Cui Dongmei. Atlas of Histology: with functional and clinical correlations. 1st ed
Подождите немного. Документ загружается.

CHAPTER 18
■
Male Reproductive System
345
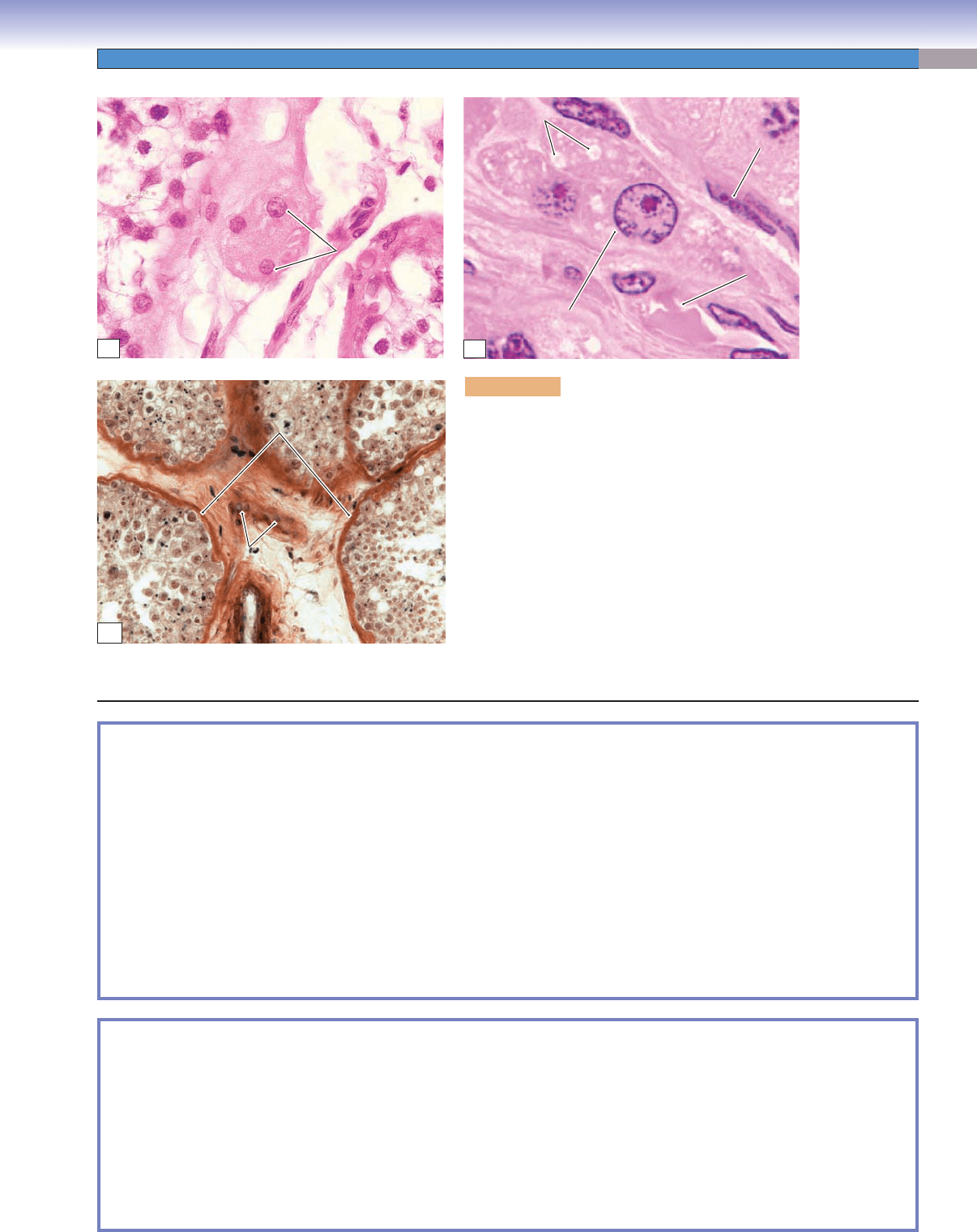
Figure 18-14C Rete Testis
Figure 18-15A,B Ductuli Efferentes
Figure 18-15C Clinical Correlation: Testis Seminoma
Extratesticular Genital Ducts
Figure 18-16 Ductus Epididymis
Figure 18-17A,B Epithelium of the Ductus Epididymis
Figure 18-18A Ductus Deferens, Spermatic Cord
Figure 18-18B,C Ductus Deferens
Figure 18-19A,B Ejaculatory Duct, Prostate Gland
Figure 18-19C Epithelium of the Prostatic Urethra
Accessory Genital Glands
Figure 18-20A,B Prostate Gland
Figure 18-20C Clinical Correlation: Prostate Cancer
Figure 18-21A,B Seminal Vesicles
Figure 18-21C Seminal Vesicle with Seminal Fluid
Penis
Figure 18-22 Overview of the Penis
Synopsis 18-3 Clinical and Pathological Terms for the Male Reproductive System
Introduction and Key Concepts for the
Male Reproductive System
The male reproductive system is composed of (1) a pair of testes
where spermatogenesis takes place; (2) a series of genital ducts
that include intratesticular genital ducts and extratesticular
genital ducts (which function to carry spermatozoa from the
testes to their destination); (3) three major accessory genital
glands: the prostate gland, seminal vesicles, and bulbourethral
glands; and (4) the penis, which is the male copulatory
organ. The main functions of the male reproductive system
include production of spermatozoa, fertilization of the
ovum in the female reproductive tract, production of sex
hormones (testosterone) to develop and maintain secondary
male sex characteristics, and performance of sexual activity
(copulation).
Testis
The testis consists of numerous convoluted seminiferous
tubules that are lined by seminiferous epithelium supported
by a basement membrane. The seminiferous epithelium
hosts various stages of spermatogenic cells (spermatogonia,
spermatocytes, and spermatids), which are protected,
nourished, and supported by Sertoli cells. The Sertoli cells also
produce testicular fl uid, anti-Müllerian hormone, androgen-
binding protein (ABP), etc. Between the seminiferous tubules,
there is loose connective tissue that contains a special type of
cells called the interstitial cells of Leydig. These cells mainly
produce testosterone hormone that promotes spermatogenesis
and the development of male sexual organs as well as maintains
secondary male sexual characteristics. The testis is covered by
the tunica albuginea (capsule), tunica vaginalis (mesothelial
sac), and an outer layer of wrinkled thin skin, the scrotum.
Spermatogenesis takes place in the seminiferous epithelium of
the tubules (see Figs. 18-9 to 18-13B).
Intratesticular Genital Ducts
The intratesticular genital ducts are located within the testis,
including the tubuli recti, rete testis, and ductuli efferentes.
1. Tubuli recti: These are short, straight tubules lined by
simple cuboidal epithelium. They carry the newly produced
spermatozoa in testicular fl uid from the seminiferous tubules to
the rete testis in the mediastinum of the testis (Fig. 18-14B).
2. Rete testis: This is a maze of anastomosing tubules with an
irregular lumen and is lined by simple cuboidal epithelium
(Fig. 18-14C). This network of interconnecting tubules
conducts the sperm atozoa and testicular fl uid into the
ductuli efferentes.
3. Ductuli efferentes: These convoluted tubules are alternatively
lined by two cell types: nonciliated cuboidal cells and ciliated
columnar cells. The ductuli efferentes absorb some testicular
fl uid and move the spermatozoa to the head of the epididymis
(Fig. 18-15A,B).
