnar to the transitional epithelium that is character-
istic of the urinary system. Here is an example of prostatic
urethral epithelium at higher magnifi cation; it is taken from
the dashed box indicated in Figure 18-19B. The epithelium
of the duct of the prostate gland is simple columnar epithe-
lium with round nuclei. The prostatic secretions are delivered
into the prostatic urethra through numerous small ducts of
the prostate gland.
CUI_Chap18.indd 365 6/2/2010 7:39:03 PM
366
UNIT 3
■
Organ Systems
Accessory Genital Glands
Stroma
Stroma
Stroma
Lumen
Lumen
Lumen
Prostatic
Prostatic
concretions
concretions
Prostatic
concretions
A
Prostatic concretion
Prostatic concretion
(corpora amylacea)
(corpora amylacea)
Prostatic concretion
(corpora amylacea)
Lumen of the
Lumen of the
prostate gland
prostate gland
Lumen of the
prostate gland
Connective
Connective
tissue
tissue
Connective
tissue
Columnar
Columnar
epithelium
epithelium
Columnar
epithelium
B
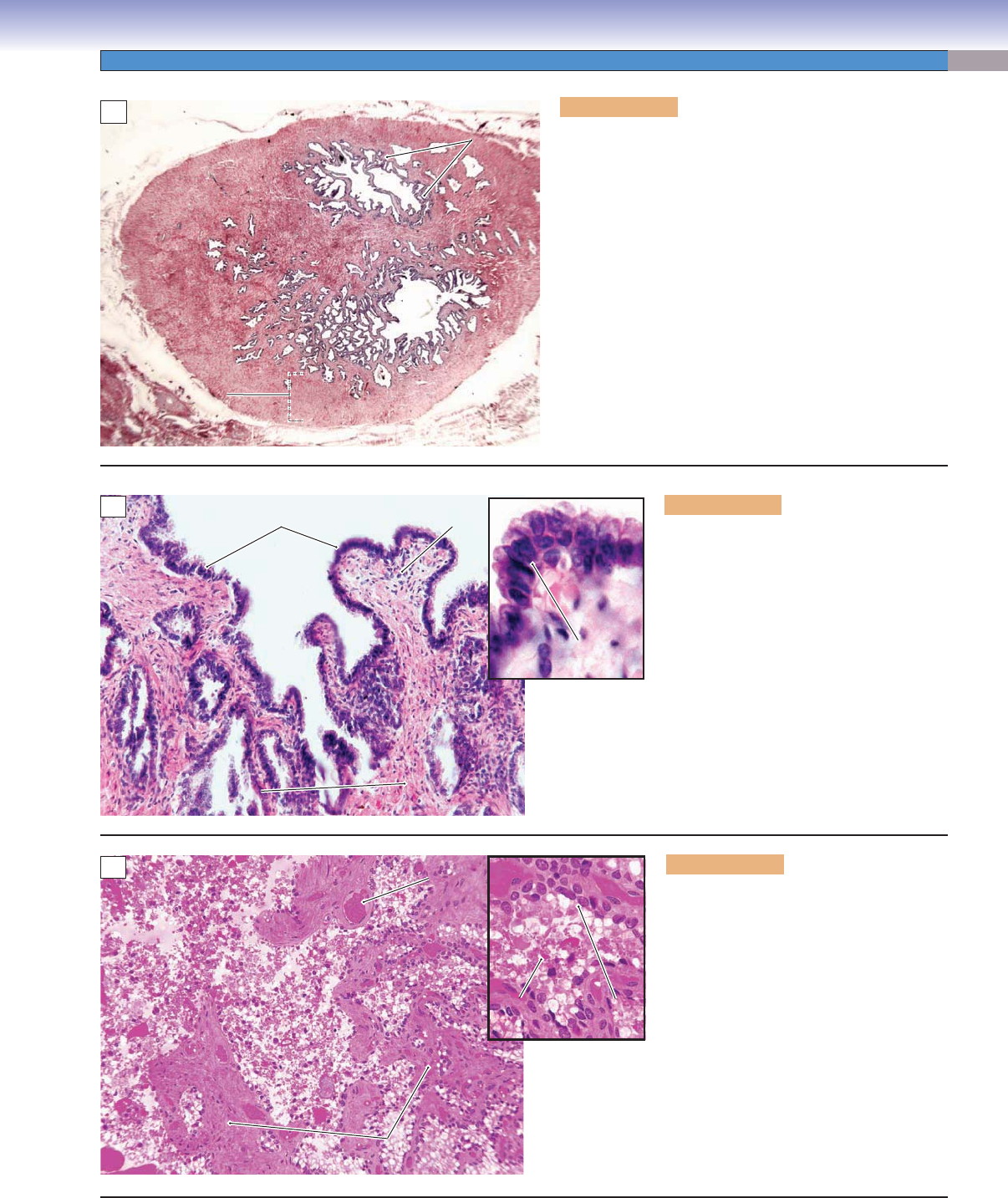
Figure 18-20A. Prostate gland. H&E, 34
The prostate gland is similar to a chestnut in size and shape. It
surrounds the initial portion of the urinary urethra (prostatic urethra)
where the urethra exits the bladder. The prostate gland is penetrated
by two ejaculatory ducts and the urethra (Fig. 18-19A–C). It contains
many (about 30–50) highly branched tubuloalveolar glands (com-
pound tubuloalveolar glands). Each gland has a duct that empties its
products into the prostatic urethra. The mucosa of the prostate gland
is highly folded and is lined by simple columnar epithelium, which is
supported by a stroma (thin layer of connective tissue strands with
many smooth muscle cells). Here is an example of the prostate gland
with its characteristically irregular lumen that may contain prostatic
concretions. These concretions are also known as corpora amylacea
and are more prominent in older men; they are composed of material
secreted by the prostate gland.
