Caballero B. (ed.) Encyclopaedia of Food Science, Food Technology and Nutrition. Ten-Volume Set
Подождите немного. Документ загружается.


disorder. The formal criteria as defined by the Ameri-
can Psychiatric Association in 1994 are listed below:
1.
0002 Refusal to maintain body weight at or above a
minimally normal weight for age and height (e.g.,
weight loss leading to maintenance of body weight
less than 85% of that expected; or failure to make
expected weight gain during period of growth,
leading to body weight less than 85% of
expected).
2.
0003 Intense fear of gaining weight or becoming fat,
even though underweight.
3.
0004 Disturbance in the way in which one’s body
weight or shape is experienced, undue influence
of body weight or shape on self-evaluation, or
denial of the seriousness of the current low body
weight.
4.
0005 In postmenarcheal females, amenorrhea, i.e., the
absence of at least three consecutive menstrual
cycles. (A woman is considered to have amenor-
rhea if her periods occur only following hormone,
e.g., estrogen, administration.)
Subtypes
1.0006 Restricting type: during the current episode of
AN, the person has not regularly engaged in
binge-eating or purging behavior (i.e., self-induced
vomiting or the misuse of laxatives, diuretics, or
enemas).
2.
0007 Binge-eating/purging type: during the current epi-
sode of AN, the person has regularly engaged in
binge-eating or purging behavior (i.e., self-induced
vomiting or the misuse of laxatives, diuretics, or
enemas).
Prevalence
0008 AN is, in about 90% of cases, a disorder of females,
typically between the ages of 12 and 40. Studies of the
age of onset of this disorder reveal bimodal peaks at
14 and 18 years of age; at these ages, the demands of
secondary sexual development and autonomy in the
context of leaving home may be related to the
increased incidence. The current accepted prevalence
rate for AN among western adolescent and young
adult women is approximately 0.5–1.0%. AN is,
relatively speaking, a culture-bound disorder limited
to industrialized societies with western values.
Etiology and Groups at Risk
0009 The etiology of this disorder is unknown; most clin-
icians and researchers endorse a multidimensional
model of AN which acknowledges psychological, bio-
logical, and social risk factors that exist at the level of
the individual, the family, and society. While dieting is
almost ubiquitous behavior among women in western
society, the significant medical and psychiatric mani-
festations of AN and its characteristic psychological
features argue for the definition of AN as a distinct
disorder, and not a simple exaggeration of current
western values; indeed, AN was recognized long
before our cultural preoccupation with being thin.
0010At the level of the individual, women who by career
choice experience pressures both to be thin and to
achieve may be particularly vulnerable. This includes
ballerinas, fashion models, and gymnasts, in whom
thinness and perfectionism are not only demanded
but also equated. Conflicting pressures on women to
nurture and to perform professionally may intensify
concerns about control that are shifted on to weight
regulation as a focus. Further, chronic physical illness,
physical or sexual abuse, or other traumas which
heighten preoccupation with the body as a reflection
of control or self-esteem may increase vulnerability
to AN.
0011At the familial level, there may be a magnification
of social idealization of thinness and denigration of
obesity. Genetic influences through vulnerability to a
variety of psychiatric disorders such as depression,
alcoholism, and eating disorders themselves in other
family members may also play a role. First-degree
relatives of AN subjects also display an elevated
prevalence of eating disorders over controls. Twin
studies indicate an increased concordance rate for
monozygotic (identical) versus dizygotic (nonidenti-
cal) twins.
0012At the societal level, the last 75 years have wit-
nessed shifting models of the ideal female form
toward thinness, in contrast to the increasing bio-
logically ideal weights for women in the context of
good nutrition. However, it must be remembered that
the decription of AN in 1874 long predates our
cultural preoccupation with thinness and a broader
understanding of this disorder must be sought.
Psychopathology
0013The focal behavioral point of AN is the individual’s
relentless pursuit of thinness and the associated con-
viction that her body is too large. This latter belief
may emanate from a variety of sources, from a past
history of obesity (with its attendant social humili-
ation and a sense of failure) to physical or sexual
abuse which has led to body loathing. Alternatively,
AN may reflect a symbolic focus on the body in a
search for personal mastery that in turn reflects a
sense of personal ineffectiveness. It may also allow
retreat from the maturational demands of adoles-
cence, as expressed by the development of secondary
244 ANOREXIA NERVOSA

sexual characteristics. Associated psychopathological
features often include a fear of losing control in many
spheres, self-esteem that is highly contingent on the
opinions of others, an all-or-nothing thinking style
that allows no middle ground between being thin
and being fat, and a pervasive sense of helplessness.
Clinical Features
0014 The initial manifestations of AN are deceptively
benign; the disorder frequently commences with
dieting behavior which is itself common in the west-
ern female population. However, this particular form
of dieting leads to increased criticism of one’s appear-
ance and greater social isolation than typical adoles-
cent dieting behavior; further, weight goals continue
to drift downward as they are approached. Food
aversion becomes more general than specific and,
as emaciation progresses, the individual exhibits a
marked denial of her illness. A typical but not univer-
sal characteristic of AN is a distortion of body image
in which the individual overestimates her body size
substantially, believing herself to be fat even when
thin. This perceptual disturbance is usually accom-
panied by feelings of loathing of one’s appearance.
0015 At the level of behavior, routine dieting evolves into
more elaborate food avoidance and other activities to
counteract the effect of ingested calories. Individuals
restrict their intake dramatically, skip meals, or
secretly dispose of food. Elaborate rituals related to
eating develop, and decreased consumption of food is
paralleled by increasing cognitive preoccupation with
it. This translates into thinking, reading, and dream-
ing about food or working in food-related industries.
