Tadrous P.J. Diagnostic criteria handbook in histopathology: a surgical pathology vade mecum
Подождите немного. Документ загружается.


JWBK208-12 December 8, 2007 16:4 Char Count= 0
Liver, Biliary Tract and Pancreas 159
paracetamol: sharply defined perivenular necrosis with little inflam
n
mixed hepatitic/cholestatic picture with duct damage (e.g. flucloxacillin/paraquat)
r
Alcohol: perivenular ballooning with PMN (cf. lymphocytes) ± Mallory hyaline/steatosis/fibrosis
r
Biliary disease: may show granulomas in PBC (but ! d/dg IVDA)
relative lack of lobular disease
CuBP (black dots with orcein or blue dots with a Victoria blue stain)
greater ductular proliferation ± ductopaenia with relative lack of cholestasis
CPC (autoAbs, etc.)
r
2
◦
cholestasis: liver cell damage confined to cholestatic areas, lack of spotty necrosis
r
AIH: hard to distinguish from acute hepatitis (esp. HAV) .
.
. need CPC (auto/viral Abs, etc.)
r
Chronic hepatitis/cirrhosis: distinguish bridging/confluent necrosis from fibrosis (vide infra)
Features Favouring Necrosis cf. Fibrosis
r
Other assoc
d
features of acute hepatitis
r
Elastic is absent (elastic takes time to develop so is a sign of chronicity)
r
Residual hepatocyte plate structure is preserved (although collapsed) on reticulin stain
r
Stroma is more haemorrhagic with more M (! don’t confuse ceroid M for hepatocytes)
r
Bile ductular proliferation and PMN
Chronic Viral Hepatitis
General Points
r
Def
n
of chronic hepatitis: continuing clinicopathological disease for ≥6 months
excludes PBC, PSC,
1
AT deficiency and Wilson’s disease.
usu. due to viruses, autoimmunity and drugs
r
Traditional classification into CAH, CPH and CLH is no longer used because all may co-exist and the
difference depends on interface activity whereas other factors (confluent necrosis, fibrosis, etc.) may
be more significant – hence the current vogue for histological grading and staging schemes
r
‘Activity’ has two aspects: interface and lobular.
Portal Inflammation and Interface Activity
r
Predominantly T4 cells and some plasma cells (T8 cells at the advancing front of interface hepati-
tis/activity)
r
Interface activity = spill-over of inflam
n
beyond the PT limiting plate (± hepatocyte apoptosis) with
lymphocytes closely adhered to (peripolesis) or apparently within (emperipolesis) hepatocytes. It is
helpful to see lymphocytes at the hepatocyte-hepatocyte interface (otherwise it could just be sinusoidal
infiltration)
r
Hepatitic damage to bile ducts ± portal phlebitis (cf. the central phlebitis in acute hepatitis)
r
It is no longer necessary to see dead/dying hepatocytes to diagnose interface activity
Lobular Activity
r
Focal spotty necrosis: this term includes perivenular parenchymal inflam
n2
or acute-type necrosis – not
just apoptoses (Councilman bodies), although these are also included
r
Confluent necrosis: may be linking +/ bridging (C-C +/ P-C but only P-C is used in the Ishak grade)
±hepatitic rosettes (surrounded by inflam
y
/connective tissue and usu. lack a lumen cf. d/dg cholestatic
rosettes that may also show a connection to bile ductules, contain bile and stain for biliary CK)
Viral Co-Infection
r
HBV: if serology +ve for HBV with tissue immuno −ve for HBsAg, suspect co-HCV or co-HDV
r
HIV and HBV: a higher % progress to chronicity but they show lower histological activity. May get
‘reactivation’ lobular hepatitis in severe AIDS, even if +ve for HBsAb (may even get FCH)
r
HIV and HCV: synergistic – both the HIV and HCV pursue a worse course (incl. ↑ risk of HCC)
Hepatitis B (HBV)
3
r
Ground glass hepatocytes (eccentric nucleus ±clear rim around the ground glass cytoplasmic inclusion
cf. d/dg oncocytic change) ± lymphocyte emperipolesis
2
does not include inflam
y
cells only in the sinusoids; ! exclude cross-cuts of inflamed PT septa
3
HBV is the only one out of A, B, C, D, E that is a DNA virus

JWBK208-12 December 8, 2007 16:4 Char Count= 0
Liver, Biliary Tract and Pancreas 160
r
Sanded nuclei (core Ag or HDV), ↑ anisonucleosis ± large cell dysplasia (q.v.)
r
↑ Replication (and ↑ histological activity unless immunosuppressed) if immuno shows:
◦
1
membranous staining for HBsAg (not just cytoplasmic)
◦
2
HBcAg +vity (esp. if there is cytoplasmic staining)
r
90% of cases become e&sAg−ve, Ab +ve: this indicates protective Ab virus elimination
r
10% of cases become e&sAg+ve, Ab −ve: this indicates chronic hepatitis (active)
r
50% of chronic hepatitics seroconvert to eAg −ve, Ab +ve (assoc
d
with clinical and histological
exacerbation) to become chronic carriers
r
mutants:
◦
1
pre-core: eAg not expressed, eAb +ve despite ongoing replication and active disease
◦
2
sAg: vaccine resistant
Hepatitis C (HCV)
r
Bx changes do not correlate with clinical/biochemical severity .
.