Extratesticular Genital Ducts
The extratesticular genital ducts located outside the testis
include the ductus epididymis, ductus deferens, ejaculatory
ducts, and urethra. These ducts are paired tubules except the
urethra, which is a single tubule.
CUI_Chap18.indd 345 6/2/2010 7:38:09 PM
346
UNIT 3
■
Organ Systems
1. Ductus epididymis: Each ductus epididymis is a highly
convoluted tube (about 6 m long) that has three regions:
head, body, and tail (Figs. 18-16 to 18-17B). They are lined
by pseudostratifi ed columnar epithelium with long stereo-
cilia that absorb large volumes of testicular fl uid from the
lumen and secrete a variety of substances, including glycero-
phosphocholine, which inhibits capacitation of spermatozoa
from occurring in the male reproductive tract. The tail of the
epididymis is the region where spermatozoa mature and are
stored.
2. Ductus deferens: Each ductus deferens is a long tube that
courses partly within a spermatic cord. Its proximal end
connects with the tail of the epididymis. The distal portion
becomes enlarged and is known as the ampulla. After its
junction with the duct of the seminal vesicle, the ductus
deferens continues its course to form the ejaculatory duct.
The ductus deferens is lined by pseudostratifi ed columnar
epithelium and surrounded by a thick muscularis consisting
of three layers of smooth muscle (Fig. 18-18A–C).
3. Ejaculatory ducts: The two ejaculatory ducts are surrounded
by the prostate gland (Fig. 18-19A,B). They are straight
tubes, lined by pseudostratifi ed columnar and simple
columnar epithelium. The ejaculatory ducts open into the
prostatic urethra at the colliculus seminalis. The colliculus
seminalis is a median elevation of the verumontanum, the
portion of the male prostatic urethra where the ducts open.
4. Urethra: The urethra is a long tube (about 20 cm) lined by
various types of epithelium. It is a common passage shared by
the urinary system and reproductive system in the male. It can
be divided into three regions: the prostatic, the membranous,
and the spongy (penile) urethra. The prostatic urethra, lined
by transitional epithelium, is connected with the bladder at
its proximal end and passes through the prostate gland. The
prostatic urethra is wider than other parts of the urethra and
has two ejaculatory ducts opening into the urethra. The short
membranous urethra is lined by pseudostratifi ed columnar
epithelium; it is the intermediate and narrowest part of the
urethra. The membranous urethra connects the prostatic
urethra to the spongy urethra. The spongy urethra, also called
the penile urethra, is lined by stratifi
ed columnar epithelium.
It passes through the penis and is the longest segment of the
urethra (Fig. 18-22).
Accessory Genital Glands
The accessory genital glands are exocrine glands that include
the prostate gland, paired seminal vesicles, and bulbourethral