Figure 18-20B. Prostate gland. H&E, 272
A lumen in the prostate gland is shown housing a prostatic concretion
(corpora amylacea). This is composed of calcifi ed prostatic secretions
that typically display concentric rings. These structures increase in
number with age. The secretion of the prostate gland contains prote-
olytic enzymes, acid phosphatase, citric acid, fi brinolysin, and lipids.
The epithelial cells are columnar in shape with basally located round
nuclei. The prostate gland produces secretions that empty into the ure-
thra to mix with spermatozoa and seminal vesicle fl uid to form semen.
The prostatic secretion plays important roles in liquefying the coagu-
lated semen, helping to expel the spermatozoa, and increasing their
motility and survival rate after the semen has been transported into the
female reproductive tract.
CLINICAL CORRELATION
Figure 18-20C.
Prostate Cancer. H&E, 96; inset 164
Prostate cancer is the most common cancer in men and typically affects
men over the age of 50 years. It can be seen in younger men but is unusual
before the age of 40. The etiology of prostate cancer is elusive, but known
risk factors include a positive family history
, African American race,
androgenic hormonal infl uences, and environmental factors. The major-
ity of prostate cancers are adenocarcinomas arising from the glandular
component of the prostate. Patients may present with urinary symptoms,
such as diffi culty initiating or stopping the urine stream, or dysuria (pain
on urination). Other patients may fi rst present with bone pain due to
advanced metastatic disease. Many patients are diagnosed with prostate
cancer through screening programs utilizing the digital rectal exam and
the serum prostate-specifi c antigen (PSA) test, and a needle biopsy if indi-
cated. Histologically, the appearance of prostate cancer is highly varied,
from well-formed tubular structures to individual infi ltrating malignant
cells. Prostate cancers are graded histologically on the Gleason system,
from 1 (well differentiated) to 5 (poorly differentiated). Treatment of pros-
tate cancer may involve chemotherapy, hormonal manipulation, radiation
therapy (external beam and radioactive implants), or radical prostatectomy.
For some patients, particularly the elderly, watchful waiting may be a rea-
sonable alternative.
Note the prominent
nucleoli (malignant cells)
Prostate
cancer
C
CUI_Chap18.indd 366 6/2/2010 7:39:08 PM
CHAPTER 18
■
Male Reproductive System
367
Figure 18-21A. Seminal vesicles. H&E, 11
The seminal vesicles are paired glands that develop from
the ductus deferens. Each seminal vesicle consists of a
single highly convoluted tube with a duct that connects to
the terminal portion (ampulla) of the ductus deferens. The
ampulla of the ductus deferens is continuous with the ejacu-
latory duct. The mucosa of the seminal vesicles is extensively
branched and folded and lined mostly by pseudostratifi ed
columnar epithelium. The epithelium is supported by a thin
layer of connective tissue (lamina propria), and beneath
it is the muscularis composed of inner circular and outer
longitudinal smooth muscle. Contraction of the muscularis
pushes the seminal secretion into the ejaculatory duct during
ejaculation.
Folded
Folded
mucosa
mucosa
Folded
mucosa
Lumen
Lumen
Lumen
Lumen
Lumen
Lumen
Muscularis
Muscularis
Muscularis
A
Epithelium
Epithelium
Epithelium
Lamina propria
Lamina propria
Lamina propria
Pseudostratified
Pseudostratified
columnar epithelium
columnar epithelium
Pseudostratified
columnar epithelium
Smooth
Smooth
muscle
muscle
Smooth
muscle
B
Epithelial
Epithelial
cell
cell
Epithelial
cell
Seminal
Seminal
fluid
fluid
Seminal
fluid
Blood
Blood
vessel
vessel
Blood
vessel
Seminal
Seminal
fluid
fluid
Seminal
fluid
Seminal
Seminal
fluid
fluid
Seminal
fluid
Mucosa
Mucosa
Mucosa
C
Figure 18-21B. Seminal vesicle. H&E,
278; inset 635
This is an example of the mucosa of the
seminal vesicle. The nonciliated, pseu-
dostratifi ed columnar epithelium (inset),
underlying lamina propria, and some
smooth muscle fi bers are shown here. The
epithelium of the seminal vesicle varies from
simple to pseudostratifi ed columnar epithe-
lium. The mucosa appears branched and
folded. The epithelium contains basal cells
and secretory cells with abundant rough
endoplasmic reticulum and well-developed
Golgi complexes.
Figure 18-21C. Seminal vesicle with sem-
inal fl uid. H&E, 139; inset 328
The seminal vesicles produce large volumes
of seminal fl uid, which contributes about
70% of the volume of semen. Seminal fl uid
contains fructose and other sugars, prosta-
glandins, fl avins, phosphorylcholine, mucus,
vitamin C, and proteins. The fructose pro-
vides an energy source for sperm motility;
the fl avins, also known as lipochrome pig-
ment, add a yellowish color to the seminal
fl uid and have a strong fl uorescent quality
under the ultraviolet light. The inset shows
seminal epithelium and seminal fl uid (vis-
cous material) fi lling the lumen of a seminal
vesicle.
