Tadrous P.J. Diagnostic criteria handbook in histopathology: a surgical pathology vade mecum
Подождите немного. Документ загружается.

color-plates December 8, 2007 16:39 Char Count= 0
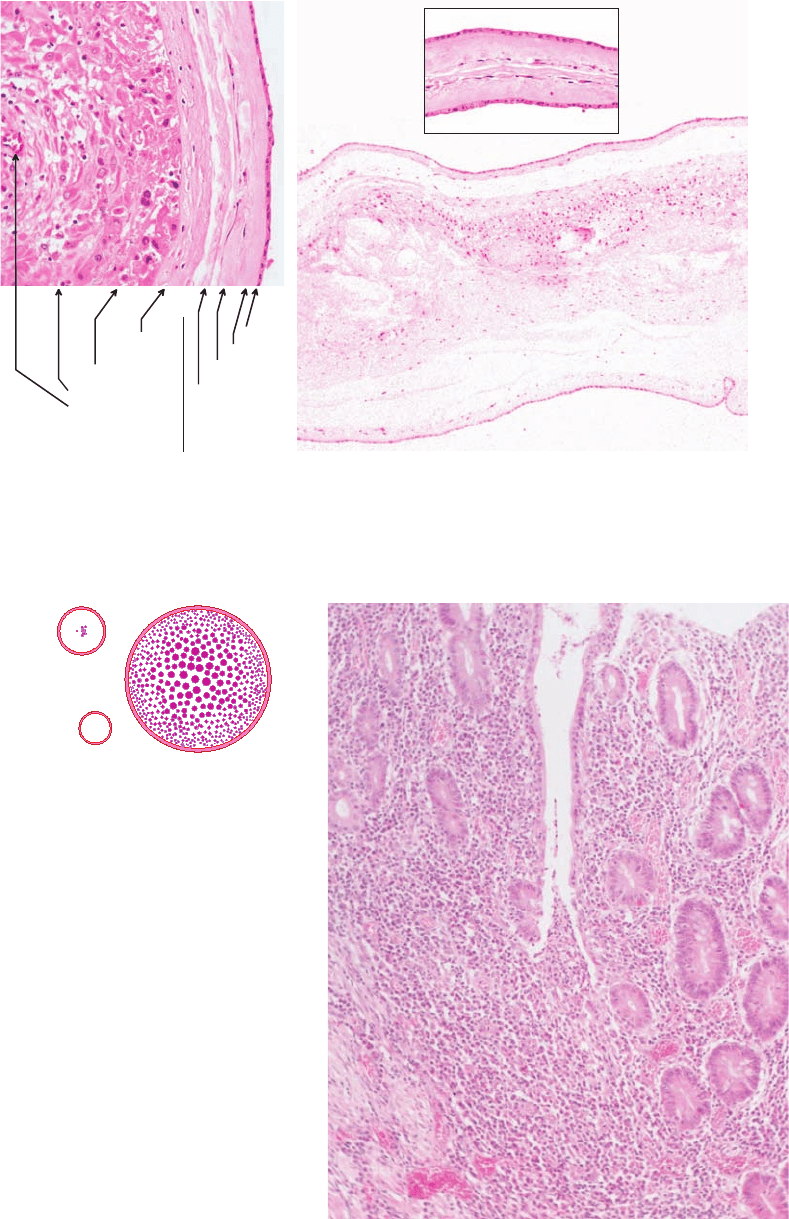
Layers of the Normal Chorion & Amnion Intertwin Membranes
Cellular
& Reticular
Trophoblastic
Decidual (incl.
