Caballero B. (ed.) Encyclopaedia of Food Science, Food Technology and Nutrition. Ten-Volume Set
Подождите немного. Документ загружается.


are common findings. The disease is characterized by
bleeding from inflamed colonic mucosa, tenesmus,
mucus discharge, and abdominal pain. The majority
of patients remain asymptomatic. Diversion colitis
is likely caused by a deficiency of SCFA, which serve
as luminal nutrients for colonocytes. The differen-
tial diagnosis for diversion colitis includes acute
self-limited colitis, antibiotic-associated colitis, and
preexisting UC or CD. The definitive treatment of
diversion colitis is restoration of intestinal continuity.
Surveillance for cancer in the diverted segment is not
necessary, provided that the underlying condition for
which the operation was performed has no malignant
potential. Randomized controlled studies have not
confirmed a beneficial role of SCFA in the treatment
of diversion colitis, a peculiar finding. These studies
were hampered by the small sample size and short
duration of treatment. In those with preexisting IBD,
SCFA combined with antiinflammatory drugs may be
effective.
0025 A low-residue diet is recommended during acute
phases of colitis, the idea being that insoluble par-
ticles irritate the bowel and make diarrhea worse.
Recently, however, the rarity of UC in developing
countries, together with the ability of dietary fibre
to affect colonic function and its bacterial content,
has suggested that a low intake of fiber might be a
factor in causing UC. A high-fiber diet can be pre-
scribed for patients during quiescent phases of
disease.
0026 Initial studies suggested a reduced postoperative
morbidity and mortality in patients with UC receiving
TPN. However, parenteral nutrition is not an effect-
ive primary therapy for UC. Retrospective studies
have failed to provide evidence for the use of TPN
in inducing remission of UC. Moreover, five prospect-
ive studies investigating the use of TPN in inducing
remission in UC failed to show any benefit for TPN
versus control groups. In all five studies, there was a
mean 37% initial response rate and only a 12% sus-
tained response rate. TPN appears to have little influ-
ence on refractory patients with active disease, and
rarely can TPN avert colectomy. TPN can be useful to
prepare the malnourished patient for surgery as well
as providing postoperative nutritional support. There
have been relatively few studies looking at the use of
elemental diets in UC. It is generally considered that
enteral nutrition is not effective in achieving remis-
sion in active ulcerative colitis.
0027 The role of diet and nutrition in patients with IBD
remains controversial. By applying an orderly and
comprehensive approach to management, many of
the complications of IBD can be contained or pre-
vented. While the role of diet continues to evolve, its
efficacy in the management of IBD is undisputed.
Diet and Nutrition in Irritable Bowel
Syndrome
0028Irritable bowel syndrome (IBS) is defined as a func-
tional bowel disorder in which abdominal pain is
associated with defecation or a change in bowel
habit, with features of disordered defecation and dis-
tention. Criteria for IBS have been formalized in the
Rome Criteria (Table 6). IBS is a disorder that can be
diagnosed positively on the basis of a series of symp-
tom criteria and limited evaluation to exclude organic
disease. The incidence of IBS has been estimated to be
1% per year. Prevalence data estimate a range of 2.9–
20%. Patients have been divided into subgroups
based on the predominant symptom. Symptom sub-
groups include constipation-predominant IBS, diar-
rhea-predominant IBS, and IBS with alternating
bowel movements. The prevalence of IBS is lower in
the elderly and higher in female patients. Only 10–
25% of patients with IBS seek medical care. The
economic impact in the USA is estimated at $25 bil-
lion annually. IBS accounts for 2.4–3.5 million phys-
ician visits in the USA annually, making it the most
common diagnosis in gastroenterologists’ practice
(12% of primary care visits, 28% of all gastroenter-
ologist’s patients).
Pathophysiology
0029There is no single physiological mechanism respon-
sible for symptoms of IBS. IBS is considered a bio-
psychosocial disorder resulting from a combination
of psychosocial factors, altered motility and transit,
and increased sensitivity of the intestine or colon
(Table 7). It has been hypothesized that altered per-
ipheral functioning of visceral afferents and the cen-
tral processing of afferent information are important
in the altered somatovisceral sensation and motor
dysfunction in patients with IBS. It has been postu-
lated that persistent neuroimmune interactions after
tbl0006Table 6 Criteria for the diagnosis of IBS
Manning criteria Pain relieved by defecation
More frequent stools at the onset of pain
Looser stools at the onset of pain
Visible abdominal distention
Passage of mucus
Sensation of incomplete evacuation
Rome II criteria At least 12 weeks or more, which need
not be consecutive in the previous
12 months of abdominal pain or
discomfort with two of three features:
relief with defecation, onset associated
with a change in the frequency of stool,
onset associated with a change in
the appearance of stool
1536 COLON/Diseases and Disorders
infectious gastroenteritis resulting in continuing sen-
sorimotor dysfunction might be a cause of IBS. Infec-
tious diarrhea precedes the onset of IBS symptoms in
7–30% of patients.
0030 In some patients, carbohydrate intolerance may
contribute to the symptoms of IBS. Data suggest
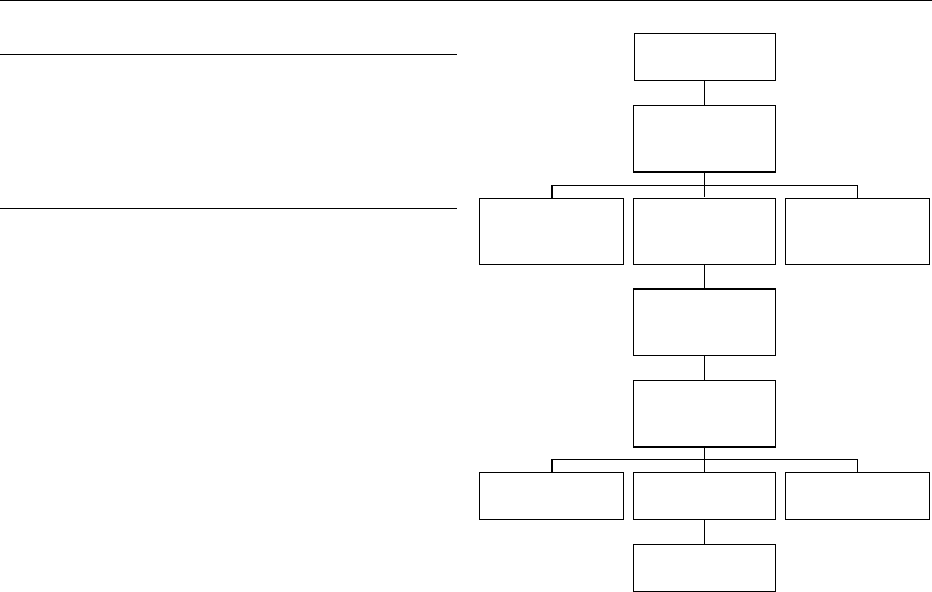
that food allergens may play a role in IBS (Figure 1).