glands. (1) The prostate gland is a collection of about 40 small
tubuloalveolar glands lined by simple columnar epithelium and
supported by a connective tissue stroma. Prostatic secretions
contain proteolytic enzymes, acid phosphatase, citric acid,
fi brinolysin, and lipids (Fig. 18-20A,B). (2) Each seminal
vesicle has a single convoluted tube with a branched and folded
mucosa lined by pseudostratifi ed columnar epithelium. The
epithelium is supported by a thin connective tissue layer that
is surrounded by two layers of smooth muscle (muscularis).
The seminal vesicle produces seminal fl uid containing fructose,
prostaglandins, fl avins, phosphorylcholine, vitamin C, and
proteins (Fig. 18-21A–C). Semen is a mixture of seminal fl uid,
prostatic secretion, spermatozoa, and testicular fl uid. (3) The
bulbourethral glands are a small pair of glands lined by simple
columnar epithelium. They produce preejaculate (preseminal)
fl uid that lubricates the urethra before ejaculation.
Penis
The penis is an external genital organ that consists of three
cylinders of erectile tissue, including the corpora cavernosa
(two) and the corpus spongiosum (one). The corpus spongiosum
contains the urethra in its center. The penis has a unique blood
supply (dorsal arteries, deep arteries, and helicine arteries)
and drainage (superfi cial veins, arteriovenous shunts) that are
correlated with its erection (Fig. 18-22).
CUI_Chap18.indd 346 6/2/2010 7:38:09 PM
CHAPTER 18
■
Male Reproductive System
347
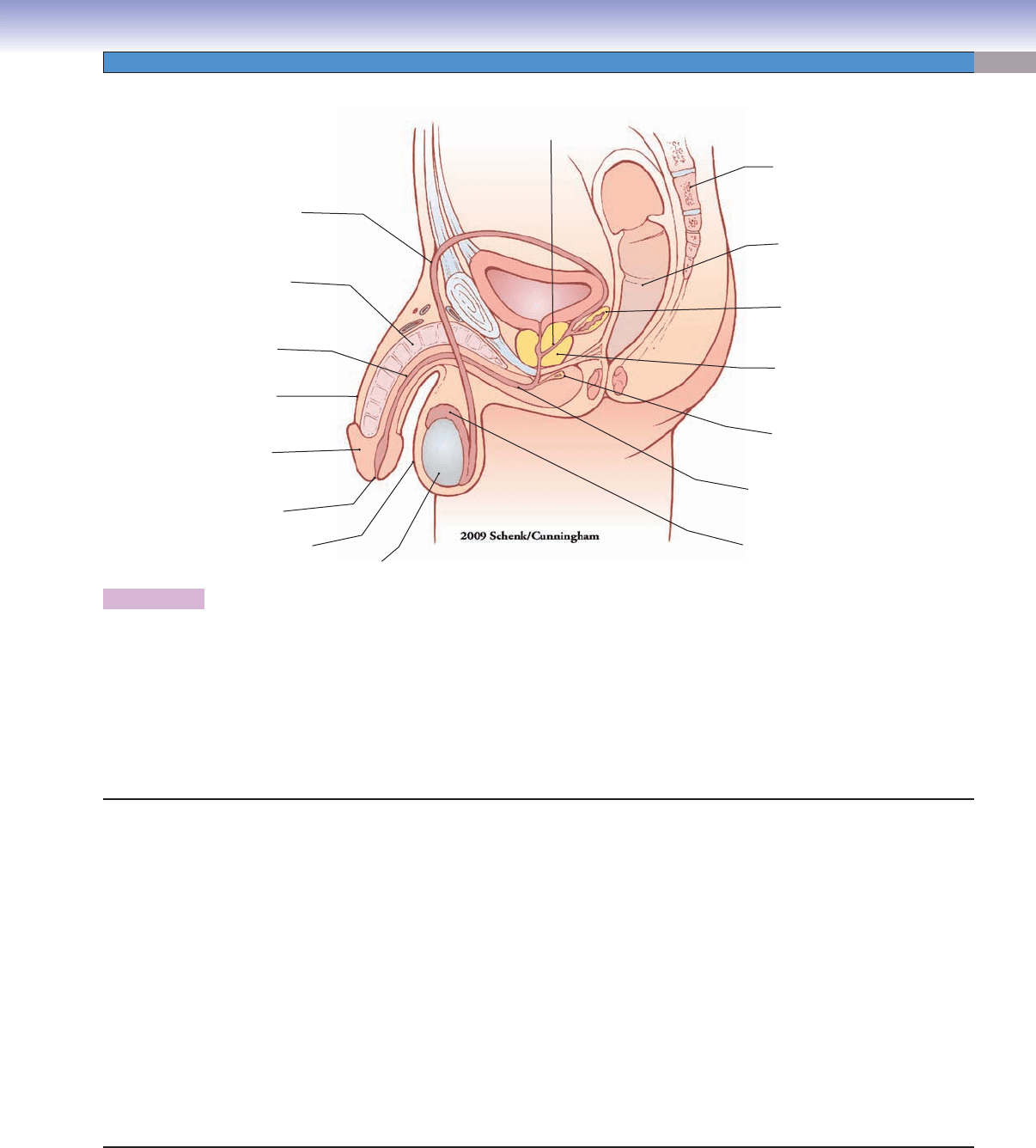
Seminal
vesicle
Prostate
gland
Bulbourethral
gland
Bladder
Sacral
vertebra
Rectum
Ejaculatory
duct
Ductus
deferens
Corpus
cavernosum
Penile
urethra
Urethra
Urethral
orifice
Glans
penis
Penis
Epididymis
Tes t is
Scrotum
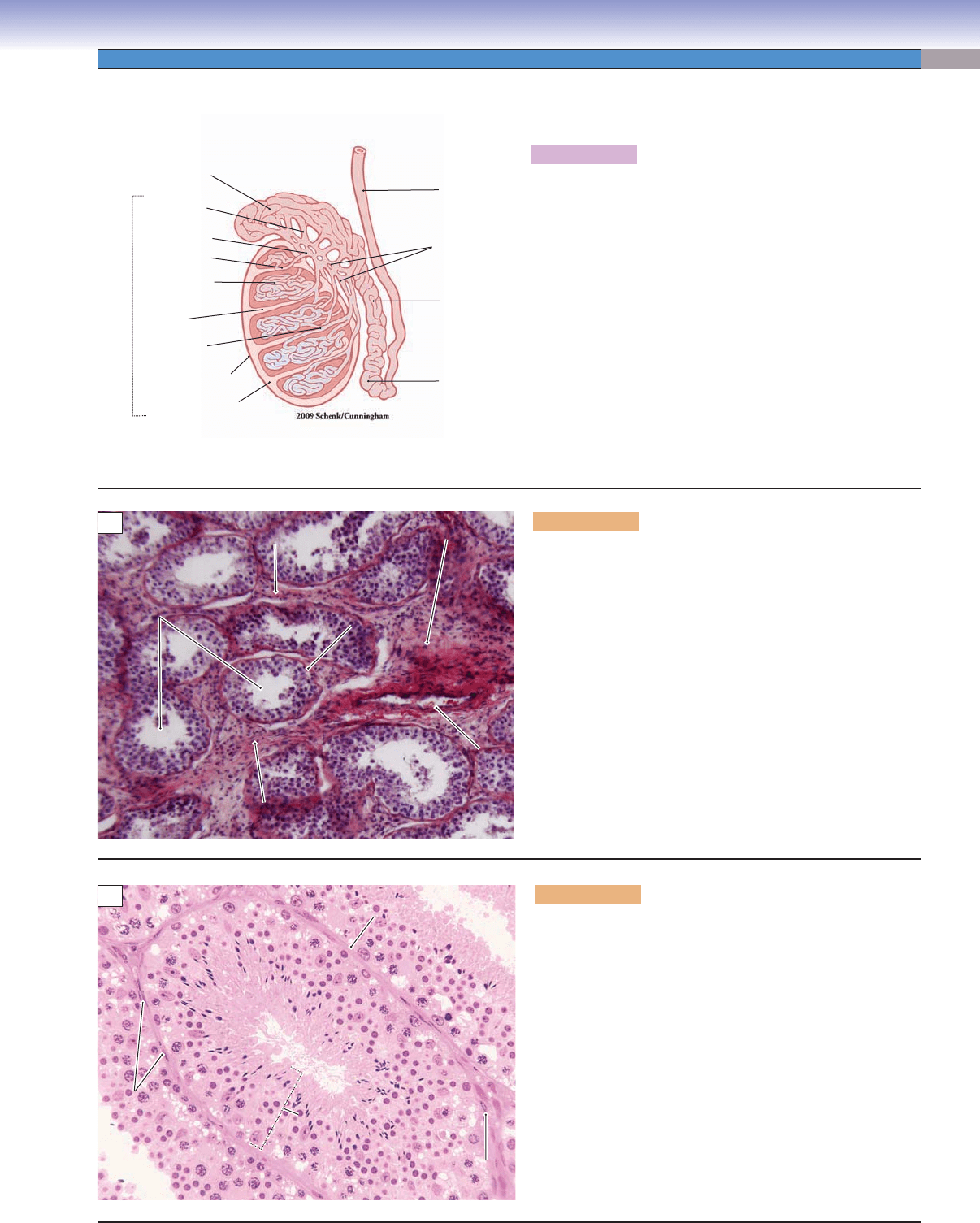
Figure 18-1. Overview of the male reproductive system.
The male reproductive system includes the testes, genital ducts, accessory genital glands, and penis. There are two testes where sper-
matogenesis takes place and sex hormones (testosterone) are produced. The genital ducts include intratesticular genital ducts and
extratesticular genital ducts. The intratesticular genital ducts comprise the tubuli recti, rete testis, and ductuli efferentes, which are
located inside of the testis. The extratesticular genital ducts comprise the ductus epididymis, ductus deferens, ejaculatory duct, and
urethra. The accessory genital glands include three major glands: the seminal vesicles, prostate gland, and bulbourethral glands. Two
ejaculatory ducts meet with the prostatic urethra before it continues its course through the urogenital diaphragm as the membranous
urethra and then through the penis as the penile urethra. The penis is composed of three cylinders of spongy erectile tissue including
the two corpora cavernosa and the corpus spongiosum (containing the urethra).