. Bx gives independent information
r
Lymphoid follicles (1
◦
or 2
◦
– germinal centres are esp. characteristic) ± hepatitic BD damage
r
Mild-moderate steatosis (macro and microvesicular)
r
Sinusoidal lymphocytes (d/dg EBV)
r
Synergistic with OH: suggest OH if severe fat or pericellular/venular fibrosis or ballooning and PMN
r
Fe in Kupffer ∝ poor response to Rx; Fe in parenchyma:
◦
1
PCT
◦
2
cirrhosis
◦
3
haemochromatosis
r
Granulomas (PT or lobular) – but not assoc
d
with chronic ductopaenia and not causing BD destruct
n
r
Extrahepatic effects: cryoglobulinaemia, GN
4
,Sj¨ogren’s; PAN, LP, PCT, lymphoma (low grade B-cell
e.g. LPL, MZL and MALTomas incl. hepatic/salivary 1
◦
– not TCL or HL), autoAb e.g. ALKM,
anti-thyroid, ANA (a false +ve due to cross-reactivity with HCV Ags) and antiphospholipid (but usu.
without the TMA of antiphospholipid Ab syndrome)
Hepatitis D (Delta Agent, HDV)
r
Co-infection/super-infectionwith HBV is assoc
d
with active/fulminant disease (recurrent acute hepatitis
is characteristic), cirrhosis and HCC; may see periportal morule cells (multivacuolated hepatocytes)
r
Immuno (nuclear +vity for delta agent) is more reliable than serology
r
Inhibits HBV replication →
◦
1
HBV immuno can become −ve,
◦
2
↓ mortality in Tx patients
r
Chronic HDV may have an ALKM-3 AIH component
The Modified Histological Activity Index (HAI) for Chronic Hepatitis – Table 12.1
r
! Sub-capsular/peri-hilar biopsies show unrepresentative accentuation of fibrosis +/ necrosis
The Royal College of Physicians/BSG categories for HCV hepatitis
r
Mild: stage ≤ 2 AND either combined grade ≤3/18
or A grade ≤ 1
AND C grade ≤ 1 AND B grade = 0(D grade = any)
r
Moderate: stage 3–5 AND/OR combined grade >3/18
r
Cirrhotic: stage = 6 (any grade)
Differential Diagnosis of Chronic Viral Hepatitis
r
Acute hepatitis A: interface activity and plasma cells ++ can give impression of AIH or chronic viral
hepatitis .
.
. look for lobular changes and CPC
r
AIH: serology, plasma cells ++, interface ++ with rosetting, parenchymal collapse
! HCV can give false +ve ANA
! an AIH component may accompany hepatitis B, C and D
! d/dg drug-induced AIH-like disease
r
Metabolic:
1
AT deficiency: DPAS +ve globules (! exclude concomitant viral infection)
Wilson’s disease: Mallory hyaline, fat, Cu, broad vascular fibrous septa
r
Drug-induced: viral-type chronic hepatitis is rare but can occur (e.g. with -methyldopa – but AIH-like
chronic hepatitis is commoner with this drug)
r
PBC: early lesions difficult to distinguish from HCV which may show bile duct damage and loss. Later:
◦
1
granulomatous BD destruct
n
;
◦
2
ductular prolif
n
,
◦
3
chronic cholestasis periportal/septally
r
PSC, PBC and other biliary diseases: deposition of Cu/CuBP at an early stage of liver disease favours
a biliary disease (but any cause of end-stage liver disease can cause CuBP to accumulate)
4
membranoproliferative or ADP (both may be due to cryoglobulins)
JWBK208-12 December 8, 2007 16:4 Char Count= 0
Liver, Biliary Tract and Pancreas 161
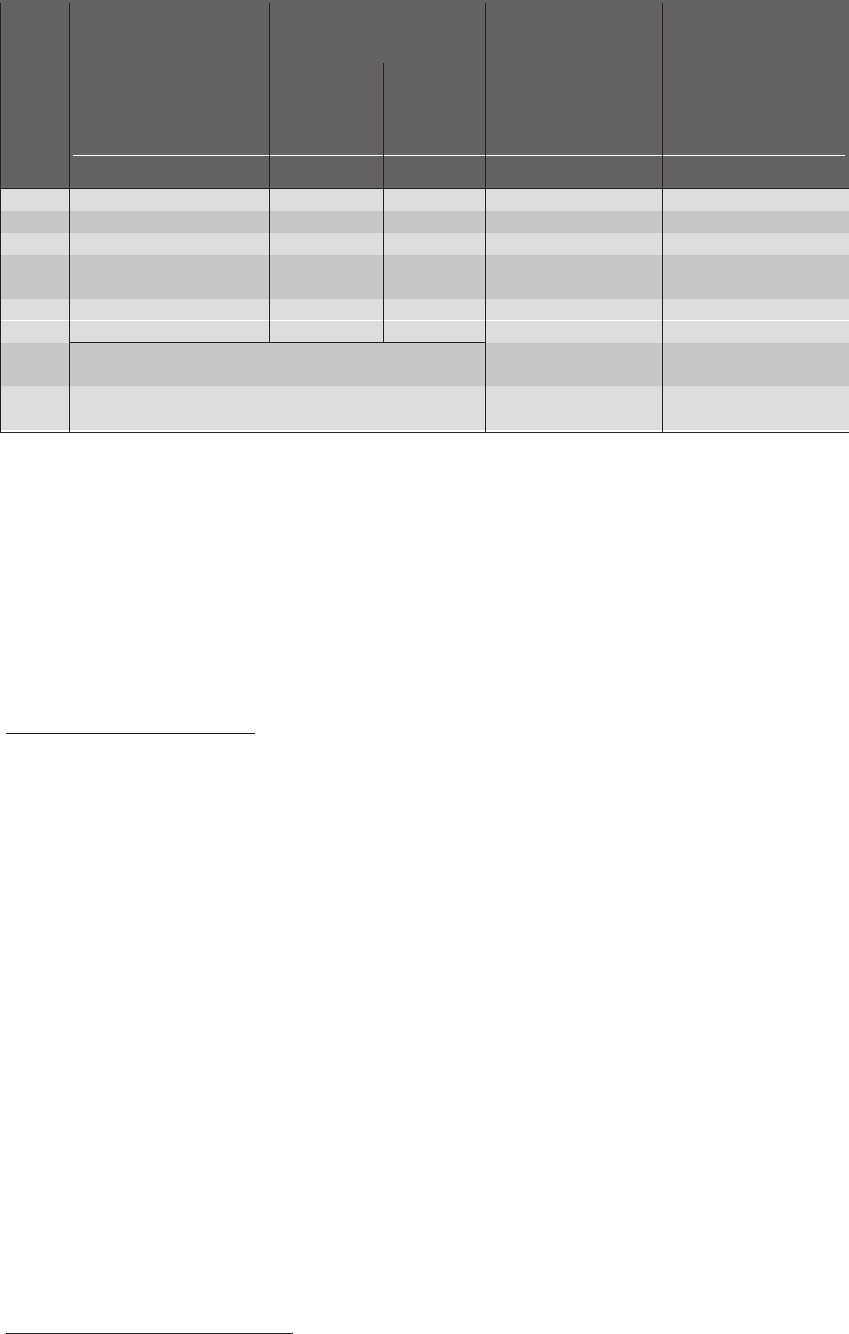
TABLE 12.1 Grade and stage in heptatitis
SCORE ACTIVITY
#
c
INFLAMMATORY CONFLUENT FIBROSIS
INFILTRATE NECROSIS
WITHIN SEPTA & (% of acini
PORTALTRACTS Interface Lobular (foci with confluent
(% of septa/ per x10 necrosis in
(% of septa/PTs af fected) PTs af fected) objective)
*
a zonal pattern) (% of PTs expanded)
D Grade A Grade C Grade B Grade Stage
0 none none none none none
1 mild (in ≤ 100%) focal & <50% ≤1 focal (not zonal)
†
<50% ± short septa
‡
2 moderate (in ≤ 100%) focal & >50% 2–4 <50% (zone 3 only) >50% ± short septa
3 100%, some with continuous 5–10 >50% (zone 3 only) >50% & occ. P-P links
a severe infiltrate around <50%
4 100%, all with a continuous >10 occasional bridging marked linking/bridging
severe infiltrate around >50% to zone 1 (P-C) (P-P +/ P-C)
5 multiple P-C bridges as for score 4 plus
occasional nodules
6 ≥ 1 acinus shows zonal cirrhosis (even if
necrosis in all 3 zones only probable)
**
This grading & staging system is a modification of Knodell’s HAI & is based on Ishak K, Baptista A, Bianchi L, et al.