CUI_Chap18.indd 367 6/2/2010 7:39:12 PM
368
UNIT 3
■
Organ Systems
Penis
Dorsal
Dorsal
artery
artery
Dorsal
artery
Helicine artery
Helicine artery
Helicine artery
Superficial
Superficial
dorsal vein
dorsal vein
Superficial
dorsal vein
Deep
Deep
dorsal vein
dorsal vein
Deep
dorsal vein
Corpora
Corpora
cavernosa
cavernosa
Corpora
cavernosa
Corpora
Corpora
cavernosa
cavernosa
Corpora
cavernosa
Urethra
Urethra
Urethra
Urethra
Urethra
Urethra
Skin
Skin
Skin
Corpus
Corpus
spongiosum
spongiosum
Corpus
spongiosum
Tunica
Tunica
albuginea
albuginea
Tunica
albuginea
Erectile
Erectile
tissue
tissue
Erectile
tissue
Sinuses (vein)
Sinuses (vein)
Sinuses (vein)
Urethral glands
Urethral glands
(Littré glands)
(Littré glands)
Urethral glands
(Littré glands)
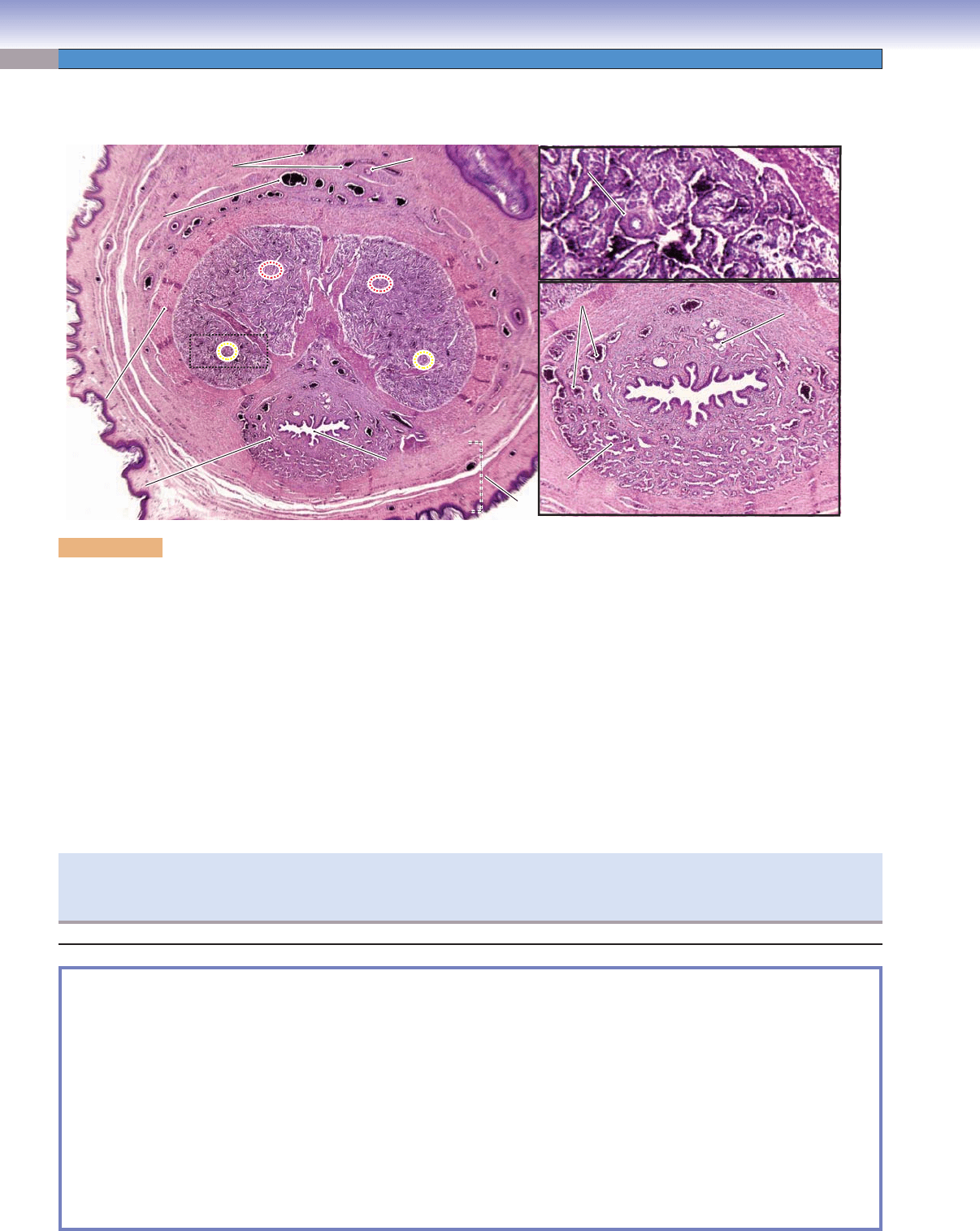
Figure 18-22. Overview of the penis. H&E, 13; inset (upper) 67; inset (lower) 26
The penis is composed of three cylinders of erectile tissue: the two corpora cavernosa and the corpus spongiosum as shown on the left.
Each cavernosa is surrounded by a tunica albuginea (thick and dense connective tissue); the corpus spongiosum is surrounded by a thin
layer of connective tissue with some smooth muscle fi bers. The penile (spongy) urethra is enclosed in the center of the corpus spongiosum
and extends into the terminal end (glans) of the penis. Each cylinder contains erectile tissue composed of a trabecular network of veins
(sinuses) surrounded by collagen, elastic fi bers, and smooth muscle cells. The three cylinders, with their tunica albuginea, are surrounded
by hairless thin skin containing arteries, veins, nerves, and connective tissue and covered by stratifi ed squamous epithelium. The two red
circles indicate the position of the deep arteries; the yellow circles indicate the position of the helicine arteries in the corpora cavernosa.
The penis is supplied by the dorsal arteries, and blood drains into the dorsal veins. A special blood vessel arrangement called
an arteriovenous (A-V) shunt allows blood to fl ow directly from arteries to veins. In the erect state, the arteriovenous shunt closes,
which results in blood being forced from the helicine arteries into the sinuses (cavernous spaces) in the erectile tissue (right upper
inset). Dilation of the sinuses produces penile erection. Erection is activated by parasympathetic stimulation through the spinal
nerves and the sacral parasympathetic preganglionic motor neurons in the spinal cord (S2–S4). The right lower photomicrograph
shows the penile urethra surrounded by erectile tissue and sinuses (veins) fi lled with blood. The urethral glands (Littré glands) are
mucous glands in the submucosa of the penile urethra, also called paraurethral (periurethral) glands. The secretion of the urethral
glands lubricates the urethra and contributes to the semen during ejaculation.
