Caballero B. (ed.) Encyclopaedia of Food Science, Food Technology and Nutrition. Ten-Volume Set
Подождите немного. Документ загружается.


appendicitis-like attack, diarrhea (lasting several
weeks), fever, rash, nausea, headache, and vomiting.
The minimum infectious dose is unknown. Illness
onset is usually between 24 and 48 h after intake,
although the incubation period can be as long as
11 days.
0002 Y. enterocolitica is widely distributed in the envir-
onment, in lakes and stream waters, which are
sources of the organisms to warm-blooded animals.
Animals from which Y. enterocolitica has been isol-
ated include cats, birds, dogs, guinea-pigs, rats,
horses, chickens, cattle, swine, lambs, and fish. Cer-
tain biotypes and serogroups are associated with a
specific host. A principal source or reservoir of viru-
lent Y. enterocolitica are pigs. Virulent strains of
Y. enterocolitica often reside in the oral cavity and
the gastrointestinal tract of pigs. Serogroups 0:3 and
0:9 are mainly associated with pork tongues
and tonsillar area. Despite this, it has been shown
that pork meat has accidentally been a vehicle for
yersiniosis.
0003 There are four serogroups of Y. enterocolitica asso-
ciated with pathogenicity: 0:3, 0:5, 0:8, and 0:9. The
genes encoding for invasion of mammalian cells
are located on the chromosome, while a 40–50-
MDa plasmid encodes most of the other virulence-
associated phenotypes. The 40–50-MDa plasmid is
present in almost all pathogenic Yersinia species,
and the plasmids appear to be homologous. Although
heat-stable enterotoxin has been isolated from most
clinical isolates, it is uncertain whether this toxin
plays a role in the pathogenicity of the organism.
0004 Y. enterocolitica have been detected in a wide var-
iety of processed foods, particularly pasteurized milk,
dairy products, vacuum-packaged meats, seafood,
vegetables, and many ready-to-use foods. Incidence
varies between countries. The most common Y. enter-
ocolitica serogroups in human infections are 0:3, 0.5,
27, 0:8, and 0:9. In Europe, Africa, and Japan,
serogroups 0:3 and 0:9 are the most common. These
serogroups are prevalent in Denmark, Belgium, and
Sweden, and are a significant cause of gastrointestinal
illnesses in those countries.
Growth Requirements
Temperature
0005 Y. enterocolitica is a psychrotroph and can grow at
temperatures as low as 0
C and as high as 44
C, the
optimum range being 22–29
C. For biochemical re-
actions, the optimum temperature is about 28
Cin
pure culture, but it is a poor competitor at this tem-
perature. Multiplication can occur between 2and
0
C, but growth is very slow. At 3
C, it takes 200 h
to increase 2 logarithmic cycles in culture medium.
Growth at 0–2
C in milk after 20 days has been
observed. Generation times at 4
C appear to be
strain-dependent, varying between 16 and 26 h in
pasteurized milk, and growth is preceded by an
extended lag time of up to 40 h. Increases in levels
of up to 5 log increments in 10–14 days have been
recorded in a variety of artificially contaminated
cooked foods stored at 4
C. Growth at 0–1
Con
pork and chicken has been observed and on raw
beef kept for 10 days at 0–1
C. Growth is slightly
slower in the presence of competitor organisms but at
4
C competes better against other psychrotrophic
bacteria. In milk at 4
C, Y. enterocolitica grow and
reach numbers of up to 10
7
CFU ml
1
in 7 days,
and compete well with the background flora.
pH
0006The pH range for growth is 4.6–9.0, with an opti-
mum pH of 7.0–8.0. The minimum pH at which
growth can occur varies between strains and also
depends on storage temperature and the acidulant
used. The following values have been found for six
strains of Y. enterocolitica with the pH adjusted with
HCl and incubated for 21 days: 4.42–4.80 at 4
C;
4.36–4.83 at 7
C; 4.26–4.50 at 10
C and 4.18–4.36
at 20
C. Growth inhibition at low pH is greater at
4
C than at 20
C, and the use of organic acids raises
the minimum pH for growth. When organic acids are
used to adjust pH, the order of their effectiveness is
acetic >lactic > citric. Acetic acid is the most inhibi-
tory organic acid commonly used in food, preventing
growth below 5.7 at 4
C and 5.1 at 20
C. It has also
been shown that tolerance to high pH values is de-
pendent on temperature and on the medium used.
Growth has been demonstrated at pH 9.5 at 10
C
but not at 6
C. Under the same pH and temperature
conditions, the inhibitory effects of acids are quite
different. At a high pH (5.8), the order of inhibition
of Y. enterocolitica 0:9 at 4
C is formic acid > acetic
acid > propionic acid > lactic acid, whereas at a
lower pH (4.2) the order is formic acid > lactic
acid > acetic acid > propionic acid. The mechanisms
of the interaction of these acids inside bacterial cells
differ under aerobic and anaerobic conditions. While
the inhibitory effect of lactic acid is enhanced under
anaerobic conditions, the acetic and formic acids
are less effective.
Heat Tolerance
0007According to available data, the heat resistance
of Y. enterocolitica seems to vary widely among
different strains. Strains of Y. enterocolitica are not
particularly heat-resistant. Sublethal injury to
6240
YERSINIA ENTEROCOLITICA
/Properties and Occurrence

Y. enterocolitica cells has been reported after heat
treatment at 47
C for more than 12 min. However,
the magnitude of the effect depends on growth
temperature. In the range of 4–20
C, the growth
temperature does not influence heat resistance at
54–66
C for Y. enterocolitica. However, when cells
are grown at 37
C, heat resistance increases fourfold.
The heat resistance of Y. enterocolitica is also influ-
enced by the pH of the heating medium. The pH of
maximum heat resistance in citrate phosphate buffer
is pH 7 for cells grown at 37
C but pH 5 for those
grown at 4
C. In both, the magnitude of the pH effect
on heat resistance is constant at all heating tempera-
tures. Different studies have been carried out in milk as
pasteurization and thermalization are achieved
effectively when the inoculum does not exceed 10
8
CFU ml
1
.
Freezing
0008 Refrigeration reduces the multiplication capacity of
Y. enterocolitica but does not inhibit it completely.
Growth at low temperatures depends on other
factors, mainly on pH. Good growth has been ob-
served at 4
C, when the pH is neutral, but very little
growth has been detected at a slightly acidic pH (5.4).
