Cui Dongmei. Atlas of Histology: with functional and clinical correlations. 1st ed
Подождите немного. Документ загружается.

CHAPTER 12
■
Urinary System
235
CLINICAL CORRELATIONS
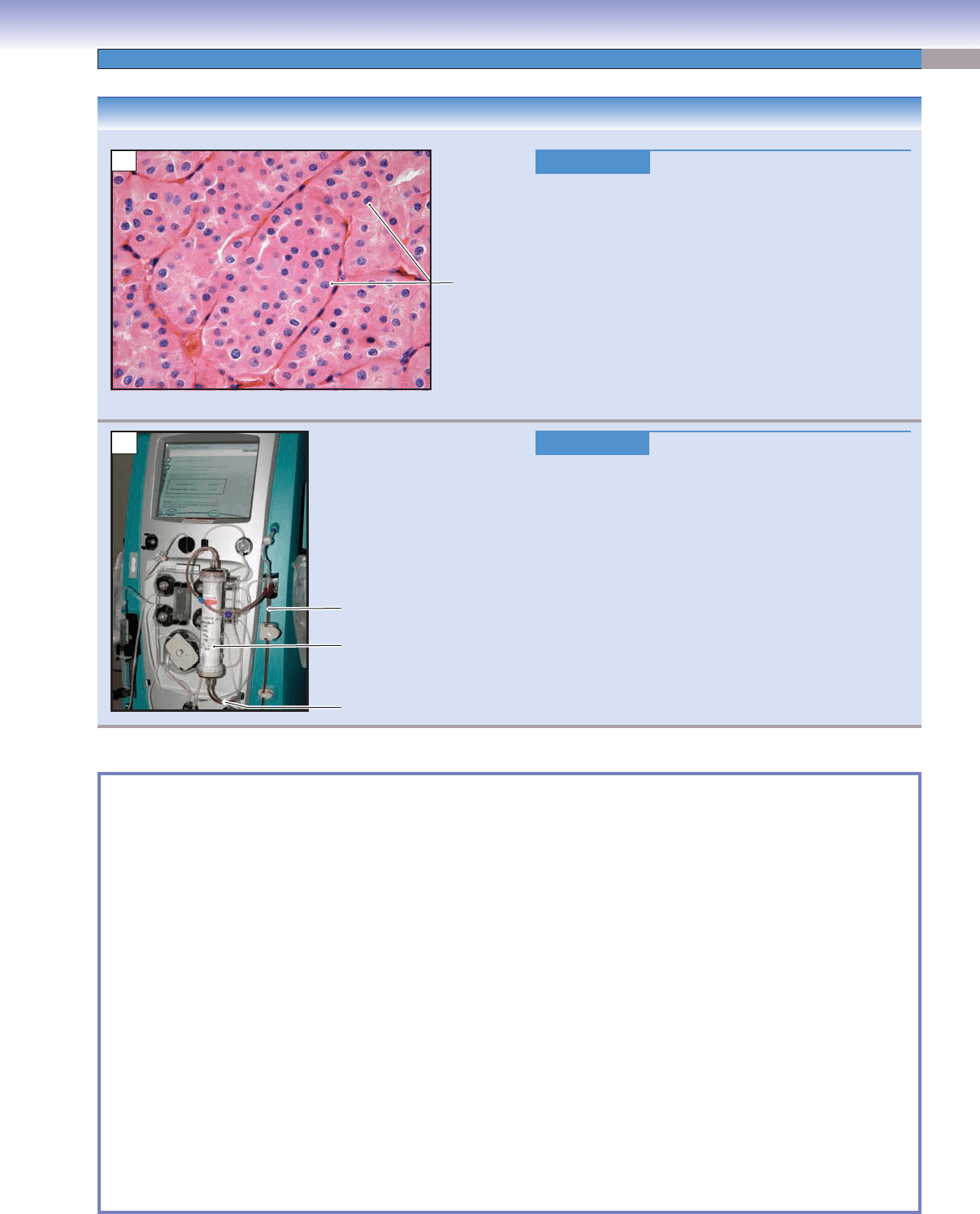
Figure 12-12A.
Renal Oncocytoma. H&E, 216
Renal oncocytoma is a benign and less common neoplasm
of the kidney and originates from the epithelium of the
proximal tubules. It is typically a solid, encapsulated mass
with homogeneous enhancement in radiographic imaging.
Gross examination shows a spherical mass with a mahog-
any cut surface and a tan, fl
eshy central scar. Histologi-
cally, the tumor cells are large with abundant eosinophilic
cytoplasm due to the presence of numerous mitochondria.
The cells are arranged in sheets or in a tubulocystic pat-
tern. It is usually asymptomatic and detected as an inci-
dental renal mass on imaging. Treatment options include
surgical excision of the kidney (nephrectomy) or removal
of a portion of the kidney (partial nephrectomy).
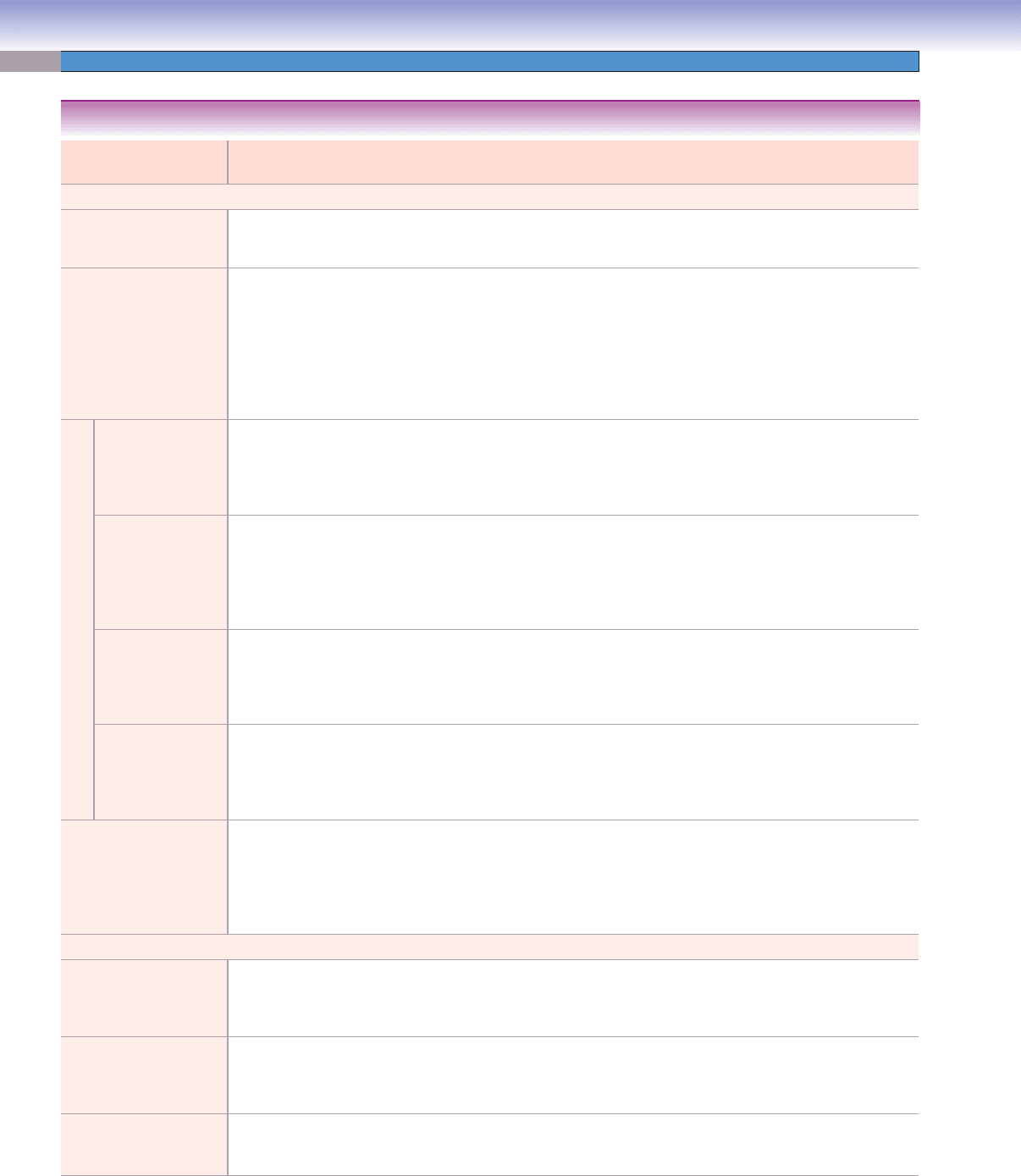
Figure 12-12B.
