Jan Lindhe. Clinical Periodontology
Подождите немного. Документ загружается.

status of diabetes in an individual patient, as in the
longer term metabolic control could indicate the
probable outcome of periodontal therapy. In addi-
tion, it is now accepted that periodontal therapy
can improve metabolic control in diabetics, mean-
ing that the relationship is two-way and periodon-
tal therapy is beneficial to the control of both dis-
eases.
6.
Medications such as phenytoin, cyclosporin and
nifedipine may predispose to gingival overgrowth
in patients with gingivitis.
7.
Genetic traits, which result in diseases that modify
the periodontal structures or change the immune
or inflammatory responses, can result in gross peri
-
odontal destruction in the affected individual and
although the destruction seen may imitate perio-
dontitis this is not etiopathologically chronic peri-
odontitis.
Stress
Stress and other psychosomatic conditions may have
direct anti-inflammatory and/or anti-immune effects
and/or behavior mediated effects on the body's de-
fenses. Hence both conditions may conceptually be
relevant to the etiology of chronic periodontitis and
necrotizing ulcerative conditions. Recent studies have
suggested that academic stress and financial stress
may be associated with an increased risk of periodon
-
tal disease. Most of the literature on stress and peri-
odontal conditions is quite old, however, and reports
of acute necrotizing ulcerative gingivitis (or trench
mouth) were made on stressed soldiers on the front
line during World War I. It is understood that stress
may be immunosuppressive and that acute necrotiz-
ing ulcerative gingivitis may occur in the immuno-
suppressed (also in HIV patients), but there is insuffi-
cient data as yet to substantiate the assumption that
psychosocial factors are indeed of etiological impor-
tance in chronic periodontitis.
Genetics
There is convincing evidence from twin studies for a
genetic predisposition to the periodontal diseases.
The twin studies have indicated that risk of chronic
periodontitis has a high inherited component but that
gingivitis is a general and common response which is
unlikely to be linked with particular genes. A great
deal of research is underway attempting to identify
the genes and polymorphisms associated with all
forms of periodontitis. It is likely that chronic perio-
dontitis involves many genes, the composition of
which may vary across individuals and races. Much
attention has focused on polymorphisms associated
with the genes involved in cytokine production. Such
polymorphisms have been linked to an increased risk
for chronic periodontitis but these findings have yet
to be corroborated.
SCIENTIFIC BASIS FOR
PERIODONTAL THERAPY
Periodontitis is initiated and sustained by microbes
which are present in supra and subgingival plaque in
the form of uncalcified and calcified (calculus)
biofilms. Initial periodontal therapy or basic treat-
ment of periodontitis involves the removal of both sub
and supragingival plaque. The clinical outcome is
largely dependent on the skill of the operator in re-
moving subgingival plaque and the skill and motiva-
tion of the patient in practising adequate home care.
A further variable is the innate susceptibility of the
patient which is related to the way in which their
innate, inflammatory and immune systems operate in
response to the microbial challenge. In addition, local
and systemic risk factors can influence the quantity
and quality of both the microbial challenge and the
host response to these pathogens. The relative contri-
bution of these risk factors has yet to be fully deter-
mined but their influence would be negated if the
periodontium was kept free of microbial plaque, and
thus subgingival debridement and patient's home
care are of vital importance.
Studies have been conducted which indicate the
relative importance of operator and patient-based in-
terventions (for further detail see Chapters 20 and 21)
and only a brief summary is presented below.
Tooth loss
There is an established literature strongly supporting
the concept that periodontal treatment of chronic pe-
riodontitis is effective, and numerous long term stud-
ies show low rates of tooth loss ( 0.1 tooth lost/year)
in treated and well-maintained periodontitis patients
(Lindhe & Nyman 1984, Nabers et al. 1988). Patients
who, following treatment, were not complying with
maintenance care had double the rate of tooth loss per
year (0.2 teeth/year) (Becker et al. 1984), and un-
treated patients lost approximately 0.6 teeth/year
(
Becker et al. 1979). Thus there is substantial evidence
supporting the concept that periodontal therapy and
subsequent maintenance care are beneficial in main-
taining the dentition.
Subgingival instrumentation and
maintenance
The effects of cause related periodontal therapy were
studied intensively during the 1980s and the work of
Egelberg and his colleagues will be described now.