Weighing oneself becomes not only a frequent ritual
but also a regulator of subsequent eating, socializa-
tion, and self-esteem. In addition to calorie restric-
tion, individuals may exercise intensively for the
express purpose of weight loss, or use purgative tech-
niques such as diuretics, diet pills, laxatives, or self-
induced vomiting.
0016 Initially, because the consequences of the disorder
are consistent with the individual’s desire to be thin
and in control, there is seldom the motivation to seek
help or to acknowledge the evolving AN as a prob-
lem. Rather, the individual with AN may contact a
nutritionist, physician, or other health professional,
seeking advice on dieting in the absence of obesity or
help in dealing with the secondary medical and
psychiatric effects of starvation.
Physiological Effects
0017 Virtually no body system is spared the effects of
nutritional deprivation in AN. The changes are too
extensive to enumerate here; they reflect not only loss
but also homeostatic compensatory mechanisms to
minimize energy expenditure in the context of de-
creased energy intake. Loss of menstrual function is
the most classically recognized of these sequelae, to
the point that it is a diagnostic criterion thought to
reflect disturbances in gonadotropin function in the
hypothalamus. Other common starvation effects
include lowered body temperature and heart rate,
dry skin and the development of a fine body hair,
abdominal bloating and constipation, and edema.
Psychological Effects
0018Starvation due to AN also produces distinct psycho-
logical effects such as depressed, irritable, or anxious
mood, cognitive preoccupation with food, and de-
creased concentration. Individuals with AN may
appear to suffer from a coexistent depressive illness
and are vulnerable to the long-term development of
such disorders. However, many of the psychological
sequelae of the disorder – which are more troubling to
the affected individual than the dieting itself – are
reversible with adequate nutrition.
Nutritional Status
0019The food restriction of AN may be severe. Individuals
may abstain from all solid foods for days at a time or
subsist on as little as 200–500 calories per day. Typic-
ally, there is an avoidance of perceived high-calorie,
high-fat foods – and foods become imbued with
moral as well as nutritional value. Individuals may
develop frank cachexia, with vigorous dieting and
exercise behaviors persisting at weights as low as
30 kg. Fasting hypoglycemia, abnormal glucose toler-
ance tests, and increased insulin sensitivity are among
the metabolic responses to this form of starvation.
Elevations of cholesterol and carotene may occur
and plasma zinc levels have variably been reported
as low. Low platelet, red blood cell and white blood
cell counts, accompanied by a relative paucity of
precursors in bone marrow, have been described as a
consequence of the disorder.
0020The nutritional status of AN patients may have
implications for the chronicity of the disorder. Brain
neurotransmitters such as serotonin and norepineph-
rine (noradrenaline) are integral in the hypothalamic
regulation of appetitive behavior. Serotonin synthesis
itself is dependent on the dietary availability of its
precursor, the essential amino acid tryptophan. Tryp-
tophan availability may be decreased in AN, and
both neuroendocrine provocation tests and cerebro-
spinal fluid metabolite assays indicate altered sero-
tonin activity in AN. This may be associated with
ANOREXIA NERVOSA 245

disturbances in satiety, thought (with increased obses-
sionality and perfectionism), mood, and sleep found
in AN. Delayed gastric emptying may occur in re-
sponse to the decreased volume of food consumed.
This further contributes to altered senses of satiety; an
augmented sense of fullness may perpetuate food re-
striction.
Diagnosis
0021 The diagnostic criteria of the American Psychiatric
Association listed above reflect the confluence of bio-
logical, behavioral, and psychological factors charac-
teristic of AN. However, clinicians may perceive them
as arbitrary, particularly with regard to the degree of
weight loss required and the presence of amenorrhea
as essential for diagnosis. Epidemiological research
requires dichotomous criteria, while clinical practice
demands the recognition from a dimensional perspec-
tive of disorders in evolution. The diagnosis of AN in
a young woman with weight loss requires consider-
ation of other medical and psychiatric illnesses with
a superficially similar presentation. These include
endocrine disorders, bowel disease, malignancy, de-
pression, schizophrenia, and conversion disorder. All
of these differential diagnoses typically lack the
central psychological preoccupation of AN – the
relentless pursuit of thinness.
Treatment
0022 The goal of treatment of AN includes but is not
limited to nutritional rehabilitation. Clearly, if weight
gain is the only purpose of therapy for an individual
dedicated to the attainment of weight loss, her com-
mitment to the treatment will be poor. At the same
time, however, treating personnel cannot ignore the
nutritional status of the individual while focusing on
psychological issues; when this occurs, it results in
collusion with the denial by the individual of her
illness and obscures the connection between food
deprivation and its sequelae.
0023 The initial phase of treatment is a careful diagnos-
tic assessment, with emphasis on both the evolution
of the disorder and its various sequelae. A family
assessment is often relevant, particularly in younger
patients, both to understand familial influences and
to substitute education for guilt. A target weight
range is established, allowing the minor fluctuations
that are normal (1–2 kg). This range should be able to
be maintained without dieting, should allow the
return of normal menstrual function, and should
reflect consideration of the individual’s longitudinal
weight history. Generally, a target weight range is
above 90% of the average for an individual’s weight
and height or a body mass index (kg m
2
) greater
than 20. Despite a seemingly encyclopedic knowledge
of nutrition, these individuals usually require direct-
ive counseling regarding meal frequency, portion size,
and macronutrient selection. A daily diary of eating
and associated thoughts, feelings, and behaviors may
be helpful. An initial intake of 1500 calories per day is
usually sufficient to promote weight gain without
inducing the gastric dilatation that can complicate
refeeding. A rate gain of 0.5–1.0 kg per week is desir-
able; more rapid weight gain may induce its own
complications, including hypophosphatemia and
edema, as well as mistrust in an individual who is
reluctantly relinquishing weight control. Caloric
intake is usually increased by 200–300 calories per
week toward a goal of 2400–3000 calories per day.