Hemodialysis.
Hemodialysis is a common treatment for end-stage kidney
disease. The dialyzer is a canister containing thousands of
small fi
bers through which blood is passed. The fi bers are
made up of semipermeable membranes with small pores
allowing wastes and extra fl uids to pass from the blood
into a solution. A cleansing fl uid called dialysate is pumped
around the fi bers. Solute and extra fl uids are cleared from
the blood compartment by either diffusion or ultrafi ltra-
tion, depending on the concentration gradient and pres-
sure difference between the blood and the dialysate. The
cleansed blood is returned via the circuit back to the body.
Hemodialysis is usually given three times a week and can
be done in a dialysis center or at home. The model illus-
trated here is commonly used in critical care units.
Neoplastic
oncocytic
cells
A
Blood from patient
Blood back to patient
Dialyzer
B
SYNOPSIS 12-1 Clinical and Pathological Terms for the Urinary System
Glomerulonephritis ■ : Refers to primary glomerular disease not related to infection of the kidneys themselves. The causes of
glomerulonephritis are heterogeneous, such as viral or bacterial infection; drugs; and malignancy, resulting in many distinct
clinical entities including focal and segmental glomerulonephritis and membranous nephropathy. The causes are often not
identifi ed (idiopathic glomerulonephritis).
Glomerulopathy
■ : Refers to secondary glomerular injury as a result of systemic diseases, such as diabetes mellitus and
systemic lupus erythematosus.
Glomerulosclerosis
■ : Scarring or sclerosis of the renal glomeruli in diseases such as diabetic nephropathy and focal segmental
glomerulosclerosis.
Dysuria
■ : Pain or burning upon urination, most often caused by a urinary tract infection affecting the bladder (cystitis) or
urethra (urethritis).
Frequency
■ : The need to urinate more often than normal without an increase in total urine output; common causes include
lower urinary tract infection and benign prostatic hyperplasia; other less common causes include tumors and extrinsic
bladder compression.
Hematuria
■ : The presence of blood in the urine, causes of which include trauma, infection, tumors of the urinary system,
kidney stones, and hyperplasia of the prostate gland; hematuria may be microscopic or “macroscopic,” meaning visible
to the unaided eye.
Lithotripsy
■ : Extracorporeal shock wave lithotripsy is a procedure for treating kidney and ureteral stones using focused
high-energy shock waves that pass through the body and break stones into small pieces that can then pass into the urine
and be eliminated.
Urgency
■ : A strong urge to urinate, most often caused by a lower urinary tract infection or other causes of bladder irritation
such as interstitial cystitis, which mainly affects females.
CUI_Chap12.indd 235 6/2/2010 6:37:14 PM
236
UNIT 3
■
Organ Systems
Structure Epithelial Lining
of the Tubules
Characteristics of the Tubules Main
Locations
Main Functions
Nephron
Renal corpuscle Simple squamous
epithelium
Composed of glomerulus (blood
vessels covered by podocytes) and
Bowman capsule
Renal cortex Filters blood and forms
urine
Proximal convoluted
tubule
Simple cuboidal
epithelium with
long microvilli
(brush border)
Long and highly convoluted
tubule; relatively small lumen and
acidophilic cytoplasm; abundant
mitochondria; numerous
basolateral plasma membrane
enfoldings
Renal cortex Drains fl uid from the renal
corpuscle to the loop of
Henle; reabsorbs 70%–80%
Na
+
and Cl
−
and water; also
reabsorbs glucose, amino
acids, and proteins and