Badersten et al. (1984) utilized patients with severe
chronic periodontitis to study the effects of cause re-
lated periodontal therapy. The patients had a multi-
tude of sites with deep pockets (up to 12 mm). Initial
oral hygiene instruction was provided at two to three
CHRONIC PERIODONTITIS • 213
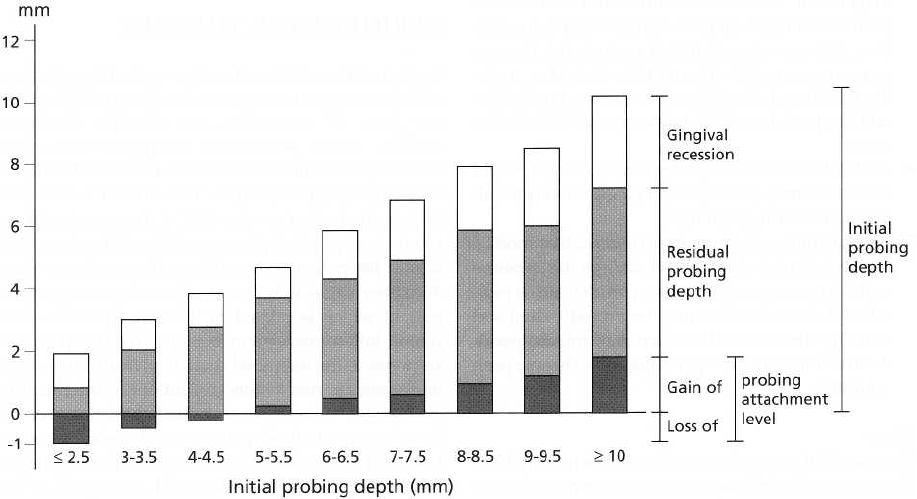
Clinical changes between 0-24 months in sites with different initial probing depths
Fig. 8-3. Data from the Badersten et al. (1984) study showing the clinical changes at 2 years according to baseline
pocket depth.
visits during the first month of the study. Additional
instruction and reinforcement of self-performed
plaque control was provided, as required, during the
2 years of the study. Subgingival debridement was
performed at 3, 6 and 9 months and the results were
evaluated over 2 years. Only minimal improvements
in the periodontal indices occurred during the first 3
months in which no scaling and root planing was
performed. Following supra and subgingival instru-
mentation, and gradually up until 12 months from
baseline, the periodontal indices improved markedly.
In the final 12 months of the 2-year period, no signifi
-
cant further improvements in the clinical condition
occurred. These results demonstrate that chronic pe-
riodontitis can be treated successfully by intensive
initial non-surgical periodontal therapy and this out-
come can be maintained over time with supportive
periodontal therapy (SPT).
Fig. 8-3 shows further data from the Badersten et al.
(1984) study and reports the clinical changes at 2 years
according to baseline pocket depth. It can be seen that
pocket depth reduction after therapy is an arithmetic
combination of gingival recession and gain or loss of
clinical attachment. At the end of the study the mean
pocket depth reduction was 1.5 mm although it is clear
from Fig. 8-3 that the initially deeper pockets had the
largest reduction in pocket depth over the 2 years and
the greatest clinical attachment gain. An interesting
feature is the fact that the sites with initially shallow
pockets tended to lose clinical attachment over the
study period. Several theories have been proposed to
explain this fact. The most plausible explanation for
the loss of clinical attachment at shallow sites is the
trauma caused by subgingival instrumentation to the
supracrestal connective tissue attachment and the
subsequent remodeling of the marginal tissues. The
best predictor of further clinical attachment loss was
residual deep pockets that occurred after treatment.
Thus, Claffey and Egelberg (1995) found that at re-
evaluation, patients with multiple sites with residual
probing depth >_ 6mm after active treatment had a
greater risk for additional attachment loss than pa-
tients with mainly shallow sites.
EFFECT OF SURGICAL
TREATMENT
Surgical treatment of chronic periodontitis lesions
permits visualization and access to the root surfaces
and thus has clear advantages over a non-surgical
approach for the cleaning of root surfaces. Tissues may
also be manipulated and lesions modified, or granu-
lation tissue surgically removed. The efficacy of sur-
gical periodontal therapy compared within the vari-
ous surgical treatment modalities and compared to
non-surgical therapy has to be considered from the
extensive scientific literature on these matters (for
further detail see Chapter 25).
COMPARISONS OF SURGICAL
AND NON-SURGICAL THERAPY
Kaldahl et al. (1993) reviewed a large body of work on
the advantages of different periodontal treatment mo-
214 • CHAPTER 8
dalities over others. Although the best assessment of
clinical outcome is achieved from longer-term studies,
actually following patients over the long term creates
new confounding problems and these can reduce the
benefit imparted by the longitudinal element of the
investigation. For example, the patient drop-out in-
creases over time which may increase the bias in the
selection of the final group for analysis (usually the
less motivated patients or less successfully treated
patients will drop out). In addition, tooth loss may
occur for which we do not know the reason and sites
associated with such teeth are lost for longitudinal
analysis. Nevertheless, useful long-term studies have
been conducted over 5 to 8 years and have typically
made intra-patient comparisons of different peri-
odontal treatment modalities using split mouth de-
signs. In the Kaldahl et al. (1993) review, some com-
prehensive summary statements were arrived at. In
general:
1. Surgical and non-surgical periodontal therapy can
improve periodontal clinical outcome measures.
2.
Surgical therapy created greater short-term reduc-
tions in probing depth than non-surgical therapy
although longer-term results varied between main-
taining greater probing depth reduction or show-
ing no differences with non-surgical therapy.
3.
Flap surgery with and without osseous resection
gave variable probing depth reductions in the short
term. Some studies favored osseous resection
whilst others showed no difference in probing
depth reduction.
4.
Flap surgery without osseous resection tended to
produce greater better short and long-term gains in
attachment levels.
5.
In both short and long-term studies, surgery pro-
duced a greater loss of probing attachment in sites
with initially shallow pockets. In sites with deeper
pockets short and long-term studies reported no
difference in attachment level change for non-sur-
gical and surgical therapy.
