Tadrous P.J. Diagnostic criteria handbook in histopathology: a surgical pathology vade mecum
Подождите немного. Документ загружается.

JWBK208-11 December 8, 2007 16:3 Char Count= 0
Alimentary Tract 139
r
Grading: UK National Dataset method is based on the most poorly diff. area as:
poorly diff: i.e. diffuse / signet ring / non-cohesive tumours
other: usu. intestinal type / cohesive growth pattern
r
Grading: WHO method is based on the proportion of tumour composed of glands:
well diff: >95%
moderately diff: 50–95%
poorly diff: <50%
r
Types of gastric carcinoma other than typical intestinal-type adenocarcinoma:
signet ring carcinoma (WHO def
n
requires >50% signet ring type)
mucinous carcinoma (WHO def
n
requires >50% mucinous type)
SCC, ASC, SmCC, ChC, carcinosarcoma and spindle cell carcinoma
medullary carcinoma (>50% is poorly diff, lymphoid stroma, lack of fibrous tissue)
anaplastic carcinoma with extensive PMN infiltration
malignant rhabdoid tumour (vimentin +ve)
hepatoid (bile canaliculi & AFP +ve, typical adenocarcinoma foci elsewhere)
metastatic (very rare, may be multiple, usu. submucosal centric and arise by lymphatic or
blood spread from: melanoma, breast, thyroid, testis, lung, oesophagus and elsewhere)
Differential Diagnosis of Signet Ring Carcinoma of Stomach (esp. on Frozen Section)
r
ILC of the breast
r
Signet ring carcinoma from other 1
◦
sites: e.g. prostate, bladder, cholangiocarcinoma, etc.
r
Malakoplakia (variant with non-mineralised PAS +ve bodies), muciphages or xanthelasma
r
Signet ring lymphoma / mesothelioma / melanoma / ovarian stromal tumour / uterine leiomy-
oma/sarcoma / amphicrine MTC, signet ring morphology in CNS tumours (oligodendroglioma and
ependymoma)
Neuroendocrine Pathology of the GIT
r
The following criteria and terms relate to the upper GIT but some apply them in the colon also
r
Hindgut (rectosigmoid) carcinoids are different. They arise in the submucosa, are usu. trabecular and
poor prognostics are: invasion of muscularis propria, size >1 cm (add esp. if >2 cm), lymph/blood
vasc. invasion, tumour ulceration, mitotic count.
r
d/dg includes glomus tumour, paraganglioma and adenocarcinoma
NE cell hyperplasia
r
Def
n
: ↑ numbers of NE cells within a pre-existing gland / crypt:
r
Confined to the mucosa (by definition)
r
May be linear or nodular with nodules no wider than the width of a normal gland / crypt (sometimes
called ‘micronodules’ hence ‘micronodular hyperplasia’)
r
Each nodule surrounded by BM
r
Adenomatoid hyperplasia =≥5 micronodules close to each other with interposed BM
NE Cell Dysplasia (= pre-carcinoid)
r
Fusion of micronodules with loss of intervening BM
r
Micronodules enlarge beyond the size of a normal gland / crypt
r
Total size >0.15 mm but <0.5 mm in max.
r
± Cytological atypia
r
± Microinvasion of the lamina propria
Microcarcinoid (= Tumourlet)
r
Def
n
: NE-proliferation >0.5mm , the upper measurement limit is not defined but it must be confined
to the mucosa and not macroscopically (clinically / endoscopically) visible
Carcinoid
r
Def
n
: a well diff. NE-proliferation >0.5mm which either:
◦
1
invades the muscularis mucosae or
◦
2
is large enough to be macroscopically visible (clinically / endoscopically).