produces calcitriol (active
form vitamin D)
The Loop of Henle
Thick descending
limb (proximal
straight tubule)
Simple cuboidal
epithelium with
long microvilli
(brush border)
Similar to proximal convoluted
tubule but shorter and straight;
small mitochondria; no
basolateral plasma membrane
enfoldings
Medullary
ray and outer
zone of the
renal medulla
Absorptive function
is similar to proximal
convoluted tubule but
less signifi cant
Thin descending
limb (descending
thin segment)
Simple squamous
epithelium
Thin, small tubule; epithelial cells
may reveal basolateral enfoldings
and small microvilli
Partial outer
zone and most
of the inner
zone of the
renal medulla
Highly permeable to water
(loss of water from lumen to
interstitium); less permeable
to salt (keeps or may gain
some Na
+
and Cl
−
in the
lumen)
Thin ascending
limb (ascending
thin segment)
Simple squamous
epithelium
Similar to descending thin
segment; may have basolateral
enfoldings and small microvilli
Inner zone
of the renal
medulla
Impermeable to water
(retains water); highly
permeable to salt (loss of
Na
+
and Cl
−
from the lumen
to the interstitium)
Thick ascend-
ing limb (distal
straight tubule)
Simple cuboidal
epithelium with
short microvilli
Straight tubule; numerous
mitochondria; less acidophilic
cytoplasm; many basolateral
plasma membrane enfoldings
Medullary
ray and outer
zone of the
renal medulla
Impermeable to water
(retains water); highly
permeable to salt (loss of
Na
+
and Cl
−
from the lumen
to the interstitium)
Distal convoluted
tubule
Simple cuboidal
epithelium with
short microvilli
Numerous mitochondria;
basolateral plasma membrane
enfoldings; less acidophilic
cytoplasm; highly convoluted
tubule
Renal cortex Reabsorbs Na
+
and
secretes K
+
, if aldosterone
stimulation is present;
reabsorbs bicarbonate ions
and secretes ammonium to
adjust pH
Collecting System
Collecting tubule Simple cuboidal
epithelium with
few microvilli
Straight tubule; much less
acidophilic cytoplasm; more than
one cell type
Renal cortex Highly permeable to water;
loss of water from the
lumen to the interstitium
when ADH is present
Collecting duct Simple columnar Large straight tubule; clear
cytoplasm and distinct
boundaries between cells;
well- developed basal enfoldings
Medullary
ray and renal
medulla
Highly permeable to water;
loss of water from the
lumen to the interstitium
when ADH is present
Papillary duct Simple columnar
epithelium
Short duct; links collecting duct
to the minor calyx
Bottom tip of
the pyramid
of the medulla
Conducts urine
TABLE 12-1 Kidneys
CUI_Chap12.indd 236 6/2/2010 6:37:16 PM
CHAPTER 12
■
Urinary System
237
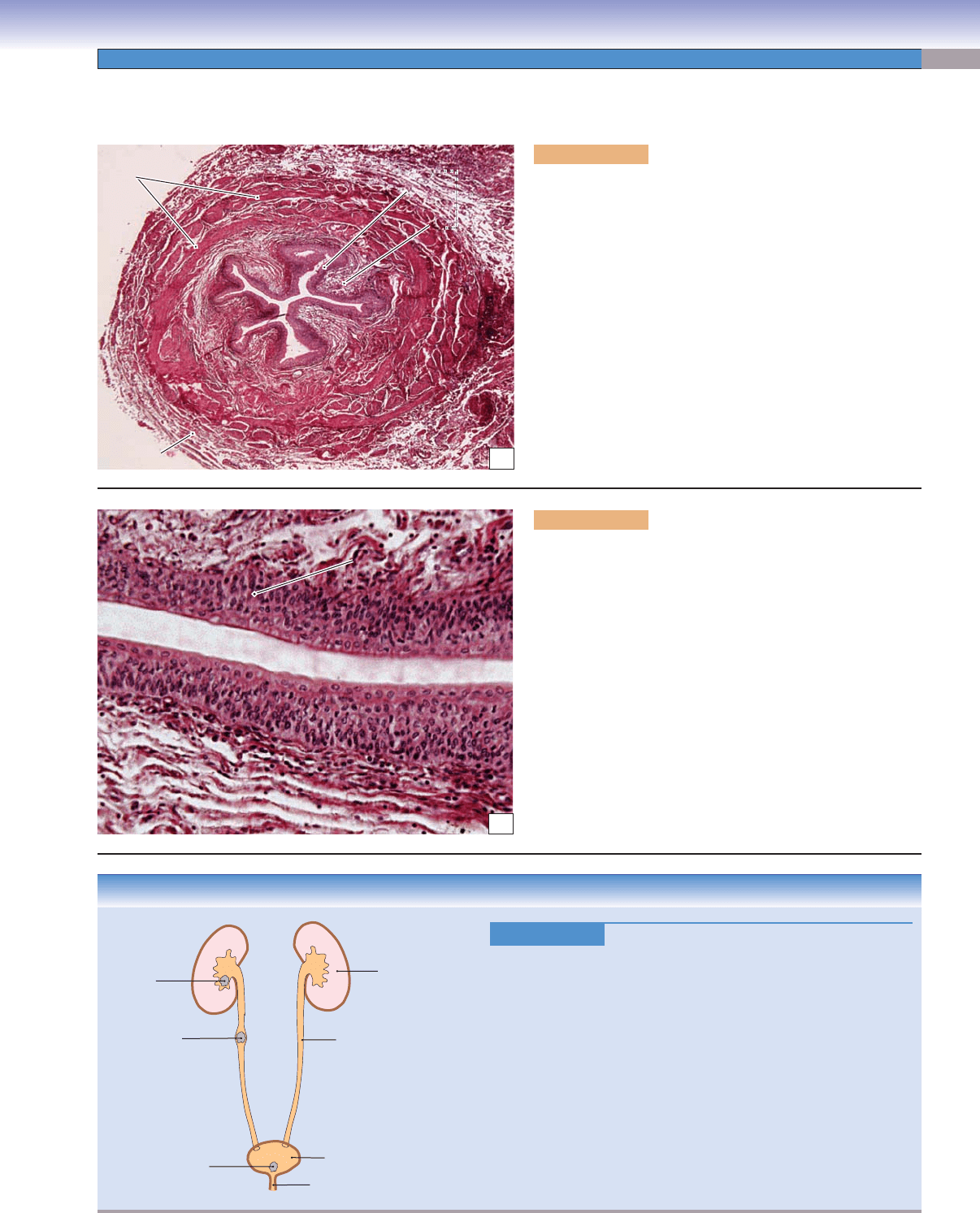
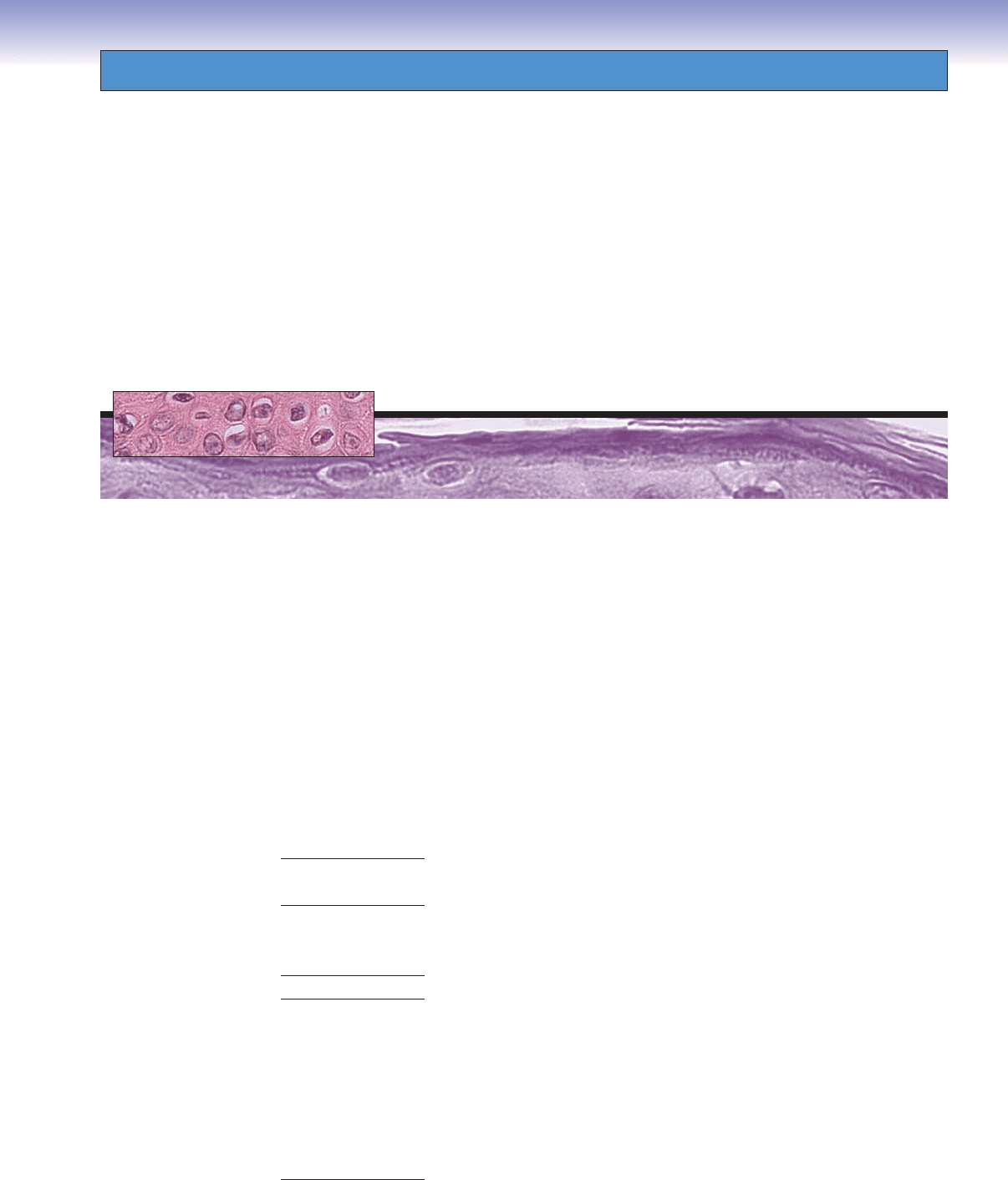
Figure 12-13A. Ureter. H&E, 61
The ureter is a small muscular tubule lined with transitional
epithelium. It carries urine from the renal pelvis to the urinary
bladder. The wall of the ureter is composed of mucosa,
muscularis, and adventitia. The mucosa consists of transitional
epithelium and loose connective tissue (lamina propria). The
middle layer, the muscularis, is relatively thick and contains
inner longitudinal and outer circular smooth muscle layers.
These two muscle layers are often diffi cult to distinguish. The
wall of the ureter becomes thicker as it nears the bladder. As
it approaches the urinary bladder, the ureter may also contain
a third layer of smooth muscle. The adventitia layer is com-
posed of connective tissues, nerve fi bers, and blood vessels. It
provides protection, blood supply, and nervous innervation
to the ureter.