Symptoms often improve with dietary exclusion.
Stress and emotions affect gastrointestinal function
and cause symptoms in patients with IBS. Psychologic
symptoms that are more common in patients with IBS
include somatization, anxiety, hostility, phobia, and
paranoia.
Diagnosis
0031 Many patients’ symptoms fluctuate over time. Re-
gardless, IBS is a ‘safe’ diagnosis. Patients with IBS
have a benign course without any risk of developing
organic disease. The diagnosis of IBS first involves a
careful assessment of the patient’s symptoms. Man-
ning or Rome criteria can be used to identify patients
with IBS. A thorough physical examination and a
limited series of initial investigation are needed to
exclude organic structural, metabolic, or infectious
diseases. Investigations include hematology and
chemistry tests, erythrocyte sedimentation rate, stool
examination for occult blood, ova, and parasites, and
possible flexible sigmoidoscopy.
Food Intolerance
0032 Data from dietary elimination and food challenge
studies support the role of diet in the pathogenesis
of a subgroup of IBS patients. The term ‘food intoler-
ance’ encompasses nonimmunologically mediated
adverse reactions to food, which resolve following
dietary elimination and are reproduced by food chal-
lenge. Food allergy or hypersensitivity is used to
describe conditions in which an immunological mech-
anism may be demonstrable. Food aversion is a psy-
chological avoidance response. A prevalence for food
intolerance of 5% has been reported in the general
population. Food hypersensitivity is a common per-
ception amongst IBS patients with 20–65% attribut-
ing their symptoms to adverse food reactions. The
effect of dietary exclusion followed by food challenge
has been investigated in several trials. Food intoler-
ances have been recognized in 6–58% of cases, with
milk, wheat, and eggs being the most commonly
implicated foods. In the largest study, the effect of
an exclusion diet was evaluated in 200 IBS patients.
Symptomatic improvement was reported in 91/189
(48%) patients and was maintained for a mean of
14.7 months. Following dietary challenge, 73/91
(80.2%) of responders identified one or more food
intolerances. The investigators conclude that a por-
tion of IBS patients may benefit from dietary
manipulation.
0033The bowel mucosa acts as a physical barrier to a
variety of intraluminal dietary and microbial anti-
gens. Under normal physiological conditions intact
food antigens can penetrate the mucosal barrier via
transcellular or paracellular routes. The mechanism
by which the mucosal immune system maintains a
state of immunological tolerance is not clear. Studies
demonstrating a positive response to elimination diets
support the role of a food hypersensitivity reaction in
IBS. An immune-mediated food hypersensitivity re-
sponse involving IgE and IgG antibodies has been
postulated as the underlying mechanism in patients
with IBS.
0034While there is no clear evidence to suggest that IBS
is an infective condition, up to 30% of patients de-
velop symptoms after an episode of gastroenteritis.
Food antigen
challenge
Mucosal antigen
processing
(B cells, T cells)
IgG
response
IgE
immediate and
delayed reaction
Other non-IgE
mediated
Mast cell
sensitization
degranulation
Release of
mediators
(histamine etc)
Abnormal mucosal
sensitivity
Abnormal
secretory response
Abnormal
motility
Irritable bowel
syndrome
fig0001Figure 1 Pathogenesis of food hypersensitivity in IBS.
tbl0007 Table 7 Pathophysiology of IBS
Biopsychosocial disorder
Abnormal motility
Heightened visceral perception
Psychologic distress
Intraluminal factors – lactose, bile acids, short-chain fatty acids,
food allergen
Postinfectious alteration of gut function
COLON/Diseases and Disorders 1537

Infective and inflammatory conditions of the bowel
cause an increased mucosal permeability, thereby ex-
posing the immune system to an increased load of
dietary and microbial antigens. The production of a
variety of proinflammatory and immunomodulatory
cytokines may serve to prime the mucosal and sub-
mucosal immune system establishing a hypersensitiv-
ity response. Altered bowel flora has been reported in
patients with IBS. Restoration of bowel flora whether
by dietary manipulation or through the use of pro-
biotics has been suggested as a treatment for IBS.
Treatment
0035 The dietary treatment of patients with IBS has
centered around bran supplementation, manipulating
the dietary fiber content of the diet and the identifica-
tion of food intolerance. There are currently no
evidence-based guidelines on how dietitians should
treat patients with IBS. An in-depth assessment of a
patient’s dietary intake is essential prior to any thera-
peutic dietetic intervention. A history regarding the
onset of symptoms in relation to any dietary changes
is often useful. Dietary intervention needs to be indi-
vidualized with respect to the patient’s symptoms.
Of the eight studies evaluated, five identified food
intolerance as a major contributor to symptoms.
There are no randomized control trials in this area
primarily due to the impracticality of constructing a
trial design. In all trials, the methods used to assess
the effect of intolerance to suspect foods on symp-
toms varied. In summary, seven studies mentioned
dairy products, six coffee, and five wheat. Others
cite eggs, corn, potatoes, onions, fruits, and vege-
tables. In the majority of the studies, the patients
with diarrhea responded favorably to an exclusion
diet compared to other subtypes of IBS. The recom-
mendation that elimination diets control the
symptoms of IBS is based on poorly designed and
incomplete trials. The absence of any objective symp-
tom assessment in the trials raises questions about
their validity.
0036 The mainstay of dietary therapy for IBS has
centered around the manipulation of dietary fiber.