r
The following is a guide to aggressiveness but the terms ‘benign’, ‘borderline’ and ‘malignant’ are best
avoided since all carcinoids are potentially malignant
r
‘Benign’: <1cm , no angioinvasion, tumour limited to mucosa / submucosa
r
‘Borderline’: either
◦
1
<1cm with angioinvasion but limited to mucosa / submucosa or
◦
2
1–2cm, no angioinvasion, limited to mucosa / submucosa

JWBK208-11 December 8, 2007 16:3 Char Count= 0
Alimentary Tract 140
r
Mucinous carcinoid / goblet cell carcinoid: more aggressive cf. other carcinoids and is probably a form
of argyrophil adenocarcinoma (for details, see ‘Appendix’, p. 152)
r
Atypical carcinoid: any of the following:
◦
1
necrosis (usu. punctate, not extensive)
◦
2
mitoses >2/10 hpf
◦
3
cytological atypia (e.g. prominent nucleoli)
r
‘Malignant’: any of the following: functioning tumour (NE peptide effects)
1–2cm with angioinvasion
>2cm without angioinvasion
invades the muscularis propria or beyond
Types of upper GI / gastric carcinoid
r
Any type of carcinoid may have a sub-population of cells expressing any other NE peptide
r
The four main types of NE cell (and tumours) in the stomach / upper GI are:
◦
1
ECL-cell (histamine, 5-HT or no product in carcinoids):
proliferate in response to hypergastrinaemia (any cause)
d/dg EC-cell: ECL-cell is +ve for VMAT-2, CgA, Grimelius; −ve for serotonin and argentaffin
gastric ECL-cell carcinoids occur usu. in the proximal stomach and are typed as:
Type I: assoc
d
with ↑gastrinaemia 2
◦
to chronic atrophic gastritis
usu. multiple, small & arise on a
Type II: assoc
d
with ↑gastrinaemia without atrophy e.g. MEN 1/ZE background of ECL-cell hyperplasia
Type III: sporadic and more likely to be solitary & show features of malignancy / atypia (vide supra)
◦
2
EC-cell (serotonin) tumours occur in the distal duodenum, acinar pattern
◦
3
G-cell (gastrin) proximal duodenum, trabecular, may cause ZE syndrome, ± MEN-1
◦
4
D-cell (somatostatin) → somatostatinoma (50% have NF-1):
periampullary, glandular/acinar pattern, psammoma bodies
immuno/stains: somatostatin +ve, ! CgA / Grimelius may often be negative
d/dg: well diff adenocarcinoma (! esp. on FS) but somatostatinoma has low grade NE nuclei,
low/absent mitoses & somatostatin +ve immuno
Gastrointestinal Stromal Tumour (GIST)
r
Occur in any part of GI tract (and 7% are extra GI: mesenteric ones have worse prog. cf. omental)
r
Spindle cell type:
variable cellularity
interlacing bundles / whorls of uniform spindle cells with blunt nuclei
± paranuclear vacuole
± multinucleated ‘wreath’ cells
± prominent vascularity
± neural features (e.g. palisaded nuclei)
± skeinoid fibres (extracellular globoid / curvilinear collagen aggregates)
stroma may be hyaline or myxoid
± foci of liposarcoma / chondrosarcoma / RMS
r
Epithelioid type:
sheets / nests
rounded / vacuolated / clear / epithelioid / plasmacytoid cells
variable nuclear atypia to (very rarely) frank pleomorphism with large nucleoli
± multinucleated tumour cells
thought to have worse prognosis cf. spindle type but is indolent if part of Carney triad
8
r
Gastrointestinal autonomic nerve tumour (GANT):
a non-myogenic GIST of either spindle / epithelioid type
diagnosis depends on ultrastructural features (processes, synapses, vesicles, etc.)
often has peritumoural lymphoid infiltrates (similar to some deep Schwannomas)
possibly worse prog. cf. other GISTs but no longer necessary to separate out this sub-type
r
Immuno +ve: c-kit (membrane accentuation), DOG-1 (useful for CD117 −ve GIST – some of these
also respond to Glivec
R
), CD34, CD171 (in 75%); nestin, (± neural +/ smooth muscle markers),
PDGFR (as for DOG-1 but also +ve in 25% of desmoids)
8
Carney triad =
◦
1
epithelioid GIST,
◦
2
pulmonary chondroma and
◦
3
non-adrenal paraganglioma
JWBK208-11 December 8, 2007 16:3 Char Count= 0
Alimentary Tract 141
r
d/dg (c-kit [CD117] is +ve in many things – see also p. 16 – do not use Ag retrieval):
leiomyoma / sarcoma: c-kit −ve, CD171 −ve, desmin +ve,ERmaybe+ve (−ve in GIST)
cellular Schwannoma of the GIT
9
/ MPNST: c-kit −ve, S100 +ve; nestin & CD171 rarely +ve
fibromatosis: c-kit +ve (but with cytoplasmic blob [myofibroblast] pattern not membranous),
PDGFR ±ve, CD171 & CD34 −ve; (! don’t mis-call a post-op desmoid ‘recurrent GIST’)
inflammatory fibroid polyp: CD34 +ve (like GIST), eosinophils (see p. 138)
SFT: triad of CD99, Bcl-2, CD34 +ve; some are also c-kit +ve (see p. 324)
spindle cell carcinoma and mesothelioma: CK +ve (rare in GISTs) and −ve for c-kit and CD34
glomus tumour (vs. epithelioid GIST) – see pp. 285–286
r
Prognosis (NB: it is good practice never to report a GIST as ‘benign’):
good prognostics are: spindle type with only smooth muscle markers
any type with only neural markers
<1cmand incidental finding (these may be truly benign)
gastric or omental site
bad prognostics are: frank invasion (= malignant, whatever the mitotic count / size)
recurrence after Rx: abdominal cavity and liver commonest sites
pleomorphism is irrelevant to prognosis in epithelioid tumours
grading ∝ size and mitotic count but SI GISTs may be more aggressive for any given size
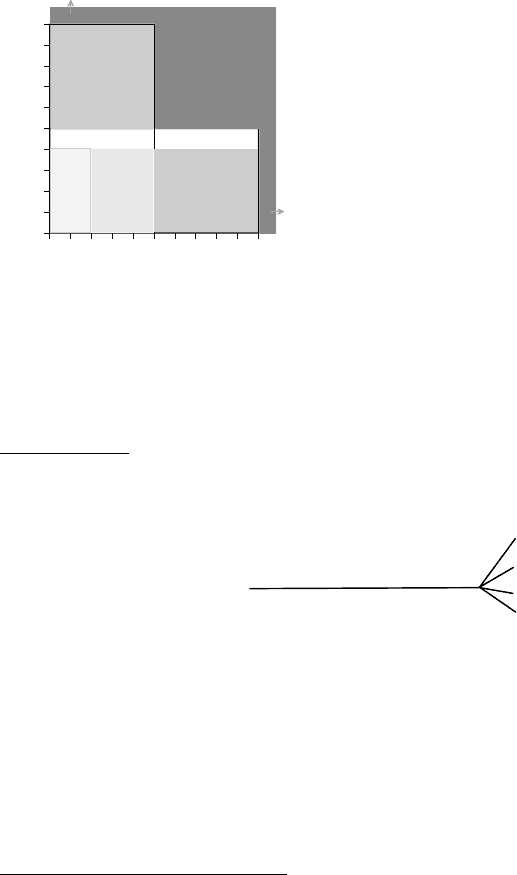
any tumour >10cm or with >10/50 hpf mitoses is high risk (see Figure 11.2)
if it has >20–50 mitoses / 50 hpf it is considered very high grade
(< 5 cm)
(< 2cm)
0510
0
5
10
2
4
very
low
low
intermediate
intermediate
high
Mitotic Count (per 50 hpf)
Size of maximum dimension (cm)
FIGURE 11.2 GIST risk groups.