Muscularis
Muscularis
Muscularis
Adventitia
Epithelium
Epithelium
Epithelium
Lamina
Lamina
propria
propria
Lamina
propria
Mucosa
Mucosa
Mucosa
A
CLINICAL CORRELATION
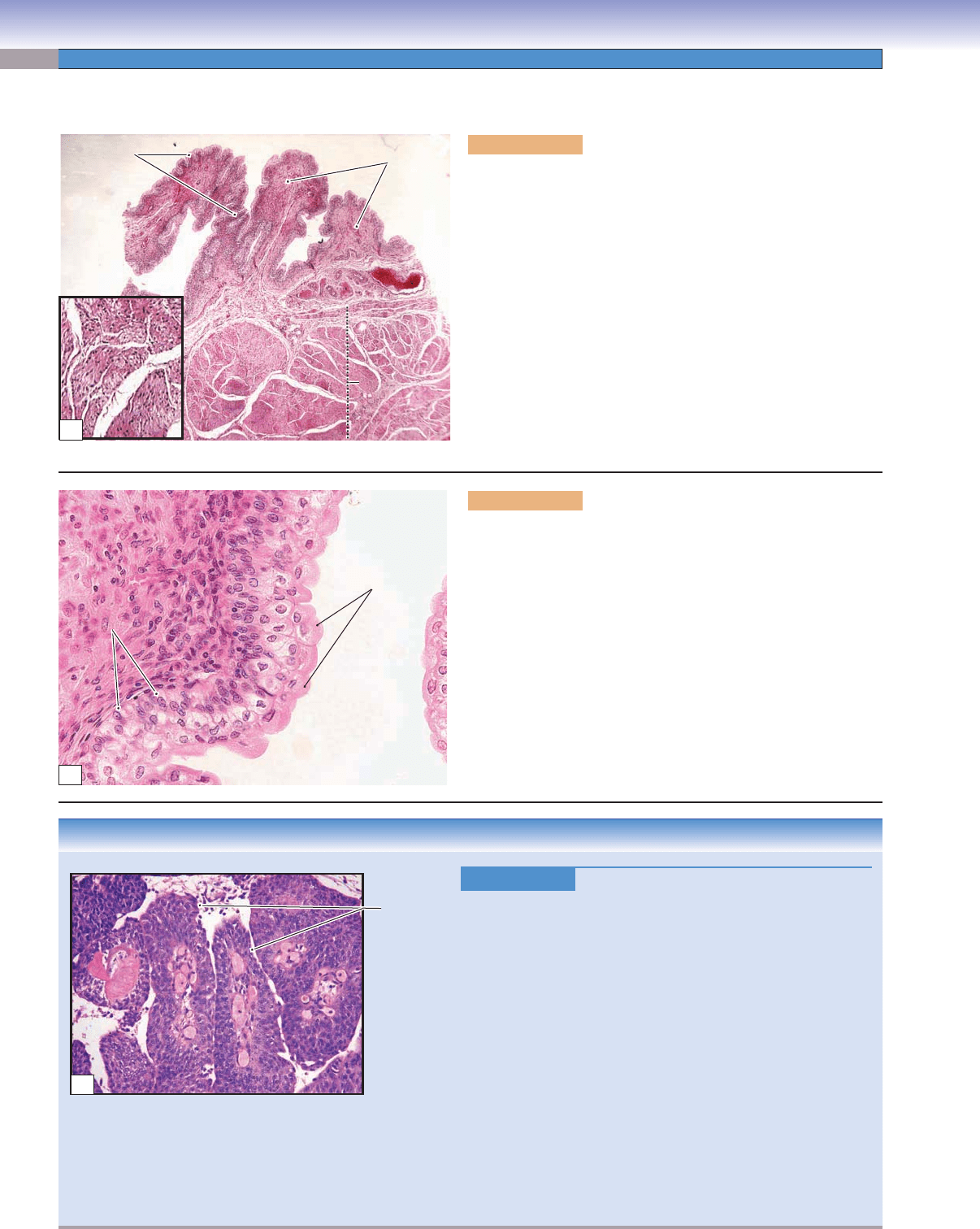
Figure 12-13C.
Nephrolithiasis (Renal Stones).
Nephrolithiasis (renal stones) is common in clinical practice.
Symptoms range from vague abdominal pain to renal colic
and hematuria when stones pass from the renal pelvis into the
narrow portion of the ureter
. Most renal stones are composed of
the calcium salts, calcium oxalate, or calcium phosphate. Other
less common forms include uric acid, magnesium ammonium
phosphate (struvite), and cystine stones. Risk factors for the
development of kidney stones include dietary factors, metabolic
abnormalities, abnormal urine pH, family history of renal stones,
frequent upper urinary tract infections, and low fl uid intake.
Struvite stones are associated with urinary tract infection with
urea-splitting bacteria such as Proteus species. Treatment varies
based upon the location and size of the stones and includes
analgesics, shock wave lithotripsy, ureteroscopy, and surgery.
D. Cui &T. Yang
Stone
in kidney
Stone
in ureter
Kidney
Ureter
Bladder
Urethra
Stone
in bladder
C
Ureters
Transitional
Transitional
epithelium
epithelium
Transitional
epithelium
Luman
Luman
Lumen
Lamina propria
Lamina propria
(connective tissue)
(connective tissue)
Lamina propria
(connective tissue)
B
Figure 12-13B. Transitional epithelium, ureter. H&E,
190
Transitional epithelium lines the urinary tract from the
urinary calyces to the bladder. This type of epithelium can
change shape as it is stretched to accommodate a change in
volume. Cells on the surface layer appear round and dome
shaped when the bladder is in a relaxed state. These cells
become fl attened and the layers of cells are reduced in number
when the epithelium is stretched. The transitional epithelium
lining the urinary tract is also called urothelium; it has tight
junctions and thick cytoplasm (Figs. 12-14B and 12-15A,B).
The lumen of the ureter appears as a white space here.
CUI_Chap12.indd 237 6/2/2010 6:37:16 PM
238
UNIT 3
■
Organ Systems
Urinary Bladder
CLINICAL CORRELATION
Figure 12-14C.
Urothelial (Transitional) Carcinoma. H&E,
108
Urothelial carcinoma may arise in the urinary bladder
, ureters, or
renal pelvis and is the most common urinary bladder carcinoma.
More than 90% of bladder cancers originate from the transi-
tional epithelium (urothelium) in the urinary system. Urothelial
carcinoma is most prevalent in older men but may occur at any
age. Risk factors include cigarette smoking, exposure to arylam-
ines and radiation, long-term use of cyclophosphamide, and
infection by the parasite Schistosoma haematobium. Infection
with S. haematobium is also a risk factor for the development
of squamous cell carcinoma of the urinary bladder. Symptoms
include painless gross hematuria, frequency, urgency, and dysu-
ria. Urothelial carcinomas typically display a papillary morphol-
ogy and are subdivided into low and high grade depending on
cytologic features and the amount of architectural disorder pres-
ent. Treatment includes transurethral resection, chemotherapy,
immunotherapy, and radical cystectomy. Tumors have a high
recurrence rate after local excision.
Papillae in
urothelial
carcinoma
C
Figure 12-14A. Urinary bladder, bladder wall. H&E, 17;
inset 82
The urinary bladder has three layers (mucosa, muscularis, and
adventitia/serosa), similar to those in the ureter, but its wall is
much thicker. Thick mucosa and muscularis layers make up the
wall of the urinary bladder. The mucosa is composed of exten-
sively folded transitional epithelium and lamina propria. This
arrangement gives the bladder the distensibility needed to store
urine. The muscularis consists of three smooth muscle layers: the
inner longitudinal, middle circular, and outer longitudinal smooth
muscle. These three smooth muscle layers are arranged in two dif-
ferent orientations to help the urinary bladder contract to empty
urine effi ciently. The outer layer of the bladder is mainly covered
by adventitia (connective tissue); its superior (free) surface is cov-
ered by serosa, which is a layer of connective tissue with a lining
of mesothelium.