JHepatol(1995); 22:696-9
*
i.e. focal inflam
n
/apoptosis/‘lytic’ cell dropout. Focal inflam
n
does not include diffuse sinusoidal infiltration by inflam
y
cells. It is ‘interface’-type inflam
n
but in a pericentral location.
†
i.e. contiguous groups of hepatocytes are necrotic (not apoptotic) but without a clear zonal pattern (d/dg HSV or TB).
‡
septa due to interface activity tend to be curved, cellular & stain for retic but not type I collagen until mature.
this is sometimes called ‘incomplete cirrhosis’ which, here, appears to mean ‘not quite fully cirrhotic’ rather than the
more tightly defined entity of incomplete septal cirrhosis (q.v.).
**
! Avoid overcalling cirrhosis due to artefactual Bx fragmentation.
r
Leukaemia/lymphoma: no true piecemeal necrosis; lymphoid cells may look ‘clonal’/‘pure culture’
(i.e. not mixed inflam
n
); some claim scarring is absent while others describe possible fibrosis incl. P-P
linking
Autoimmune Hepatitis (AIH)
r
Type 1: classic lupoid CAH: ANA/ASGP-R/ANCA, assoc
d
with other system autoimmunity
r
Type 2: idiopathic in children (in adults it is usu. due to HCV = Type 2b), ALKM-1, ALC
r
Type 3: assoc
d
with SLP auto-Abs (also called SLA), no other system autoimmunity
r
Type 4: assoc
d
with anti F-actin smooth muscle Abs (ASMA)
r
↑ Globulinaemia and autoAbs (>1:80 adult or 1:20 child) though some may be −ve at presentation
and many auto-Abs e.g. ANA or ASMA are not specific to AIH so other features must be present
r
Plasma cells ++, interface hepatitis ++, ± cholestasis/bile duct damage; in acute AIH there is also
severe lobular plasma cell-rich inflam
n
± giant cells and ballooning
r
± Central necrosis ± bridging, ± acute/fulminant hepatitis (d/dg HAV) esp. in childhood type 2 AIH
r
Zone 3 variant: centrilobular necroinflam
n
, usu. with plasma cell clusters ± congest
n
± PT inflam
n
r
d/dg AMA −ve PBC: in AIH inflam
n
is more uniform and intense, shows lobular activity and lacks
typical PBC duct damage
r
d/dg zone 3 variant vs. venous outflow obstruction
r
‘Probable AIH’(→trial of steroids) if:
◦
1
mild changes or
◦
2
lack typical Abs or
◦
3
other possible aetiological factors are present
Overlap Syndromes
r
Steroid-responsive cholangiopathic autoimmune hepatitides (! long-term steroids may worsen PBC)
r
Mixed AIH/PSC: uncommon, often in children
r
Mixed AIH/PBC
5
:
◦
1
AMA −ve, ANA/ASMA +ve and the inflam
n
has some PBC-like features or
◦
2
AMA +ve with AIH-type inflam
n
or
◦
3
clinically, any patient with ≥ 2 features of AIH and ≥ 2 features of PBC
5
AMA -ve types are sometimes called ‘autoimmune cholangiopathy’ or ‘immunocholangitis’.

JWBK208-12 December 8, 2007 16:4 Char Count= 0
Liver, Biliary Tract and Pancreas 162
Intrahepatic Bile Ducts
Cholestasis
r
Perivenular canalicular bilirubinostasis (seen in acute hepatitis, drugs, ischaemia, post-op, etc.)
r
Cholestatic liver cell rosettes (usu. have a lumen and are surrounded by other hepatocytes)
r
Biliary interface activity (biliary piecemeal necrosis):
is the main clue to diagnosing a 1
◦
biliary disorder (obstructive, inflam
y
, etc.)
is defined by three features:
◦
1
cholate stasis,
◦
2
ductular react
n
,
◦
3
fibroplasia
◦
1
Cholate Stasis:
feathery degeneration of periportal hepatocytes which acquire Cu and CK7/19 +vity
later bilirubin and Mallory hyaline (in zone 1) also accumulate ± xanthomatous M
◦
2
Ductular Reaction:
proliferation of ductules and neocholangioles at the limiting plate
6
± PMN due to irritant effect of bile (not seen in other causes of ductular proliferation e.g.