Based on Fletcher et al. 2002 and Wong
et al. 2003.
Lymphoma
See also Chapter 10: Lymphoreticular.
r
A solid swathe of lymphocytes covering the whole Bx suggests
lymphoma (but it may be more subtle)
r
MALToma: low grade is assoc
d
with H. pylori and may respond
to antibiotics (high grade = DLBCL)
r
An LEL is defined as a group of ≥3 IELs with destruction of
epithelium (CK immuno may help e.g. CAM5.2; also T & B
to demonstrate B-cells [unlike the T-cells of focally enhanced
gastritis])
r
True LEL may also be seen in severe chronic gastritis not just
MALToma
r
CD20 immuno may fail (false −ve) if patient previously Rx
with anti-CD20 Ab .
.
. use CD79a
r
If a post-Rx Bx shows dense diffuse or nodular infiltrates or H. pylori then further Rx is indicated
r
d/dg includes glomus tumour in the stomach (see pp. 285–286)
Small Intestine
Causes of Malabsorption
r
Flora: blind loops / diverticula
r
Intestinal: sprues (incl. coeliac disease) bacterial (MAI, Tropheryma whippelii)
radiation viral
infection protozoal (Giardia lamblia)
lymphoma / amyloid (e.g. Waldenstr¨om) helminthic (Diphylobothrium latum)
drugs including chemoRx
r
Digestion: pancreatic, gastric and biliary diseases
r
Lymphatic obstruction: lymphangiectasis and LN pathology
r
Endocrine disorders: Addison’s pernicious anaemia (PA), thyroid, DM
r
Short gut syndromes: resections, fistulous short circuit
r
Biochemical: IEM (e.g. disaccharidase deficiencies and abetalipoproteinaemia)
r
Vascular insufficiency of the gut
r
NB: to diagnose crypt atrophyone should see ≥4 villi in a row(this gives assurance of proper orientation)
and to exclude patchy disease (e.g. some cases of Coeliac) you need ≥ 3–5 Bx
9
not encapsulated like other Schwannomas and may have peritumoural lymphoid infiltrates / follicles

JWBK208-11 December 8, 2007 16:3 Char Count= 0
Alimentary Tract 142
Villous Atrophy of the Crypt Hyperplastic Type
Coeliac disease
r
Clin: +ve serology for anti tTG Abs is more specific cf. anti gliadin (both are unreliable if <2 years
old)
r
Some cases show nearly normal villous architecture, however these have a greater concentration of
IELs near the tip of the villi cf. the base (i.e. loss or reverse of the normal gradient of IELs)
r
IELs are usu. > 30-40 / 100 villous (not crypt) enterocytes in established coeliac disease
r
↑ l.p. chronic inflam
y
cells (esp. plasma cells); ↓ height of enterocytes and brush border ±vacuolation
r
d/dg acute (HLO-assoc
d
or peptic) duodenitis: ↑PMN, gastric metaplasia
10
++, HLO (hard to identify
in small bowel because they are fewer and more coccoid)
r
d/dg refractory coeliac disease – see p. 115; for other d/dg vide infra
Other causes
r
Tropical sprue: also affects the TI villi (unlike coeliac disease) in the later stages of the condition
r
HIV enteritis (also has ↑ crypt apoptoses)
r
Iatrogenic: drugs (e.g. mefenamic acid, NSAID), radioRx, post surgical blind loops, etc.
r
↑ IELs in other immune diseases (CVID, SLE, allergies, GVHD, CIBD), infections, ischaemia, etc.