6.
Supragingival plaque control alone gave markedly
inferior results to plaque control combined with
subgingival root debridement.
REFERENCES
Badersten, A., Nilveus, R. It Egelberg, J. (1984). Effect of nonsur-
gical periodontal therapy. II. Severely advanced periodonti-
tis.
Journal of Clinical Periodontology
11, 63-76.
Becker, W., Becker, B.E. & Berg, L.E. (1984). Periodontal treatment
without maintenance. A retrospective study in 44 patients.
Journal of Periodontology
55, 505-509.
Becker, W., Berg, L. & Becker, B.E. (1979). Untreated periodontal
disease: a longitudinal study.
Journal of Periodontology
50,
234-244.
Claffey, N. & Egelberg, J. (1995). Clinical indicators of probing
attachment loss following initial periodontal treatment in
advanced periodontitis patients.
Journal of Clinical Periodon-
tology
22(9), 690-696.
Flemmig, T.F. (1999). Periodontitis. Annal of Periodontology 4,
32-38.
Kaldahl, W.B., Kalkwarf, K.L. & Patil, K.D. (1993). A review of
longitudinal studies that compared periodontal therapies.
Journal of Periodontology 64,
243-253.
Kinane, D.F. & Chestnutt, I. (2000). Smoking and Periodontal
Disease. Critical Reviews Oral Biological Medicine 11, 356-365.
Lindhe, J. & Nyman, S. (1984). Long-term maintenance of pa-
tients treated for advanced periodontal disease.
Journal
of
Clinical Periodontology
11(8), 504-514.
Nabers, C.L., Stalker, W.H., Esparza, D., Naylor, B. & Canales, S. (
1988). Tooth loss in 1535 treated periodontal patients.
Journal
of
Periodontologi
59(5), 297-300.
Socransky, S.S., Haffajee, A.D., Goodson, J.M. & Lindhe, J. (1984).
New concepts of destructive periodontal disease.
Journal of
Clinical Periodontology
11, 21-32.
CHRONIC PERIODONTITIS • 215
CHAPTER 9
Aggressive Periodontitis
MAURIZIO S. TONETTI AND ANDREA MOMBELLI
Classification and clinical syndromes
Epidemiology
Primary dentition and permanent dentition
Screening
Etiology and pathogenesis
Diagnosis
Clinical, microbiologic, genetic
Principles of therapeutic intervention
Periodontitis is an infection that can manifest itself
with polymorph clinical presentations. This has led to
the recognition of different clinical syndromes. Until
recently, the question of whether or not these dissimi
-
lar clinical presentations represented different forms
of disease has been open to discussion. Today several
lines of evidence support the existence of truly differ-
ent forms of periodontitis. These include:
1.
The growing clinical consensus of differential prog-
nosis and need for specific treatment approaches
for the various syndromes
2.
Heterogeneity in etiology with possible therapeu
tic
implications
3.
Heterogeneity in genetic and environmental sus-
ceptibility
At the 1999 international classification workshop, the
different forms of periodontitis were reclassified into
three major forms (chronic, aggressive and necrotiz-
ing forms of periodontitis) and into periodontal mani-
festations of systemic diseases. This chapter deals
with aggressive, type 1, periodontitis. Until recently,
this group of diseases was defined primarily based on
the age of onset/diagnosis and was thus named early
onset periodontitis (EOP). Features of this form of
disease, however, can present themselves at any age
and this form of periodontitis is not necessarily con-
fined to individuals under the arbitrarily chosen age
of 35.
Aggressive periodontitis (AgP) comprises a group
of
rare, often severe, rapidly progressive forms of
periodontitis often characterized by an early age of
clinical manifestation and a distinctive tendency for
cases to aggregate in families. At the above mentioned
classification workshop, AgP periodontitis was char-
acterized by the following major common features
(
Lang et al. 1999):
•
Non-contributory medical history
•
Rapid attachment loss and bone destruction
•
Familial aggregation of cases
Frequently AgP presents early in the life of the indi-
vidual; this implies that etiologic agents have been
able to cause clinically detectable levels of disease over
a relatively short time. This fact is central to the current
understanding of these diseases, since it implies infec
-
tion with a highly virulent microflora and/or a high
level of subject susceptibility to periodontal disease.
AgP, however, can occur at any age. Diagnosis of AgP
requires exclusion of the presence of systemic diseases
that may severely impair host defences and lead to
premature tooth loss (periodontal manifestations of
systemic diseases).
The existence of specific forms of AgP has also been
recognized based on specific clinical and laboratory
features: localized aggressive periodontitis (LAP, for-
merly known as localized juvenile periodontitis or
UP)
and generalized aggressive periodontitis (GAP,
formerly termed generalized juvenile periodontitis
(
GJP) or generalized early onset periodontitis, G-EOP)
(
Tonetti & Mombelli 1999).