The ability of Y. enterocolitica to withstand freezing
has been shown: cultures of Y. enterocolitica can
survive for several weeks at 20
C without any
reduction in the number of viable cells. Also, in stud-
ies with frozen foods, 3–4 logarithmic reductions
have been found to occur after 4 weeks of storage
at 18
C. Despite this, Y. enterocolitica has been
isolated from a wide range of frozen foods.
Irradiation
0009 The ability of Y. enterocolitica to survive g-radiation
depends on the food composition/treatment and
the presence of preservatives. As Y. enterocolitica is
more radiosensitive than other common foodborne
pathogens such as Salmonella and Listeria, it can be
completely eliminated at a dose range of 3–4 kGy.
With low numbers of Y. enterocolitica (D
10
values
between 0.25 and 0.30 kGy), a contamination of up
to 10
3
–10
4
CFU g
1
can be positively controlled by a
1–1.5-kGy dose. Thus, the average dose of 1 kGy
recommended by the FDA appears to be adequate
for eliminating Yersinia. While irradiation even at
6 kGy fails to prevent survival in raw pork, the bac-
terium is completely suppressed in cooked ham and
salami treated with lower doses of radiation. Faster
recovery of radiation-injured cells in raw meat than
in cured meat with spices or in cooked ham demon-
strates that Y. enterocolitica in irradiated products
can be inhibited by using combination processes
including irradiation.
Preservatives and Packaging
0010The behavior of Y. enterocolitica in response to vari-
ous preservatives depends on the temperature and
level of the chemical, pH, and amount of sodium
chloride present. At low pHs and temperatures, po-
tassium sorbate is very effective against Y. enteroco-
litica. In contrast, other preservatives such as sodium
phosphite and sodium hypophosphite are inhibitory
at relatively high pH values. Packaging containing
high levels of carbon dioxide is very effective at
delaying growth and can cause complete inhibition.
Y. enterocolitica can survive sodium chloride con-
centrations of 6–7% at specific temperature and
pH levels. Although 7% NaCl is inhibitory at 3
C,
growth occurs with 5% NaCl. Other preservatives
such as potassium sorbate, sodium hypophosphite,
sodium phosphite, and curing salt delay or inhibit
the growth of this microorganism.
Predictive Modeling
0011Predictive models are used to describe the behavior of
microorganisms under different conditions such as
temperature, pH, water activity, oxidation–reduction
potential, and additives. They may be applied in vari-
ous ways to ensure the microbial safety and quality.
The main objective is to describe mathematically the
growth or inactivation of microorganisms in food
under prescribed food conditions.
0012Several models charting the growth and survival of
Yersinia enterocolitica have been developed by study-
ing the effect of different factors, such as: pH (4–8.5);
organic acids (acetic, lactic, sulfuric, and citric
acid); temperature (0–42
C); NaCl concentration
(0–10.5%); sodium nitrite (0–200 p.p.m.), strain
with and without plasmids related to virulence
agents, and mild heat treatment (50–60
C). These
models have been validated in different foods such
as pa
ˆ
te
´
, packed cold smoked salmon, UHT milk,
yogurt, mayonnaise, meat and meat products, eggs,
fish, and tofu; in general, predictive models oversti-
mate growth rate values on the fail-safe side, i.e., the
prediction always describes faster growth rates than
the values observed in real foods.
Epidemiological and Clinical Features
0013From an epidemiological standpoint, Y. enterocolitica
is widespread in nature, occurring in the gastrointest-
inal tract of an array of animal hosts, including
mammals, avian species, and cold-blooded species,
and is occasionally isolated in humans. Of all sources,
swine appear to be the major source of strains
YERSINIA ENTEROCOLITICA
/Properties and Occurrence 6241

pathogenic for humans. Several outbreaks have
been reported where infection has been associated
with contact with pigs, and indirect contact with
contaminated pork products and other foods
(Table 1). Some outbreaks in families were attributed
to exposure to cats and dogs. On rare occasions, it
can be transmitted as a result of the bacterium passing
from stools or soiled fingers of one person to
the mouth of another person. This may happen
when basic hygiene and handwashing habits are in-
adequate.
0014 In general, sporadic or food-related outbreaks are
more frequent in regions where pigs are the carriers of
this microorganism. Seasonality seems to play a role
in the incidence of this microorganism in focal geo-
graphical areas, with a higher frequency noted during
cooler periods of the year.
0015 Children are infected more often than adults, and
confirmed cases or Y. enterocolitica in humans corres-
pond to 1 in 100 000 persons per year. In the USA, it is
estimated to cause 3000–20 000 cases each year.
Most recently, it has been shown that humans can
be asymptomatic, since clinically normal blood
donors have supplied Yersinia enterocolitica-infected
blood resulting in fatal septicemia in transfused
patients. Nevertheless, 90% of cases originate from
food.
0016Human clinical infections with Y. enterocolitica
occur most frequently after the intake of food or
water contaminated with this pathogen. The infec-
tious dose estimated to be sufficient to cause human
illness is approximately 10
7
cells, but consumer sus-
ceptibility will vary according to individual levels of
immunocompetence, age, and general health. After
intake, the bacteria pass through the stomach, colon-
ize the epithelial cell surface of the small intestinal
mucosa, and cause diarrhea, possibly by producing
the enterotoxin YST. This microorganism can also
invade epithelial cells, attach to M cells, and pene-
trate Peyer’s patches, where it multiplies with the
help of several surface components that enable it to
resist phagocytosis and survive complement-medi-
ated killing. The invasion process and virulence factor
production are complex processes that are thermore-
gulated by both plasmid and chromosomally encoded
information. Continued proliferation of bacteria
results in inflammation leading to the formation of
local microabscesses and ulceration of the overlying
epithelium. In a relatively short period, ingested
Y. enterocolitica reach the terminal ileum, spread to
the mesenteric lymph nodes, and enter the blood
stream.