Lamina
propria
Muscularis
Muscularis
Muscularis
Smooth muscle
Smooth muscle
Smooth muscle
Submucosa
Submucosa
Submucosa
Epithelium
A
Lamina
Lamina
propria
propria
Lamina
propria
Basal cells
Basal cells
Basal cells
Dome-shaped
surface cells
B
Figure 12-14B. Urothelium, bladder wall. H&E, 278
This fi gure shows the urothelium (transitional epithelium) in a
relaxed state. The urothelial lining of the urinary bladder is thicker
than that of the ureter. The basal cells of the urothelium are cuboi-
dal or columnar in shape, the cells in the middle layer of the urothe-
lium are polygonal, and the surface cells are dome shaped and
bulge into the lumen when the bladder is empty (relaxed state).
When the bladder is full, the urothelium is stretched, the cells
become fl attened, and the thickness of the urothelium is greatly
reduced (see Fig. 3-17B).
CUI_Chap12.indd 238 6/2/2010 6:37:21 PM
CHAPTER 12
■
Urinary System
239
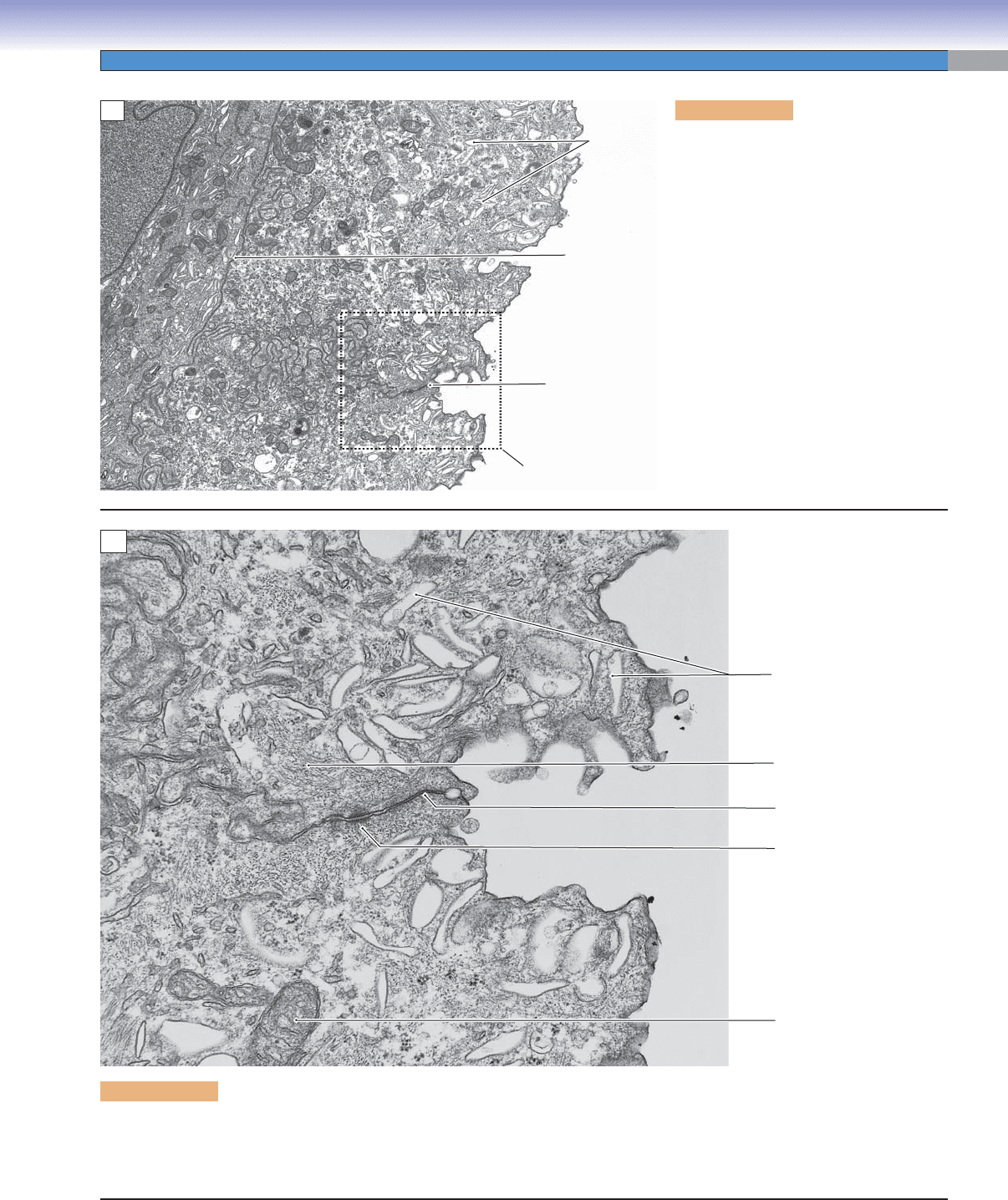
Figure 12-15A. Transitional epithelium,
urinary bladder. EM, 7,280
This fi gure shows the surface of transitional
epithelium and the border between the
cells of the top layer and the underlying
layer. There are many fl attened vesicles
(membrane vesicles) in the cytoplasm of
these cells. The vesicles are more numer-
ous close to the apical region of the cyto-
plasm. These vesicles are formed from the
surface membrane when the bladder is in a
relaxed state. It is important to recall that
the surface of the transitional epithelium
of the bladder is highly convoluted when
the bladder is empty (relaxed). This may
create many “pseudovesicles”; most of the
vesicles disappear when the surface of the
epithelium is stretched and fl attened in the
distended state. The boxed area indicates
Figure 12-15B at higher magnifi cation.