In spite of its rare occurrence AgP has been the focus
of many investigations aimed at understanding its
etiology and pathogenesis. Difficulties in gathering
sufficiently large populations, however, have resulted
in few clinical studies addressing both diagnostic and
therapeutic procedures for these subjects. Utilization
of both clinical and advanced diagnostic procedures
as well as of a variety of treatment approaches remains
largely anecdotal and somehow based on the specific
218 • CHAPTER 9
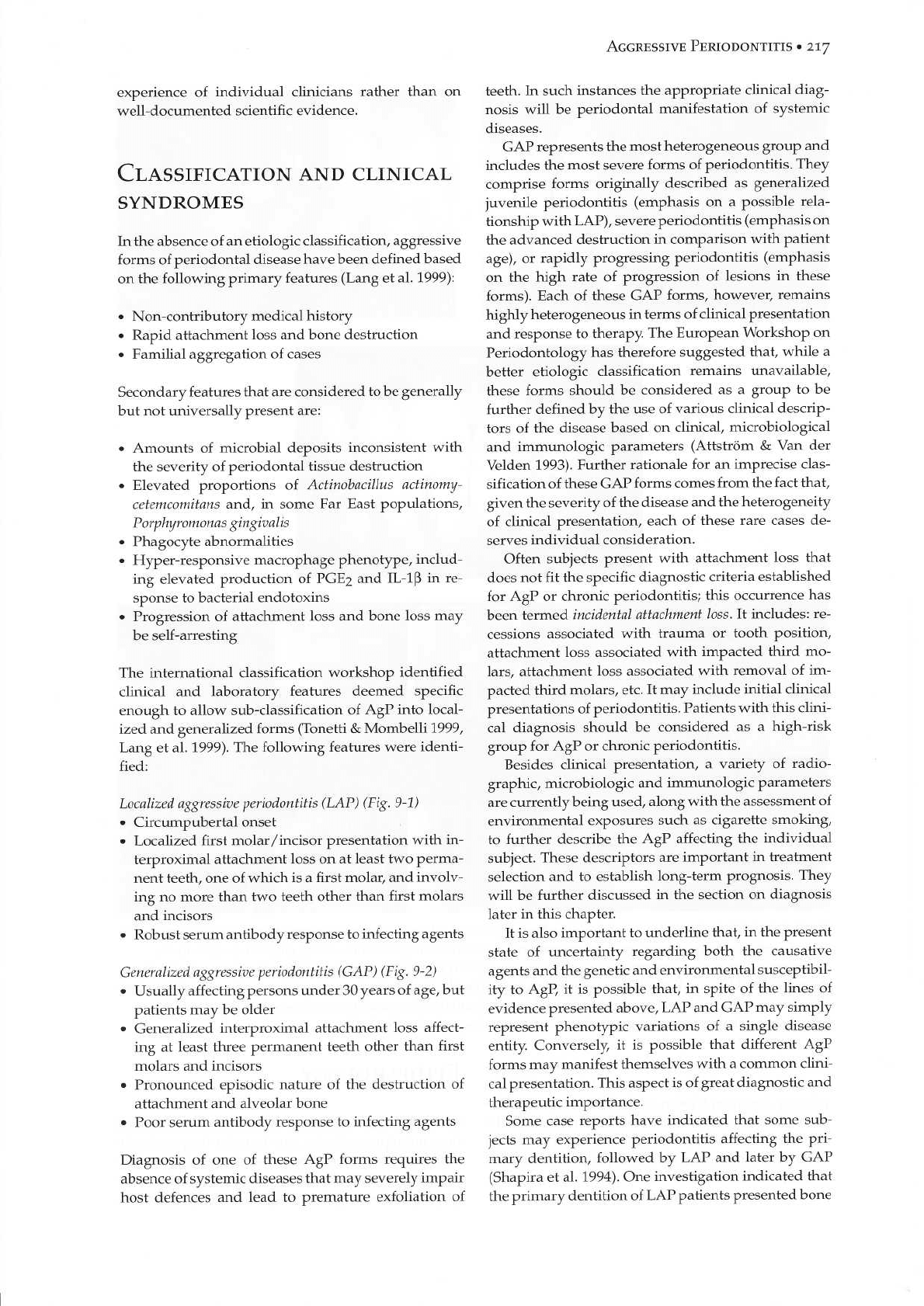
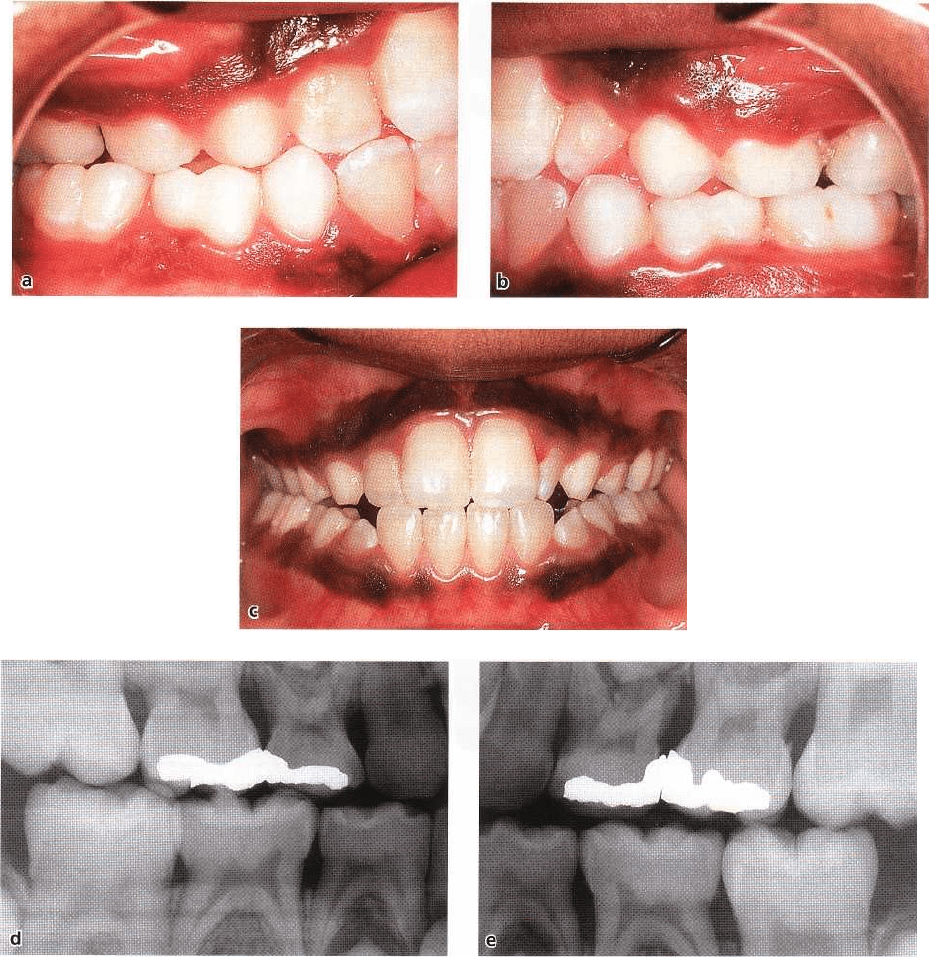
Fig. 9-1. (a-c) Clinical appearance of the periodontal tissues of a 15-year-old girl suffering from localized aggressive
periodontitis. Note the proper oral hygiene conditions and the scalloped outline of the gingival margin. In the
lower
anterior region, the interdental papilla between teeth 31 and 32 has been lost. Intraoral radiographs (d) show
the
presence of localized angular bony defects, associated with clinical attachment level loss, at the mesial aspect of
tooth
46, 36 and at the distal aspect of tooth 31. No significant bone loss and/or attachment loss was detectable in