0017From a clinical standpoint, Y. enterocolitica is
a common human pathogen that causes a variety
tbl0001 Table 1 Outbreaks of foodborne Y. enterocolitica infection
Vehicle Number of cases(confirmed) Biogroup(s) Country Year
Pasteurized milk 1000 (172)
a
13a, 13b USA 1982
3(3)
b
6,30 UK 1984
19(19)
b
10K UK 1985
17(17)
b
6,30 UK 1985
Chocolate milk 218 (38)
c
8 USA 1976
250
d
USA 1978
Cream deserts 4
e
Belgium 1975
Powered milk/turkey chow mein 239(159)
b
8 USA 1981
Bean sprouts 16
f
8 USA 1982
Tofu 87(56)
g
8, tacoma(21) USA 1981
Chitterlings 14
h
USA 1988
Pork 1
i
USA 1994
Pork (pork cheese) 5(3)
b
3 Hungary 1983
a
From Tacket C, Narain J, Sattin R et al. (1984) A multistate outbreak of infections caused by Yersinia enterocolitica transmitted by pasteurized milk. Journal
of the American Medical Association 251: 383–486.
b
From Greenwood MH (1993) Yersinia enterocolitica. Properties and occurrence In: Macrae R, Robinson RK and Sadler MJ (eds) Encyclopaedia of Food
Science, Food Technology and Nutrition. London: Academic Press.
c
From Black R, Jackson R, Tsai T et al. (1978) Epidemic Yersinia enterocolitica infection due to contaminated chocolate milk. New England Journal of
Medicine 298: 76–79.
d
From Silliker J (1986) Yersinia enterocolitica. Food Technology 8: 22.
e
From Richard J, Moiner J, Cornu C, Goor M and Dereume G (1975) Le
´
ndemie
a
`
Yersinia enterocolitica dans le Tournaisis. Lille Medical 20(1): 36–43.
f
From Cover T and Aber R (1989) Yersinia enterocolitica. New England Journal of Medicine 231: 16–24.
g
From Aulisio C, Stanfield J, Weagent S and Hill W (1983) Yersiniosis associated with tofu consumption: serological, biochemical and pathogenicity
studies of Yersinia enterocolitica isolates. Journal of Food Protection 46: 226–230.
h
From Lee L, Gerber A and Lonsway D et al. (1990) Yersinia enterocolitica 0:3 infections in infants and children, associated with the household preparation
of chitterlings. New England Journal of Medicine 322: 984–987.
i
From Stoddard J, Wechsler D, Nataro J and Casella J (1994) Yersinia enterocolitica infection in a patient with sickle cell disease after the exposure to
chitterlings. American Journal of Pediatric Hematology and Oncology 16: 153–155.
6242
YERSINIA ENTEROCOLITICA
/Properties and Occurrence

of intestinal and extraintestinal syndromes, with
varying degrees of severity, ranging from mild
gastroenteritis to mesenteric lymphadenitis (often
confused with appendicitis), and septicemia. Infec-
tions caused by this microorganism may also reveal
postinfectious immunological sequelae, including
erythema nodosum, arthritis, miocarditis, and glo-
merulonephritis.
Occurrence in Foods
0018 Foods analyzed for Y. enterocolitica show that the
distribution of this microorganism is fairly exten-
sive; it has been isolated in beef, lamb, pork,
oysters, shrimp, crabs, and water. The vast majority
of these isolates are avirulent, and virulent strains
seldom occur in any of these foods. Studies have
examined the fecal droppings of rats near slaughter-
houses and have found that the rats carried virulent
Y. enterocolitica probably picked up from the
pork that was being processed at the slaughter-
houses.
0019 The 68% positive samples of porcine tongues taken
from freshly slaughtered animals have been isolated,
and these represent six serogroups, 0:8 being the
most common and 0:6, 30 the second most common,
followed by other serogroups including 0:3, 0:13, 7,
0:18, and 0:46. Several studies performed in Brazil
have reported positive isolations of Yersinia entero-
colitica from raw milk (16.8%), pasteurized milk
(1.7%), raw beef (80%) and chicken (60%), ground
beef, liver, and pork (20%). In one study performed
in the USA, after examining 100 milk samples, 12
raw samples and one pasteurized sample yielded
Yersinia enterocolitica. Another study of this product
in France reported that 81% of raw milk samples
were positive, the predominant serovar being
0:5 (Table 2).
0020 Outbreaks of yersiniosis have been reported in
which chocolate, coleslaw, tofu, bean sprout, pas-
teurized milk, and pork chitterlings have been
singled out as vehicles (Table 1). One of the first
and most important outbreaks occurred in the USA,
where 220 schoolchildren were taken ill; it was
confirmed that Y. enterocolitica had caused the
problem and that chocolate milk was the vehicle of
infection. This milk was prepared at a small dairy by
means of vat pasteurization; the chocolate was
added after pasteurization and mixed with a paddle;
hence, there was plenty of potential postprocessing
contamination. In another case, the vehicle of trans-
mission was tofu (soyabean curd) that had been
packaged in untreated spring water contaminated
with Y. enterocolitica.
0021Both virulent and avirulent strains of Y. enteroco-
litica have been isolated from a variety of dairy prod-
ucts. Three milkborne outbreaks occurred in the
USA, two attributable to serogroup 0:8 and one to
serogroup 0:13a, 13b. In 1982, there was an outbreak
linked to pasteurized milk; 170 cases were confirmed,
although epidemiological studies revealed that
more than 1000 people were infected. The strain
was also isolated from the plastic carrying cases
used to carry the milk after bottling. In this case,
outdated milk had been brought to a pig farm
in carrying cases. The cases were placed in mud
and manure, the milk poured into troughs for the
pigs, and the carrying cases brought back to the
plant and superficially washed. Although it was con-
firmed that the pigs were the source of infection,
it was impossible to determine exactly how the
microorganism had reached the milk from the
carrying cases.
Prevention of Food Contamination
0022Food-related toxic infections caused by Yersinia
enterocolitica seem to be related to foods in
cold storage. In this situation, it is difficult to define
preventive measures (repeated washing of vegetables,
mainly in collective restaurants, strengthening of
the cold chain, etc.) that enable the spread of this
food-related infection to be restricted. These limita-
tions to prevention highlight the importance of
monitoring human infections (networks of expert
doctors, control laboratories, and reference labora-
tories for studying strains). The prevention of food-
borne disease depends on careful food production,
handling of raw products, and preparation of fin-
ished foods. Hazards can be introduced at any
point from farm to table. Monitoring and control
technologies systematically applied to food produc-
tion by the HACCP are highly effective for prevent-
ing foodborne illness.
