Townsend Courtney M.Jr., Evers B. Mark. Atlas of General Surgical Techniques: Expert Consult
Подождите немного. Документ загружается.

CHAPTER 102 • Donor Nephrectomy 1135
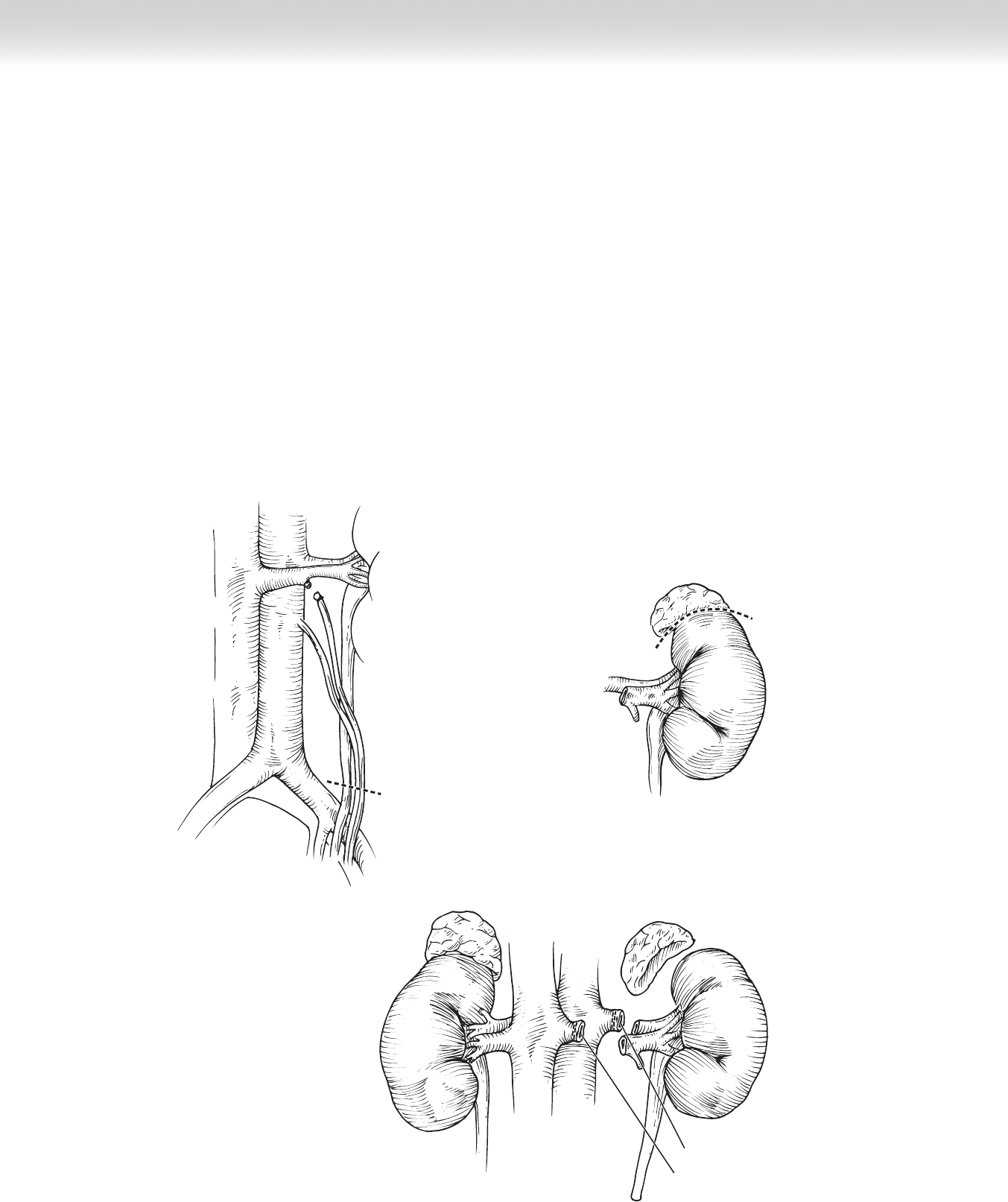
◆ The adrenal vein can also be divided at this time. It is always assumed (although present
only approximately a third of the time) that there are posterior lumbar veins present and if
not readily dissected at this juncture, they can be taken when the kidney is further mobi-
lized. The gonadal vein can also be used to facilitate dissection of the ureter. Tracing the
vein to the lower pole of the kidney, the ureter is mobilized with its essential periureteral fat
down to the iliac vessels (Figure 102-9).