infection, alcohol, venous outflow obstruction or isolated ductular hyperplasia)
7
◦
3
Fibroplasia: accompanies the ductular reaction and is loose/oedematous and at the periphery
of the PT/septum (→ clear ‘halo’ effect around septa/PTs)
r
Biliary cirrhosis: monolobular arch. (i.e. retained central venule ± ‘jig-saw’ parenchyma), clear halo
around septa, lots of zone 1 Cu/CuBP and loose lamellar fibrosis in the septa suggest a biliary origin
Vanishing Bile Duct Syndrome
Adequacy of sampling
r
10 PTs are needed (some say 20) to diagnose ductopaenia by the 50% rule (i.e. ≥50% of PT arteries
are unaccompanied by a BD). Also, sig. BD loss is present if <80% of PTs have a BD
r
However there is evidence that, for BD loss to be statistically significant, the minimal % BD loss
required varies with the n˜o. of PTs in the Bx e.g. for a Bx with 4 PTs you need 100% loss, for 8 PTs
you need ≥75% loss, etc. (see Tadrous and Goldin, 1997)
(Sub)acute BD loss
r
Acute cholestasis with little or no biliary interface activity
r
Causes incl. GVHD, liver Tx rejection, some drugs, treated HL
Chronic BD loss
r
Little cholestasis but prominent biliary interface activity → cirrhosis
r
Causes incl. PBC, PSC/SSC, liver Tx rejection, sarcoid, ischaemia, some drugs and infections
Septal/large duct disease
r
PSC and childhood extrahepatic biliary atresia may cause ductopaenia
Other causes
r
Idiopathic adulthood ductopaenia (diagnosis of exclusion, some are progressive like PSC/PBC)
r
Infantile/childhood: syndromic e.g. Alagille, Zellweger,
1
AT ↓, CF, Down’s, etc.
non-syndromic e.g. PFIC (cholestasis, cholate stasis, inflam
n
and cirrhosis),
d/dg BRIC (canalicular cholestasis only)
Staging of PBC and PSC
r
In a Bx, report the highest stage present (not the predominant stage). Some recommend using the HAI
I changes confined to the PT
II interface activity (chronic inflam
y
and biliary) ± short radiating septa
III scarring, incl. significant septa or P-P linkage (‘biliary fibrosis’)
IV biliary cirrhosis
Primary Biliary Cirrhosis (PBC)
r
Clin.: FM (9:1), anti-M2 AMA +ve in >95%, ± Sj¨ogren’s, PSS, coeliac, etc.
r
Early: mixed chronic inflam
y
infiltrate in PT (predom. lymphoid) with granulomas =‘florid bile
small BD epithelial damage and regeneration, intraepithelial lymphocytes
duct lesion’
patchy changes (! sampling may result in non-specific PT inflam
n
only)
6
ductular prolif
n
(often lumenless) is seen in many conditions with limiting plate hepatocyte damage
7
isolated ductular hyperplasia (i.e. with no other lesion) is a cause of prolonged ↑ in ALT +/ GT
JWBK208-12 December 8, 2007 16:4 Char Count= 0
Liver, Biliary Tract and Pancreas 163
r
Medium term: vestigial CK7/19 or PAS +ve elements
condensation of fibrous tissue
where BDs used to be
lymphoid aggregates ± foamy M
r
Late: progressive BD loss (the smaller the duct the more likely it is to be lost)
biliary interface activity
biliary cirrhosis and cholestasis
r
Other: mild lobular inflam
n
incl. sinusoid lymphocytosis ± small granulomas
lymphocytic interface hepatitis ± occ. plasma cells and the odd germinal centre (d/dg
viral/AIH)
± Councilman bodies (some say that hepatocyte damage or other sig. lobular activity is
not typical of PBC and should suggest a superimposed process or an overlap syndrome)
r
d/dg: sarcoid (vs. AMA −ve PBC) granulomas are not targeted at BDs, may cluster and are ≈ bare
r
d/dg: drugs, PSC, viral or AIH, HL and any cause of vanishing BDs
Primary Sclerosing Cholangitis (PSC)
r
Clin.: M>F, ± colonic CIBD, pancreatitis, multifocal fibrosclerosis, osteopaenia, cholangioCA
r
Radiol: abnormal MRI cholangiogram or ERCP (otherwise = ‘small duct PSC’)
r
Macro: normal → dilated irregular ducts → segmental/hemi cirrhosis (i.e. more uneven cf. PBC)
r
Largest BDs: periduct fibrosis extending to fat, prolif
n
of periductal glands
severe (mainly lymphoplasmacytic) inflam
n
(! d/dg severe hepatitis)
ulceration (± acute inflam
n
and bilirubin impregnation) ± dysplasia
r
Large BDs: tortuosity ± mixed inflam
n
± follicles ± interface activity (biliary ± AIH-like)
d/dg PBC but PSC has: less inflam
n
but more oedema
sparse/no intraepithelial lymphocytes/granulomas
concentric lamellar (‘onion skin’) and hyaline fibrosis
nodular scarring ± adjacent parenchymal collapse
larger ducts also involved
± cholangitis
earlier cholestasis
r
Small BDs: BDs vanish (replaced by a hyaline/fibrous scar)
PT arteries appear to proliferate (due to tortuosity 2
◦
to PT fibrous shrinkage)
r
Gallbladder: l.p. lymphocytic + plasma cell inflam
n
(esp. if diffuse and acalculous) ± fibrosclerotic
vasc. changes
r
d/dg SSC (HIV, post-op ischaemia, mastocytosis, HX, etc.): can’t distinguish from PSC by histol.
r
d/dg: PBC and any other cause of vanishing bile duct syndrome (q.v.)
r
d/dg extrahepaticor large duct obstruction (q.v.) from anycause incl. PSC (they may coexist)or recurrent
suppurative cholangitis (healing → fibrous scar replaces duct) due to Clonorchis/ascarids
Dubin-Johnson Syndrome
r
Variably-sized lipofuscin-like granules in (predom. zone 3) hepatocytes but no cholestasis
Caroli Disease and Syndrome
r
Clin.: disease is sporadic, no portal HT; syndrome (=disease +congenital hepatic fibrosis) is usu. AR
r
Dilated bile ducts (upto 2cm ) with thickened walls and marked chronic inflam
n
r
Lining: BD epithelium (bland or reactive atypia or dysplasia) or denuded with bile encrustation ± M
r
± Surrounding small duct proliferation: d/dg atresia (q.v.)