0023Primary control of the microorganism would
require changes to current slaughtering practice. The
‘bagging technique’–the method of enclosing the
anus and rectum of pigs in a plastic bag during
slaughter – has been introduced in several slaughter-
houses, mainly in Norway, and it has been shown that
this effectively reduced carcass contamination by
Yersinia enterocolitica. The removal of the head,
tongue, and pharynx at an early stage of slaughter
and improvements in the way in which intestines are
removed would also help to prevent carcass contam-
ination. Additional practices, such as the exclusion of
tonsillar tissue from sale or the scalding of tongue and
head meat prior to the dispatch of products may also
be necessary.
YERSINIA ENTEROCOLITICA
/Properties and Occurrence 6243
tbl0002 Table 2 Occurrence of Yersinia enterocolitica on food
Food Percentage of samples Serogroup(s) Country
Raw milk 81
a
0:5 France
12
b
USA
18.2
c
Canada
16.8
d
Brazil
30
e
Morocco
Raw milk, goat 71
f
Australia
Pasteurized milk 1
b
USA
13.7
d
Brazil
Traditional fermeted milk 6.3
e
Morocco
Cheese 9.2
c
Canada
4
e
Morocco
Turkish Feta cheese 28.8
g
Turkey
Salmon and trout 23
h
UK
Raw beef and chicken 80
i
Brazil
Ground meat and liver 60
i
Brazil
Ground meat 48
j
Germany
Porcine tongues 68
k
0:8; 1:6, 30; 0:3; 0:13, 7; 0:8; 0:46 USA
50.8
l
USA
Chitterling >50
m
0:3 USA
Pork meat 26.7
e
USA
20
i
Brazil
10.83
n
0:3, 3B phage type 2; 0:3, 4 phage type 8; biotype 1; 2 Japan
17
o
0:3 Norway
Drinking water 5
p
Germany
54
q
USA
Vegetables 1
r
Italy
7
s
France
50
t
France
a
From Vidon D and Delmas C (1981) Incidence of Yersinia enterocolitica in raw milk in Eastern France. Applied and Environmental Microbiology 41: 353–359.
b
From Moustafa M, Ahmed A and Marth E (1983) Occurrence of Yersinia enterocolitica in raw and pasteurized milk. Journal of Food Protection 46: 276–278.
c
From Schiemann D (1978) Association of Y. enterocolitica with the manufacture of cheese and occurrence in pasteurized milk. Applied and Environmental
Microbiology 36: 274–277.
d
From Tibana A, Warnken M, Nunes M et al. (1987) Occurrence of Yersinia enterocolitica in raw and pasteurized milk in Rio de Janeiro, Brazil. Journal of
Food Protection 50: 580–583.
e
From Hamama A, El Marrakchi A and El Othmani F (1992) Occurence ofYersinia enterocolitica in milk and dairy products in Morocco. International Journal
of Food Microbiology 16: 69–77.
f
From Hughes J and Jensen N (1981) Yersinia enterocolitica in raw goat’s milk. Applied and Environmental Microbiology 41: 309–310.
g
From Simsek O and Arici M (1994) Pathogenic microorganisms in cheese and their foodborne disease. In: Cheese With All Aspects, 2nd edn, Tekirdag
˘
:
Trakya University.
h
From Davies A, Capell C, Jehanno D, Nychas G and Kirby R (2001) Incidence of foodborne pathogens on European fish. Food Control 12: 67–71.
i
From Warnken A, Nunes M and Noleto A (1987) Incidence of Yersinia enterocolitica in meat samples purchased in Rio de Janeiro, Brazil. Journal of Food
Protection 50: 578–579, 583.
j
From Kleinlein N, Unterman F and Beissner H (1989) Occurrence of Salmonella and Ye r s i n ia species as well as Listeria monocytogenes in minced meat.
Fleischwirtschaft 69: 1474–1476.
k
From Doyle MP, Hugdahl MB and Taylor SL (1981) Isolation of virulentYersinia enterocolitica from porcine tongues. Applied and Environmental Microbiology
42: 661–666.
l
Harmon MC (1984) A study of the incidence and pathogenic potential of Yersinia enterocolitica in Indiana pork. Dissertation Abstracts International, B 44:
3707.
m
From Lee LA, Gerber DR, Lonsway JD et al. Yersinia enterocolitica O:3 infections in infants and children, associated with the household preparation of
chitterlings. New England Journal of Medicine 322: 984–987.
n
From Fukushima H, Hoshima K, Nakamura R and Ito Y (1987) Occurrence of Ye r s i n ia spp. in raw beef, pork and chicken. Zentralblatt fur Bakteriologie
Mikrobiologie und Hygiene (B) 184: 50–59.
o
From Johannessen G, Kapperud G and Kruse H (2000) Occurrence ofYersinia enterocolitica in Norwegian pork products determined by PCR method and a
traditional culturing method. International Journal of Food Microbiology 54: 75–80.
p
From Schindler P (1984) Isolation of Yersinia enterocolitica from drinking water in South Bavaria. Zentralblatt fur Bakteriologie Mikrobiologie und Hygiene
180: 76–84.
q
From Langeland G (1983) Yersinia enterocolitica and Yersinia enterocolitica-like bacteria in drinking water and sewage sludge. Acta Pathologica,
Microbiologica et Immunologica Scandinavica 91: 179–185.
r
From Gola S, Previdi M, Mutti P and Belloli S (1990) Microbiological investigation of frozen vegetables, incidence of Listeria and other psychrotrophic
pathogens. Industria Conserve 65: 36–38.
s
From Catteau M, Krembel C and Wauters G (1985) Yersinia enterocolitica in raw vegetables. Science Aliments 5: 103–106.
t
From Darbas H, Riviere M and Obertic J (1985) Ye r s i ni a in refrigerated vegetables. Science Aliments 5: 81–84.
6244
YERSINIA ENTEROCOLITICA
/Properties and Occurrence
0024 Although normal detergents and disinfectants used
in the food industry are effective for eliminating Yer-
sinia enterocolitica, their effect is reduced if fatty
residues are present. The regular use of steam
cleaning instead of cleaning with hot water at 85
C
has been used successfully at a milk pasteurization
plant.
0025 Handlers of meal are the last critical control point
before foods reach the table. Therefore, several prac-
tical food-handling precautions could reduce the risk
of contamination of food by this microorganism.