◆ The gonadal vein can be divided at this time. The surgeon can now proceed with probably
one of the more technically demanding parts of the operation—dissection of the adrenal
gland from the upper pole of the kidney (Figure 102-10).
◆ The presence of an adrenal artery is less consistent than the vein but should be looked for.
Next, the renal artery is dissected to the level of the aorta. If there are any lumbar veins,
they may be divided at this time as necessary (Figure 102-11).
FIGURE 102 –10
Renal artery
Renal vein
FIGURE 102 –11
FIGURE 102 –9

1136 Section XV • Miscellaneous Procedures
◆ It is only at this time that the kidney is further mobilized with takedown of the lateral
attachments of the kidney. Throughout the procedure, the patient should be well hydrated
and actively excreting urine. Once the kidney is completely free, a 6- to 8-cm Pfannenstiel
incision is made without entrance into the peritoneum. This incision is unnecessary, of
course, with a hand-assisted laparoscopic approach. The ureter can now be transected
(see Figure 102-9).
◆ Mannitol (12.5 g) or furosemide (Lasix) (10 to 20 mg), or both, is administered before
clamping the renal artery and vein in some centers, but I prefer volume loading to promote
natriuresis.
◆ Communication between the donor and recipient team is essential to streamline the
sequence of events. If the recipient room is not yet ready for implantation, the pneumoperi-
toneum can be released in the donor and the nephrectomy can be delayed. When both
rooms are synchronized, systemic heparinization of the donor (also optional) can be
performed.
◆ An Endocatch bag is now placed through the peritoneum via the Pfannenstiel incision, and
the kidney is loaded. It is important that the donor is completely relaxed to minimize
trauma as the kidney is removed. The renal artery and renal vein are then transected
(see Figure 102-11) with a vascular linear stapler or clip device, or both, and the kidney is
removed to the back table by one of the senior assistants or implanting surgeon.
◆ The staple lines of the donated kidney vessels and ureter are excised and the renal artery is
fl ushed with ice-cold preservation solution.
3. CLOSING
◆ The time from intracorporeal vessel clamping to vessel fl ushing with ice-cold solution is
defi ned as warm ischemia time and is usually approximately 2 to 4 minutes. The time from
vessel clamping to reperfusion in the recipient is cold ischemia time. The donor surgeon, in
the interim, is ensuring hemostasis in the donor with reestablishment of the pneumoperito-
neum, so that all staple lines can be reevaluated and confi rmed to be intact. The use of a
linear staple device or clip on the renal artery is a matter of surgeon preference. There is
some evidence to support the improved safety of stapling devices versus clips, which can
fall off. Reversal of heparin is optional once the donor kidney artery and vein are transected.
◆ Once hemostasis is ensured, the pneumoperitoneum is released and the fascia is closed.