A clinical condition called erectile dysfunction is characterized by the inability to produce or maintain an erection of the penis. This
happens due to insuffi ciency of dilation of the sinuses in the erectile tissue. The causes are varied, including hormonal disorders,
neurological problems, hypertension, psychological factors, smoking, and alcohol use.
SYNOPSIS 18-3 Clinical and Pathological Terms for the Male Reproductive System
IGCN ■ : Noninvasive intratubular or in situ lesions within the seminiferous tubules that give rise to the majority of adult germ
cell tumors of the testis; IGCN is often found adjacent to testicular germ cell tumors on histologic examination (Fig. 18-15C).
Cryptorchidism
■ : Lack of, or incomplete, descent of a testis, from the abdominal cavity into the scrotum; the testis may
remain intra-abdominal or be found in the inguinal canal; an undescended testis is a risk factor for the development of
testicular tumors (Fig. 18-15C).
Gonadal dysgenesis
■ : Abnormal development of the gonads with resultant alterations in sexual development; gonadal dys-
genesis is a risk factor for the development of testicular tumors; the underdeveloped gonad is often referred to as a “streak
gonad” (Fig. 18-15C).
PSA
■ : A protein synthesized by prostatic epithelial cells; elevated serum PSA levels are associated with benign processes such
as benign prostatic hypertrophy as well as adenocarcinoma of the prostate; the PSA test is used as a screening test for prostate
cancer as well as a tumor marker in patients with a history of prostate cancer who have received treatment (Fig. 18-20C).
CUI_Chap18.indd 368 6/2/2010 7:39:17 PM
369
19
Female Reproductive
System
Introduction and Key Concepts for the Female Reproductive System
Figure 19-1 Overview of the Female Reproductive System
Figure 19-2 Orientation of Detailed Female Reproductive Organ Illustrations
Ovaries
Figure 19-3A Overview of the Ovary
Figure 19-3B Development of the Ovarian Follicle
Figure 19-4A,B Primordial Follicles, Ovary
Figure 19-5A,B Primary Follicles, Ovary
Figure 19-6A Secondary Follicles, Ovary
Figure 19-6B Graafi an Follicles, Ovary
Figure 19-7A Corpus Luteum, Ovary
Figure 19-7B Corpus Albicans, Ovary
Figure 19-7C Clinical Correlation: Granulosa Cell Tumor
Figure 19-8 Events of the Female Reproductive Cycle
Oviducts (Fallopian Tubes)
Figure 19-9A Oviduct (Fallopian Tube)
Figure 19-9B Epithelial Cells Lining the Oviduct
Uterus
Figure 19-10A Menstrual Phase of the Endometrium
Figure 19-10B Proliferative Phase of the Endometrium
Figure 19-10C Secretory Phase of the Endometrium
Figure 19-11A Implantation, Endometrium of the Uterus
Figure 19-11B Clinical Correlation: Endometrial Adenocarcinoma
Figure 19-11C Clinical Correlation: Uterine Leiomyoma
Figure 19-12A Cervix
Figure 19-12B Clinical Correlation: Cervical Cancer
CUI_Chap19.indd 369 6/19/2010 12:20:04 PM

370
UNIT 3
■
Organ Systems
Figure 19-13A Overview of the Placenta
Figure 19-13B Fetal Portion of the Placenta
Figure 19-14A Umbilical Cord
Vagina
Figure 19-14B Vagina
Mammary Glands
Figure 19-15A Overview of the Mammary Gland
Figure 19-15B Inactive (Resting) Mammary Gland
Figure 19-15C Active (During Pregnancy) Mammary Gland
Figure 19-16A Nipple, Mammary Gland
Figure 19-16B Clinical Correlation: Adenocarcinoma of the Breast (Breast Cancer)
Synopsis 19-1 Clinical and Pathological Terms for the Female Reproductive System
Introduction and Key Concepts for the
Female Reproductive System
The female reproductive system comprises the ovaries, oviducts,
uterus, vagina, external genitalia, and mammary glands.
The external genitalia (vulva) includes the labia minora, labia
majora, mons pubis, clitoris, and vestibule. Female secondary
sex characteristics appear at puberty, along with the monthly
menstrual cycle. This cycle of changes in the reproductive sys-
tem is infl uenced by interactions among the hypothalamus,
pituitary gland, ovaries, and uterus; related events occur peri-
odically during each menstrual cycle (Fig. 19-8). The menstrual
cycle is infl uenced by hormones including follicle-stimulating
hormone (FSH), luteinizing hormone (LH), estrogen, and
progesterone. These hormones cause changes in the female
reproductive organs and their functions, promote development
of follicles and oocytes, and produce an ideal environment
for fertilization, implantation, and fetal growth. The female
reproductive system plays an important role in the production
and regulation of female hormones (estrogen and progester-
one) and in the development and maintenance of female sex
characteristics.
Ovaries
The ovaries are paired, almond-shaped structures located in
the upper part of the pelvic cavity. Their size and position vary
depending on the age and reproductive state of the individual.
The ovaries are suspended by the mesovarium of the broad liga-
ment and are attached to the uterus by the ligament of the ovary
(Fig. 19-1). Each ovary has a cortex and medulla. The cortex
contains numerous developing follicles in various stages as
well as postovulatory structures, a corpus luteum, and several
corpora albicans. Each developing follicle contains an oocyte.
The medulla is composed of loose connective tissue and blood
vessels, nerve fi bers, and lymphatic vessels (Fig. 19-3A).
1. Primordial follicles: In the earliest stage of follicular
development, primordial follicles rest at the periphery of the
cortex. Each primordial follicle consists of a primary oocyte
surrounded by a single layer of squamous supporting cells
called follicular cells (Fig. 19-4A,B). The oocyte is small
(about 20–30 μm) and is in prophase (dictyotene) of meiosis
I. The nucleus of the oocyte has a pale appearance and
contains decondensed chromatin.