Rees et al. conducted a critical review of clinical trials
examining the effect of dietary fiber on symptoms in
patients with IBS. In the review, it was shown that six
out of eight investigations detected no significant dif-
ference in most of the symptoms of IBS between fiber
and placebo. In the eight trials, the amount of supple-
ment varied, the form in which the fiber was adminis-
tered differed, and the type of fiber supplement was
different. The literature does not support any benefi-
cial effects of increasing insoluble nonstarch polysac-
charides in IBS patients. Increasing insoluble wheat
products in the diet may be of some benefit in patients
with predominantly symptoms of constipation. Many
patients complain of bloating with higher doses of
fiber. Bran is reported to be no better than placebo
in relief of overall IBS symptoms and may be worse
than a normal diet for symptoms of IBS caused by
intraluminal distention. Fiber may induce bloating by
increasing residue loading and bacterial fermentation
without accelerating the onward movement of the
increased residue. Nonetheless, there appears to be
significant improvement in constipation if sufficient
quantities of fiber (20–30 g day
1
) are consumed. As
a result, it is common practice to start with a low
dose, increasing gradually, and abandoning high
levels of supplementation (> 30 g day
1
) if patients
experience worsening of symptoms. Therefore, it can
be concluded that fiber may have a role in treating
constipation with a minimal role in the relief of
abdominal pain and diarrhea.
0037The role of carbohydrate and sorbitol is not rou-
tinely considered in the management of IBS. Trials
cannot confirm a true malabsorption of carbo-
hydrates in patients with IBS. Nonetheless, studies
have shown that patients with IBS develop symptoms
after being exposed to a sorbitol diet, when compared
to controls. One-third of those with IBS reported
lactose intolerance on a subjective basis. The percent-
age of lactose maldigesters in patients with IBS is
the same as in healthy subjects, but the number of
subjects reporting lactose intolerance is higher (60%
compared to 27%). There is a strong relationship
between subjective lactose intolerance and IBS. The
inconclusive findings of, and association of, lactose
intolerance and IBS can be explained by poorly
designed studies. Lactose intolerance has been associ-
ated with GI symptoms, and whether this is due to
lactase deficiency or increased sensitivity cannot be
answered.
0038In summary, the goal of dietary manipulation in
patients with IBS is to help patients control their
symptoms. Dietary assessment is essential for all
patients with determination of their present dietary
intake. Any unusual or abnormal eating practices
need to be assessed in relation to the patient’s symp-
toms. It is important to obtain a detailed history of
the onset of symptoms and their relation to the indi-
vidual’s eating pattern. Exclusion diets should be tried
only when patients complain of multiple food intoler-
ance, and single food avoidance has not helped
control symptoms. Patients taking large quantities
of sorbitol should be discouraged of such practice,
especially if their symptoms are predominantly pain
and diarrhea. A milk-free or lactose-free diet should
be tried in those patients in whom dairy products are
associated with symptoms. Patients continuing on
this diet should take calcium supplements. A trial of
1538 COLON/Diseases and Disorders

a wheat-free diet may be helpful. If a patient’s pre-
dominant symptom is constipation, an assessment of
fluid intake should be undertaken. Regular meal pat-
terns should be encouraged in all patients. Finally, an
assessment of the type and quantity of nonstarch
polysaccharides consumed should be made. The add-
ition of bran and insoluble fibers should be dis-
couraged, unless the individual feels this is of direct
benefit in symptom control. More emphasis should be
placed on increasing the proportion of foods contain-
ing a higher concentration of soluble nonstarch
polysaccharides.
Diet and Nutrition in Diverticular Disease
0039 Diverticular disease is a term encompassing diverticu-
losis and diverticulitis. Diverticulosis occurs in at
least one person in two over the age of 50 years.
The prevalence of diverticular disease is age-
dependent, increasing from less than 5% at age 40,
to 30% by age 60, to 65% by age 85. A male prepon-
derance was noted in early series, but more recent
studies have suggested either an equal distribution
or a female preponderance. There are geographic
variations in both the prevalence and pattern of di-
verticulosis. Westernized nations have prevalence
rates of 5–45%, depending upon the method of diag-
nosis and age of the population. Diverticular disease
in these countries is predominantly left-sided. The
findings are markedly different in Africa and Asia,
where the prevalence is less than 0.2%, and diverticu-
losis is usually right-sided. Diverticulosis or diverticu-
lar disease of the colon is due to pseudodiverticula in
that the wall of the diverticulum is not a full-thickness
colonic wall, but rather outpouchings of colonic
mucosa through points of weakness in the colonic
wall where the blood vessels penetrate the muscularis
propria. These diverticula are prone to infection or
‘diverticulitis’ presumably because they trap feces
with bacteria. Among all patients with diverticulosis,
70% remain asymptomatic, 15–25% develop
diverticulitis, and 5–15% develop some form of
diverticular bleeding. Diverticulitis represents micro-
or macroscopic perforation of a diverticulum. The
primary process is thought to be erosion of the diver-
ticular wall by increased intraluminal pressure or
inspissated food particles; inflammation and focal
necrosis ensue, resulting in perforation. If the infec-
tion spreads beyond the confines of the diverticula in
the colonic wall, an abscess is formed. Patients pre-
sent with increasing left lower quadrant pain and
fever, often with constipation and lower abdominal
obstructive symptoms such as bloating and disten-
tion. Some patients with severe obstructive symptoms
may actually describe nausea or vomiting. This can
occur with or without abscess formation. The diag-
nosis of acute diverticulitis is often made on the basis
of the history and the physical examination. On
physical examination, the patient often has localized
tenderness in the left lower quadrant and, with severe
infection and an abscess, may have rebound tender-
ness in the left lower quadrant. A palpable mass is
often identifiable where the sigmoid colon (the most
common site of diverticulitis) is infected. Computed
tomographı
¨
c (CT) scanning has become the optimal
method of investigation in patients suspected of
having acute diverticulitis, being employed for diag-
nosis, assessment of severity, therapeutic interven-
tion, and quantification of resolution of the disease.
CT scan may be helpful in outlining the colon and
identifying an abscess, and is preferable to barium
enema for diagnosis in patients with acute illness.
After resolution of an episode of acute diverticulitis,
the colon requires full evaluation by colonoscopy,
barium enema, or both to establish the extent of
disease and to rule out coexistent lesions, such as
polyps or carcinoma.
Etiology
0040It has been speculated that low dietary fiber predis-
poses to the development of diverticular disease. In
one study, Burkitt and Painter demonstrated that indi-
viduals in the UK eating a Western diet low in fiber had
colonic transit times of 80 h and a mean stool weight of
110 g day
1
. In comparison, Ugandans eating very
high fiber diets had transit times of 34 h and greater
stool weights (> 450 g day
1
). The longer transit times
and smaller stool volumes were felt to contribute to the
development of diverticular disease through the in-
crease in intraluminal pressures that predispose to
diverticular herniation. The etiology of diverticular
disease is unknown. The leading theory suggests that
altered colonic motility plays a major role in the devel-
opment of diverticula. Higher resting, postprandial
and neostigmine stimulated pressures in diverticular
patients suggest that a delay in transport with augmen-
tation of water reabsorption could cause excessively
high pressures forcing mucosa to herniate.