Villous Atrophy of the Crypt Atrophic Type
r
Chemo/radioRx (chemoRx causes ↑crypt apoptoses, radiation-induced villous atrophy is a transient
event) – see p. 148 for other morphological features of chemo/radioRx
r
Folate & vitamin B12 deficiency
r
Prolonged TPN
r
Drugs e.g. progestagens, NSAID
r
HIV enteritis (also has ↑ crypt apoptoses)
Whipple’s Disease
r
M F; middle-age; usu. diffuse but can be patchy and submucosal after antibiotics
r
l.p. packed with M with intensely DPAS +ve coarse granules (but may be Gaucher-like after Rx)
r
Villi show large lipid vacuoles in the l.p. (dilated lacteals)
r
Stains: EM +/ immuno for T. whippelii;ZN−ve (d/dg MAI has ZN +ve fine rods)
Drug Reactions (incl. NSAID)
r
Vacuolation of villous tip enterocytes (d/dg coeliac / infections)
r
Atrophy of villi (crypt hyperplastic or atrophic) and apoptoses in crypts (with chemoRx)
r
Chronic inflam
n
(incl. eosinophils)
r
Ulceration which may be transverse peptic-like, pseudomembranes (if extensive), ± perforation
r
Diaphragm disease: the diaphragms contain submucosa but not muscularis propria and they have
mucosal prolapse changes [± ulcerat
n
] and submucosal fibrosis at the diaphragm aperture
Common Variable Immunodeficiency (CVID)
r
Lack of plasma cells in l.p., ± villous atrophy, ± Giardia, CMV, Candida, etc., ± MALToma
r
Nodular lymphoid hyperplasia ± granulomas
For more details, see p. 351.
Brunner’s Gland Hyperplasia, Nodule(s) and Adenoma
r
↑Amount of normal lobulated Brunner’s gland tissue with intervening slips of smooth muscle
r
The difference between these entities is an arbitrary matter of size/amount of glands
Lymphoma
See also Chapter 10: Lymphoreticular.
r
Small intestinal MALToma:
LEL are less prominent & DLBCL transformation more common (cf. gastric)
multifocality and stage are important prognostics
solid sheets of blasts = DLBCL (Bcl-2 & p53 may be prognostic)
r
Others: EATL, IPSID, EBV-assoc
d
high grade B-cell (HIV / PTLD), Burkitt’s, FCL
10
in general, anywhere in the alimentary tract, heterotopias are distinguished from metaplasias by the presence of gastric parietal or
chief cells or pancreatic acinar cells or adrenocortical cells

JWBK208-11 December 8, 2007 16:3 Char Count= 0
Alimentary Tract 143
Post-Colectomy Ileitis (= Pre-stomal ileitis or Neoterminal ileitis)
r
Occurs months to years post colonic surgery (for UC, colonic carcinoma or other causes), FM
r
Wall thickening ± stricture
r
Patchy variable acute and chronic inflam
n
± ulcerat
n
, fissures and TLA but no granulomas or bugs
r
d/dg Crohn’s disease: but in post-colectomy ileitis there is a history of colectomy, CPC and review
of past specimens confirms UC or show no evidence of Crohn’s, granulomas are absent and TLA are
limited to areas of deep mucosal fissuring/activity
CIBD
r
Duodenum: focal aggregates of PMN in the l.p. and epithelium may be the only sign in Crohn’s
r
TI: patchy active inflam
n
and UACL are typical of Crohn’s and strongly favour Crohn’s over UC
r
TI: the ‘backwash ileitis’ of UC occurs with right-sided UC and shows diffuse superficial activity (no
erosions or deep ulcers and no UACL) – it is not a contraindication to the formation of a pouch.
Lower GI
Infective Colitis
General bacterial colitis
r
Oedema
r
Mild to moderate inflammation, PMN dominant
r
Inflammation tends to be more superficial in the mucosa and surface epithelium
r
Cryptitis with preserved architecture (except amoebic colitis)
r
Beaded crypt absceses (‘string of pearls’ sign)
r
Crypt withering (also seen in radioRx effect and ischaemia)
r
Microgranulomas (≥ 5M) away from inflamed crypts – esp. in Salmonella / Campylobacter
r
Haemorrhage
r
Tufting of surface epithelium (may be antibiotic-related)
r
Resolution (i.e. it goes away on F/U)
Entamoeba Histolytica
r
Crypt distortion
r
‘Flask-shaped’ ulcers (have overhanging edges)
r
Amoebae have pale-staining spherical nuclei (unlike M nuclei that are darker and bean-shaped)
r
Amoebae have engulfed RBC (unlike non-pathogenic Entamoeba coli)
r
Amoebae stain magenta with DPAS – sensitive method to detect them – and are CD68 –ve
r
d/dg carcinoma (macro / radiology) and UC (histology)
Clostridium difficile
11
(Pseudomembranous Colitis)
r
Multiple discrete foci of disrupted crypts
r
Affected crypts are dilated superficially
r
A ‘volcanic spray’-like exudate forms a ‘mushroom cloud’ pseudomembrane of cellular debris, fibrin,
mucus and inflam
y
cells (! similar exudate can occur in SRUS – need to see underlying mucosa)
r
Intervening mucosa is normal
r
d/dg ischaemic colitis, severe CIBD / defunctioned UC, CMV, Shigella, E. coli, (rarely) acute CC
r
d/dg PMC may also be caused by drugs, e.g. gold, not just antibiotic-assoc
d
C. difficile infection
Chronic idiopathic Inflammatory Bowel Disease (CIBD)
Common pitfalls in diagnosis
r
Pericryptal cells (pseudogranulomas)
r
Muciphage collections (pseudogranulomas)
r
Cryptolytic lesions (foreign-body-type granuloma adjacent to a crypt that has spilled its mucin) seen in:
UC, diversion colitis, pouchitis, diverticular disease-assoc
d
colitis, etc.; usu. in superficial l.p.