other
areas of the dentition. Diagnosis: localized aggressive periodontitis (LAP).
loss at primary molars in 20-52% of the cases, suggest
EPIDEMIOLOGY
ing that at least some LAP cases may initially affect the
primary dentition (Sjodin et al. 1989, 1993). Further-
more, in LAP subjects an association between the Given the recent definition of AgP and the fact that it
number of
lesions and the age of the subject has been does not represent just a new term for the previously
described,
suggesting an age-dependent shift from defined EOP, epidemiological studies available relate
localized to generalized
forms of AgP (Hormand & primarily to EOP. Relatively few investigations em-
Frandsen 1979, Burmeister et al.
1984).
ploying different epidemiological techniques have es-
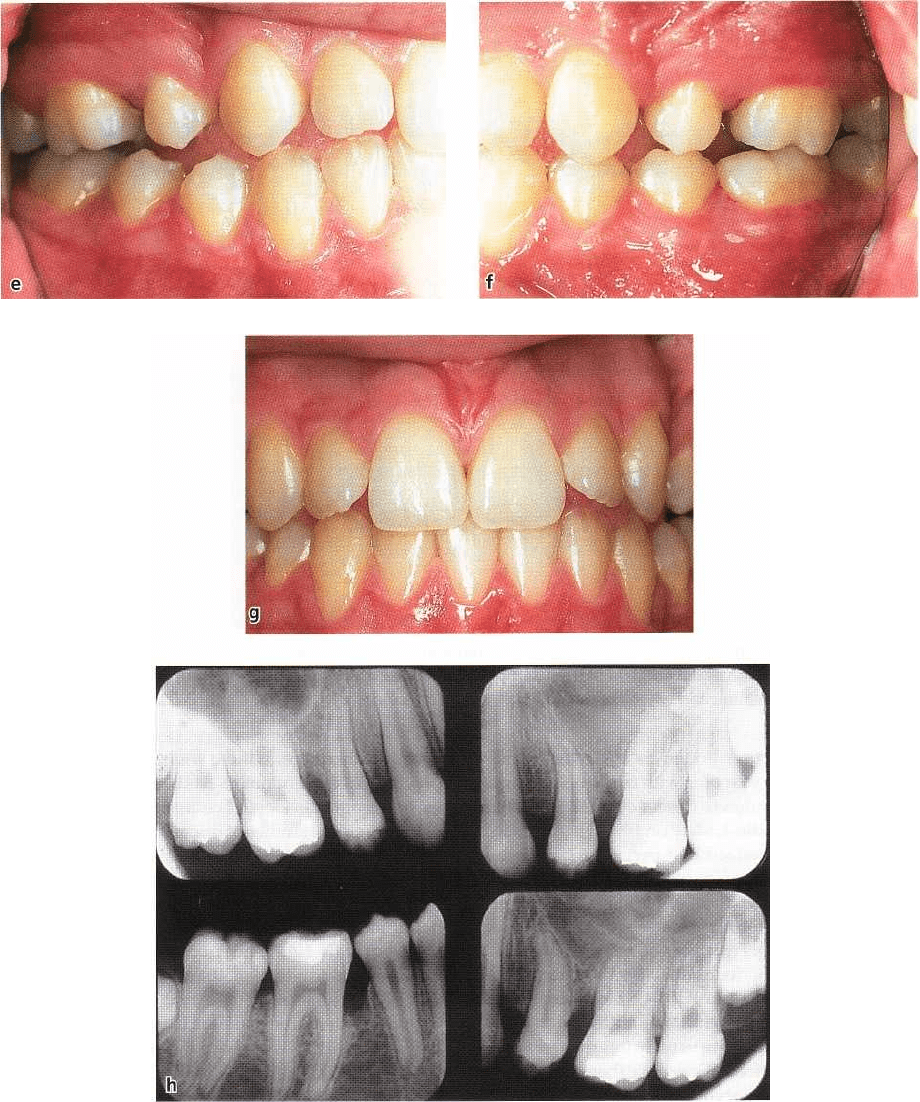
Fig. 9-1. (e-g) Clinical appearance of the 14-year-old sister of the proband depicted in (a-d). Note that in spite of
the excellent oral hygiene status, bleeding on probing was provoked in the mesial of the molars, where deep
pockets were present. (h) Angular bone loss is evident on the mesial of 16, 26 and 46.