CHAPTER 102 • Donor Nephrectomy 1137
OPEN LEFT DONOR NEPHRECTOMY
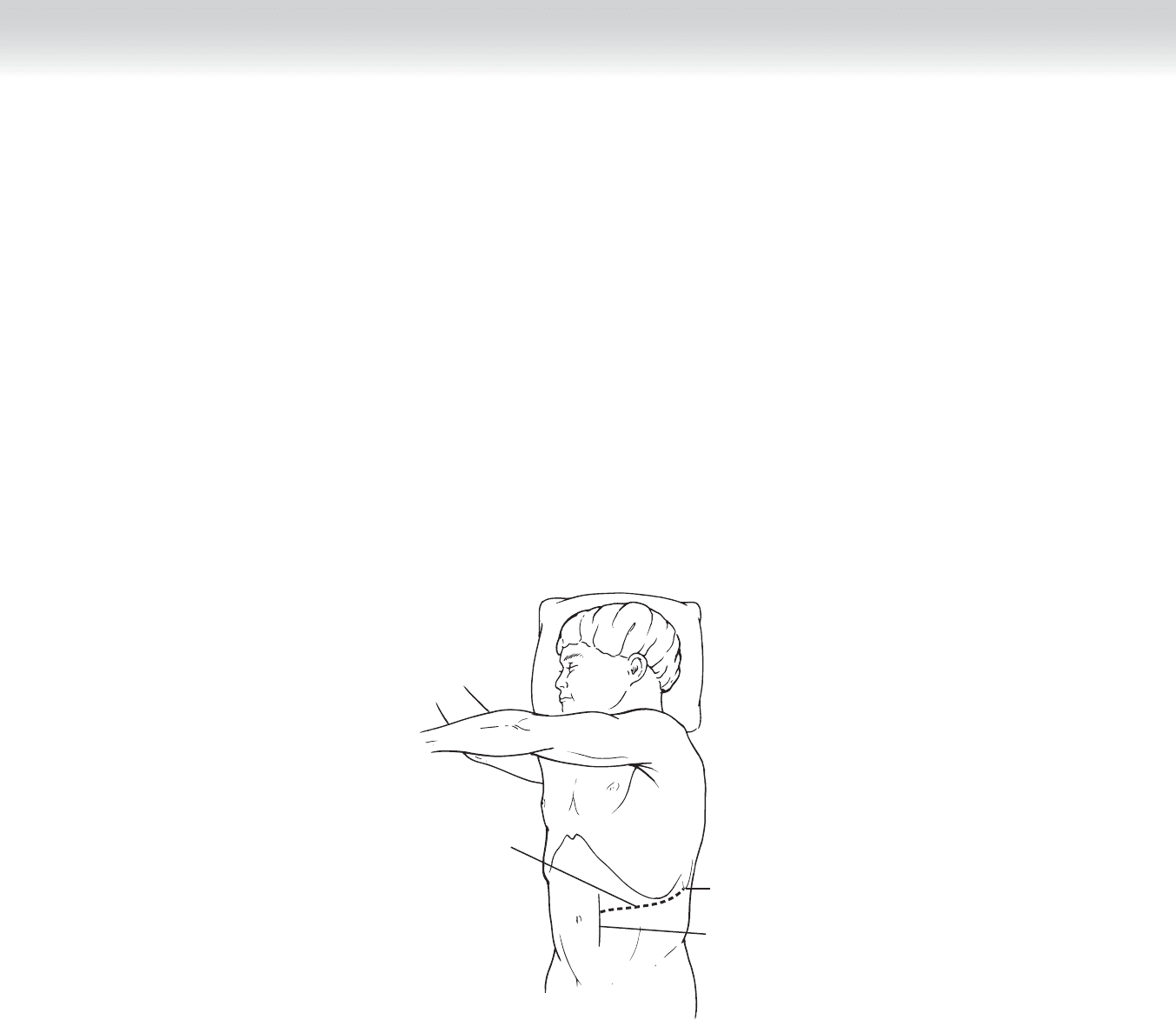
◆ Although most donor nephrectomies are performed laparoscopically, there will always be
occasion to perform open donor nephrectomy electively or with laparoscopic failure. Simi-
lar to patient positioning for a laparoscopic procedure, the patient is placed in a modifi ed
lateral decubitus position with the hips rotated posteriorly. An axillary roll is placed and
the arms are fl exed at the elbow and padded. A second roll is placed between the patient’s
knees, with the lower limb fl exed at the knee. The kidney rest is elevated and the patient
is secured. The operating table is fl exed in the middle so that the patient’s fl ank is taut
(Figure 102-12).