To date, controlled clinical trials indicate no role for
drugs in the promotion of eating or weight gain in
AN; food remains the drug of choice; there is modest
evidence that the antidepressant fluoxetine may assist
weight-recovered AN patients to maintain weight
gain, possibly through an antiobsessional effect.
0024Psychotherapy is usually offered in conjunction
with nutritional rehabilitation, and builds on the
establishment of a therapeutic relationship. Issues
include the recognition of feelings, self-trust, and dis-
connecting one’s sense of self-worth from body
weight. A variety of approaches, from psychodynamic
to cognitive-behavioral, may be employed. Family
therapy may be particularly helpful for the younger
AN patient.
0025Hospitalization is not necessary for the majority of
individuals with AN; rather, it is reserved for cases
where the weight loss has been either precipitously
acute or impinging on basic function, where medical
sequelae such as hypokalemia pose an imminent risk,
where suicidal tendencies accompany the AN, where
AN coexists in a threatening fashion with another
illness such as diabetes mellitus, or where other
forms of treatment have been ineffective.
Prognosis
0026AN is a usually gradual, initially covert, and some-
times chronic disorder. Long-term follow-up studies
indicate that while two-thirds of patients show even-
tual improvement or recovery, less than one-third
recover within 3 years. More disturbing, some long-
term follow-up studies have indicated a mortality rate
of 10–20% as a consequence of AN. In addition,
these women are vulnerable over the long term to
the development of mood disorders, anxiety dis-
orders, and substance abuse, regardless of whether
the AN is active or quiescent. They are also sus-
ceptible to such diverse medical complications as
246 ANOREXIA NERVOSA
osteoporosis with pathological bone fractures and a
form of brain tissue atrophy. Beyond reversal of the
nutritional deprivation and weight loss, there is no
established method of tertiary prevention.
See also: Adolescents; Bulimia Nervosa; Famine,
Starvation, and Fasting; Premenstrual Syndrome:
Nutritional Aspects; Slimming: Slimming Diets;
Metabolic Conseqences of Slimming Diets and Weight
Maintenance
Further Reading
American Psychiatric Association (1994) Diagnostic and
Statistical Manual of Mental Disorders, 4th edn. Wash-
ington, DC: American Psychiatric Association.
American Psychiatric Association (2000) Practice guideline
for the treatment of patients with eating disorders.Amer-
ican Journal of Psychiatry 157 (suppl): 1–39.
Garfinkel P, Lin E, Goering P et al. (1996) Should amenor-
rhea be required for the diagnosis of anorexia nervosa?
Evidence from a Canadian community sample. British
Journal of Psychiatry 168: 500–506.
Garner DM and Garfinkel PE (eds) (1997) Handbook of
Treatment for Eating Disorders, 2nd edn. New York:
Guilford Press.
Goldbloom D (1997) Evaluating the efficacy of pharmaco-
logic agents in the treatment of eating disorders. Essen-
tial Psychopharmacology 2: 71–88.
Goldbloom D and Kennedy S (1995) The medical compli-
cations of anorexia nervosa. In Brownell KD and Fair-
burn CG (eds) Eating Disorders and Obesity: A
Comprehensive Handbook, pp. 266–270. New York:
Guilford Press.
Kaplan AS and Garfinkel PE (eds.) (1993) Medical Issues
and the Eating Disorders: The Interface. New York:
Brunner/Mazel.
Katzman D, Lambe E, Ridgley J, Goldbloom D, Mikulis D
and Zipursky R (1996) Cerebral gray matter and
white matter volume deficits in adolescent females
with anorexia nervosa. Journal of Pediatrics 129:
794–803.
Kaye WH, Gwirtsman H, Obarzanek E and George DT
(1988) Relative importance of calorie intake needed to
gain weight and level of physical activity in anorexia
nervosa. American Journal of Clinical Nutrition 47:
989–994.
Kennedy S and Goldbloom D (1994) Advances in the treat-
ment of anorexia nervosa and bulimia nervosa. CNS
Drugs 1: 201–212.
Szmukler G, Dare C and Treasure J (eds) (1995) Handbook
of Eating Disorders. Chichester: John Wiley.
Anthropometry See Nutritional Assessment: Anthropometry and Clinical Examination
ANTIBIOTIC-RESISTANT BACTERIA
J J Klawe and M Tafil-Klawe, The Ludwik-Rydygier
Medical University, Bydgoszcz, Poland
Copyright 2003, Elsevier Science Ltd. All Rights Reserved.
Bacterial Resistance to Antimicrobial
Agents
0001 The antimicrobial resistance may be intrinsic or ac-
quired. Intrinsic–innate resistance may be considered
a fundamental property of the organism: it was pre-
sent in bacterial strains isolated before the antibiotic
era. Some organisms can produce enzymes that chem-
ically modify a specific drug. Bacteria may also use
the system to transport detrimental compounds out of
a cell, using efflux pumps.
0002 Acquired resistance is not found in species strains,
unless they have been exposed to antimicrobial drugs.
Acquired resistance may occur as a result of spontan-
eous chromosomal mutation or by acquisition of
extrachromosomal elements, such as plasmids and
transposons.
0003Chromosomal mutation can occur during treat-
ment or in the absence of the agent, against which
resistance develops. Extrachromosomal pieces of
DNA, called plasmids (R plasmids), contribute to
bacterial virulence or to antimicrobial resistance.
Genes of resistance to antimicrobial agents may be
transferred from chromosomes to plasmids or from
plasmids to chromosomes, as a result of classic re-
combination. The plasmid and chromosome re-
combine pieces of DNA in areas of genetic
homology. The presence of a rec A gene is needed.