r
Isolated crypt abscesses (can be seen adjacent to focal lesions / other situations)
r
Branching crypts (seen at normal innominate grooves and in any situation of regeneration / growth)
r
Normal chronic ‘inflam
n
’ and NE cells of the caecum; normal rectal NE cells (vs. NE cell hyperplasia)
r
‘Atrophy’ at the anorectal margin (normal histology)
r
Infective colitis (esp. amoebic / CMV)
11
NB: difficile is a Latin word of four syllables (di-fi-chi-lay) – not French
JWBK208-11 December 8, 2007 16:3 Char Count= 0
Alimentary Tract 144
r
Ischaemic colitis
r
Beh¸cet’s, peritumoural and diverticular disease-associated colitis (esp. d/dg Crohn’s disease)
r
Post-colectomy ileitis (!do not call it Crohn’s disease in a patient with established UC) – see p. 143
r
Diversion reaction / colitis
r
Ileoanal pouch changes
r
Drug-induced colitis e.g. bowel prep colitis (esp. d/dg Crohn’s) or cholestyramine / polystyrene
colitis
r
Failure to correlate clinical information and macroscopic appearances / distribution with histology
Per-operative diagnosis of CIBD (incl. FS)
r
Used during some ileoanal pouch-forming procedures because Crohn’s disease is a contra-indication
r
Determine: Crohn’s disease / UC / don’t know (not ‘indeterminate colitis’ q.v.)
r
Macro appearances at surgery helps (see macro features of Crohn’s disease and UC, below)
r
FS from: the largest LN – granulomas? (be wary of pitfalls and acceptable criteria)
full-thickness lesional bowel – characteristic features present?
full-thickness ‘normal’ interlesional bowel – is disease truly patchy?
Ulcerative Colitis (UC)
r
Macro: diffuse involvement of diseased colon from distal to proximal (± backwash ileitis)
specific skip lesions can occur (appendix & caecal patch) ± rectal sparing if treated
r
Micro (mucosal):
crypt distortion (!beware of nearby causes e.g. ulcers, lymphoid aggregates, innominate
grooves)
surface villosity
chronic inflam
n
: diffuse throughout the full thickness of the mucosa and length of the Bx and
continuous throughout the involved segment (except with the UC skip lesions vide supra);
tends to be worse distally
acute activity (PMN in the 1.p [esp. if >100 per mm] / cryptitis / crypt abscesses): this is
diffuse but patchiness can occur
◦
1
at the junction of involved and uninvolved bowel and
◦
2
in
cases of treated UC
mucin depletion (associated with activity, weak feature)
cryptolytic granulomas and muciphage collections may be seen in UC
quiescent UC: the lamina propria may be hypocellular
distortion and atrophy (crypt bases do not reach the m.m.)
NE cell hyperplasia and Paneth cell metaplasia
patchiness of disease severity is OK for UC (as opposed to patchiness of disease presence in
Crohn’s) as not all sites may be at the same degree of severity of inflam
n
. Finding quiescent
UC in between two active biopsies is OK. Finding completely normal bowel in between two
diseased biopsies is not (consider Crohn’s or other d/dg, however, fulminant UC may be patchy
with rectal sparing)
the rectal mucosa in UC may return to histological normality esp. after Rx .
.
. a normal rectal
Bx does not exclude UC
r
Micro (transmural / resection): diffuse inflammation can occur transmurally at sites of ulceration
Crohn’s disease
r
Macro: SI involvement ± colon favours Crohn’s (but isolated Crohn’s colitis is possible)
fat-wrapping, serosal exudate, thickening of bowel wall, strictures, fistulae
skip lesions, fissures, snail-track ulcers, cobblestone mucosa, etc.