blood vessels)
AMNION
(avascular)
Epithelial
Compact
Fibroblastic
Spongy
CHORION
DIAMNIOTIC MONOCHORIONIC
DIAMNIOTIC DICHORIONIC
Inset is x3
cf. main picture
(chorion is present between the amniotic layers)
FIGURE 5.3
FIGURE 8.1
FIGURE 11.3
7

color-plates December 8, 2007 16:39 Char Count= 0
fovea
lamina cribrosa
sclerae
RETINA
CORNEA
1
2
3
4
5
choroid
(vascular & pigmented)
KEY (Retina)
1. Bruch's (basement) membrane
2. Retinal pigment epithelium (RPE)
3. Layer of rods & cones (outer segment)
4. Layer of rods & cones (inner segment)
5. Outer nuclear layer
6. Outer plexiform layer
7. Inner nuclear layer
8. Inner plexiform layer
9. Ganglion cell layer (scant to many nuclei thick)
10. (Optic) Nerve fibre layer (with retinal vessels)
OLM = Outer limiting membrane
endothelium
epithelium (non-keratinised)
basement membrane
(PAS
+
ve)
Bowman's layer / membrane
(PAS
-
ve)
Descemet's (basement) membrane
stroma (avascular)
ora serrata
SCLERA
6
8
7
9
10
3
4
5
retinal vessels
2
OLM
1
FIGURE 14.1
Sertoli cells
Spermatozoa
Spermatids
1° Spermatocytes
Pale & Dark Type A Spermatogonia Type B Spermatogonia
FIGURE 16.1
a
b
cde
FIGURE 17.1
intestine
lateral
ala
excretory
column
canaliculus
BAYLISASCARIS
TOXOCARA
nucleus
FIGURE 23.1
8

JWBK208-01 December 8, 2007 15:57 Char Count= 0
Exam Advice 1
1. Advice for Exam Candidates
Introduction
There is no ‘secret’ or ‘technique’ that will ensure success in the MRCPath exam and by far the best way to
prepare is to do lots and lots and lots of routine diagnostic and autopsy work in as many busy general and
specialist hospitals as you can over the years of your training. You should attend one of the major diagnostic
histopathology courses and one of the major cytopathology courses close to your exam because they help
fill gaps in your knowledge and give you confidence. Going over slide collections is tempting but is often
not very helpful because slide collections are made up of fascinomas whereas the exam is made up of
routine surgicals.
The examiner is looking for evidence that you will be a safe and effective pathologist when
left to your own devices. Safe means that you know your limitations (know when to refer or defer) and
have a mature approach to diagnosis i.e. you make diagnoses based on a combination of multiple factors:
clinical, constellations of morphological criteria, ancillary results, etc. with due consideration of appropriate
differentials and with regard to the consequences of your decisions. Diagnosis by picture-matching or
putting undue emphasis on a single feature is not appropriate for consultant-standard candidates. Effective
means you have sufficient knowledge and experience to be able to make a confident diagnosis in the
majority of the cases – anyone can muddle through by sitting on the fence or referring every case – but this
can cause harm by means of delayed diagnosis (= delay in getting appropriate treatment) or by causing
the patient to undergo unnecessary repeat diagnostic clinical procedures.
As a trainee, try to avoid the comfort of staying in one institution for longer than 18 months.
Moving around gives you a broader vision, you learn new ‘tricks’ from new colleagues and new ways
of approaching the same conditions. This builds breadth of experience rather than depth – and both are
important.
It is vitally important to ensure that you keep good timing – many have failed because they
haven’t given themselves time to answer all the questions or study all the cases. Take every opportunity
you get to do mock exams and ensure that you are strict with yourself over timing. Take a watch or clock
with you to the exam (but not one with an audible alarm). You are also well advised to check in advance
the quality and build of the microscope available in the centre and consider taking your own instrument to
the exam: making diagnoses in the pressure of the exam is stressful enough without having to fiddle with
an unfamiliar objective turret, field of view, focus mechanism and maladjusted illumination system.
In diagnostic practice, knowledge (of what diseases exist and what criteria define them) is more
important than a visual memory for pictures. The histopathology of any one disease entity is defined by
the presence of a set of morphological (± clinical) criteria. Because any one or more of these criteria may
dominate in a given instance of that disease, the overall histological picture may look dramatically different
to a picture of the same disease occurring in another patient – the criteria for making that diagnosis, however,
are the same. This is why pattern matching for diagnosis is potentially dangerous (pattern matching is only
useful to recognise the presence or absence of any individual morphological criterion) and that is why this
book concentrates on defining diagnostic criteria rather than illustrations of ‘typical lesions’. Knowledge
is built up over the years by getting into a habit of reading, teaching and doing. Knowledge is just as
important for the practical exam as it is for the written exam – and even more so for real life diagnostic
practice. A suggested reading list is given in the ‘General Bibliography’ of this book (see page xxiv).