Cross-contamination of foods can be avoided by sep-
arating cooked and raw food and also by washing
food handlers’ hands, cutting boards, and contamin-
ated surfaces. Practical recommendations can be
followed by consumers, such as avoiding the con-
sumption of raw or undercooked pork, raw milk, or
related byproducts, and washing hands carefully
before eating, preparing food after contact with
animals, and after handling raw meat. After handling
raw chitterlings, it is recommended that hands and
fingernails be cleaned thoroughly with soap and
water before touching children or their toys, bottles,
or pacifiers.
See also: Epidemiology; Freezing: Principles; Heat
Treatment: Ultra-high Temperature (UHT) Treatments;
Chemical and Microbiological Changes; Electrical
Process Heating; Irradiation of Foods: Basic Principles;
pH – Principles and Measurement; Preservatives:
Classifications and Properties; Yersinia enterocolitica:
Detection and Treatment
Further Reading
Adams MR and Moss MO (1995) Food Microbiology.
Cambridge: The Royal Society of Chemistry.
Bottone EJ (1999) Yersinia enterocolitica: overview and
epidemiological correlates. Microbes and Infection
1: 323–333.
Doyle MP and Cliver DO (1990) Yersinia enterocolitica. In:
Cliver DO (ed.) Foodborne Diseases, pp. 223–
228.San Diego, CA: Academic Press.
Eley AR (1992) Microbial Food Poisoning. London: Chap-
man & Hall.
Forsythe SJ (2000) The Microbiology of Safe Food. Oxford:
Blackwell Science.
Greewood MH (1993) Yersinia enterocolitica. Properties
and occurrence. In: Macrae R, Robinson RK and Sadler
MJ (eds) Encyclopaedia of Food Science, Food Technol-
ogy and Nutrition. London: Academic Press.
Jay JM (2000) Modern Food Microbiology, 6th edn.
Gaithersburg, MD: Aspen.
Schiemann DA (1989) Yersinia enterocolitica and Yersinia
pseudotuberculosis In: Doyle MP (ed.) Foodborne
Bacterial Pathogens, pp. 601–672. New York: Marcel
Dekker.
Detection and Treatment
A Ramesh, B P Padmapriya, S Bharathi and
M C Varadaraj, Central Food Technological Research
Institute, Mysore, India
Copyright 2003, Elsevier Science Ltd. All Rights Reserved.
Background
0001Yersinia enterocolitica is an invasive enteropathogen
prevalent in the environment and often isolated from
soil, water, food, and clinical sources. The serotypes
of Y. enterocolitica associated with disease in humans
are O:3, O:9, O:8, and O:5, 27, and all harbor a
70–75-kb virulence plasmid. The bacterium has
been recognized as a significant foodborne pathogen
owing to its ability to survive in both vacuum-packed
and refrigerated food samples. Thus, in the light of
food hygiene and public health, it is imperative to
develop rapid methods of detecting Y. enterocolitica.
Various methods consisting of conventional cultural
methods, detection of virulence plasmid, immu-
nological methods, and rapid nucleic acid-based
techniques have been described for the detection and
identification of Y. enterocolitica. In an infection, the
principal clinical feature in humans is abdominal pain
and diarrhea accompanied by fever. Reactive arthritis
and erythema nodosum have also been reported as
common complications. Several cases of diarrhea
resulting from Y. enterocolitica infection resolve on
their own, thus avoiding the need for an antibiotic
treatment. However, in the case of a severe infection,
antibiotics are administered. The following section
describes the methods of detection and treatment of
Y. enterocolitica.
Detection of
Yersinia enterocolitica
0002The common food samples associated with Y. enter-
ocolitica infection are pork, milk and milk products,
and raw vegetables. The detection of pathogenic
strains of Y. enterocolitica from food samples and
clinical specimens is mainly based on the isolation of
the bacterium. A scheme of the different detection
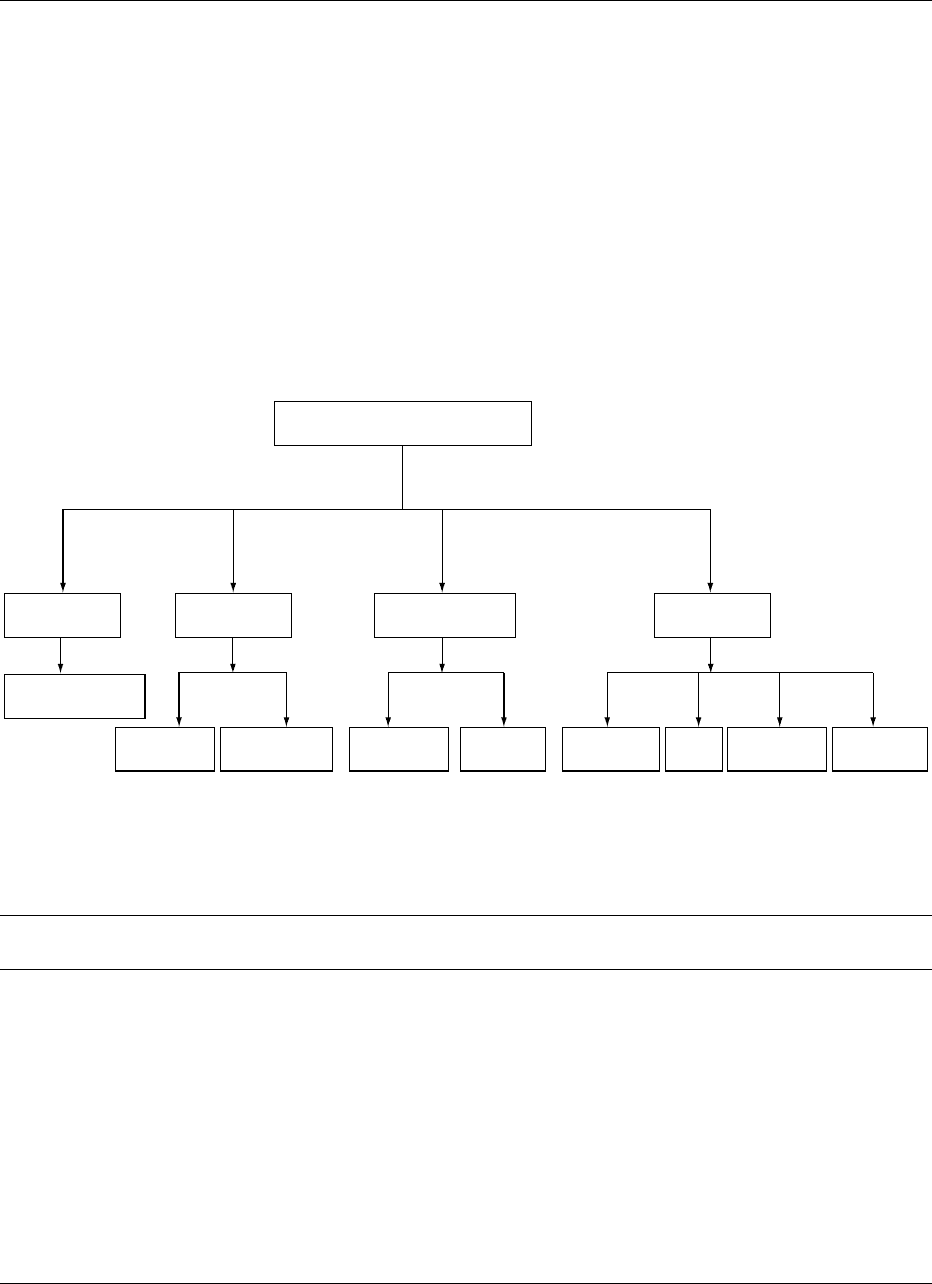
methods followed for Y. enterocolitica is shown in
Figure 1.