0041A recent report that evaluated a cohort of over
47 000 men provided strong evidence for the role of
dietary fiber. After adjustment for age, energy-
adjusted total fat intake, and physical activity, total
dietary fiber intake was noted to be inversely associ-
ated with the risk of symptomatic diverticular disease.
The relative risk was 0.58 for men in the highest quin-
tile compared to those in the lowest quintile for fiber
intake. The observation that diverticular disease is less
common in vegetarians than nonvegetarians is also
compatible with a role for dietary fiber, since vege-
tables and fruits are important sources of fiber.
COLON/Diseases and Disorders 1539
0042 Other dietary factors that might contribute to
the pathogenesis of diverticular disease have been
examined. There is no substantially increased risk
associated with smoking, caffeine, or alcohol. How-
ever, an association has been noted between obesity
in men under 40 years and acute diverticulitis. This
finding is compatible with observations that the risk
of symptomatic diverticular disease is particularly
increased (relative risk 2.35–3.32, 95% confidence
interval) by a diet characterized by a high intake of
total fat or red meat and a low intake of dietary fiber.
Treatment
0043 The treatment of diverticular disease can be divided
into prevention of diverticulosis, uncomplicated di-
verticulosis, and complicated diverticulosis (Table 8).
0044 The mainstay of treatment for preventing diver-
ticulosis is a diet high in fruit and vegetable fiber.
This suggestion is based on observations that low-
fiber diets are associated with colonic diverticulosis.
Recommendations are also based on results from the
Health Professionals Follow-up Study, which showed
an inverse association between insoluble dietary fiber
intake and the risk of developing symptomatic diver-
ticular disease. In particular, the greatest reduced risk
was in those consuming a diet high in fruit and
vegetable fiber, with an average consumption of 32 g
day
1
.
0045 The management of uncomplicated diverticulosis
involves a diet high in fruit and vegetable fiber. The
majority of patients with diverticular disease will
remain asymptomatic. Therefore, this group of pa-
tients consists of the largest treatment group. There
are no data to support any therapeutic recommenda-
tions in this group of patients. There have been mul-
tiple uncontrolled studies demonstrating the effect of
fiber in patients with diverticulosis, but the lack of
a placebo group complicates the results. Other well-
conducted studies have reported conflicting results
regarding the use of fiber. Despite conflicting data, it
appears safe to recommend a diet high in fiber for
patients with uncomplicated diverticular disease.
0046 Complicated diverticulosis includes diverticulitis
and hemorrhage (Table 9). Patients with mild diver-
ticulitis can be treated as outpatients with broad-
spectrum oral antibiotics with activity against anaer-
obes and Gram-negative rods. Patients should be on
the alert for symptoms of increasing pain, fever, or
inability to tolerate oral foods. Such patients are
treated with a clear liquid diet. Patients admitted to
hospital with more severe diverticulitis should be
placed on bowel rest with clear liquids or nothing
by mouth. Intravenous fluid therapy is required. In
addition, intravenous antibiotics should be initiated
to target colonic anaerobes and Gram-negative rods.
Improvement is expected within 2–4 days, at which
point the diet can be advanced. In patients hospital-
ized with acute diverticulitis, 15–30% will require
surgery. After resolution of acute diverticulitis, the
likelihood of recurrence and the role of elective surgi-
cal resection are important to prevent further attacks.
The risk of recurrence after an acute attack ranges
from 7 to 62%. Recurrent attacks are less likely to
respond to medical and diet therapy and often require
emergent surgery. Therefore, elective surgery is often
recommended after two attacks of acute diverticu-
litis.
Diet and Nutrition in Infectious Colitis
0047Infectious or noninfectious causes may be responsible
for acute diarrhea, and in selected patients, both
can occur simultaneously. Noninfectious causes
of diarrhea include drugs, food allergies, primary
gastrointestinal diseases such as inflammatory bowel
disease, and other disease states such as thyrotoxico-
sis and the carcinoid syndrome (Table 10). A variety
of infectious diseases cause acute diarrhea. Diarrheal
diseases represent the second most common cause of
death worldwide and the leading cause of childhood
death. Diarrhea results in 300–400 deaths per year in
children in the USA, approximately 200 000 hospital-
izations, 1.5 million outpatient visits, and more than
one billion dollars in direct medical costs. Acute diar-
rheal disease is generally defined as three loose stools
(or two loose stools with abdominal symptoms) or
more than 250 g of stool per day for up to 7 days.
When diarrhea lasts for 14 days, it can be considered
persistent; the term chronic generally refers to
diarrhea that lasts for at least a month. It is useful to
categorize infectious diarrheal diseases by the portion
tbl0008 Table 8 Management of patients with diverticulosis
Prevention High-fiber diet
Uncomplicated High-fiber diet
No antispasmodics
No antibiotics
Complicated Broad-spectrum antibiotcs
Bowel rest
Surgical consult
tbl0009Table 9 Complications of diverticulosis
Fistula
Obstruction
Hemorrhage
Perforation
Peritonitis
Abscess
1540 COLON/Diseases and Disorders
of the intestine that they are prone to infect since the
presenting symptoms vary by region. The initial
evaluation of patients with acute diarrhea should
include a history of the duration of symptoms and
the frequency and characteristics of the stool. The
clinical and epidemiologic history is central to patient
medical evaluation and management. Diarrhea may
be categorized as mild (no change in normal activ-
ities), moderate (forced change in activities), or severe
(disability generally with confinement to bed). There
should be an attempt to elicit the severity of illness,
evidence of dehydration and extracellular volume
contraction (e.g., with orthostatic vital signs), and
character of stool pattern. Fever and peritoneal signs
may be clues to infection with an invasive enteric
pathogen (Shigella, Salmonella,orCampylobacter).