There follows some generaladviceonapproaching the practical aspects ofthe MRCPathexam. The
examis in the process of changing as postgraduate medical education in the UK also undergoes restructuring
towards ‘run through’ training with a defined curriculum and competency-based assessments. The moves
are towards standardisation, centralisation and modularisation. In particular the autopsy component has
been separated off from the main exam as autopsy training becomes more specialised. Gynae cytology may
eventually also become a separate module. For details of the latest exam structures and what’s expected of
candidates see the documents posted on the RCPath website, www.rcpath.org.uk.
At the end of this chapter I suggest a small (and incomplete) list of conditions you should always
think about before arriving at a diagnosis (the ‘Never Forget Group’) and finally, for the desperate, I provide
a list of mnemonics found throughout this book.
Diagnostic Criteria Handbook in Histopathology: A Surgical Pathology Vade Mecum. Paul J. Tadrous
Copyright
C
2007 by John Wiley & Sons, Ltd. ISBN: 978-0-470-51903-5

JWBK208-01 December 8, 2007 15:57 Char Count= 0
Exam Advice 2
The Diagnostic Slides
Short Surgical Pathology Cases (usu. 20 cases)
r
You get 9 minutes to write a structured report for each one:
◦
1
description,
◦
2
diagnosis,
◦
3
clinical
comment. You don’t need all three for straightforward cases (obviously,
◦
2
is essential).
r
Avoid lists of stains – if you feel the need for further stains or procedures always state why each stain
is needed and what you would expect to see (i.e. how it will help you decide amongst the differentials).
In the set of 20 surgical short cases it would be unusual to put in a case that needs lots of extra stains /
procedures to arrive at a preferred diagnosis (this is the point of the long cases).
r
Avoid lists of differentials and always attempt to give a preferred diagnosis. If your confidence level
in your preferred diagnosis is low, say so, and discuss the most likely alternatives with reasons for
and against. It is highly frowned upon for a differential to span the benign – malignant divide. This is
clinically a useless position for a pathologist to maintain. If you are really stuck in this decision it may
be a case you will have to ‘refer for second opinion’ but you can’t do this too often (see below).
r
Use formal language in your reports without anecdotes or use of ‘note style’ writing. For example: ‘On
this section alone my preferred diagnosis is X rather than Y. However, my degree of confidence is not
high and, given the importance of making the distinction between X and Y in this case, I would like
to ...’ [continue, for example, with one of the following]:
‘...examine further levels to look for [state the features that will help]’
‘...perform a Congo red for amyloid to substantiate the H&E findings’
‘...refer the case for a second opinion’
‘...further sub-classify the lesion by making reference to a major dermatopathology textbook
[or, better still, state a precise reference]’.
r
An exam pass-standard candidate should be able to give a preferred or definite diagnosis for most of
the 20 cases (at least 17 of the 20 as a general rule of thumb).
Long Surgical Pathology Cases
r
These will be something like a renal, bone marrow trephine or liver biopsy with special stains or a
tumour with special stains. Special stains may include tinctorial, immuno & EM ± macro photo.
r
Compose a formal and structured report as you would normally do in routine practice. Give your
preferred diagnosis ± a limited differential with reasons (as described for the short cases above).
r
Show the examiner that you are able to interpret the significance of the special stains: positivity,
negativity, strength / grade and distribution / pattern of staining, artefactual changes, etc.
r
You may get an unexpected result in the specials – the examiners are trying to see how you cope, e.g.
a probable follicular lymphoma with a negative CD10 stain.
r
You may get an impossibly difficult case – this is deliberate and you are not expected to give the
diagnosis but the examiner wants to see how you handle something you can’t do. This will be where
your experience and judgement – or lack of it – will really show.