Many plasmids are composed of two parts: the resist-
ance genes, or R genes, which code for the resistance
traits, and the resistance transfer factor, which codes
ANTIBIOTIC-RESISTANT BACTERIA 247

for the transfer of the plasmid to other bacteria by
conjugation.
0004 Transposons, however, can insert into chromo-
somes in areas where no homology exists, inde-
pendent of a rec A gene. Thus, transposons are less
restrictive and play a major role in the transfer of
resistance among many different species.
Biochemical Mechanisms of Bacterial
Resistance
0005 The biological mechanisms of bacterial resistance
may be classified into four groups:
1.
0006 modification of the target site of the antimicrobial
agent – for example, resistance to rifampin caused
by alteration of the targeted RNA polymerase;
2.
0007 enzymatic inactivation of the agent – production
of b -lactamases, enzymes that hydrolyze the b-
lactam ring of the b-lactam antibiotics;
3.
0008 decreased membrane permeability and entry of the
agent – resistance to tetracycline is due to de-
creased accumulation of the antimicrobial agent;
4.
0009 a combination of two or more mechanisms – for
example, resistance of Neisseria gonorrhoeae.
Examples of Emerging Antimicrobial
Resistance
Enterococci
0010 The Enterococci are a group of bacteria that are a
part of the normal intestinal flora. Many enterococci
have plasmid-encoded resistance genes. This group of
bacteria is intrinsically less susceptible to many
common antimicrobials. Enterococci cause nosoco-
mial infections, an old problem that has occurred
ever since the first hospitals were established. Now-
adays, nosocomial infections make up at least half of
all cases of infectious disease treated in the hospitals
and may range from very mild to fatal. Enterococci
are a common cause of nosocomial urinary-tract in-
fections as well as wound and blood infections.
Staphylococcus aureus
0011 Many people, including healthcare personnel, are
carriers of this organism. It is a common cause of
nosocomial pneumonia and surgical infections. Hos-
pital strains are resistant to a variety of antibiotics.
Over the past 50 years, most strains have acquired
resistance to penicillin, due to the acquisition of a
gene encoding the enzyme penicillinase. New strains,
methicillin-resistant Staphylococcus aureus, are
resistant to methicillin and to other b-lactam drugs.
Staphylococcus aureus has also been reported to have
become vancomycin-resistant.
Staphylococcus
Species other than
S. aureus
0012These normal skin flora can colonize the tips of intra-
venous catheters. The resulting biofilms continuously
seed organisms into the bloodstream, thus increasing
the risk of systemic infection.
Streptococcus pneumoniae
0013Some strains, now isolated, are resistant to penicillin.
This acquired resistance is due to the modifications in
the chromosomal genes coding for different penicil-
lin-binding proteins, which decrease their affinities
for the drug. The nucleotide changes are due to the
acquisition of chromosomal DNA from other species
of Streptococcus.
Mycobacterium tuberculosis
0014Treatment of infections of Mycobacterium tubercu-
losis has always been a complicated process, often
requiring a combination of two or three different
drugs taken for 6 months or more. Mycobacterium
tuberculosis is developing resistance to first-line
drugs. Strains that are resistant to isoniazid and
rifampin are called multiple drug-resistant Mycobac-
terium tuberculosis.
Pseudomonas
species
0015These bacteria grow in a large number of moist,
nutrient-poor environments, such as the water in the
humidifier of a mechanical ventilator. Pseudomonas
species are resistant to many antimicrobial drugs.
They are a common cause of hospital-acquired pneu-
monia and infections of the urinary tract and burn
wounds.
Slowing down the Emergence and Spread
of Antimicrobial Resistance
0016More effort from healthcare workers to identify the
causative agent of infectious diseases and to prescribe
suitable antimicrobials is necessary to slow down the
spread of antimicrobial resistance. Also, patients need
to be vigilant, and a great effort must be made to
educate the public about the appropriateness and
limitations of antibiotics.
See also: Mycobacteria; Staphylococcus: Properties
and Occurrence; Detection; Food Poisoning
Further Reading
Advisory Committee on Microbiological Safety of Foods
(UK) (1999) Report on Microbial Antibiotic Resistance
in Relation to Food Safety. London: The Stationery
Office.
248 ANTIBIOTIC-RESISTANT BACTERIA

Howard BJ (1994) Clinical and Pathogenic Microbiology.
London: Mosby.
Jacoby GA and Archer GL (1991) New mechanisms of
bacterial resistance to antimicrobial agents. New Eng-
land Journal of Medicine 324: 601–612.
McDougal LK and Thornsberry C (1986) Role of beta-
lactamase in staphylococcal resistance to penicillinase-
resistant penicillins and cephalosporins. Journal of Clin-
ical Microbiology 23: 832–839.
Nester EW, Anderson DG, Roberts CE, Jr., Pearsall NN and
Nester MT (2001) Microbiology – A Human Perspec-
tive. London: McGraw-Hill Higher Education.
Patterson JE and Zervos MJ (1990) High-level gentamicin
resistance in enterococcus: Microbiology, genetic basis
and epidemiology. Reviews of Infectious Diseases 12:
644–652.
ANTIBIOTICS AND DRUGS
Contents
Uses in Food Production
Residue Determination
Uses in Food Production
K N Woodward, Veterinary Medicines Directorate,
Weybridge, UK
This article is reproduced from Encyclopaedia of Food Science,
Food Technology and Nutrition, Copyright 1993, Academic Press.
Background
0001 Veterinary medicines are used to improve or maintain
the health of animal species regardless of whether
these are intended for food production. They are
designed and manufactured to cover a wide variety
of prophylactic and therapeutic purposes, and they
are administered to household pets, exotic species,
and wild animals in addition to food-producing
animals.