Diagnostic clues may be provided by questioning
about factors that might expose a patient to potential
pathogens such as residence, occupational exposure,
recent and remote travel, pets, and hobbies. A food
history may also provide clues to a diagnosis. Con-
sumption of unpasteurized dairy products, raw or
undercooked meat or fish, or organic vitamin prepar-
ations may suggest certain pathogens. In addition, the
timing of symptoms with regard to exposure to sus-
pected offending food can be important clues to the
diagnosis. Symptoms that begin within 6 h suggest
ingestion of a preformed toxin of Staphylococcus
aureus or Bacillus cereus (Table 11). Symptoms that
begin at 8–14 h suggest infection with Clostridium
perfringens. Symptoms that begin at more than 14 h
suggest infection with viral agents, particularly if
vomiting is the most prominent feature, or bacterial
contamination of food with enterotoxigenic or
enterohemorrhagic E. coli. It is also important to
ask about recent antibiotic use (as a clue to the pres-
ence of Clostridium difficile infection). In the absence
of specific clues in the history, a stool culture should
be obtained in patients with the signs of more severe
illness. Gross examination of the stool for blood, pus,
and mucus is the single most important laboratory
test to begin the evaluation of an acute diarrheal
illness. This should be followed by microscopic exam-
ination of the stool for inflammatory cells. A stool
specimen should be submitted for culture if the stool
is inflammatory (i.e., with white cells and/or mucus).
Specific media, methods, or stains may be required
to isolate or identify organisms of interest. A routine
stool culture will identify Salmonella, Campylobac-
ter, Shigella, Aeromonas, and most strains of Yersinia.
A stool culture that is positive for one of these patho-
gens in a patient with acute diarrheal symptoms can
be interpreted as a true positive, although antibiotic
therapy is not required for all of these organisms.
Other organisms that should be considered in selected
situations include enterohemorrhagic Escherichia
coli, viruses, vibrios, Giardia, Cryptosporidia,and
Cyclospora.
Treatment
0048The management of patients with acute diarrhea
begins with general measures such as hydration and
alteration of diet. Antibiotic therapy is not required in
most cases, since the illness is usually self-limited.
Nevertheless, empiric and specific antibiotic therapy
can be considered in certain situations.
0049For most cases of acute diarrhea, the most import-
ant form of therapy consists of fluid combined with
tbl0010 Table 10 Noninfectious causes of diarrhea
Drugs
Thyroid disease
Carcinoid syndrome
Lactose deficiency
Short gut
Gastrinoma
Tumor
Cystic fibrosis
Schwanoma
IBD
Celiac disease
IBS
tbl0011 Table 11 Infectious causes of diarrhea
Agent Clinical features Syndrome
Staphylococcus aureus, Bacillus cereus
(preformed toxin)
Nausea, vomiting, watery
diarrhea
Gastroenteritis
Enteric pathogen Abdominal pain, cramps,
voluminous stools
Acute watery diarrhea
Shigella, Campylobacter,
Salmonella, Escherichia coli,
Yersinia, Aeromonas spp., noncholera
vibrios, Chlamydia trachomatis
Small volume stools,
urgency, tenesmus, dysentery
Colitis, proctitis
Parasite (Giardia, Cryptosporidium,
Cyclospora, Microsporidium), bacterial overgrowth
Depends upon location
of disease
Persistent, chronic diarrhea
COLON/Diseases and Disorders 1541
electrolytes. Particular attention should be given to
the immunocompromised and the elderly. Solutions
containing sodium in the range of 45–75 mEq l
1
are
required. For dehydrated patients, aggressive fluid
therapy is required. Oral fluids with Na 60–90 mEq
l
1
, K 20 mEq l
1
, Cl 80 mEq l
1
, citrate 30 mEq l
1
,
and glucose 20 g l
1
are often recommended. In non-
dehydrated healthy persons with acute diarrhea, fruit
juices with saltine crackers supplemented with broths
and soups can meet the fluid and salt needs in most
cases. In all cases, calories should be provided to
facilitate enterocyte renewal. Historically, boiled
starches/cereals with salt combined with crackers,
bananas, yogurt, soup and boiled vegetables have
been used successfully. Diet can return to normal
when stools are formed. Starchy foods have the ad-
vantage of containing a small percentage of simple
proteins that are easily hydrolyzed and well absorbed.
Once rehydration is complete and food has been re-
introduced, the oral electrolyte solution is continued
to replace ongoing losses from stool and for mainten-
ance. The rehydration fluid can be safely continued if