2. Primary follicles: At puberty, the primordial follicles begin
to grow, the oocyte increases its size, and the supporting
follicle cells also increase in size and become cuboidal
cells. These follicle cells are now called granulosa cells.
When the oocyte of the primary follicle is surrounded
by a single layer of granulosa cells, the follicle is called a
unilaminar primary follicle. As the oocyte increases in size,
the granulosa cells build up more layers, and the follicle is
called a multilaminar primary follicle (Fig. 19-5A,B). The
zona pellucida, a gel-like layer between the oocyte and the
granulosa cells, fi rst appears in the multilaminar primary
follicle (Fig. 19-5B).
3. Secondary follicles: As granulosa cells continue to prolifer-
ate, the follicle size increases, and spaces fi lled with follicular
fl uid (liquor folliculi) develop among the cells. These spaces
merge to become a single large space called the antrum. The
stromal cells that cover the follicle develop into a layer called
the theca folliculi. The theca folliculi is well developed in the
secondary follicle, and it includes the theca interna and theca
externa (Fig. 19-6A).
4. Graafi an
(preovulatory) follicle: In its fi
nal stage, the
follicle reaches a maximum size of up to 25 mm (2.5 cm).
This follicle has a large antrum fi lled with liquor folliculi.
It has reached its mature stage and is ready to release the
oocyte (ovulation). The oocyte has reached its maximum
size, and is embedded in a mound of granulosa cells that
protrude into the antrum (Fig. 19-6B). The granulosa cells
that are in immediate contact with the oocyte are called the
corona radiata and remain with the oocyte at ovulation.
The graafi an follicle bulges from the surface of the ovary. In
response to a sharp increase in the level of LH (LH surge),
the oocyte resumes meiotic division, becomes arrested as a
secondary oocyte, and ovulation then occurs.
CUI_Chap19.indd 370 6/19/2010 12:20:12 PM
CHAPTER 19
■
Female Reproductive System
371
5. Postovulatory structures: After ovulation, the remainder
of the graafi an follicle develops into the corpus luteum
(Fig. 19-7A) and continues to produce steroid hormones. If
fertilization and implantation occur, the corpus luteum will
remain active and continue to produce progesterone during
the fi rst 6 months of pregnancy. If fertilization does not
occur, the corpus luteum degenerates after 10 to 14 days and
becomes the corpus albicans (Fig. 19-7B).
Oviducts (Fallopian Tubes)
The oviducts are paired, muscular, open-ended tubes that receive
the ovum and provide an ideal environment for fertilization. Each
oviduct has four regions: the infundibulum, ampulla, isthmus,
and intramural portion (Fig. 19-1). Fertilization usually occurs in
the ampulla of the oviduct. The oviduct wall has a mucosa con-
taining ciliated cells and secretory (peg) cells in its epithelium, a
muscularis layer, and a serosa outer covering (Fig. 19-9A,B).
Uterus
The uterus is a pear-shaped muscular organ that connects
to the two oviducts and to the vagina via the cervix. It is
the site for implantation and placentation. Implantation
is the attachment of the blastocyst to the uterine wall; pla-
centation is the establishment of a placenta that nourishes
the developing embryo and fetus via the umbilical cord.
The uterus has a thick wall, which consists of endometrium
(mucosa), myometrium (muscularis), and serosa. The uterus
can be divided into three regions: the fundus, body, and cervix
(Fig. 19-1). The endometrium undergoes the following mor-
phological and functional changes during the menstrual cycle.
1. Menstrual phase: This is the initial stage (from days 1 to 4
of the cycle). The functional layer (functionalis) of the
endometrium sloughs off and bleeds about 2 weeks after
ovulation if fertilization does not occur (Fig. 19-10A).
2. Proliferative phase: Following the menstrual phase (days
5–14 of the cycle), the functionalis of the endometrium
recovers and rebuilds itself. Its glands appear straight, and
its surface is smooth (Fig. 19-10B).
3. Secretory phase: At this phase (days 15–28 of the cycle), the
endometrium becomes ready for implantation. The endo-
metrium thickens, and the glands appear coiled with large
lumens and a sawtooth appearance. These changes are mainly
infl uenced by progesterone (Fig. 19-10C). If a blastocyst becomes
embedded in the endometrium (implantation), the development
of the placenta takes place within a short time (Fig. 19-11A).
Vagina
The vagina is a muscular tube that connects the cervix to the
external genitalia. It consists of mucosa, muscularis, and adven-
titia (Fig. 19-14B) and functions as a copulatory organ and
birth passage.
Mammary Glands
The mammary glands are paired exocrine glands located
beneath the skin on the chest. These glands can be classifi ed as
compound tubuloalveolar glands. In the female, the mammary
glands undergo morphological and functional changes in response
to female hormones (estrogen, progesterone). In later pregnancy,
the mammary glands prepare to produce milk (lactation) for the
newborn infant (Figs. 19-15A–C and 19-16A).