Conventional Methods of Detection
0003Yersinia enterocolitica is a Gram-negative rod or
ovoid, facultatively anaerobic, oxidase-negative,
catalase-positive nonsporulating motile bacterium.
The isolation of this bacterium from food samples is
difficult, because it is present in low numbers and is
slow growing compared to other coexisting members
YERSINIA ENTEROCOLITICA
/Detection and Treatment 6245
of the enterobacteriaceae present in the background
microflora. This underscores the need for a selective
enrichment technique to facilitate the isolation of the
bacterium. A basic isolation scheme involves preen-
richment in a highly nutritious, well-buffered medium
containing peptone, yeast extract, and mineral salts at
temperatures ranging from 4 to 37
C over 1–9 days.
The salient features of the various types of enrichment
procedures are indicated in Table 1.
0004 Selective enrichment media like bile oxalate sor-
bose (BOS) broth, and phosphate buffer saline
(PBS) supplemented with sorbitol and bile salts
with a postenrichment alkali treatment has been
widely used to enrich Y. enterocolitica from food
samples. This method is simple, sensitive, and rapid,
eliminating a large number of contaminating
non-Yersinia species. Y. enterocolitica is also a psy-
chrotroph, capable of growing under refrigerated
conditions. Hence, cold enrichment can increase the
isolation rate of the bacterium. Irgasan–ticarcillin–
chlorate (ITC) enrichment has been shown to be
more efficient in isolating pathogenic bioserotype
from pork. The enriched culture is plated on to
the selective media cefsulodin–irgasan–novabiocin
tbl0001 Table 1 Enrichment broth and growth conditions used for the isolation of Yersinia enterocolitica
Primary
enrichment
Incubation
temperature (
C)
Incubation
period(days)
Secondary
enrichment
Incubation
period (days)
Incubation
temperature (
C)
MRB 23 5
PB 4 14
PB 4 14 MRB 23 5
CMB 23 28 MRB 23 5
SC 37 1
RMC 22 3
BHI 8–10 2 SB 22–28 2
ITC RT 2
PBS 4 2
PBSSB 4 21
BHI 8–10 2 KOH RT
BHI 8–10 2 SC RT 2
HOBS 4 5
PBS 4 21 MRB 27 2
BOS 22 3–5
BHI, brain–heart infusion broth; BOS, bile–oxalate–sorbitol broth; CMB, cooked meat broth; HOBS, hemoglobin–oxalate–bile–sorbitol
broth;ITC, irgasan–ticarcillin–chlorate; MRB, modified Rappaport broth; PB, Butterfields phosphate buffer; PBS, phosphate-buffered saline;
PBSSB, phosphate-buffered saline–sorbitol–bile salts; RMC, restrictive MgCl
2
broth; SB, sorbitol bile broth; SC, selenite cystine.
Detection of Yersinia enterocolitica
Conventional
method
Immunological
methods
Virulence plasmid
mediated methods
Nucleic acid
methods
Enrichment/Plating
on selective media
Agglutination Immunoassays
Low calcium
response
CV and CR
binding
Gene probe PCR
5' nuclease
assay
PCR-ELISA
fig0001 Figure 1 Schematic representation of the various detection methods for Yersinia enterocolitica.
6246
YERSINIA ENTEROCOLITICA
/Detection and Treatment
(CIN) agar and incubated for 24–48 h at 32–37
Cto
obtain characteristic colonies with a deep red center
(like a bull’s eye) with an entire edge and a transparent
border measuring 0.5–1.0 mm in diameter. Suspected
Yersinia colonies from CIN plates are selected and
suspended individually in trypticase soya broth
(TSB) for further characterization through diagnostic
biochemical tests, as indicated in Table 2. Yersinia
enterocolitica has been essentially classified into six
biogroups, i.e., 1A, 1B, 2, 3, 4, and 5. Biotype 6 is
rare.
0005 Current methods based on selective enrichment
merely detect the presence of Y. enterocolitica, and
these methods fail to recover all pathogenic biosero-
types. Further improvements in the specific detection
of the bacteria can be achieved through immuno-
logical and nucleic acid-based methods.
Immunological Detection of
Y. enterocolitica
0006 Immunological methods have been reported since the
early detection of Y. enterocolitica as an advancement
over conventional microbiological tests. The methods
that have been widely accepted include agglutination
tests and immunoassay.
0007 Agglutination tests Latex slide agglutination and
tube agglutination (Widal) tests are commonly used
and form the basis for many commercially available
kits for the rapid detection of Y. enterocolitica O:3
and O:9 antibodies in the serum. Latex of 0.9 mm
particle size was coated with specific antibodies
raised against serotypes O:3, O:5, O:6, O:8, and
O:9 of Y. enterocolitica. The latex reagents specific-
ally detected the O-antigen of Y. enterocolitica, with
no cross-reactivity between the serotypes. Alcohol-
treated bacterial cells are used as antigens in some
cases, and an agglutination titer of 640 or a fourfold
or greater increase in the titer is an indication of
recent or actual infection. Commercial kits are
available to detect O:3 and O:9 antigens of
Y. enterocolitica individually or in combination,
using the latex agglutination method.