0002 Most countries possess a governmental regulatory
authority charged with assessing veterinary medicines
and granting some form of marketing authorization
before a product may be sold, and the UK’s system is
used here to exemplify this in practice. Veterinary
medicines, like their human counterparts, are asses-
sed against three basic criteria – efficacy, quality, and
safety – although the terms of these criteria differ
from country to country. The efficacy is the ability
of the drug to accomplish the task claimed for it by its
producer. Quality refers to pharmaceutical quality;
the levels of contaminants must meet acceptable cri-
teria, the shelf-life must be as claimed by the manu-
facturer, and the product must be produced to
appropriate standards. Safety means that the product
must not harm the animal patient, the environment,
the users of veterinary medicines, or the consumer of
food of animal origin. This latter aspect is of para-
mount importance when assessing the safety of veter-
inary medicines. When a veterinary drug is given to
an animal, most of the dose will be excreted in urine,
feces, and expired air, but small amounts will remain
in body tissues. These are known as residues, and it is
the responsibility of regulatory authorities to ensure
that these do not pose a threat to the consumer when
veterinary medicines are used in food-producing
animals.
Uses of Veterinary Medicines
0003In general, veterinary medicines are available to treat
most of the types of animal disease state that are
encountered in humans. In practice, diseases such as
cancer are not usually treated in food-producing
species, largely for economic reasons, although they
are frequently dealt with in companion animal
medicine. The majority (but not by any means all)
of the medicines used in food-producing animals are
for the prevention or treatment of diseases caused by
infectious agents. These fall into a number of categor-
ies, and they are described briefly below.
Antibiotic and Antimicrobial Agents
0004Antibiotics are antibacterial agents derived from
living organisms, but the term includes closely related
synthetic analogs. The archetypal compound is peni-
cillin, the structure of which has now formed the basis
for a wide range of naturally occurring and semisyn-
thetic analogs. Other major categories of antibiotics
ANTIBIOTICS AND DRUGS/Uses in Food Production 249

used in veterinary medicine are the tetracyclines, the
aminoglycosides, the macrolides, and the polymixins.
Sulfonamides constitute the major class of antimicro-
bial agent, drugs that are unrelated to naturally
occurring compounds. A number of sulfonamides
have been prepared for fast, medium, or long-acting
functions. Sulfadimidine is one of the most widely
used sulfonamide drugs in veterinary medicines, par-
ticularly in pig production, where it is employed to
combat respiratory disease.
Ectoparasiticides
0005 Cattle and sheep are often subject to attack by ecto-
parasites. For example, in the UK and other parts of
Europe (and indeed elsewhere) cattle are susceptible
to attack by the warble fly (Hypoderma spp.), which,
in addition to causing animal suffering, results in
considerable economic loss. Sheep scab is another
disease that poses serious animal welfare and eco-
nomic problems, and in several countries, including
the USA and the UK, it is a notifiable disease. Both
diseases are treated and prevented by the application
of organophosphorus compounds. For warble fly,
treatment is usually in the form of a relatively viscous
formulation that is spread on to the back of the
animal (a pour-on formulation); in the case of sheep
scab, dipping and showering are the most therapeut-
ically and economically effective methods currently
available.
0006 Fish too are susceptible to external parasites, and
as fish farming (aquaculture) becomes more import-
ant, so the effects of disease become more significant.
Salmon farming is a fast-growing industry in many
parts of the world, particularly in North America,
Chile, Norway, and Scotland. Salmon are vulnerable
to infestation by the sea louse, an arthropod that
attacks the external surface of the fish and in severe
cases causes death.
Anthelmintics
0007 ‘Anthelmintics’ is a term almost universally abused to
describe agents used to treat internal parasite infest-
ations and not merely those caused by helminth
worms. Many of the diseases caused by internal para-
sites can be extremely distressing to affected animals,
and all can result in substantial economic losses. A
number of drugs have been developed to combat
these diseases, including the benzimidazoles, levami-
sole and invermectin.
0008 The first benzimidazole to achieve widespread use
in veterinary medicine was thiabendazole, but newer
compounds include albendazole, oxfendazole, fen-
bendazole, and mebendazole. Levamisole is extreme-
ly efficacious in the treatment of gastrointestinal
nematodes in cattle, sheep, and pigs. Ivermectin is a
mixture of two closely related compounds derived
from abamectin, a metabolite of Streptomyces aver-
mitilis, and it has found wide use as an antiparasitic
agent in veterinary medicine (and in some areas of
human medicine).
Antifungal Agents
0009In veterinary medicine, several drugs have found uses
as antifungal agents for application to the external
surfaces of the body. These include ketoconazole,
thiabendazole, aliphatic acids, and benzoic acid.
Nystatin and griseofulvin are extensively used as
systemic treatments for fungal infections in both
food-producing and other species.
Steroid Hormones
0010It has long been known that testosterone exerts ana-
bolic effects in both humans and animals, and testos-
terone and chemically related steroid hormones
have been widely used for this purpose in beef
production. However, the EC has prohibited the
growth-promoting uses of steroid hormones in
animal production, although certain so-called zoo-
technical (e.g., synchronization of estrous for mating)
and therapeutic (e.g., treatment of recurrent abor-
tion) uses are still permitted using naturally occurring
compounds or closely related derivatives. In other
countries, notably in the North and South Americas,
the growth-promoting uses of steroid hormones are
legally permitted.