CUI_Chap19.indd 371 6/19/2010 12:20:12 PM
372
UNIT 3
■
Organ Systems
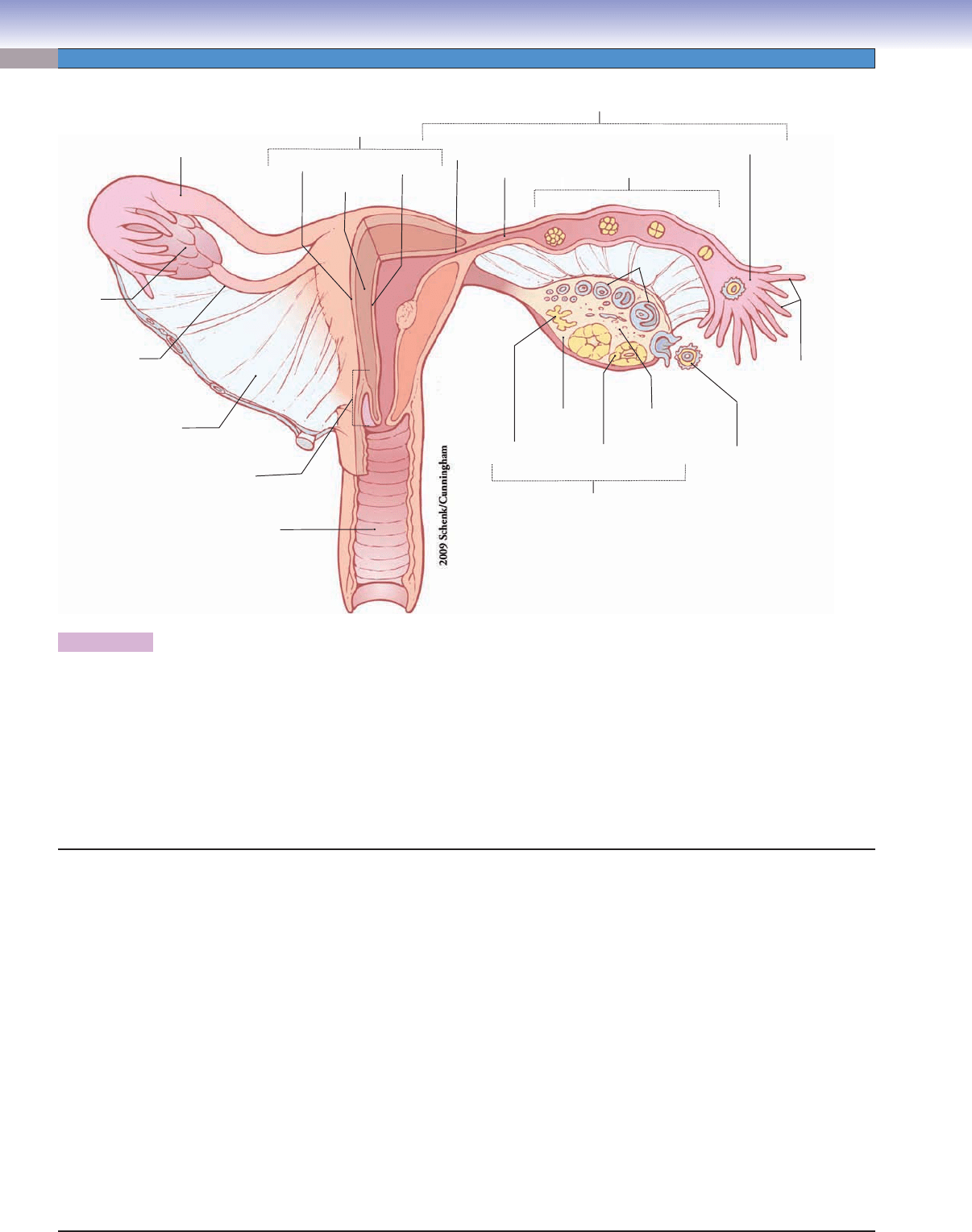
Figure 19-1. Overview of the female reproductive system.
The female reproductive system functions in reproduction and the secretion of female hormones that maintain female sex character-
istics. It consists of two ovaries, two oviducts, the uterus, the vagina, external genitalia, and two mammary glands. Each ovary has
a medulla and cortex that contain different stages of the developing follicles, corpus luteum, and corpus albicans. The oviduct is a
muscular tube, which captures and transports the ovulated oocyte and functions as the normal site of fertilization. It can be divided
into the infundibulum, ampulla, isthmus, and intramural portions. The uterus is a thick-walled chamber that can be divided into three
regions: the fundus, body, and cervix. The fundus and body of the uterus are composed of endometrium, myometrium, and serosa; the
endometrium undergoes extensive changes during the menstrual cycle. The mucosa of the cervix does not undergo structural changes
during the menstrual cycle; however, secretions of the mucosa change based on hormone levels during the menstrual cycle. Most of the
female organs undergo some degree of change during the menstrual cycle in response to changes in levels of various hormones.
Ovulated
oocyte
Fimbriae
Ovary
Corpus
albicans
Medulla
Cortex
Corpus
luteum
Follicles
Infundibulum
Isthmus
Intramural
portion
Ampulla
Oviduct (fallopian tube)
Uterus
Endometrium
Myometrium
Fundus
Oviduct (fallopian tube)
Ovary
Ligament
of ovary
Cervix
Vagina
Broad ligament
Body
Perimetrium
I. Ovaries
A. Cortex (contains ovarian follicles and connective tissue)
1. Primordial (resting) follicles
2. Primary (growing) follicles
3. Secondary (antral) follicles
4. Graafi an follicle
5. Corpus luteum (postovulatory structure)
6. Corpus albicans (postovulatory structure)
B. Medulla (contains loose connective tissue, blood vessels,
lymphatic vessels, and nerve fi bers)
II. Oviducts/fallopian tubes (contain mucosa, muscularis, and
serosa)
A. Infundibulum
B. Ampulla