other foods or fluids are introduced.
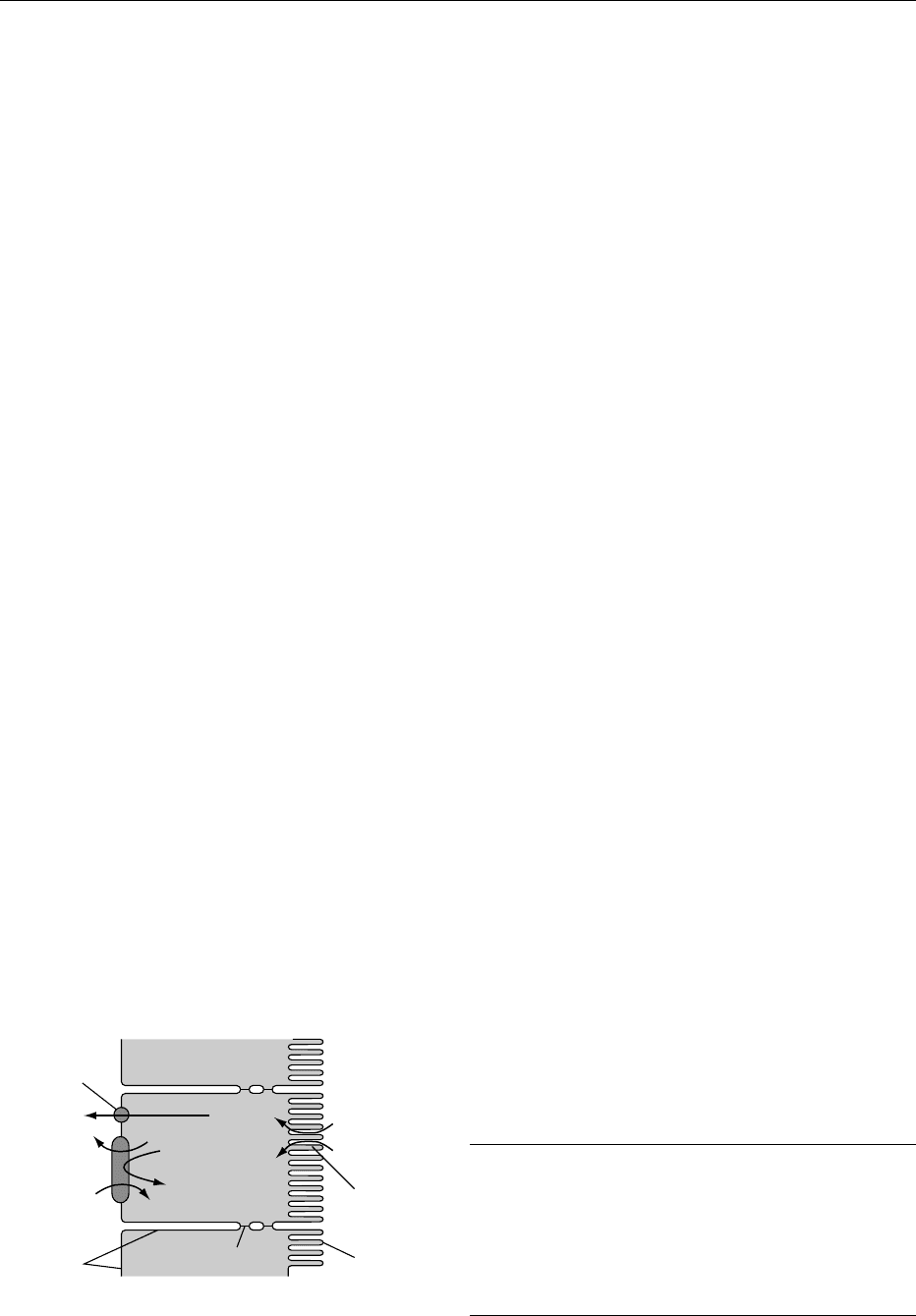
0050 Oral rehydration solutions were first developed in
the USA in the early 1950s following the realization
that, in many small-bowel diarrheal illnesses,
intestinal glucose absorption via sodium–glucose
cotransport remains intact. Thus, in diarrheal disease
caused by any organism that turns on small-bowel
secretory processes, the intestine remains able to
absorb water if glucose and salt are also present to
assist in the transport of water from the intestinal
lumen (Figure 2). From this point of view, it would
seem desirable not to restrict food in acute diarrheal
illnesses. Carefully controlled trials of various regi-
mens and solutions for oral rehydration have been
conducted in nearly every country in the world. The
American Academy of Pediatrics Committee on
Nutrition endorses the use of oral fluid therapy and
posttreatment feeding.
0051A composition of oral rehydration solution (per
liter of water) has been recommended by the World
Health Organization (Table 12).
0052Homemade solutions of sugar and salt can also be
used for oral rehydration. An appropriate mixture is
half a teaspoon of salt (3.5 g) and 8 teaspoons of
sugar (40 g) in 1 liter of water. These homemade
solutions lack sufficient amounts of potassium.
Moreover, potentially harmful errors in mixing have
been reported. The electrolyte concentrations of
fluids used for sweat replacement (e.g., Gatorade)
are not equivalent to oral rehydration solutions,
although they may be sufficient for the otherwise
healthy patient with diarrhea who is not dehydrated.
Diluted fruit juices and flavored soft drinks along
with saltine crackers and broths or soups may also
meet the fluid and salt needs in these less severely ill
individuals. If available, racecadotril, an enkephali-
nase inhibitor, may be an effective adjunct to oral
rehydration solutions. In one study, it reduced the
output and duration of watery diarrhea in a study of
135 Peruvian boys, aged 3–35 months.
0053Several problems with glucose-based oral rehydra-
tion solutions have limited their use. While this ther-
apy effectively replaces the fluids lost in the stool, it
does not decrease the stool volume. The continued
diarrhea often leads to self-imposed cessation of ther-
apy by the user. Glucose-based solutions prepared
with an electrolyte concentration higher than that of
the recommended solutions as a result of the addition
of too much solute can produce an increase in
diarrhea and hypernatremia.
0054In summary, oral rehydration has become the main-
stay for management of acute diarrheal illness caused
by infection. Glucose electrolyte solutions should
be used for rehydration (75–90 mmol of sodium per
liter) and maintenance (40–60 mmol of sodium
per liter). The ratio of carbohydrate to sodium should
not exceed 2:1. Oral rehydration solutions may be
used to treat mild, moderate, and severe dehydration.
Mixing of dry ingredients and water at home is ac-
ceptable if guidelines are strictly followed. Feeding
Intestinal lumen
Dietary glucose
High (dietary) Na
+
Epithelial cells
Low Na
+
High K
+
Blood
High Na
+
Low K
+
Glucose
Glucose
Tight junction
Basolateral
membrane
Glucose
Glut 2
Apical
membrane
Na
+
/glucose
symport
protein
2 Na
+
2 Na
+
ADP + P
i
K
+
K
+
Na
+
ATP
Na
+
Na
+
/K
+
ATPase
fig0002 Figure 2 Sodium–glucose transporter.
tbl0012Table 12 Composition of oral rehydration solution
Ideal 3.5 g of sodium chloride
2.9 g of trisodium citrate or 2.5 g of sodium
bicarbonate
1.5 g of potassium chloride
20 g of glucose or 40 g of sucrose
Homemade 1.5 teaspoons (3.5 g) of salt
8 teaspoons (40 g) of sugar
1 l of water
1542 COLON/Diseases and Disorders
should be reintroduced within the first 24 h of the
onset of diarrhea.
See also: Antioxidants: Natural Antioxidants; Body
Composition; Calcium: Properties and Determination;
Carbohydrates: Classification and Properties; Colon:
Structure and Function; Dietary Fiber: Properties and
Sources; Enteral Nutrition; Fish Oils: Production; Folic
Acid: Properties and Determination; Infection, Fever,
and Nutrition; Inflammatory Bowel Disease; Iron:
Properties and Determination; Malnutrition: The Problem
of Malnutrition; Parenteral Nutrition
Further Reading
Camilleri M (2001) Management of the irritable bowel
syndrome. Gastroenterology 120: 652–668.
Drossman DA (2000) The Functional Gastrointestinal
Disorders. McLean, UA, USA: Allen Press.
DuPont HL (1997) Guidelines on acute infectious diarrhea
in adults. The Practice Parameters Committee of the
American College of Gastroenterology 92(11): 1962.