Structures of the Male Reproductive System
I. Testes
A. Testicular tunicate
1. Tunica vaginalis
2. Tunica albuginea
3. Tunica vasculosa
4. Medastinum testis
5. Special cells (interstitial cells of Leydig)
B. Seminiferous tubules
1. Spermatogenic cells
2. Sertoli cells
II. Genital ducts
A. Intratesticular genital ducts
1. Tubuli recti
2. Rete testis
3. Ductuli efferentes
B. Extratesticular genital ducts
1. Ductus epididymis
2. Ductus (vas) deferens with spermatic cord
3. Ejaculatory ducts
4. Urethra (prostatic, membranous, and spongy/penile
urethra)
III. Accessory genital glands
A. Prostate gland
B. Seminal vesicles
C. Bulbourethral glands
IV. Penis
A. Tunica albuginea
B. Corpus cavernosum
C. Corpus spongiosum and spongy/penile urethra
CUI_Chap18.indd 347 6/2/2010 7:38:09 PM
348
UNIT 3
■
Organ Systems
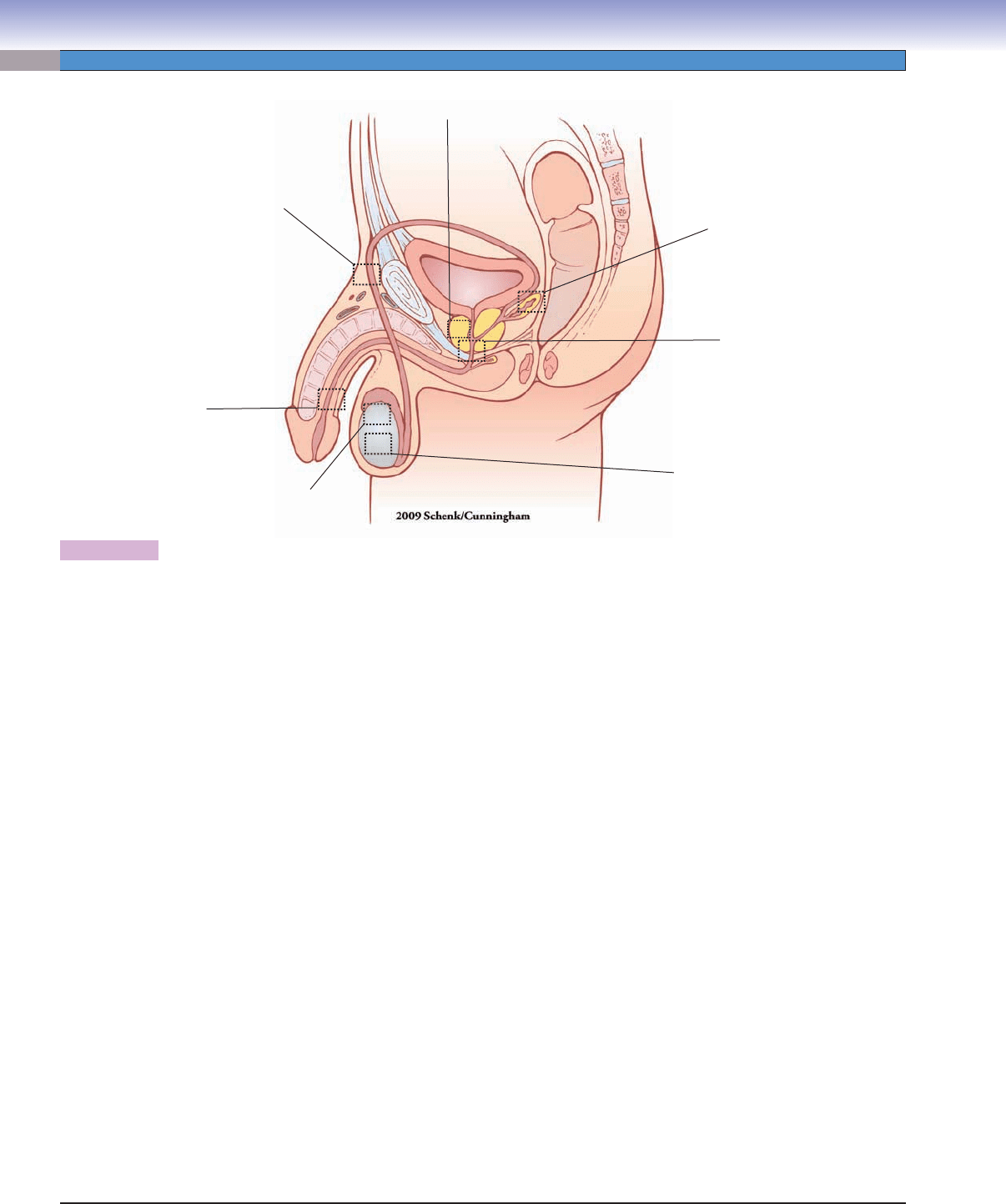
Fig. 18-18A,B,C
Fig. 18-3A to
Fig. 18-13B
Fig. 18-14A to
Fig. 18-15B
Fig. 18-22
Fig. 18-21A,B,C
Fig. 18-20A,B,C
Fig. 18-19A,B,
C
Figure 18-2. Orientation of detailed male reproductive system illustrations.
Structures of the Urinary System with Figure Numbers
Testis:
Seminiferous tubules
Figure 18-3A
Figure 18-3B
Figure 18-3C
Figure 18-4A
Figure 18-4B
Figure 18-5
Figure 18-6A
Figure 18-6B
Figure 18-7
Figure 18-8
Spermatogenesis
Figure 18-9
Figure 18-10
Figure 18-11A,B
Figure 18-12A,B
Figure 18-13A,B
Intratesticular genital ducts:
Tubuli recti
Figure 18-14A
Figure 18-14B
Rete testis
Figure 18-14C
Ductuli efferentes
Figure 18-15A
Figure 18-15B
Figure 18-15C
Extratesticular genital ducts:
Ductus epididymis
Figure 18-16
Figure 18-17A
Figure 18-17B
Ductus deferens and spermatic cord
Figure 18-18A
Figure 18-18B
Figure 18-18C
Ejaculatory ducts
Figure 18-19A
Figure 18-19B
Prostatic urethra
Figure 18-19C
Accessory genital glands:
Prostate gland
Figure 18-20A
Figure 18-20B
Figure 18-20C
Seminal vesicles
Figure 18-21A
Figure 18-21B
Figure 18-21C
Penis:
Figure 18-22
CUI_Chap18.indd 348 6/2/2010 7:38:10 PM
CHAPTER 18
■
Male Reproductive System
349
Ductus
deferens
Ductus
epididymis
(tail)
Ductus
epididymis
(body)
Medastinum
Ductus epididymis
(head)
Test i s
Ductuli
efferentes
Rete testis
Tubuli recti
Tubuli recti
Tunica vaginalis
Tunica albuginea
Septum
Seminiferous
tubule
A
Lumen of the
Lumen of the
seminiferous tubules
seminiferous tubules
Lumen of the
seminiferous tubules
Interstitial connective
Interstitial connective
tissue
tissue
Interstitial connective
tissue
Septum
Septum
Septum
Basement
Basement
membrane
membrane
Basement
membrane
Tubuli recti
Tubuli recti
Tubuli recti
Septum
Septum
Septum
B
Myoid
Myoid
cells
cells
Myoid
cells
Seminiferous
Seminiferous
tubule
tubule
Seminiferous
tubule
Seminiferous
Semin
ifero
u
s
epithelium
ep
ithe
l
iu
m
Seminiferous
epithelium
Lumen
Lumen
Lumen
Fibroblast
Fibroblast
Fibroblast
Seminiferous
Seminiferous
tubule
tubule
Seminiferous
tubule
Basement
Basement
membrane
membrane
Basement
membrane
C
Figure 18-3A. Overview of the testis.
Each testis is composed of many convoluted seminiferous
tubules. The anterior portion of the testis is covered by a closed
sac of peritoneum called the tunica vaginalis (mesothelial sac).
The tunica albuginea is a thick layer of capsule (dense connec-
tive tissue) that surrounds and divides the testis into small lob-
ules; the connective tissue continues at the posterior part and
becomes thicker and forms the vertically oriented connective
tissue mass called the mediastinum. The mediastinum contains
the rete testis, which consists of a labyrinth of small channels
that collect sperm from the tubuli recti. The ductus epididymis
is a single long, highly convoluted duct that receives sperm
from the ductuli efferentes. The epididymis is divided into
three parts: the head, body, and tail. The tail of the epididymis
connects with the ductus deferens. The testes play important
roles in the production of sperm and secretion of testosterone
(sex hormone).