Cytology
r
Gynae short cases: at the end of your report you should give an appropriate recommendation for
management based on the patient’s age and previous smear history. State if inadequate and why.
r
Non-gynae short cases should result in clear and unambiguous results. State if inadequate and why.
r
For the long cases bear in mind problems of interpreting special stains and ensure you have the necessary
controls.
r
Make sure you are aware of (and familiar with) the common pitfalls: atrophic smear vs. severe
dyskaryosis, decoy cells in urine vs. malignant cells, etc., etc., etc.
The Viva Voce and Macroscopic Pathology exam
r
Display effective communication skills: address the questioner, look them in the eye, don’t mumble,
use clear expressive and articulate language, don’t waffle and don’t fight.
r
If you don’t know the answer to a question be honest and up-front. Say you don’t know about that
particular thing but what you do know is... [something closely related to the question] – and let the
examiner stop you if they want to. Don’t use ‘politician speak’ or weasel words to try and ‘fool’ the
examiner: the examiner will not be fooled – and neither will they be impressed.
r
The viva is part of an OSPE with a strict marking scheme so you cannot use it to admit ‘mistakes’ you
made in the practical (.
.
. there’s no point discussing the cases with your fellow candidates).

JWBK208-01 December 8, 2007 15:57 Char Count= 0
Exam Advice 3
The Autopsy
General
r
This will be done on a separate day to the rest of the exam and possibly at a different centre.
r
You will be allowed up to 3 hours to conduct the autopsy (excluding presentation and write-up).
r
Review the notes and consent form and write a summary: age, date of death, clinical history.
r
Conduct a risk assessment (use the local form / questionnaire where available).
r
Ask the examiner about arrangements for contacting clinicians / students to attend the presentation.
r
Discuss any special requirements anticipated (e.g. X-rays for neonates, microbiology, FS facilities).
r
Do not criticise the instruments – although ask for others if required.
r
On external examination: check identity, check for LNp and – ! – remember to check the back of the
body.
r
Health and safety is very important, slackness here can easily fail you:
maintain an orderly instrument layout and demonstrate safe handling of them
be clean and tidy at all times
do not leave pools of blood in the body cavities – rinse and sponge out.
Evisceration
r
Consider taking ascitic fluid for culture if there is intra-abdominal sepsis.
r
Remember to check for pneumothorax.
r
The MTO may remove the cranium but you could be expected to remove the brain.
r
Remove the diaphragm intact by cutting it flush with the thoracic wall.
r
After removing the organs, clean the inside and outside of the body and check the inside of the rib cage
for fractures (haemorrhage) and check for scoliosis / crush fractures of the spine.
r
Ask if it is routine to remove the femur. [NB: This is not expected in the current MRCPath exam.]
r
Ask if you are expected to fix the brain (the preferred option) or dissect it fresh.
Organ Systems
r
Show the examiner you have a good-quality dissecting technique: open both iliac veins down to the
femorals at the level of the great saphenous vein; keep the pericardium (and display it); assess the skull
thickness for Paget’s disease; don’t spill gastric contents or bile (open these structures into containers);
don’t leave part of the right atrium behind (you will have trouble demonstrating the SA node when
asked). Also, it is generally not good if the examiner opens the 1
st
part of the duodenum for you to reveal
the ulcers you missed! Remember the carotid and vertebral arteries (at least inspect the intracranial
portions of the vertebrals [the current MRCPath doesn’t require a full dissection]).
r
Show that you can think of things relevant to the clinical history or PM findings: remember the lymph
nodes, bone marrow and tonsils in patients with lymphoproliferative disease; be prepared to comment on
the renal arteries in someone with HT; take CSF by syringe from the 3
rd
/4
th
ventricle for microbiology
if there is reason to suspect meningitis or brain abscess.
r
Show you have a good knowledge base: know your normal weights and measures, be prepared to
discuss specialist dissection techniques and their indications (inflation of the lungs, vertebral arteries,
conducting system, middle ear, etc.), issues of health and safety, consent and the Law (e.g. the Human
Tissue Act, the Coroner’s rules and when to refer a case to the Coroner), macro staining methods (for
MI, amyloid, iron, etc.), toxicology, the future of autopsy (minimally invasive, radiologically assisted,
sub-specialised, etc.), mortuary design and other topical issues.