0008Immunoassays The lack of sensitivity and specifi-
city of the agglutination tests hinders their ap-
plication as a routine detection method. However,
immunoassays like surface adhesion immunofluores-
cence (SAIF) technique, enzyme immunoassay (EIA),
immunoblot, and enzyme-linked immunosorbent
assay (ELISA) can alleviate this problem. SAIF has
been used to detect Y. enterocolitica in broth and
enriched meat cultures, with a polycarbonate mem-
brane to trap the cells on the surface of the membrane
prior to detection by immunofluorescence.
0009EIA was developed for the detection of Yersinia
immunoglobulin (Ig) complexes of known Ig class.
Immune complexes are attached to polystyrene
microtiter plates by rabbit antihuman immunoglobu-
lins. Detection of Y. enterocolitica O:3 antigens was
demonstrated using Fab fragments of alkaline phos-
phatase-conjugate antibody against the same sero-
type. Methods to differentiate serological responses
to Y. enterocolitica O:9 from responses to Brucella
have been very successful. However, immunoblots
tbl0002 Table 2 Differentation of Yersinia enterocolitica biogroups
Test Biogroup
1A 1B2345 6
a
Indole production þ þ
Esculin hydrolysis þ/
Voges–Prausker test þ þ þþþþ
L-Ornithine decarboxylase þ þ þþþþ/þ
Pyrazinamidase þ þ
Lipase þ þ
D-Glucosidase þ
Acid from
Inositol þ þ þþþþ þ/
Salicin þ
L-Sorbose þ þ þþþ þ
Tr e h a l o s e þ þ þþþ þ
D-Xylo se þþþþV þ
Sucrose þ þ þþþþ
a
This biotype is relatively rare.
V, variable reacton.
Modified from Bottone EJ (1999) Yersinia enterocolitica: overview and epidemiological correlates. Microbes and Infection 1: 323–333; Wauters G (1981)
Antigens of Yersinia enterocolitica. In: Bottone EJ (ed.), pp. 41–53. Boca Raton, FL: CRC Press.
YERSINIA ENTEROCOLITICA
/Detection and Treatment 6247

and ELISA targeting the Yersinia outer membrane
proteins (YOPs) are more sensitive and specific than
other serological tests for yersiniosis.
0010 Monoclonal antibodies specific for the lipopolysac-
charide (LPS) O antigens of Y. enterocolitica serotype
O:3 can be used for the detection of Y. enterocolitica
in colony immunoblots. This method has been shown
to be sensitive in detecting a single colony of Y. enter-
ocolitica in the presence of 3.110
8
heterologous
organisms. Besides, the assay was specific with no
significant cross-reactivity against any related sero-
types. An immunoblot kit called recom Blot Yersinia
IgG and recom Blot IgM/IgA has been developed and
provides recombinant Yersinia antigens in a test strip
format to detect IgG, IgM, or IgA antibodies directed
against Y. enterocolitica and Y. pseudotuberculosis.
0011 ELISAs using either purified lipopolysaccharide
or formalinized whole cells expressing virulence
plasmid-coded surface antigen (pYV
þ
cells) can be
performed to detect Y. enterocolitica. It has been
shown that ELISA can specifically detect pYV anti-
bodies in sera, cross-adsorbed to formalinized pYV-
cured Y. enterocolitica O:3 cells prior to the assay.
The serological response against YOPs using AB-
ELISA was used to detect the O:9 serotype of
Y. enterocolitica. In order to avoid interference by
Y. enterocolitica O:9 LPS with YOPs in serological
analysis, an antigenic preparation of YOPs was
obtained from Y. enterocolitica O:7. There is a high
degree of homology between YOPs of different Yersi-
nia species and an absence of cross-reactivity between
Y. enterocolitica O:7 LPS and Y. enterocolitica O:9
LPS. The commercially available Y. enterocolitica
ELISA kit provides a high diagnostic sensitivity
capable of differentiating IgG from IgA and IgM.
0012 Although a host of immunological methods are
available to detect Y. enterocolitica for clinical appli-
cations, the use of these assays in a food system is
comparatively limited. An immunomagnetic separ-
ation technique has been shown as an efficient device
to sequester Y. enterocolitica in food samples and
facilitate its sensitive detection. The major factors
limiting the use of immunological techniques for the
detection of Y. enterocolitica in food systems are
the cross-reactivity with the background microflora
present in food samples and the inhibitors present in
the food matrix itself.
Detection of Virulent Plasmid-bearing (pYV
1
)
Strains
0013 The pathogenic strains of Y. enterocolitica are char-
acterized by the presence of a 70–75-kb plasmid
which encodes for a number of virulence factors
manifested as conspicuous colony morphology, auto-
agglutination, dye binding capacity, and low calcium
response. Plasmid-mediated phenotypic expression
has been used to detect virulent strains and to
discern them from avirulent plasmid-less strains.
In a calcium-deficient medium like the brain–heart
infusion agarose (BHO) calcium response of viru-
lent strain was tested. At 37
C, plasmid-bearing
virulent cells (pYV
þ
) appear as pin-point colonies
0.36 mm in diameter, whereas avirulent cells
(pYV
) form distinctly larger colonies. The CIN
agar medium incorporated with crystal violet can
distinguish between pathogenic and nonpathogenic
strains. At 32
C, the colony morphology appears
similar for both the strains. However it has been
demonstrated that at 37
C, plasmid-bearing patho-
genic strains appear as densely stained microcolo-
nies compared to the nonpathogenic strains. Direct
detection of a plasmid-bearing virulent strain of Y.
enterocolitica has been carried out in artificially
contaminated food samples like pork chops, ground
pork, cheese, and zucchini. Enriched samples plated
on BHO incorporated with Congo red and incu-
bated at 37
C form red pin-point colonies as a
manifestation of plasmid-mediated dye binding
and a low calcium response. Thus, the Congo red
binding technique is suitable for direct detection
and isolation of pathogenic Y. enterocolitica using
a single medium.