r
Assoc
d
with autosomal recessive polycystic kidney disease, choledochal cyst(s) and cholangioCA
r
d/dg biliary ectasias 2
◦
to PSC
Congenital Hepatic Fibrosis
r
Usu. AR (but AD occurs) ± Caroli disease ± portal HT, cholangitis, cholangioCA, polycystic kidney
disease (AR and AD types), TS, Meckel-Gruber and many more syndromes
r
Liver carved up into irregular islands (‘jig-saw’) by fibrous tissue
r
Elongated irregular BD-like structures at the limiting plate and separate BDs centrally within the septa
r
No cholestasis or sig. inflam
n
unless complicated by ascending cholangitis (or Caroli)
r
± Mallory hyaline but no sig. lobular activity/necrosis
r
Assoc
d
with malformation of intrahepatic portal vein branches (may be small/absent)
r
d/dg cirrhosis: this has regenerative nodules ± inflam
n
/necrosis

JWBK208-12 December 8, 2007 16:4 Char Count= 0
Liver, Biliary Tract and Pancreas 164
Alagille’s Syndrome (Arteriohepatic Dysplasia)
r
Sporadic/AD, dysmorphic baby, CVS anomalies, ± portal HT
r
Canalicular cholestasis ± hepatocellular giant cells, biliary interface activity and evidence of biliary
epithelial damage (lymphocytes, PMN, ± lumenal fibro/epithelial obliteration)
r
Chronic BD loss (for def
n,
see ‘Vanishing Bile Duct Syndrome’, p. 162)
von Meyenburg Complexes (vMC or Bile Duct Hamartoma)
r
Para-PT, usu. <5mm, ± multiple; assoc
d
with cavernous haemangioma, cholangioCA, ADPCKD
8
r
Round with irregular (branched, angulated, ectatic) and inter-connected ducts in cellular fibrous stroma
r
Cytology: bland, ± inflam
y
atypia if intralumenal PMN, ± bile plugs, ± intralumenal mucin (rare
and not intracellular as in d/dg adeno
CA or BD adenoma) or amorphous eosinophilic proteinaceous
secretions
r
Immuno: mCEA has a lumenal pattern (cf. cytoplasmic in adenocarcinoma)
r
d/dg adenocarcinoma: good circumscription, bland cytology, bile plugs, vMC gland architecture and
lack of intracellular mucin all favour vMC
r
d/dg multiple vMC vs. congenital hepatic fibrosis: use CPC
r
d/dg BD adenoma (q.v.) is bigger with less stroma, smaller (and more packed) ducts and no bile plugs
Extrahepatic and Large Bile Ducts
Large Duct Obstruction in Neonates (Extrahepatic Biliary Atresia)
r
Early: PT oedema, BD (and ductular) prolif
n
± PMN ± inspissated bile (d/dg sepsis q.v.)
r
Lobules may show cholestasis (esp. zone 3) ± a few zone 1 multinucleated hepatocyte GC
r
Later: BD loss progressing to 2
◦
biliary cirrhosis (see section on Cholestasis, p. 162)
r
Obliterated extrahepatic duct(s) show fibrosis ± chronic inflam
n
± residual epithelial cells
r
FS during Kasai procedure:
9
are there genuine BDs (cf. para-scar blind saccules)?
BD lumen of ≥100–200
at the proximal resection margin sug-
gests likely success (else the procedure may be abandoned)
r
d/dg incl. many things (so definitive diagnosis should not be solely histological):
neonatal hepatitis: atresia has ductular prolif
n
, sig. PT fibrosis, less retic collapse/lobular
disarray, fewer GC (and these tend to be in zone 1 cf. widespread) and more cholestasis
prolonged TPN (≥3 weeks) and obstructive choledochal cyst show similar histology .
.
. need
CPC
some cases of CMV or
1
AT↓ or other IEM
Large Duct Obstruction in Adults
r
Early changes: zone 3 cholestasis with enlarged Kupffer cells, PT oedema
r
Later in PT: mixed inflam
n
incl. PMN ±eos., ±concentric BD fibrosis (d/dg PSC, which may coexist)
r
Later in lobules: feathery degeneration and mild changes reactive to bile: apoptosis, mitosis and inflam
n
r
≈ Specific changes (helpful in the d/dg but not always present):
para-PT lobular bile infarcts: a bile infarct is an area of pale/foamy/rounded/pyknotic or dead
hepatocytes (! d/dg M) and fibrin ± bile-staining
PT bile extravasates with M response ± giant cells
marginal bile ductular prolif
n
with the ductules orientated ≈ parallel to the limiting plate
r
If untreated → cholate stasis → 2
◦
biliary cirrhosis
r
d/dg drug reaction (if eos. prom.): obstruction rarely shows bland cholestasis without ductular prolif
n
r
d/dg alcohol (ASH) (if PMN prom.): OH has more lobular activity (incl. PMN, Mallory and steatosis)
r
d/dg acute hepatitis: necrosis (without bile infarcts) with bridging favours hepatitis
r
d/dg ductular prolif
n
of cholate stasis: biliary piecemeal necrosis has more irregular ductules, many
without lumena and not arranged ≈ parallel to the limiting plate (as may occur in marginal prolif
n
)
r
d/dg space occupying lesions may show similar changes but with sinusoid dilatation
r
d/dg TPN can also be a mimic in adults but more commonly it shows steatosis and less/no PT changes
r
d/dg sepsis and 2
◦
ascending cholangitis (q.v.)
r
d/dg autoimmune pancreatitis: plasma cells in liver are +ve for IgG4 and patients have ↑ serum IgG4
8
The lesions of ADPCKD are thought to arise by dilatation of vMCs and peribiliary glands.
9
some say it makes no difference if ducts are found at FS or what their is - the procedure may still work. Others say that a total
lumenal area (of all hilar ducts) ≥ 100000 m
2
is a good prognostic.