Flattened
Flattened
vesicles
vesicles
Flattened
vesicles
Border between
Border between
two cell layers
two cell layers
Border between
two cell layers
Junctional
Junctional
complex
complex
Junctional
complex
Fig. 12-14B
Fig. 12-14B
Fig. 12-14B
A
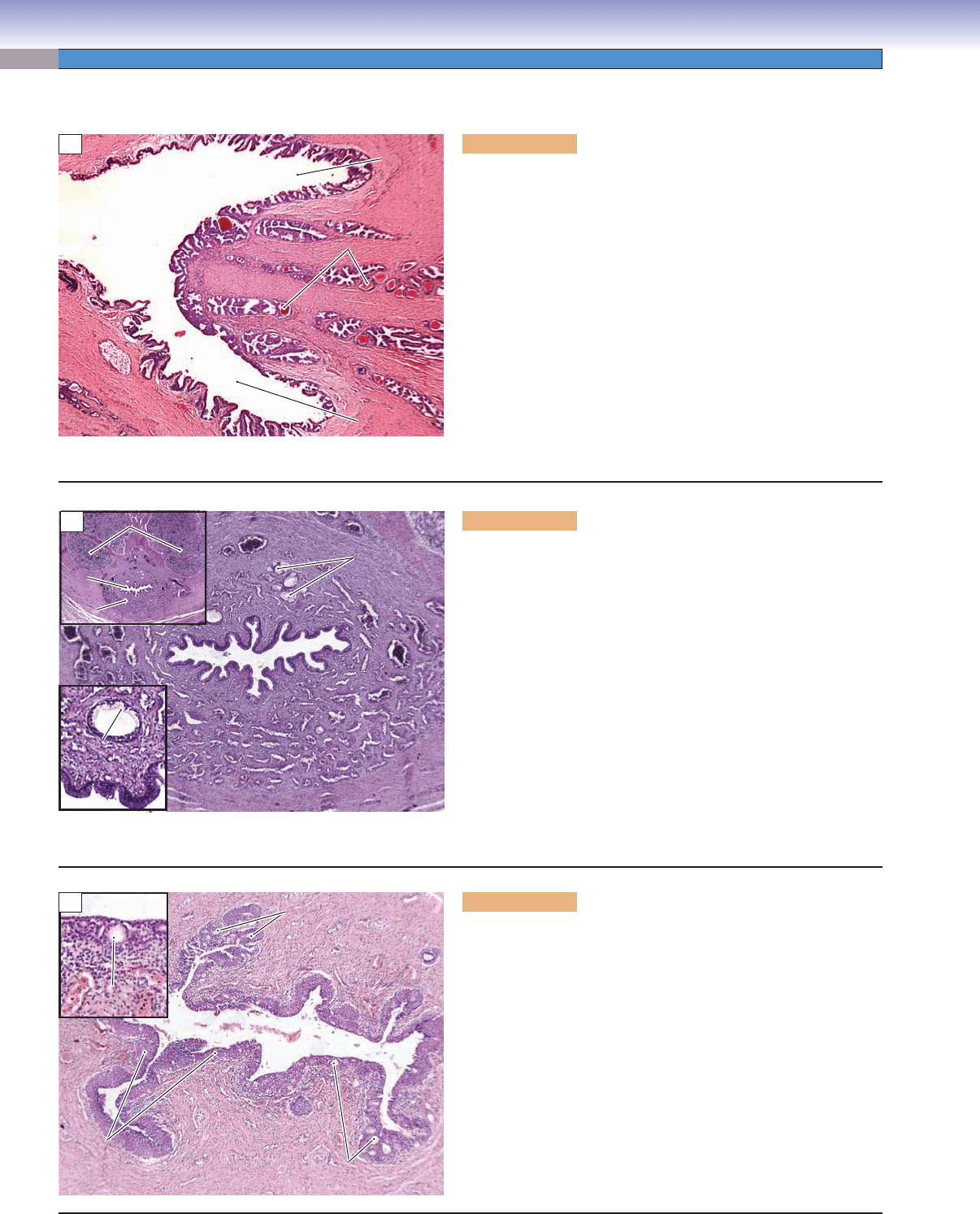
Figure 12-15B. Transitional epithelium, urinary bladder. EM, 35,753
A higher power view of the surface of the top layer cells in the transitional epithelium is shown. The junction complex indicates the
border of neighboring cells. Tight junctions (zonula occludens) and desmosomes (macula adherens) can be observed here. The cells
are fi lled with fl attened vesicles and tonofi laments.
Flattened
Flattened
vesicles
vesicles
Flattened
vesicles
Tonofilaments
Tonofilaments
Tonofilaments
Tight junction
Tight junction
Tight junction
Desmose
Desmose
Desmosome
Mitochondrion
Mitochondrion
Mitochondrion
B
CUI_Chap12.indd 239 6/2/2010 6:37:26 PM
240
UNIT 3
■
Organ Systems
Prostatic
Prostatic
urethra
urethra
Prostatic
urethra
Ejaculatory
Ejaculatory
duct
duct
Ejaculatory
duct
Prostatic glands
Prostatic glands
with concretions
with concretions
Prostatic glands
with concretions
Ejaculatory
Ejaculatory
duct
duct
Ejaculatory
duct
A
Figure 12-16A. Prostatic urethra, male urethra. H&E, 17
The urethra provides for the passage of urine from the bladder to
the outside of the body. The male urethra is signifi cantly different
from that of the female. It is a long tube (18–20 cm), which passes
through the prostate and penis. The male urethra can be divided
into three parts: prostatic, membranous, and penile (spongy) based
on its anatomical location. This fi gure shows a cross section of the
prostatic urethra connecting to two ejaculatory ducts, surrounded
by the prostate. The prostatic urethra is a short segment (3–4 cm),
usually lined by transitional epithelium. This portion of the ure-
thra is surrounded by prostatic glands. The membranous urethra
is narrow and short (1–2 cm) and passes through the deep perineal
pouch. It is lined by pseudostratifi ed columnar epithelium and sur-
rounded by an inner longitudinal smooth muscle and an outer skel-
etal muscle of the external urethral sphincter. The penile (spongy)
urethra is the longest segment (12–14 cm).
Submucosal
Submucosal
glands of Littré
glands of Littré
Submucosal
glands of Littré
Erectile tissue of the
Erectile tissue of the
corpus spongiosum
corpus spongiosum
Erectile tissue of the
corpus spongiosum
Urethra
Urethra
Urethra
Submucosal
Submucosal
glands of Littré
glands of Littré
Submucosal
glands of Littré
Urethra
Urethra
Urethra
Corpus spongiosum
Corpus spongiosum
Corpus spongiosum
Corpora cavernosum
Corpora cavernosum
Corpora cavernosum
B
Figure 12-16B. Penile (spongy) urethra, male urethra. H&E, 34;
inset 6 (upper), 170 (lower)
The penile urethra is also called the spongy urethra because it passes
through the penis and is surrounded by erectile tissue (corpus spon-
giosum). The terms “cavernous” or “bulbous” urethra may also be
used to refer to the penile urethra. The penile urethra is lined by
pseudostratifi ed columnar epithelium. Close to the tip of the penis,
the lining becomes stratifi ed squamous epithelium. This view shows
the urethra in the corpus spongiosum, surrounded by spongy erec-
tile tissue. Within the lining of pseudostratifi ed columnar epithe-
lium are clusters of mucus-secreting cells, the glands of Littré. The
glands of Littré located in the epithelium are called intraepithelial
glands of Littré; similar glands found in the submucosa are termed
submucosal or extraepithelial glands of Littré. The secretions of the
mucous cells of these glands protect the urethra from the effects of
the urine. The upper left inset shows the urethra associated with the
corpus spongiosum and corpora cavernosa in the penis.
Intraepithelial
Intraepithelial
glands of Littré
glands of Littré
Intraepithelial
glands of Littré
Stratified
Stratified
squamous
squamous
epithelium
epithelium
Stratified
squamous
epithelium
Intraepithelial
Intraepithelial
glands of Littré
glands of Littré
Intraepithelial
glands of Littré
Intraepithelial
Intraepithelial
glands of Littré
glands of Littré
Intraepithelial
glands of Littré
Smooth muscle
Smooth muscle
Smooth muscle
Urethra
Urethra
Urethra
C
Figure 12-16C. Urethra, female urethra. H&E, 34; inset 177
The female urethra is 4 to 5 cm long, much shorter than the male
urethra. It conveys urine from the urinary bladder, passing inferi-
orly through the pelvic fl oor and exiting anterior/superior to the
vaginal opening in the vestibule. The female urethra is initially
lined by pseudostratifi ed columnar epithelium, which changes to
stratifi ed squamous epithelium as it approaches the external open-
ing of the urethra. It has a thick lamina propria with many elastic
fi bers and venous plexi. The glands of Littré are also present in
the female urethra. Its wall is surrounded by longitudinal smooth
muscle. The middle portion of the wall of the urethra is surrounded
by the outer layer of the external urethral sphincter, which has the
same function as in the male urethra.