Presentation and Writing a Report
r
Periodically clean, dry and arrange the organs and instruments during the presentation.
r
Start with the history then, in order: cause of death in ONS format →predisposing pathology → other
major findings → trivia. Avoid lists of negatives. Demonstrate good interpretative skills.
r
Be slick (e.g. you should be able to demonstrate the coronary arteries swiftly) and point specifically to
pathology with a probe. Your manual dexterity (throughout the autopsy) is part of the assessment.
r
Demonstrate good communication skills and show a good rapport with the clinicians.
r
After presentation write the report and block index (ask the examiner for details – some may allow you
to dictate). Remember to put the cause of death in the ONS format (for those over 28 days old) and do
not use modes of dying as a substitute for a cause of death (see Chapter 25: Autopsy).

JWBK208-01 December 8, 2007 15:57 Char Count= 0
Exam Advice 4
The Frozen Sections Exam
r
Give a clear and unambiguous answer that will help the management – not a detailed report / diagnosis.
r
If you are really stuck, you may ‘defer to paraffin’ but do this once too often and you will fail. Although
in real life there is the possibility of requesting further levels on a FS or more tissue from the surgeon,
the cases chosen for the exam are unlikely to require this.
r
Remember FS artefacts (e.g. the lack of lacunar cells in NSHL or Orphan Annie nuclei in PTC) and
be prepared to mention the possibility and utility of imprint cytology.
The ‘Never forget’ Group
Don’t make a diagnosis until you’ve considered the following – the mnemonic, ‘CAMMeLS’, will help
you to remember:
r
Chemotherapy / radiotherapy / inflammatory atypia
r
Amyloid
r
Melanoma (1
◦
/2
◦
)
r
Metastatic / 2
◦
carcinomas (e.g. RCC metastatic to mucosae, skin or bone)
r
Leukaemia: CLL, chloroma / ‘granulocytic sarcoma’ (AML / CGL)
r
Sarcoid / Crohn’s (incl. extra-intestinal Crohn’s) / reaction to malignancy: when faced with true
epithelioid granulomas
Mnemonics
Mnemonic Index
Condition/entity Mnemonic Chapter
‘Never forget’ group of diseases CAMMeLS Chapter 1: Advice for Exam
Candidates
Atheroma (complications of) CUT Chapter 6: Vascular
Abbreviated list of T-cell / NK lymphomas: THE PSALM Chapter 10: Lymphoreticular
Morphological types of myoepithelial cells: SPEC Chapter 11: Alimentary Tract
Neuroendocrine cell tumours: EDGE Chapter 11: Alimentary Tract
Causes of malabsorption: FIDLES BV Chapter 11: Alimentary Tract
Drug effects in the small bowel VACU Chapter 11: Alimentary Tract
Drug effects in the large bowel PUMICE Chapter 11: Alimentary Tract
Hepatocellular carcinoma variants: PC STAGS Chapter 12: Liver, Biliary Tract
and Pancreas
Nephrotic and nephritic syndromes: POH / OHO Chapter 15: Renal Medicine
Causes of 2
◦
membranous GN: SIND Chapter 15: Renal Medicine
Causes of 2
◦
FSGN: S.H.I.P. Chapter 15: Renal Medicine
Causes of nephrotic syndrome DASHIN Chapter 15: Renal Medicine
Infiltrating lobular carcinoma of the breast: CAST Chapter 18: Breast
MEN 1 (Wermer’s syndrome): All the ‘P’s Chapter 19: Endocrine
Painful lumps in skin / subcutis: TEABAGSPEND Chapter 20: Skin
Leukocytoclastic vasculitis (associations): MAID Chapter 20: Skin
Blistering diseases of the skin: PErHEPS Chapter 20: Skin
Distribution of bullous pemphigoid: WOLF Chapter 20: Skin
Epidermolysis bullosa acquisita (associations): ABC Chapter 20: Skin
Carcinomas metastatic to bone: The 5 ‘B’s Chapter 22: Osteoarticular
Albright’s syndrome: All the ‘P’s Chapter 22: Osteoarticular
Sarcomas positive for cytokeratins (CK): PEARLS Chapter 21: Soft Tissues
Malignant fibrous histiocytoma (MFH): MAGIC Skin Chapter 21: Soft Tissues
Kaposi sarcoma (clinical types): CELTA Chapter 21: Soft Tissues
Kaposi sarcoma (classical type): WIELDA Chapter 21: Soft Tissues
Kaposi sarcoma (endemic type): SMACS Chapter 21: Soft Tissues
Kaposi sarcoma (lymphadenopathic type): RAW Chapter 21: Soft Tissues
Kaposi sarcoma (transplant associated): LAFS Chapter 21: Soft Tissues
Kaposi sarcoma (AIDS associated): MDM Chapter 21: Soft Tissues
Causes of shock CHAOS Chapter 25: Autopsy

JWBK208-01 December 8, 2007 15:57 Char Count= 0
Exam Advice 5
Bibliography
Stamp, G.W.H. and Wright, N.A. (1990) Advanced Histopathology,1
st
edn, Springer-Verlag, Berlin & Heidelberg.