JWBK208-12 December 8, 2007 16:4 Char Count= 0
Liver, Biliary Tract and Pancreas 165
HIV Cholangiopathy (= AIDS Cholangiopathy)
r
Occurs in late HIV with low CD4 count
r
Due to Cryptosporidium/microsporidium/CMV infection
r
MRI, ERCP and histology are all similar to that seen in PSC (q.v.)
Liver Transplant Pathology
FS of Potential Donor Liver
r
Exclude contraindications to Tx: severe macrovesicular steatosis, neoplasia or chronic hepatitis
r
Mild portal triaditis is acceptable provided there is no clinical/serological evidence of viral disease
Reperfusion Injury (e.g. in the Baseline Bx at
1
2
hour)
r
Cholestasis (intrahepatocyte and canalicular) lasts a few weeks
r
Ballooning without necrosis is also transitory
r
Mild focal endothelialitis is acceptable without implying rejection
r
± Lipopeliosis (fatty expansion of sinusoids) may occur in steatotic transplants
r
Tiny foci of hepatocyte necrosis ± local PMN (usu. resolve within days)
r
Widespread PMN or zones 1&3 necrosis with subcapsular accentuation is a poor prognostic
Transplant Rejection
Hyperacute (humoural) rejection
r
Occurs hours to 1 week after Tx
r
Early: sinusoid engorgement, fibrin, PMN, Ig and C3
r
Later: extensive zone 3 haemorrhagic coagulative necrosis
Acute rejection
r
Occurs in the first 2 months (after Tx or after reduction in immunosuppression); requires ≥2 of:
◦
1
venular endothelialitis (predom. PT but, if severe, extends to zone 3 necrosis ± regenerat
n
/
congest
n
)
◦
2
mixed PT inflam
n
(eos., lymphocytes [usu. T8], blasts, M, plasma cells, PMN) ±interface if
severe
◦
3
BD epithelial vacuolation/regenerative atypia ± lymphocytes +/ PMN (! d/dg ascending
cholangitis)
r
± Arterial endothelialitis/fibrinoid indicate severe rejection and
r
± Zone 3 necroinflam
n
not 2
◦
to venular endothelialitis
↑ risk of chronic rejection
r
Atypical acute rejection has zone 3 necroinflam
n
, congestion ± dropout but no sig. PT anomaly
r
In early rejection PT inflam
n
is predominantly lymphocytic, other cells (esp. eos.) ↑ with severity
r
Immunosuppression Rx quickly removes endothelialitis and decreases eos. and mononuclear cells .
.
.
if Rx started prior to initial Bx look for BD epithelial damage and be wary of grading severity
r
Grade (via the Banff Rejection Activity Index – see Bibliography and www.tpis.upmc.edu)
≥ moderate rejection (i.e. RAI ≥6 or infiltrate expanding most PTs) requires additional Rx
only grade if rejection is the predominant cause of the abnormalities
only grade if Bx is adequate: ≥5 PTs available, ≥2 H&E sections at each of ≥2 levels
r
d/dg: recurrent viral hepatitis (esp. HCV): HCV chronic hepatitis occurs >4 months post Tx and is
favoured by high serum HCV RNA, predominantly lymphocytic inflam
n
, ↑ interface, ↑ fibrosis, sig.
lobular activity (steatosis, sinusoidal dilatat
n
, necroinflam
n
, etc.) and lack of venular endothelialitis. If
features are equivocal, consider simultaneous HCV and rejection.
r
d/dg other causes of endothelialitis e.g. severe HCV (i.e. endothelialitis alone is not proof of reject
n
)
r
d/dg: other causes of zone 3 necroinflam
n
: reperfusion injury, chronic reject
n
, viral hepatitis, AIH,
calcineurin inhibitors, vasc. occlusion (any vessel) and idiopathic chronic hepatitis
Chronic rejection
r
Occurs ≥ 60 days (post Tx or reduction in immunosuppression)
r
Medium and larger arteries: prolif and obliterative endarteritis with foam cells → ischaemia (q.v.)
r
PT early changes:
cytologically atypical BD atrophy (nuclei: irregular distribution, drop-out, ↑ size and hy-
perchromasia; cytoplasm: eosinophilia and syncytia) with ↓ inflam
y
infiltrate as rejection
progresses
mild BD loss (≥50% of PTs have a BD) and mild PT artery loss (≥75% of PTs have an
arteriole)

JWBK208-12 December 8, 2007 16:4 Char Count= 0
Liver, Biliary Tract and Pancreas 166
r
PT late: marked BD loss (<50% of PTs have a BD), PT artery loss (<75% of PTs have one)
r
Zone 3 early: necroinflam
n
(± pigment M, cell dropout and mild fibrosis)
r
Zone 3 late: ballooning, cholestasis, severe fibrosis ± foam cells in sinusoids/smaller vessels
r
d/dg recurrent chronic biliary disease (PBC/PSC): rejection has ↓inflam
n
in PT, no florid BD granulo-
mas, no ductular prolif
n
or PT fibrous expansion. PSC/PBC usu. recur late (≥ 1 year)
r
d/dg: other causes of zone 3 necroinflammation or vanishing BD syndrome (vide supra)
Idiopathic chronic hepatitis
r
Occurs >1 year post Tx, ↓ endothelialitis, ↓ BD damage, ↑ interface, ↑ zone 3 spotty necrosis
r
Not obviously viral, AIH or drug-related. (? is a form of delayed acute reject
n
)
Recurrent and De Novo Disease in the Graft
r
Most look similar to the disease in the native liver but may be modified by immunosuppression
r
PSC must be distinguished from chronic rejection (vide supra) and ischaemic SSC (which usu. presents
<6 months post Tx unlike recurrent PSC)
Infection post Liver Tx:
r
Opportunistic (e.g. CMV): look for mini-microabscesses (PMN aggregates) +/ granulomas
r
Fibrosing Cholestatic Hepatitis (FCH) may occur in the 1
st
few months of recurrent HBV/HCV with
widespread viral immunopositivity. It shows:
◦
1
PT ductular reaction with fine reticular fibrosis,
◦
2
florid
hepatocyte ballooning but minimal inflam
n
,
◦
3
cholestasis.
r
New/recurrent HBV: usual acute/chronic hepatitis (± more aggressive) or steatosis +/ FCH
r
New/recurrent HCV: usual histology (±ductular reaction/confluent necrosis) or predominantly lobular
apoptoses with mild PT changes or FCH
Other Post Tx Complications
r
Vascular thromboses can lead to infarcts (usu. in the 1
st
2 weeks post Tx)–!exclude d/dg fungi
r
SSC/biliary anastomotic obstruction (cholestasis + ductular reaction + PT oedema and PMN)
r
Drug effects incl. cholestasis +/ zone 3 necrosis/fibrosis – d/dg acute rejection/ischaemia
r
PTLD may present as a mass lesion or as PT infiltrates d/dg acute rejection infiltrate (which is EBV &
HHV8 −ve)
Graft vs. Host Disease (GVHD)
r
Due to foreign lymphocytes from BMTx, non-irradiated blood or solid organs (e.g. SI or liver Tx).