Tip of
11th/12th rib
Incision for
open left
nephrectomy
Edge of rectus
abdominis
FIGURE 102 –12

1138 Section XV • Miscellaneous Procedures
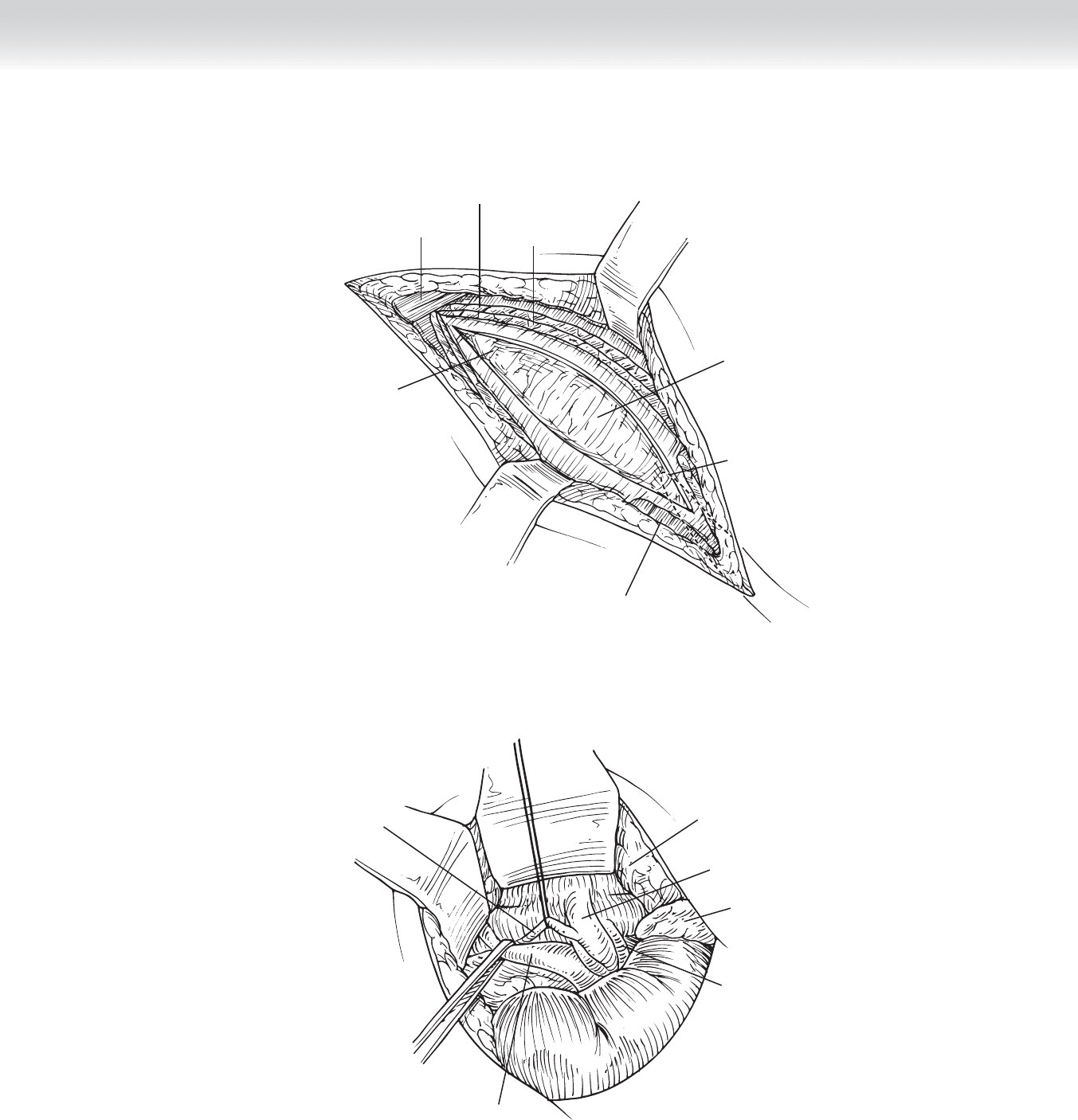
◆ The incision is placed over the distal end of the 11th or 12th rib, extending from the mid-
axillary line posteriorly to the lateral edge of the rectus abdominis muscle anteriorly at the
level of the umbilicus. The latissimus dorsi muscle posteriorly and external oblique muscle
anteriorly are fi rst incised, followed by the internal oblique and transversus abdominis
muscles to expose the peritoneum and its contents (Figure 102-13).