Weir, J., Benbow, E.W. and McMahon, R.F.T. (2004) How to pass and how to fail the MRCPath in histopathology part 2, ACP News (Winter 2004),
39–43.
Web sites
www.rcpath.org.uk (accessed April 2006) MRCPath Part 2 examination – Autopsy module: Guidelines for examiners and candidates (2004), Royal
College of Pathologists.

JWBK208-02 December 8, 2007 21:25 Char Count= 0
Histotechniques 6
2. Histological Techniques
K¨ohler Illumination
K¨ohler Illumination for Photography and Image Analysis
Setting up the microscope for K¨ohler illumination
For even illumination and optimum contrast do the following.
Condenser
Diaphragm (CD)
10
20
Field
Diaphragm (FD)
Condenser
focus control
FIGURE 2.1 Controls relevant to
K¨ohler illumination
1. Put a specimen on the stage, fully open both the field diaphragm
(FD) and the condenser diaphragm (CD) and focus the image at low
power (e.g. ×10 or the lowest power at which full field illumination
is achieved without the need to ‘flip down’ part of the condenser lens
system. This is because the full set of condenser optics is needed
for the following steps).
2. Close the FD and adjust the condenser focus control (! not the
main microscope focus control) until you see a sharp image of the
FD.
3. Centre the image of the FD by adjusting the condenser centration
screwsusu. found near the base of the condenser. Some microscopes
have a locking screw which must be loosened before adjusting
the centration screws. It should be re-tightened when centration is
complete.
4. Adjust the FD aperture such that its image just disappears beyond the field of view. As the aperture of
the FD is increased you may find it easier to make fine adjustments to the condenser centration.
5. Now adjust the CD aperture to match the numerical aperture of the objective. This may be done by
either a direct or indirect method:
Direct method: remove one of the eyepieces and look down at the aperture of the objective with your
eye ≈ 5–10cm away from the eyepiece holder tube. Adjust the CD until its boundary is just within the
aperture of the objective.
Indirect method: leave the eyepieces in place and look at the specimen. Slowly close the CD until a
slight drop in image brightness is first perceived.
6. Adjust brightness and colour-balance using the illumination power control or filters only – do not adjust
the diaphragms or condenser focus because this will alter image quality / sharpness. For imaging work,
note that a change of objective or any of the controls above will alter the amount of light getting through
to the imaging device – so re-calibration / re-metering will be necessary.
7. Whenever you change objective you should repeat steps 4 and 5 above to match the new field of view
and objective numerical aperture. If you change the slide you may also need to repeat steps 1 and 2 because
the preparation may be of slightly different optical thickness. [NB: low power objectives may require some
modification of the condenser such as swinging a lens out or, with very low power (≤×2) the condenser
may have to be removed altogether or the CD fully opened or a condenser diffuser inserted.]