Regulatory Control of Veterinary
Medicines
0011Regulatory control of the uses of veterinary medicines
is almost universal, and, as described earlier, drugs
must meet exacting standards of efficacy, quality, and
safety. In the UK, for example, human and veterinary
medicines are controlled by the Medicines Act 1968
and by integrated EC legislation. Product licences and
other forms of marketing authorization are granted
by a licensing authority established under the act. The
Licensing Authority is defined in the act as the Health
and Agriculture Ministers acting together, and in
practice, responsibility is given over to civil servants
working in the Department of Health for human
medicines, and in the Veterinary Medicines Director-
ate (VMD) of the Ministry of Agriculture, Fisheries
and Food (MAFF) for veterinary medicines. Applica-
tions for product licences are submitted to the VMD
by companies together with the quality, efficacy, and
safety data. Staff of the VMD then vigorously assess
these data and submit them with their appraisals to
250 ANTIBIOTICS AND DRUGS/Uses in Food Production

the independent Veterinary Products Committee ap-
pointed under the Medicines Act. This committee
may then recommend licensing, require further infor-
mation, or refuse the application. When a product is
not recommended for licensing, companies have
recourse to an appeals procedure, whereby they can
submit their arguments. (See Legislation: Contamin-
ants and Adulterants.)
0012 Essentially similar systems exist in other countries,
including other member states of the EC. For this
latter group, national laws are amended from time
to time to incorporate EC legislation. Three European
directives are worthy of note for the impact that these
have had on national legislation within the EEC.
0013 The two Veterinary Medicines Directives (81/
851/EEC and 81/852/EEC) provide a legislative
framework for the European ‘licensing’ of conven-
tional veterinary medicines. They establish an expert
committee, the Committee for Veterinary Medicines
Products, and offer a system of control, including a
multistate authorization procedure within the EC.
Moreover, they provide comprehensive guidelines on
safety, quality and efficacy. The so-called Feed Addi-
tives Directive (70/524/EEC) covers both medicinal
and nonmedicinal ingredients intended to be added to
the animal feeds. Although conventional veterinary
medicines and medicinal feed additives are therefore
dealt with separately at community level, in the
UK, they are subject to the same treatment under
the Medicines Act, once they have been accepted
by the EC.
0014 On a worldwide basis, the marketing authorization
of veterinary medicines and the steps preceding this
can be summarized briefly as follows: development of
a drug and its formulations; testing to fulfill the
requirements of safety, quality and efficacy; submis-
sion of an application for marketing authorization
with the data from safety, quality, and efficacy tests
to the appropriate national authorities; appraisal, as-
sessment, and consideration by those authorities;
granting or refusal (or requirement for further stud-
ies) of marketing authorization.
Safety Data Requirements
0015 Safety data with respect to consumer safety can be
divided into two main categories: toxicity data and
residues data. In recent years, there has been an in-
creasing demand for data on microbiological safety
with respect to possible effects on the gastrointestinal
flora of consumers.
Toxicology Studies
0016 Toxicology data usually take the form of the results
from a package of studies using laboratory species
and in-vitro tests. Pharmacokinetic and pharmaco-
dynamic data are also used where relevant in the
interpretation of the results of these endeavors. The
precise requirements for toxicology testing differ
from country to country, but in general terms, they
are exemplified by those of the EC, which include the
following:
.
0017single-dose (acute) toxicity;
.
0018repeated-dose toxicity;
.
0019reproductive toxicity: effects on reproduction;
effects on the embryo or fetus and teratogenicity
(birth defects);
.
0020mutagenicity studies;
.
0021carcinogenicity (induction of tumors) studies;
.
0022pharmacodynamics.
.
0023pharmacokinetics;
.
0024observations in humans.
0025There are three basic aims in conducting toxicology
studies: to identify a no-observed effect level (NOEL),
to calculate an acceptable daily intake (ADI), and to
determine a maximum residues limit (MRL).
0026The NOEL is the lowest dose level, usually quoted
in milligrams per kilogram bodyweight, below which
an effect or range of effects do not occur in the species
being investigated (usually mice or rats). It is usually
necessary to eliminate those effects thought to be
irrelevant – usually because they are known to occur
only in rodents or because they represent a phenom-