◆ Although well described, taking the tip of the 12th rib is not usually necessary. Care is
taken not to enter the peritoneal cavity medially or the pleural space anterior laterally. The
peritoneum and its contents are bluntly refl ected medially to expose Gerota’s fascia and the
retroperitoneal space (Figure 102-14).
◆ A fi xed retractor greatly facilitates exposure. The gonadal vein and ureter are fi rst identifi ed
and traced inferiorly to the iliac artery and superiorly to Gerota’s fascia, which can now be
opened.
◆ The upper pole of the kidney is then dissected from the adrenal gland, with care given not
to injure the pancreas. As with the laparoscopic nephrectomy, the renal vein is identifi ed,
and the gonadal, adrenal, and lumbar veins can be divided at this time.
◆ The renal artery is dissected to the aorta, avoiding injury to small polar branches. The sur-
geon should also try to avoid traction on the kidney, because this can lead to vasospasm
and acute tubular necrosis in the recipient postoperatively.
◆ The proximity of the diaphragm and pleural space should be kept in mind to prevent pneu-
mothorax. Just as in laparoscopic nephrectomy, volume loading and saline natriuresis of the
donor remains an important component of renal protection and cannot be overemphasized.
CHAPTER 102 • Donor Nephrectomy 1139
Latissimus
muscle
Gerota’s
fascia
Internal
oblique muscle
External
oblique muscle
Rectus
muscle
Peritoneum
12th rib
FIGURE 102 –13
Peritoneum
retracted
Renal vein
Adrenal gland
Renal artery
Ureter
Gonadal
vein
FIGURE 102 –14
1140 Section XV • Miscellaneous Procedures
RIGHT LAPAROSCOPIC DONOR NEPHRECTOMY
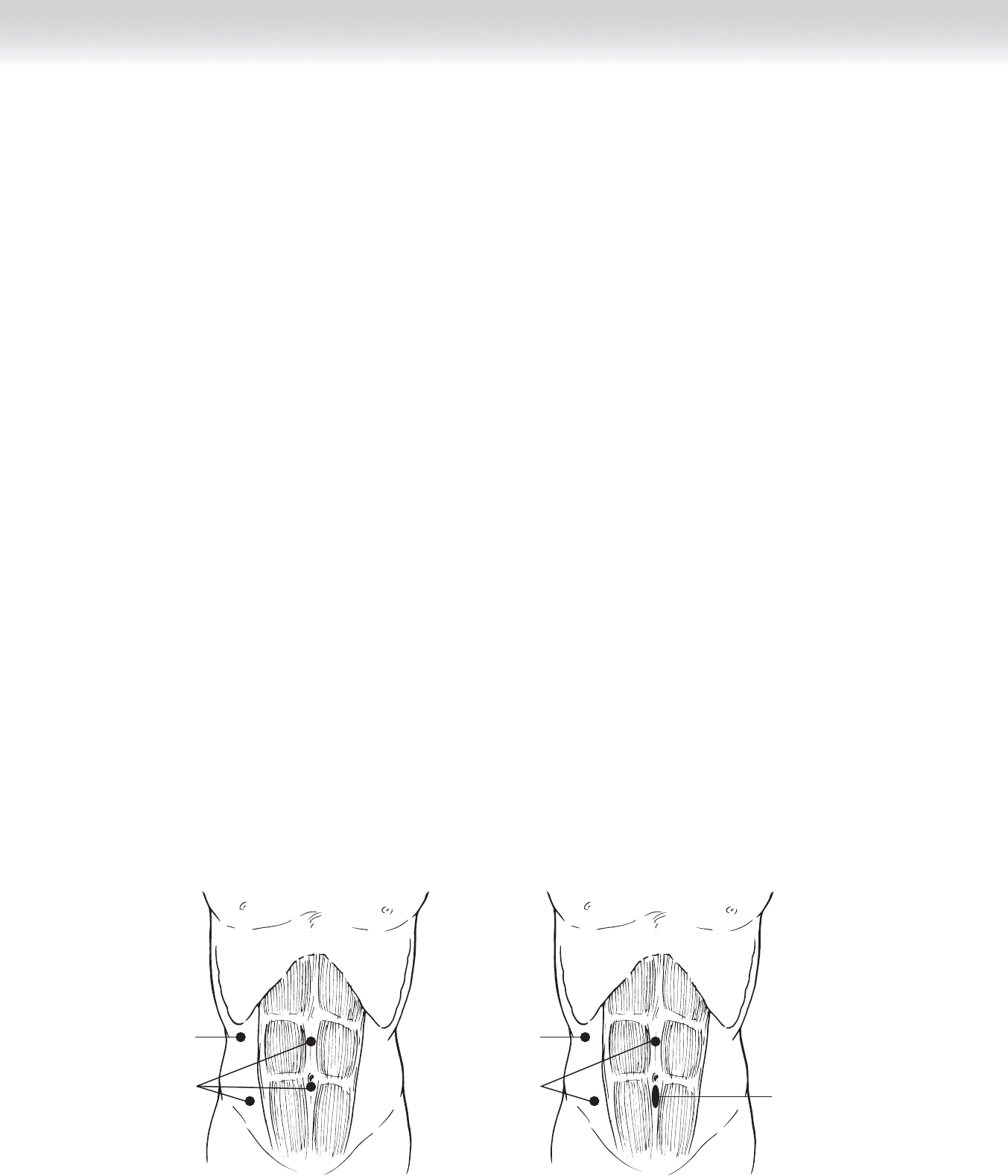
◆ Several modifi cations to the left donor nephrectomy can be made to counter the technical
challenges posed by a right nephrectomy. The patient is placed in a modifi ed lateral decubi-
tus position with the right side up. Port sites are placed on the opposite side of the body
but in a more cephalad position as for left nephrectomy, with an additional liver retractor
port (Figure 102-15).
◆ Either of these upper ports can be used to retract the right lobe of the liver superiorly to
facilitate dissection of the upper pole of the right kidney.