K¨ohler Illumination in Diagnostic Practice
The above method is unnecessary for day-to-day work and may have disadvantages (e.g. any spec of dust
on filters over the FD may be constantly in the field of view causing an irritating distraction). Thus most
pathologists set up their microscope as described above once only and then leave the CD open to that extent
which is appropriate for the highest power objective commonly used (usu. ×40 or ×63), only opening it
further if they go to a higher power (e.g. ×100 oil immersion). Leaving the CD open like this has negligible
detrimental effects for direct viewing at lower power objectives. It is also common to keep the condenser in
a slightly de-focused position in order to get dust particle images blurred enough so as to be unnoticeable.
The FD is usu. left completely open at all times. Precise K¨ohler re-adjustment may, however, be necessary
when using very high power lenses e.g. looking for bacteria in Gram, ZN or CFV preparations.
Diagnostic Criteria Handbook in Histopathology: A Surgical Pathology Vade Mecum. Paul J. Tadrous
Copyright
C
2007 by John Wiley & Sons, Ltd. ISBN: 978-0-470-51903-5

JWBK208-02 December 8, 2007 21:25 Char Count= 0
Histotechniques 7
Counting Mitotic Figures and Ki-67 Proliferation Labelling Index
r
Only include definite mitoses in metaphase/anaphase (furry chromosomes and no nuclear membrane).
r
Scan the section for the most mitotically active area and start the count at that field. In some tumours
– e.g. breast – you must count at the growing edge of the tumour (not the centre).
r
For counts per 10hpf there are two methods:
1. count 3 or 4 sets of 10 fields and give the highest count;
2. count 100 hpf and divide the count by 10.
r
For counts per 50hpf count the n˜o. of mitoses in 50 hpf.
r
An hpf usu. means a ×40 objective with a standard wide field ×10 eyepiece. You should state the area
(e.g. in mm
2
) or diameter (in mm) of your hpf whenever giving a mitotic count in a report.
r
Mitotic count decreases with time from excision to fixation (up to 50% fewer if >12 hours) so are usu.
higher in frozen sections cf. paraffin sections.
r
For Ki-67, use the most active area and either
◦
1
count the n˜oof+ve nuclei in 2000 tumour cells and
divide by 20 to givea%or
◦
2
give the n˜oof+ve tumour cell nuclei per 10 hpf.
Fixation
Formaldehyde
r
Covalently cross-links peptides to inhibit degradation and ‘fix’ structure
r
A standard fixative as 4 % aqueous saline solution (=10 % formalin) – cheap and widely available
r
Good membrane structural preservation for LM (and, to a lesser extent, EM)
r
Good Ag preservation when combined with Ag retrieval methods (heat, protease, washing, sonic)
r
Slow tissue penetration rate (≈500 /hour) with even slower optimal fixation rate (≈80 /hour) because
it takes time for the cross-links to form even when formalin is present
r
Induces fluorescence in biogenic amines (e.g. noradrenaline and melanin precursors) / alters the fluo-
rescence properties of other native tissue structures
r
Some aqueous molecules / antigens (Ags) can diffuse out of the tissue
r
If not buffered, varying pH can cause varying artefacts, such as nuclear shrinkage and hyperchromasia
and variable cytoplasmic staining intensity
r
Can form birefringent formalin pigment in bloodied areas
r
Increases the weight of specimens (sometimes by almost 10%)
r
The volume of fixative should be ≥ 10× the specimen volume for adequate fixation
Alcoholic Fixatives
r
Disrupts hydrophobic bonds → denatures tertiary structure leaving 1
◦
and 2
◦
structure intact
r
Examples include: 70% ethanol, Carnoy’s (=ethanol, chloroform, acetic acid – excellent for fixing
tissue inks onto specimens at cut-up), formol alcohol, etc.
r
Faster tissue penetration cf. formalin (.
.
. good for cytology / rapid process / FS post-fixation)
r
Better preservation of large peptide Ags and less induced autofluorescence (.
.
. good for some IF)
r
Better preservation of nucleic acids (with Carnoy’s)
r
Worse preservation of membrane structure .
.
. sometimes combined with acetone (which has better
membrane-preserving properties but worse Ag preservation) e.g. for cytology
r
Can show worse differential tissue shrinkage artefacts cf. Formalin
Bouin’s
r
An example of a combination fixative, ingredients: picric acid, formaldehyde, acetic acid
r
Advantages: stains tissue yellow .