Detection by Nucleic Acid Probes
0014The physiological traits encoded by the virulent plas-
mid are only expressed at 37
C, which also favors
plasmid loss accompanied by elimination of virulent
traits. Thus, the instability of the plasmid limits its use
as a tool for detecting virulent Y. enterocolitica in
clinical and food samples. The emergence of nucleic
acid probes has provided an efficient tool to detect
genes in Y. enterocolitica that encode specific
pathogenic traits. Such gene probes can be used in
colony- or dot-blot hybridization to directly detect
Y. enterocolitica in the presence of high background
microflora.Additionally,these probes canbeevaluated
as a substitute to tissue culture-based assay to ascertain
the invasive phenotype of pathogenic strains.
0015The target regions in a probe-based diagnostic
assay can be unique sequences within chromosomal
DNA, ribosomal RNA, or plasmid DNA. The riboso-
mal RNA is widely preferred as a target gene owing to
its ubiquity and relatively high copy number, which
enhances the assay sensitivity. The GENE-TRAK col-
orimetric hybridization assay for Y. enterocolitica has
been developed, employing probes directed against
specific signature sequences of 16 s rRNA. This assay
has been shown to be a convenient alternative to
conventional microbiological procedures, yielding
presumptive results in a significantly shorter time.
6248
YERSINIA ENTEROCOLITICA
/Detection and Treatment

However, this method lacks the discriminatory power
to differentiate virulent from avirulent strains.
0016 Probes targeting virulence plasmid genes can be
employed to specifically detect pathogenic Y. entero-
colitica serogroups and distinguish them from en-
vironmental Yersinia species, which are frequently
encountered in food samples. A synthetic radio-
actively labeled 19-mer oligonucleotide probe based
on the plasmid-encoded Yersinia adhesin A (Yad A)
gene has been used in colony hybridization to
detect pathogenic Y. enterocolitica in pork samples.
The probe demonstrates a superior estimation of
virulent strains in the samples than conventional
methods. Polymerase chain reaction (PCR)-generated
nonradioactive probes are safe, inexpensive, and
shelf-stable, and can be used in the detection of
the organism. In colony hybridization, the DIG
(digoxigenin)-labeled PCR-generated Vir F and Yad
A amplicons are able to detect pathogenic Y. entero-
colitica in artifically contaminated food samples and
indicate equivalence with the PCR assay and pheno-
typic test for pathogenicity.
0017 Spontaneous loss of plasmids in Y. enterocolitica
during in-vitro replication is frequently encountered
either in the environment or in the laboratory. This
fosters the need to develop probes targeting the
chromosomally encoded virulence factors like the
attachment invasion locus (Ail) and the heat-stable
enterotoxin (Yst). The gene coding for the attachment
invasion locus (Ail) has been found uniquely in patho-
genic strains of Y. enterocolitica, whereas the invasion
(Inv) gene in all Yersinia spp. DIG-labeled Inv and
Ail probes has been used to differentiate pathogenic
from nonpathogenic strains. A PCR-amplified DIG-
labeled Yst probe has been used in colony hybridiza-
tion to detect and differentiate between pathogenic
and nonpathogenic strains in naturally and artificially
contaminated pork and milk samples following
enrichment in ITC enrichment broth. The hybridiza-
tion results are concordant with those from biochem-
ical and serological tests, and a detection limit of
10 colony-forming units (CFU) ml
1
in the original
sample has been achieved. The use of a multi-
plex riboprobe can be adopted as a comprehensive
strategy to detect multiple targets, thus enhancing
assay sensitivity and ensuring detection of virulent
Y. enterocolitica irrespective of plasmid loss.
Detection by Polymerase Chain Reaction
0018 The use of gene probe-based hybridization assays
to detect Y. enterocolitica is limited by the lack of
sensitivity. PCR allows rapid and selective identifica-
tion of Y. enterocolitica and fulfils the criteria for
specificity and sensitivity. The Yad A gene located
on the virulence plasmid (pYV) encoding for an outer
membrane polymeric protein has been used as a target
to detect the presence of pathogenic Y. enterocolitica in
retailed pig tongue and minced meat. However, loss of
pYV is frequently encountered under certain condi-
tions of handling, especially in food samples. This
leads to the possibility of false-negative results. The
chromosomally encoded attachment invasion locus
(Ail) is characteristically associated with virulence
and can be an appropriate target to detect pathogenic
Y. enterocolitica. Ail-specific primers have been used
in PCR to identify virulent strains in blood, and the
levels of sensitivity achieved indicate the potential of
PCR in the diagnosis of transmission-related bactere-
mia caused by Y. enterocolitica. A two-step PCR
targeting the Ail gene has been employed to detect
pathogenic strains in environmental water, and the
results have demonstrated a superior specificity and
sensitivity over cultural methods.
0019A PCR method based on the targeting of the rfb
C gene involved in the biosynthesis of the O side chain
of Y. enterocolitica O:3 has enabled the detection
and differentiation between pathogenic strain of
Y. enterocolitica of serotype O:3 and Y. pseudotuber-
culosis and other pathogenic Y. enterocolitica. PCR
enables reliable and sensitive detection when applied
to pure cultures, but its efficiency is markedly curtailed
when applied to food and clinical samples. This is
mainly due to the potential inhibitors or high levels of
background microflora present in such samples.
Therefore, adequate sample preparation is required
to either eliminate such inhibitors or concentrate target
cells to yield satisfactory detection levels. Selective
enrichment followed by buoyant density gradient cen-
trifugation provides an efficient sample preparation
method prior to PCR. This treatment method has
facilitated the detection of 10 CFU ml
1
of the bacter-
ium in pork using a multiplex PCR simultaneously
targeting the plasmid-borne Yad A gene and the Yersi-
nia-specific 16S rRNA region. Immunomagnetic sep-
aration (IMS) of the target cells from meat samples has
enabled a nested PCR assay to detect 10–30 CFU g
1
meat in the presence of 10
6
-fold excess background
microflora. Thus, IMS provides an efficient way of
excluding the PCR inhibitors from the sample and
has the potential to be exploited for automation.
0020Methods for detecting virulent Y. enterocolitica
based on PCR involve gel electrophoresis for product
analysis and the use of ethidium bromide to stain
the gels, which is hazardous and impractical for rou-
tine analysis in food monitoring laboratories. The
fluorogenic 5
0
nuclease assay is an attractive option
for rapid detection of virulent Y. enterocolitica. The
assay exploits the 5
0
–3
0
nuclease activity of Taq DNA
polymerase and releases a probe with a fluorescent
reporter dye and a quencher, which hybridizes to
YERSINIA ENTEROCOLITICA
/Detection and Treatment 6249