Maternal lymphocytes can produce similar pathology in the immunocompromised fetus
r
Clin.: changes occur in the liver (jaundice and cholestatic LFTs), skin & gut (and, if chronic, also in
LN, muscle, lung, lacrimal & salivary glands)
r
1
st
month: lobular focal inflam
n
, focal necrosis and Councilman bodies (d/dg viral hepatitis, CMV, etc.
– but these usu. have less BD damage cf. GVHD)
r
2
nd
month: PT lymphocytes (T8 and CD56 +ve NK cells) – mild (cf. liver Tx reject
n
)
BD atypia (incl. stratificat
n
, hyperchromasia, vacuolat
n
and ↑NCR), distort
n
and loss
parenchymal bilirubinostasis without biliary interface activity
r
3
rd
month: BD loss, PT fibrosis, endothelialitis (≈diagnostic if present, in the absence of other causes)
r
Longer term: ± connective tissue plugs in veins, ± 2
◦
biliary cirrhosis (clin./radiol. d/dg SSC)
r
Other BMTx assoc
d
disease: viral hepatitis, transfusion siderosis, VOD, NRH, infection, PTLD
Sepsis and Infections
Sepsis
r
Cholangiolitis lenta: periportal cholangioles dilated with bile plugs with PMN in +/ around them
without suppurative cholangitis = sepsis
with suppurative cholangitis = ascending cholangitis (q.v.) or toxic shock syndrome
r
Any bile plug may be a sign of sepsis, the larger the plug (from canaliculus to portal tract bile duct) the
stronger the association
r
Other features: steatosis, perivenular necrosis, microabscesses, clumps of cocci and PMN
Ascending Cholangitis (Suppurative Cholangitis)
r
2
◦
to obstruct
n
, bacteria, helminthes (Clonorchis, ascarid or schistosomal), opportunistic infect
n
, etc.
r
Affects the smaller (portal tract) bile ducts; large ducts may look normal

JWBK208-12 December 8, 2007 16:4 Char Count= 0
Liver, Biliary Tract and Pancreas 167
r
More PMN (cf. biliary irritation alone) and PMN aggregates within BD walls and lumens
r
± Bacterial colonies ± PT abscesses ± portal pyelephlebitis/thrombosis ± cholangiolitis lenta
r
± Lobular changes: PMN in sinusoids; parenchymal necrosis
Some Specific Causative Organisms
Salmonella (Typhoid)
r
Sinusoid lymphocytosis,
10
Kupffer cell hyperplasia, erythrophagocytosis
r
Granulomas that may necrotise (but no Langhans giant cells)
r
Microvesicular steatosis
Brucella
r
Kupffer cell hyperplasia ± focal hepatocyte necrosis
r
Granulomas (anything from microgranulomas to tuberculoid type)
Coxiella burnetii (Q-Fever)
r
Fibrin-ring granuloma (small, PMN, M, ring of fibrin) are typical but non-specific (see ‘Drugs’)
r
Non-specific granulomas, foci of necrosis, steatosis, inflam
n
and fibrosis ± cirrhosis
Listeria
r
Viral hepatitis-like
r
Microabscesses with Gram +ve rods
r
Granulomas
Francisella tularensis (Tularaemia)
r
Granulomas may be indistinguishable from TB or sarcoid
Bartonella
r
Cat scratch granulomas i.e. irregular shape with periph palisaded M and central PMN/necrosis
r
Bacillary peliosis hepatis is the equivalent to bacillary angiomatosis (see p. 319) and not the bland blood
filled cystic dilatations of ordinary peliosis hepatis (this may also occur with infections, be idiopathic
or be assoc
d
with drugs, cachexia, Tx (liver/renal), asphyxia and tumours)
HIV (and AIDS)
r
May get a mild lobular hepatitis upon seroconversion ± sinusoidal lymphocytosis (d/dg EBV)
r
Children may show a giant cell hepatitis or a GVHD-like picture with lobular and PT lymphocytes
r
Hepatocyte and Kupffer cell Fe (± EMH) is usu. 2
◦
to transfusions/haemolysis
r
Reaction to opportunists may be suppressed and microbes may roam free within the sinusoids .
.
. should
always stain for opportunists (DPAS, ZN ± Grocott/CMV immuno)
r
Peliosis hepatis (ordinary and bacillary types)
r
Tumours: HCC (due to HCV), 1
◦
DLBCL, 2
◦
HL, KS (d/dg bacillary angiomatosis/peliosis), etc.
r
Vide supra for association with HBV/HCV and cholangiopathy; vide infra for drug reactions
Other viruses (EBV, CMV, etc.)
See ‘Acute Hepatitis’ (p. 158) and ‘Infection post Liver Tx’, (p. 166).