timated the prevalence and the progression of EOP in the employed epidemiological methodologies and the
primary and permanent dentition(s) of children definition of EOP.
and young adults. All available investigations, how-
ever, indicate that early onset (aggressive) forms of
periodontal diseases are detectable in all age and eth- Primary dentition
nic groups (Papapanou 1996). Wide variation in
prevalence, however, has been reported, with some Little evidence is available concerning the prevalence
studies showing up to 51.5% affected individuals. of AgP affecting the primary dentition. In the few
These differences are probably due to differences in studies from industrialized countries, marginal alveo-
AGGRESSIVE PERIODONTITIS • 219
220 • CHAPTER 9
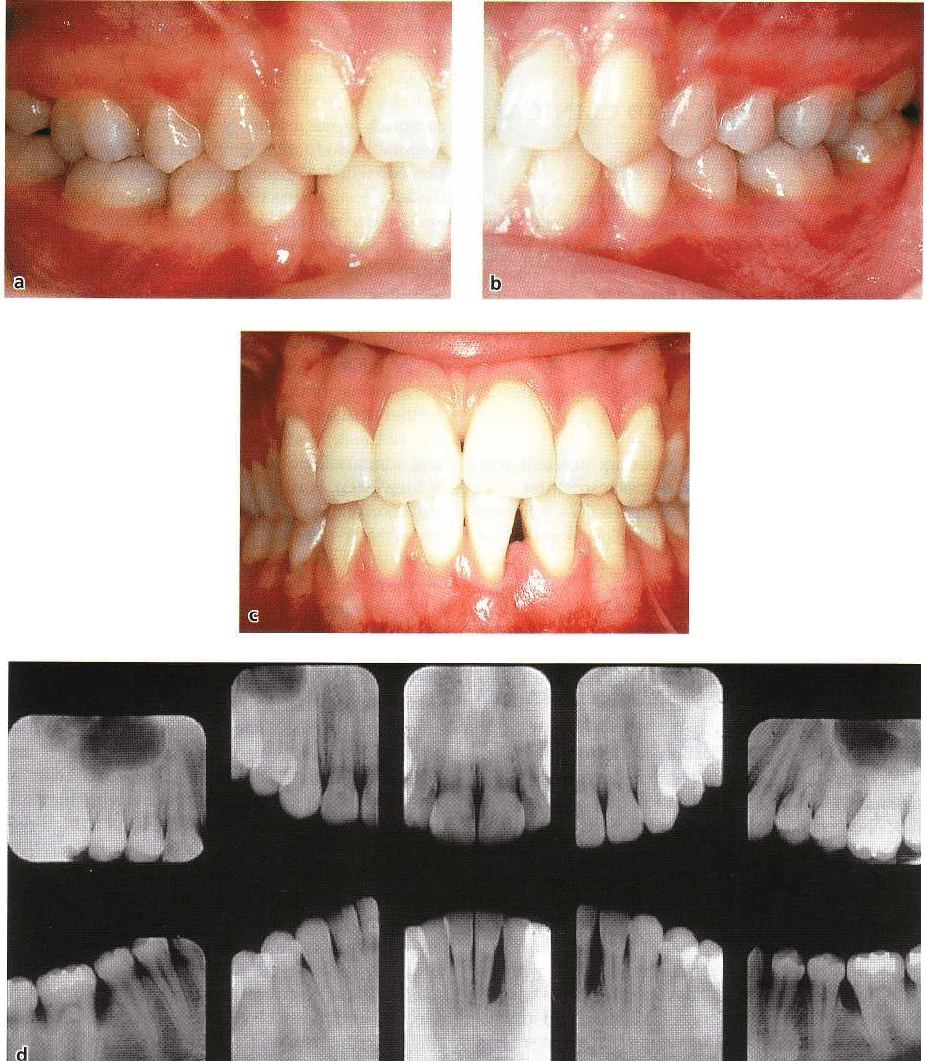
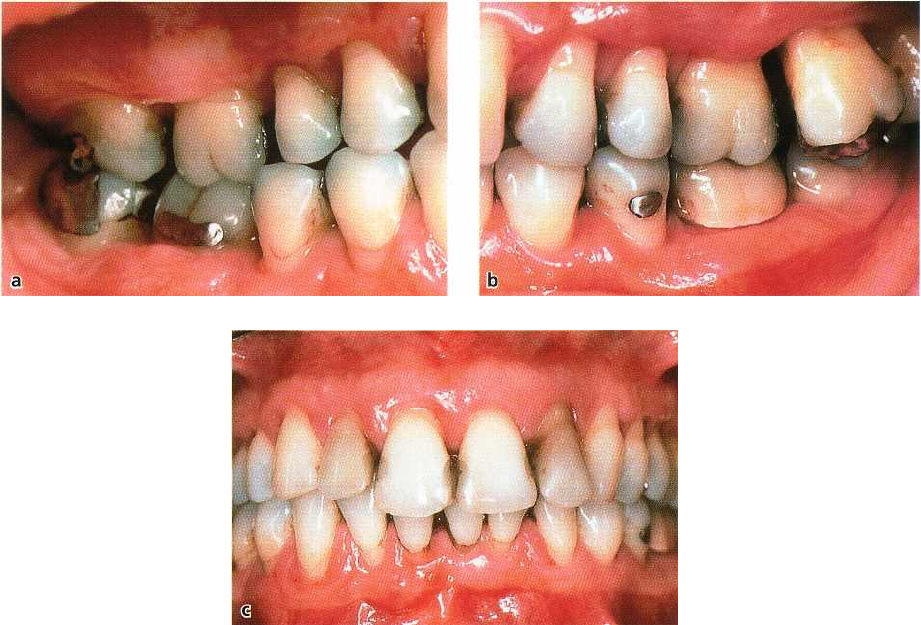
Fig. 9-2. (a-c) Clinical presentation in 1990 of a 32-year-old female with generalized severe bone loss and clinical at
tachment loss, recession of the gingival margin and presence of deep periodontal pockets. Presence of local
factors, and intense inflammation and edema of the gingival margin are evident.
lar bone loss has been found to affect the primary
dentition of 5 to 11 year olds with frequencies ranging
from 0.9-4.5% of subjects (Sweeney et al. 1987, Bim-
stein et al. 1994, Sjodin & Mattson 1994). In this respect,
it should be emphasized that periodontitis affecting
the primary dentition does not necessarily mean pres-
ence of an aggressive form of periodontitis, but may
indicate a chronic form of disease with relative abun-
dance of local factors (plaque and calculus). A clinical
case of localized periodontitis affecting the primary
dentition is illustrated in Fig. 9-3. More severe cases
affecting the primary dentition and leading to tooth
exfoliation early in life are usually interpreted as peri-
odontal manifestations of systemic (hematologic) dis-
eases, such as leukocyte adhesion deficiency (see
Chapter 2 and Fig. 9-4).
Permanent dentition
In the permanent dentition of 13 to 20-year-old indi-
viduals, the majority of studies have reported a preva-