◆ Alternatively, the upper midline port can be placed more superiorly as for a left nephrectomy.
◆ This port site and the liver retractor site can be incorporated into a subcostal incision fol-
lowing complete laparoscopic dissection to retrieve the kidney. Some authors have also sug-
gested using this mini incision to place a Satinsky clamp across the base of the right renal
vein so that the inferior vena cava (IVC) can be sutured closed, because stapling devices can
signifi cantly shorten an already short right renal vein.
◆ It is essential to mobilize the duodenum medially to expose the IVC to access the right
renal vein. There are occasional small anterior branches on the renal vein that can be easily
avulsed. The right renal artery can also be identifi ed at this time and dissected out.
◆ The kidney is then mobilized medially, and the vascular dissection is completed. It is
important to remember that the right gonadal vein drains directly into the IVC and is
unavailable as a guide to the ureteric dissection.
◆ For hand-assisted laparoscopic right nephrectomy, the port sites are as illustrated in
Figure 102-16.
Dissection and
camera ports
Liver retractor
Hand-
assist port
FIGURE 102 –16
Dissection and
camera ports
Liver retractor
FIGURE 102 –15

CHAPTER 102 • Donor Nephrectomy 1141
OPEN RIGHT DONOR NEPHRECTOMY
◆ For open right nephrectomy, the patient is set up as for a left nephrectomy, with the right
side up. The main differences with the right nephrectomy are that the kidney is somewhat
lower, the renal vein is thinner and shorter, and the gonadal vein drains into the IVC.
RETROPERITONEAL LAPAROSCOPIC APPROACH TO THE KIDNEY
◆ Some centers advocate a retroperitoneal approach to right and left nephrectomy; the main
advantages appear to be avoidance of the peritoneal cavity, decreased risk of ileus, and
lesser hemodynamic effects with unilateral pneumoperitoneum.
◆ The disadvantages of a laparoscopic retroperitoneal approach are a smaller working space, a
steeper learning curve, and some reports of more prolonged warm ischemia times.
USE OF THE ROBOT
◆ The robot can be used for either pure laparoscopic or hand-assisted nephrectomy. The
advantages include retention of binocular vision and greater fl exibility of the operating
head.
◆ The chief disadvantage is expense.