Drugs/Iatrogenic
Generalities (with examples)
r
Clin.: usu. subside on removing the drug (or persist if taken for >6 months) & relapse if restarted
r
Eosinophils – but ! these may be present in small N˜os in other things e.g. AIH, HCV, etc.
r
Zone 3 cholestasis alone [‘bland cholestasis’] (anabolic steroids, oral contraceptives, [pregnancy])
r
Cholestatic hepatitis [zone 3 bile, lobular inflam
n
, ±eos] (phenothiazines, Augmentin
R
, erythromycin)
r
Cholestatic acute hepatitis [≈ d/dg HAV-type with necrosis] (halothane, isoniazid )
r
Ascending cholangitis (phenothiazines, allopurinol)
r
Vanishing bile ducts ± PBC-like (flucloxacillin, paraquat, ibuprofen, erythromycin, phenothiazines)
r
SSC (ischaemia, post-op/post liver Tx, intra-arterial floxuridine)
r
Granulomas esp. if atypical, of NST (d/dg idiopathic or 2
◦
to lymphoma) or accompanied by eos. Some
specific types are linked to drugs (e.g. fibrin-ring granuloma with allopurinol d/dg Q-fever, HL, viruses,
CTD, leishmaniasis, Toxoplasma, etc. and lipogranulomas with oral mineral oils – usu. para central
venules cf. d/dg steatohepatitic ones)
r
Chronic hepatitis (-methyldopa, zidovudine-like anti-retrovirals, isoniazid, nitrofurantoin, aspirin)
r
AIH-like, type 1 (ANA +ve, ASMA −ve) (minocycline, -methyldopa)
10
d/dg of lymphocytes in dilated sinusoids include: typhoid, EBV (infectious mononucleosis), HCV, HIV, malaria (tropical
splenomegaly syndrome) and CLL.
JWBK208-12 December 8, 2007 16:4 Char Count= 0
Liver, Biliary Tract and Pancreas 168
r
Macrovesicular steatosis (OH, cortisone, oestrogens, methotrexate)
r
Microvesicular steatosis (i.v. tetracyclines)
r
Mixed steatosis (microvesicular and macrovesicular) ±giant mitochondria (2
◦
to mitochondrial damage
due to OH, valproate, antivirals e.g. zidovudine and Reye’s syndrome initiated by salicylates)
r
NASH (TPN, oestrogens & tamoxifen, nifedipine, didanozine, amiodarone, cortisone)
r
Fibrosis/cirrhosis (OH, vitamin A, methotrexate)
r
Zone 1 necrosis [d/dg PET] (cocaine, phosphorus, ferric sulphate, aflatoxin & other toxins)
r
Zone 2 necrosis [d/dg VHF] (frusemide)
r
Zone 3 necrosis [coagulative necrosis ± ductular prolif
n
] (cocaine, paracetamol – aggravated by OH,
CCl
4
)
r
Veno-occlusive disease (chemo/radioRx, bush teas, OH may cause veno-occlusion)
r
Hepatic vein thrombosis → Budd-Chiari (prolonged progesterone e.g. OCP, pregnancy)
r
Peliosis hepatis (azathioprine, tamoxifen)
r
Siderosis (ribavirin causes haemolysis hepatocyte and Kupffer cell Fe, OH may cause haemolysis)
r
Lamellar inclusion phospholipidosis (co-trimoxazole, amiodarone)
r
Neoplasia (oestrogens, androgens, vinyl chloride monomer, aflatoxin, thorotrast, post-Tx/immuno-
suppression)
Methotrexate
r
Damage ∝ dose, interval, cumulative dose, OH, obesity, diabetes, reason for Rx (psoriasis > RhA)
r
Nuclear hyperchromasia, glycogenation and anisonucleosis
r
Steatosis, ballooning, necrosis
r
Fibrosis → micronodular cirrhosis (cirrhosis is rare with cumulative dose <1.5g)
r
PT show a mixed infiltrate (lymphocytes, M, PMN)
r
Grading is via the classification of Roenigk et al., 1982 – see table 12.2
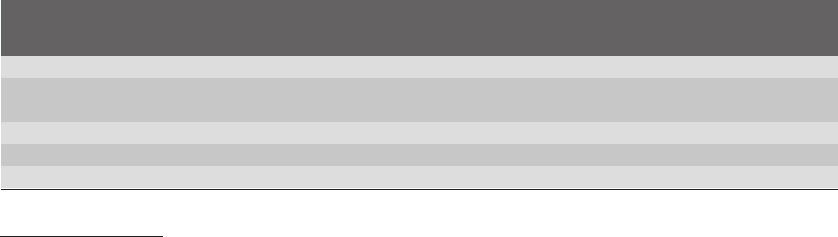
TABLE 12.2 Grading methotrexate liver damage
Nuclear Liver cell Portal
Grade Steatosis variability necrosis inflam
n
Fibrosis
I none/mild mild none mild none
II moderate/ moderate/ moderate/ moderate/ none or mild PT expansion without
severe severe severe severe septa or limiting plate disruption
IIIa any any any any mild with septa
IIIb any any any any moderate to severe with septa
IV any any any any cirrhosis
Vascular Disorders
General Features of Ischaemia
r
Zone 3 accentuated changes ± patchy/sharp demarcation depending on cause
r
Cholestasis, ballooning, hepatocyte atrophy or dropout of hepatocyte clusters
r
If more chronic: perivenular and pericellular fibrosis ± cirrhosis (! d/dg alcohol)
r
If severe and acute: infarction (coagulative ± haemorrhagic necrosis)
Portal Vein Thrombosis
r
Large portal vein (Virchow’s triad: alterat
n
in endothelium/flow/coagulat
n
) e.g. MPD, sepsis, tumour
r
Small portal vein: local PT disease (e.g. cirrhosis, schistosomiasis, hepatitis, PBC, PSC, vasculitis,
sarcoid)
r
Maybe2
◦
to systemic venous HT (e.g. Budd-Chiari syndrome/VOD, CCF)
r
May be idiopathic (small vein obliteration is particularly marked)
r
Veins: large – thromboses/recanalisation; small – obliterat
n
/dilatat
n
(to give ‘ectopic’ PT veins)
r
Acute thrombosis → (pseudo)infarct of Zahn (= a wedge of congest
n
& atrophy) ±↑apoptoses
r
Other: partial atrophy of lobe, partial nodular transformation, NRH or no histological abnormality
r
If portal vein thrombosis extends to occlude splenic vein ostium → venous bowel infarction
Portal Hypertension
r
Many causes or idiopathic, Bx may be normal or show variable anomalies:
r
Perisinusoidal sclerosis, dilated (‘ectopic’) PT veins or fibrotic PT with small, inconspicuous veins
r
Incomplete septal cirrhosis +/ NRH
r
↑ Visibility and dilatation of PT lymphatics