Testis
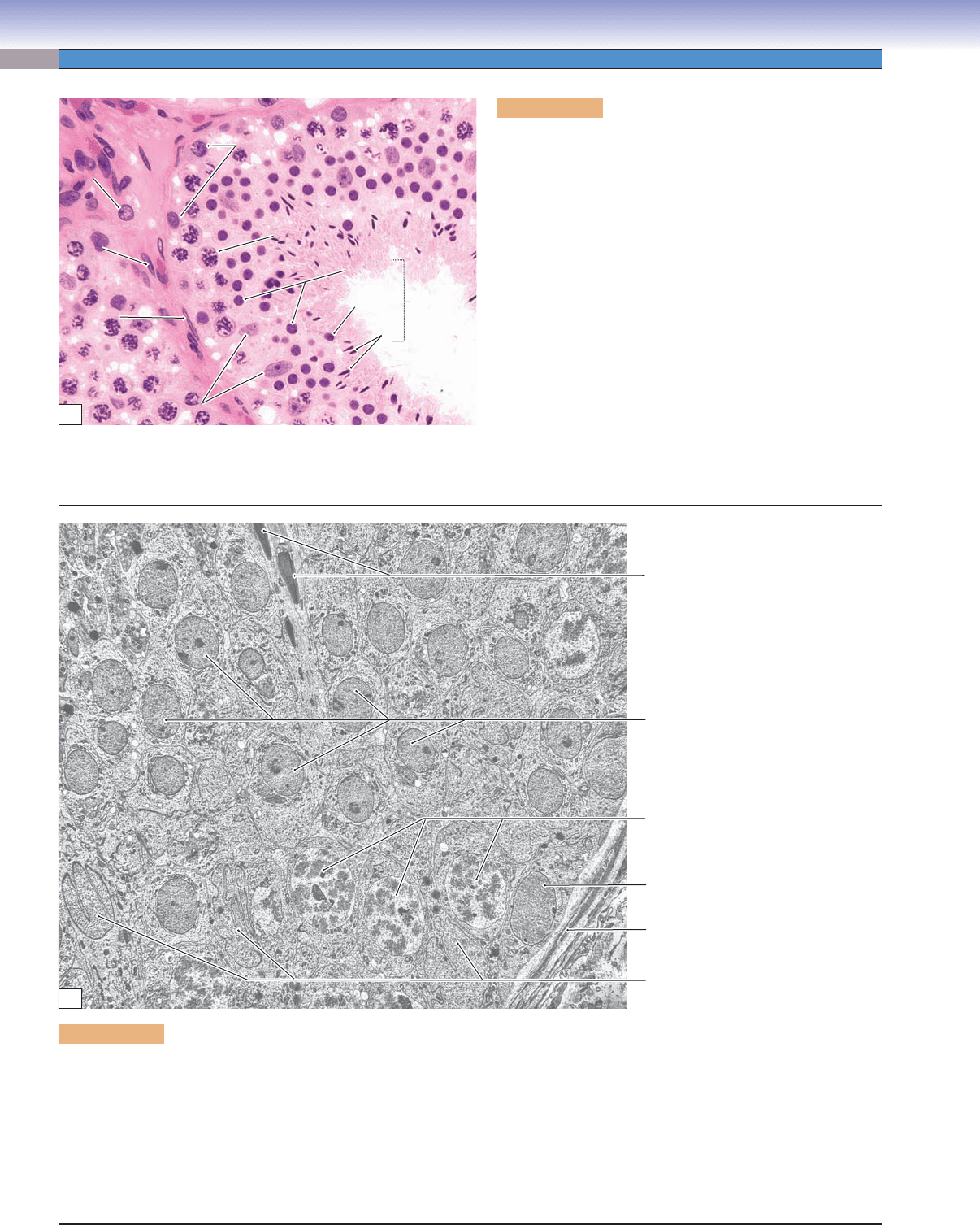
Figure 18-3B. Seminiferous tubules of the testis. H&E,
122
Seminiferous tubules are the main functional components of
the testis. Each of the several hundred seminiferous tubules
in each testis is a highly coiled tubule lined by a stratifi ed
germinal (seminiferous) epithelium containing various stages of
spermatogenic cells. The seminiferous epithelium is supported
by the basement membrane. Cross sections of some seminifer-
ous tubules and a connective tissue septum are shown here.
The tubuli recti (straight tubules) are located in the connec-
tive tissue septa. The connective tissue between neighboring
tubules, which contains small vessels and endocrine cells, is
called interstitial connective tissue.
Figure 18-3C. Seminiferous tubule. H&E, 281
This is an example of a single seminiferous tubule, consisting
of germinal epithelium and its basement membrane. The
seminiferous tubule is surrounded by a very thin connective
tissue containing a few fi broblasts. Another type of cell, the
myoid cell, has the appearance of smooth muscle cells, with fl at
and elongated nuclei. These cells surround the seminiferous
tubules and contract to help the movement of the testicu-
lar fl uid in which the spermatozoa are suspended. Neigh-
boring seminiferous tubules are in close contact with one
another. The various stages of the spermatogenic cells include
spermatogonia, spermatocytes (primary and secondary), and
spermatids (early, intermediate, and late). They are present in six
different specifi c combinations of cell types that defi ne the st ages
of the cycle of the seminiferous epithelium (Figs. 18-11A
to 18-13B).
CUI_Chap18.indd 349 6/2/2010 7:38:11 PM
350
UNIT 3
■
Organ Systems
Spermatids
Spermatids
Spermatids
Spermatogonia
Spermatogonia
Spermatogonia
Primary
Primary
spermatocyte
spermatocyte
Primary
spermatocyte
Interstitial cell
Interstitial cell
of Leydig
of Leydig
Interstitial cell
of Leydig
Intermediate
Intermediate
Intermediate
Early
Early
Early
Sertoli
Sertoli
cells
cells
Sertoli
cells
Fibroblast
Fibroblast
Fibroblast
Late
Late
Late
Interstitial connective
Interstitial connective
tissue
tissue
Interstitial connective
tissue
Myoid
Myoid
cell
cell
Myoid
cell
A
Late spermatids
Early spermatids
Primary spermatocytes
Sertoli cell nuclei
Sertoli cells
Sertoli cells
Basement
membrane
Sertoli cells
Sertoli cells
Spermatogonium
B
Figure 18-4A. Cells in the seminiferous tubules. H&E, 458
There are two types of cells in the seminiferous tubules:
spermatogenic (germ) cells and supporting (Sertoli) cells. The
spermatogenic cells consist of
1. Spermatogonia: These cells have round or oval nuclei and
are located near the basement membrane. They can be sub-
divided into type A and type B cells. Type A cells are stem
cells that divide slowly and give rise to type B cells.
2. Spermatocytes: These derivatives of spermatogonia B cells
undergo meiosis. They move toward the lumen and can be
divided into primary (fi rst meiotic division) and secondary
(second meiotic division) spermatocytes. Primary sperma-
tocytes in prophase are most commonly seen in sections.
Their large nuclei contain strands of condensed chromo-
somes. Secondary spermatocytes complete the second mei-
otic division very quickly, so they are rarely seen.
3. Spermatids: These cells have small interphase nuclei that
range from spherical to thin and elongated. They can be
classifi ed as early, intermediate, or late spermatids, based
mainly on the appearance of the nucleus.