.
. easy to find LNs or embed small fragments (e.g. brain Bx)
good nuclear detail (e.g. spermatocytic seminoma)
small antigens are less soluble → enhanced sensitivity on immuno (e.g. AFP)
good for fixing India ink onto specimens prior to cutting
r
Disadvantages: degrades RNA and DNA .
.
. not good for ISH / PCR / Feulgen cytometry
causes undue differential shrinkage (e.g. glomeruli)
picric acid is explosive when dry .
.
. can’t use as a fixative in ordinary processors
more expensive than formalin
some Ags don’t survive the acid fixation or they show altered staining patterns
(e.g. prostate lumenal cell +vity for the protein product of c-erbB-2 [=the proto-
oncogene of type 2 EGFR, also known as HER2, the rat equivalent being neu]).

JWBK208-02 December 8, 2007 21:25 Char Count= 0
Histotechniques 8
Additives to Standard Fixatives
r
E.g. mercurials (obsolete due to health and safety), aprotinin and zinc
r
These enhance peptide antigenicity by inhibiting natural tissue proteases thereby hindering autolysis
Effects of Fixation on Staining
r
Fat retention: osmium / dichromates > formalin / glutaraldehyde acetone / OH
r
Protein retention: formalin / glutaraldehyde > osmium / dichromates > acetone / OH
r
Enzyme activity: acetone / OH > formalin / glutaraldehyde
r
Different methods alter the acidophilia:basophilia balance between tissue structures
r
Fe is leached out by acid fixatives
r
Effects of resin embedding: tissue and Ag occlusion, dye retention (e.g. due to hydrophobicity)
r
Formalin reduces colour contrast of many trichrome methods – use Bouin’s fixative (alternatively
pre-treat formalin-fixed tissues with picric acid and trichloroethylene)
Hard Tissues
Decornification
r
Softens tough keratinous tissues e.g. toe-nail
r
Phenol (outmoded due to health and safety)
r
Commercial alternatives available
Decalcification
r
Acids or Ca
2+
chelating agents – often mixed with formalin for combined decalcification/fixation
r
Strong acids (e.g. nitric) are rapid but give worse cytological and antigenic preservation
r
Weak acids (e.g. formic) are a good compromise between speed and Ag preservation
r
Chelators (e.g. EDTA) are the slowest but give best Ag / enzymic preservation
r
surface / superficial decalcification: bathe the cut-surface of a wax tissue block in HCl
Assessing when Decalcification is Complete
r
Standard time – uniform specimens (e.g. trephine Bx) may be known to decalcify within a set time for
a given decalcification agent and can be standardised for any given lab
r
X-raying specimens: expensive and has additional health and safety requirements for operators
r
Chemical tests of residual Ca
2+
in the decalcification fluid: when changing the fluid, add ammonia and
ammonium oxalate to the spent fluid. If CaOH precipitates out (fluid turns cloudy) the specimen needs
more decalcification → add fresh decalcification fluid.
Undecalcified Sections
r
Sections of bone can be cut with a diamond knife and ground down to histological thinness
r
This allows routine staining (usu. with von Kossa or Goldner’s method – p. 11) and assessment of
calcification front and osteoid seam thickness for assessing metabolic bone diseases e.g. osteomalacia
Staining (Principles)
Dye Nomenclature
r
Mordanted dyes are dyes complexed to metal ions. The metal ion forms a covalent bond with the tissue
thus cementing (mordanting) the dye in place e.g. iron haematoxylin (celestin blue) is used in HVG
because VG is an acidic counterstain and will complex with and remove ordinary haematoxylin
r
Acid dyes are those whose coloured species are anionic e.g. eosin
r
Basic dyes are those whose coloured species are cationic e.g. methylene blue or alum haematoxylin
(by means of its Al
3+
mordant)
r
Neutral dyes: both the anion and cation are coloured e.g. the Romanowsky mixture (p. 10)
Immunohistochemical Methods
Labelling Technologies
1. Fluorophore: very sensitive and can be used for quantitation if used with a direct method but fluorescence
fades with time so no good for permanent preparations