enon induced by excessive doses – and then select the
study thought to be of most relevance, although in
practice, the lowest NOEL from the battery of tests is
often used.
0027The ADI is calculated by dividing the NOEL by an
arbitrary safety factor. This is usually 100 for minor
toxic effects, but factors of up to 2000 may be used
with severe effects or when the battery of tests is
considered to be deficient in some relatively minor
aspect; if deficient in some major area, e.g., if a car-
cinogenicity study has not been conducted, an ADI
may not be set. The ADI is often expressed in terms of
human weight by use of the additional factor of
65 kg, this being widely accepted as representing
human adult weight. Hence, the ADI can be
expressed (in milligrams per day) as follows:
ADI ¼ðNOEL 65Þ= safety factor:
The MRL is the maximum permitted level of the drug
residue, which regulatory authorities perceive as
being acceptable in food of animal origin on the
basis of the results of the safety studies described
earlier. As such, it is often difficult to describe in
purely arithmetical terms, for, although it is based
primarily on the ADI, it must take into account
other factors, not least of which is the intake of the
ANTIBIOTICS AND DRUGS/Uses in Food Production 251
food commodity in question. Every consumer has a
varied intake of most of the products of food of
animal origin, such as muscle, fat, kidney, and liver;
some, for example, eat more liver or kidney than
others. To try to cover the majority of possibilities,
the Food and Agriculture Organization, World
Health Organization (FAO/WHO) Joint Expert
Committee on Food Additives (JECFA) has recom-
mended standard daily intake values of 300 g of
muscle, 100 g of liver, 50 g of fat, 50 g of kidney,
100 g of egg, and 1.51 of milk to be used in the
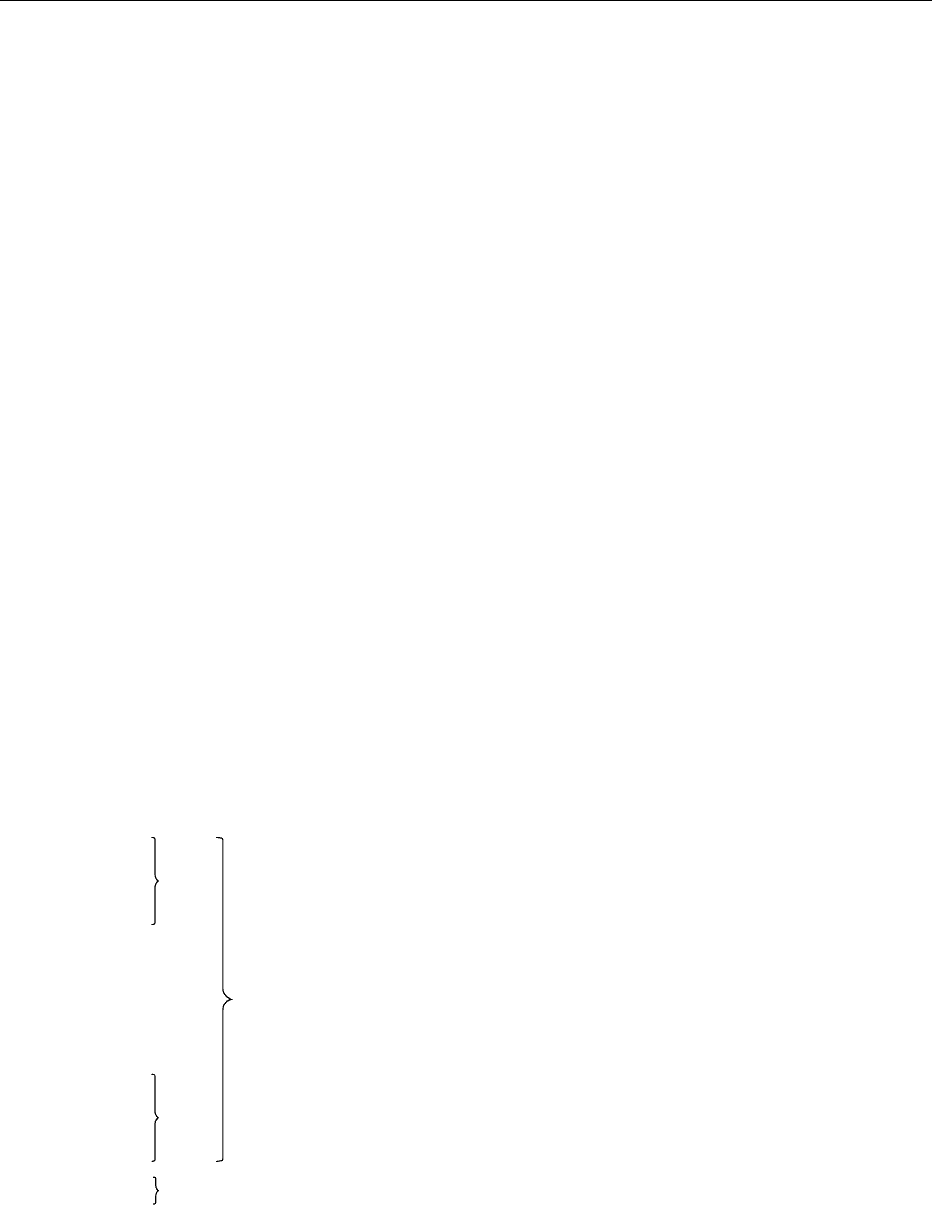
elaboration of MRLs. The types of food-producing
animals are shown in Figure 1. In general terms, the
ADI is ‘spread’ across the different types of food
commodity, bearing in mind their relative standard
intakes, so that MRLs, which will not result in the
ADI being exceeded, can be elaborated.
0028 When considering values for MRLs, a major factor
that must be taken into account is the chemical nature
of the residues and their resultant biological activity.
This is an extremely complex area and one that is not
without controversy. Most chemicals, including vet-
erinary medicines, when given to animals are con-
verted to a range of metabolites, usually but not
exclusively by the liver. Consequently, the residues
present in tissue may be the parent compound or a
mixture of metabolites or both. Moreover, either the
parent drug or its metabolites may be highly reactive
and may therefore combine with cellular constituents
to give rise to so-called bound residues. In these cir-
cumstances, it is desirable and sometimes essential to
know to what extent these may be released to yield
potentially harmful substances following consump-
tion of products of animal origin. The most likely
place for such a release to occur is in the gastrointest-
inal tract of the consumer, and a number of animal as
well as several chemical models have been developed
in an attempt to provide information on this area of
hazard assessment. One of these makes use of a tech-
nique known as relay toxicology, although in this
context, relay pharmacology might be more appro-
priate. The radiolabeled drug is administered to the
food-producing animal, which is later slaughtered,
and its tissues, known to contain bound residues,
are fed to laboratory animals such as rats. Detection
of radioactivity in the plasma (for example) of these
animals would indicate that the bound residues are
bioavailable and, as a result of digestive processes,
have been released for subsequent absorption. Chem-
ical methods using solvent extraction and acid–base
treatments investigate the ease with which bound
residues can be released. These methods then deter-
mine whether or not the contribution from bound
residues needs to be taken into account in the MRL
setting procedure.
0029As indicated earlier, microbiological safety testing
has been proposed for use in the hazard assessment
process and indeed has been incorporated into
some testing guidelines, including those of the EC.
The requirement for such testing is based on the
premise that residues of some antibiotic and antimi-
crobial compounds may have the potential to affect
adversely the gastrointestinal flora of the consumer,
either by favoring the growth of resistant bacteria or
by allowing the growth of organisms not normally
found in any numbers in the gastrointestinal tract, by
reducing the numbers of other organisms that nor-
mally suppress them. This is an extremely controver-
sial area of safety assessments for two main reasons.