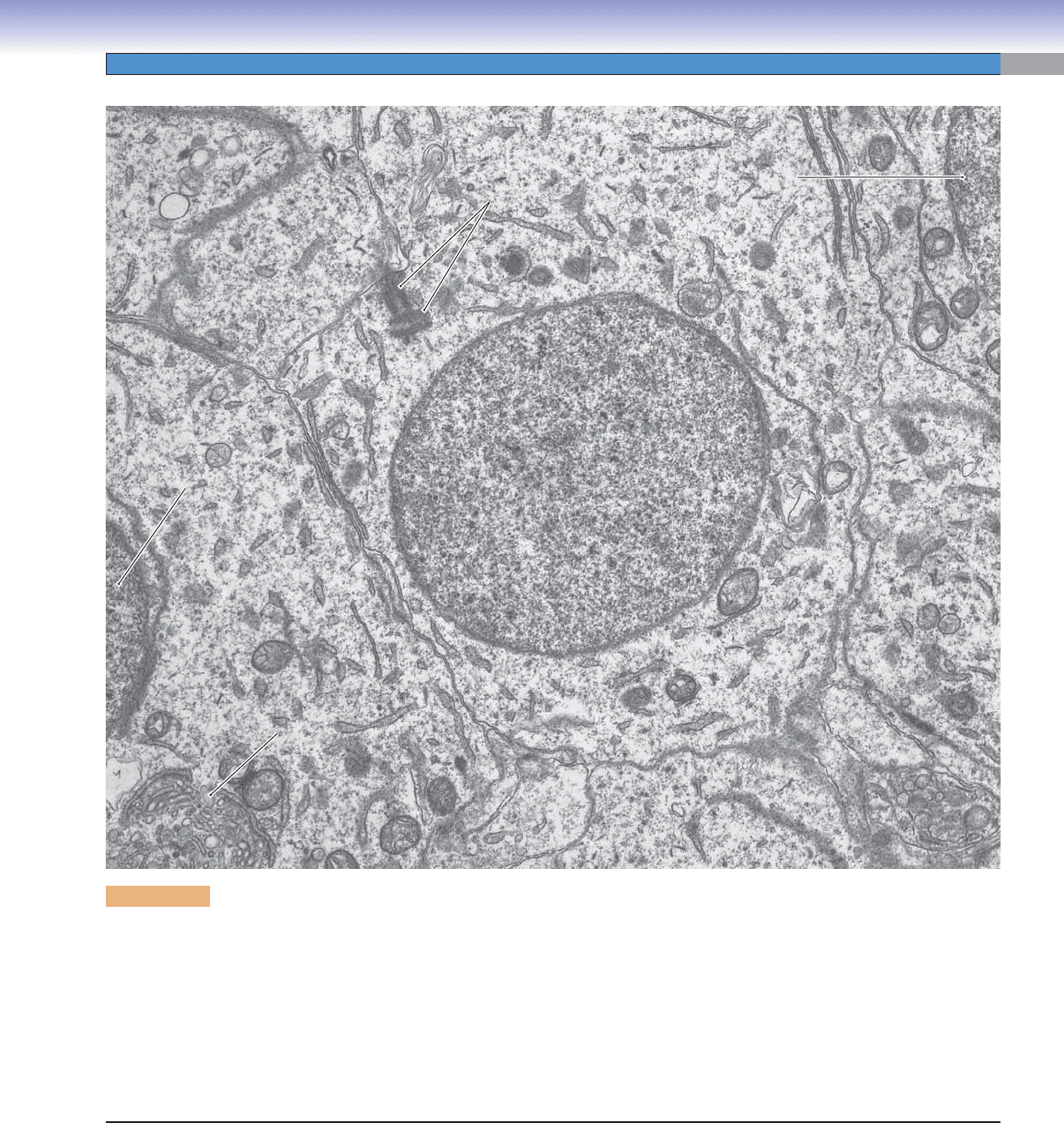
Figure 18-4B. Seminiferous epithelium. EM, 4,600
This low magnifi cation view shows almost the full thickness of the seminiferous epithelium. Sertoli cells are the nongerm cells that
organize the epithelium and divide it into two compartments, basal and adluminal (Fig. 18-12A). The only cell type in the basal com-
partment is the spermatogonium, which, like the Sertoli cells, contacts the basement membrane. This patch of epithelium appears to
be in stage one of the six stages (cell associations) of seminiferous epithelium. The adluminal compartment contains three cohorts of
cells, each at a different stage of spermatogenesis. The least advanced cells are primary spermatocytes in prophase of meiosis I. The
chromosomes of these diploid cells have begun condensing, and homologous pairs have aligned into synaptonemal complexes. Early
spermatids, which appear as small, undifferentiated cells, predominate in the middle and superfi cial regions of the epithelium. The third
and most advanced cell type here is the late spermatid. The heads of a few can be seen surrounded by the cytoplasm of a Sertoli cell.
CUI_Chap18.indd 350 6/2/2010 7:38:16 PM
CHAPTER 18
■
Male Reproductive System
351
Nucleus of
Nucleus of
early spermatid
early spermatid
Nucleus of
early spermatid
Nucleus of
Nucleus of
early spermatid
early spermatid
Nucleus of
early spermatid
Centrioles
Centrioles
Centrioles
Nucleus of
Nucleus of
early spermatid
early spermatid
Nucleus of
early spermatid
Golgi complex
Golgi complex
Golgi complex
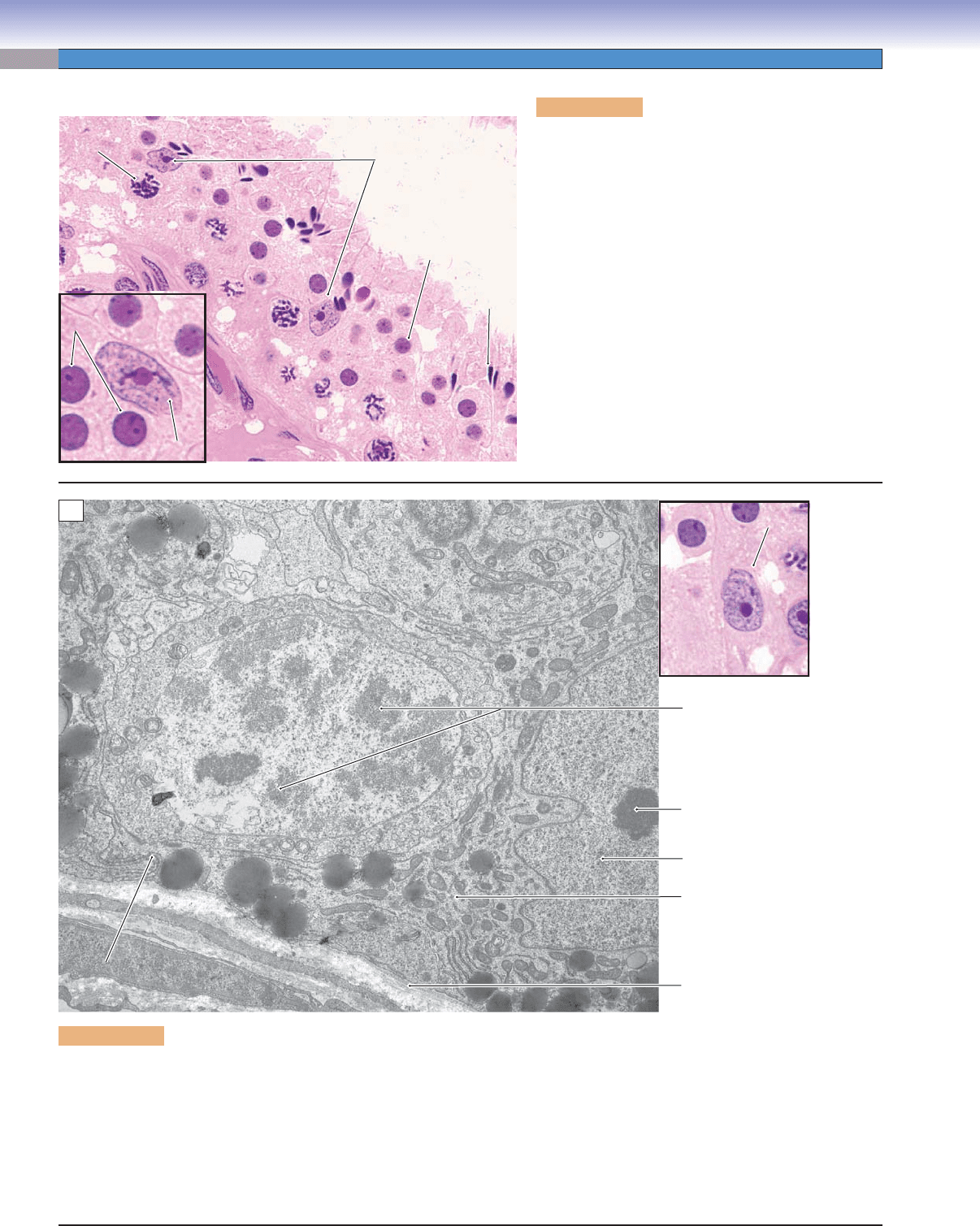
Figure 18-5. Seminiferous epithelium, early spermatid. EM, 17,000
Completion of meiosis II by secondary spermatocytes produces spermatids. These are haploid cells that do not divide but undergo
spermiogenesis, that is, morphological differentiation into spermatozoa. The cells in this image are early spermatids that have not
yet acquired many of the specializations of spermatozoa. The interphase nucleus in the center is still spherical, and the chromatin is
not yet highly condensed. The Golgi complex, visible in the cell on the left, will be the site of development of the acrosomal vesicle
and, ultimately the acrosome, which will form a cap on one side of the nucleus. Note that the plane of section happens to pass
through the central cell’s centrosome with its pair of centrioles. One member of the pair will organize the development of the fl agel-
lum with its axoneme of microtubules. The other centriole will participate in the fi rst cleavage division if the spermatozoan fertilizes
a secondary oocyte. This spermatid is linked to its cohort spermatids by cytoplasmic bridges, although this is not evident in this
image. Like all cells engaged in spermatogenesis, spermatids are embedded in cytoplasmic processes of Sertoli cells.
CUI_Chap18.indd 351 6/2/2010 7:38:19 PM
352
UNIT 3
■
Organ Systems
Sertoli cell
Sertoli cell
Sertoli cell
Early
Early
spermatid
spermatid
Early
spermatid
Early
Early
spermatid
spermatid
Early
spermatid
Late
Late
spermatid
spermatid
Late
spermatid
Sertoli cells
Sertoli cells
Sertoli cells
Primary
Primary
spermatocyte
spermatocyte
Primary
spermatocyte
A
Chromosomes in nucleus
of primary spermatocyte
Nucleolus of Sertoli cell
Nucleus of Sertoli cell
Cytoplasm of Sertoli cell
Basal lamina of
seminiferous epithelium
Sertoli cell
Sertoli cell
Sertoli cell
Tight junction
Tight junction
between sertoli cells
between sertoli cells
Tight junction
between sertoli cells
B
Figure 18-6A. Sertoli cells, seminiferous tubules.
H&E, 732; inset 1,603
Sertoli cells have pale oval or irregularly shaped nuclei,
and nucleoli are often present. They are irregular colum-