Abnormalities are worst on the mesenteric aspect
r
Micro (mucosal Bx ± submucosa):
there is less crypt distortion and less mucin depletion (cf. UC)
patchiness of inflam
n
– both acute and chronic, both within and between biopsies, esp. sin-
gle crypt abscesses flanked by normal crypts. Completely normal intervening biopsies in a
series
epithelioid granulomas, esp. when multiple, small (<200), between crypts and abutting the
muscularis mucosae (d/dg infective microgranulomas, cryptolytic lesions, pseudogranulomas)
patchy lamina propria fibrosis and oedema (d/dg ischaemia which is favoured by mucosal
capillary telangiectasia and siderophages – but these are not always seen)
disproportionate submucosal inflam
n
(not assoc
d
with an ulcer)
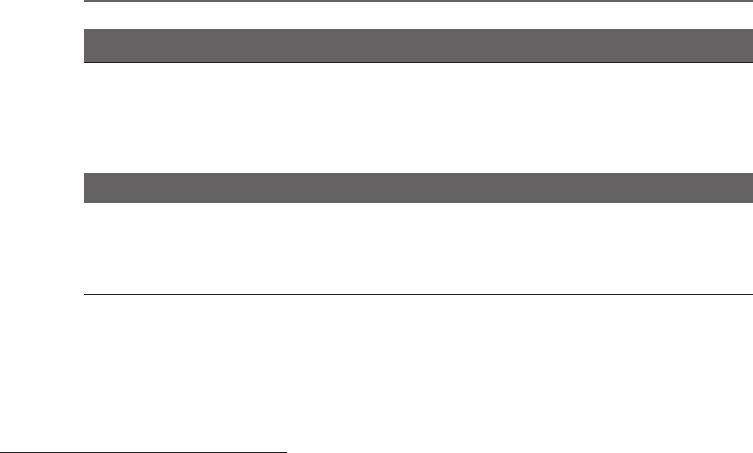
the typical Crohn’s aphtha begins at the crypt base as a triangular (‘mountain-top’) ulcer
pointing upwards sending a stream of PMN up the crypt and often overlying a lymphoid

JWBK208-11 December 8, 2007 16:3 Char Count= 0
Alimentary Tract 145
aggregate (see Figure 11.3). Fissures
develop as continuations of the angles
at the base of the ulcer. The adjacent
mucosa is normal. It is useful in d/dg
UC but is not specific for Crohn’s.
r
Micro (transmural / resection):
inflam
n
is transmural with patchy dis-
crete lymphoid aggregates, seen esp.
running along serosa
granulomas (following lymphatics) are
found in two-thirds of cases; ± granulo-
matous lymphovasculitis
fibrosis and oedema (±submucosal lym-
phangiectasia & neuronal hyperplasia –
not seen in UC – ± perineural chronic
inflam
n
)
deep fissures (esp. if narrow, lined by
inflam
n
and arising from the base of
Crohn’s-like aphthae)
well-formed, sarcoid-like epithelioid
granulomas in draining lymph nodes
help establish the diagnosis esp. in per-
operative frozen section
r
d/dg TB is favoured by confluent granulomas,
caseous necrosis or ≥10 granulomas per Bx
r
d/dg Crohn’s-like reaction (macro & micro) lim-
ited to a DD segment or peritumoural
r
d/dg idiopathic granulomatous appendicitis: only the appendix is affected, no other signs of Crohn’s
r
d/dg Beh¸cet’s colitis: deep/perforating ileocaecal ulcers or colitis histologically identical to Crohn’s
r
d/dg focal inflam
n
may occur in inflam
y
polyps or anastomotic lines and does not favour Crohn’s
FIGURE 11.3 Crohn’s aphtha
Indeterminate Colitis (IC)
r
Only diagnose when small bowel disease has been excluded clinically and whole colon sampling is
available (colectomy or multiple biopsies)
r
Using CPC and Bx findings try to qualify IC with a probable aetiology: UC, Crohn’s (subserosal
lymphoid aggregates unrelated to ulcers or gross skip lesions), other (e.g. infective / obstructive),
unknown
r
IC should be considered a temporary diagnosis pending F/U whenever possible
Acute type IC
r
A confident pre-op Bx diagnosis of UC should not be overruled by indeterminate resection findings
r
Macro: usu. acute severe segmental colitis affecting the middle 1/3 of the colon
ulceration ± extensive denudation ± toxic megacolon
± transverse fissures
r
Micro:
non-cryptolytic/non-foreign-body granulomas exclude IC (esp. if beyond the mucosa)
undermining ulcers with adjacent mucosa showing normal / minimal architectural or inflam-
matory response (pronounced and diffuse architectural distortion favours UC)
fissuresmaybe transmural but are ‘V’-shaped (cf. thinner in Crohn’s disease) and showminimal
adjacent inflam
n
(more prominent in Crohn’s)
myocytolysis with capillary engorgement in parafissural muscularis propria
transmural inflam
n
is diffuse (cf. aggregates in Crohn’s) and restricted to areas of severe
ulceration
Non-acute type IC
r
A confident endoscopic / pre-op Bx diagnosis should not be overruled by subsequent IC findings
r
Micro (if normal colonoscopy): abnormalities not sufficient for diagnosis of microscopic colitis
r
Micro (if abnormal colonoscopy): features not diagnostic of a specific colitis e.g. UC, Crohn’s, drugs,
ischaemia, infection, diverticular disease-assoc
d
colitis, etc.
r
d/dg non-specific colitis (vide infra)
JWBK208-11 December 8, 2007 16:3 Char Count= 0
Alimentary Tract 146
Non-Specific Colitis and Focal Active Colitis
r
Only diagnose non-specific chronic colitis if:
you can’t suggest even a probable aetiology and
features similar to IC (Non-Acute) but IC is not diagnosable due to limited sampling
r
Diagnosis should come with a recommendation for F/U or further investigation
r
Focal active inflam
n
with no other abnormality (= focal active colitis), incl. no evidence of chronicity
(unlike non-specific colitis) is also non-specific and may be due to infection, drugs, ischaemia, etc.