First, despite the use of antibiotic and antimicrobial
drugs in veterinary medicine for many years, there is
no evidence to suggest that harmful effects have
arisen in the human population as a result of bio-
logical changes in the gut flora. Second, the tests
proposed to identify these effects have not been valid-
ated, so that even if the effects do exist, it is not
known whether or not the proposed tests would actu-
ally detect them.
0030There are three tests currently available. Human
volunteer studies involve the administration of the
drug and subsequent examination of feces and
the oral cavity for changes in floral composition. The
major alternative involves the use of germ-free
rodents in which human gut flora have been seeded
into the gastrointestinal tract. These are then given
the drug under investigation and changes in the gut
Pigs
Rabbits
Horses
Fish
Bees Honey
Poultry
Game birds
Pigeons
Eggs
Cattle
Sheep
Goats
Milk
Meat, fat, kidney, liver
fig0001 Figure 1 Major food-producing species and their products im-
portant in considering maximum residues limits (MRLs) and resi-
dues studies. Reproduced from Antibiotics and Drugs: Uses in
Food Production, Encyclopaedia of Food Science, Food Technology
and Nutrition, Macrae R, Robinson RK and Sadler MJ (eds),
1993, Academic Press.
252 ANTIBIOTICS AND DRUGS/Uses in Food Production

flora monitored. The third approach makes use of
in-vitro studies of the susceptibilities of various
types of bacteria to antibacterial drugs, before and
after exposure to low, sublethal levels of the drug. The
numerical results in terms of dose can then be
employed in the calculation of the ADI.
Residue Studies
0031 Having determined an MRL value (or values) for a
drug, it is then essential to ensure that residues in the
tissues or other products of food-producing animals
do not exceed these. This is achieved by determining
the withdrawal (or withholding) period for the drug
in question. Small groups of animals are treated with
the medicine, usually at the maximum dose recom-
mended for its use in practice. The animals are then
slaughtered in a serial manner after various intervals
to determine when residue levels fall below the MRL.
This time period for depletion of residues to below
the MRL is then usually chosen as the withdrawal
period; animals must be retained unmedicated during
this time as the minimum interval between drug ad-
ministration and slaughter. Where appropriate, milk,
eggs, and honey must be discarded until this min-
imum time has elapsed.
Enforcement
0032 There is little point in progressing through the various
procedures detailed above if the withdrawal period is
ignored, and unacceptable levels of residues result.
There is often pressure to ensure that animals are
sent to slaughter at particular times, and this can
lead to abuse.
0033 To ensure that withdrawal periods are observed,
most countries operate some form of residues surveil-
lance scheme. In the UK, for example, over 40 000
samples are taken annually from slaughterhouses,
and these are tested for residues of various veterinary
drugs in compliance with the requirements of the EC
Residues Directive (86/469/EEC). Other EC member
states carry out similar surveillance in order to
comply with the requirements of this directive. The
system allows enforcement officers to trace carcases
back to farms to determine why the problem arose
and, where necessary, to take legal proceedings
against offenders.
The Codex Alimentarius Commission
0034 The Codex Alimenatarius Commission is a joint
WHO and FAO body, and one of its objectives is
to ensure that food of plant and animal origin
worldwide is safe for human consumption. It has
recently commenced work on establishing MRLs for
veterinary drugs, having been involved for many
years in setting these for pesticide residues. The
Codex is advised on toxicological and residues issues
by JECFA, the published scientific reports of which
summarize the major conclusions and the proposed
MRLs.
0035Given the international standing of the Codex
system and of the JECFA, it seems likely that the
MRL values that it promulgates will find their way
eventually into various national regulations. In par-
ticular, it offers a basis for scientific assessment not
currently available in some poorer and less developed
nations.
Concluding Considerations
0036In most countries of the world, veterinary medicines
are assessed for their ability to induce toxic effects,
and these effects and the doses that produce them are
taken into account when calculating the ADI, which
is in turn used to determine an MRL value or values.
Residues studies are then used to determine when
levels of the drug and its metabolites are depleted to
below the MRL in food-producing animals. Residues
surveillance is essential to ensure that withdrawal
periods are observed and, moreover, to ensure that
the consumer is not exposed to unacceptable residue
levels.
See also: Hormones: Steroid Hormones; Legislation:
Codex; Parasites: Occurrence and Detection
Further Reading
Anonymous (1987) Anabolic, Anthelmintic and Antimicro-
bial Agents. The 22nd Report of the Steering Group on
Food Surveillance. The Working Party on Veterinary
Residues in Animal Products. London: Her Majesty’s
Stationery Office.
Booth NH and McDonald LE (eds) (1988) Veterinary
Pharmacology and Therapeutics, 6th edn. Iowa City,
IA: Iowa State University Press.
Brander GC, Pugh DM, Bywater RJ and Jenkins WL (1991)
Veterinary Applied Pharmacology and Therapeutics, 5th
edn. London: Ballie
`
re Tindall.
Commission of the European Communities (1989) The
Rules Governing Medicinal Products in the European
Community, vol. V. Luxembourg: Office for Official
Publications of the European Communities.
European Federation of Animal Health (Seminar) (1989)
Rationale view of antimicrobial residues. An assessment
of human safety. Advances in Veterinary Medicine, sup-
plement to the Journal of Veterinary Medicine No.42.
International Programme on Chemical Safety (1987) Prin-
ciples for the Safety Assessment of Food Additives
and Contaminants in Food. Environmental Health
Criteria 70. Geneva: World Health Organization.
ANTIBIOTICS AND DRUGS/Uses in Food Production 253