C. Isthmus
D. Intramural portion
III. Uterus (contains endometrium, myometrium, and serosa)
A. Menstrual cycle
1. Proliferative phase
2. Secretory phase
3. Menstrual phase
IV. Cervix (contains mucosa, branched cervical glands, dense
connective tissue, and a few smooth muscle cells)
A. Internal os (opening of cervix)
B. Endocervical canal (portion between uterus and
external os)
C. External os (opening of ectocervix)
D. Ectocervix (portion that projects into the vagina)
V. Vagina (contains mucosa, muscularis, and adventitia)
VI. Mammary gland
A. Compound tubuloalveolar glands
B. Lactiferous sinuses
C. Lactiferous ducts
D. Nipple
Structures of the Female Reproductive System
CUI_Chap19.indd 372 6/19/2010 12:20:12 PM
CHAPTER 19
■
Female Reproductive System
373
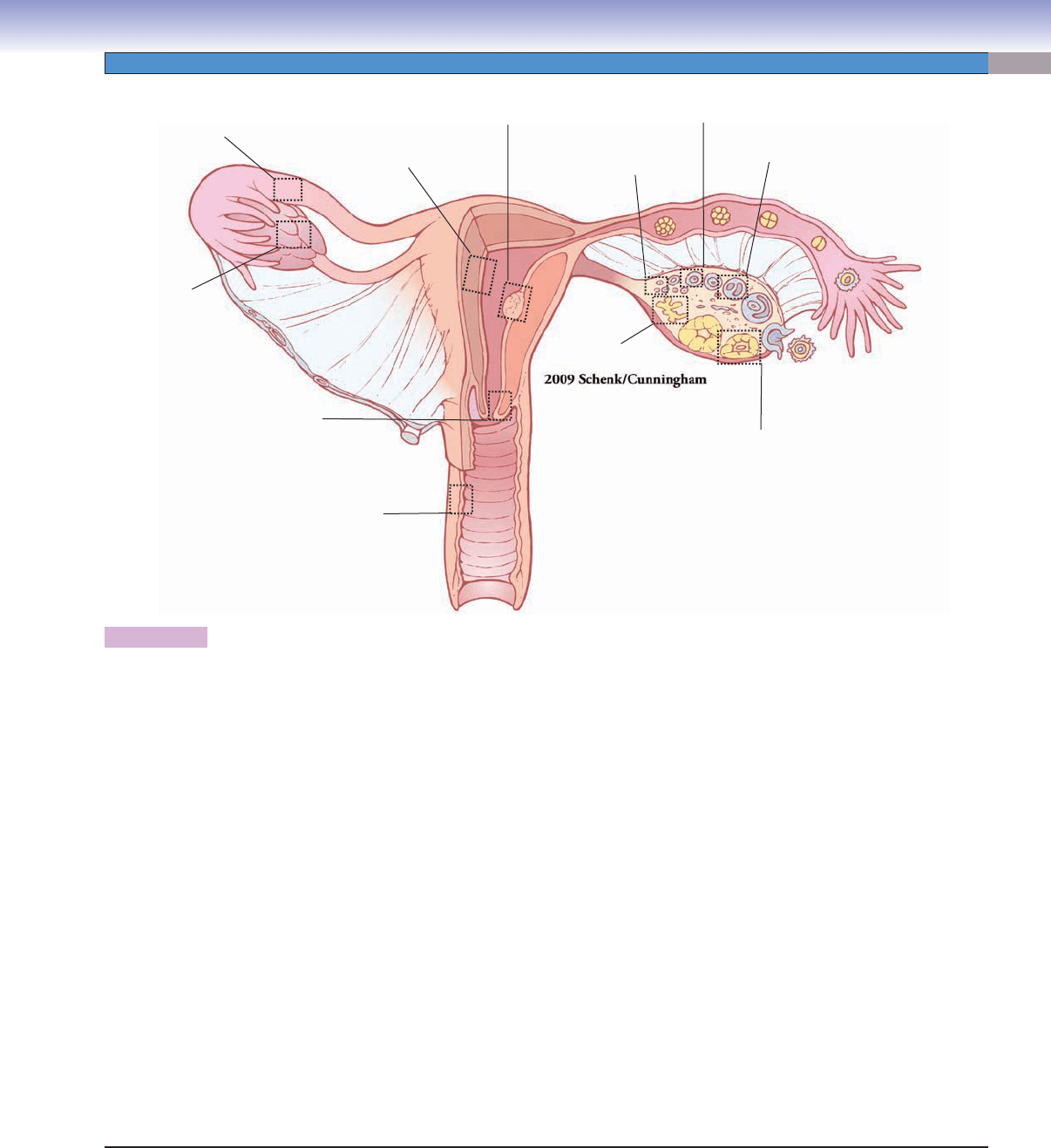
Figure 19-2. Orientation of detailed female reproductive system illustrations.
Fig. 19-5A,B
Fig. 19-6A
Fig. 19-7A
Fig. 19-7B
Fig. 19-4A,B
Fig. 19-10A,B,C
Fig. 19-11A
Fig. 19-3A
to Fig. 19-7B
Fig. 19-9A,B
Fig. 19- 14B
Fig. 19-12A
Ovaries
Figure 19-3A
Figure 19-3B
Figure 19-4A
Figure 19-4B
Figure 19-5A
Figure 19-5B
Figure 19-6A
Figure 19-6B
Figure 19-7A
Figure 19-7B
Figure 19-7C
Oviducts (Fallopian tubes)
Figure 19-9A
Figure 19-9B
Uterus
Figure 19-10A
Figure 19-10B
Figure 19-10C
Figure 19-11A
Figure 19-11B
Figure 19-11C
Cervix
Figure 19-12A
Figure 19-12B
Placenta
Figure 19-13A
Figure 19-13B
Umbilical cord
Figure 19-14A
Vagina
Figure 19-14B
Mammary glands
Figure 19-15A
Figure 19-15B
Figure 19-15C
Figure 19-16A
Figure 19-16B
Structures of the Female Reproductive System
CUI_Chap19.indd 373 6/19/2010 12:20:13 PM
374
UNIT 3
■
Organ Systems
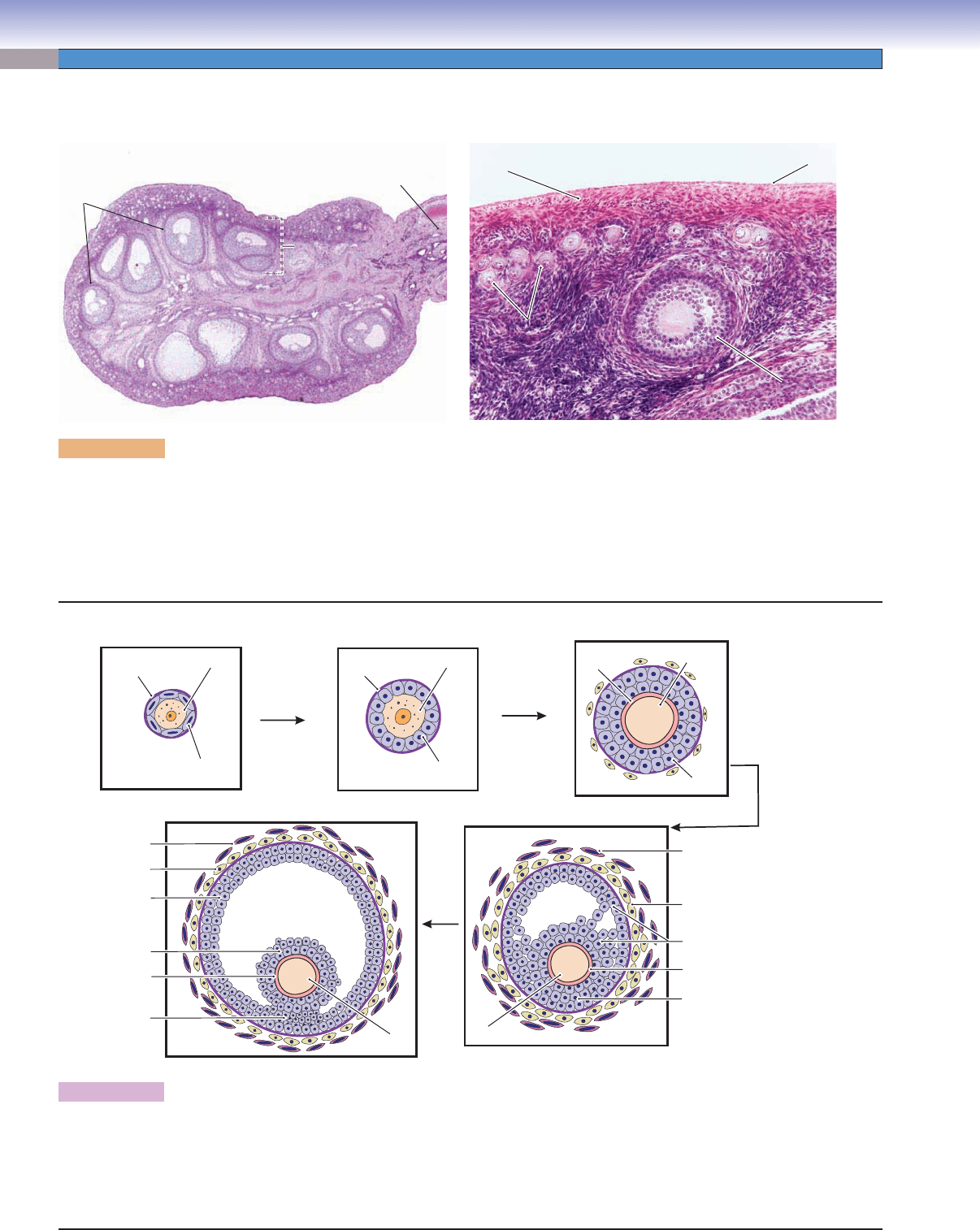
Figure 19-3A. Overview of the ovary. H&E, left 17; right 129
The ovaries are paired organs covered by a simple, usually cuboidal, mesothelium (sometimes called germinal epithelium) and a
tunica albuginea (connective tissue). Each ovary is divided into a cortex and a medulla. The cortex contains various stages of fol-
licles including primordial follicles, primary follicles, secondary follicles, and, occasionally, graafi an follicles. It may also contain the