nar cells with many folded cytoplasmic processes form-
ing compartments for the spermatogenic cells. They
form tight junctions (zonulae occludentes) with the
neighboring Sertoli cells thereby providing a blood-
testis barrier to protect spermatogenic cells from being
harmed by autoimmune reactions. Sertoli cells con-
trol hormones, nutrients, and other substances pass-
ing through the compartments and maintain the ideal
environment for spermatogenesis. They play important
roles in supporting, protecting, and nourishing sper-
matogenic cells as well as in secreting testicular fl uid
(rich in fructose) to help in transporting spermatozoa
out of the seminiferous tubules. They also secrete
ABP, anti-Müllerian hormone, and inhibin and activin
hormones.
Figure 18-6B. Sertoli cell and primary spermatocyte, seminiferous epithelium. EM, 7,900; inset (color) H&E, 1,005
Sertoli cells, the only somatic cells of the seminiferous epithelium, are dynamic cells with a long list of functions in support of
spermatogenesis. Their processes envelope and support the germ cells throughout the many stages of meiosis and spermiogenesis.
In this view, cytoplasmic extensions of the Sertoli cell (with its nucleus at the left edge) enshroud the primary spermatocyte that has
entered prophase of meiosis I and isolate it from the basal compartment so that it is no longer accessible to the immune system. Note
also the example of the junctional complexes (including tight junctions) that couple adjacent Sertoli cells and, thereby, establish a
controlled and specialized environment in support of the cells that are undergoing spermatogenesis. Other functions of Sertoli cells
are secretion of testicular fl uid, concentration of androgens, and phagocytosis of the residual bodies jettisoned by late spermatids as
they complete spermiogenesis.
CUI_Chap18.indd 352 6/2/2010 7:38:22 PM
CHAPTER 18
■
Male Reproductive System
353
Seminiferous
Seminiferous
tubule
tubule
Seminiferous
tubule
Leydig
Leydig
cells
cells
Leydig
cells
Seminiferous
Seminiferous
tubule
tubule
Seminiferous
tubule
A
Lipid vacuoles
Lipid vacuoles
of Leydig cell
of Leydig cell
Lipid vacuoles
of Leydig cell
Leydig cell
Leydig cell
Leydig cell
Fibroblast
Fibroblast
Fibroblast
Lumen of
Lumen of
capillary
capillary
Lumen of
capillary
B
Basement membrane
Basement membrane
of the
of the
seminiferous tubule
seminiferous tubule
Basement membrane
of the
seminiferous tubule
Leydig
Leydig
cells
cells
Leydig
cells
C
Figure 18-7. Interstitial cells of Leydig. H&E, left 263; right
2,016; iron hematoxylin stain, 237
The interstitial cells of Leydig are located in the interstitial (connec-
tive) tissue near the blood capillaries and between the seminiferous
tubules. These cells have round nuclei and pale-stained cytoplasm with
lipid drops (lipid vacuoles) in the peripheral region of the cytoplasm,
which give them a bubbly appearance (like many steroid-producing
cells). These cells contain abundant smooth endoplasmic reticulum,
which contributes to steroid hormone production. The interstitial cells
of Leydig derive from the mesoderm and are usually large in size (about
20 μm in diameter) compared with other cells in the connective tissue.
They are the endocrine cells that produce the important male sex
hormone, testosterone. Testosterone plays important roles in develop-
ing and maintaining male sex characteristics, stimulating muscle and
bone growth, and increasing bone density. A small amount of testoster-
one is also produced by the adrenal glands and ovaries in the female.
SYNOPSIS 18-1 Functions of Sertoli Cells
Support ■ : Provide physical support and nutrition for the different stages of spermatogenic cells.