STEP 4: POSTOPERATIVE CARE
◆ A Foley catheter is left in the donor overnight.
◆ The patient is monitored for bleeding.
◆ Early ambulation (on day of surgery) is encouraged.
◆ The patient should not take food or fl uids the fi rst day and should start clear liquids the
next day.

1142 Section XV • Miscellaneous Procedures
STEP 5: PEARLS AND PITFALLS
◆ Success of the live donor kidney transplant begins with optimal hemodynamic management
of the donor. Adequate hydration of the donor preoperatively and intraoperatively cannot
be overemphasized.
◆ Ensure diuresis before clamping of the vessels to counter the effects of renal artery traction
and the effect of the pneumoperitoneum on renal blood fl ow.
◆ Coordinate between the donor and recipient operating rooms to minimize cold ischemia
time.
SELECTED REFERENCES
1. Potter SR, Buell JF, Hanaway M, Woodle ES: Laparoscopic live donor nephrectomy: Rationale, techniques
and implications. Semin Dial 2001;14:365-372.
2. Ratner LE, Fabrizio M, Chavin K, et al: Technical considerations in the delivery of the kidney during
laparoscopic live-donor nephrectomy. J Am Coll Surg 1999;189:427-430.
3. Bolte SL, Chin LT, Moon TD, et al: Maintaining urine production and early allograft function during
laparoscopic donor nephrectomy. Urology 2006;68:747-750.
1143
STEP 1: SURGICAL ANATOMY
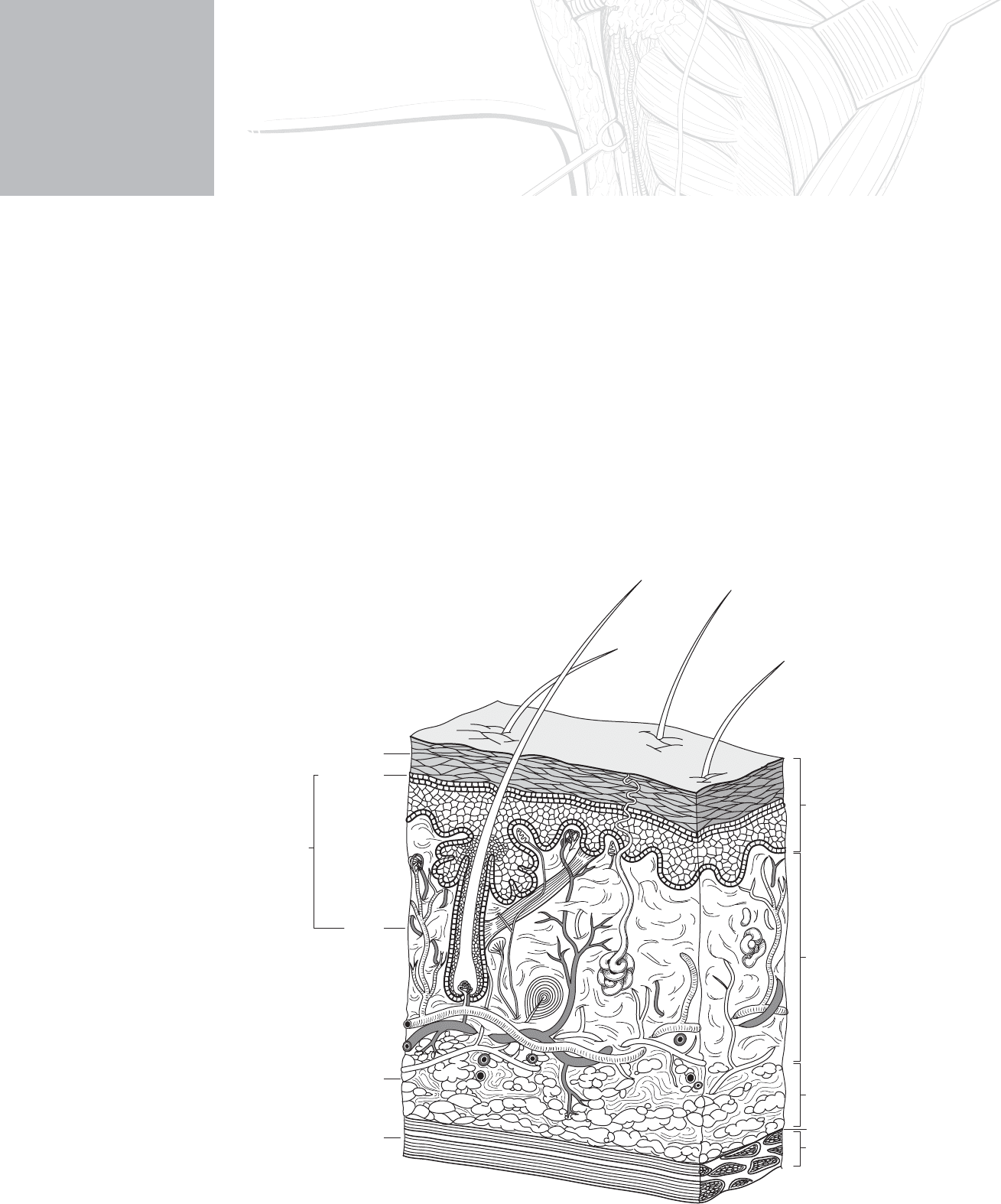
◆ Figure 103-1 shows a detailed cross-section of the skin.
CHAPTER
103
Skin Graft—Split Thickness
and Full Thickness
James J. Gallagher and David N. Herndon
Epidermis
First degree burn
Second degree burn
Third degree burn
Fourth degree burn
Deep
Dermis
Subcutaneous fat
Muscle
Fascia
Superficial
FIGURE 103–1

1144 Section XV • Miscellaneous Procedures
INDICATIONS
◆ The most common reason for skin grafting is a deep second- or third-degree burn (see
Figure 103-1).
◆ Other causes include infection, cancer, reconstruction, and trauma.
◆ Burn injury that is clearly third degree should be surgically excised and grafted promptly
unless it is small enough to allow healing by secondary intention.
◆ Second-degree burns are either superfi cial or deep partial thickness. This distinction can be
diffi cult to determine clinically.
◆ As a general rule, burns that will heal within 2 to 3 weeks with good wound care should be