Urethra
CUI_Chap12.indd 240 6/2/2010 6:37:29 PM
241
13
Integumentary
System
Introduction and Key Concepts for the Integumentary System
Layers of the Skin
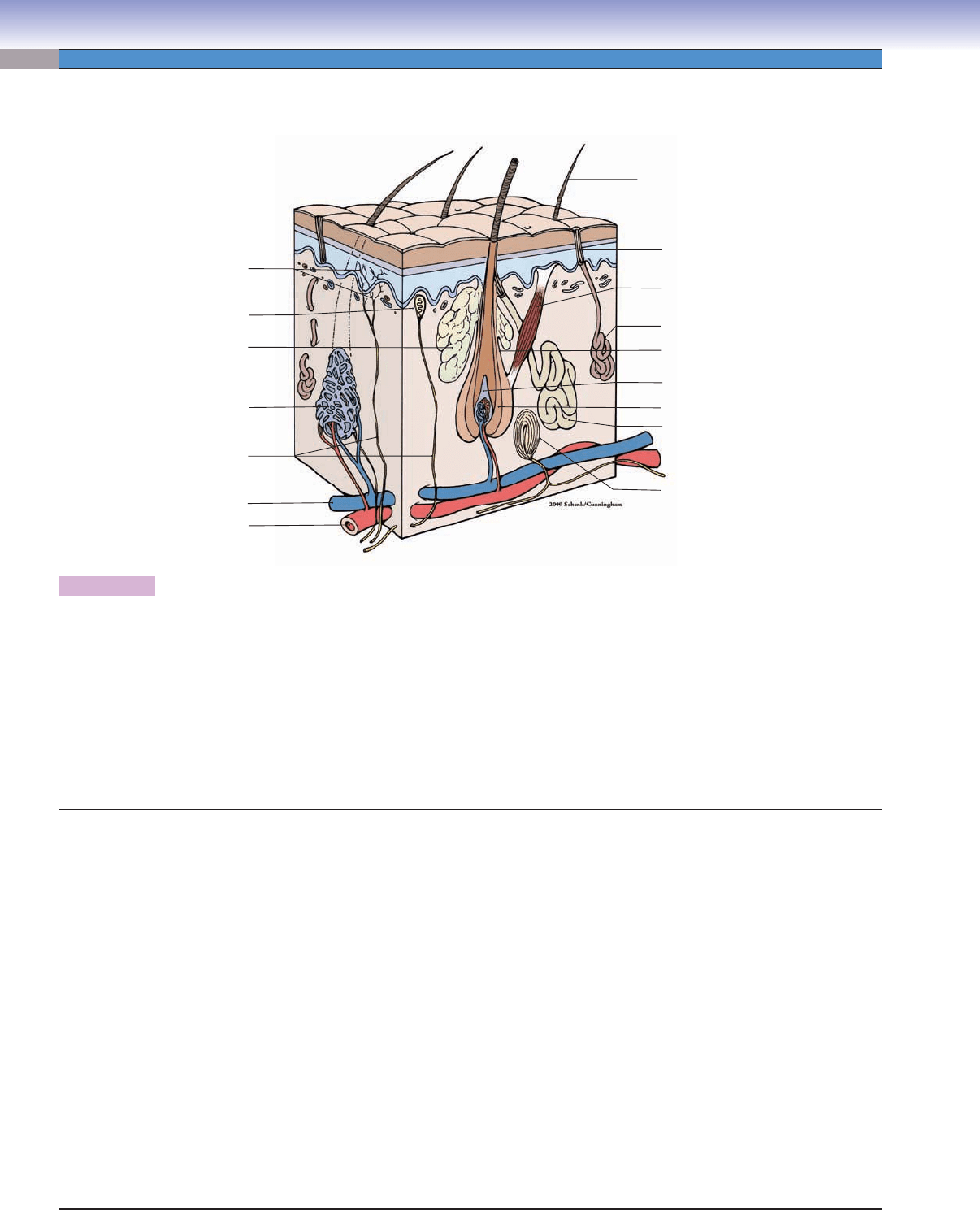
Figure 13-1 Overview of the Structure of the Skin
Figure 13-2 Overview of the Layers of the Epidermis
Synopsis 13-1 Functions of the Skin
Thick Skin
Figure 13-3A Thick Skin, Palm
Figure 13-3B Layers of the Epidermis, Palm
Figure 13-3C Dermal Papilla, Palm
Thin Skin
Figure 13-4A–C Thin Skin
Figure 13-5A Stratum Corneum of the Epidermis, Thin Skin
Figure 13-5B Clinical Correlation: Squamous Cell Carcinoma
Figure 13-6A Keratinocytes in the Stratum Spinosum, Thin Skin
Figure 13-6B Clinical Correlation: Basal Cell Carcinoma
Figure 13-7A Special Types of Cells in the Epidermis, Thin Skin
Figure 13-7B Melanocyte
Figure 13-8A Clinical Correlation: Malignant Melanoma
Figure 13-8B Clinical Correlation: Melanocytic Nevus
Table 13-1 Comparison of Thick and Thin Skin
Accessory Structures
Figure 13-9A Sebaceous Gland, Thin Skin (Scalp)
Figure 13-9B Eccrine Sweat Gland, Thin Skin (Scalp)
Figure 13-9C Apocrine Sweat Gland, Labia
Figure 13-10A,B Hair Follicles
Figure 13-10C Clinical Correlation: Androgenetic Alopecia
Figure 13-11A Nails, Finger
CUI_Chap13.indd 241 6/2/2010 8:20:41 AM
242
UNIT 3
■
Organ Systems
Introduction and Key Concepts
for the Integumentary System
The skin and its accessory structures form the integumentary
system. The skin covers the entire surface of the body and is
the largest organ of the body in terms of its weight and volume.
The accessory structures of the skin include hair, nails, and three
types of glands: sebaceous, eccrine sweat, and apocrine. The
skin is composed of several types of tissues: epithelium, con-
nective tissue, muscles, blood vessels, and nervous tissue. The
functions of skin include (1) Protection: The skin serves as a
barrier between the internal tissues and the outside world, pre-
venting damage to the internal tissues by physical trauma, toxic
chemicals, radiation, and sunlight. (2) Prevention of dehydra-
tion: The skin forms a waterproof barrier, which prevents the
loss of body fl uids. (3) Regulation of body temperature: Evapo-
ration of sweat released onto the body surface by the eccrine
glands as well as dilation of the capillary network and arterio-
venous anastomoses (shunts) in the skin help to regulate body
temperature. (4) Somatosensory function: Sensory receptors in
the skin transduce physical energy in an individual’s surround-
ings into action potentials that are carried by peripheral nerves
to the central nervous system where the sensations of touch,
pressure, pain, warmth, cold, vibration, etc. are generated.
(5) Immunological function: The Langerhans cells and lympho-
cytes in the skin play roles in the cutaneous immune response.
(6) Production of vitamin D: Vitamin D, an essential vitamin,
is synthesized from precursors in the skin under the effects of
steroids and sunlight.
Layers of the Skin
The skin can be divided into two basic layers: epidermis
and dermis. The epidermis is a maximally keratinized strati-
fi ed squamous epithelium, which is composed of fi ve named
layers of cells called keratinocytes. (1) The stratum basale is
the deepest layer of the epidermis and it borders the dermis.
A single layer of cuboidal or tall cuboidal cells lies on the base-
ment membrane. Many of these cells are stem cells that actively
divide and give rise to the cells in the other four layers. The epi-
dermal keratinocytes are renewed constantly, with the top layer
of cells continually being shed and new cells from the stratum
basale replacing them. It takes about 3 to 4 weeks for kerati-
nocytes to fi nish their renewal cycle. In addition to the kerati-
nocyte stem cells, two special types of cells, melanocytes and
Merkel cells (Merkel disks), are found in the stratum basale.