Protection
■ : Form blood-testis barrier by tight junctions between adjacent Sertoli cells that protect spermatogenic cells
from autoimmune destruction; also control hormones, nutrients, and other substances being transported in and out of the
seminiferous tubules.
Phagocytosis
■ : Remove residual bodies after excess cytoplasm is shed from the spermatids during maturation of the spermatozoa.
Secretion
■ : (1) Secrete and release fructose-rich fl uids (testicular fl uid) to help nourish and move sperm from the seminifer-
ous tubules to the epididymis; (2) secrete anti-Müllerian hormone to prevent oviducts from developing from the Müllerian
duct in the early stages of the male embryo; (3) secrete androgen-binding protein (ABP) to maintain the concentration of
testosterone in the seminiferous tubules, thereby promoting spermatogenesis; (4) secrete glial cell–derived neurotrophic
factor (GDNF) to promote survival and differentiation of the spermatids (GDNF is better known for promoting development
of neurons); and (5) produce inhibin and activin hormones to provide negative and positive feedback to the hypothalamus,
thereby regulating follicle-stimulating hormone (FSH) secretion by the pituitary gland.
SYNOPSIS 18-2 Functions of Testosterone
The interstitial cells of Leydig secrete testosterone, which is the major male sex hormone. Its functions include:
Promoting development of male sex organs in early fetal development.
■
Promoting male sexual characteristics, such as growth of beard and axillary hair, enlargement of the larynx, and deepening ■
the voice.
Increasing muscle growth, thickness of the skin, and sebaceous gland secretion.
■
Promoting bone growth and increasing bone density. ■
Increasing basal metabolism and physical energy. ■
Promoting spermatogenesis. ■
CUI_Chap18.indd 353 6/2/2010 7:38:24 PM
354
UNIT 3
■
Organ Systems
D. Cui
Interstitial (Leydig) cell
Interstitial (Leydig) cell
Interstitial (Leydig) cell
Hypothalamus
Inhibin (–)
Activin (+)
FSH (+)
)(gonadotrophs
LH (+)
()gonadotrophs
(–)
(–)
GnRH (+) LH
GnRH (+) FSH
Pituitary gland
Increases
concentration
of testosterone
Inhibin & activin
hormones
ABP
Sertoli cell
Sertoli cell
Sertoli cellSertoli cell
Sertoli cell
Sertoli cell
(+)
Inhibits female organ
development
Anti-Müllerian
hormone
Promotes
spermatogenesis
Supports development of
male sex organs and
maintains male sexual
characteristics;
promotes spermatogenesis
(+)
Testosterone
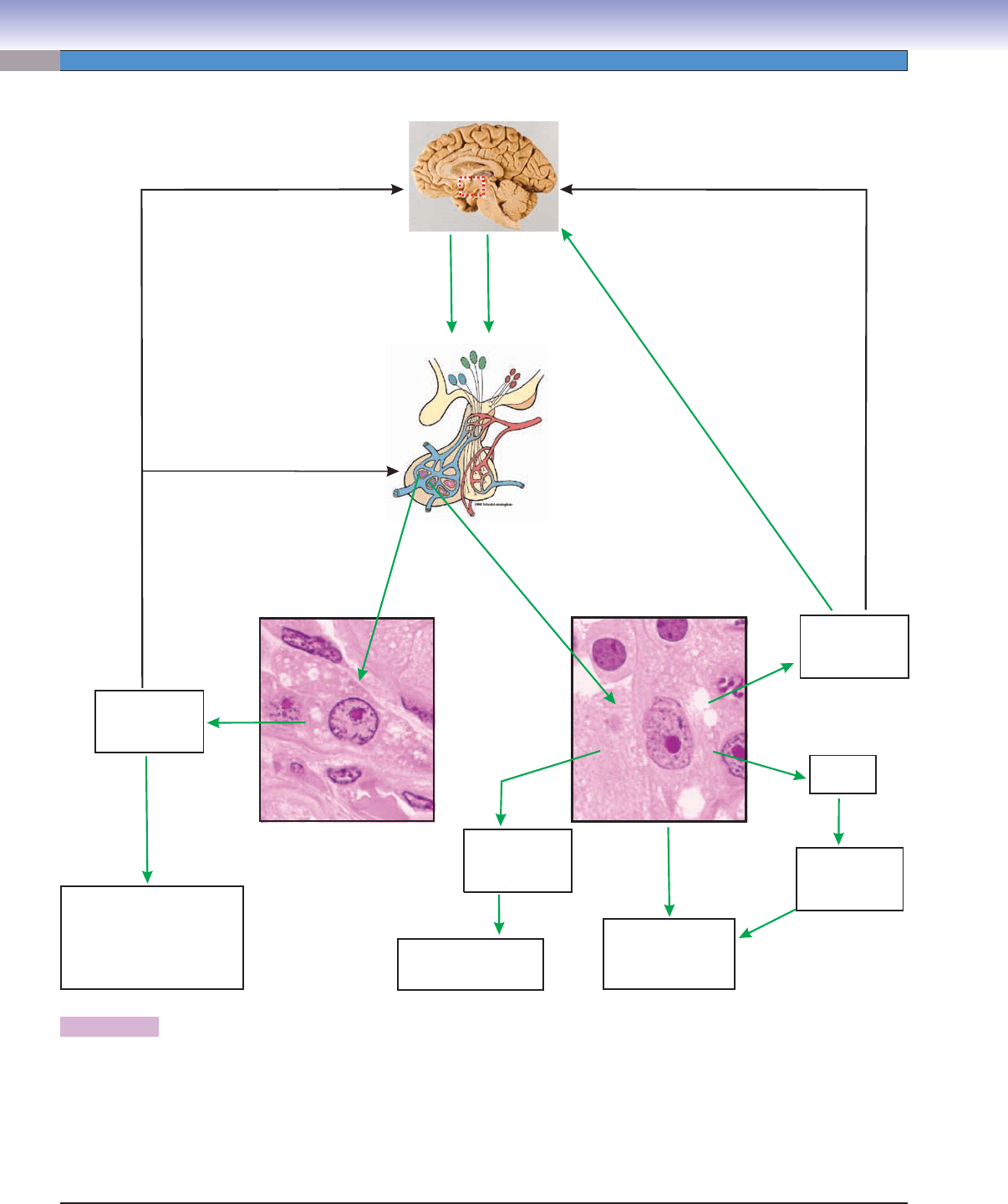
Figure 18-8. Hormone regulation involving the testicular cells (interstitial cells of Leydig and Sertoli cells). H&E, 1,005
The preoptic nucleus in the hypothalamus secretes gonadotropin-releasing hormone (GnRH), which stimulates the pituitary gland
to produce and release luteinizing hormone (LH) and FSH. Secretion of testosterone by the interstitial cells of Leydig is stimulated
by the LH produced by the gonadotrophs in the adenohypophysis of the pituitary gland. An excessive level of testosterone sends
negative feedback to the hypothalamus to inhibit production of GnRH, resulting in decreased secretion of LH in the pituitary gland.
Sertoli cells that release ABP are stimulated by FSH, which stimulates production of the ABP. Sertoli cells also secrete anti-Müllerian
hormone as well as inhibin and activin hormones. The inhibin hormone suppresses and activin hormone stimulates the production
of GnRH, which infl uences FSH production by the gonadotrophs in the adenohypophysis of the pituitary gland.
CUI_Chap18.indd 354 6/2/2010 7:38:28 PM