corpus luteum, a temporary endocrine gland formed by components of an ovulated follicle. A degenerated corpus luteum persists
in the ovary as the corpus albicans. Most follicles degenerate (undergo atresia) before ovulation and are then called atretic follicles.
The medulla contains connective tissue with blood vessels, nerve fi bers, and lymphatic vessels.
Ligament
of ovary
Germinal epithelium
Germinal epithelium
Germinal epithelium
Tunica albuginea
Tunica albuginea
Tunica albuginea
Primordial
Primordial
follicle
follicle
Primordial
follicle
Primary follicle
Primary follicle
(multilaminar)
(multilaminar)
Primary follicle
(multilaminar)
Medulla
Medulla
Medulla
Secondary
follicles
Cortex
Cortex
Cortex
A
D.Cui
D.Cui
Theca interna
Granulosa cells
Corona radiata
(granulosa cells)
Cumulus
oophorus
Zona pellucida
Theca externa
Theca interna
Granulosa cells
Granulosa cells
Zona pellucida
Theca externa
Oocyte (1°–2°)
Oocyte (1 )
o
Antrum
Antrum
Antrum
Antrum
Antrum
Antrum
Graafian follicle
Secondary follicle
Granulosa cell
Follicular
(squamous) cell
Granulosa
(cuboidal)cell
Primordial follicle
Primary follicle (unilaminar)
Primary follicle (multilaminar)
Basement
membrane
Basement
membrane
Oocyte (1 )
o
Oocyte (1 )
o
Oocyte (1 )
o
Zona
pellucida
B
Figure 19-3B. Development of the ovarian follicles.
This illustration shows ovarian follicles from early to late stages: the primordial (resting) follicle, the unilaminar primary follicle, the multi-
laminar primary (growing) follicle, the secondary (antral or vesicular) follicle, and the graafi an (preovulatory) follicle. Each of these follicles
contains a primary (1
0
) oocyte, which is an immature ovum. A secondary oocyte is formed shortly before ovulation, when the oocyte com-
pletes the fi rst meiotic division. The secondary oocyte does not undergo the second meiotic division unless fertilization occurs. Note that the
follicles are not drawn to scale; a graafi an (preovulatory) follicle is approximately 1,000 times the diameter of a primordial follicle.
Ovaries
CUI_Chap19.indd 374 6/19/2010 12:20:14 PM