Microscopic Colitis (Lymphocytic Colitis [LC] / Collagenous Colitis [CC])
r
Prolonged watery diarrhoea with (nearly) normal endoscopy. Assoc
d
with coeliac disease
r
Transverse colon (cf. sigmoid) may be the most sensitive Bx site for diagnostic features
r
Lymphoplasmacytic infiltrate of the lamina propria
r
Epithelial damage (flattening, detachment, ↑lymphocytes (≥20 per 100 enterocytes in LC)
r
Collagen band (strands parallel to the lumen, 7–90 thick, may contain vessels) – in CC only (! may
also get collagen band in other things e.g. metaplastic polyps – so use multiple criteria, as usual)
r
PMN may be seen in LC / CC (some say that mild crypt distortion is also allowed)
r
d/dg PMC vs. severe acute CC (quite rare, use CPC)
r
d/dg amyloidosis vs. CC: surface epithelial damage in CC; CR +vity & CPC in amyloid
Diverticular Disease-Associated Colitis
r
Four main types occur (possibly together):
◦
1
lumenal narrowing → obstructive colitis proximal to the diverticular disease (DD) segment
◦
2
impacted stools → localised ischaemia (= crescentic fold colitis)
◦
3
more diffuse inflam
n
affects the whole DD segment – segmental colitis
◦
4
redundant fold prolapse → inflammatory myoglandular polyp-like change (≈ ‘cap polyp’)
r
Mild forms of crescentic fold and segmental colitis show: mild diffuse chronic inflammation
surface pus / erosions
normal architecture
r
Severe forms can mimic CIBD with gland distortion, crypt abscesses, TLA, etc.
r
d/dg CIBD:
DD colitis tends to be around the mouths of the diverticula, sparing the intervening mucosa
UC or Crohn’s affecting only the sigmoid is unusual
TLA in DD colitis tend to radiate out from an affected diverticulum unlike Crohn’s
Obstructive Colitis
r
Varies from mild superficial ulceration to severe (resembling indeterminate colitis)
r
Haemorrhage and congestion in adjacent mucosa
r
The 2–3cm of mucosa immediately proximal to the obstruction is spared
Ischaemia
r
Acute changes include ulceration and haemorrhagic necrosis starting with the most superficial layers
of the mucosa (earliest changes) to deeper (with more prolonged / severe ischaemia)
r
Long term ischaemia: stromal haemosiderosis and changes similar to d/dg chronic radiation enteritis
(q.v.) but without the atypical stromal fibroblasts and vessel wall damage
Amyloid
r
Usu. 2
◦
(to Crohn’s, RhA, etc.)
r
d/dg collagenous colitis (vide supra): lack of surface epithelial cell damage goes against CC
r
d/dg collagen in systemic sclerosis / myopathies in the muscularis propria (do CR / SAP immuno)
Endometriosis
r
Endometrial glands and stroma (do CD10 if necessary) – unlike d/dg colonic carcinoma
r
May infiltrate all layers the bowel wall
r
May give radiological and clinical features suggestive of malignancy
r
! d/dg carcinoma – overcalling endometriosis as carcinoma is the main danger
r
d/dg SRUS
r
d/dg colitis cystica profunda (but endometrial glands are not mucinous)
JWBK208-11 December 8, 2007 16:3 Char Count= 0
Alimentary Tract 147
r
d/dg Crohn’s (clinically, due to adhesions, deformity and fibrosis with PR bleeding of endometriosis)
r
d/dg ischaemia (due to intermittent bleeding and pain and fibrosis with haemosiderin on histology)
Diversion Proctocolitis
r
Lymphoid hyperplasia and diffuse chronic inflammation = diversion reaction
r
+ Aphthae and acute inflammation = diversion colitis
r
Lumenal narrowing and thickening of the submucosa and muscularis propria
do not imply
r
± Occ. well-formed mucosal epithelioid granulomas (controversial) Crohn’s
r
Microcarcinoids
r
Involution (if severe may preclude re-anastomosis):
excessive adipose infiltration of submucosa and muscularis propria
mucosal atrophy
r
Normal architecture unless prior CIBD
r
UC / indeterminate colitis:
(get worse after diversion)
transmural lymphoid aggregates .
.
. a diagnosis of Crohn’s must not
fissures
be based solely on the histology
granulomas (incl. in LN) of the defunctioned rectum
pseudomembranous colitis (PMC)
r
Crohn’s disease:
(gets better)
↑ fibrosis
granulomas hyalinase (± Schaumann bodies)
Ileal Reservoirs and Pouchitis (= Chronic Relapsing Acute Pouchitis)
r
↑Chronic inflam
n
& a degree of crypt hyperplastic villous atrophy is normal but
r
Subtotal villous atrophy (colonization
12
= Type C mucosa) is a minor risk factor for dysplasia →F/U
r
Active pouchitis clinical: diarrhoea, blood, pain, contact bleeding on endoscopy
r
Active pouchitis histol.: acute inflammation, surface erosion and focal superficial ulceration – UC-like
r
d/dg exclude: infection, prolapse, ischaemia (i.e. ischaemia as a 1
◦
cause of the pathology [e.g. due to
surgical complications])
r
d/dg Crohn’s disease:
any single feature of Crohn’s may be present in the pouch without Crohn’s being the cause
of it:
granulomas (esp. in lymphoid follicles) – but granulomas in SI beyond the pouch
favour Crohn’s
vertical fissures (usu. seen in relation to ruptured deep crypt abscesses / anastomoses)
fistulae (e.g. colovesical)
.