Feldman M, Sleisenger MH and Fordtran JS (eds) (1998)
Gastrointestinal and Liver Diseases, 6th edn. Phila-
delphia, PA: W.B. Saunders.
Greenberg GR (1992) Nutritional support in inflammatory
bowel disease: Current status and future directions.
Scandinavian Journal of Gastroenterology 27(supple-
ment 192): 117–122.
Guerrant RL, Gilder TV and Steiner T (2001) IDSA Practice
guidelines for the management of infectious diarrhea.
Clinical Infectious Diseases 32: 331.
Hawkins C (1990) Ulcerative colitis: dietary therapy. In:
Inflammatory Bowel Diseases. Edinburgh, UK: Church-
ill-Livingstone.
Jeejeebhoy KN (2002) Clinical nutrition. Management of
nutritional problems of patients with Crohn’s disease.
Canadian Medical Association Journal 166(7): 913–
918.
Kohler L, Sauerland S and Neugebauer E (1999) Diagnosis
and treatment of diverticular disease: Results of a con-
sensus development conference. The Scientific Commit-
tee of the European Association for Endoscopic Surgery.
Surgical Endoscopy 13: 430.
Parks TG (1975) Natural history of diverticular disease of
the colon. Clinical Gastroenterology 4: 53.
Practice Parameters for the Treatment of Sigmoid Diverticu-
litis. The Standards Task Force. The American Society of
Colon and Rectal Surgeons. Diseases of the Colon and
Rectum 43: 289.
Ramaswamy K (2001) Infectious diarrhea in children.
Gastroenterology Clinics of North America 30(3):
611–624.
Rosenberg IH (1990) Diet and nutritional therapy in
Crohn’s disease. In: Inflammatory Bowel Diseases.
Edinburgh, UK: Churchill-Livingstone.
Stollman NH and Reskin JB (1999) Diagnosis and manage-
ment of diverticular disease of the colon in adults. Ad
Hoc Practice Parameters Committee of the American
College of Gastroenterology. American Journal of
Gastroenterology 94: 3110.
Cancer of the Colon
S-W Choi and J B Mason, Tufts University, Boston,
MA, USA
Copyright 2003, Elsevier Science Ltd. All Rights Reserved.
Background
0001Colorectal cancer is the second most common cancer
in terms of incidence and mortality for both men and
women in most of the developed countries of the
world. Molecular-genetic studies indicate that colon
carcinogenesis is due to a time-dependent accumula-
tion of aberrations in tumor suppressor genes and
oncogenes in the colonic epithelial cell, leading to
abnormal expression of critical, cancer-related pro-
teins. These aberrations, the most well characterized
of which are mutations, offer a molecular explan-
ation for the generally accepted sequence of colon
carcinogenesis: normal mucosa, hyperproliferative
epithelium, adenoma, and carcinoma.
0002The majority of colorectal cancers (65–85%) are
described as ‘sporadic’ and have no apparent under-
lying genetic predisposition, whereas it is estimated
that at least 5% of colorectal cancers are due to
inherited mutations in major genes (‘hereditary’
colon cancer), and up to an additional 30% may
be due to minor susceptibility genes (‘familial’ colo-
rectal cancer). Hereditary nonpolyposis colorectal
cancer and familial adenomatous polyposis are the
two major varieties of hereditary colorectal cancer
syndromes.
0003Migrant studies and other epidemiologic studies
indicate that the incidence of sporadic colon cancer is
strongly associated with environmental determinants,
in particular diet. A diet rich in foods from
plant sources (vegetables, fruits, and whole grains)
is associated with decreased risk, whereas diets high
in animal fat and red meats are associated with in-
creased risk for colorectal cancer. Making appropri-
ate changes in dietary habits and/or supplementing
the diet with particular nutrients that are thought
to be protective is therefore an attractive approach
to preventing this cancer, although it should be
emphasized that the prevention of colorectal cancer
by this means probably requires long-term changes
COLON/Cancer of the Colon 1543

over a decade or more in order to effect a meaningful
response.
Epidemiology
0004 Rates of colorectal cancer vary considerably with
geography. The disease is common in the USA,
Australia, New Zealand, Scandinavia, and Western
Europe, and is relatively uncommon in Asia, Africa,
and South America. Incidence rates vary approxi-
mately 20-fold around the world, with the highest
rates seen in the developed world and the lowest in
India. The international differences, migration data,
and recent rapid changes in incidence rates in Italy,
Japan, urban China, and male Polynesians in Hawaii
show that colon cancer is highly sensitive to changes
in the environment. Among immigrants and their
descendants, incidence rates rapidly reach those of
the host country, sometimes within the migrating
generation. The 20-fold international difference may
be explained, in large part, by dietary and other en-
vironmental differences; indeed, although incidence
rates in Japan have been low even until quite recently,
the highest rates in the world are now seen among
Hawaiian Japanese.
0005 However, colorectal cancer has long been known
to occur more frequently in certain families, and there
are several rare genetic syndromes that convey a
markedly elevated risk. For example, familial adeno-
matous polyposis, an autosomal dominant hereditary
disease, has 90–100% penetrance, with essentially all
affected individuals developing colon adenomas, and
later colon cancer. Colorectal cancer arising in this
setting is thought to have nearly a 100% genetic
basis. Colorectal cancer is thus causally related to
both genes and environment.
Fat
0006 In Western diets, much of the fat is derived from
animal products and may constitute 40–45% of
total caloric intake. The relationship between dietary
fats and cancer has long been recognized and has
received considerable attention as a possible risk
factor in the causation of colon cancer. A recent eco-
logical study observed that mortality data of color-
ectal cancer for 22 European countries, the USA, and
Canada were correlated with consumption of animal
fat. Increased concentrations of bile acids and fatty
acids in the intestine, resulting from a high-fat diet, is
suggested as an explanation for the epidemiological
association between high intake and high rates of
colorectal cancer. Bile acids and fatty acids are con-
sidered to be major irritants of the colonic mucosa
and are thought to link the high-risk Western-style
diet to colon cancer. However, the link between
animal fat and colorectal cancer is not entirely con-
sistent. The majority of case-control studies of diet
and cancer have shown no significant associations.
Furthermore, prospective and intervention studies of
fat in studies of the precursor adenoma have yielded
conflicting results. The risk of developing an aden-
oma was reduced by a low-fat diet in a prospective
study of 45 000 US health professionals, but not in
an intervention study of 400 adenoma patients in
Australia.
0007Not all dietary fats are detrimental in this regard.