The melanocytes are melanin producing cells which are in con-
tact with the keratinocytes that are located immediately above
the stratum basale (Fig. 13-7A,B). The Merkel cells (Merkel cell
neurite complexes or Merkel disks) are sensory receptor cells,
which respond to continuous touch stimuli. (2) The stratum
spinosum contains polyhedral keratinocytes, which become
more fl attened in the superfi cial part of this layer. The plasma
membrane of neighboring cells is connected by desmosomes
(macula adherens). Langerhans cells (modifi ed macrophages)
are an additional cell type often found in this layer. (3) The
stratum granulosum contains keratinocytes, which are fl attened
cells with keratohyalin granules in their cytoplasm. These gran-
ules are basophilic in appearance in H&E stained sections (Fig.
13-3B). This layer is more prominent in the thick skin than in
the thin skin. (4) The stratum lucidum is a thin layer that is
only found in the thick skin. It contains a few layers of fl attened
cells, which are densely packed together and lie beneath the
stratum corneum. Their nuclei become pycnotic as they begin
to degenerate. (5) The stratum corneum is the most superfi cial
layer, which contains numerous extremely fl attened cells com-
pletely fi lled with keratin. These cells have no nuclei or organ-
elles and are technically dead cells. The cells on the surface are
continuously shed. The dermis is a connective tissue layer deep
to the epidermis. It contains the blood vessels, nerves, and affer-
ent sensory receptors, including Meissner corpuscles and free
nerve endings. The hypodermis is a transition (subcutaneous)
layer below the dermis of the skin, which contains loose con-
nective tissue, adipose tissue, nerves, arteries, and veins (Figs.
13-2 and 13-4A).
Thick Skin Versus Thin Skin
Thick skin is found in only a few places in the body, such as
the palms of the hands and soles of the feet. It has a very thick
epidermis. The stratum corneum is particularly prominent,
being about 10 times thicker than that of thin skin. Thick
skin has numerous eccrine sweat glands, but has no sebaceous
glands or apocrine sweat glands. In contrast, thin skin, which
covers the rest of the body, has a thin epidermis and its stratum
corneum is much thinner than that of thick skin. The epidermis
of thin skin consists of only four layers; the stratum lucidum is
lacking in thin skin. Thin skin contains all three types of glands
(Fig. 13-9A–C).
Accessory Structures of the Skin
Accessory structures of the skin include glands, hair, and nails:
(1) The glands of the skin include sebaceous glands, eccrine
sweat glands, and apocrine sweat glands (Fig. 13-9A–C). The
sebaceous glands secrete into hair follicles to keep the skin soft
and moist and serve as a barrier to protect the skin. The eccrine
sweat glands are important in regulating body temperature; they
are found in both the thin and thick skin. The apocrine sweat
glands are also called sexual scent glands; their function in
humans is not clear. They may be involved in thermoregulation
and are found only in some special regions of thin skin, such
Figure 13-11B Nail Root (Matrix) and Nail Bed
Figure 13-11C Clinical Correlation: Molluscum Contagiosum
Development of the Skin
Figure 13-12A Fetal Skin (5 to 9 Weeks)
Figure 13-12B Fetal Skin (Fifth Month)
Synopsis 13-2 Pathological Terms for the Integumentary System
CUI_Chap13.indd 242 6/2/2010 8:20:48 AM
CHAPTER 13
■
Integumentary System
243
as the axilla, nipple, and perianal and genital areas. (2) Hair is
found in thin skin: the scalp, pubic region, and armpit (axilla)
in adults have more abundant thick hair than other surfaces
of the skin on the body. Hair growth is discontinuous and is
controlled by various hormones. The hair follicles produce and
maintain hair growth. The cycles of hair growth include three
stages (from early to late): the anagen phase (active growth
stage, lasting 2–6 years), the catagen phase (regression phase,
lasting about 3 weeks), and the telogen phase (resting stage,
lasting about 3 months). The hair shaft is shed as the follicle
goes through the growth cycle and a new hair replaces it. In
cross section, a hair follicle looks rather like an onion, with sev-
eral rings or layers. The central part is the hair shaft, which has
a scaly surface called the cuticle. The hair shaft is surrounded
by an inner root sheath (with its own cuticle) and outer root
sheath. The outer root sheath is covered by a connective tis-
sue sheath (Fig. 13-10A). The deep end of the hair follicle is
expanded into the hair bulb, which is composed of a dermal
papilla (hair papilla) and a hair root composed mostly of the
hair matrix. The hair matrix is capable of cell division and gives
rise to the hair shaft (Fig. 13-10B). (3) The nail is a translucent
keratinized hard plate resting on the dorsum of the tip of each
digit. The nail plate stems from the base of the nail (nail matrix)
and grows over the nail bed toward the tip of the fi nger or toe.
The components of the nail include the nail root (nail matrix),
nail plate, the eponychium (nail cuticle), perionychium (nail
wall), and hyponychium (Fig. 13-11A,B).
Development of the Skin
The skin develops from ectoderm and mesoderm. The epithe-
lial cells of the epidermis are ectodermal derivatives, whereas
Langerhans cells, the dermis (connective tissue), and subcutis
(hypodermis) develop from the mesoderm. Melanocytes and
Merkel cells originate from the neural crest. The basal cells of
the epidermis give rise to the accessory structures (hair follicles,
nails, and glands) of the skin (Fig. 13-12A,B).
CUI_Chap13.indd 243 6/2/2010 8:20:49 AM
244
UNIT 3
■
Organ Systems
Hair shaft
Duct of eccrine sweat gland
Eccrine sweat gland
Hair root plexus
Nerve
Vein
Artery
Sebaceous gland
Free nerve ending
Meissner corpuscle
Hair papilla
Hair follicle
Hair root
Apocrine sweat gland
Pacinian corpuscle
Arrector pili muscle
Figure 13-1. Overview of the structure of the skin.
The skin is composed of epithelium, connective tissue, muscles, nerves, blood vessels, and associated structures (glands, hair follicles,
and nails). It can be divided into two basic layers: epidermis and dermis (Fig. 13-2). The epidermis is the superfi cial layer of the skin.
It consists of a stratifi ed squamous epithelium (Fig. 13-2). The dermis is a layer of connective tissue beneath the epidermis. There is a
transition layer between the skin and underlying muscle called the hypodermis (subcutaneous layer), which, strictly speaking, is not
a component of the skin but is closely associated with the skin (Fig. 13-2). This layer contains loose connective tissue, adipose tissue,
nerves, arteries, and veins. The skin contains several sensory structures, which respond to somatosensory stimuli. These include free
nerve endings (pain or temperature), Merkel disks (continuous touch), and Meissner corpuscles (touch). Pacinian corpuscles (vibra-
tion) can be found in the subcutaneous layer (hypodermis). For the function and details of the sensory receptors, see Chapter 7,
“Nervous Tissue,” Figure 7-8A–C. There are several types of glands in the skin, including sebaceous glands, eccrine sweat glands,
and apocrine sweat glands.
Structures of the Skin
I. Layers of the skin
A. Epidermis
1. Stratum corneum
2. Stratum lucidum
3. Stratum granulosum
4. Stratum spinosum
5. Stratum basale
B. Dermis
1. Papillary layer
a. Free nerve endings
b. Meissner corpuscles
2. Reticular layer
C. Hypodermis (subcutaneous layer)
1. Loose connective tissue
2. Adipose tissue
3. Pacinian corpuscles
4. Arteries and veins
5. Nerves
II. Accessory structures
A. Glands
1. Sebaceous glands
2. Eccrine sweat glands
3. Apocrine sweat glands
B. Hair
1. Hair shaft
2. Hair follicles
C. Nail
1. Nail bed
2. Nail matrix
3. Eponychium
4. Hyponychium
D. Sensory receptors
1. Meissner corpuscles
2. Free nerve endings
3. Pacinian corpuscles
4. Merkel cells (Merkel cell neurite complexes or Merkel disks)
Layers of the Skin
CUI_Chap13.indd 244 6/2/2010 8:20:49 AM