.
. a first diagnosis of Crohn’s should never be made on pouch histology alone
r
St Mark’s pouchitis score (score acute and chronic features separately) – based on Shepherd et al.
(1987) – see table 11.1:
TABLE 11.1 St Mark’s pouchitis score
Acute: (add PMN and ulceration scores to get a total score out of 6)
Score PMN Infiltrate Ulceration
0 absent absent
1 (mild) restricted to surface epithelium and focal
*
superficial
2 (moderate) + crypt abscesses (occasional)
3 (severe) + crypt abscesses (numerous) widespread & deeper
Chronic: (add chronic inflammatory cell and atrophy scores to get a total score out of 6)
Score Cellular Infiltrate Villous Atrophy
0 normal normal architecture
1 (mild) focal minor anomalies
2 (moderate) partial
3 (severe) more extensive subtotal
∗
‘restricted to surface epithelium’ includes cryptitis
Melanosis Coli (Pseudomelanosis)
r
Lipofuscin 2
◦
to chronic apoptosis
r
Anthraquinones, NSAID, etc.
r
d/dg haemosiderosis (ischaemia) and brown bowel syndrome (muscle)
12
‘colonization’ (colonic phenotypic change) also connotes a change in mucin type to colonic
JWBK208-11 December 8, 2007 16:3 Char Count= 0
Alimentary Tract 148
Drug Reactions (incl. NSAID)
r
PMC or acute self limiting colitis (e.g. with antibiotics)
r
Ulceration ± superficial PMN infiltrates
r
Melanosis / Microscopic colitis
r
Ischaemia (incl. stricture & diaphragm disease)
r
Crypt apoptoses
r
Eosinophil infiltrates
r
Specifics: Bowel Prep Colitis: focal proximal active colitis (d/dg Crohn’s)
Cholestyramine or Polystyrene sulphonate: can mimic CIBD (ZN +ve crystals)
Barium Granuloma: blue-grey / light green ‘foamy’ Mφ with birefringent crystals
(stain red with rhodizonate – as does Pb, Zn, Sr and Hg)
Chemotherapy / Radiation
r
NB: vitamin B12 / folate deficiency show similar cytological atypia to chemoRx changes
Early changes
r
Ulceration and mucosal necrosis
r
Apoptoses
r
Epithelial cells may show a syncytial-like appearance
r
Marked cell enlargement with nuclear atypia d/dg dysplasia / carcinoma:
gland architecture is preserved
nuclear abnormalities too bizarre for neoplasia forming such good glands
NCR not markedly increased (esp. given degree of nuclear atypia)
cytological atypia also present in surrounding endothelial and stromal cells
no mitoses (except in normal numbers and in their normal locations)
no infiltrative growth
Later changes
r
Chronic ulceration
r
Fibrosis / stricture / adhesions
d/dg Crohn’s disease (! in this regard note that there have
r
± Chronic inflam
n
in lamina propria been case reports of radiation-assoc
d
granulomas)
r
Hyaline fibrosis of the lamina propria
r
Crypt loss (and ‘withering’) with single large dark crypts standing out (regenerative hyperplasia)
r
Radiation fibroblasts (plump, vesicular nuclei, binucleate forms, etc.)
r
Colitis cystica profunda is also assoc
d
with radioRx
r
Vascular changes: ectatic capillaries, endarteritis obliterans, foamy M accumulation with hyaline
change in vessel walls
Squamous Metaplasia in the Rectum (causes)
r
Upgrowth from the anus 2
◦
to distal rectal ulceration
r
Repeated self-induced trauma by insertion of foreign objects
r
Radiation-induced
r
Persistent chronic inflammation (e.g. in UC)
Common Variable Immunodeficiency (CVID)
r
Lack of plasma cells in l.p., ± Cryptosporidia, etc., ± MALToma
r
± Nodular lymphoid hyperplasia ± granulomas. See p. 351 for more detail.
Graft vs. Host Disease (GVHD)
r
In the first 3 weeks post BMTx it is impossible to differentiate from pre-BMTx chemoRx changes
r
Apoptoses in basal enterocytes, chronic inflammatory cells are few
r
± More extensive necrosis and ulceration and PMN
r
Crypt loss with NE gravestones and regenerative crypt distortion
r
Fibrosis of lamina propria (helps to distinguish from d/dg UC) ± transmural fibrosis
r
d/dg: ↑apoptoses of crypts is also seen in HIV, CMV, drugs / viruses, chemoRx, radioRx
Angiodysplasia (of Upper or Lower GIT)
r
Ectatic veins in the submucosa (may extend through to subserosa and become conglomerated)
r
Communicate with ectatic capillaries in l.p. (not always seen but diagnose with caution if not seen)
r
Arterial component seen if severe (but diagnosis should not be made in those with angiomas)
r
Bleeds are assoc
d
with age, true diverticula (those with all muscle coats), aortic stenosis, etc.