allowed to do so without grafting. During this period, the clinician has a number of choices
to manage the second-degree wound: removal of blisters and tangential excision of dead
tissue followed by the application of homograft, xenograft, Biobrane, or other artifi cial skin.
Alternatively, these burns may be treated with serial dressing changes with a topical antimi-
crobial, typically silver sulfadiazine. Clinical judgment is the best guide as to burns that will
heal and those that will not.
◆ The following is a review of debridement and grafting strategies for burns, as well as mod-
ern techniques of skin grafting for all skin defects.
◆ Free skin grafts will take to (in order of declining take rate) healthy dermis, fascia, fat, mus-
cle, periosteum, and peritenon. Granulation tissue growth indicates a healthy bed for graft-
ing; the granulation tissue maybe removed before the graft is placed, or it may be left in
place depending on physician judgment. Removal improves topographic irregularities, as
well as the biofi lm of bacterial colonization that may decrease graft take. Removal is associ-
ated with increased operative blood loss.
◆ Modern dermatomes come in a variety of types. Most are powered by compressed air or
electricity (Figure 103-2).
◆ Calibration for depth of harvest is in the thousandths of an inch. Typically, a graft is taken
between 8 and 15 thousandths of an inch; the choice of depth varies with the area to be
grafted and the overall needs of the patient. We have found that the calibrations can be
inaccurate, and we routinely use the sharp edge of a scalpel to act as a mechanical check of
cutting depth. Reharvesting of donor sites is limited by the healing rates of the donor sites,
with thinner harvest sites obviously healing quicker. Each time the donor is harvested, the
epithelium is taken with some amount of dermis. The epithelium regrows, but the underly-
ing dermis does not. Deeper donor sites have the potential to produce more scarring.
Defects to the head and neck area are best covered with skin from above the clavicles. The
shaved head provides a reliable donor site with excellent healing potential; a caution is in
order to avoid areas of alopecia (senescent or autoimmune). Donor site placement should