Intake of vegetable fat is usually shown not to be
associated with risk of the cancer. Also, European
epidemiologic studies indicate an inverse relationship
between fish consumption and colorectal cancer and
an inverse correlation with fish and fish oil consump-
tion when expressed as a proportion of total or
animal fat. These effects were seen in populations
with a high fat intake, indicating that the type of fat
in the diet is critical in determining cancer risk. Con-
sumption of fish products rich in o-3 polyunsaturated
fatty acids (PUFA), such as eicosapentaenoic and
docosahexaenoic acid, is associated with a low inci-
dence of colorectal cancer and adenoma. Moreover,
PUFAs have been shown to normalize altered prolif-
erative patterns of the colonic mucosa in human sub-
jects at high risk for colon cancer. These results
emphasize that the enhancing effect of colon carcino-
genesis by dietary fat depends on the type of fat as
well as the fatty acid composition of the fat.
Meat
0008Most case-control studies show an increased risk for
development of colorectal cancer in those individuals
consuming high amounts of meat, especially red meat
(this includes lamb, pork, and beef). A high intake of
processed meat is also associated with colorectal
cancer risk in two cohort studies. Possible mechan-
isms underlying this epidemiological association
include the heterocyclic amines (which are carcino-
genic and mutagenic) that are formed when meat is
cooked. The possibility that meat alters nitrogen
metabolism within the lumen of the intestine and
enhances the production of endogenous promoters
and carcinogens within the colon is also an attractive
mechanism. In a review of several large prospective
cohort studies, colon cancer risk was associated with
red-meat consumption but not with total or animal
fat, which suggests that the risk associated with red-
meat consumption is independent of its fat content.
0009In contrast, consumption of fish or chicken is not
associated with risk and might even reduce the occur-
rence of colorectal cancer. A cohort study in Iowa
1544 COLON/Cancer of the Colon

women and European prospective studies did not
found any significant association between overall
meat intake and colon cancer, and two prospective
studies show that consumption of white meat or fish
is not associated with risk and might even reduce the
occurrence of colorectal cancer. A study of Seventh-
day Adventists – a predominantly vegetarian popula-
tion – reported that meat intake was not associated
with risk of colorectal cancer.
0010 The data suggest an independent association
between red-meat consumption and the risk of color-
ectal cancer; neither the total protein nor the total fat
content of the meat seems to be responsible for this
affect.
Calories
0011 Case-control studies suggest that excess calories
enhance the risk of colonic carcinogenesis, although
it is very difficult to distinguish between energy intake
and the intake of dietary fat. In an animal study,
carcinogen-induced colon tumors were inhibited by
calorie restriction, even though the calorie-restricted
rats ingested twice as much fat as control rats. In
other animal studies, the incidence and multiplicity
of colon tumors were significantly inhibited in
animals fed diets containing 20–30% fewer calories
than controls.
0012 Obesity appears to be a risk factor for colorectal
cancer independent of dietary fat intake. Positive cal-
orie balance and the resulting accumulation of body
fat during adult life increase the risk of colon cancer.
Even a moderate degree of overweight (body mass
index (kg m
2
) > 26) is associated with increased
rates of colorectal cancer. Therefore, maintaining
weight in a desirable range appears to be protective.
Vegetables and Fruits
0013 Among the most consistent data that are available
from the observational epidemiologic literature are
those suggesting that a higher intake of plant foods
lowers the risk of cancers at almost every site. The
overwhelming majority of descriptive, case-control,
and cohort epidemiologic studies have suggested
an inverse relationship between consumption of
vegetables and fruits and colorectal cancer risk.
0014 There are many biologically plausible reasons why
consumption of vegetables and fruits might reduce
the likelihood of cancer. Numerous compounds in
vegetables and fruits that might exert anticarcino-
genic effects have been identified, such as carote-
noids, vitamin C and E, folate, flavonoids, phenols,
isothiocyanates, and fiber. Each of these phytochem-
icals and bioactive compounds has been shown to
exert some anticarcinogenic activity in laboratory
models of cancer.
0015Vegetables are observed more consistently to
convey a protective effect against colorectal cancer
than fruit in studies from many countries. This may
be due to a difference in composition between vege-
tables and fruits. An average serving of fruit is sub-
stantially higher in sugar, calories, and vitamin C, but
lower in carotenoids, vitamin B
6
, and folate relative
to vegetables. Conversely, raw vegetables tend to be
lower in fiber (especially the soluble variety) than
both cooked vegetables and fruits. Alternatively, a
high vegetable intake, more than a high fruit intake,
may merely reflect a generally healthier diet, that is,
one relatively low in energy, fat, and sugar.
0016Although the vast majority of case-control and
cohort studies have observed a protective effect of
vegetables and fruits on colorectal carcinogenesis,
the Iowa Women’s Health Study, a large prospective
cohort study, observed that total intake of neither
vegetables nor fruits reduced the relative risk of color-
ectal cancer. Similar results were obtained when each
vegetable or fruit item was independently analyzed,
except garlic. The data from the meta-analyses
of colorectal and stomach cancer suggest that a
high intake of raw and cooked garlic may be associ-
ated with a protective effect against stomach and
colorectal cancers. Garlic contains glutathione-S-
transferase, which is thought to be involved in
the detoxification of several potential carcinogens.
Individuals consuming more than one garlic clove
per week had a 32% reduction in the risk of colo-
rectal cancer compared to those not eating any garlic.
Fiber
0017The fiber hypothesis is an old hypothesis that origin-
ated from an epidemiologic study in which African
blacks consuming high-fiber, low-fat diets were ob-
served to have a lower mortality from colorectal
cancer than African whites consuming a low-fiber,
high-fat diet. The majority of subsequent observa-
tional epidemiologic and case-control studies support
a protective effect of fiber-rich diets. The effect is
thought to be mediated by the shorter intestinal tran-
sit time that accompanies a high-fiber diet and the
resultant decrease in duration of exposure of the co-
lonic mucosa to potential carcinogens, as well as an
increase in stool bulk, which would dilute the colonic
contents, including any potential carcinogens.
0018Fiber is found in vegetables, fruits, whole grains,
seeds, nuts, and legumes and consists of nonpoly-
saccharides (such as lignin) and nonstarch polysac-
charides (including cellulose, hemicellulose, pectin,
gums, and mucilages). Earlier data suggested that a
COLON/Cancer of the Colon 1545