lence of periodontitis of less than 1% (usually 0.1-0.2%
in Caucasian populations). The risk of developing
periodontitis at such an early age, however, does not
seem to be shared equally in the population: among
US schoolchildren 5-17 years of age, the prevalence of
periodontitis has been estimated to range from about
0.2% for whites to about 2.6% for blacks (Loe & Brown
1991). Furthermore, in these young age groups higher
prevalence of periodontitis has been reported in stud-
ies from some developing countries (see Chapter 2).
Longitudinal studies of disease progression in ado-
lescents indicate that subjects with signs of destructive
periodontitis at a young age are prone to further dete-
rioration. Such deterioration appears to be more pro-
nounced at initially affected sites, and in patients di-
agnosed with LAP and from low socio-economic
classes. Deterioration of the periodontal status in-
volves both an increase in extent (number of lesions
within the dentition) and an increase in severity of
lesions (further alveolar bone loss at initially diseased
sites, Fig. 9-5) (Clerehugh et al. 1990, Lissau et al. 1990,
Albandar et al. 1991a,b, 1993, Aass et al. 1994).
Some epidemiological investigations have re-
ported high prevalence of attachment loss in adoles-
cents and young adults that did not fit the charac-
teristics of recognized periodontitis clinical syn-
dromes. Such occurrences have been termed incidental
attachment loss, and have been reported in 1.6-26% of
the subjects. This group is thought to comprise both
initial forms of periodontitis (including AgP) and a
variety of defects such as recession due to traumatic
tooth-brushing, attachment loss associated with re-
moval of impacted third molars, etc.
Conclusion
A small but significant proportion of children and
AGGRESSIVE PERIODONTITIS • 221
Fig. 9-2. (d-f). Previous radio-
graphic examinations were avail-
able from 1984 and 1987. Compari
son of the radiographs obtained
over the 6-year period from 1984
to 1990 indicates that most of the
periodontal destruction occurred
during the last 3 years. The pa-
tient had been smoking 20 ciga-
rettes/day for more than 10 years.
Diagnosis: Generalized aggressive
periodontitis (GAP) in a cigarette
smoker.
young adults is affected by some form of periodonti-
tis. A substantial proportion of these subjects is
thought to be affected by AgP. Given the severity of
these forms of periodontal diseases and their tendency
to progress, early detection of periodontitis, and AgP
in particular, should be a primary concern of both
practitioners and public health officers. The whole
population, including children and young adults,
should receive a periodontal screening as part of their
routine dental examination.
Screening
Given the low prevalence of AgP patients within the
population, cost-effective detection of cases requires
utilization of a sensitive screening approach, i.e. the
application of a diagnostic approach able to correctly
identify most of the cases with disease. The objective
of screening is the detection in a population of possi-
bly diseased subjects that would require a more com-
prehensive examination. In periodontology, the most
sensitive diagnostic test for the detection of periodon-
titis is the measurement of attachment loss by probing.
Application of this diagnostic procedure in the mixed
dentition and in teeth that are not fully erupted, how-
ever, may be difficult.
In younger subjects, therefore, a currently utilized
screening approach is the measurement of the dis-
tance between the alveolar crest and the cemento-
enamel junction on bite-wing radiographs. An advan-
tage of this approach relates to the fact that in most
industrialized countries bite-wing radiographs of
children and young adolescents in mixed dentition are
routinely taken for caries prevention programs; these
radiographs should therefore be screened not only for
carious lesions but also for the presence of marginal
alveolar bone loss.
Recent investigations have attempted to determine
the "normal" distance between the cemento-enamel
222 • CHAPTER
9
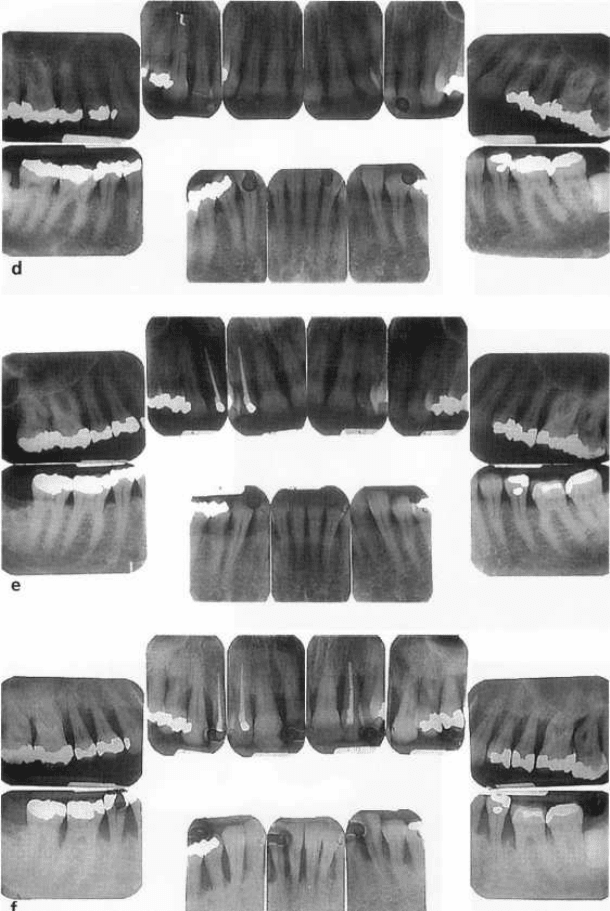
Fig. 9-3. Seven-year-old African-American female presenting with radiographic alveolar bone loss and probing at-
tachment loss at the primary molars and permanent first molars and incisors: (a-c) clinical photographs, buccal
view; (d-e) bite-wing radiographs. Clinical presentation shows moderate plaque accumulation, localized gingival
inflammation, with ulceration of the gingival margin and loss of the interdental papilla mesial of #65. 4-6 mm pock-
ets with bleeding on probing were present in the primary molar regions. Bone loss and attachment loss were lim-
ited to the molar region. The mesial aspects of the first permanent molars are also initially involved. Radiographic
subgingival calculus is evident. Note that the upper left posterior sextant seems to be more severely affected than
the other posterior segments. Diagnosis: localized aggressive (type 1) periodontitis.
junction and the alveolar crest of primary and perma-
nent molars in 7 to 9-year-old children (Sjodin &
Mattson 1992, Needleman et al. 1997). Median dis-
tances at primary molars were 0.8 to 1.4 mm. These
values were in agreement with those previously re-
ported for primary molars of 3 to 11-year-old children
(Bimstein & Soskolne 1988). The cemento-enamel
junction of permanent molars was 0 to 0.5 mm apical
to the alveolar crest in 7 to 9 year olds. These values
were age-dependent, and related to the state of erup-
tion of the tooth. In general, however, it should be
noted that the majority of children present with dis-
tances significantly smaller than the 2-3 mm consid-
ered normal for the completely erupted dentitions of
adults. In children, significantly greater distances have
been detected at sites with caries, fillings or open
contacts, indicating that these factors may contribute
to bone loss in similar ways to in adult patients. Fur-
thermore, presence of one of these local factors may
suggest a local cause of bone loss, other than perio-
